Hibernoma is a rare benign soft tissue tumor originating from the remnants of fetal brown fat1). It is most frequently seen in areas in which there is a preponderance of brown fat, such as thigh, shoulder, back, neck, and mediastinum2). Hibernoma in the epidural space is extremely rare with only one case reported in the literature3). Herein, we report another case of epidural hibernoma and discuss the clinical, radiographical, and pathological features of this unusual entity.
A 56-year-old previously healthy man presented to the urology outpatient clinic with new onset of progressive lower urinary tract symptoms over 14 months. He had no voiding symptoms. Ultrasound of the urinary tract and prostate-specific antigen level were normal. He complained of lumbar pain associated with bilateral symmetrical paresthesias of the lower limbs mainly in the dorsum of the foot and toes. The paresthesias were fluctuating with nocturnal aggravation. These neurologic symptoms occurred a few months before the onset of urological symptoms. Urodynamic study demonstrated an overactive bladder. The patient was referred to the neurosurgery clinic to rule out spinal pathology.
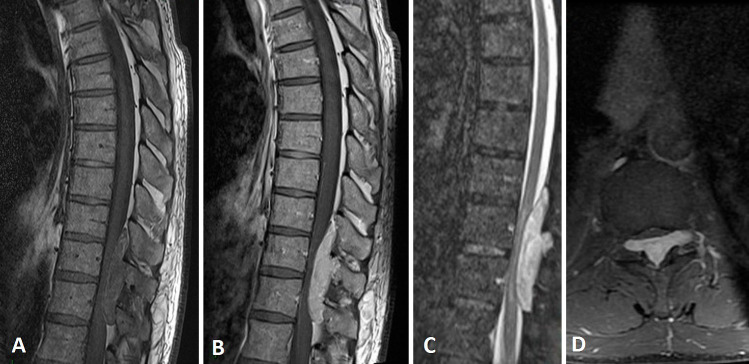
The neurologic exam revealed hypoesthesia on pinprick stimulation and altered two-point discrimination on the dorsum of the foot. There was no proprioceptive pain, temperature sensation, or motor deficit. Magnetic resonance imaging of the spine showed an atypical epidural posterior lesion at the level of T10-T11 compressing the cord. The lesion was isointense when homogenously enhanced with gadolinium on T1-weighted images and hyperintense on short tau inversion recovery (Fig. 1).
Figure 1.
Preoperative sagittal magnetic resonance imaging of the spine shows an atypical extradural posterior lesion at the level of T10-T11 compressing the cord, which is isointense on T1-weighted image (A), homogenously enhanced with gadolinium (B), and hyperintense on short tau inversion recovery (C). The tumor extended into lateral recesses bilaterally at the level of T10-T11 as shown on the axial view (D).
The case was discussed in a spine tumor board meeting and the decision was taken to proceed with lesion resection. Medullary arteriography was performed preoperatively and the artery of Adamkiewicz was at the level of T12 on the left side.
The patient was taken to the operating room. A posterior midline approach was performed. Microscopic laminectomy T10-T11-T12 revealed a well-circumscribed mass occupying the dorsal epidural space, compressing the dural sac, and extending into lateral recesses bilaterally. It was dissected from the dura matter and completely resected (Fig. 2).
Figure 2.

Picture of the resected epidural firm red-yellowish fatty mass measuring ~5 cm in the craniocaudal direction.
On microscopic examination, the tumor was found to be composed of a large number of brown fat cells with round centrally placed nuclei, prominent nucleoli, and abundant and finely vacuolated cytoplasm (Fig. 3).
Figure 3.
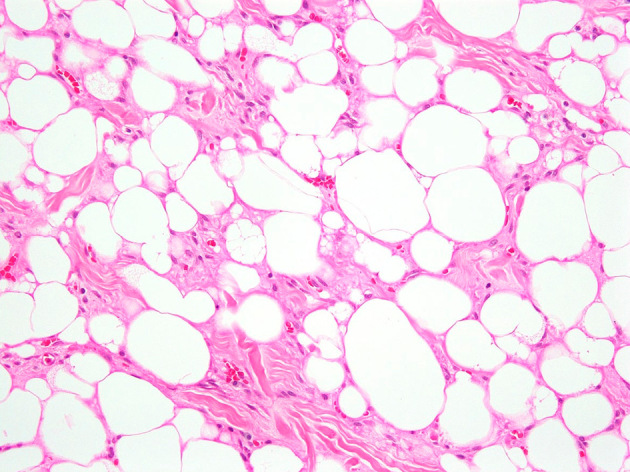
Photomicrograph of the excision specimen showing a hibernoma with the typical features of a prominent mixture of adipocytes of fetal type. Numerous multivacuolated adipocytes and smaller polygonal cells with abundant cytoplasm are noted, which are characteristic of typical hibernoma (hematoxylin and eosin stain, original magnification 200×).
The patient was seen in the outpatient clinic 6 weeks after discharge and his neurologic symptoms were markedly improved. Magnetic resonance images at the latest follow-up 6 months after the surgery confirmed the absence of any residual disease or medullary compression (Fig. 4).
Figure 4.
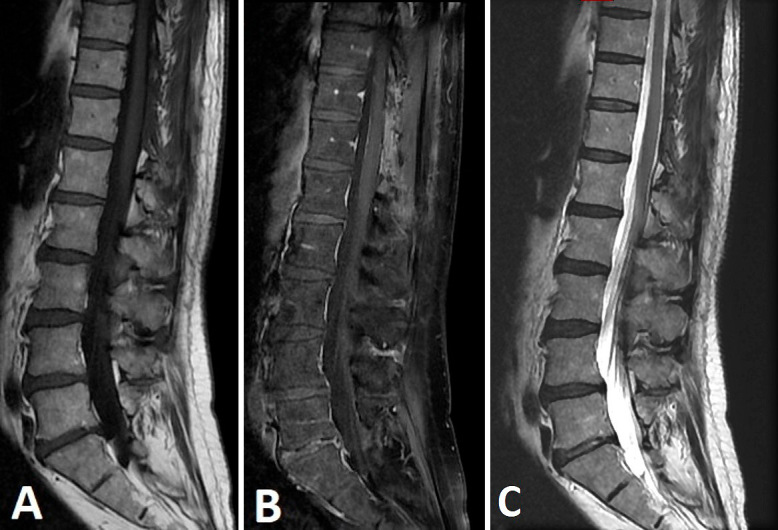
Postoperative sagittal T1-weighted image before (A) and after gadolinium (B), and T2-weighted (C) magnetic resonance imaging of the spinal cord at the 6-month follow-up showing the absence of any residual contrast uptake or medullary compression.
Hibernoma is rarely reported in the literature as a spinal tumor, with only two cases of intradural extramedullary mass and one case of epidural mass. Shuangshott et al. reported the first case of subdural hibernoma in 1974, in which a 14-year-old boy had a subdural mass that extended from the third to the fifth lumbar vertebrae with compression of the cauda equine and spina bifida of the fifth lumbar vertebra4). In 1988, Perling et al. described the first case of epidural hibernoma as a complication of corticosteroid treatment for juvenile rheumatoid arthritis in a 6-year-old boy3). Chitoku et al. reported in 1998 a case of spinal hibernoma as an intradural extramedullary mass at C7 in a 35-year-old lady5). Other cases of spinal hibernomas are mainly intraosseous in the thoracic, lumbar vertebrae, and sacrum6-9).
To the best of our knowledge, this is only the second case of spinal hibernoma reported in the literature as an epidural mass. Our patient had inexplicable storage urinary symptoms. Further, he was not taking corticosteroid drugs as documented in the case reported by Perling et al. This may question the origin of the spinal hibernoma as a distinct entity from epidural lipomatosis.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: None.
Author Contributions: All authors contributed equally to this manuscript. All of the authors have read, reviewed, and approved the manuscript.
Ethical Approval: This article does not contain any studies with human participants performed by any of the authors.
Informed Consent: Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
References
- 1.Klevos G, Jose J, Pretell-Mazzini J, et al. Hibernoma. Am J Orthop (Belle Mead NJ). 2015;44(6):284-7. [PubMed] [Google Scholar]
- 2.Furlong MA, Fanburg-Smith JC, Miettinen M. The morphologic spectrum of hibernoma: a clinicopathologic study of 170 cases. Am J Surg Pathol. 2001;25(6):809-14. [DOI] [PubMed] [Google Scholar]
- 3.Perling LH, Laurent JP, Cheek WR. Epidural hibernoma as a complication of corticosteroid treatment: case report. J Neurosurg. 1988;69(4):613-6. [DOI] [PubMed] [Google Scholar]
- 4.Shuangshott S, Menakanit W. Intraspinal hibernoma. Br J Surg. 1974;61(7):580-2. [DOI] [PubMed] [Google Scholar]
- 5.Chitoku S, Kawai S, Watabe Y, et al. Intradural spinal hibernoma: case report. Surg Neurol. 1998;49(5):509-13. [DOI] [PubMed] [Google Scholar]
- 6.Hafeez I, Shankman S, Michnovicz J, et al. Intraosseous hibernoma: a case report and review of the literature. Spine (Phila Pa 1976). 2015;40(9):E558-61. [DOI] [PubMed] [Google Scholar]
- 7.Westacott L, Collins A, Dickenson I. Intraosseous hibernoma in the sacrum of an adult. Int J Surg Pathol. 2016;24(8):749-52. [DOI] [PubMed] [Google Scholar]
- 8.Myslicki FA, Rosenberg AE, Chaitowitz I, et al. Intraosseous hibernoma: five cases and a review of the literature. J Comput Assist Tomogr. 2019;43(5):793-8. [DOI] [PubMed] [Google Scholar]
- 9.Kumar R, Deaver MT, Czerniak BA, et al. Intraosseous hibernoma. Skeletal Radiol. 2011;40(5):641-5. [DOI] [PubMed] [Google Scholar]