Abstract
Background
Occlusal splints are routinely used in dental offices to diagnose and treat abnormalities of the masticatory system. There are different occlusal splints, each of which can address various conditions. They may treat individuals with temporomandibular disorders (TMDs) and bruxism or be used for occlusal stabilization and dentition wear reduction.
Methods
The literature in the National Library of Medicine's Medline Database was reviewed using the Mesh terms 'occlusal splints' AND 'Temporomandibular Disorders.
Conclusion
Occlusal splints can treat a wide variety of TMDs. They can treat bruxism, headaches, postural imbalances related to TMDs, and decreased vertical dimension of occlusion (VDO). However, there is no clear evidence that occlusal splints are superior to physiotherapy in treating TMDs. In the long-term follow-up, they were equally effective as other therapies.
Keywords: Occlusal splint, Temporomandibular disorders, Night guard, Stabilization splint, Temporomandibular joint disorders
Abbreviations: TMD, Temporomandibular disorder; TMJ, Temporomandibular joint; ICP, Intercuspal position; VDO, Vertical dimension of occlusion; AADR, American Association for Dental Research
1. Introduction
Occlusal splints, known as night guards, orthotics appliances, and oral appliances, are used frequently in dental practices (Crout, 2017). There are many types of occlusal splints, each of which can be used to address various conditions. Occlusal splints are beneficial for reducing tension, decreasing muscle activity, and preventing harmful effects caused by bruxism and temporomandibular disorders (TMDs). Treatment options for TMDs include reassurance, patient education, occlusal splint therapy, or physiotherapy. Dylina et al. defined occlusal splint therapy as “the art and science of establishing neuromuscular harmony in the masticatory system and creating a mechanical disadvantage for parafunctional forces with removable appliances” (Dylina, 2001). It can treat individuals with TMD and bruxism for occlusal stabilization and to reduce dentition wear (Yadav & Karani, 2011).
Additionally, it aids in diagnosing and treating various masticatory system disorders (Yadav & Karani, 2011). It disperses stress on individual teeth by leveraging a larger surface area encompassing all arch teeth (Yadav & Karani, 2011). Consequently, the strain was evenly distributed, and muscular symmetry was attained (Yadav & Karani, 2011). The primary goal of occlusal splint therapy is to protect temporomandibular joint (TMJ) discs from dysfunctional stresses that can result in perforations or permanent displacements (Yadav & Karani, 2011). It has been demonstrated that occlusal splints considerably reduce TMD symptoms in most patients (Yadav & Karani, 2011). They are also frequently used to treat patients with internal derangement and other TMDs that cause tension-type headaches and cervical, neck, and orofacial pain (ASH, 1986, Attanasio, 1997, Boero, 1989, Nelson, 1995). Other therapeutic objectives include enhancing jaw muscle function and decreasing associated pain by establishing a stable, balanced occlusion (Dylina, 2001). Before determining the role of splint therapy in each patient, thorough examination and differential diagnosis are required.
2. Materials and methods
A literature search of the National Library of Medicine's Medline Database was conducted through PubMed in August 2022. This search used the Mesh terms 'occlusal splint' and 'Temporomandibular Disorders' to retrieve all available articles in the literature written in the English language.
Given the expected low number of articles dealing with the association of interest, all the articles in the search output were included in this review. This was independent of study type and quality. The only exclusion criterion was whether the article topic was unrelated to the research question. All articles were retrieved as full text. In addition, all reference lists were screened for articles that might be relevant to this review but did not surface in the search output. Lastly, a thorough search was performed on Google Scholar, but it did not yield any more articles on the subject of this review.
3. Discussion
3.1. Occlusal splint working mechanism:
Occlusal splints prevent patients from achieving maximum intercuspation (Yadav & Karani, 2011). Therefore, the patient must position his jaw properly with stops of equal intensity on all teeth, which facilitates the seating of the condyle in centric relation (Capp, 1999, Dylina, 2001, Ré et al., 2009). Thus, it produces new muscle and articular balance (Ré et al., 2009, Yadav and Karani, 2011). The conventional course of the intercuspal position (ICP) is disrupted by separating the teeth and reducing the direct influence of cuspal inclination (Capp, 1999). Therefore, the patient's habits will be disrupted, and they will no longer clench their teeth, protecting their TMJ, teeth, and associated structures (Ré et al., 2009).
3.2. Occlusal splint Indications:
-
•
Patients with masticatory myalgia or TMJ arthralgia (Yadav & Karani, 2011).
-
•
Patients with myospasms or myositis (Yadav & Karani, 2011).
-
•
Patients with a history of trauma or inflammatory joint conditions and existing causes of parafunctional activity, such as bruxism (Dylina, 2001, Gibreel et al., 2021, Yadav and Karani, 2011).
-
•
Patients with unstable occlusion (Yadav & Karani, 2011).
-
•
Patients with stress-related pain symptoms, such as tension headaches and neck pain of muscular origin (Dylina, 2001, Gibreel et al., 2021, Kurita et al., 1997, Solberg et al., 1975, Yadav and Karani, 2011).
3.3. Occlusal splint types:
Classification of occlusal splints, according to Dawson (Dawson, 1989), includes:
-
•
Permissive Splints
-
•
Directive Splints (Non-Permissive Splints)
-
•
Pseudo Permissive Splints
3.3.1. Permissive splints
This permits complete separation of the condyles with uniform tooth contact (Alqutaibi & Aboalrejal, 2015). This eliminates the source and impact of muscle coordination issues (Yadav & Karani, 2011). It achieves balanced muscular function and eliminates abnormal occlusal contact (by reducing parafunctional activity) (Kui et al., 2020). This work modifies the occlusion so that the teeth no longer impede the entire seating of the condyles (Kui et al., 2020). Consequently, muscular activity can also be controlled (Kui et al., 2020).
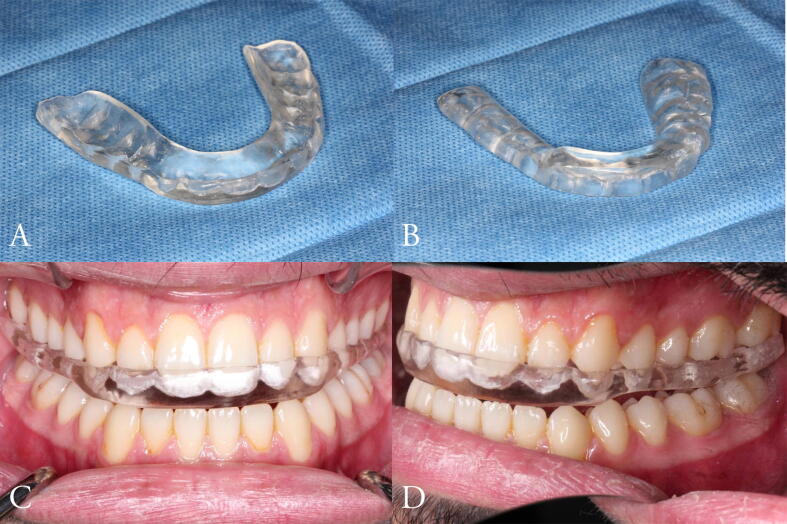
3.3.1.1. Flat plane stabilizing appliance (The Michigan Splint)
It increases occlusal stability, muscle relaxation, mandibular posture deprogramming, and vertical dimension modification (Alqutaibi & Aboalrejal, 2015). Indications for the Michigan splint include TMJ and muscle disorders and pain, severe bruxism, diagnosis and treatment of trauma from occlusion to any part of the masticatory system, and the establishment of optimal condylar positions before definitive occlusion (Alqutaibi and Aboalrejal, 2015, Ramfjord and Ash, 1994). Following dental rehabilitation or orthodontic treatment, it is not necessary to maintain the vertical dimensions of the splint (RAMFJORD & ASH, 1994). If the Michigan splint is too thick, swallowing, lip sealing, or speech may be impeded (RAMFJORD & ASH, 1994). (Fig. 1).
Fig. 1.
A. Michigan Splint. B. Frontal view of the Michigan Splint. C. Lateral view of the Michigan Splint.
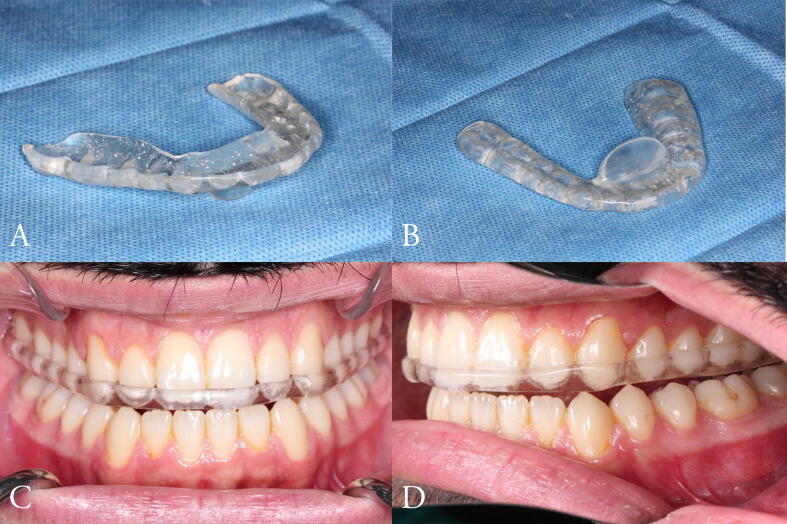
3.3.1.2. Anterior Bite Plane
They are used in the event of muscular disorders related to orthopedic instability or a sudden change in the occlusal state (Alqutaibi & Aboalrejal, 2015). It disengages all teeth except the incisors, reducing the clenching force on muscles, parafunctional movement, and TMJ strain (Alqutaibi & Aboalrejal, 2015). It prevents clenching by preventing the posterior teeth from performing functional or parafunctional behaviors (Kui et al., 2020). (Fig. 2).
Fig. 2.
A,B. Anterior Bite Plane. C. Frontal view of the Anterior Bite Plane. D. Lateral view of the Anterior Bite Plane.
3.3.2. Directive splints (non-permissive splints)
Align or place condyle-disc assemblies (Alqutaibi & Aboalrejal, 2015). It should only be used when a certain condylar location is necessary (Yadav & Karani, 2011). When joint pain occurs, the splint moves the mandible forward. These splints are helpful in two clinical situations: severe trauma with retrodiscal effusion and painful disk displacements that do not go away(Kui et al., 2020).
3.3.2.1. Anterior repositioning splint
It treats reciprocal clicking, stabilizes the condyle-disk relationship, and reduces retrodiscal tissue compression by moving the condyle away from the fully seated joint position (Alqutaibi & Aboalrejal, 2015). The beneficial effects of the anterior repositioning splint on the TMJ are pain and noise reduction and mandibular function improvement in patients with arthrogenous TMDs, which may be attributed to restoring normal disc-condyle relationship (Al-Moraissi et al., 2020, Boero, 1989). (Fig. 3).
Fig. 3.
A,B. Anterior Repositioning Splint. C. Frontal view of the Anterior Repositioning Splint. D. Lateral view of the Anterior Repositioning Splint.
3.3.2.2. Posterior bite plane
This appliance aims to achieve a horizontal maxillomandibular relationship, major vertical dimension changes, and mandibular repositioning (Alqutaibi & Aboalrejal, 2015). It is indicated in cases of severe loss of vertical dimension of occlusion (VDO) or when significant changes in the anterior positioning of the mandible are required, as it is placed only on the posterior teeth, disoccluding the anterior teeth; However, there is no significant scientific evidence, although some authors have reported that this type of splint may improve athletic performance by increasing physical strength (Alqutaibi & Aboalrejal, 2015). (Fig. 4).
Fig. 4.
A. Posterior Bite Plane. B. Frontal view of the Posterior Bite Plane. C. Lateral view of the Posterior Bite Plane.
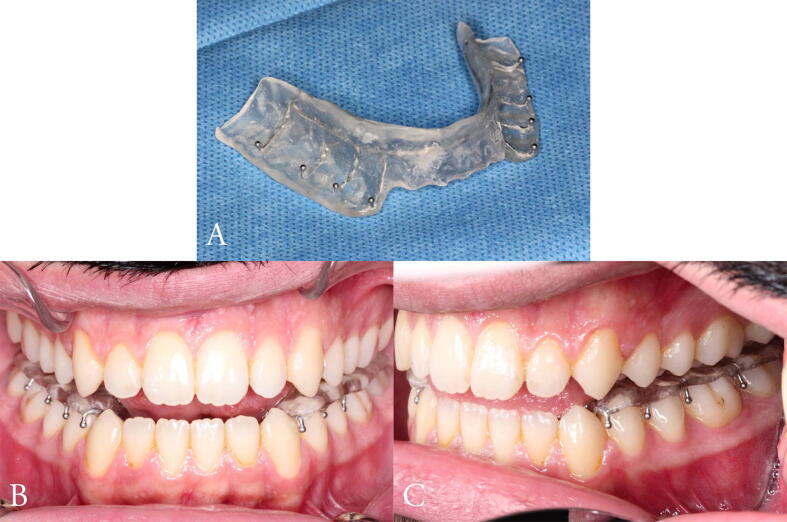
3.3.2.3. Distraction splint (Pivot Appliance)
A mandibular splint makes occlusal contact only with the most posterior teeth (Alqutaibi and Aboalrejal, 2015, Boero, 1989). Fig. 5. It can treat internal disc derangements and intracapsular inflammation (Alqutaibi & Aboalrejal, 2015). Upon clenching the splint, the condyle is pulled downward, which removes the traumatic load and allows the disc to regain its normal position (Alqutaibi and Aboalrejal, 2015, Boero, 1989). As the mandible rotates around the splint, it reduces pressure within the TMJ by unloading the joints(Kui et al., 2020). In addition, it can be used as a unilateral pivot appliance with only unilateral occlusal contact, which is placed as far back as possible. When the mouth is closed, the pivot loads the TMJ on the opposite side and slightly unloads the TMJ on the same side (Kui et al., 2020).
Fig. 5.
A. Distraction Splint. B. Frontal view of the Distraction Splint. C. Lateral view of the Distraction Splint.
3.3.3. Pseudo permissive splints:
They are usually fabricated from resilient materials designed to separate maxillary teeth. The function of these splints differs greatly from permissive splints; therefore, they may exacerbate bruxism, possibly by causing premature posterior contacts due to their imbalance. The treatment aims to achieve even and simultaneous contact with the opposing teeth. A patient with acute TMD can be treated with it as an emergency, as it is quick to fabricate (Dawson, 1989).
3.3.3.1. Soft rubber splint
A resilient appliance achieves even and simultaneous contact with opposing teeth to relieve pain, discomfort, myalgia, bruxism, and clenching (Alqutaibi & Aboalrejal, 2015). It can be easily fabricated and used as an emergency treatment for patients with acute TMD (Alqutaibi and Aboalrejal, 2015, Boero, 1989). This splint was more effective than rigid stability splints in treating myogenous TMDs, but less effective in treating arthrogenous TMDs (RAMFJORD & ASH, 1994). (Fig. 6).
Fig. 6.
A. Soft Rubber Splint. B. Frontal view of the Soft Rubber Splint. C. Lateral view of the Soft Rubber Splint.
3.3.3.2. Hydrostatic splint (Equalizer)
It is a prefabricated splint that do not requires a dental impression (Yadav & Karani, 2011). It is a reservoir filled with fluid placed over the teeth to treat TMJ, headache, neck and shoulder pain, and mandibular repositioning (Alqutaibi and Aboalrejal, 2015, Boero, 1989). The splint was made of elastic materials (Kui et al., 2020). The inability of soft rubber splints to balance occlusal contacts renders them inappropriate for effective splint therapy, as they are typically positioned in the maxillary arch (Kui et al., 2020).
3.4. Utilization period:
To our knowledge, there are no fixed rules for how long an occlusal splint should be worn. However, according to Yadav et al. (Yadav & Karani, 2011), the duration of treatment varies according to the type of therapy and rate of recovery to prevent involuntary parafunctional motor activities such as bruxism and clenching. It is recommended that patients wear splints only at night. Those unable to manage their habits when awake may have to keep their splint during the day. Some patients may develop a negative dependence on the occlusal splint due to their parafunctional habits, so they should only wear them for a few months. However, in cases where occlusal splints cause recurrent parafunctional behaviors, the splint must be constantly worn at night. A splint that does not cover all teeth or make balanced contact with the opposing teeth should not be worn for four to six weeks. Wearing them constantly for twenty-four hours a day might cause irreversible changes in occlusion. Individuals with intracapsular pathology who wear anterior bite splints for longer than two weeks have a higher risk of compression. Thus, it is recommended for acute musculoskeletal problems that last for a short time or emergency care.
3.5. Occlusal splint therapy for bruxism patients:
Bruxism is a jaw or muscle response characterized by the clenching or grinding of the teeth (de Baat et al., 2021). TMJ issues can be exacerbated by habits such as tooth grinding (Kitsoulis et al., 2011). Bruxism can result in maxillofacial issues, facial deformation, hearing loss, tooth wear, grinding, crushing, fractures, and severe tooth damage (Kitsoulis et al., 2011). Bruxism must be treated; otherwise, the teeth and bones may become worn or cracked because of excessive wear pressure (Gholampour et al., 2019). A mismatch between the physiological loading input and the stress generated is one of the biomechanical causes of bruxism. An occlusal splint can help establish this equilibrium by aiding the neuromuscular reaction and reducing strains on the TMJ-related ligaments and joints (Gholampour et al., 2019). The forces on both sides of the mandible are not necessarily balanced and consistent in individuals with bruxism (Gholampour et al., 2019). However, the flexibility of the splint material can facilitate both bilateral and simultaneous loading (Gholampour et al., 2019). Using splints may reduce muscle activity and avoid the undesirable effects of bruxism, such as grinding sounds, tooth wear, and pain (Beddis et al., 2018). Occlusal splints should provide balanced occlusal contact over the arch (Beddis et al., 2018). A study was conducted to determine the maximum stress in the jawbone in patients with bruxism, which was found to be approximately-four times higher than normal; however, after using an occlusal splint, the maximum stress was decreased by 71.0 % (Gholampour et al., 2019). Occlusal splints improve mandibular movements, chronic pain, and pain intensity reduction (S. H. Zhang et al., 2020). In a separate trial, people with bruxism who did not wear splints were eight times more likely to break their porcelain laminate veneers than those who wore splints (Granell-Ruíz et al., 2014). Occlusal splints are a non-invasive treatment option for patients with TMD; they effectively treat bruxism by preserving the biomechanical balance between physiological loading and stress generated by stress relaxation (Gholampour et al., 2019).
3.6. Correction of decreased vertical dimension of occlusion (VDO) by occlusal splint:
Parafunctional muscle activity such as clenching or teeth grinding can decrease the vertical dimension of occlusion (VDO), leading to TMDs. As a part of reversible occlusal therapy, the occlusal splint is beneficial in cases of decreased VDO (Guguvcevski et al., 2017) and reduces the majority of the signs and symptoms associated with TMDs (Chandu et al., 2004, Torii, 2011). Reduced VDO can be treated and corrected by increasing the distance between the teeth using occlusal splints (Li et al., 2010). After restoring the VDO with the splint, definitive prosthetic treatment can be provided (Guguvcevski et al., 2017).
3.7. Comparison between occlusal splint therapy and physiotherapy in patients with painful TMDs:
In dental practice, occlusal splint therapy is a frequent treatment for TMDs (Garrigós-Pedrón et al., 2019, Pficer et al., 2017; C. Zhang et al., 2016). Physiotherapy is an additional therapeutic option for joint and muscle pain, as it enhances strength, mobility, and coordination while reducing joint and muscle discomfort (Rashid et al., 2013). The efficacy of exercise therapy for the treatment of TMD has been examined in previous studies (Armijo-Olivo et al., 2016, Eliassen et al., 2019, la Touche et al., 2022). Some authors have suggested that therapeutic activities performed under the supervision of a physiotherapist may have an additional effect on patient well-being, which may be related to the superiority of physiotherapy over occlusal splint therapy (L. Zhang et al., 2021). Several studies have demonstrated the efficacy of therapeutic exercise techniques in treating TMD owing to improvements in local analgesia, muscular function, and blood flow (Dostalová et al., 2012, Rashid et al., 2013). Few studies have demonstrated the efficacy of exercise therapy with occlusal splint therapy for treating chronic TMDs (Armijo-Olivo et al., 2016, Eliassen et al., 2019). Olivier et al. (Armijo-Olivo et al., 2016) conducted a systematic evaluation and found that exercise did not provide clear superiority over other conservative therapies for TMD. Zhang et al. (L. Zhang et al., 2021) conducted a second study to assess the efficacy of occlusal splint therapy and exercise therapy in alleviating pain and enhancing mandibular movement during the treatment. The outcomes were comparable, and the exercises did not demonstrate a clear advantage over occlusal splints in treating TMDs (L. Zhang et al., 2021). Additionally, Wanman et al. (Wänman & Marklund, 2020) researched three groups of patients with symptomatic disc displacement and reduction. This study examined the efficacy of occlusal splint therapy with jaw exercise programs and found that both treatments had similar favorable effects on the perceived intensity of TMJ clicking sounds (Wänman & Marklund, 2020).
3.8. The effects of occlusal splint therapy for individuals with migraine or tension-type headache with TMD:
Individuals with TMDs are susceptible to migraines and tension-type headaches (Saha et al., 2019). Several studies have been conducted to understand the relationship between headaches and TMDs to conclude that temporomandibular disorders are the second most common cause of musculoskeletal discomfort and that tension-type headaches are strongly associated with TMDs (Kostrzewa-Janicka et al., 2013, Manrriquez et al., 2021). In addition to the increasing prevalence of chronic headaches, TMDs can exacerbate primary headaches (Saha et al., 2019). Positive connections were found between headaches and TMDs, and a significant association between cause and effect (Cooper & Kleinberg, 2009). In a study conducted on patients with migraine and tension-type headaches, TMDs were treated with occlusal splint therapy. They showed a considerable reduction in the severity of headaches and an improvement in the physical quality of life (Saha et al., 2019). Another study examined the prevalence of TMDs and the frequency of headaches (Cooper & Kleinberg, 2009). Researchers have discovered that treating TMDs significantly reduces or eliminates tension-type headaches in a large proportion of individuals (Cooper & Kleinberg, 2009). In addition, a study examining the association between TMD treatment and their influence on headache treatment found that the treatment of TMDs greatly reduced headache frequency and intensity (Costa et al., 2015). Several studies and strong evidence suggest that occlusal splint therapy for TMDs may help to treat and reduce migraine and tension-type headaches (Cooper and Kleinberg, 2009, Costa et al., 2015, D’Ermes et al., 2012, Kostrzewa-Janicka et al., 2013, Manrriquez et al., 2021, Quayle et al., 1990, Saha et al., 2019).
3.9. The influence of the occlusal splint and therapy exercises on the postural stability of individuals with symptoms of TMDs:
The posture is defined as the position of the human body in space (Oliveira et al., 2019). A balance should be maintained between the masticatory cycles; once there is an imbalance, it could impact the postural equilibrium of the body (Oliveira et al., 2019). Because occlusal splints are used to treat TMD, their effects on postural balance were investigated, and the outcome revealed that occlusal splints had beneficial effects on postural balance and control (Oliveira et al., 2019). A prospective study evaluating the effects of occlusal splints on posture showed that they increased postural control in all motion-related domains (Zoghbi et al., 2021). Researchers have also investigated the effect of TMD treatment on the mobility of the spine, and there was a significant increase in mobility, indicating a good effect on posture control (Walczyńska-Dragon et al., 2014). In another study, occlusal splints were used to evaluate the spinal posture of patients with TMDs (Ferrillo et al., 2022). This study demonstrated that occlusal therapy improves postural balance and control (Ferrillo et al., 2022). According to the results of these trials, occlusal splint therapy for patients with TMDs dramatically improved postural balance and control (Ferrillo et al., 2022, Oliveira et al., 2019, Walczyńska-Dragon et al., 2014, Zoghbi et al., 2021).
3.10. The Short- and Long-Term effects of occlusal splints and other treatment Techniques:
The long-term efficacy of occlusal therapies in treating TMDs is debatable (Pficer et al., 2017), and researchers should consider both the short- and long-term therapeutic effects in their investigations. Numerous practitioners have sought to produce recommendations for diagnosing and treating TMDs to provide direction for proper treatment (Greene, 2010). According to the American Association for Dental Research (AADR), policy the treatment should be evidence-based and offer the greatest possibility for long-term relief (Greene, 2010). Numerous ancient and contemporary clinical trials and systematic reviews have proven the efficacy of occlusal splint therapy in reducing pain intensity and enhancing masticatory performance in patients with painful TMDs (Conti et al., 2012, Ekberg et al., 2003). Multiple therapeutic methods exist to alleviate the symptoms of TMDs in the muscles and joints of the jaw. An occlusal splint, designed to increase occlusal stability (RAMFJORD & ASH, 1994) and reduce muscular tension (Glaros et al., 2007), is one of the most popular treatments. A study compared two groups using occlusal splints and other treatment modalities to determine the short- and long-term efficacy of TMDs (Pficer et al., 2017). The occlusal splint provided patients with TMDs with short-term benefits, but its long-term effect was comparable to other therapeutic modalities (Pficer et al., 2017). Another study was conducted to determine the effectiveness of oral splints in reducing pain intensity in patients with TMDs during both short- and long-term treatment. (Fouda, 2020). In short-term trials, the efficacy of occlusal splint therapy for pain reduction was superior to that of the control group; however, in long-term studies, it becomes inconsequential (Fouda, 2020). In conclusion, studies have demonstrated that therapy using occlusal splints resulted in positive short-term outcomes. In long-term follow-ups, its efficacy was comparable to other treatment methods (Fouda, 2020, Pficer et al., 2017).
4. Conclusion
As discussed in the literature, occlusal splints can treat various TMDs. It can treat bruxism, headaches, postural imbalances related to TMDs, and decreased VDO. However, there is no clear evidence that occlusal splints are superior to physiotherapy in treating TMDs. In the long-term follow-up, they were equally effective as other therapies.
Ethical approval
This article does not include any studies involving human participants or animals performed by the author.
An exemption letter was provided by the Institutional Review Board (IRB) (No. E-22–7136).
Funding
None.
CRediT authorship contribution statement
Hamad Albagieh: Conceptualization, Project administration, Resources, Supervision, Validation. Ibrahim Alomran: Investigation, Writing – original draft, Writing – review & editing, Project administration, Supervision, Resources, Validation, Visualization, Methodology. Abdulrahman Binakresh: Investigation, Resources, Visualization, Writing – original draft, Writing – review & editing. Nawaf Alhatarisha: Resources, Writing – review & editing, Writing – original draft. Meteb Almeteb: Resources, Writing – review & editing, Writing – original draft. Yousef Khalaf: Resources, Writing – review & editing. Abdulrahman Alqublan: Resources, Writing – review & editing. Mohammad Alqahatany: Investigation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
Footnotes
Peer review under responsibility of King Saud University. Production and hosting by Elsevier.
References
- Al-Moraissi E.A., Farea R., Qasem K.A., Al-Wadeai M.S., Al-Sabahi M.E., Al-Iryani G.M. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: network meta-analysis of randomized controlled trials. Int. J. Oral Maxillofac. Surg. 2020;49(8) doi: 10.1016/j.ijom.2020.01.004. [DOI] [PubMed] [Google Scholar]
- Alqutaibi A.Y., Aboalrejal A.N. Types of Occlusal Splint in Management of Temporomandibular Disorders (TMD) Journal of Arthritis. 2015;04(04) doi: 10.4172/2167-7921.1000176. [DOI] [Google Scholar]
- Armijo-Olivo S., Pitance L., Singh V., Neto F., Thie N., Michelotti A. Effectiveness of manual therapy and therapeutic exercise for temporomandibular disorders: Systematic review and meta-analysis. Phys. Ther. 2016;96(1) doi: 10.2522/ptj.20140548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASH, M. M. 1986. Current concepts in the aetiology, diagnosis and treatment of TMJ and muscle dysfunction. Journal of Oral Rehabilitation, 13(1). https://doi.org/10.1111/j.1365-2842.1986.tb01551.x [DOI] [PubMed]
- Attanasio R. Intraoral orthotic therapy. Dent. Clin. N. Am. 1997;41(2) doi: 10.1016/s0011-8532(22)00087-8. [DOI] [PubMed] [Google Scholar]
- Beddis H., Pemberton M., Davies S. Sleep bruxism: An overview for clinicians. Br. Dent. J. 2018;225(6) doi: 10.1038/sj.bdj.2018.757. [DOI] [PubMed] [Google Scholar]
- Boero R. The physiology of splint therapy: a literature review. Angle Orthod. 1989;59(3):165–180. doi: 10.1043/0003-3219(1989)059<0165:TPOSTA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Capp N.J. Occlusion and splint therapy. Br. Dent. J. 1999;186(5) doi: 10.1038/sj.bdj.4800069. [DOI] [PubMed] [Google Scholar]
- Chandu A., Suvinen T.I., Reade P.C., Borromeo G.L. The effect of an interocclusal appliance on bite force and masseter electromyography in asymptomatic subjects and patients with temporomandibular pain and dysfunction. J. Oral Rehabil. 2004;31(6) doi: 10.1111/j.1365-2842.2004.01377.x. [DOI] [PubMed] [Google Scholar]
- Conti P.C.R., de Alencar E.N., da Mota Corrêa A.S., Lauris J.R.P., Porporatti A.L., Costa Y.M. Behavioural changes and occlusal splints are effective in the management of masticatory myofascial pain: A short-term evaluation. J. Oral Rehabil. 2012;39(10) doi: 10.1111/j.1365-2842.2012.02327.x. [DOI] [PubMed] [Google Scholar]
- Cooper B.C., Kleinberg I. Relationship of temporomandibular disorders to muscle tension-type headaches and a neuromuscular orthosis approach to treatment. Cranio - Journal of Craniomandibular and Sleep Practice. 2009;27(2) doi: 10.1179/crn.2009.016. [DOI] [PubMed] [Google Scholar]
- Costa Y., Porporatti A., Stuginski-Barbosa J., Bonjardim L., Speciali J., Conti P. Headache Attributed to Masticatory Myofascial Pain: Clinical Features and Management Outcomes. J. Oral Facial Pain Headache. 2015;29(4) doi: 10.11607/ofph.1394. [DOI] [PubMed] [Google Scholar]
- Crout D.K. Anatomy of an occlusal splint. Gen. Dent. 2017;65(2) [PubMed] [Google Scholar]
- D’Ermes V., Basile M., Rampello A., di Paolo C. Influence of occlusal splint on competitive athletes performances. Ann. Stomatol. 2012;3(3–4) [PMC free article] [PubMed] [Google Scholar]
- Dawson P.E. Evaluation, Diagnosis, and Treatment of Occlusal Problems. J. Oral Rehabil. 1989;2(32) [Google Scholar]
- de Baat C., Verhoeff M., Ahlberg J., Manfredini D., Winocur E., Zweers P., Rozema F., Vissink A., Lobbezoo F. Medications and addictive substances potentially inducing or attenuating sleep bruxism and/or awake bruxism. J. Oral Rehabil. 2021;48(3) doi: 10.1111/joor.13061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dostalová T., Hlinakova P., Kasparova M., Rehacek A., Vavrickova L., Navrátil L. Effectiveness of physiotherapy and GaAlAs laser in the management of temporomandibular joint disorders. Photomed. Laser Surg. 2012;30(5) doi: 10.1089/pho.2011.3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dylina T.J. A common-sense approach to splint therapy. J. Prosthet. Dent. 2001;86(5) doi: 10.1067/mpr.2001.118878. [DOI] [PubMed] [Google Scholar]
- Ekberg E.C., Vallon D., Nilner M. The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial. J. Orofac. Pain. 2003;17(2) [PubMed] [Google Scholar]
- Zoghbi A. el, Halimi M., Hobeiche J., Haddad C. Effect of occlusal splints on posture balance in patients with temporomandibular joint disorder: a prospective study. J. Contemp. Dent. Pract. 2021;22(6) doi: 10.5005/jp-journals-10024-3094. [DOI] [PubMed] [Google Scholar]
- Eliassen M., Hjortsjö C., Olsen-Bergem H., Bjørnland T. Self-exercise programmes and occlusal splints in the treatment of TMD-related myalgia—Evidence-based medicine? In Journal of Oral Rehabilitation. 2019;46(11) doi: 10.1111/joor.12856. [DOI] [PubMed] [Google Scholar]
- Ferrillo M., Marotta N., Giudice A., Calafiore D., Curci C., Fortunato L., Ammendolia A., de Sire A. Effects of Occlusal Splints on Spinal Posture in Patients with Temporomandibular Disorders: A Systematic Review. Healthcare. 2022;10(4) doi: 10.3390/healthcare10040739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fouda, A. A. H. 2020. No evidence on the effectiveness of oral splints for the management of temporomandibular joint dysfunction pain in both short and long-term follow-up systematic reviews and meta-analysis studies. In Journal of the Korean Association of Oral and Maxillofacial Surgeons (Vol. 46, Issue 2). https://doi.org/10.5125/JKAOMS.2020.46.2.87. [DOI] [PMC free article] [PubMed]
- Garrigós-Pedrón M., Elizagaray-García I., Domínguez-Gordillo A.A., Del-Castillo-Pardo-de-Vera J.L., Gil-Martínez A. Temporomandibular disorders: Improving outcomes using a multidisciplinary approach. J. Multidiscip. Healthc. 2019;12 doi: 10.2147/JMDH.S178507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gholampour S., Gholampour H., Khanmohammadi H. Finite element analysis of occlusal splint therapy in patients with bruxism. BMC Oral Health. 2019;19(1) doi: 10.1186/s12903-019-0897-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibreel M., Perea-Lowery L., Vallittu P.K., Lassila L. Characterization of occlusal splint materials: CAD-CAM versus conventional resins. J. Mech. Behav. Biomed. Mater. 2021;124 doi: 10.1016/j.jmbbm.2021.104813. [DOI] [PubMed] [Google Scholar]
- Glaros A.G., Owais Z., Lausten L. Reduction in parafunctional activity: A potential mechanism for the effectiveness of splint therapy. J. Oral Rehabil. 2007;34(2) doi: 10.1111/j.1365-2842.2006.01660.x. [DOI] [PubMed] [Google Scholar]
- Granell-Ruíz M., Agustín-Panadero R., Fons-Font A., Román-Rodríguez J.L., Solá-Ruíz M.F. Influence of bruxism on survival of porcelain laminate veneers. Medicina Oral Patologia Oral y Cirugia Bucal. 2014;19(5) doi: 10.4317/medoral.19097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene, C. S. 2010. Managing the care of patients with temporomandibular disorders: A new guideline for care. In Journal of the American Dental Association Vol. 141, Issue 9. https://doi.org/10.14219/jada.archive.2010.0337. [DOI] [PubMed]
- Guguvcevski L., Gigovski N., Mijoska A., Zlatanovska K., Arsova-Gigovska A. Temporomandibular disorders treatment with correction of decreased occlusal vertical dimension. Open Access Macedonian Journal of Medical Sciences. 2017;5(7) doi: 10.3889/oamjms.2017.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitsoulis P., Marini A., Iliou K., Galani V., Zimpis A., Kanavaros P., Paraskevas G. Signs and symptoms of temporomandibular joint disorders related to the degree of mouth opening and hearing loss. BMC Ear, Nose and Throat Disorders. 2011;11(1) doi: 10.1186/1472-6815-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kostrzewa-Janicka J., Mierzwinska-Nastalska E., Rolski D., Szczyrek P. Occlusal stabilization splint therapy in orofacial pain and tension-type headache. Adv. Exp. Med. Biol. 2013;788 doi: 10.1007/978-94-007-6627-3_27. [DOI] [PubMed] [Google Scholar]
- Kui A., Pop S., Buduru S., Negucioiu M. The use of occlusal splints in temporomandibular disorders - an overview. Acta Stomatologica Marisiensis Journal. 2020;3(2) doi: 10.2478/asmj-2020-0008. [DOI] [Google Scholar]
- Kurita H., Kurashina K., Kotani A. Clinical effect of full coverage occlusal splint therapy for specific temporomandibular disorder conditions and symptoms. J. Prosthet. Dent. 1997;78(5) doi: 10.1016/S0022-3913(97)70067-2. [DOI] [PubMed] [Google Scholar]
- la Touche R., Boo-Mallo T., Zarzosa-Rodríguez J., Paris-Alemany A., Cuenca-Martínez F., Suso-Martí L. Manual therapy and exercise in temporomandibular joint disc displacement without reduction. A systematic review. Cranio - Journal of Craniomandibular and Sleep Practice. 2022;40(5) doi: 10.1080/08869634.2020.1776529. [DOI] [PubMed] [Google Scholar]
- Li Y., Zhang Z.G., Wu S.Y., Qiao Y.G. A novel experimental design model for increasing occlusal vertical dimension. Journal of Craniofacial Surgery. 2010;21(2) doi: 10.1097/SCS.0b013e3181cfe986. [DOI] [PubMed] [Google Scholar]
- Manrriquez S.L., Robles K., Pareek K., Besharati A., Enciso R. Reduction of headache intensity and frequency with maxillary stabilization splint therapy in patients with temporomandibular disorders-headache comorbidity: a systematic review and meta-analysis. Journal of Dental Anesthesia and Pain Medicine. 2021;21(3) doi: 10.17245/jdapm.2021.21.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson S.J. Principles of stabilization bite splint therapy. Dental Clinics of North America. 1995;39(2) doi: 10.1016/s0011-8532(22)01786-4. [DOI] [PubMed] [Google Scholar]
- Oliveira S.S.I., Pannuti C.M., Paranhos K.S., Tanganeli J.P.C., Laganá D.C., Sesma N., Duarte M., Frigerio M.L.M.A., Cho S.C. Effect of occlusal splint and therapeutic exercises on postural balance of patients with signs and symptoms of temporomandibular disorder. Clinical and Experimental Dental Research. 2019;5(2) doi: 10.1002/cre2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pficer J.K., Dodic S., Lazic V., Trajkovic G., Milic N., Milicic B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short and long term effects. PLoS One. 2017;12(2) doi: 10.1371/journal.pone.0171296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quayle A.A., Gray R.J.M., Metcalfe R.J., Guthriet E., Wastell D. Soft occlusal splint therapy in the treatment of migraine and other headaches. J. Dent. 1990;18(3) doi: 10.1016/0300-5712(90)90048-J. [DOI] [PubMed] [Google Scholar]
- Ramfjord S.P., Ash M.M. Reflections on the Michigan occlusal splint. J. Oral Rehabil. 1994;21(5) doi: 10.1111/j.1365-2842.1994.tb01164.x. [DOI] [PubMed] [Google Scholar]
- Rashid A., Matthews N.S., Cowgill H. Physiotherapy in the management of disorders of the temporomandibular joint - Perceived effectiveness and access to services: A national United Kingdom survey. Br. J. Oral Maxillofac. Surg. 2013;51(1) doi: 10.1016/j.bjoms.2012.03.009. [DOI] [PubMed] [Google Scholar]
- Ré, J.-P., Perez, C., Darmouni, L., Carlier, J., & J.D, O. 2009. The occlusal splint therapy. International Journal of Stomatology & Occlusion Medicine, 2, 82–86. https://doi.org/10.1007/s12548-009-0015-y.
- Saha F.J., Pulla A., Ostermann T., Miller T., Dobos G., Cramer H. Effects of occlusal splint therapy in patients with migraine or tension-type headache and comorbid temporomandibular disorder: A randomized controlled trial. Medicine (United States) 2019;98(33) doi: 10.1097/MD.0000000000016805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg W.K., Clark G.T., Rugh J.D. Nocturnal electromyographic evaluation of bruxism patients undergoing short term splint therapy. J. Oral Rehabil. 1975;2(3) doi: 10.1111/j.1365-2842.1975.tb00915.x. [DOI] [PubMed] [Google Scholar]
- Torii K. A Case Report of the Symptom-Relieving Action of an Anterior Flat Plane Bite Plate for Temporomandibular Disorder. Open Dent. J. 2011;4(1) doi: 10.2174/1874210601004010218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walczyńska-Dragon K., Baron S., Nitecka-Buchta A., Tkacz E. Correlation between TMD and cervical spine pain and mobility: Is the whole body balance TMJ related? Biomed Res. Int. 2014;2014 doi: 10.1155/2014/582414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wänman A., Marklund S. Treatment outcome of supervised exercise, home exercise and bite splint therapy, respectively, in patients with symptomatic disc displacement with reduction: A randomised clinical trial. J. Oral Rehabil. 2020;47(2) doi: 10.1111/joor.12888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav S., Karani J.T. The Essentials of Occlusal Splint Therapy. International Journal Od Prosthetic Dentistry. 2011;2(1) [Google Scholar]
- Zhang S.H., He K.X., Lin C.J., Liu X.D., Wu L., Chen J., Rausch-Fan X. Efficacy of occlusal splints in the treatment of temporomandibular disorders: a systematic review of randomized controlled trials. Acta Odontol. Scand. 2020;78(8) doi: 10.1080/00016357.2020.1759818. [DOI] [PubMed] [Google Scholar]
- Zhang C., Wu J.Y., Deng D.L., He B.Y., Tao Y., Niu Y.M., Deng M.H. Efficacy of splint therapy for the management of temporomandibular disorders: A meta-analysis. Oncotarget. 2016;7(51) doi: 10.18632/oncotarget.13059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L., Xu L., Wu D., Yu C., Fan S., Cai B. Effectiveness of exercise therapy versus occlusal splint therapy for the treatment of painful temporomandibular disorders: A systematic review and meta-analysis. Annals of Palliative Medicine. 2021;10(6) doi: 10.21037/apm-21-451. [DOI] [PubMed] [Google Scholar]