Summary
Background
This study projects the trend of disease burden and economic burden of diabetes in 33 Chinese provinces and nationally during 2020–2030 and investigates its spatial disparities.
Methods
Time series prediction on the prevalence and disability-adjusted life-year (DALY) rates of diabetes was conducted using a Bayesian modelling approach in 2020–2030. The top-down method and the human capital method were used to predict the direct and indirect costs of diabetes for each Chinese province. Global and local spatial autocorrelation analyses were used to identify geographic clusters of low-or high-burden areas.
Findings
Diabetes prevalence in Chinese adults aged 20–79 years was projected to increase from 8.2% to 9.7% during 2020–2030. During the same period, the total costs of diabetes would increase from $250.2 billion to $460.4 billion, corresponding to an annual growth rate of 6.32%. The total costs of diabetes as a percentage of GDP would increase from 1.58% to 1.69% in China during 2020–2030, suggesting a faster growth in the economic burden of diabetes than China's economic growth. Consistently, the per-capita economic burden of diabetes would increase from $231 to $414 in China during 2020–2030, with an annual growth rate of 6.02%. High disease and economic burden areas were aggregated in Northeast and/or North China.
Interpretation
Our study projects a significant growth of disease and economic burden of diabetes in China during 2020–2030, with strong spatial aggregation in northern Chinese regions. The increase in the economic burden of diabetes will exceed that of GDP.
Funding
National Natural Science Foundation of China, Outstanding Young Scholars Funding.
Keywords: Diabetes, Disease burden, Economic burden, Spatio-temporal analysis
Abbreviations: DALY, Disability-adjusted life-year; GDP, Gross domestic product; SDI, Sociodemographic index; IMF, International monetary fund; IDF, International diabetes federation; UNDESA, United Nations Department of Economic and Social Affairs; GBD, Global Burden of Disease; WHO, World Health Organization
Research in context.
Evidence before this study
A rapid increase in the disease burden of diabetes has been reported in China in recent decades. Diabetes has placed heavy economic burdens on China's healthcare systems and projecting the trend of disease and economic burden in China is important for its intervention. We searched PubMed and Google Scholar between Jan 1, 2000, and June 30, 2022, using the terms “China” or “Chinese”, “cost(s) of diabetes” or the search term “diabetes” in combination with “economic cost(s)”, “economic burden”, “cost burden”, “cost of illness”, “indirect cost(s)”, “direct cost(s)”, “direct expenditure”, or “health expenditure” in the title. We searched these published articles reporting the economic burden of diabetes in China as a whole and/or predicting the trends until 2025 or 2030. Our search found no research articles projecting the future economic burden of diabetes in Chinese provinces. Further, estimates without thorough consideration of the disparity in Gross Domestic Product (GDP) in provinces would likely contribute to biases in estimating the Chinese economic burden of diabetes.
Added value of this study
We projected the disease burden and economic burden of diabetes in Chinese adults aged 20–79 years and its trends based on a national-level and provincial-level representative data source in China. The total economic costs of diabetes were projected to increase from $250.2 billion to US$460.4 b during 2020–2030, representing an annual growth rate of 6.32%. In line with increased total costs, the per-capita cost of diabetes increased from US$231 in 2020 to US$414 in 2030, representing an annual growth rate of 6.02%. Further, the total economic costs as a percentage of GDP were projected to increase from 1.58% to 1.69% during 2020–2030. The positive growth indicated that the overall growth rate of the total economic burden of diabetes exceeds GDP growth. Spatial autocorrelation analysis showed the regions with high-risk total costs of diabetes as a percentage of GDP are largely aggregated in Northeast and North China.
Implications of all the available evidence
We projected a significant growth of disease and economic burden of diabetes in China during 2020–2030, with strong spatial aggregation in northern Chinese regions. We also project that the increase in economic burden will exceed that of GDP, even without considering the adverse effects of COVID-19 on both the economy and diabetes. Effective and innovative strategies remain a priority for diabetes prevention and control in the country.
Introduction
Diabetes mellitus is a fast-growing ongoing global health emergency in the new millennium.1,2 In China, a combination of population growth,3 urbanisation,4 aging,5 an increase in obesity rate6 and a sedentary lifestyle7 have led to a substantial increase in the diabetes population from 98.4 million to 140.9 million during 2013–2021.8,9 Globally, the age-standardised disability-adjusted life-year (DALY) rates attributable to type 2 diabetes increased from 628.3/100,000 person-years to 801.5/100,000 person-years during 1990–2019.10 In comparison, the corresponding DALY rate increased 71.5% from 414/100,000 person-years in 1990 to 710/100,000 person-years in 2017 in China.11 The upsurge in the diabetes epidemic had led to a substantial economic burden in China.
Only a few studies evaluated the economic burden of diabetes in China. The direct costs of diabetes refer to the economic resources directly consumed for the prevention and medical treatment of diabetes and related complications,12 whereas the indirect economic costs are caused by premature mortality, disability and reduced work efficiency and work time.13 In 2015, Bommer et al., in their global studies of the economic burden of diabetes, estimated the burden in China to be $222.3 billion, accounting for ∼2.0% of the total gross domestic product (GDP) in the country.14 Among these, the indirect costs accounted for 36.3% of the total economic burden of diabetes.14 This study further predicted the economic burden of diabetes in China was projected to reach $ 631.7 billion (∼2.9% of the GDP) by 2030.14 In addition, the International Diabetes Federation (IDF) estimated that the direct costs of diabetes would be $109 and $165 billion in China in 2019 and 2021, respectively,1,9 but did not provide any estimates of indirect costs. Integrating indirect costs in the total estimation of the economic burden of diabetes is essential for developing better societal support for individuals living with diabetes.
Estimation of the economic burden of diabetes relies on accurate data on the disease burden of diabetes, which can largely associate with the economic development in a jurisdiction. A previous study has demonstrated that Chinese provinces with moderate Gross Domestic Product (GDP) per capita tend to have a much higher disease burden of diabetes than counterparts with lower or higher GDP per capita.15 This disparity in GDP leads to geographical differences in the allocation of healthcare resources for diabetes prevention and treatment.16 Large variations in diabetes disease burden and economic development occur across the 33 Chinese provinces and special administration regions (SARs). Estimates without thorough consideration of the geographical differences would likely contribute to biases in estimating the economic burden. Our study aims to forecast the future development of the disease burden and economic burden of diabetes in 33 Chinese provinces and SARs during 2020–2030 and investigate its spatial disparities. The study will provide direct evidence to inform health funding allocation for China's next 5-year plan (2026–2030).
Methods
Data collection
We adopted diabetes data for China from the Global Burden of Disease Study (GBD) 2019 for projection. Age-, sex-, year-specific prevalence, and DALY rates of diabetes during 1990–2019 were extracted, along with population size, for all Chinese provinces. We extracted the prevalence of diagnosed diabetes patients in China and provinces from IDF (2019) and the China Chronic Disease and Risk Factors Surveillance study (2013), respectively.17 According to the World Population Prospects report released by the United Nations Population Department in 2019, China's population data was extracted for 2020–2030, stratified by 5-year age group and sex. The World Health Organization (WHO) reported China's health expenditure as a percentage of GDP during 2000–2018.16 The China Statistical Yearbook reported the rural-urban ratio by the province during 2005–2019 and the GDP by the province during 2000–2019.18 We extracted health expenditure as a percentage of GDP in 33 Chinese provinces and SARs (excluding Taiwan Province of China) during 1990–2019 from the China Health Statistics Yearbook in 2020.19
Spatio-temporal analysis of the disease burden of diabetes during 2020–2030
The temporal trend of the disease burden of diabetes (the prevalence and DALY rates of diabetes) was projected using a Bayesian model20 for prediction for 33 Chinese provinces and SARs during 2020–2030, stratified by a 5-year age group and sex (Detail in Appendix pp2).
In the study, we used spatial autocorrelation to evaluate the spatial distribution of the prevalence and DALY rates of diabetes in China. The analysis was performed in the years 2020, 2025, and 2030. A spatial cluster analysis of the prevalence and DALY rates of diabetes was performed, using spatial autocorrelation. We used the Global Moran's I index to calculate the correlation statistics for all the relevant spatial regions of the data and deduced whether the factors (the prevalence and DALY rates) in the studied region were clustered.21 Anselin Local Moran's I22 and Hot-Cold Spots23 analysis identified the presence of spatial clusters or regions with high or low risk of the analysed variables. A high-risk region surrounded by other high-risk regions may be identified as ‘hot spot’ (detail in Appendix pp2).
Estimating the economic burden
We defined the total economic burden (or total costs) of diabetes as the sum of direct and indirect costs (details in Appendix pp3-pp4 and Fig. S1).
Estimating the direct costs caused by diabetes
We estimated the direct costs for diabetes in the age group 20–79 using a top-down approach for China and its provinces during 2020–2030 (details in Appendix pp3). A critical component of the method is the ratio of diabetes health expenditure for people with diabetes (diagnosed or undiagnosed) compared to those without diabetes. These ratios have been significantly refined by the work of Bommer et al.,24 providing estimates for the ratio about whether diabetes is diagnosed or not, with much more specificity with age, sex, and rural versus urban areas (Table S1).
Where = the group-specific total direct costs for diabetes, = the population in each group, = group-specific per capita health expenditure, = prevalence of diagnosed diabetes, = prevalence of undiagnosed diabetes, = age-specific, sex-specific, and location-specific cost ratios for people with diagnosed diabetes, = age-specific, sex-specific, and location-specific cost ratios for people with undiagnosed diabetes.
Estimating the indirect costs caused by diabetes
Diabetes can lead to absenteeism, job loss, or reduced productivity while at work. The indirect costs were measured by calculating the value of a year of lost productive labour. Our study used the human capital approach to estimate the indirect costs for diabetes in the age group 20–79 (details in Appendix pp4). The human capital approach was based on the per capita GDP to calculate the economic losses caused by the loss of adjusted life years (DALYs) of diseases. Because of the different productivity levels of each age group, each age group was given certain weights for productivity. Specific calculation method of the indirect economic burden of disease25:
Different age groups have different productivity weights. For example, the international standards defined the productivity weights of people aged 20–44, 45–59, and 60 and above to be 0.75, 0.80, and 0.1, respectively.26
The direct and indirect economic burden (as baseline) for 33 Chinese provinces and SARs were calculated based on actual diabetes prevalence and DALY data in 2019. The direct and indirect economic burdens during 2020–2030 were calculated based on the projected diabetes prevalence and DALY burden during the same period.
Spatio-temporal analysis of the economic burden of diabetes during 2020–2030
We used the estimated annual percentage change (EAPC) to quantify temporal trends of diabetes economic burden using the natural logarithm model in the Chinese provinces from 2020 to 2030 (detail in Appendix pp 4).27,28
We used the same methods for the analysis of disease burden to analyse the spatial distribution of the economic burden-related indicators (per capita economic burden of diabetes and total costs as a percentage of GDP) (detail in Appendix pp4).
Statistical analyses
Statistical analyses were performed using the R (v3.5.1, https://www.r-project.org/). A probability value of P < 0.05 was considered statistically significant. The Global Moran's I, Anselin Local Moran's I, and Hot-Cold Spots were implemented in ArcGIS (v10.2, ESRI, Redlands, CA, USA).
Role of funding source
The funders of the study had no role in the design or conduct of the study, including data collection, management, analysis, or interpretation of the results; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Results
The spatio-temporal trend of diabetes prevalence by province
In China, the prevalence of diabetes in the age group 20–79 increased from 4.7% in 1990 to 8.0% in 2019, corresponding to an increase of 71.1% (Fig. S2a). We predicted that the prevalence would further increase from 8.2% in 2020 (∼88.7 million people living with diabetes) to 9.7% (∼108.4 million) in 2030 in China (Fig. S2a).
The prevalence was projected to rise in 33 Chinese provinces and SARs during 2020–2030, compared to 2019 (Table S2). The highest prevalence was in Beijing in 2019 (14.8%) and was projected to increase from 15.2% to 17.0% during 2020–2030.
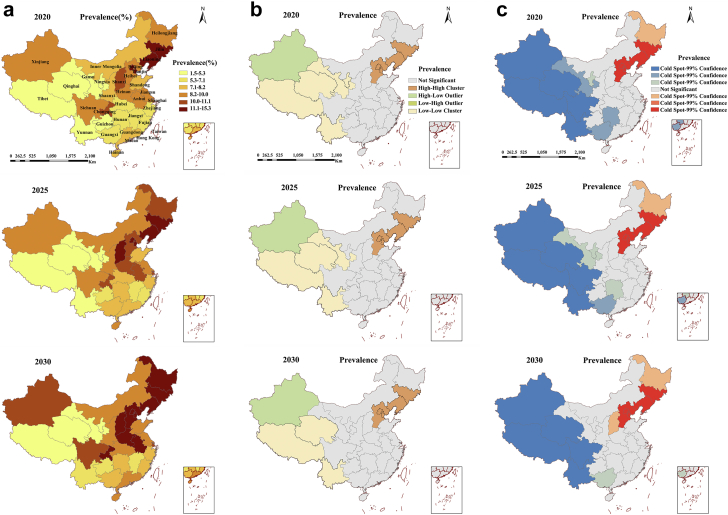
Provinces with a high prevalence of diabetes were mostly distributed in Northeast, North, and East China, whereas low prevalence provinces were distributed in Southwest and Northwest China (Fig. 1a). Consistently, spatial autocorrelation analysis also showed that regions with a high-risk prevalence of diabetes were mainly aggregated in Northeast and North China (local Moran analysis, P < 0.001), whereas regions with low-risk prevalence, were aggregated in Southwest China during 2020–2030 (Fig. 1b). A hot spot analysis also demonstrated similar findings (Fig. 1c).
Fig. 1.
Spatial distribution (a), local Moran analysis (b) and hot spot analysis (c) of the prevalence of diabetes in China for 2020, 2025 and 2030.
The spatio-temporal trend of DALY of diabetes by province
The DALY rates of diabetes in Chinese adults increased from 547/100,000 person-years in 1990 to 825/100,000 person-years in 2019, corresponding to an increase of 50.8% (Fig. S2b). We predicted that the DALY rates would further increase from 846/100,000 person-years in 2020 to 1165/100,000 person-years in 2030 in China (Fig. S2b).
The DALY rates caused by diabetes increased to various extents in 33 Chinese provinces and SARs during 2020–2030, and spatial autocorrelation analysis showed no significant spatial distribution trend across the country.
The spatio-temporal trend of the economic burden of diabetes by province
Based on the current trend projection, China's GDP will grow from $15.9 trillion in 2020 to $27.2 trillion in 2030.
In China, we projected that the total costs of diabetes in adults would increase from $250.2 billion in 2020 to $460.4 billion in 2030, corresponding to an annual growth rate of 6.32% (5.99%–6.65%) during 2020–2030 (Table 1, Table S3). The total costs of diabetes were projected to rise in 33 Chinese provinces and SARs during 2020–2030 (the annual growth rate ranged from 5.15% to 8.02%, Table 1).
Table 1.
Projection of total costs (direct costs and indirect costs) of diabetes in China and its provinces (US $billion).
| Province | Baseline |
Projection |
Annual growth rate (%) during 2020–2030 | |||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2025 | 2030 | |||
| Northeast | Heilongjiang | 4.8 (3.8, 0.9) | 5.1 (4.1, 1.1) | 6.9 (5.5, 1.4) | 8.5 (7.0, 1.5) | 5.23 (5.65, 3.51) |
| Jilin | 4.4 (3.3, 1.1) | 4.8 (3.6, 1.2) | 6.6 (4.7, 1.9) | 8.2 (5.9, 2.3) | 5.62 (5.20, 6.74) | |
| Liaoning | 9.7 (7.4, 2.3) | 10.5 (8.0, 2.6) | 14.5 (10.7, 3.7) | 17.9 (13.8, 4.1) | 5.44 (5.71, 4.56) | |
| North | Beijing | 17.8 (15.6, 2.3) | 19.1 (16.6, 2.5) | 26.1 (21.9, 4.3) | 33.5 (27.8, 5.7) | 5.84 (5.39, 8.36) |
| Hebei | 10.6 (8.6, 2) | 11.5 (9.2, 2.3) | 16.0 (12.6, 3.4) | 20.4 (16.5, 3.9) | 5.93 (6.06, 5.43) | |
| Inner Mongolia | 5.8 (4.5, 1.3) | 6.3 (4.9, 1.4) | 9.1 (6.6, 2.5) | 12.3 (8.7, 3.7) | 7.01 (6.00, 9.92) | |
| Shanxi | 6.0 (5.0, 1.0) | 6.5 (5.3, 1.2) | 9.1 (7.2, 1.9) | 11.8 (9.4, 2.5) | 6.22 (5.88, 7.62) | |
| Tianjin | 5.3 (3.9, 1.4) | 5.8 (4.2, 1.6) | 8.1 (5.5, 2.7) | 10.6 (7, 3.6) | 6.25 (5.30, 8.37) | |
| East | Anhui | 6.6 (4.9, 1.7) | 7.2 (5.3, 1.9) | 10.5 (7.3, 3.2) | 13.8 (9.8, 3.9) | 6.80 (6.55, 7.45) |
| Fujian | 5.9 (4.1, 1.8) | 6.4 (4.4, 2.0) | 9.3 (6.0, 3.2) | 11.9 (7.9, 4) | 6.36 (6.05, 7.00) | |
| Jiangsu | 18.4 (12.6, 5.8) | 20 (13.5, 6.5) | 29.6 (18.8, 10.8) | 38.9 (25.1, 13.8) | 6.89 (6.46, 7.70) | |
| Jiangxi | 3.3 (2.8, 0.5) | 3.6 (3.0, 0.6) | 5.2 (4.2, 1.0) | 6.8 (5.6, 1.2) | 6.56 (6.26, 8.01) | |
| Shandong | 14 (9.6, 4.4) | 15.2 (10.3, 4.9) | 21.8 (14.1, 7.7) | 28.1 (18.7, 9.4) | 6.35 (6.23, 6.59) | |
| Shanghai | 10.3 (8.1, 2.2) | 11.1 (8.6, 2.5) | 14.9 (11.2, 3.7) | 18.3 (14.2, 4.1) | 5.15 (5.24, 4.83) | |
| Zhejiang | 10.5 (7.8, 2.8) | 11.4 (8.3, 3.1) | 16.1 (11.2, 4.9) | 20.9 (14.8, 6.1) | 6.24 (6.03, 6.74) | |
| South | Guangdong | 23.5 (18.1, 5.4) | 25.4 (19.4, 6) | 35.2 (25.5, 9.7) | 45.1 (32.6, 12.5) | 5.93 (5.42, 7.38) |
| Guangxi | 4.0 (3.0, 1.0) | 4.3 (3.2, 1.2) | 6.3 (4.4, 1.9) | 8.3 (5.8, 2.5) | 6.69 (6.27, 7.75) | |
| Hainan | 1.3 (1.1, 0.3) | 1.4 (1.1, 0.3) | 2.0 (1.5, 0.5) | 2.6 (2, 0.6) | 6.41 (6.02, 7.80) | |
| Central | Henan | 11.3 (8.8, 2.5) | 12.2 (9.4, 2.8) | 17.4 (12.9, 4.5) | 22.7 (17.1, 5.6) | 6.45 (6.17, 7.33) |
| Hubei | 7.5 (5.9, 1.6) | 8.1 (6.3, 1.8) | 11.7 (8.6, 3) | 15.4 (11.5, 3.9) | 6.59 (6.26, 7.64) | |
| Hunan | 8.1 (6.0, 2.0) | 8.8 (6.5, 2.3) | 12.9 (9.1, 3.8) | 17 (12.1, 4.9) | 6.88 (6.51, 7.84) | |
| Northwest | Gansu | 1.9 (1.5, 0.4) | 2.0 (1.6, 0.4) | 3.0 (2.3, 0.6) | 3.9 (3.2, 0.8) | 6.81 (6.92, 6.40) |
| Ningxia | 1.0 (0.9, 0.1) | 1.1 (0.9, 0.1) | 1.5 (1.3, 0.2) | 2.0 (1.7, 0.3) | 6.71 (6.45, 8.18) | |
| Qinghai | 0.9 (0.7, 0.2) | 0.9 (0.7, 0.2) | 1.4 (1.0, 0.4) | 1.9 (1.3, 0.6) | 7.36 (6.43, 9.80) | |
| Shaanxi | 6.7 (5.5, 1.2) | 7.2 (5.9, 1.3) | 10.6 (8.2, 2.5) | 14.3 (10.8, 3.5) | 7.11 (6.32, 10.01) | |
| Xinjiang | 4.9 (4.2, 0.8) | 5.3 (4.5, 0.8) | 7.3 (6.0, 1.3) | 9.4 (7.8, 1.6) | 5.94 (5.77, 6.78) | |
| Southwest | Chongqing | 5.0 (3.7, 1.4) | 5.5 (3.9, 1.5) | 8.5 (5.7, 2.8) | 11.8 (7.8, 4) | 8.02 (7.15, 9.96) |
| Guizhou | 2.4 (1.7, 0.7) | 2.6 (1.9, 0.8) | 4.1 (2.7, 1.4) | 5.7 (3.6, 2) | 7.96 (6.94, 10.14) | |
| Sichuan | 11.7 (9.4, 2.3) | 12.7 (10.1, 2.6) | 18.4 (13.9, 4.4) | 24.1 (18.2, 5.8) | 6.62 (6.13, 8.31) | |
| Tibet | 0.2 (0.1, 0) | 0.2 (0.1, 0) | 0.2 (0.1, 0.1) | 0.3 (0.2, 0.1) | 5.69 (4.10, 9.04) | |
| Yunnan | 3.6 (2.9, 0.7) | 3.9 (3.1, 0.8) | 5.6 (4.2, 1.3) | 7.3 (5.6, 1.7) | 6.55 (6.28, 7.50) | |
| SARs | Hong Kong | 3.2 (2.1, 1.1) | 3.5 (2.2, 1.3) | 4.9 (3.1, 1.8) | 5.9 (4.0, 2.0) | 5.41 (5.86, 4.57) |
| Macao | 0.4 (0.2, 0.2) | 0.4 (0.2, 0.2) | 0.6 (0.3, 0.3) | 0.7 (0.4, 0.3) | 6.01 (7.46, 4.19) | |
| Total | 231.0 (177.7, 53.3) | 250.2 (190.2, 60) | 355.2 (258.4, 96.8) | 460.4 (337.8, 122.6) | 6.32 (5.98, 7.31) | |
SARs: Special administrative regions.
We projected the direct costs of diabetes would increase from $190.2 b in 2020 to $337.8 b in 2030 in China, corresponding to an annual growth rate of 5.98% (5.82%–6.13%) (Table 1, Table S3). The direct costs of diabetes were projected to rise in 33 Chinese provinces and SARs during 2020–2030 (the annual growth rate ranged from 4.10% to 7.46%, Table 1).
In comparison, we projected the indirect costs of diabetes would increase from $60.0 b in 2020 to $122.6 b in 2030, corresponding to an annual growth rate of 7.31% (6.47%–8.15%) (Table 1, Table S3). The indirect costs of diabetes were projected to rise in 33 Chinese provinces and SARs during 2020–2030 (the annual growth rate ranged from 3.51 to 10.14%, Table 1). Notably, the indirect costs, as a percentage of the total costs, have increased by 2.6% from 24.0% to 26.6% during 2020–2030 in China, corresponding to an annual growth rate of 0.93% (0.44%–1.42%) (Table S4), and corresponding changes in Chinese provinces and SARs ranged between −7.4% and 10.3%.
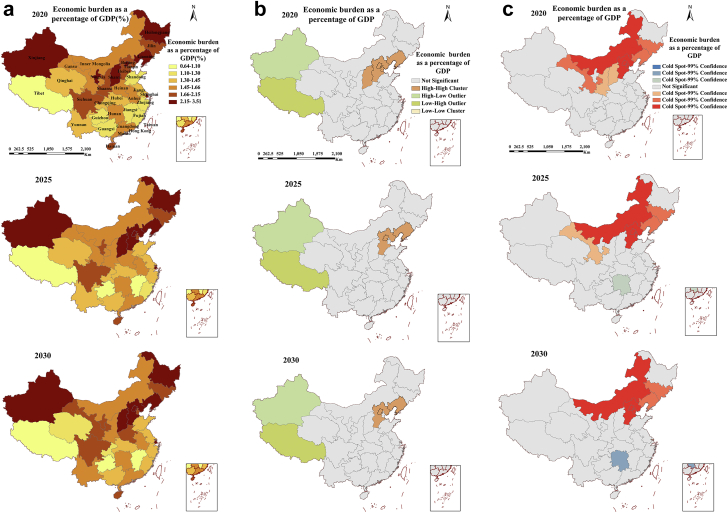
The spatio-temporal trend of the economic burden of diabetes as a percentage of GDP by province
Nationwide, the total costs of diabetes would grow faster than China's GDP growth rate during 2020–2030. We projected that the total costs of diabetes as a percentage relative to its corresponding GDP would increase from 1.58% to 1.69% in China during this period, corresponding to an annual growth rate of 0.76% (0.64–0.88%) (Table S4). Across 33 Chinese provinces and SARs, the estimated percentages increased from 0.69% to 3.51% in 2020 to 0.64%–3.22% in 2030, corresponding to a varying range of annual growth rate of −0.92–3.71% during 2020–2030 (Table S5).
Provinces with high total costs of diabetes as a percentage of GDP were largely distributed in northern China, whereas the low percentage counterparts were distributed in Southwest, South and Southeast China (Fig. 2a). Consistently, spatial autocorrelation analysis showed provinces with high-risk percentages were mainly aggregated in Northeast and North China (local Moran analysis, P < 0.001), but the aggregation of low-risk percentage provinces was not observed (Fig. 2b). A hot spot analysis also demonstrated similar findings (Fig. 2c).
Fig. 2.
Spatial distribution (a), local Moran analysis (b) and hot spot analysis (c) of the cost as a share of GDP of diabetes in China for 2020, 2025 and 2030.
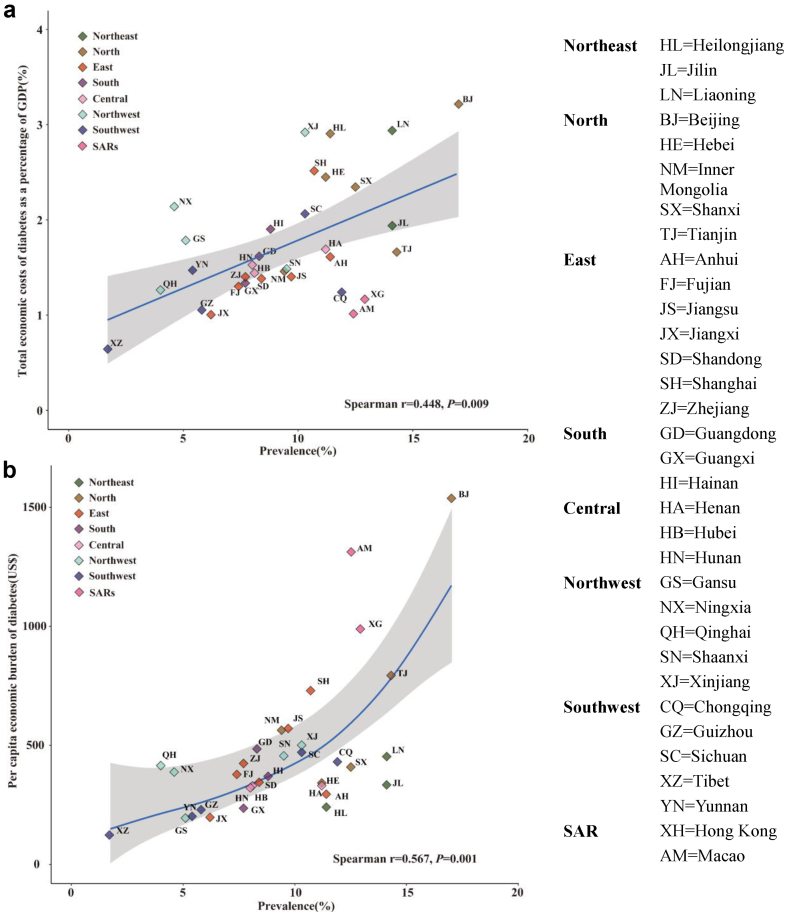
The total costs of diabetes as a percentage of GDP were positively correlated with the prevalence of diabetes in all 33 Chinese provinces and SARs in 2030 (Spearman r = 0.448, P = 0.009, Fig. 4a).
Fig. 4.
The Pearson correlation between total economic costs of diabetes as a percentage of GDP (a), per capita economic burden of diabetes (b) and prevalence of diabetes in all 33 Chinese provinces and SARs in 2030.
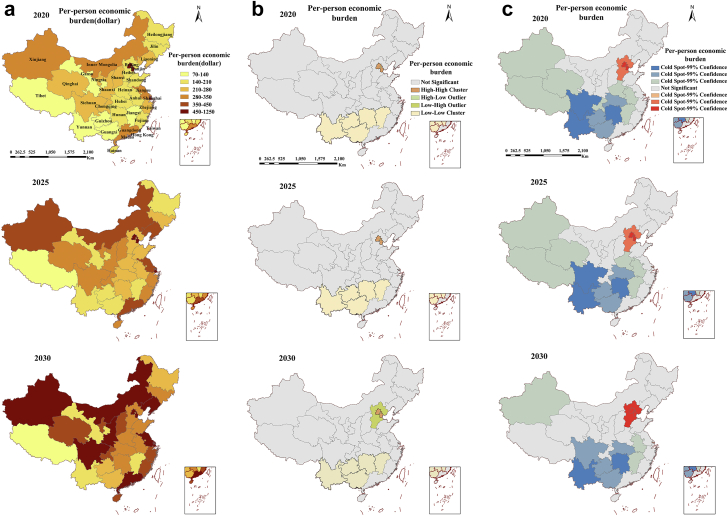
The spatio-temporal trend of the per-capita economic burden of diabetes by province
We projected that the per capita economic burden of diabetes would increase from $231 in 2020 to $414 in 2030 in China, corresponding to an annual growth rate of 6.02% (5.73%–6.31%) (Table S3). Across 33 Chinese provinces and SARs, the estimated per capita economic burden increased from $71–$931 in 2020 to $124–$1538 in 2030, corresponding to a range of annual growth rate of 4.56%–7.70% during 2020–2030 (Table S6).
Provinces with a high per capita economic burden of diabetes were mainly distributed in North China (Beijing, Tianjin) and East China (Shanghai) in 2020 and 2025, and with some additional regions to be on the list in 2030, including Northeast China (Liaoning), North China (Inner Mongolia), Northwest China (Shaanxi, Xinjiang), Southwest China (Sichuan), East China (Jiangsu) and South China (Guangdong) (Fig. 3a). Consistently, spatial autocorrelation analysis showed that regions with high-risk per capita economic burden of diabetes were mainly aggregated in North China (Beijing and Tianjin) (local Moran analysis, P < 0.001), whereas aggregation of regions with low-risk per capita economic burden was aggregated in Southwest China during 2020–2030 (Fig. 3b). A hot spot analysis also demonstrated similar findings (Fig. 3c).
Fig. 3.
Spatial distribution (a), local Moran analysis (b) and hot spot analysis (c) of the per-person economic burden of diabetes in China for 2020, 2025 and 2030.
The per capita economic burden of diabetes was positively correlated with the prevalence of diabetes in all 33 Chinese provinces and SARs in 2030 (Spearman r = 0.567, P = 0.001, Fig. 4b).
Discussion
Our study reports that the diabetes prevalence in Chinese adults aged 20–79 years was projected to increase from 8.2% in 2020 to 9.7% in 2030. The total costs of diabetes were projected to increase from $250.2 billion to $460.4 billion over the same period, representing an annual growth rate of 6.32%. In line with increased total costs, the per-capita cost of diabetes increased from $231 in 2020 to $414 in 2030, representing an annual growth rate of 6.02%. Moreover, the total costs as a percentage of GDP are projected to increase from 1.58% to 1.69% during 2020–2030, indicating a more rapid growth rate of the economic burden of diabetes than that of the country's GDP growth. Furthermore, the indirect costs as a percentage of the total costs will also increase from 24.0% to 26.6% in the same period. The regions with high diabetes prevalence and with a high economic burden of diabetes are largely aggregated in Northeast and/or North China.
Our study projected an ongoing increase in the prevalence of diabetes in the Chinese adult aged 20–79 years from 8.2% in 2020 to 9.7% in 2030, consistent with previous studies.29,30 The ongoing growing trend of diabetes prevalence in China may attribute to multiple factors such as the increasing prevalence of overweight and obesity, environmental pollution, changes in dietary patterns, urbanisation, aging, and diabetogenic effects of COVID-19.31, 32, 33, 34 Our study further demonstrates that the regions with a high risk of diabetes prevalence are largely concentrated in Northeast and North China during 2020–2030, consistent with other studies.35 These regional differences are likely due to the geographical differences in the exposure to certain risk factors.30,36 For example, studies have reported that the prevalence of obesity is markedly higher in northern China than in the southern regions of China.36 Similarly, high PM2.5 concentration is more frequently reported in northern provinces in China such as Beijing, Tianjin, Hebei, Shandong, and Henan provinces.37 Furthermore, significant differences in dietary patterns and lifestyle between northern and southern China also add to the observed disparity in diabetes prevalence in the country.17
Our study projected an almost doubling in the total costs of diabetes (from $250.2 billion to $460.4 billion) during 2020–2030 in China, an annual growth rate of 6.32%. The total economic burden of diabetes as a percentage of GDP would also increase from 1.58% to 1.69% in China during this period, with an estimated annual growth rate of 0.76%. Similar positive growth is also observed in most of the 33 Chinese provinces and SARs. The positive growth indicated that the overall growth rate of the total economic burden of diabetes in China is significantly higher than that of GDP growth in 2020–2030, suggesting more healthcare resources are required to combat the increasing demand for diabetes care. Consistently, we also estimate that the per-capita cost of diabetes will increase steadily (from $231 in 2020 to $414) in 2030 in China. This increase accurately portrays the rising economic burden of diabetes on individuals. The spatial aggregation of the high economic burden of diabetes in Northeast and North China is likely due to the disproportionate disease burden of diabetes and the relatively low GDP in northern China.
Based on the above findings, we recommend multi-fold policy changes and interventions to reverse the projected growing trend and spatial inequality of the disease and economic burden of diabetes in China. To address these increasing burdens, fortunately, the Chinese government has enacted the ‘Healthy China 2030’ plan to strengthen the prevention and control of chronic diseases. Accordingly, we propose three potential interventions. Firstly, early intervention and education on diabetes should be significantly scaled-up, with a strong focus on early diabetes diagnosis and treatment in high-risk areas. Secondly, we recommend integrating current hospital-based diabetes care with community-based prevention and treatment. The integrated models will improve accessibility and treatment adherence for diabetic patients, and also enable better follow-up of pre-treatment monitoring in pre-diabetic individuals. Thirdly, our study calls for orchestrated cooperation between multiple governmental bodies and institutions in diabetes prevention and treatment. Improving affordability of the health insurance for rural residents, lowering pharmaceutical costs, and improving the accessibility to basic diabetes drugs are essential for reducing the burden of diabetes in China. Furthermore, education to promote healthy lifestyles, regular medical care, and blood sugar control are beneficial for diabetes control on the individual level.
Our study demonstrates that indirect costs account for about a quarter of the total costs for diabetes and the percentage is increasing during 2020–2030. The indirect costs as a percentage of the total costs will increase from 24.0% to 26.6% during 2020–2030 in China, at an annual growth rate of 0.93%. The impact of the increasing rate on people's well-being and the economy should not be overlooked. Reduced or lost productivity due to diabetes imposes a significant potential burden on China's labour force and economic activities. Reduction in the indirect economic burden can be achieved by improving the self-management ability of diabetic patients, controlling blood glucose levels with appropriate medications, and preventing the occurrence of complications and disabilities. Besides, the government health institutions need to take active measures in the allocation of medical resources for ensuring that sufficient societal and financial support is provided to the carers of diabetic patients, in an effort of alleviating severe complications of diabetes.
This study has several limitations. First, we assumed a constant diagnosis rate of diabetes patients as reported by the IDF 20191 between 2020 and 2030. In reality, the diagnosis rate will likely increase and the direct costs of diabetes may have been conservatively estimated. Second, the study forecasted the GDP of 33 Chinese provinces and SARs for 2020–2030 without considering the economic impact of unexpected events such as COVID-19. Our study was based on an optimistic view of the Chinese GDP forecast results, which may lead to an overestimation of the indirect economic burden of diabetes. Furthermore, because COVID-19 exacerbates diabetes and increases the risk of diabetic complications leading to disability or premature death, this portion of the DALY burden of diabetes caused by COVID-19 has not been accounted for, potentially underestimating the indirect costs of diabetes. Third, in our study, our prediction of future outcomes for DALY rates did not take into consideration of the impact of diabetes prevalence but project the future trend of DALY rate based on trends during 1990–2019. The simplified approach may result in potential bias in the calculation of DALY during 2020–2030. Fourth, our study did not stratify diabetes by its types, as China's national reports on health expenditure and other economic indicators on diabetes did not provide type-specific data. Fifth, we calculate the productivity loss and indirect economic burden based on DALY weights, and this approach cannot reflect the composition of indirect economic burden (absenteeism, presenteeism, and labour-force dropout). Finally, GBD's analysis of diabetes prevalence and DALY rates has its limitation due to the limited availability of primary data. Although GBD has provided a standardised approach for estimating the disease burden of diabetes across all Chinese provinces, substantial data adjustments were required and may deviate from the actual disease burden in the provinces.38
In conclusion, our study projects a significant growth of disease and economic burden of diabetes in China during 2020–2030, with strong spatial aggregation in northern Chinese regions. We also project that the increase in economic burden will exceed that of GDP, even without considering the adverse effects of COVID-19 on both the economy and diabetes. The indirect economic burden of diabetes remains a growing and significant part of the total economic burden of diabetes in China. Effective and innovative strategies remain a priority for diabetes prevention and control in the country.
Contributors
Dr LZ had full access to all the data in the study and took responsibility for the integrity of the data and the data analysis accuracy. Study concept and design: All authors; Acquisition of data: JL, ML, MS; Analysis and interpretation of data: JL, ML, CL, MS; Drafting of the manuscript: LZ, JL; Critical revision of the manuscript for important intellectual content: ZC, CL, YW, GZ; Statistical analysis: JL, ML, MS; Administrative, technical, or material support: all authors; Obtained funding: LZ; Study supervision: LZ, GZ.
Data sharing statement
To download GBD data used in the analyses in this article please visit the Global Health Data Exchange GBD 2019 website (https://ghdx.healthdata.org/gbd-2019).
Declaration of interests
All authors declare that they have no competing interests.
Acknowledgements
Funding statement: This study was supported by the National Natural Science Foundation of China (Grant number: 8191101420 (LZ)), Outstanding Young Scholars Funding (Grant number: 3111500001(LZ)), Xi'an Jiaotong University Basic Research and Profession Grant (Grant number: xtr022019003 (LZ), xzy032020032(LZ)), Xi'an Jiaotong University Young Talent Support Grant (Grant number: YX6J004(LZ)), National Key R&D Program of China (2022YFC2505100 (MS)), the National Natural Science Foundation of China (12171387 (MS)); China Postdoctoral Science Foundation (2018M631134 (MS), 2020T130095ZX (MS)); and Young Talent Support Program of Shaanxi University Association for Science and Technology (20210307 (MS)). The funders had no role in the study design, data collection, data analysis, interpretation or writing of the manuscript.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100700.
Contributor Information
Guihua Zhuang, Email: zhuanggh@mail.xjtu.edu.cn.
Lei Zhang, Email: lei.zhang1@monash.edu.
Appendix A. Supplementary data
References
- 1.International Diabetes Federation IDF diabetes atlas. 2019. http://www.diabetesatlas.org 9th ed. Belgium.
- 2.Zimmet P.Z., Magliano D.J., Herman W.H., Shaw J.E. Diabetes: a 21st century challenge. Lancet Diabetes Endocrinol. 2014;2(1):56–64. doi: 10.1016/S2213-8587(13)70112-8. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2017 Population and Fertility Collaborators (2018) Population and fertility by age and sex for 195 countries and territories, 1950-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1995–2051. doi: 10.1016/S0140-6736(18)32278-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farrell K., Westlund H. China's rapid urban ascent: an examination into the components of urban growth. Asian Geogr. 2018;35(1):85–106. [Google Scholar]
- 5.Palmer A.K., Gustafson B., Kirkland J.L., Smith U. Cellular senescence: at the nexus between ageing and diabetes. Diabetologia. 2019;62(10):1835–1841. doi: 10.1007/s00125-019-4934-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NCD Risk Factor Collaboration (NCD-RisC) (2016) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patterson R., McNamara E., Tainio M., et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur J Epidemiol. 2018;33(9):811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.International Diabetes Federation IDF diabetes atlas. 2013. http://www.diabetesatlas.org 6th ed. Belgium.
- 9.International Diabetes Federation IDF diabetes atlas. 2021. https://diabetesatlas.org/atlas/tenth-edition/ 10th ed. Belgium.
- 10.Liu J., Bai R., Chai Z., Cooper M.E., Zimmet P.Z., Zhang L. Low- and middle-income countries demonstrate rapid growth of type 2 diabetes: an analysis based on Global Burden of Disease 1990-2019 data. Diabetologia. 2022;65(8):1339–1352. doi: 10.1007/s00125-022-05713-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou M., Wang H., Zeng X., et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ettaro L., Songer T.J., Zhang P., Engelgau M.M. Cost-of-illness studies in diabetes mellitus. Pharmacoeconomics. 2004;22(3):149–164. doi: 10.2165/00019053-200422030-00002. [DOI] [PubMed] [Google Scholar]
- 13.Seuring T., Archangelidi O., Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. 2015;33(8):811–831. doi: 10.1007/s40273-015-0268-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bommer C., Sagalova V., Heesemann E., et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963–970. doi: 10.2337/dc17-1962. [DOI] [PubMed] [Google Scholar]
- 15.Tang K., Wang H., Liu Y., Tan S.H. Interplay of regional economic development, income, gender and type 2 diabetes: evidence from half a million Chinese. J Epidemiol Community Health. 2019;73(9):867–873. doi: 10.1136/jech-2018-211091. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization . 2018. Global health expenditure database (GHED)https://apps.who.int/nha/database/Select/Indicators/en [Google Scholar]
- 17.National Center for Chronic and Non-communicable Disease Control and Prevention . 2013. Chinese center for disease control and prevention, China chronic disease and risk factors surveillance report. [Google Scholar]
- 18.National Bureau of Statistics of China . China Statistics Publishing House; 2020. China Statistical Yearbook.http://www.stats.gov.cn/tjsj/ndsj/2020/indexch.htm [Google Scholar]
- 19.National Health Commission of the People's Republic of China . China Union Medical University Press; 2020. China health statistics Yearbook. [Google Scholar]
- 20.Pedroza C. A Bayesian forecasting model: predicting U.S. male mortality. Biostatistics. 2006;7(4):530–550. doi: 10.1093/biostatistics/kxj024. [DOI] [PubMed] [Google Scholar]
- 21.Getis A. Reflections on spatial autocorrelation Regional science & urban economics. 2007;37(4):491–496. [Google Scholar]
- 22.Zulu L.C., Kalipeni E., Johannes E. Analyzing spatial clustering and the spatiotemporal nature and trends of HIV/AIDS prevalence using GIS: the case of Malawi, 1994-2010. BMC Infect Dis. 2014;14:285. doi: 10.1186/1471-2334-14-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Getis A., Ord J.K. Local spatial association statisticss distribution:distribution issues and an application. Geogr Anal. 1995;24:286–306. [Google Scholar]
- 24.Bommer C., Heesemann E., Sagalova V., et al. The global economic burden of diabetes in adults aged 20-79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5(6):423–430. doi: 10.1016/S2213-8587(17)30097-9. [DOI] [PubMed] [Google Scholar]
- 25.Cai L., He J., Zhao K., et al. Sciences Press; 2016. Theories and practices in study of burden of chronic diseasea; pp. 45–46. [Google Scholar]
- 26.Murray C.J., Kreuser J., Whang W. Cost-effectiveness analysis and policy choices: investing in health systems. Bull World Health Organ. 1994;72(4):663–674. [PMC free article] [PubMed] [Google Scholar]
- 27.Gao S., Yang W.-S., Bray F., et al. Declining rates of hepatocellular carcinoma in urban Shanghai: incidence trends in 1976-2005. Eur J Epidemiol. 2012;27(1):39–46. doi: 10.1007/s10654-011-9636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu J., Ren Z.-H., Qiang H., et al. Trends in the incidence of diabetes mellitus: results from the Global Burden of Disease Study 2017 and implications for diabetes mellitus prevention. BMC Public Health. 2020;20(1):1415. doi: 10.1186/s12889-020-09502-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu Y., Wang L., He J., et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–959. doi: 10.1001/jama.2013.168118. [DOI] [PubMed] [Google Scholar]
- 30.Li Y., Teng D., Shi X., et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997. doi: 10.1136/bmj.m997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xi B., Liang Y., He T., et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993-2009. Obes Rev. 2012;13(3):287–296. doi: 10.1111/j.1467-789X.2011.00944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang J., Wang Z., Du W., et al. Twenty-five-year trends in dietary patterns among Chinese adults from 1991 to 2015. Nutrients. 2021;13(4) doi: 10.3390/nu13041327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rubino F., Amiel S.A., Zimmet P., et al. New-onset diabetes in Covid-19. N Engl J Med. 2020;383(8):789–790. doi: 10.1056/NEJMc2018688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang L., Shang X., Sreedharan S., et al. Predicting the development of type 2 diabetes in a large Australian cohort using machine-learning techniques: longitudinal survey study. JMIR Med Inform. 2020;8(7) doi: 10.2196/16850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou M., Astell-Burt T., Bi Y., et al. Geographical variation in diabetes prevalence and detection in China: multilevel spatial analysis of 98,058 adults. Diabetes Care. 2015;38(1):72–81. doi: 10.2337/dc14-1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tang D., Bu T., Feng Q., Liu Y., Dong X. Differences in overweight and obesity between the North and South of China. Am J Health Behav. 2020;44(6):780–793. doi: 10.5993/AJHB.44.6.4. [DOI] [PubMed] [Google Scholar]
- 37.Liang F., Yang X., Liu F., et al. Long-term exposure to ambient fine particulate matter and incidence of diabetes in China: a cohort study. Environ Int. 2019;126:568–575. doi: 10.1016/j.envint.2019.02.069. [DOI] [PubMed] [Google Scholar]
- 38.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.