Abstract
Background:
Following acute brain injury (ABI), patients in the intensive care unit (ICU) often undergo hourly or every-other-hour exams (“neurochecks”) to monitor for neurodeterioration. We assessed healthcare provider attitudes towards neurocheck frequency and evaluated providers’ ideal neurocheck frequency.
Methods:
This was a cross-sectional, online survey distributed in Spring 2021 at a tertiary care academic medical center. Providers from multiple ICU and neuroscience clinical specialties including attending faculty, medical trainees, advanced practice providers and bedside nurses were invited to participate.
Results:
Among 177 participants, 61 (34%) and 116 (66%) self-identified as ordering and performing providers, respectively. The survey response rate was 58% among physicians and 51% among bedside nurses with neurological expertise. The most common medical and non-medical reasons for ordering hourly neurochecks were “a specific diagnosis with anticipated course” and “standard of care”, respectively. Compared to ordering providers, performing providers felt guidelines regarding neurocheck frequency (p<0.01) and duration (p<0.01) should be proscriptive. Conversely, ordering providers felt hourly neurochecks were detrimental to patients with acute brain injury (p=0.02) and believed they would not utilize hourly neurochecks if there was another mode of monitoring available (p=0.03). Performing providers identified multiple patient-related factors impacting the difficulty of and their willingness to perform frequent neurochecks, and only 70% of neurochecks were perceived to be performed as ordered. Both ordering and performing providers preferred every-other-hour neurochecks following ABI.
Conclusions:
This survey revealed clinically relevant differences in ordering versus performing provider attitudes about frequent neurochecks. Providers preferred every-other-hour rather than hourly neurochecks.
Keywords: ICU, neurocheck, neurological exam, neuromonitoring, critical care
INTRODUCTION
Following acute brain injury (ABI), patients often undergo monitoring in the intensive care unit (ICU), because there is potential for secondary injury and further decline.1 Such neurological decline often manifests as a change in the neurologic exam; thus, frequent neurological assessments (“neurochecks” or “neuroassessments”) are used to monitor for changes that require urgent medical or surgical interventions.
Given the lack of reliable and readily available modes of non-invasive continuous monitoring in the setting of ABI, guidelines and consensus statements for a variety of neurologic diagnoses recommend “frequent neuroassessments”.2–4 However, these guidelines and consensus statements stop short of specifying a frequency, duration, or content of the assessments. Hence, in many US institutions, neurocheck frequency has defaulted to being performed every hour (Q1) or every-other-hour (Q2) (personal communication5).
In our clinical experience, frequent neurochecks are often ordered via protocol (e.g., as part of an order set) with minimal consideration regarding the personalized indication, optimal frequency and duration. As a consequence, frequent neurochecks can persist for excessive lengths of time,6 which can place patients at risk for sleep fragmentation and delirium. Alternatively, infrequent neurochecks may permit major clinical deterioration prior to bedside detection. As part of an effort to better guide future evidence-based practice, we conducted a needs assessment to identify barriers to the execution of clinical trials randomizing patients to different frequencies of neurochecks. Such information regarding barriers to implementation will also be critical to influence change regardless of the results of a randomized study.
At our tertiary care academic medical center, patients with acute brain injury are maintained on hourly neurochecks per protocol—at least in the short-term—and we sought to describe and investigate the attitudes towards these hourly neurochecks of both the healthcare personnel primarily ordering them and those who are primarily performing them. Given the conceptual framework above, we aimed to test the hypotheses that ordering providers (e.g. physicians) and performing providers (e.g. bedside ICU nurses) differ in their opinions regarding the optimal frequency of neurochecks following acute brain injury, as well as differ in their underlying attitudes towards neurochecks; further, we sought to understand challenges to effective neurocheck completion.
METHODS
Standard Protocol Approvals, Registration, and Patient Consents
This project was reviewed and approved by the Institutional Review Board (IRB) at UC San Diego (#201038). Informed consent was obtained from all participants, though a waiver of documented consent was granted by the IRB.
Study Design and Administration
This cross-sectional survey-based evaluation was performed at a tertiary care academic medical center. Providers from multiple ICU and neuroscience clinical specialties including attending faculty, trainees, advanced practice providers (APPs) and bedside nurses (RN) were invited to complete a survey about frequent neurochecks consisting of multiple choice, Likert scale, and write-in questions (see supplementary material, Appendix 1). Survey questions were initially developed using a working group model, and then reviewed for content and question type (e.g. Likert vs sliding scale) by a researcher with expertise in both neuroethics and survey-based research (JE). Answer choices were randomized when the order of the answer choices was not important. Surveys were maintained through the SurveyMonkey® web-based platform, and used branching logic to provide the next relevant question based on the answer to the previous question.
Bedside nurse recruitment was performed using group emails from nursing managers and ICU medical directors, as well as flyers posted in high visibility areas (e.g. break rooms, staff bathrooms) in the units of interest. Emails to nursing included 127 specialty trained bedside neuro-nurses. Physician and APP recruitment was performed using direct emails with links to the survey, with a focus on providers in the fields of neurocritical care, anesthesia critical care medicine, pulmonary critical care medicine, trauma and acute surgical critical care, and clinical inpatient neurosciences including neurology and neurosurgery. In total, 112 physicians and APPs were sent direct emails. Surveys could be completed using a desktop computer or a smartphone. Participant informed consent was obtained. The survey was open for completion for 6 weeks in late March to early May 2021. Participants were only allowed to complete the survey once. A raffle incentive was offered for clicking on the link to view the study, at which point the participants could complete the survey and submit their contact details for the raffle or decline the survey and still submit their name and contact for the raffle.
Survey Analysis
Survey responses were evaluated together, and also stratified by ordering versus performing provider, specialty (e.g., neurological versus non-neurological), and years of experience.
Descriptive statistics were used to summarize survey data. We used Chi-squared tests to compare categorical responses by strata (e.g., ordering versus performing providers). We used ANOVA for analyses involving categorical variables with three or more groups, and any significant variance was further investigated using Bonferroni post-hoc comparisons test. Analyses were performed using STATA 16.1 (College Station, TX) and p<0.05 denoted statistical significance.
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator.
RESULTS
Respondents
181 participants completed the survey; 177 of these fully identified their healthcare role and were included in analysis (Table 1). The response rate for physicians and advanced practice practitioners was 58%, and the response rate was 51% for bedside nurses with known neurological expertise staffing the neurocritical care and trauma ICUs. However, the overall response rate could not be calculated given the various modes of distribution and fluctuating staffing among ICUs including traveling nurses. Physicians and APPs predominantly self-identified as ‘ordering providers’ (n=61), while all bedside nurses self-identified as ‘performing providers’ (n=112) (Table 1).
Table 1.
Respondent Characteristics (N = 177)a
| Healthcare Role |
||
|---|---|---|
| Physician/Advanced Practice | Nurse | |
|
|
||
| n = 65 | n = 112 | |
| Hourly Neurocheck Role b | ||
| Ordering Provider | 61 (94%) | 0 (0%) |
| Performing Provider | 4 (6%) | 112 (100%) |
| Stage of Career c | ||
| Early | 10 (30%) | 14 (12%) |
| Middle | 11 (33%) | 31 (28%) |
| Late | 12 (36%) | 66 (59%) |
| ICU Specialty | ||
| Neurological d | 20 (31%) | 65 (59%) |
| Non-Neurological | 45 (69%) | 46 (41%) |
| Predominant Shift (RNs Only) | ||
| Day | 69 (62.2%) | |
| Night | 32 (28.8%) | |
| Mixed | 10 (9.0%) | |
| Exams Observed, median (p25, p75, range) e | 20 (5, 20, 0–20) | |
| Exams Performed, median (p25, p75, range) f | 125 (75, 200, 1–200) | |
| Ideal Neurocheck Frequency, median (mode) | q2 hours (q2 hours) | q2 hours (q2 hours) |
Abbreviations: APP: Advanced Practice Provider; ICU: Intensive Care Unit; IMU: Intermediate Care Unit; MD/DO: Physician; Q2: Every 2 hours; RN: bedside nurse
All values N (%) unless otherwise stated; excludes 4 respondents who were “unknown”.
Self-identified role.
For physicians and APP, only prompted to enter stage of career if training was completed (e.g. attending physician), N=33. For bedside nurse, N=111. Early = Fewer than 5 years out of training; Middle = 5–10 years out from training; Late = More than 10 years out from training.
Among physicians/APPs includes neurology, neurocritical care, and neurosurgery; among nurses, includes neurological ICU, neurosurgery, stroke and general non-ICU neurology.
N = 55; observed number capped at 20; outliers omitted
N = 107; performed number capped at 200; outliers omitted
Neurocheck Attitudes and Perceptions
Both performing and ordering providers’ ideal neurocheck frequency for patients with ABI was every-other-hour (Q2) without a significant difference in the median or distribution of responses (Table 1). Only 17% of ordering providers and 21% of performing providers disagreed with the statement, “If I had ABI, I would want Q1 neuroassessments performed on me for fewer than 24 hours”.
As compared to ordering providers, performing providers felt stronger that guidelines should specify a frequency as well as duration of “frequent neuroassessments” (p<0.01 for both frequency and duration analyses; Table 2). Alternatively, ordering providers felt more strongly that hourly neurochecks are detrimental to patients with ABI (p=0.02), and that if there was another way to monitor neurological status continuously, they would not utilize hourly neurochecks (p=0.03; Table 2). When comparing neuro- versus non-neuro-trained providers, the latter felt more strongly that the duration for frequent neurochecks be specified (p=0.01), and also that neurochecks are necessary (p=0.03). One-way ANOVA suggested that mid-career physicians and APPs felt more strongly than their early- or late-career colleagues that the duration of frequent neurochecks should be specified in guidelines (p=0.03), though post-hoc tests did not reveal which group differed (p=0.06). Otherwise, stage of career did not impact MD/APP or RN survey responses.
Table 2:
Ordering versus Performing Provider Attitudes Toward Hourly Neurochecks a
| Question | Ordering Provider | Performing Provider | P value |
|---|---|---|---|
| Guidelines outlining care for acutely brain injured patients recommend “frequent neuroassessments”. I interpret this to mean Q1 neuroassessments. | 4 (3, 4) | 3 (2, 4) | 0.09 |
| It is important for Guideline recommendations to: | |||
| Specify a frequency for neuroassessments following ABI. | 4 (3, 4.5) | 4 (4, 5) | <0.001 |
| Suggest a duration for frequent neuroassessments following ABI. | 4 (3, 5) | 4 (4, 5) | 0.008 |
| Hourly neuroassessments are: | |||
| Valuable in the care of patients with ABI. | 4 (3, 4) | 4 (3, 4) | 0.91 |
| Necessary in the care of patients with ABI. | 3 (3, 4) | 4 (3, 4) | 0.31 |
| Detrimental to patients with ABI. | 4 (3, 4.5) | 4 (3, 4) | 0.02 |
| There should be a maximum amount of time that someone is continuously monitored with Q1 neuroassessments. | 4 (3, 5) | 4 (3, 5) | 0.11 |
| I am comfortable spacing neuroassessments less frequently than hourly following ABI. | 4 (3, 4) | 4 (3, 4) | 0.41 |
| If I had another way to monitor my patients’ neurological status continuously following ABI, I would not order Q1 neuroassessments. | 4 (3.5, 5) | 4 (3, 4) | 0.03 |
| If I had ABI, I would want Q1 neuroassessments performed on me for fewer than 24 hours. | 3 (3, 4) | 4 (3, 5) | 0.48 |
Abbreviations: ABI: acute brain injury; Q1: hourly
Median (25%ile and 75%ile) Likert Score 1 to 5 are reported; 1=Strongly Disagree, 5=Strongly Agree. N = 52 ordering providers, = 94 performing providers.
The most common reasons cited for ordering hourly neurochecks were unstable clinical status with (n=46, 84%) or without (n=47, 86%) associated radiographic changes, “standard of care” (n=47, 86%), a specific diagnosis with an expected course (n=43, 78%), unstable radiography without exam change (n=36, 65%), instructed to do so by someone else (n=29, 53%), and an “abundance of caution” (n=23, 42%). When asked to choose their most important medical and non-medical reasons for hourly neurochecks, 29 (53%) and 42 (76%) of ordering providers chose “specific diagnosis with anticipated course” and “standard of care”, respectively.
Nearly 100 performing providers responded to the question concerning characteristics impacting the difficulty and their willingness to complete hourly neurochecks. Neuroassessments were felt to be much more difficult when working with patients who were aggressive (78%), spoke a different primary language (75%), were non-compliant or annoyed (61%), were delirious (57%) or aphasic (41%; Figure 1). Regarding willingness, respondents were less (versus more) willing to perform hourly neurochecks in patients displaying aggression (83%), sleeping/resting (82%), expressing annoyance (77%), delirious (59%), speaking a different language (55%), or who were aphasic (37%) (Figure 2). A median of 70% (IQR 50, 85) of neuroassessments were completed as ordered. Providers reported increased willingness to perform hourly neurochecks when the patients were familiar to them.
Figure 1:

Self-reported difficulty in performing hourly neurochecks (n = 97). Responses ranged from 1 (makes it much easier) to 5 (makes it much harder) in response to the prompt: “Indicate the degree to which the following patient-related factors impact the difficulty of obtaining relevant clinical information during hourly (Q1) neuroassessments.”
Figure 2:
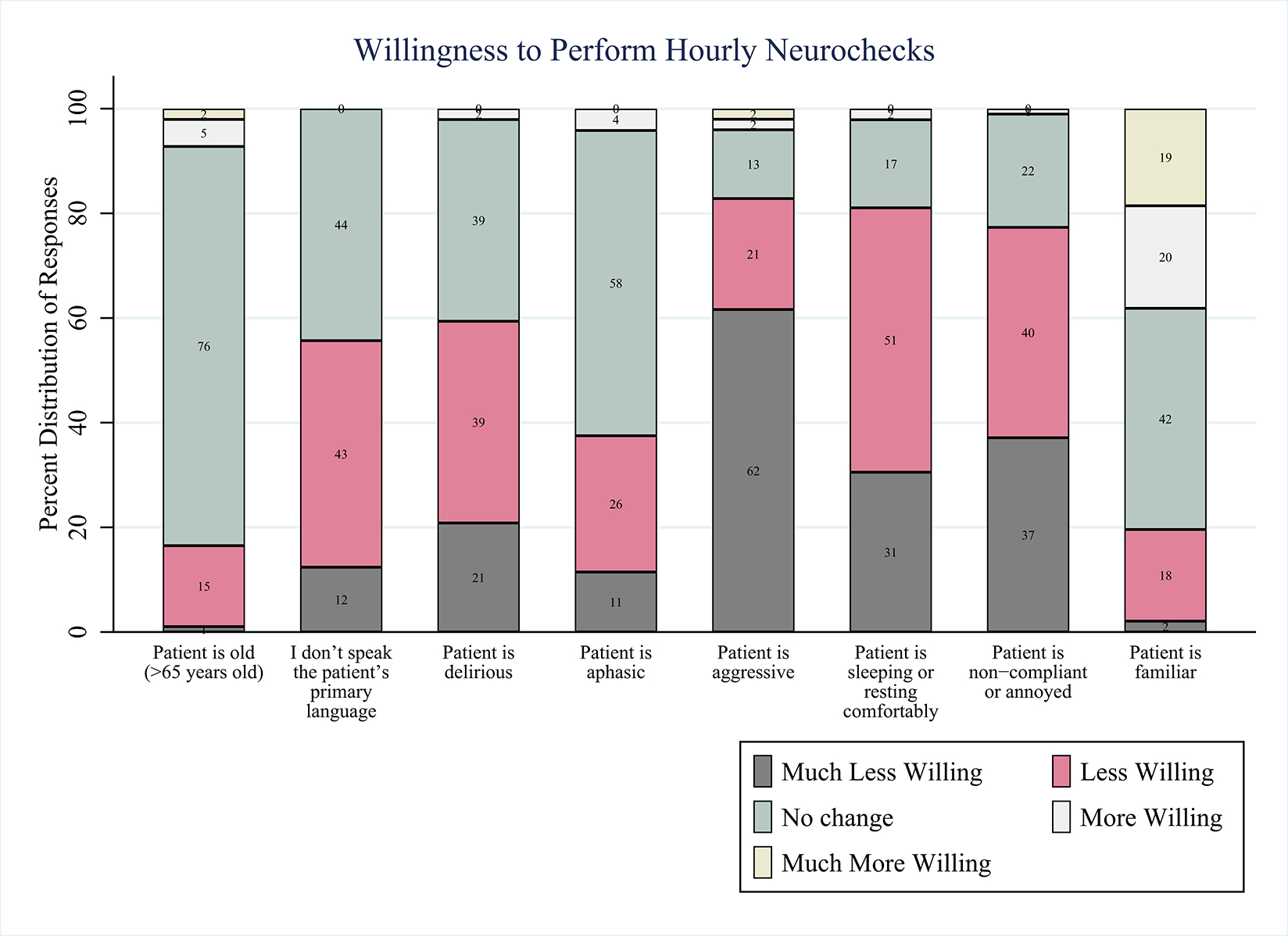
Self-reported willingness in performing hourly neurochecks, n=95–99 depending on the characteristic queried. Responses ranged from 1 (much less willing) to 5 (much more willing) in response to the prompt: “Indicate the degree to which the following patient-related factors impact your willingness to perform hourly (Q1) neuroassessments.”
Ordering providers reported increased willingness to discontinue hourly neurochecks in delirious (n=30, 55%), non-compliant (n=27, 49%) and/or elderly (>90 years; n=24, 44%) patients. They were much more likely to discontinue hourly neurochecks in those individuals whose care plan transitioned to a focus on comfort (n=44, 80%). Conversely, the presence of aphasia made 36% (n=20) of ordering respondents less likely to discontinue hourly neurochecks.
DISCUSSION
To our knowledge, this is the first study to evaluate attitudes regarding hourly neurochecks involving both ordering and performing providers. We found that most healthcare providers prefer every-other-hour assessments following ABI. Furthermore, there are multiple perceived barriers to the completion of frequent neurochecks, for example, differences in primary spoken language, patient aggression, and delirium. Of note, 30% of hourly neurochecks were perceived as not being completed as ordered, which may reflect patient-specific characteristics, provider limitations, or administration/management issues.
This survey revealed a number of apparent gaps. First, there is a gap between providers’ beliefs that patients with ABI should receive hourly neurochecks and whether they would want Q1 exams for themselves. This observation suggests that Q1 exams may often be ordered out of an abundance of caution or due to believed “standard of care” practices rather than what providers deemed clinically necessary. Also supporting this “abundance of caution” theory is the high percentage of orders placed for that given reason, as well as the large number (42%) of ordering providers who would defer hourly neurochecks if there was another way to monitor their patients’ neurological status. Prior literature also notes that 40% of providers feel hourly exams are too frequent.7
Another gap exists between the need for monitoring and the perceived harm. Ordering providers were more willing to discontinue these hourly neurochecks in patients with delirium and felt strongly these assessments may be detrimental to patients. Ordering providers were also more likely to discontinue neurochecks in elderly patients, perhaps related to perceived increased delirium risk in this population.8, 9
Our data also suggest an opportunity for improved communication between care providers ordering versus performing the neurological exams. Given how individuals self-identified their roles, this finding more readily reflects an opportunity for improved communication between doctors/APPs and nurses. There are multiple factors that affect a provider’s difficulty or willingness in performing neurochecks, especially language barriers and patient compliance. Understanding the need for neurochecks may help improve providers’ willingness to perform them and explaining these assessments to patients may also improve their compliance.
Lastly, there is a significant gap between providers with and without neuro-specialization. At our institution, patients with ABI who are cared for in a non-neurological ICU rely on recommendations from specialty trained neuro-provider consultants. The desire for a specified duration of hourly neurochecks and feeling that these exams are necessary may reflect an institutional paradigm whereby these frequent exams are universally recommended by neurospecialists following acute brain injury, with the tradeoff that they may also persist unnoticed prior to being discontinued.6
As with any survey-based study, there was potential for selection, response, and participation biases. We attempted to reduce these factors by providing multiple modes for participation amongst the various ICUs and advertised the survey in a non-leading way. Ultimately, we had a good response rate amongst clinicians and although a total response rate could not be calculated the data reflected a seemingly representative sample of nurses that mirror the frequency with which they care for these patients (e.g., neuro-nurses made up a larger portion of the sample than nurses in the medical ICU or cardiovascular ICU). More day nurses completed the survey than night nurses, however, this discrepancy may reflect the fact that night staffing is in many cases covered by travelling nurses. In order to mitigate response bias, the survey was constructed to avoid leading language. Honest self-reporting was encouraged by offering a completely anonymized interface. However, it is possible that the results reported here reflect a systematic response bias rather than the hypothesized effect, especially with questions inquiring about individual work ethic.
There was general agreement (i.e., lack of statistical difference) between ordering and performing providers that guideline-based recommendations regarding frequent neurochecks be clarified and refined, though the changes sought by ordering versus performing providers differed. Further investigations must evaluate the short- and long-term impact of hourly neurochecks, with an emphasis on fine-tuning guidelines to weigh temporal profiles and risk factors for neurodeterioration for specific disease,1, 10, 11 as well as outlining criteria for neurocheck weaning and/or discontinuation. Prior studies have revealed that approximately one-quarter of hourly neurocheck orders are changed to no neurochecks, suggesting that they are not required for the whole time they are ordered.6 We must be thoughtful and mindful about our patients and balance the risk for neurodeterioration with the potential negative consequences of around-the-clock exams. Frequent arousals for neurochecks (and other care interventions) may have unintended consequences such as delirium that can potentially hinder recovery via sleep fragmentation.12, 13 Further, delirium in the neurointensive care unit leads to higher morbidity and mortality, prolonged ICU and hospital stay, and increased health care costs.14
Future studies can utilize the findings here to justify rigorous study of neurocheck frequency insofar as a large portion of providers believe every-other-hour neurochecks to be ideal following acute brain injury. One might hypothesize that a reduction in the frequency or duration of hourly neurochecks may have a positive impact on outcomes—or at least no change on balance—and further study is needed. Additionally, we require a better understanding of the impact of these frequent assessments on the healthcare system, which may help providers determine when and for how long hourly neurochecks should be utilized.
Supplementary Material
Funding:
Dr. Kamdar is supported by a Paul B. Beeson Career Development Award through the National Institutes of Health/National Institute on Aging (K76 AG059936).
Footnotes
Disclosure(s): Drs. Malhotra, Owens, and Kamdar are funded by the NIH. Dr. Malhotra reports income from Equillium, Corvus, Jazz and Livanova related to medical education. ResMed Medication Company provided a philanthropic donation to UC San Diego. Dr. Owens reports consulting income from Gwell Health and Nitto Denko Asia, and receives research support from Masimo and Samsung, all outside the current work. Drs. LaBuzetta, Kazer, Stone and Evans report no disclosures.
Credits: JNL and BBK had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. JNL, RLO, AM, JHE and BBK contributed to the study design, data interpretation, and the writing of the manuscript. MK and LS contributed to data collection and writing of the manuscript.
REFERENCES
- 1.Lord AS, Gilmore E, Choi HA, et al. Time course and predictors of neurological deterioration after intracerebral hemorrhage. Stroke 2015;46:647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Diringer MN, Bleck TP, Claude Hemphill J 3rd, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit Care 2011;15:211–240. [DOI] [PubMed] [Google Scholar]
- 3.Hemphill JC 3rd, Greenberg SM, Anderson CS, et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2015;46:2032–2060. [DOI] [PubMed] [Google Scholar]
- 4.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019;50:e344–e418. [DOI] [PubMed] [Google Scholar]
- 5.LaBuzetta JN. Personal communication: Variability in Q1 versus Q2 Practices Following Acute Brain Injury Among 18 Neurocritical Care Units Across the USA Among 18 academic neurocritical care ICUs across the Unites States (UCLA Medical Center, Massachusetts General Hospital, Brigham and Womens Hospital, Beth Israel Deaconess Medical Center, University of Pittsburgh, Yale New Haven, Duke University, University of Miami, Shock Trauma, University of Michigan, Brown University, New York University, Chriastiana Care, Rush University, Chicago Catholic, UT Austin, University of Washington, University of Colorado Denver; ), 7 performed Q1 neurochecks for 24 hours regardless of stability. 2 performed Q2 upon admission to the ICU. All others performed Q1 until radiographic stability was determined, then transitioned to Q2. edMay 2021. [Google Scholar]
- 6.LaBuzetta JN, Hirshman BR, Malhotra A, et al. Practices and Patterns of Hourly Neurochecks: Analysis of 8,936 Patients With Neurological Injury. J Intensive Care Med 2021:8850666211029220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goswami S, Husmann K, Braksick S. Neurocheck frequency and the contribution to delirium in neurological intensive care units. Society for Critical Care Medicine; 2020. [Google Scholar]
- 8.Eckstein C, Burkhardt H. Multicomponent, nonpharmacological delirium interventions for older inpatients : A scoping review. Z Gerontol Geriatr 2019;52:229–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hou Y, Dan X, Babbar M, et al. Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol 2019;15:565–581. [DOI] [PubMed] [Google Scholar]
- 10.Maas MB, Berman MD, Guth JC, et al. Neurochecks as a Biomarker of the Temporal Profile and Clinical Impact of Neurologic Changes after Intracerebral Hemorrhage. J Stroke Cerebrovasc Dis 2015;24:2026–2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maas MB, Rosenberg NF, Kosteva AR, et al. Surveillance neuroimaging and neurologic examinations affect care for intracerebral hemorrhage. Neurology 2013;81:107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McLaughlin DC, Hartjes TM, Freeman WD. Sleep Deprivation in Neurointensive Care Unit Patients From Serial Neurological Checks: How Much Is Too Much? J Neurosci Nurs 2018;50:205–210. [DOI] [PubMed] [Google Scholar]
- 13.Shehabi Y, Riker RR, Bokesch PM, et al. Delirium duration and mortality in lightly sedated, mechanically ventilated intensive care patients. Crit Care Med 2010;38:2311–2318. [DOI] [PubMed] [Google Scholar]
- 14.Haymore JB, Patel N. Delirium in the Neuro Intensive Care Unit. Crit Care Nurs Clin North Am 2016;28:21–35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator.


