Lumbar disc herniation is a common disease, but the incidence of extraforaminal and intraforaminal disc herniation is relatively rare1). In particular, L1-L2 extraforaminal disc herniation is extremely rare, and to the best of our knowledge, there are no reports of pure L1 radiculopathy caused by L1-L2 extraforaminal disc herniation. This case presents that L1 radiculopathy causes meralgia paresthetica-like pain and radiating buttock pain, thus providing useful guidance for clinicians and future researchers.
A 43-year-old Japanese man initially presented with slight left back pain when practicing a golf swing. His left back pain improved within a week, but left anterolateral thigh, groin, and buttock pain appeared and progressively worsened. Two weeks later, he was taken to a hospital in an ambulance due to severe left anterolateral thigh pain. Initial conservative therapy consisting of nonsteroidal anti-inflammatory drugs and epidural nerve block failed. Two days after admission, he was transferred to our hospital for specialized treatment.
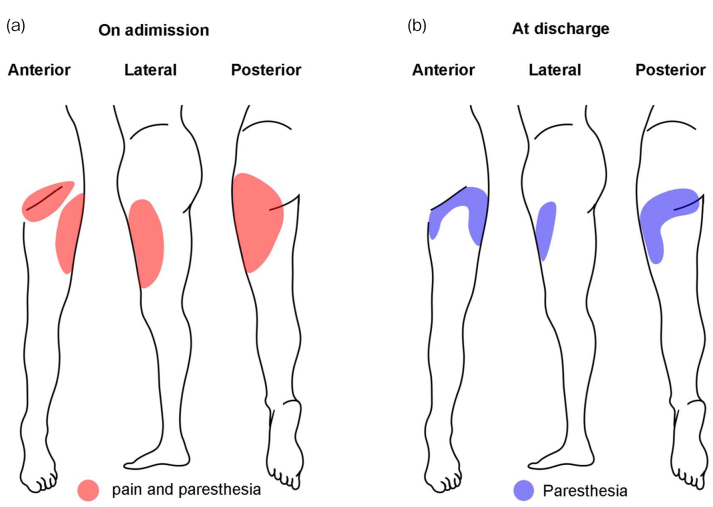
Lower limb neurological examination revealed no motor deficit with normal deep tendon reflexes. Sensory examination revealed paresthesia and pain in the left buttock, proximal anterolateral thigh, and groin area, but no clear hypesthesia (Fig. 1).
Figure 1.
Distribution of pain and paresthesia.
The area of pain was drawn by the patient before (a) and after the treatment (b). Drawings demonstrate pain and paresthesia on the proximal anterolateral thigh and groin area, similar to meralgia paresthesia (a). The pain was relieved immediately after the surgery (b). Red: pain and paresthesia; blue: paresthesia.
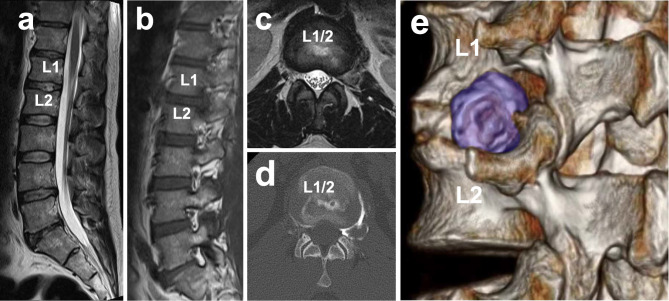
Lumbar spine radiographs showed no transitional vertebra or instability in the lumbar spine. Magnetic resonance imaging (MRI) and disco-computed tomography (CT) revealed a large left extraforaminal herniated nucleus pulposus at L1-L2 with compression of the L1 nerve root (Fig. 2). There was no other nerve root compression, with no spinal canal stenosis or foraminal stenosis.
Figure 2.
Magnetic resonance imaging (MRI) and disco-computed tomography (CT).
Sagittal T2-weighted image reveals no spinal canal stenosis (a). Left paramedian sagittal T1-weighted MRI image reveals no foraminal stenosis or intraforaminal herniation other than the L1–L2 disc level (b). Axial T2-weighted MRI at the L1–L2 level reveals far lateral disc herniation without paramedian disc herniation (c). Axial disco-CT view (d) and three-dimensional reconstructed CT image (e) reveal leakage of the contrast medium only into the extra and intraforaminal region from the L1–L2 disc level. Blue; herniated disc.
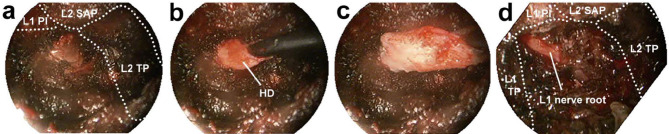
His initial Oswestry disability index (ODI) was 40%. The visual analog scale (VAS) for pain and numbness in the buttock and lower limb were both 6/10. On the day of admission, the patient received a selective left L1 root block under fluoroscopic guidance. Selective nerve root block was effective and provided immediate relief of all pain (VAS-pain, 1-2/10), but these symptoms exacerbated the next day. Microendoscopic discectomy was performed 10 days after admission (Fig. 3). Immediately after the surgery, all his pain was relieved although the patient complained of slight paresthesia on the left buttock, groin, and proximal anterolateral thigh. The patient left the hospital without any preoperative pain 6 days after the surgery (ODI, 0%; VAS-pain, 0/10; VAS-numbness, 1/10). Three months after the surgery, VAS numbness improved and was rated as 0/10.
Figure 3.
Microendoscopic discetomy (MED).
The patient was placed in a prone position under general anesthesia. An ~18-mm skin incision was made 45 mm lateral to the midline on the L1–L2 disc level. Through the incision, the paraspinal muscles were gently stripped. Then, an endoscopic obturator is inserted and directed using fluoroscopy till the bony junction of pars interarticularis (PI) with the transverse process (TP) of the L1 lumbar vertebrae. The obturator is then removed, followed by the insertion of an endoscopic working sheath and an endoscope. Under endoscopic visualization, soft tissues were dissected on L1 PI, L2 superior process (SAP), and L1 and L2 TPs. Then, drilling is started at the lateral end of PI and TP. During removal of the intertransverse process ligament, a ruptured disc was founded (a) and then removed, and huge and small pieces of herniated discs (HD) were resected (c, d) followed by confirmed no compression for the L1 nerve root (d). Left; Cranial, Right; Caudal.
L1-L2 extraforaminal disc herniation and T12-L1 paramedian disc herniation can cause L1 radiculopathy. However, T12-L1 paramedian disc herniation often compresses multiple roots, resulting in multiradiculopathies2,3). Thus, only L1-L2 extraforaminal disc herniation potentially leads to pure L1 radiculopathy. In this case, L1-L2 extraforaminal disc herniation entrapped only the L1 nerve root without any other lumbar nerve root compression on MRI. Additional disco-CT and selective diagnostic nerve root block could improve the diagnostic accuracy. Furthermore, surgical discectomy immediately relieved all pain, providing the evidence that L1 entrapment by the L1-L2 extraforaminal disc herniation causes all his symptoms.
All previously reported far-lateral L1-L2 disc herniation contains L1-L2 central or paramedian disc herniation, which can be referred to as radiculopathy of other nerve roots4), and thus, it remains controversial whether L1 radiculopathy causes meralgia paresthetica-like pain4,5). This patient had pain and paresthesia in the ilioinguinal, genitofemoral, and lateral femoral cutaneous nerve areas (meralgia paresthetica-like pain), supporting the findings of a previous study4). Additionally, the patient experienced radiating pain in the left buttock area. This buttock pain would be caused by compression of lateral branches of lumbar dorsal rami of the L1 nerve root, which compose the superior cluneal nerve and innervate the upper-lateral and medial surface of the buttock6). Therefore, radiating buttock pain would help distinguish L1 radiculopathy from meralgia paresthetica.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Grant-in-Aid for Scientific Research (C).
Author Contributions: H.K. contributed to the acquisition of data, designed, interpreted results, and wrote and prepared the manuscript. Y.N. and K.H. contributed to interpreted results. All authors read and approved the final manuscript.
Ethical Approval: This study was approved by the Kyushu University Institutional Review Board (IRB approval No.29-411).
Informed Consent: The patient provided informed consent in this study.
References
- 1.Porchet F, Fankhauser H, De Tribolet N. Extreme lateral lumbar disc herniation: clinical presentation in 178 patients. Acta Neurochir. 1994;127(3-4):203-9. [DOI] [PubMed] [Google Scholar]
- 2.Tokuhashi Y, Matsuzaki H, Uematsu Y, et al. Symptoms of thoracolumbar junction disc herniation. Spine. 2001;26(22):E512-8. [DOI] [PubMed] [Google Scholar]
- 3.Golbakhsh M, Mottaghi A, Zarei M. Lower thoracic disc herniation mimicking lower lumbar disk disease: a case report. Med J Islam Repub Iran. 2017;31:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang SN, Kim DH. L1 Radiculopathy mimicking meralgia paresthetica: a case report. Muscle Nerve. 2010;41(4):566-8. [DOI] [PubMed] [Google Scholar]
- 5.Yang SN, Kim DH. L2 rather than L1 radiculopathy mimics meralgia paresthetica reply. Muscle Nerve. 2010;42(5):842. [DOI] [PubMed] [Google Scholar]
- 6.Maigne JY, Doursounian L. Entrapment neuropathy of the medial superior cluneal nerve: nineteen cases surgically treated, with a minimum of 2 years' follow-up. Spine. 1997;22(10):1156-9. [DOI] [PubMed] [Google Scholar]