Abstract
Introduction
This study aimed to identify factors associated with adjacent vertebral fracture (AVF) incidence after balloon kyphoplasty (BKP).
Methods
To perform the analyses, 133 vertebrae of 128 patients who underwent BKP for osteoporotic vertebral compression fracture were retrospectively investigated. According to the presence of AVF throughout a 1-year period following BKP, patients were divided into AVF (n = 22) and non-AVF (n = 111) groups. The groups were compared with respect to pre- and postoperative parameters, including the incidence of recompression of augmented vertebrae (RAV). RAV was defined as a decrease in anterior vertebral body height of at least 5 mm within the 3 months that followed BKP. To identify factors associated with AVF incidence, univariate and multivariate analyses were performed.
Results
The univariate analysis revealed that the AVF group had a lower cement augmentation ratio, greater preoperative wedge angle, lower preoperative vertebral body height, lower postoperative vertebral body height 3 months post-BKP, and a greater change in vertebral body height and rate of RAV than the non-AVF group. Multivariate analysis revealed that low preoperative vertebral body height and RAV occurrence were associated with AVF incidence.
Conclusions
To the best of our knowledge, this study is the first to indicate that RAV is a risk factor for AVF. Study findings indicate that the incidence of AVF can be decreased if RAV development is avoided.
Keywords: adjacent vertebral fracture, balloon kyphoplasty, osteoporotic vertebral compression fracture, recompression of augmented vertebrae
Introduction
Osteoporotic vertebral compression fractures (OVF) are a major health problem in an aging society as they cause kyphosis, back pain, restricted pulmonary function, and gastrointestinal dysfunction1). The main methods used to manage symptomatic OVF are conservative treatments, such as rest, corset use, and medication. However, despite adequate conservative treatment, some cases of severe back pain or nonunion require surgery. In older patients, OVF should be treated using procedures that are as minimally invasive as possible. Minimally invasive vertebral augmentation with balloon kyphoplasty (BKP) has become very popular2-4). Multiple previous studies have reported that BKP is a safe and effective technique for treating OVF and it significantly reduces back pain and improves quality of life5-8). However, in some rare cases, complications, including cement extrusion into the spinal canal, infection, and pulmonary embolism, have occurred after the procedure9). Relative to other complications of BKP, the incidence of adjacent vertebral fracture (AVF) is relatively high, with a postoperative rate that ranges from 6.5% to 25%1,9-14). AVF has been reported to cause revision surgery and persistent pain after vertebroplasty or BKP15-17).
Many investigators have attempted to determine risk factors for AVF after using cement augmentation techniques, including vertebroplasty or BKP. Bone mineral density (BMD), intravertebral cleft, cement leakage into a disc, and high cement volume have been reported as risk factors of AVF after vertebroplasty18-21). Preoperative compression severity, greater surgical correction, and female sex have been reported as risk factors of AVF after BKP12,15,22). Although many risk factors have been discussed, the precise identities of risk factors remain controversial.
Augmented vertebral body height loss after BKP has been reported23-26); however, its clinical significance is unknown. In this study, we referred to the height loss phenomenon after BKP as recompression of augmented vertebrae (RAV). This study aimed to identify potential risk factors of AVF after BKP.
Material and Methods
Patient selection
Clinical data of 176 patients with symptomatic OVF treated with BKP from January 2011 to October 2019 at our hospital were retrospectively collected. A total of 186 vertebrae were treated with BKP, including 164 one-level compression fractures and 11 two-level fractures. Patients who did not have X-ray follow-up data at ≥3 months post-BKP, who had missing data, and who underwent posterior instrumentation combined with BKP were excluded from the study.
Surgical procedure and postoperative care
Balloon kyphoplasty was performed using a spinal balloon device with patients under general anesthesia. Patients were placed in a prone position on a four-poster frame. A deflated balloon was inserted into the vertebral body via a bilateral transpedicular approach and inflated to restore the height of the injured vertebra and create an internal cavity. The balloon was then deflated, and the remaining cavity was filled with cement under low pressure. After surgery, patients were permitted self-ambulation as soon as possible. Back braces were applied to all patients after surgery for 1-3 months. Osteoporotic medications, including bisphosphonates, vitamin D, or parathyroid hormone, were prescribed after the procedure.
Patient data collection
Patient information, medical records, and radiological images were collected pre- and postoperatively. Patient information collected included age, sex, body mass index, conservative treatment period before BKP, and follow-up period after BKP. According to the presence of AVF within the year that followed BKP, patients were divided into AVF and non-AVF groups.
Image assessment
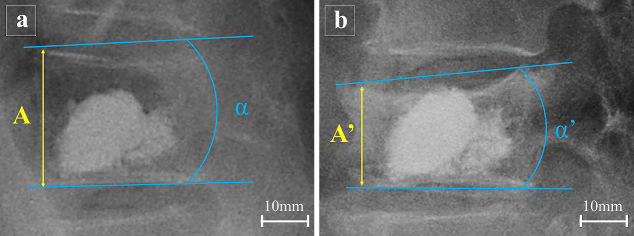
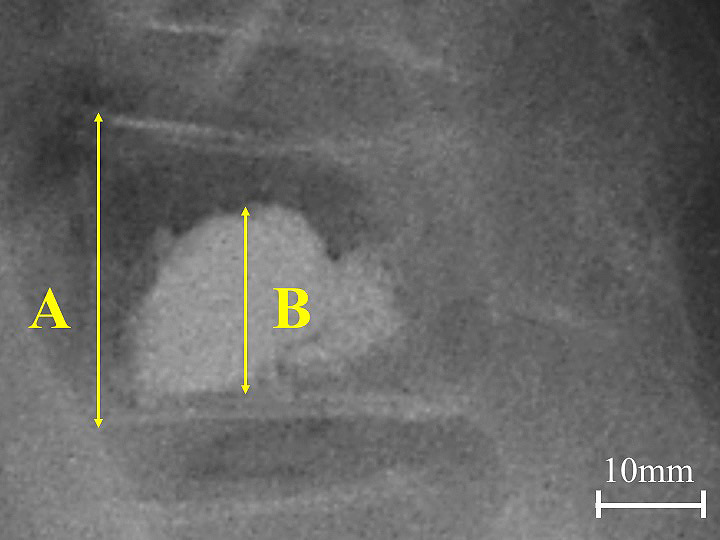
Plain radiographs were assessed based on lateral views in the lateral position before surgery and 1 week and 3 months postoperatively. All radiological parameters were measured twice by two orthopedic surgeons individually and independently (intraclass correlation coefficient > 0.8); the average of the two measurements was used. Fracture level was classified as thoracolumbar (Th11-L2) and non-thoracolumbar (Th10, L3-5). The intravertebral cleft within the injured vertebra was defined as a radiolucent shadow on lateral radiography or computed tomography. Cement leakage was defined as cement extending into disc space and was assessed via X-ray or computed tomography. Cement augmentation ratio was calculated using the following formula: [vertebral height/augmented cement height] × 100 (Fig. 1)21). The wedge angle was defined as the angle between the superior and inferior endplate of the compressed vertebra considered. Vertebral body height was measured at the anterior wall of the compressed vertebra (Fig. 2). RAV was defined as a decrease in anterior vertebral body height of at least 5 mm between 1 week and 3 months post-BKP.
Figure 1.
Calculation of cement augmentation ratio.
Anterior vertebral body height and cement height is indicated with A and B, respectively. Cement augmentation ratio was calculated via the following formula: [B/A] ×100.
Figure 2.
Measurement of vertebral body height and wedge angle.
X-rays obtained (a) 1 week postoperatively and (b) 3 months postoperatively are shown. Pre- and postoperative vertebral body height are indicated with A and A´, respectively. Pre- and postoperative wedge angle are indicated with α and α´, respectively. Change in vertebral height is A – A´ and change in wedge angle is α – α´. Recompression of augmented vertebra is defined as A – A´ ≥ 5.
Statistical analysis
All analyses were conducted using SPSS 21.0. Values of p < 0.05 were considered statistically significant. Quantitative data are presented as a mean ± standard deviation, and a Shapiro-Wilk test was used to assess the normality of the data distribution. The differences between groups in continuous variables were examined using Student's t-test and Mann-Whitney U test for parametric and nonparametric data, respectively, while categorical data were compared using the chi-square. Indices that were significantly different in the univariate analysis were inputted into the multivariate logistic regression correlation analysis to determine factors associated with AVF incidence. A stepwise method was used in the multivariate analysis. Odds ratios (ORs) and 95% confidence intervals were calculated and assessed the goodness of fitting of logistic regression models by Hosmer-Lemeshow test.
Results
A total of 133 vertebrae of 128 patients were examined in this study. The locations and numbers of treated vertebral bodies were as follows: Th10 (n = 2), Th11 (n = 5), Th12 (n = 34), L1 (n = 45), L2 (n = 25), L3 (n = 14), L4 (n = 4), and L5 (n = 4). In 22 patients (17%), AVF was identified throughout the 3- to 12-month postoperative period. The AVF and non-AVF group consisted of 22 and 111 patients, respectively. Table 1 shows baseline characteristics of the AVF and non-AVF groups. The mean age of the AVF and non-AVF group was 78.8 and 77.9 years (p = 0.44), respectively. There were no significant differences between the groups regarding sex, body mass index, preoperative conservative period before BKP, postoperative follow-up period after BKP, and incidence rates of thoracolumbar fracture (Th11-L2) and intravertebral cleft.
Table 1.
Baseline Characteristics of the AVF and Non-AVF Groups Pre- and Post-surgery.
| AVF (n=22)
Mean±SD or N (%) |
Non-AVF (n=111)
Mean±SD or N (%) |
P-value | |
|---|---|---|---|
| Age, years | 78.8±4.6 | 77.9±7.1 | 0.444 |
| Sex, female | 15 (68%) | 82 (74%) | 0.583 |
| BMI, kg/m2 | 20.1±3.6 | 22.1±4.0 | 0.126 |
| Preoperative conservative treatment period, days | 69.5±41.2 | 65.4±73 | 0.800 |
| Postoperative follow-up period, weeks | 25.5±20.2 | 24.5±20 | 0.298 |
| Thoracolumbar fracture (Th11–L2) | 21 (95%) | 88 (79%) | 0.057 |
| Intravertebral cleft | 1 (4.5%) | 21 (19%) | 0.096 |
AVF, adjacent vertebral fracture; BMI, body mass index; SD, standard deviation; N, number
Table 2 shows radiological measurements of the AVF and non-AVF groups before and after BKP. There were no significant differences between the groups regarding total cement volume and the incidence rate of cement leakage into a disc. There were no neurologic symptoms observed in cases with cement leakage. The cement augmentation ratio was lower in the AVF group (68.9%) than in the non-AVF group (73.7%, p = 0.036). The wedge angle before BKP was greater in the AVF group (15.2°) than in the non-AVF group (13.0°, p = 0.025), whereas there were no significant differences between groups regarding wedge angle 1 week and 3 months post-BKP. Vertebral body height before BKP and 3 months after BKP was lower in the AVF group than in the non-AVF group (16.7 mm vs. 20.3 mm, p < 0.01 and 17.1 mm vs. 22.1 mm, p < 0.01, respectively), whereas there was no significant vertebral body height difference observed between the groups 1 week after BKP. There were no significant differences observed between the groups in wedge angle change 1 week and 3 months after BKP; however, the vertebral body height change of the AVF group was greater than that of the non-AVF group (5.1 mm vs. 3 mm, respectively; p < 0.01). Further, the AVF group had a greater incidence rate of RAV (64%) than the non-AVF group (64% vs. 12%, respectively; p < 0.01). Thus, in univariate analysis, there were significant differences between the two groups in six indices: cement augmentation ratio, preoperative wedge angle, preoperative vertebral body height, vertebral body height at 3 months, postoperative difference of vertebral body height for 3 months, and incidence of RAV. When the six indices that statistically differed between groups were input into a multivariate logistic regression correlation, the multivariate analysis revealed that vertebral body height before BKP (OR = 0.82) and incidence of RAV (OR = 21.9) were associated with the incidence of AVF (Table 3). In addition, the Hosmer-Lemeshow test has a p-value of 0.932, indicating that the logistic regression analysis model has no fit problem.
Table 2.
Radiological Measurements for the AVF and Non-AVF Groups.
| AVF (n=22)
Mean±SD or N (%) |
Non-AVF (n=111)
Mean±SD or N (%) |
P-value | |
|---|---|---|---|
| Total cement volume, mL | 5.1±1.2 | 5.0±1.3 | 0.839 |
| Cement leakage into a disc, N (%) | 4 (18%) | 14 (13%) | 0.343 |
| Cement augmentation ratio, % | 68.9±10.1 | 73.7±9.7 | 0.036 |
| Wedge angle, degrees | |||
| Preoperatively | 15.2±3.2 | 13.0±9.7 | 0.025 |
| 1 week postoperatively | 10.4±3.8 | 9.6±6.6 | 0.395 |
| 3 months postoperatively | 13±4.4 | 11.9±6.7 | 0.322 |
| Postoperative difference at 1 week and 3 months | 2.6±2.4 | 2.4±2.4 | 0.656 |
| Vertebral body height, mm | |||
| Preoperatively | 16.7±4.4 | 20.3±5.4 | 0.004 |
| 1 week postoperatively | 22.1±3.5 | 24.1±4.6 | 0.058 |
| 3 months postoperatively | 17.1±2.7 | 22.1±3.5 | <0.001 |
| Postoperative difference at 1 week and 3 months | 5.1±2.8 | 3±2.1 | <0.001 |
| Incidence of RAV, N (%) | 14 (64%) | 13 (12%) | <0.001 |
AVF, adjacent vertebral fracture; SD, standard deviation; RAV, recompression of augmented vertebra; N, number
Table 3.
Multivariate Analysis of Factors Associated with AVF Incidence.
| OR | P-value | 95% CI | |
|---|---|---|---|
| Cement augmentation ratio | 0.587 | ||
| Wedge angle, preoperatively | 0.975 | ||
| Vertebral height, preoperatively | 0.820 | 0.002 | 0.725–0.928 |
| Vertebral body height, 3 months postoperatively | 0.307 | ||
| Postoperative vertebral body height difference at 1 week and 3 months | 0.984 | ||
| RAV | 21.891 | <0.001 | 6.219–77.058 |
AVF, adjacent vertebral fracture; RAV, recompression of augmented vertebra; OR, odds ratios; CI, confidence interval
Case presentation
The patient was a 78-year-old woman with an L2 vertebral fracture (Fig. 3a) who underwent BKP following conservative treatment. A postoperative radiograph showed improvement in the vertebral body height and wedge angle of L2, while the cancellous bone remained around the cement in the vertebral body (Fig. 3b). A postoperative radiograph, one month after BKP, showed loss of the augmented vertebral body height (Fig. 3c). She had an adjacent vertebral fracture, six months after BKP (Fig. 3d).
Figure 3.
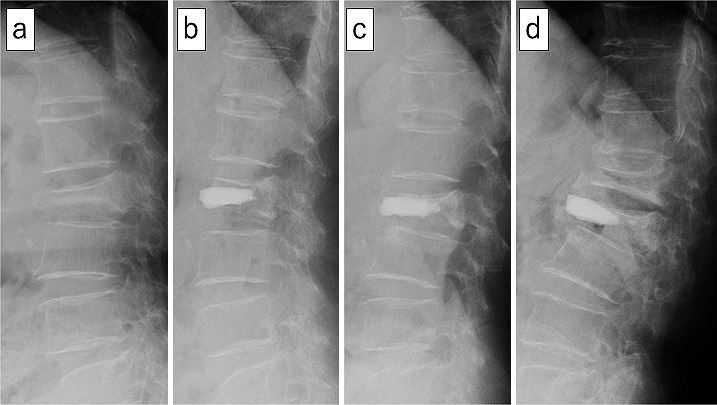
A 78-year-old woman with AVF after augmented vertebral body height loss following BKP.
(a) Preoperative radiograph (lateral view) showing the L2 vertebral fracture (vertebral body height=10 mm).
(b) Postoperative radiograph (lateral view), 1 week after BKP, showing cancellous bone remaining around the cement in the vertebral body.
(c) Postoperative radiograph (lateral view), 1 month after BKP, showing loss of augmented vertebral body height (RAV).
(d) Postoperative radiograph (lateral view), 6 months after BKP, showing an adjacent vertebral fracture at L1.
Discussion
This study retrospectively investigated risk factors that affect AVF incidence after BKP for symptomatic OVF. Via multivariate analysis, low vertebral body height before BKP and the incidence of RAV after BKP were associated with AVF incidence. Preoperative vertebral body height has previously been examined as a risk factor for AVF12,15). Meanwhile, the association between RAV and the incidence of AVF has not been previously examined. To the best of our knowledge, this study is the first to focus on the association between RAV and the incidence of AVF and the first to indicate that RAV is a risk factor for AVF.
Movrin et al. reported that BMD is a risk factor for the development of AVF after vertebroplasty or BKP13). Certainly, there is a strong relationship between bone density and bone strength, and it is reasonable to use BMD to assess AVF risk. However, there have been reports of significant differences in the prevalence of vertebral fractures among individuals with similar BMD27,28), as well as reports of no significant differences in BMD concerning the incidence of AVF after BKP12,15). In this study, we excluded BMD from the analysis due to missing data to avoid reducing the statistical power of the analysis. For reference, the preoperative DXA values were 66.9 ± 11.6 g/cm3 and 61.1 ± 11.7 g/cm3 in the AVF (n = 16) and non-AVF group (n = 91), respectively, in this study, with no significant difference.
Several studies have indicated that preoperative compression severity is associated with AVF risk12,15). Compression severity has been assessed based on wedge angle or vertebral height. Civelek et al.12) demonstrated that increased preoperative wedge angle was a risk factor of AVF after BKP but did not examine preoperative vertebral height. Takahashi et al.15) indicated that both greater preoperative wedge angle and low vertebral height were associated with AVF upon univariate analysis, but only wedge angle was identified as a significant risk factor upon multivariate analysis. Moreover, wedge angles above 25° were reported as high-risk indicators of AVF. In this study, preoperative wedge angle and vertebral height were identified as significant risk factors for AVF via univariate analysis, but only vertebral height significantly affected risk via multivariate analysis. Although wedge angle and vertebral body height are strongly correlated and are factors that indicate vertebral body collapse, when endplate deformation occurs during vertebral body collapse and the angles are not easy to measure, wedge angle measurements may not be accurate29). Therefore, we consider vertebral body height to be more suitable for assessing the risk of AVF after BKP than wedge angle.
RAV is a phenomenon in which vertebral body height is lost after BKP. Movrin et al.13) showed that the average loss of augmented vertebrae height was about 5% after BKP in the first postoperative year. Several researchers have revealed that height loss of augmented vertebra is associated with persistent low back pain and the aggravation of kyphotic deformity. Further, it was reported that 10%-30% of these effects occur in the 3-month period following BKP. Moreover, older age, intravertebral cleft, low cement volume, and low cement augmentation ratio were reported as risk factors of RAV23-26,30). However, the association between RAV and AVF incidence has not been revealed, and there is no unified name or definition for the vertebral body height loss phenomenon. In this study, we referred to vertebral body height loss as RAV and defined it as a 5 mm height loss that occurs throughout the 3-month period following BKP.
We consider RAV to be the result of cancellous bone collapse between cement and endplates. It occurs due to load stress on the cement-augmented vertebral body. Although the causes of RAV are multifactorial, the occurrence of RAV may indicate the presence of increased stress on the anterior side of the vertebra. Furthermore, the incidence of RAV increases the kyphotic angle of cement-augmented vertebrae, which may further increase stress on adjacent vertebral bodies and create a biomechanical environment in which AVF is likely to develop31). Vertebral fracture has been reported to increase compressive strain in the anterior region of the adjacent vertebrae32,33). Luo et al.34) investigated creep deformation change after vertebral fracture. Following fracture, creep deformation of the fractured vertebral body significantly increased, especially in the anterior region, and similar changes were observed at the adjacent level. In addition, Takano et al.35) revealed that vertebral fracture increased stress concentration in the affected vertebrae and the adjacent vertebrae using finite element analysis. These results suggest that AVF is caused not only by bone fragility but also by the increase in stress concentration in the adjacent vertebrae. Therefore, one of the causes of AVF may be the increase in stress concentration in the adjacent vertebrae associated with the onset of RAV.
The results of this study suggest that the incidence of AVF can be decreased if RAV development is avoided. Previous studies have shown that RAV is caused by the cancellous bone that remains between the cement and the endplate24). Because both AVF and RAV are associated with poor postoperative outcomes, the use of an adequate cementing technique, which could prevent RAV and AVF, may improve postoperative outcomes of BKP. Kobayashi et al. suggested that augmented cement should come in contact with both endplates to avoid the incidence of RAV, especially in elderly patients30). Therefore, we suggest that it is appropriate to augment cement so that it contacts the endplates of compressed vertebrae.
This study has several limitations. First, it was retrospective, which can introduce bias and errors. Second, the postoperative follow-up periods considered were not consistent and ranged widely from 3 to 12 months. However, there was no significant difference in the postoperative follow-up period between groups (Table 1). Therefore, this limitation was not likely to influence findings. Third, the definition of RAV has not been determined. Finally, we did not evaluate BMD and osteoporotic medications in this study due to missing data. Despite these limitations, this study provides important information regarding the association between RAV after BKP and subsequent AVF.
Conclusion
The retrospective assessment of 128 patients with symptomatic OVF treated with BKP identified low preoperative vertebral body height and RAV occurrence as significant risk factors associated with AVF incidence. This study is the first to indicate that RAV is a risk factor of AVF and suggests that AVF can be decreased if RAV development is avoided.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contributions: Yohei Yamada and Satoshi Kato wrote and prepared the manuscript, and all the authors participated in the study design.
Ethical Approval: Ethical approval was waived by the ethics committee due to the retrospective study design.
Informed Consent: Informed consent for publication was obtained by all participants in this study.
References
- 1.Frankel BM, Monroe T, Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007;7(5):575-82. [DOI] [PubMed] [Google Scholar]
- 2.Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31(17):1983-2001. [DOI] [PubMed] [Google Scholar]
- 3.Klazen CA, Lohle PN, Vries J de, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376(9746):1085-92. [DOI] [PubMed] [Google Scholar]
- 4.Zhang T. Does percutaneous vertebroplasty or balloon kyphoplasty for osteoporotic vertebral compression fractures increase the incidence of new vertebral fractures? A meta-analysis. Pain Phys. 2017;20(1):E13-28. [PubMed] [Google Scholar]
- 5.Bouza C, López T, Magro A, et al. Efficacy and safety of balloon kyphoplasty in the treatment of vertebral compression fractures: a systematic review. Eur Spine J. 2006;15(7):1050-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hadjipavlou AG, Tzermiadianos MN, Katonis PG, et al. Percutaneous vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures and osteolytic tumours. J Bone Jt Surg Br. 2005;87(12):1595-604. [DOI] [PubMed] [Google Scholar]
- 7.Taylor RS, Fritzell P, Taylor RJ. Balloon kyphoplasty in the management of vertebral compression fractures: an updated systematic review and meta-analysis. Eur Spine J. 2007;16(8):1085-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garfin SR, Buckley RA, Ledlie J, et al. Balloon Kyphoplasty for symptomatic vertebral body compression fractures results in rapid, significant, and sustained improvements in back pain, function, and quality of life for elderly patients. Spine. 2006;31(19):2213-20. [DOI] [PubMed] [Google Scholar]
- 9.Pflugmacher R, Schroeder RJ, Klostermann CK. Incidence of adjacent vertebral fractures in patients treated with balloon kyphoplasty: two years' prospective follow-up. Acta Radiol. 2006;47(8):830-40. [DOI] [PubMed] [Google Scholar]
- 10.Fribourg D, Tang C, Sra P, et al. Incidence of subsequent vertebral fracture after kyphoplasty. Spine. 2004;29(20):2270-7. [DOI] [PubMed] [Google Scholar]
- 11.Campbell PG, Harrop JS. Incidence of fracture in adjacent levels in patients treated with balloon kyphoplasty: a review of the literature. Curr Rev Musculoskelet Med. 2008;1(1):61-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Civelek E, Cansever T, Yilmaz C, et al. The retrospective analysis of the effect of balloon Kyphoplasty to the adjacent-segment fracture in 171 patients. J Spinal Disord Tech. 2014;27(2):98-104. [DOI] [PubMed] [Google Scholar]
- 13.Movrin I, Vengust R, Komadina R. Adjacent vertebral fractures after percutaneous vertebral augmentation of osteoporotic vertebral compression fracture: a comparison of balloon kyphoplasty and vertebroplasty. Arch Orthop Trauma Surg. 2010;130(9):1157-66. [DOI] [PubMed] [Google Scholar]
- 14.Harrop JS, Prpa B, Reinhardt MK, et al. Primary and secondary osteoporosis' incidence of subsequent vertebral compression fractures after kyphoplasty. Spine. 2004;29(19):2120-5. [DOI] [PubMed] [Google Scholar]
- 15.Takahashi S, Hoshino M, Yasuda H, et al. Development of a scoring system for predicting adjacent vertebral fracture after balloon kyphoplasty. Spine J. 2019;19(7):1194-201. [DOI] [PubMed] [Google Scholar]
- 16.Yang SC, Chen WJ, Yu SW, et al. Revision strategies for complications and failure of vertebroplasties. Eur Spine J. 2008;17(7):982-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Faciszewski T, McKiernan F. Calling all vertebral fractures classification of vertebral compression fractures: a consensus for comparison of treatment and outcome. J Bone Miner Res. 2002;17(2):185-91. [DOI] [PubMed] [Google Scholar]
- 18.Lu K, Liang CL, Hsieh CH, et al. Risk factors of subsequent vertebral compression fractures after vertebroplasty. Pain Med. 2012;13(3):376-82. [DOI] [PubMed] [Google Scholar]
- 19.Takahara K, Kamimura M, Moriya H, et al. Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women. BMC Musculoskelet Disord. 2016;17(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li YA, Lin CL, Chang MC, et al. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine. 2012;37(3):179-83. [DOI] [PubMed] [Google Scholar]
- 21.Lin EP, Ekholm S, Hiwatashi A, et al. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25(2):175-80. [PMC free article] [PubMed] [Google Scholar]
- 22.Spross C, Aghayev E, Kocher R, et al. Incidence and risk factors for early adjacent vertebral fractures after balloon kyphoplasty for osteoporotic fractures: analysis of the SWISSspine registry. Eur Spine J. 2014;23(6):1332-8. [DOI] [PubMed] [Google Scholar]
- 23.Li YX, Guo DQ, Zhang SC, et al. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42(9):2131-9. [DOI] [PubMed] [Google Scholar]
- 24.Kim YY, Rhyu KW. Recompression of vertebral body after balloon kyphoplasty for osteoporotic vertebral compression fracture. Eur Spine J. 2010;19(11):1907-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Song J, Ding L, Chen J, et al. The filling proportion of bone cement affects recollapse of vertebrae after percutaneous vertebral augmentation: a retrospective cohort study. Int J Surg. 2017;47:33-8. [DOI] [PubMed] [Google Scholar]
- 26.Yu WB, Jiang XB, Liang D, et al. Risk factors and score for recollapse of the augmented vertebrae after percutaneous vertebroplasty in osteoporotic vertebral compression fractures. Osteoporos Int. 2019;30(2):423-30. [DOI] [PubMed] [Google Scholar]
- 27.Mitra D, Elvins DM, Speden DJ, et al. The prevalence of vertebral fractures in mild ankylosing spondylitis and their relationship to bone mineral density. Rheumatology. 2000;39(1):85-9. [DOI] [PubMed] [Google Scholar]
- 28.Legrand E, Chappard D, Pascaretti C, et al. Trabecular bone microarchitecture, bone mineral density, and vertebral fractures in male osteoporosis. J Bone Miner Res. 2000;15(1):13-9. [DOI] [PubMed] [Google Scholar]
- 29.Hsu WE, Su KC, Chen KH, et al. The evaluation of different radiological measurement parameters of the degree of collapse of the vertebral body in vertebral compression fractures. Appl Bionics Biomech. 2019;2019:4021-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kobayashi M, Toribatake Y, Okamoto S, et al. Insufficient augmentation of bone cement causes recompression of augmented vertebra after balloon kyphoplasty. Spine Surg Relat Res. 2021;5(6):375-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klotzbuecher CM, Ross PD, Landsman PB, et al. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15(4):721-39. [DOI] [PubMed] [Google Scholar]
- 32.Ciarelli TE, Fyhrie DP, Parfitt AM. Effects of vertebral bone fragility and bone formation rate on the mineralization levels of cancellous bone from white females. Bone. 2003;32(3):311-5. [DOI] [PubMed] [Google Scholar]
- 33.Tzermiadianos MN, Renner SM, Phillips FM, et al. Altered disc pressure profile after an osteoporotic vertebral fracture is a risk factor for adjacent vertebral body fracture. Eur Spine J. 2008;17(11):1522-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo J, Annesley-Williams DJ, Adams MA, et al. How are adjacent spinal levels affected by vertebral fracture and by vertebroplasty? A biomechanical study on cadaveric spines. Spine J. 2017;17(6):863-74. [DOI] [PubMed] [Google Scholar]
- 35.Takano H, Yonezawa I, Todo M, et al. Biomechanical study of vertebral compression fracture using finite element analysis. J Appl Math Phys. 2017;5(4):953-65. [Google Scholar]