Abstract
Most American women become aware of pregnancy ~3–7 weeks after conceptive sex, and all must seek testing to confirm their pregnant status. The delay between conceptive sex and pregnancy awareness is often a time in which contraindicated behaviors take place. However, there is long standing evidence that passive, early pregnancy detection may be possible using body temperature. To address this possibility, we analyzed 30 individuals’ continuous distal body temperature (DBT) in the 180 days surrounding self-reported conceptive sex in comparison to self-reported pregnancy confirmation. Features of DBT nightly maxima changed rapidly following conceptive sex, reaching uniquely elevated values after a median of 5.5 ± 3.5 days, whereas individuals reported a positive pregnancy test result at a median of 14.5 ± 4.2 days. Together, we were able to generate a retrospective, hypothetical alert a median of 9 ± 3.9 days prior to the date at which individuals received a positive pregnancy test. Continuous temperature-derived features can provide early, passive indication of pregnancy onset. We propose these features for testing and refinement in clinical settings, and for exploration in large, diverse cohorts. The development of pregnancy detection using DBT may reduce the delay from conception to awareness and increase the agency of pregnant individuals.
Author summary
Pregnancy impacts everyone, and is of major psychological importance to most. Early detection of pregnancy onset could be a major boon to women seeking to plan for the future and adjust their behavior (e.g. cessation of alcohol or drug use). At present, most women become aware of their pregnancy well after implantation, and support is often limited to periodic check-ups. Given the emergence of tools that allow for continuous monitoring of physiology (i.e. wearable devices), we feel that utilizing such tools could lead to rapid progress in developing safe, personalized insights across a woman’s fertility journey. Our work here does not aim to solve this problem, but to inspire others to appreciate the reality of this opportunity, and to consider using these tools to expand our understanding and assessment of pregnancy and related events.
Introduction
Why is early pregnancy detection needed?
Automated, early pregnancy detection may substantially improve maternal and fetal health. Although population reports of pregnancy testing behavior are sparse [1–3], available cohorts indicate that most American women confirm pregnancy about 3 to 5 weeks after conception, and that nearly a quarter do so later than 5 weeks [1]. The cost of delayed pregnancy awareness is great: adoption of appropriate pregnancy habits is delayed [4,5] in the earliest, most fragile developmental window [6–9]. Moreover, unplanned pregnancy occurs at a rate of ~50% [10–13], and is associated with higher likelihood of adverse exposures [4,5,14,15], increased maternal morbidity and mortality [16,17], preterm birth and low childhood weight [18–21], elevated risk of birth defects [22,23], and poorer maternal psychological health [24,25]. As the effective window for emergency contraception is ~120 h at most [26–29], and as access to pregnancy testing and safe abortion access continues to be limited around the world [16,30], delayed confirmation poses considerable risks to pregnant individuals [16,17]. Early, passive pregnancy detection could increase the agency of a pregnant individual, speed adoption of pregnancy-safe behaviors (e.g., avoidance of environmental risk factors [7], cessation of alcohol consumption [8,31] or drug use [32]), or provide the choice to discontinue a pregnancy at an earlier gestational age [33].
What is the current state of pregnancy detection?
The development of automated tools has been limited by our low temporal resolution understanding of somatic changes in early pregnancy, and an historical reliance on single time-point hormone samples. Current clinical or over-the-counter (OTC) pregnancy tests rely on serum or urine measurements of human chorionic gonadotropin (hCG), and claim to detect elevated hCG with 99% accuracy at approximately the date of missed menses [34]. However, independent studies place most at-home test kit accuracies far lower, even weeks after missed menses [34–37]. Additionally, as pregnancy test efficacy is measured in days relative to expected missed period (i.e., about 12–17 days after conception [38]), the number of days post-conception that a test becomes accurate is both difficult to estimate [38] and likely more variable for the ~1/3 of women with irregular or long menstrual cycles [39]. Although OTC testing provides a potentially early indicator, most individuals who seek testing do not do so until weeks after a positive test may be obtained [1–3]. For unplanned pregnancies, this delay may be even more prolonged.
Why do we suspect that temperature can advance pregnancy testing?
There is evidence to suggest that passively measurable outputs with direct mechanistic ties to female reproductive physiology, such as continuous body temperature, could advance pregnancy testing [40,41]. A growing number of wearable sensors offer non-invasive, continuous body temperature measures [40,42–44]. Such timeseries, if appropriately measured and analyzed [42,45,46], provide a window onto reproductive events with great temporal granularity, and create an opportunity for precise mapping of patterns of change in pregnancy [40].
Elevation of basal body temperature (BBT) during pregnancy, and its putative relationship to progesterone, has been recognized for about a century [47–68]. However, BBT has proven too imprecise and difficult to collect for development as a reliable method of either pre-ovulatory luteinizing hormone surge [69–71], ovulation [70–74], or early pregnancy detection [75–78]. Despite this, community groups [79] frequently adapt BBT-based methods of ovulatory cycle tracking (i.e., the sympto-thermal method) in an attempt to detect pregnancy onset [80,81]. Although efforts have been made to automate the collection of BBT or similar metrics, they have focused largely on proception or contraception rather than on pregnancy detection [82–85]. Continuous (as opposed to once per day) collection of temperature is a promising alternative that appears to provide additional information about reproductive status by examining not only levels but carefully selected patterns of temperature [40–42,86,87].
For example, murine elevation of continuous body temperature can be used to detect pregnancy onset within ~12 h of conception [41]. Subsequent investigations in humans revealed continuous temperature-based predictors of the preovulatory LH surge [42], as well as prediction and detection of sickness [88]. Based on this growing body of work and on community reports, we hypothesized that features extracted from continuous distal body temperature at the finger (DBT) could provide early indicators of pregnancy. Here we report results from retrospective wearable temperature data from 3 months prior to 3 months after self-reported conception and compared this to self-reported dates of OTC or clinically confirmed pregnancy.
Results
Descriptive statistics
The thirty individuals in this feasibility cohort ranged from 25–44 years old. Ten percent were 25–29, 50% were 30–34, 23% were 35–39, and 17% were 40–44. Of all individuals, 80% discovered their pregnancy through an over the counter (OTC) test, 7% through an in-clinic test, and 13% reported an IVF-initiated pregnancy. Pregnancies in this cohort were confirmed between May of 2019 and April 2021.
Distal body temperature could cut the time to pregnancy awareness by over two thirds in this feasibility cohort
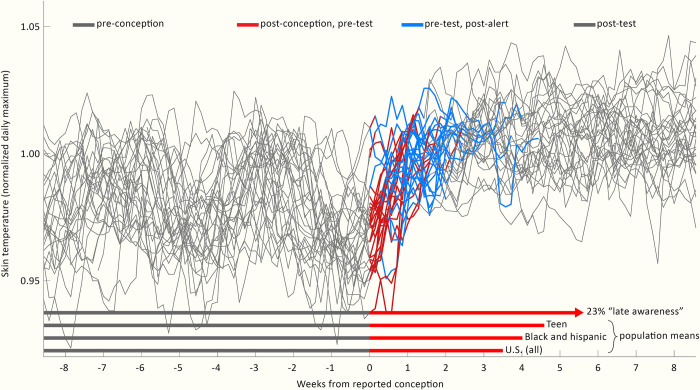
Features of DBT exhibited unique elevations following self-reported date of conceptive sex (see: Methods) in all 30 cases, as well as reproducing previous reports of approximately monthly patterning associated with the ovulatory cycle [42,43] (Fig 1). Unique DBT elevations were used to create a Retrospective Hypothetical Alert (RHA) (see: Methods) that was triggered before standard positive pregnancy test results in 29/30 cases (Fig 1). This is illustrated in Fig 1 as the transition from unconfirmed pregnancy following conception (red) into RHA-tagged pregnancy (blue), which precedes the transition back to grey that occurs upon confirmatory testing. RHA occurred a median duration of 5.5 ± 3.5 days after reported conception, whereas reported confirmation using a standard pregnancy test occurred after a median of 14.5 ± 4.2 days. The RHA-confirmed days occurred significantly earlier than pregnancy test confirmation (p = 1.05*10−8). To provide context for the potential utility of such passively-generated alerts, we highlighted comparison to average pregnancy confirmation dates, including the U.S. population at large, as well as two populations that are at higher risk of pregnancy complications, “Black and Hispanic” [89,90] and “Teen” [1,16]. Additionally, we highlighted the estimated 23% of U.S. pregnancies which are not confirmed by approximately 5 weeks after conception [1].
Fig 1. Nightly temperatures allowed generation of retrospective hypothetical alerts in advance of pregnancy confirmation by standard tests.
Individuals’ nightly maximum temperatures, aligned to the date of reported conception (grey) for all 30 participants. Red: Time between reported conception and reported test confirmation is shown in red unless (blue) an RHA occurred for that individual, at which point red is replaced by blue. At the date of test confirmation, records return to grey. Bottom: red vectors represent mean time from conception to confirmation for: the U.S. population (3.5 weeks); vulnerable sub populations of “Black and Hispanic” (3.9 weeks) and “Teen” (4.6 weeks), and the 23% of the U.S. population reporting “late confirmation” of more than 5 weeks after conception. Epidemiological data visualized from (1).
Nightly maxima uniquely reflect early pregnancy
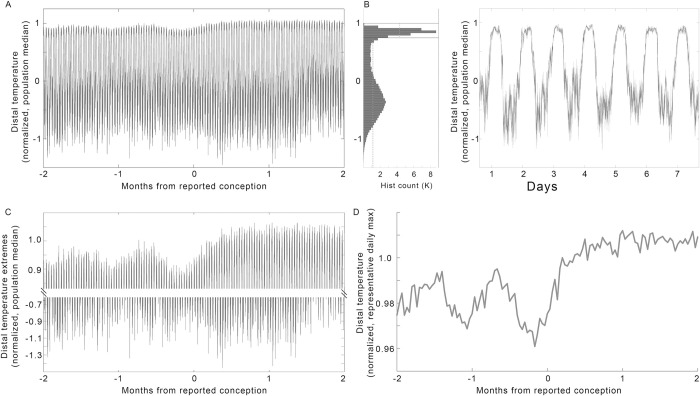
Features of DBT were extracted to assess their utility in detect pregnancy onset. Raw DBT (Fig 2A) was bimodally distributed (Fig 2B). DBT oscillated between relatively labile, lower daytime or waking values, and relatively higher, more tightly distributed nighttime or sleeping values (Fig 2B and 2D) [42,88,91]. Comparison of the daily highs (Fig 2C, top) to the daily lows (Fig 2C, bottom) confirmed that putative ovulatory cycles and pregnancy onset were apparent as changes in nightly levels. Representative nighttime temperature (see: Methods for feature derivation) from each participant for each night confirmed the ability to detect roughly monthly cycles preceding reported conception, as well as a stereotyped rise following conception (Fig 2D and 2E). When compared as a population, Nightly maxima exhibited values that were statistically elevated over previous estimated luteal phase peaks on day 8 after reported conception (χ2 = 91.41, p = 8.8*10−15, L vs. C +8 days p = 0.016) (Fig 3A and 3C light blue panel).
Fig 2. Raw temperature must be transformed to clearly reveal pregnancy onset trends.
(A) Median raw minutely temperature records from all 30 individuals, from 2 months before to 2 months after reported conception. (B) Histogram of pre-conception temperatures in (A) revealed a bimodal distribution, reflecting day-night oscillations, as seen more clearly in a zoom of one arbitrary week (C). (D) Data from A, zoomed to highlight the nightly highs (top) and daily lows (bottom). (E) Population median of the nightly temperature maxima (see: Methods) enhanced the clarity of the patterns reflecting putative ovulatory cycles and pregnancy onset contained within DBT.
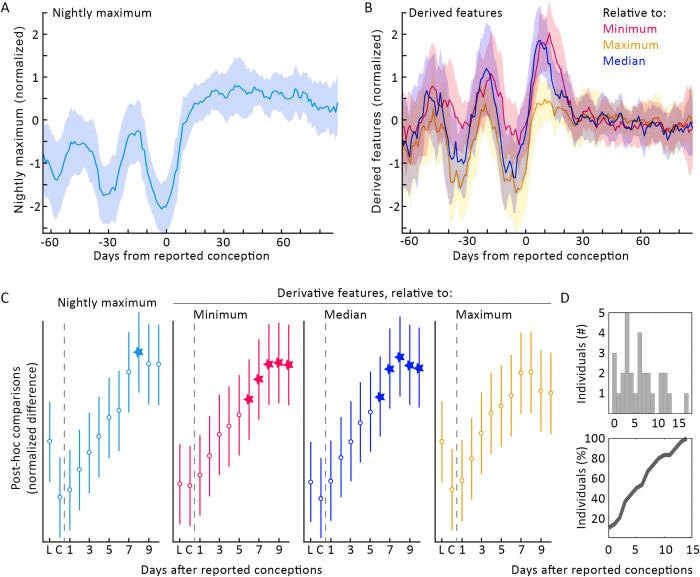
Fig 3. Transformations of nightly temperature maxima enhanced the change seen at pregnancy onset and allowed more efficient RHAs for all 30 participants.
(A) Median nightly temperature maxima ± MAD (see: Methods). (B) Overlay of the three features derived from comparison to individuals’ historical medians (blue), minima (magenta), and maxima (gold) (see: Methods). Post-hoc tests of the difference between putative luteal-phase peaks, and the difference between putative-luteal phase peaks (“L”) and days from conception (“C”), indicated significant post-conception elevation on day +8 in nightly maximum, day +6 in derived minimum, day +6 in derived median, and on no days in derived maximum. Linear (D, top) and cumulative (D, bottom) histograms of days on which these features generated an RHA (see: Methods).
Normalizing nightly maxima to within-individual history improved speed of pregnancy detection
In order to explore the feasibility of enhancing contrast at transitions from follicular to luteal phases, and from follicular phases to pregnancies, we generated second order features normalized to the average historical length of the follicular phase (17 days [39]) (see: Methods for discussion of normalization window). Normalization of an individual’s nightly maxima to the previous 17 days’ history of minima (Fig 3B and 3C red), and medians (Fig 3B and 3C dark blue) exhibited faster within-individual statistical elevations above luteal highs than did Nightly maxima. The derived feature comparing each night’s maximum to historical minima and medians reached statistically significant elevation after 6 days (relative to historical minima: χ2 = 78.00, p = 3.59*10−12, L vs. C +6 days p = 0.034, L +7 days and onward p< 1.60*10−3; relative to historical medians: χ2 = 91.0, p = 1.08*10−14, L vs. C +6 days p = 0.040, L +7 days and onward p< 4*10−3). By contrast, while comparison to historical nightly maxima (Fig 3B and 3C gold) had a significant effect of time, no individual day achieved significance after reported conceptive sex within the days assessed (χ2 = 56.74, p = 3.72*10−8, L vs. C p>0.05 on all days). Although multiple features reached group significance, on the same day, different individuals reached each feature at different times, as shown in the histogram of RHAs (Fig 3D).
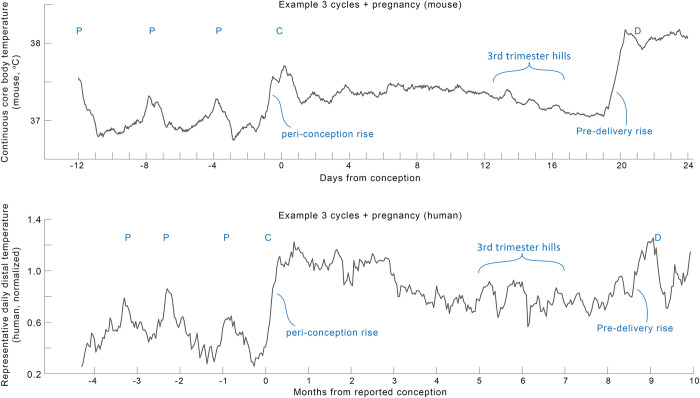
Case study: Similarity among mouse and human temperatures across pregnancy
We previously published the use of features derived from continuous core body temperature to detect pregnancies in mice, and to monitor pregnancies through delivery [41]. Here we highlighted a comparison of a mouse and a human mother across gestation (Fig 4) to support future investigations of continuous body temperature patterns beyond conception. Despite obvious differences in gestational length, body size, and the species’ reproductive physiology, we noted several striking visual similarities between the two pregnancies. Both exhibited ovulatory cycles, followed by a steep rise in temperature at conception, and a long slow decrease in temperature until around the 3rd trimester. Then, large elevations appeared in the temperature trajectory, followed by another steep rise preceding delivery. The consistency and mechanisms of these changes are beyond the scope of this manuscript. We hope that sharing this visual inspection is sufficient support the apparent existence of these conserved patterns in DBT and support more research in the field.
Fig 4.
Comparison of one example mouse (top, from (41)) and human (bottom) pregnancy profile revealed many parallel structures in continuous temperature in need of deeper mechanistic investigation. To highlight trends over daily variance, both profiles show moving means with windows of mouse (24 hours on minutely data) and human (7 days on nightly temperature maxima) data. “P”: peaks of putative ovulatory cycles, “C”: conception, “D”: delivery.
Discussion
This preliminary study supports the feasibility of passive, early pregnancy detection using continuous DBT. In this cohort, nightly temperature maxima rose rapidly in early pregnancy and reached uniquely high values an average of 5.5 days after self-reported conceptive sex. These features enabled generation of RHAs for all individuals, which illustrated that such approaches have the potential to cut time to pregnancy awareness, in this case by 2/3, as compared to reported use of pregnancy tests [1]. Additional analysis of large, diverse cohorts is necessary to understand population variability in DBT patterns and to appropriately refine the features described here before attempting to create prospective alerts. Furthermore, preliminary comparison to published murine data suggests that additional features of DBT may be useful for pregnancy applications beyond conception.
The potential utility of temperature measurement for pregnancy detection was published nearly 100 years ago [47,48,92]. Van de Velde reported a sharp rise in daily oral basal body temperature (BBT) in early pregnancy [47,48], and Buxton and Atkinson subsequently postulated its dependence on elevation of progesterone [49]. Amazingly, even finger temperature was proposed in 1949 by Burt, as a method of pregnancy monitoring [93] (although the authors were not able to locate primary follow-up studies [94–98]). Despite this, neither oral thermometry nor peripheral temperature have developed into trusted tools for early pregnancy detection [75–78,99].
Why might continuous distal temperature improve upon historical uses of oral temperature? Although skin temperature measurements taken from poorly vascularized areas may reflect environmental influences, DBT taken from the ventral portion of the fingers reflects autonomic influence on the brachial artery [100,101], and its patterns of change are not predominantly determined by an individual’s temperature environment [91]. Temperature at the periphery of the body also exhibits higher amplitude circadian and ultradian rhythms than temperature taken from the core (e.g., > 10°C vs. ~ 2–3°C), meaning that small variability in sensor accuracy or precision is less likely to perturb patterns of change assessed at the periphery [102,103]. Additionally, the greater comfort of continuous wear of a ring, as opposed to an alternative to capture core temperature, may enable the collection of data with fewer gaps, which is essential for accurately assessing temperature shifts occurring at non-standard time of day within and across individuals. As continuous measurement allows more information to be captured per unit time, DBT provides a much wider range of potential features associated with adaptation to a pregnancy than does once-per-day BBT [40,104]. For example, continuous DBT features have recently been used to anticipate LH surge onset and assist in cycle phase classification [42,43], and well as contribute to the inference of sleep-wake status and sleep stage [45,91,105,106]. Finally, DBT is temporally coupled to physiological systems that rise in output across the first trimester of pregnancy, such as progesterone [107,108], night time heart rate [109], insulin activity [110–112], luteinizing hormone [42], and cortisol [113,114].
This additional temporal structure, and more thoroughly mapped relation to hormonal output, allows intentional selection of timeseries features that reflect physiological changes. In this case, sleeping temperature measurement provides a relatively unperturbed state (akin to the state that first morning BBT roughly attempts to capture), in which an individual’s behaviors (e.g., exercise, outdoor environment) may have a more limited effect on temperature level and pattern. It is possible that this relative absence of behavioral contributions enables endocrine contributions to the DBT signal to take precedence [115,116]. As pregnancy is associated with substantial changes to hormone levels and thermoregulation, as well as cardiovascular remodeling, future research is needed to confirm that relationships between temperature and hormonal status hold in pregnant individuals.
Notably, the authors were unable to find high temporal resolution descriptions of peripheral physiology around the time of conception. It is possible that the present lack of tools for conception detection makes the study of very early natural pregnancies challenging. Some of the features we explored were more effective than others, and larger cohorts will likely reveal that some features work better in some groups than in others. If and when these or related features are developed to the point that they reliably provide information in larger cohorts, then continuous DBT may enable more precise study of the physiological changes associated with conception, including continuous glucose patterning [110,111], salivary and urinary hormone output [117,118], early cardiovascular remodeling [119]. Additionally, continuous data may allow definition of tighter critical windows for the impacts from maternal and environmental influences [8]. Much remains to be learned about physiological diversity in continuous DBT, and there are likely myriad strategies for generating predictive features. The present study supports the hypothesis that wearable devices can be used to map this physiological diversity and identify features that provide useful information on an individualized basis.
Such tools are not without risk and require careful validation at scale. False positives could result in unnecessary psychological stress or unwarranted consumption of emergency contraception [120], whereas false negatives could lead to a lack of caution in a true early gestation. Additionally, there are several limitations to a retrospective study based on wearable device data and fallible self-report [121,122]. For instance, self-report of day of conception is prone to error, as many individuals have sex multiple times during the fertile window preceding pregnancy onset [74]. Additionally, the retrospective design of the present study meant that exact dates of follicular and luteal phases prior to pregnancy onset could not be determined, necessitating the use of previously published DBT features for estimating luteal phase temperature peaks [42,43,72]. Future studies that include additional non-pregnant cycles from a larger and more diverse population are needed to obtain reliable false positive and false negative rates of detection based on the features described here, as well as the duration after conceptive sex necessary to differentiate pregnancy from other potential sources of abnormal temperature elevation. Indeed, it is possible that transient sickness, medication, metabolic or weight changes could contribute to individuals’ nighttime temperature; however, such modulations would be likely to disrupt, rather than reinforce, temperature patterns associated with ovulatory cycles and pregnancy. This study did not differentiate pregnancies that go on to have second trimester miscarriage, stillbirth, or other complications, and future work is needed to uncover if unique conception profiles are associated with these outcomes [47,78]. Moreover, health algorithms have a history of bias and failure to generalize [123], and our cohort likely represents a relatively affluent and health literate sector of society, which cannot be taken as broadly representative. For these reasons, our work supports the need for large, clinical studies on diverse populations to determine which parameters may provide precise indication of conceptive sex, fertilization, and subsequent events. More broadly, our work supports exploration of physiological diversity from timeseries data.
Our analyses of continuous DBT demonstrate the feasibility of passive, early pregnancy screening. Confirmation and augmentation of these features in clinical settings and across large, heterogeneous populations may enable development of wearable tools for pregnancy monitoring. Such tools may increase individuals’ agency and guide pregnancy testing at an earlier gestational age [8].
Methods
Study design and data collection
Ethical approval
This study and all experimental protocols were IRB approved by the Office for the Protection of Human Subjects at the University of California, San Diego. All participants gave informed consent. All research was performed in accordance with relevant guidelines and regulations.
Participants and informed consent
All data were collected retrospectively. A study invite was delivered to users of the Oura Ring app via an in-app card which linked users to information about the study, informed consent, and which allowed users to opt-in to share data with the researchers. All participants provided online written informed consent via mobile phone or computer. Participants were at least 18 years of age and there were no other age or parity restrictions, consistent with the principles of participatory research.
Data collection and management
Retrospective data had been collected using the Oura Ring (OuraRing Inc., San Francisco, CA; Oura Health Oy, Ltd., Oulu, Finland). The Oura Ring is a small, wireless sensor worn on the finger. The ring contains 3 thermistors for detection of DBT. DBT is measured 24 h a day at a resolution of once per minute. Raw DBT data are synched from the ring to the user’s smart phone when the app is opened, and then sent Oura Ring’s cloud architecture. This architecture meets CCPA and GDPR privacy and security standards, and provided encrypted, password protected data access to researchers, with the participants’ revocable consent. Data, in this case minute-by-minute DBT, were then obtained by the researchers from Oura’s cloud portal and processed as described below.
In addition to data collected by the Oura Ring, participants provided questionnaire responses. Relevant fields to this manuscript included approximate age at conception (5-year bins), the date the individual believes they had conceptive sex, and the date the individual recalls confirming the pregnancy by an over the counter (OTC) or in-lab pregnancy test. Participants could opt out of the study and remove their data from the study pool at any time for any reason. Following data collection, data were anonymized by the researchers for analysis. Note that we refer to “conceptive sex” rather than “conception”, as conception has variably been referred to as the day on which conceptive sex occurs, or the date of implantation (~7–14 days later); the American College of Gynecology defines conception as the latter.
Inclusion and exclusion criteria for submitted pregnancies
The participants for this initial study were the first thirty respondents who met the following data quality criteria and questionnaire responses: 1) No data holes > 1 h within the sleeping window in the 60 days surrounding self-reported conceptive sex; 2) Positive response for self-reported date of conceptive sex; 3) Positive response for self-reported date of pregnancy confirmation via an at-home or in-lab test; 4) Dates provided did not contain obvious typos (e.g., an individual specifying conception on a date that is currently in the future would not be included); 5) Participants did not report a miscarriage following the conception. Note that many pregnancies were ongoing at the time of this study (i.e., individuals were in their second or third trimesters at the time of data collection). This means that we could not rule out the possibility of late miscarriages, still births, or other pregnancy complications within this data set.
Data analysis
Data availability and cleaning
Raw data are proprietary under the Data Use Agreement between UCSD and OuraRing, Inc. Access can be requested of the corresponding author, but must be reviewed on a case-by-case basis by OuraRing, Inc. Data were formatted in Excel 2020 and analyses were performed in MATLAB 2021a. Briefly, data were imported from the Oura database into Excel and DBT data were extracted, beginning at midnight 90 days prior to conception and ending approximately 90 days after conception. Data were padded with zeros to obtain a common set of 180 day-long temperature files. Data were cleaned in MATLAB, with any points showing near instantaneous change, as defined by local abs (derivative) > 105 as an arbitrary cutoff set to the median value of the following hour. Very low remaining values, less than 10°C were considered periods of non-wear and were replaced with blanks. Erroneously high values were not observed, with local highs within the physiological range attributable to common activities such as exercise.
Temperature normalization to pre-pregnancy range
Cleaned data were then normalized using representative daily ranges of pre-pregnancy data to remove variance associated with individuals with differing average temperatures. Briefly, a representative nightly median was generated for each day from 12am-4am, and a representative daily median was generated for each day from 12pm-4pm. The median of nightly and daily pre-pregnancy values formed the within-individual range to which each participant was normalized. The cooler (daytime) representative value of an individual was subtracted from each data point, and the resultant number divided by the individual’s pre-pregnancy range (representative night value minus representative day value). The resultant normalized temperature was designed such that individuals’ temperature would peak at values of approximately 1.
Nightly temperature max evaluation
As finger temperature reaches its maximum values during sleep, and is relatively suppressed during the daytime hours, the median of the hottest 60 minutes of data from a broad window, 8:30pm through 12:00pm the next day, were taken as a representation of maximum temperature during the day. Data were threshold cleaned of sparse high and low outliers, and this nightly maximum variable was saved for each individual for further processing.
Nightly temperature relative to features of estimated previous follicular phase
In order to assess each night’s maximum relative to values in an approximated previous follicular phase (an average of 17 days in large populations [39]), we calculated a rolling past baseline using movmin, movmedian, and movmax functions. We selected 17 days rather than the historical choice of 14-day average follicular phase length in order to impose a stricter threshold for post-conception temperature rise, and in order to encompass the latest data on estimated cycle structure. As we do not have information on individuals’ historical dates of ovulation, we were unable to create personalized follicular phase length normalizations; such personalization will require investigation in future cohorts with measurement of ovulation. We subtracted each of the above nightly maximum values to create a series of personal-history-normalized temperature values, depicted in Fig 3. These values can be interpreted as an individual’s hottest sleeping temperatures relative to that individual’s hottest, coldest, or median sleeping values over the prior 17 days. This window was selected based on population reports of typical phase lengths and was grossly intended to improve detection of the contrast between ovulatory cycle phases and conceptions. These final features, nightly max, and nightly max relative to estimated follicular median, maximum, and minimum were normalized by subtracting each individual’s median and dividing by that individual’s median absolute deviation (M.A.D.) before averaging in order to emphasize the pattern of relative change within an individual rather than the absolute y-values of the variables as the key features.
Detecting an individual’s pregnancy onset
For each of the above variables—nightly maximum, min-normalized, max-normalized, and median-normalized—the day was specified at which the value of the features exceeded the value of the previous 2 putative luteal phases of each individual. Whichever feature of the four first crossed this threshold was used as the “confirmation day” of pregnancy onset (Fig 3).
Statistical analyses
To avoid assumptions of normality, feature values are reported as medians ± M.A.D. unless otherwise stated. For statistical comparisons of temperature features, Kruskal Wallis (KW) tests were used instead of ANOVAS to assess the trends in the 2 putative luteal phases, estimated based on elevation of temperature metrics, preceding pregnancy as compared to the days following conception. For KW tests, χ2 and p values are listed in the text. Dunn’s test was used to correct for multiple comparisons among luteal phase values and values of each of the first 10 days following self-reported conception. Figures were formatted in Microsoft PowerPoint 2019 (Microsoft Inc., Redmond, WA) and Adobe Photoshop CS8 (Adobe Inc, San Jose, CA).
Acknowledgments
The authors would like to thank the individuals who approached us with pregnancy data stories over the past many years, including the QCycle study group and the Oura community. Special thanks to those at Oura who supported logistics of this study, and to Lance Kriegsfeld, Gary Wolf, and Vyoma Shah for ongoing intellectual support of our efforts within the wearables space.
Data Availability
Data Availability and Cleaning. Code for statistics and feature generation are available at A.G.'s github. Raw data are proprietary under the Data Use Agreement between UCSD and OuraRing, Inc. Access can be requested of the corresponding author, but must be reviewed on a case-by-case basis by OuraRing, Inc. Contact: request_data_access@ouraring.com.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Branum AM, Ahrens KA. Trends in Timing of Pregnancy Awareness Among US Women. Matern Child Health J. 2017. Apr;21 (4):715–26. doi: 10.1007/s10995-016-2155-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hochman E, Elami-Suzin M, Soferman HG, Galil T, Hershkovitz Y, Tzur D, et al. Early pregnancy confirmation—the role of urine pregnancy test in military primary care clinics. Mil Med. 2012. Aug;177 (8):947–51. doi: 10.7205/milmed-d-11-00455 [DOI] [PubMed] [Google Scholar]
- 3.Ananth CV. Menstrual versus clinical estimate of gestational age dating in the United States: temporal trends and variability in indices of perinatal outcomes. Paediatr Perinat Epidemiol. 2007. Sep;21 Suppl 2:22–30. doi: 10.1111/j.1365-3016.2007.00858.x [DOI] [PubMed] [Google Scholar]
- 4.Dott M, Rasmussen SA, Hogue CJ, Reefhuis J, National Birth Defects Prevention Study. Association between pregnancy intention and reproductive-health related behaviors before and after pregnancy recognition, National Birth Defects Prevention Study, 1997–2002. Matern Child Health J. 2010. May;14 (3):373–81. doi: 10.1007/s10995-009-0458-1 [DOI] [PubMed] [Google Scholar]
- 5.Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009. Mar;79 (3):194–8. doi: 10.1016/j.contraception.2008.09.009 [DOI] [PubMed] [Google Scholar]
- 6.Choi H, Wang L, Lin X, Spengler JD, Perera FP. Fetal Window of Vulnerability to Airborne Polycyclic Aromatic Hydrocarbons on Proportional Intrauterine Growth Restriction. PLOS ONE. 2012. Apr 24;7 (4):e35464. doi: 10.1371/journal.pone.0035464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamai EM, McElrath TF, Ferguson KK. Fetal growth in environmental epidemiology: mechanisms, limitations, and a review of associations with biomarkers of non-persistent chemical exposures during pregnancy. Environ Health. 2019. May 8;18 (1):43. doi: 10.1186/s12940-019-0480-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sundermann AC, Velez Edwards DR, Slaughter JC, Wu P, Jones SH, Torstenson ES, et al. Week-by-week alcohol consumption in early pregnancy and spontaneous abortion risk: a prospective cohort study. Am J Obstet Gynecol. 2021. Jan;224 (1):97.e1–97.e16. doi: 10.1016/j.ajog.2020.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avalos LA, Roberts SCM, Kaskutas LA, Block G, Li D-K. Volume and type of alcohol during early pregnancy and the risk of miscarriage. Subst Use Misuse. 2014. Sep;49 (11):1437–45. doi: 10.3109/10826084.2014.912228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adeniyi OV, Ajayi AI, Moyaki MG, Goon DT, Avramovic G, Lambert J. High rate of unplanned pregnancy in the context of integrated family planning and HIV care services in South Africa. BMC Health Serv Res. 2018. Feb 27;18 (1):140. doi: 10.1186/s12913-018-2942-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finer LB, Zolna MR. Declines in Unintended Pregnancy in the United States, 2008–2011. N Engl J Med. 2016. Mar 3;374 (9):843–52. doi: 10.1056/NEJMsa1506575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moreira LR, Ewerling F, Dos Santos IS, Wehrmeister FC, Matijasevich A, Barros AJD, et al. Trends and inequalities in unplanned pregnancy in three population-based birth cohorts in Pelotas, Brazil. Int J Public Health. 2020. Dec;65 (9):1635–45. doi: 10.1007/s00038-020-01505-0 [DOI] [PubMed] [Google Scholar]
- 13.Yargawa J, Machiyama K, Ponce Hardy V, Enuameh Y, Galiwango E, Gelaye K, et al. Pregnancy intention data completeness, quality and utility in population-based surveys: EN-INDEPTH study. Popul Health Metr. 2021. Feb 8;19 (Suppl 1):6. doi: 10.1186/s12963-020-00227-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Than LC, Honein MA, Watkins ML, Yoon PW, Daniel KL, Correa A. Intent to become pregnant as a predictor of exposures during pregnancy: is there a relation? J Reprod Med. 2005. Jun;50 (6):389–96. [PubMed] [Google Scholar]
- 15.Ranatunga IDJC, Jayaratne K. Proportion of unplanned pregnancies, their determinants and health outcomes of women delivering at a teaching hospital in Sri Lanka. BMC Pregnancy Childbirth. 2020. Nov 5;20 (1):667. doi: 10.1186/s12884-020-03259-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Allotey P, Ravindran TKS, Sathivelu V. Trends in Abortion Policies in Low- and Middle-Income Countries. Annu Rev Public Health. 2021;42 (1):505–18. doi: 10.1146/annurev-publhealth-082619-102442 [DOI] [PubMed] [Google Scholar]
- 17.ESHRE Capri Workshop Group. Induced abortion. Hum Reprod Oxf Engl. 2017. Jun 1;32 (6):1160–9. [DOI] [PubMed] [Google Scholar]
- 18.Shah PS, Balkhair T, Ohlsson A, Beyene J, Scott F, Frick C. Intention to become pregnant and low birth weight and preterm birth: a systematic review. Matern Child Health J. 2011. Feb;15 (2):205–16. doi: 10.1007/s10995-009-0546-2 [DOI] [PubMed] [Google Scholar]
- 19.Shah PS, Shah V, Knowledge Synthesis Group On Determinants Of Preterm/lBW Births. Influence of the maternal birth status on offspring: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2009;88 (12):1307–18. doi: 10.3109/00016340903358820 [DOI] [PubMed] [Google Scholar]
- 20.Shapiro-Mendoza C, Selwyn BJ, Smith DP, Sanderson M. Parental pregnancy intention and early childhood stunting: findings from Bolivia. Int J Epidemiol. 2005. Apr;34 (2):387–96. doi: 10.1093/ije/dyh354 [DOI] [PubMed] [Google Scholar]
- 21.Rahman MM. Is Unwanted Birth Associated with Child Malnutrition in Bangladesh? Int Perspect Sex Reprod Health. 2015. Jun;41 (2):80–8. doi: 10.1363/4108015 [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y-Y, Song C-G, Wang X, Jiang Y-L, Zhao J-J, Yuan F, et al. Clinical characteristics and fetal outcomes in women with epilepsy with planned and unplanned pregnancy: A retrospective study. Seizure. 2020. Jul;79:97–102. doi: 10.1016/j.seizure.2020.05.011 [DOI] [PubMed] [Google Scholar]
- 23.Wilson RD, Genetics Committee, Wilson RD, Audibert F, Brock J-A, Carroll J, et al. Pre-conception Folic Acid and Multivitamin Supplementation for the Primary and Secondary Prevention of Neural Tube Defects and Other Folic Acid-Sensitive Congenital Anomalies. J Obstet Gynaecol Can JOGC J Obstet Gynecol Can JOGC. 2015. Jun;37 (6):534–52. doi: 10.1016/s1701-2163(15)30230-9 [DOI] [PubMed] [Google Scholar]
- 24.McCrory C, McNally S. The effect of pregnancy intention on maternal prenatal behaviours and parent and child health: results of an irish cohort study. Paediatr Perinat Epidemiol. 2013. Mar;27 (2):208–15. doi: 10.1111/ppe.12027 [DOI] [PubMed] [Google Scholar]
- 25.Qiu X, Zhang S, Sun X, Li H, Wang D. Unintended pregnancy and postpartum depression: A meta-analysis of cohort and case-control studies. J Psychosom Res. 2020. Nov;138:110259. doi: 10.1016/j.jpsychores.2020.110259 [DOI] [PubMed] [Google Scholar]
- 26.Time for plan B. Nat News. 2013. Apr 11;496 (7444):138. doi: 10.1038/496138a [DOI] [PubMed] [Google Scholar]
- 27.Li H-WR, Lo SST, Ho P-C. Emergency contraception. Best Pract Res Clin Obstet Gynaecol. 2014. Aug;28 (6):835–44. doi: 10.1016/j.bpobgyn.2014.04.011 [DOI] [PubMed] [Google Scholar]
- 28.Gemzell-Danielsson K. Mechanism of action of emergency contraception. Contraception. 2010. Nov;82 (5):404–9. doi: 10.1016/j.contraception.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 29.Upadhya KK, COMMITTEE ON ADOLESCENCE. Emergency Contraception. Pediatrics. 2019. Dec;144 (6). doi: 10.1542/peds.2019-3149 [DOI] [PubMed] [Google Scholar]
- 30.Guillaume A, Rossier C, Reeve P. Abortion around the world. An overview of legislation, measures, trends, and consequences. Population. 2018. Oct 18;Vol. 73 (2):217–306. [Google Scholar]
- 31.Denny CH, Acero CS, Naimi TS, Kim SY. Consumption of Alcohol Beverages and Binge Drinking Among Pregnant Women Aged 18–44 Years—United States, 2015–2017. MMWR Morb Mortal Wkly Rep. 2019. Apr 26;68 (16):365–8. doi: 10.15585/mmwr.mm6816a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Connery HS, Albright BB, Rodolico JM. Adolescent substance use and unplanned pregnancy: strategies for risk reduction. Obstet Gynecol Clin North Am. 2014. Jun;41 (2):191–203. doi: 10.1016/j.ogc.2014.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shrestha D, Aryal S, Sharma B. Safety, Efficacy and Acceptability of Early First Trimester Abortion using Oral Mifepristone and Sublingual Misoprostol. J Nepal Health Res Counc. 2018. Oct 30;16 (3):269–73. [PubMed] [Google Scholar]
- 34.Butler SA, Khanlian SA, Cole LA. Detection of Early Pregnancy Forms of Human Chorionic Gonadotropin by Home Pregnancy Test Devices. Clin Chem. 2001. Dec 1;47 (12):2131–6. [PubMed] [Google Scholar]
- 35.Cole LA, Khanlian SA, Sutton JM, Davies S, Rayburn WF. Accuracy of home pregnancy tests at the time of missed menses. Am J Obstet Gynecol. 2004. Jan 1;190 (1):100–5. doi: 10.1016/j.ajog.2003.08.043 [DOI] [PubMed] [Google Scholar]
- 36.Nickmans S, Vermeersch P, Van Eldere J, Billen J. Performance of qualitative urinary hCG assays. Acta Clin Belg. 2014. Aug;69 (4):277–9. doi: 10.1179/0001551214Z.00000000069 [DOI] [PubMed] [Google Scholar]
- 37.Cole LA. The utility of six over-the-counter (home) pregnancy tests. Clin Chem Lab Med. 2011. Aug;49 (8):1317–22. doi: 10.1515/CCLM.2011.211 [DOI] [PubMed] [Google Scholar]
- 38.Ecochard R, Bouchard T, Leiva R, Abdulla S, Dupuis O, Duterque O, et al. Characterization of hormonal profiles during the luteal phase in regularly menstruating women. Fertil Steril. 2017. Jul 1;108 (1):175–182.e1. doi: 10.1016/j.fertnstert.2017.05.012 [DOI] [PubMed] [Google Scholar]
- 39.Bull JR, Rowland SP, Scherwitzl EB, Scherwitzl R, Danielsson KG, Harper J. Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles. NPJ Digit Med [Internet]. 2019. Aug 27 [cited 2020 Jan 24];2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6710244/ doi: 10.1038/s41746-019-0152-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Webster WW, Smarr B. Using Circadian Rhythm Patterns of Continuous Core Body Temperature to Improve Fertility and Pregnancy Planning. J Circadian Rhythms. 2020. Sep 24;18:5. doi: 10.5334/jcr.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smarr BL, Zucker I, Kriegsfeld LJ. Detection of Successful and Unsuccessful Pregnancies in Mice within Hours of Pairing through Frequency Analysis of High Temporal Resolution Core Body Temperature Data. PloS One. 2016;11 (7):e0160127. doi: 10.1371/journal.pone.0160127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grant AD, Newman M, Kriegsfeld LJ. Ultradian rhythms in heart rate variability and distal body temperature anticipate onset of the luteinizing hormone surge. Sci Rep. 2020. Nov 23;10 (1):20378. doi: 10.1038/s41598-020-76236-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maijala A, Kinnunen H, Koskimäki H, Jämsä T, Kangas M. Nocturnal finger skin temperature in menstrual cycle tracking: ambulatory pilot study using a wearable Oura ring. BMC Womens Health. 2019. 29;19 (1):150. doi: 10.1186/s12905-019-0844-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hasselberg MJ, McMahon J, Parker K. The validity, reliability, and utility of the iButton for measurement of body temperature circadian rhythms in sleep/wake research. Sleep Med. 2013. Jan;14 (1):5–11. doi: 10.1016/j.sleep.2010.12.011 [DOI] [PubMed] [Google Scholar]
- 45.Krauchi K, Konieczka K, Roescheisen-Weich C, Gompper B, Hauenstein D, Schoetzau A, et al. Diurnal and menstrual cycles in body temperature are regulated differently: a 28-day ambulatory study in healthy women with thermal discomfort of cold extremities and controls. Chronobiol Int. 2014. Feb;31 (1):102–13. doi: 10.3109/07420528.2013.829482 [DOI] [PubMed] [Google Scholar]
- 46.Batinga H, Martinez-Nicolas A, Zornoza-Moreno M, Sánchez-Solis M, Larqué E, Mondéjar MT, et al. Ontogeny and aging of the distal skin temperature rhythm in humans. Age Dordr Neth. 2015;37 (2):29. doi: 10.1007/s11357-015-9768-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van de Velde T. Ueber den Zusammenhang zwischen Ovarialfunction, Wellenbewegung und Menstrualblutung, und ueber die Entstehung des sogenannten Mittelschmerzes / von Th. H. Van de Velde. [Internet]. Wellcome Collection. 1904. [cited 2021 May 29]. Available from: https://wellcomecollection.org/works/tcxermmu [Google Scholar]
- 48.Van de Velde T. Ideal Marriage [Internet]. Elsevier; 1926 [cited 2021 May 29]. Available from: https://linkinghub.elsevier.com/retrieve/pii/C20130066029
- 49.Buxton CL, Atkinson WB. Hormonal factors involved in the regulation of basal body temperature during the menstrual cycle and pregnancy. J Clin Endocrinol Metab. 1948. Jul;8 (7):544–9. doi: 10.1210/jcem-8-7-544 [DOI] [PubMed] [Google Scholar]
- 50.Cohen J, Iffy L, Keyser HH. Basal body temperature recordings in spontaneous abortion. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. 1976;14 (2):117–22. doi: 10.1002/j.1879-3479.1976.tb00579.x [DOI] [PubMed] [Google Scholar]
- 51.Keyser HH, Iffy L, Cohen J. Basal body temperature recordings in ectopic pregnancy. J Reprod Med. 1975. Jan;14 (1):37–40. [PubMed] [Google Scholar]
- 52.Siegler AM. Basal Body Temperature in Pregnancy. Obstet Gynecol. 1955. Jun;5 (6):830–2. [PubMed] [Google Scholar]
- 53.Davis ME. The clinical use of oral basal temperatures. J Am Med Assoc. 1946. Apr 6;130 (14):929–32. [PubMed] [Google Scholar]
- 54.ORAL BASAL TEMPERATURES AND OVULATION. J Am Med Assoc. 1946. May 4;131 (1):32–32. [Google Scholar]
- 55.Winzeler H. [Basal temperature and pregnancy]. Gynaecol Int Mon Rev Obstet Gynecol Rev Int Mens Obstet Gynecol Monatsschrift Geburtshilfe Gynakologie. 1952. Jul;134 (1):89–92. [PubMed] [Google Scholar]
- 56.Grant A, McBRIDE WG. The 100 day basal body temperature graph in early pregnancy. Med J Aust. 1959. Apr 4;46 (14):458–60. doi: 10.5694/j.1326-5377.1959.tb59135.x [DOI] [PubMed] [Google Scholar]
- 57.Vermelin H, Ribon M. [Importance of the basal temperature curve during the first months of pregnancy]. Bull Fed Soc Gynecol Dobstetrique Lang Francaise. 1959. Oct;11:401–2. [PubMed] [Google Scholar]
- 58.Knoerr K, Probst V. [Observations on the duration of pregnancy with the aid of basal temperature measurements]. Zentralbl Gynakol. 1959. Oct 31;81:1742–7. [PubMed] [Google Scholar]
- 59.Farris EJ. Basal body temperature throughout pregnancy; a report upon two patients. Hum Fertil. 1947. Dec;12 (4):106–9. [PubMed] [Google Scholar]
- 60.Lauritzen C. [Basal temperature regulation in pregnancy]. Arch Gynakol. 1958;191 (2):122–33. doi: 10.1007/BF00976984 [DOI] [PubMed] [Google Scholar]
- 61.Hartemann J. [Thermal shifts of the 4th month and diagnosis of the duration of pregnancy]. Bull Fed Soc Gynecol Dobstetrique Lang Francaise. 1961;13:518–26. [PubMed] [Google Scholar]
- 62.Hartemann J. [A guiding mark of the duration of pregnancy (fall of the basal temperature in the 4th month)]. Rev Fr Gynecol Obstet. 1961. Feb;56:113–8. [PubMed] [Google Scholar]
- 63.Hartemann J. [Decrease in the basal temperature after the 1st trimester of pregnancy (cause and value in determination of the age of the pregnancy)]. Bull Fed Soc Gynecol Dobstetrique Lang Francaise. 1960. Oct;12:421–5. [PubMed] [Google Scholar]
- 64.Birnbaum SJ. Breast temperature as a test for pregnancy. Preliminary report. Obstet Gynecol. 1966. Mar;27 (3):378–80. [PubMed] [Google Scholar]
- 65.Schildbach HR. [New data on the duration of pregnancy determined by measurement of the basal temperature]. Klin Wochenschr. 1953. Jul 15;31 (27–28):654–6. doi: 10.1007/BF01477740 [DOI] [PubMed] [Google Scholar]
- 66.Carceller Blay C, Fuster Chiner R. [Estimated duration of pregnancy by recording the basal temperature]. Rev Esp Obstet Ginecol. 1955. Aug;14 (82):195–212. [PubMed] [Google Scholar]
- 67.Weinberg W. The practical importance of basal temperature graphs for the diagnosis of pregnancy. South Afr Med J Suid-Afr Tydskr Vir Geneeskd. 1954. Dec 25;28 (52):1099–101. [PubMed] [Google Scholar]
- 68.Raffo Del Campo MA, Kupman A, Wainer A. [Progesterone and the basal temperature in the diagnosis of pregnancy]. Prensa Med Argent. 1962. Feb 9;49:329–31. [PubMed] [Google Scholar]
- 69.Bauman JE. Basal body temperature: unreliable method of ovulation detection. Fertil Steril. 1981. Dec;36 (6):729–33. doi: 10.1016/s0015-0282(16)45916-9 [DOI] [PubMed] [Google Scholar]
- 70.Direito A, Bailly S, Mariani A, Ecochard R. Relationships between the luteinizing hormone surge and other characteristics of the menstrual cycle in normally ovulating women. Fertil Steril. 2013. Jan 1;99 (1):279–285.e3. doi: 10.1016/j.fertnstert.2012.08.047 [DOI] [PubMed] [Google Scholar]
- 71.Barron ML, Fehring R. Basal Body Temperature Assessment: Is It Useful to Couples Seeking Pregnancy?: 15. [DOI] [PubMed] [Google Scholar]
- 72.de Mouzon J, Testart J, Lefevre B, Pouly JL, Frydman R. Time relationships between basal body temperature and ovulation or plasma progestins. Fertil Steril. 1984. Feb;41 (2):254–9. doi: 10.1016/s0015-0282(16)47600-4 [DOI] [PubMed] [Google Scholar]
- 73.Ecochard R, Boehringer H, Rabilloud M, Marret H. Chronological aspects of ultrasonic, hormonal, and other indirect indices of ovulation. BJOG Int J Obstet Gynaecol. 2001. Aug 1;108 (8):822–9. [DOI] [PubMed] [Google Scholar]
- 74.Ecochard R, Duterque O, Leiva R, Bouchard T, Vigil P. Self-identification of the clinical fertile window and the ovulation period. Fertil Steril. 2015. May;103 (5):1319–1325.e3. doi: 10.1016/j.fertnstert.2015.01.031 [DOI] [PubMed] [Google Scholar]
- 75.Steward K, Raja A. Physiology, Ovulation And Basal Body Temperature. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. [cited 2021 May 26]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK546686/ [PubMed] [Google Scholar]
- 76.Pahnke U, Göretzlehner G, Hofmann R. [Measurement of basal temperature for calculation of duration of pregnancy (author’s transl)]. Zentralbl Gynakol. 1979;101 (12):789–95. [PubMed] [Google Scholar]
- 77.Coopersmith BI. Thermal diagnosis of early pregnancy. Q Bull Northwest Univ Med Sch. 1952;26 (2):109–10. [PMC free article] [PubMed] [Google Scholar]
- 78.Newill RG, Katz M. The basal body temperature chart in artificial insemination by donor pregnancy cycles. Fertil Steril. 1982. Oct;38 (4):431–8. doi: 10.1016/s0015-0282(16)46577-5 [DOI] [PubMed] [Google Scholar]
- 79.Kindara. Blog | Kindara [Internet]. [cited 2021 May 17]. Available from: https://www.kindara.com/blog
- 80.Québec S. Conceiving with the Symptothermal Method [Internet]. Seréna Québec. [cited 2021 May 17]. Available from: //serenaquebec.com/en/natural-conception/conceiving-with-the-symptothermal-method/ [Google Scholar]
- 81.Using the Sympto-thermal Method of Fertility Awareness to Maximize Your Chances of Getting Pregnant [Internet]. readytogroove.github.io. [cited 2021 May 17]. Available from: http://www.readytogroove.com/the-cycle/appendix-b-the-sympto-thermal-method-for-pregnancy-assistance/
- 82.Grimes DA, Gallo MF, Grigorieva V, Nanda K, Schulz KF. Fertility awareness-based methods for contraception: systematic review of randomized controlled trials—Contraception [Internet]. [cited 2018 Sep 21]. Available from: https://www.contraceptionjournal.org/article/S0010-7824(05)00103-4/fulltext [DOI] [PubMed]
- 83.Simmons RG, Jennings V. Fertility awareness-based methods of family planning. Best Pract Res Clin Obstet Gynaecol. 2020. Jul;66:68–82. doi: 10.1016/j.bpobgyn.2019.12.003 [DOI] [PubMed] [Google Scholar]
- 84.Symul L, Wac K, Hillard P, Salathé M. Assessment of menstrual health status and evolution through mobile apps for fertility awareness. Npj Digit Med. 2019. Jul 16;2 (1):1–10. doi: 10.1038/s41746-019-0139-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Liu B, Shi S, Wu Y, Thomas D, Symul L, Pierson E, et al. Predicting pregnancy using large-scale data from a women’s health tracking mobile application. Proc Int World-Wide Web Conf Int WWW Conf. 2019. May;2019:2999–3005. doi: 10.1145/3308558.3313512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Webster W, Godfrey EM, Costantini L, Katilius J. Passive fertility prediction using a novel vaginal ring and smartphone application. Fertil Steril. 2015. Sep 1;104 (3):e98. [Google Scholar]
- 87.Aptekar D, Costantini L, Katilius J, Webster W. Continuous, Passive Personal Wearable Sensor to Predict Ovulation [21G]. Obstet Gynecol. 2016. May;127:64S. [Google Scholar]
- 88.Smarr BL, Aschbacher K, Fisher SM, Chowdhary A, Dilchert S, Puldon K, et al. Feasibility of continuous fever monitoring using wearable devices. Sci Rep [Internet]. 2020. Dec 14 [cited 2021 Feb 25];10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7736301/ doi: 10.1038/s41598-020-78355-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Alhusen JL, Bower KM, Epstein E, Sharps P. Racial Discrimination and Adverse Birth Outcomes: An Integrative Review. J Midwifery Womens Health. 2016. Nov;61 (6):707–20. doi: 10.1111/jmwh.12490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gupta R, Froeb K. Preterm Birth: Two Startling Trends, One Call to Action. J Perinat Neonatal Nurs. 2020. Jun;34 (2):99–103. doi: 10.1097/JPN.0000000000000469 [DOI] [PubMed] [Google Scholar]
- 91.Henane R, Buguet A, Roussel B, Bittel J. Variations in evaporation and body temperatures during sleep in man. J Appl Physiol. 1977. Jan;42 (1):50–5. doi: 10.1152/jappl.1977.42.1.50 [DOI] [PubMed] [Google Scholar]
- 92.HARVEY OL, CROCKETT HE. INDIVIDUAL DIFFERENCES IN TEMPERATURE CHANGES OF WOMEN DURING THE COURSE OF THE MENSTRUAL CYCLE. Hum Biol. 1932;4 (4):453–68. [Google Scholar]
- 93.Burt Catherine C. PERIPHERAL SKIN TEMPERATURE IN NORMAL PREGNANCY. The Lancet. 1949. Oct;254 (6583):787–90. [DOI] [PubMed] [Google Scholar]
- 94.McMurray RG, Katz VL. Thermoregulation in Pregnancy: Implications for Exercise. Sports Med. 1990. Sep;10 (3):146–58. doi: 10.2165/00007256-199010030-00002 [DOI] [PubMed] [Google Scholar]
- 95.Schomig G. [Skin temperature increase above the breast in pregnancy]. Geburtshilfe Frauenheilkd. 1953. Jun;13 (6):564–6. [PubMed] [Google Scholar]
- 96.Burt CC. Forearm and Hand Blood Flow in Pregnancy. In: Ciba Foundation Symposium—Toxæmias of Pregnancy: Human and Veterinary [Internet]. John Wiley & Sons, Ltd; 1950. [cited 2021 May 27]. p. 151–4. Available from: http://onlinelibrary.wiley.com/doi/abs/10.1002/9780470715147.ch15 [Google Scholar]
- 97.Burt CC. The peripheral circulation in pregnancy. (Tr. Edinburgh Obst. Soc). Edinb Med J. 1949 1950;18–26. [PubMed] [Google Scholar]
- 98.Burt CC. Symposium on Hæmodynamics in Pregnancy. IV. The Peripheral Circulation in Pregnancy. Edinb Med J. 1950. Mar;57 (3):T18–26. [Google Scholar]
- 99.Hansen TB. [Concerning premenstrual increases in temperature]. Beitrage Zur Klin Tuberk Spezifischen Tuberk-Forsch. 1913;27 (3):291–314. [PubMed] [Google Scholar]
- 100.Krauchi K, Deboer T. The interrelationship between sleep regulation and thermoregulation. Front Biosci Landmark Ed. 2010. Jan 1;15:604–25. doi: 10.2741/3636 [DOI] [PubMed] [Google Scholar]
- 101.Kräuchi K. The thermophysiological cascade leading to sleep initiation in relation to phase of entrainment. Sleep Med Rev. 2007. Dec;11 (6):439–51. doi: 10.1016/j.smrv.2007.07.001 [DOI] [PubMed] [Google Scholar]
- 102.Prendergast BJ, Beery AK, Paul MJ, Zucker I. Enhancement and Suppression of Ultradian and Circadian Rhythms across the Female Hamster Reproductive Cycle. J Biol Rhythms. 2012. Jun 1;27 (3):246–56. doi: 10.1177/0748730412441315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wang ZY, Cable EJ, Zucker I, Prendergast BJ. Pregnancy-induced changes in ultradian rhythms persist in circadian arrhythmic Siberian hamsters. Horm Behav. 2014. Jul;66 (2):228–37. doi: 10.1016/j.yhbeh.2014.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Grant AD, Wilsterman K, Smarr BL, Kriegsfeld LJ. Evidence for a Coupled Oscillator Model of Endocrine Ultradian Rhythms. J Biol Rhythms. 2018. Aug 22;33 (5):475–96. doi: 10.1177/0748730418791423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Altini M, Kinnunen H. The Promise of Sleep: A Multi-Sensor Approach for Accurate Sleep Stage Detection Using the Oura Ring. Sensors [Internet]. 2021. Jul [cited 2022 Jan 24];21 (13). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8271886/ doi: 10.3390/s21134302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Krauchi K, Wirz-Justice A. Circadian rhythm of heat production, heart rate, and skin and core temperature under unmasking conditions in men. Am J Physiol. 1994. Sep;267 (3 Pt 2):R819–829. doi: 10.1152/ajpregu.1994.267.3.R819 [DOI] [PubMed] [Google Scholar]
- 107.Deng Y, Chen C, Chen S, Mai G, Liao X, Tian H, et al. Baseline Levels of Serum Progesterone and the First Trimester Pregnancy Outcome in Women with Threatened Abortion: A Retrospective Cohort Study. BioMed Res Int. 2020;2020:8780253. doi: 10.1155/2020/8780253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Di Renzo GC, Giardina I, Clerici G, Brillo E, Gerli S. Progesterone in normal and pathological pregnancy. Horm Mol Biol Clin Investig. 2016. Jul 1;27 (1):35–48. doi: 10.1515/hmbci-2016-0038 [DOI] [PubMed] [Google Scholar]
- 109.Olsson K, Lagerstedt AS, Bergström A, Häggström J. Change of diurnal heart rate patterns during pregnancy and lactation in dogs (Canis familiaris). Acta Vet Scand. 2003;44 (3–4):105–10. doi: 10.1186/1751-0147-44-105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Golic M, Kräker K, Fischer C, Alenina N, Haase N, Herse F, et al. Continuous Blood Glucose Monitoring Reveals Enormous Circadian Variations in Pregnant Diabetic Rats. Front Endocrinol [Internet]. 2018. May 29 [cited 2021 May 29];9. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5986873/ doi: 10.3389/fendo.2018.00271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bandres-Meriz J, Dieberger AM, Hoch D, Pöchlauer C, Bachbauer M, Glasner A, et al. Maternal Obesity Affects the Glucose-Insulin Axis During the First Trimester of Human Pregnancy. Front Endocrinol [Internet]. 2020. Oct 9 [cited 2021 May 29];11. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7586307/ doi: 10.3389/fendo.2020.566673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019. Jan;42 (Suppl 1):S165–72. doi: 10.2337/dc19-S014 [DOI] [PubMed] [Google Scholar]
- 113.Stirrat LI, Walker JJ, Stryjakowska K, Jones N, Homer NZM, Andrew R, et al. Pulsatility of glucocorticoid hormones in pregnancy: Changes with gestation and obesity. Clin Endocrinol (Oxf). 2018. Apr;88 (4):592–600. doi: 10.1111/cen.13548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Smarr BL, Burnett DC, Mesri SM, Pister KSJ, Kriegsfeld LJ. A Wearable Sensor System with Circadian Rhythm Stability Estimation for Prototyping Biomedical Studies. IEEE Trans Affect Comput. 2016. Jul;7 (3):220–30. [Google Scholar]
- 115.Smarr BL, Grant AD, Zucker I, Prendergast BJ, Kriegsfeld LJ. Sex differences in variability across timescales in BALB/c mice. Biol Sex Differ. 2017;8:7. doi: 10.1186/s13293-016-0125-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sanchez-Alavez M, Alboni S, Conti B. Sex- and age-specific differences in core body temperature of C57Bl/6 mice. Age Dordr Neth. 2011. Mar;33 (1):89–99. doi: 10.1007/s11357-010-9164-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Barha CK, Salvante KG, Jones MJ, Farré P, Blais J, Kobor MS, et al. Early post-conception maternal cortisol, children’s HPAA activity and DNA methylation profiles. J Dev Orig Health Dis. 2019. Feb;10 (1):73–87. doi: 10.1017/S2040174418000880 [DOI] [PubMed] [Google Scholar]
- 118.Nepomnaschy PA, Salvante KG, Zeng L, Pyles C, Ma H, Blais JC, et al. Variation in maternal urinary cortisol profiles across the peri-conceptional period: a longitudinal description and evaluation of potential functions. Hum Reprod Oxf Engl. 2015. Jun;30 (6):1460–72. doi: 10.1093/humrep/dev086 [DOI] [PubMed] [Google Scholar]
- 119.Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014. Sep 16;130 (12):1003–8. doi: 10.1161/CIRCULATIONAHA.114.009029 [DOI] [PubMed] [Google Scholar]
- 120.Batur P, Kransdorf LN, Casey PM. Emergency Contraception. Mayo Clin Proc. 2016. Jun;91 (6):802–7. doi: 10.1016/j.mayocp.2016.02.018 [DOI] [PubMed] [Google Scholar]
- 121.Bradford VP, Graham BP, Reinert KG. Accuracy of self-reported health histories: a study. Mil Med. 1993. Apr;158 (4):263–5. [PubMed] [Google Scholar]
- 122.Kim Y-Y, Park JH, Kang H-J, Lee EJ, Ha S, Shin S-A. Level of Agreement and Factors Associated With Discrepancies Between Nationwide Medical History Questionnaires and Hospital Claims Data. J Prev Med Public Health Yebang Uihakhoe Chi. 2017. Sep;50 (5):294–302. doi: 10.3961/jpmph.17.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Futoma J, Simons M, Panch T, Doshi-Velez F, Celi LA. The myth of generalisability in clinical research and machine learning in health care. Lancet Digit Health. 2020. Sep;2 (9):e489–92. doi: 10.1016/S2589-7500(20)30186-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data Availability and Cleaning. Code for statistics and feature generation are available at A.G.'s github. Raw data are proprietary under the Data Use Agreement between UCSD and OuraRing, Inc. Access can be requested of the corresponding author, but must be reviewed on a case-by-case basis by OuraRing, Inc. Contact: request_data_access@ouraring.com.
Raw data are proprietary under the Data Use Agreement between UCSD and OuraRing, Inc. Access can be requested of the corresponding author, but must be reviewed on a case-by-case basis by OuraRing, Inc. Data were formatted in Excel 2020 and analyses were performed in MATLAB 2021a. Briefly, data were imported from the Oura database into Excel and DBT data were extracted, beginning at midnight 90 days prior to conception and ending approximately 90 days after conception. Data were padded with zeros to obtain a common set of 180 day-long temperature files. Data were cleaned in MATLAB, with any points showing near instantaneous change, as defined by local abs (derivative) > 105 as an arbitrary cutoff set to the median value of the following hour. Very low remaining values, less than 10°C were considered periods of non-wear and were replaced with blanks. Erroneously high values were not observed, with local highs within the physiological range attributable to common activities such as exercise.