Abstract
Aneurysmal subarachnoid hemorrhage (aSAH) is a severe type of acute brain injury with high mortality and burden of neurological sequelae. General management aims at early aneurysm occlusion to prevent re-bleeding, cerebrospinal fluid drainage in case of increased intracranial pressure and/or acute hydrocephalus, and cerebral blood flow augmentation in case of delayed ischemic neurological deficits. In addition, the brain is vulnerable to physiological insults in the acute phase and neurointensive care (NIC) is important to optimize the cerebral physiology to avoid secondary brain injury. NIC has led to significantly better neurological recovery following aSAH, but there is still great room for further improvements. First, current aSAH NIC management protocols are to some extent extrapolated from those in traumatic brain injury, notwithstanding important disease-specific differences. Second, the same NIC management protocols are applied to all aSAH patients, despite great patient heterogeneity. Third, the main variables of interest, intracranial pressure and cerebral perfusion pressure, may be too superficial to fully detect and treat several important pathomechanisms. Fourth, there is a lack of understanding not only regarding physiological, but also cellular and molecular pathomechanisms and there is a need to better monitor and treat these processes. This narrative review aims to discuss current state-of-the-art NIC of aSAH, knowledge gaps in the field, and future directions towards a more individualized care in the future.
Keywords: Aneurysmal subarachnoid hemorrhage, Multimodal monitoring, Neurointensive care, Precision medicine
1. Introduction
Aneurysmal subarachnoid hemorrhage (aSAH) is a severe form of acute brain injury that is treated in the neurointensive care (NIC) unit. The mainstay of NIC is to monitor systemic and cerebral physiology and to prevent and treat avoidable factors that could otherwise induce secondary brain injury.1,2 Since the initiation and development of NIC, clinical outcome has significantly improved for aSAH patients.2 However, several challenges still exist.
First, current aSAH gudielines3,4 and local management protocols5 of NIC variables such as intracranial pressure (ICP) and cerebral perfusion pressure (CPP) are either absent or to a great degree developed based on those from severe traumatic brain injury (TBI), which stands as the prototype disease in NIC. However, the same targets and threholds may not apply in both diseases.6 Second, the same NIC targets are to a great extent applied for all aSAH patients under most circumstances, despite inter- (demography, co-morbidities, extent of injury) and intraindividual (throughout the temporal course of the acute phase) differences. Third, current NIC targets such as ICP and CPP are only surrogates of the cerebral environment, but their validity to predict the actual intracranial state globally and focally may be questioned.7,8 The development of new multimodality monitoring (MMM) tools to assess cerebral blood flow (CBF; imaging and invasive probes), CBF autoregulation (e.g. pressure reactivity index), brain tissue oxygenation (btO2 and jugular bulb), and cerebral energy metabolism (microdialysis) have improved our understanding of disease pathophysiology and the cerebral effects of treatments, but their validity to guide management still remains unclear considering their inherent temporal, spatial, and logistical constraints. Fourth, the focus of NIC has been directed towards systemic and cerebral physiological optimization, but this does not address all pathomechanisms that occur on a cellular and molecular level such as neuroinflammation, neurodegeneration, and neurorepair.9,10 A better understanding of this could potentially contribute to the development of appropriate pharmacological agents and administration of these in an optimal time window based on high-resolution bedside monitoring data.
Consequently, although the development of NIC in aSAH has been a success from a historical point of view,2 there is clearly room for further improvement. The aim of this narrative review was to discuss the current knowledge gaps, the limitation of extrapolation of TBI guidelines to aSAH,3,4,11 and more particularly about fine tuning of NIC in aSAH to individualize care both in terms of cerebral physiology and molecular injury patterns.
2. Individualized therapy in neurointensive care – the role of multimodality monitoring
There are several physiological steps that affect CBF and the cerebral delivery of oxygen (CDO2) as well as nutrients (glucose and lactate; CDGlc and CDLac) and there are many pathomechanisms that may interfere (Fig. 1). Evovling secondary brain injury can be fairly detected as a neurological deterioration, clinically assessed by repeated neurological examinations, although this is more challenging in unconscious patients that require intubation, mechanical ventilation, and sedation. In classic NIC, ICP and CPP are monitored in unconscious aSAH patients and treatment aims to avoid intracranial hypertension and to ensure sufficient cerebral perfusion. However, even in case of normal ICP and CPP, disturbances in CBF, btO2, and cerebral energy metabolism are frequent.8,12, 13, 14 For that reason, there has been a development of MMM tools to enable monitoring of the different steps to achieve cerebral energy metabolism (Table 1, Table 2). Monitoring may then also include cerebral pressure autoregulation (pressure reactivity index, mean flow index), CBF (intraparenchymal probes, transcranial Doppler, and radiological imaging), brain tissue oxygenation (jugular bulb, btO2), and cerebral energy metabolism (microdialysis and radiological imaging). Ideally, a complete MMM setup enables earlier detection of impending brain injury and diagnosis of the specific pathomechanisms, which in turn predispose for more cause-specific therapies. However, so far, the implementation of MMM-based management has been limited to a few research-oriented NIC units.15,16 A major reason for this is that controversy remains regarding the validity to guide management based on these MMM-tools. For example, the microdialysis only represents a small brain region and the rationale to guide a global therapy such as CPP-levels is questionable considering the regional differences in cerebral injury patterns and pathophysiology.7 At the same time, a global measure such as jugular bulb oxygenation may be too insensitive to detect small, but important, focal cerebral oxygen disturbances. Another problem is that some methods such as radiological imaging only gives snap-shots of the cerebral status. However, even if no MMM tool is perfect, the combined analysis of the information obtained by the different techniques may provide a more accurate picture of the cerebral situation. Altogether, MMM carries great potential, despite existing limitations (Fig. 2). In the sections below, we discuss the different steps to optimize cerebral energy metabolism divided into the CBF-, oxygenation-, and nutrient-patways together with factors involved in energy metabolism (Fig. 1).
Fig. 1.
Physiological pathways, pathomechanisms, and management options to optimize cerebral energy metabolism in aSAH.
The figure describes the different pathways to ensure cerebral energy metabolism. In the CBF pathway, MAP and ICP determine CPP, which together with the cerebral autoregulation determine CBF. In the oxygenation pathway, pO2 and HgB determine the CaO2, which together with CBF constitute the CDO2. In the nutrient pathway, CaGlc and CaLac are defined as the arterial content of these metabolites, which together with CBF determine CDGlc and CDLac. CDGlc, CDLac, and CDO2 are necessary for the cerebral production of energy, which takes place in the cytosol and mitochondria of the brain cells. Several pathomechanisms may interfere with each step, which can be addressed to some extent with specifically targeted management strategies, as suggested in the figure.
AR = Autoregulation, aSAH = Aneurysmal subarachnoid hemorrhage, CaGlc = Arterial content of glucose, CaLac = Arterial content of lactate, CaO2 = Arterial content of oxygen, CBF = Cerebral blood flow, CDGlc = Cerebral delivery of glucose, CDLac = Cerebral delivery of lactate, CDO2 = Cerebral delivery of oxygen, CSD = Cortical spreading depolarization, EP = Epilepsy, FiO2 = Fraction of inspired oxygen, Hgb = Hemoglobin, HHH = Hemodilution, hypertension, and hypervolemia, ICP = Intracranial pressure, MAP = Mean arterial blood pressure, pO2 = Partial pressure of oxygen, RBCT = Red blood cell transfusion.
Table 1.
Multimodality monitoring – a selection of methods and their benefits and limitations.
| Physiological variable | Monitoring method | Advantage | Limitations |
|---|---|---|---|
| ICP | EVD | Both monitoring and treatment of ICP by CSF drainage. | Infections. Clotting of the EVD. |
| Intraparenchymal probe | Less invasive than EVD. | Does not offer ICP treatment with CSF drainage. Zero-drift. | |
| CPP | Any ICP monitor combined with arterial line for continuous systemic ABP. | Continuous global estimate of CBF. | Spatial constraints; does not take into account differences in cerebral autoregulation or vasospasm. |
| CBF autoregulation | PRx (ICP and ABP) | Measure of the global autoregulatory status. | Requires ICP-monitor. Low signal-to-noise ratio. Spatial constraints; insensitive to focal disturbances. |
| CPPopt (PRx and CPP) | Global CBF surrogate that takes into account autoregulatory status. | Requires advanced software. Still insufficiently studied in aSAH. Spatial constraints; insensitive to focal disturbances. | |
| Mx (TCD and CPP) | Easy to use bedside. May detect regional autoregulatory differences. | User-dependent. Spatial constraints; limited global spatial validity, especially in the posterior circulation | |
| Cerebral blood flow | Radiology (Perfusion-CT, Xe-CT, PET, MRI) | Both global and focal. | Logistics; Difficult to transport unstable patients to the radiology department. Time constraints; represents only a snapshot. |
| TCD | Easy to use bedside. | Measures velocity, not CBF. User-dependent. Spatial constraints; limited global spatial validity, especially in the posterior circulation. Time constraints; monitoring occurs in a limited time interval. | |
| Intraparenchymal thermal diffusion probe | Continuous CBF measure. | Spatial constraints; limited global spatial validity. | |
| Brain tissue oxygenation | Jugular bulb catheter (SjvO2) | Continuous and feasible global measure. | Spatial constraints; low sensitivity for focal ischemia. |
| Intraparenchymal device (BtO2) | Continuous and feasible focal measure. | Spatial constraints; limited global spatial validity, especially in the posterior circulation | |
| NIRS | Non-invasive. | Spatial constraints; limited global spatial validity, especially in the posterior circulation | |
| Cerebral energy metabolism | MD | Feasible for continuous evaluation. | Spatial constraints; limited global spatial validity. |
| PET | Possible to investigate focal/global complex aspects of energy metabolism. | Logistics; Difficult to transport unstable patients to the radiology department. Time constraints; represents only a snapshot. | |
| EEG | Helpful to diagnose cerebral ischemia and NCSE | Complexity; difficult to interpret bedside. |
ABP = Arterial blood pressure, CBF = Cerebral blood flow, CSF = Cerebrospinal fluid, EEG = Electroencephalography, EVD = external ventricular drain, ICP = Intracranial pressure, MD = Microdialysis, Mx = Mean flow index, NCSE = Non-convulsive status epilepticus, NIRS = Near infrared spectroscopy, PET = Positron emission tomography, PRx = Pressure reactivity index, TCD = Transcranial Doppler, Xe-CT = Xenon-enhanced computed tomography.
Table 2.
Monitoring variables, target intervals, and treatments in aSAH – international guidelines (AHA, NCC), local practices (Uppsala), and comparison with TBI (BTF).
| Variable | Target interval | Treatment |
|---|---|---|
| ICP | AHA: CSF drainage with an EVD or a lumbar drainage in case of acute hydrocephalus3 NCC: None4 Uppsala: ICP ≤20 mm Hg5 BTF: ICP ≤22 mm Hg11 |
Head elevation Hematoma evacuation Hyperventilation CSF drainage Sedation Barbiturates Decompressive craniectomy |
|
ABP/CPP i) before aneurysm occlusion ii) after aneurysm occlusion |
AHA: i) avoiding systolic bood pressure (sBP) above 160 mmHg. ii) euvolemia, no strict ABP-/CPP-target3 NCC: i) avoding MAP above 110 mmHg. ii) euvolemia, no strict ABP-/CPP-target4 Uppsala: i) sBP 120–160 mmHg and CPP ≥60 mmHg. ii) CPP ≥60 mmHg5 BTF: i) and ii) not applicable. ii) CPP between 60 and 70 mm Hg11 |
ICP control (above) Intravenous fluids Vasopressors Antihypertensives |
| CBF pressure autoregulation | AHA: No target3 NCC: No target4 Uppsala: No target5 BTF: No target11 |
CPP optimum |
| CBF | AHA: No target3 NCC: No target4 Uppsala: No target20 BTF: No target11 |
CPP-, pCO2-, and autoregulation management |
| Arterial oxygenation | AHA: RBCT may be beneficial for aSAH patients at risk of cerebral ischemia. No specific HgB or pO2 target3 NCC: HgB above 8–10 g/dL. No specific pO2 target4 Uppsala: Hgb >10 g/dL and pO2 ≥ 12 kPa5 BTF: No target11 |
Respiratory optimization Minimize blood loss Red blood cell traunsfusion |
| Arterial glucose | AHA: No specific target, but avoid hypoglycemia3 NCC: 4.4–11.1 mM4 Uppsala: 5–10 mM5 BTF: No target11 Tight glycemic control: 4.4–6.1 mM81 |
Intravenous glucose Insulin injection/infusion |
| Cerebral oxygenation | AHA: No target3 NCC: No target4 Uppsala: No target5 BTF: No target11 |
CBF and arterial oxygenation management |
| Cerebral glucose | AHA: No target3 NCC: No target4 Uppsala: No target, but clinical evaluation if cerebral glucose <0.5 mM (MD)153 BTF: No target11 MD consensus meeting 2014: Cerebral glucose >0.2–0.8 mM92 |
CBF and arterial glucose management |
| Cerebral energy metabolism | AHA: No target3 NCC: No target4 Uppsala: No target, but clinical evaluation if cerebral LPR >40 (MD)153 BTF: No target11 MD consensus meeting 2014: Cerebral LPR <25–4092 |
Optimize the variables above. |
BTF = Brain Trauma Foundation, CBF = Cerebral blood flow, CPP = Cerebral perfusion pressure, CPPopt = Optimal CPP, CSF = Cerebrospinal fluid, ICP = Intracranial pressure, LPR = Lactate-/pyruvate ratio, MD = Microdialysis.
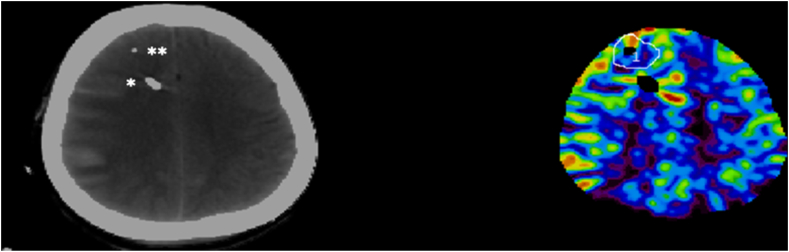
Fig. 2.
Illustration of a multimodality monitoring case in an aSAH patient.
The figure shows an example of multimodality monitoring in aSAH at our center. This aSAH patients was unconscious, intubated, and mechanically ventilated and had therefore received an EVD (∗) for ICP monitoring and cerebral microdialysis (∗∗) for energy metabolic monitoring. Xe-CT imaging was conducted during NIC to estimate global and focal CBF. In addition, CDO2 could be calculated based on CBF and the concurrent CaO2. This type of MMM setup can be used to diagnose the specific cause for imminent cerebral energy metabolic failure, by evaluating concurrent global/focal cerebral ischemia and CDO2. As illustrated, there is significant regional CBF variation, which limits the global validity of focal monitors such as the microdialysis.
aSAH = Aneurysmal subarachnoid hemorrhage, CBF = Cerebral blood flow, CaO2 = Arterial content of oxygen, CDO2 = Cerebral delivery of oxygen, EVD = External ventricular drainage, MMM = Multimodality monitoring, NIC = Neurointensive care, Xe-CT = Xenon-enhanced computed tomography.
3. Individualized therapy – physiological targets to optimize cerebral energy metabolism
3.1. Optimizing CBF
Fig. 1 describes the pathways to optimize cerebral energy metabolism. It is key to maintain a sufficiently high CBF to achieve adequate CDO2 and CDGlc/CDLac. CBF disturbances are common in aSAH8 and may be attributed to several pathomechanisms, as discussed below.
3.1.1. ICP-monitoring, thresholds, and treatments
During ictus, there is a rapid increase in ICP following the hemorrhage from the ruptured intracranial aneurysm. Thereafter, secondary ICP elevations may occur in both an acute (<24 h) and delayed (2–14 days post-ictus) fashion due to e.g. re-bleeding, acute hydrocephalus, intracerebral hemorraghe, subdural hematomas, diffuse global cerebral edema, and cerebral edema.17 High ICP may in turn induce compression of neural structures as well as lead to macro- and microvascular CBF disturbances by lowering CPP and inducing capillary collapse.18
In an aSAH cohort study of patients with EVD-monitoring due to unconsciousness or hydrocephalus, ICP elevations were found to be very common. Around 80% of the patients exhibited at least one episode of ICP above 20 mmHg for more than 5 min.19 Still, the role of ICP monitoring, the definition of elevated ICP, and protocols for when ICP-lowering treatments are warranted remain controversial. Currently, the Neurocritical Care Society (NCC) has no recommendation on ICP-monitoring or ICP-lowering treatments,4 whereas the American Heart Association (AHA) suggests cerebrospinal fluid (CSF) drainage with an EVD or a lumbar drainage in case of acute hydrocephalus,3 but the role of ICP-monitoring, per se, and ICP-lowering treatments are not stated. Due to the lack of recommendations from aSAH guidelines, most centers, including ours, have extrapolated the ICP-regime from TBI protocols.5,11,20
When the original ICP protocols are transferred from TBI there are some important aSAH-related issues that need to be considered. First, regarding indication, ICP-monitoring is chiefly considered in TBI patiens with Glasgow coma scale score ≤8. In aSAH patients, ICP-monitoring is applied more liberally also in less unconscious patients since ICP may be increased due to CSF disturbances also before ventricular dilatation appears. CSF treatment may even be used in drowsy but conscious aSAH patients in case of symptomatic acute hydrocephalus. Second, regarding ICP monitors, the EVD, with the possibility to drain CSF, is consistently used in aSAH, since CSF disturbances and acute hydrocephalus are such prominent etiologies for ICP elevations. Third, the ICP-thresholds that warrant treatment are not as investigated in aSAH as in TBI. There are some studies that have demonstrated that aSAH patients with longer monitoring episodes of ICP above 20–25 mmHg exhibit an increased risk of clinical deterioration,5 worse cerebral energy metabolism,12 unfavorable outcome,6,21 and mortality.19 These thresholds would be in accordance with those established in TBI.11,22 Fourth, regarding ICP-lowering treatments, aSAH patients may benefit much more from CSF-drainage with an EVD than in TBI, considering that the dominating reason for increased ICP is CSF disturbances and acute hydrocephalus. Hyperventilation is used in TBI to lower ICP by cerebral vasoconstriction,23 which may be more dangerous in aSAH due to the high incidence of concurrent vasospasm (see 3.1.2). Barbiturates and decompressive craniectomy (DC) are occasionally last-tier life-saving treatments in aSAH, but there is no clear evidence if they improve clinical outcome in aSAH.17,24,25 Both barbiturates and DC have more established roles as last-tier ICP-treatments in TBI,11,26,27 although the role of DC has been challenged also in TBI.28,29 Lastly, in TBI, there are some studies that support the use of individualized ICP-thresholds, defined as the ICP-level when cerebral autoregulation becomes severely deranged,30,31 but this remains to be investigated in aSAH.
Altogether, despite that ICP-elevations are frequent and escalated treatments protocols are warranted, there is currently a lack of high-quality studies as well as guideline recommendations in this area for aSAH. There is some support that many aspects of the TBI protocols may be extrapolated to aSAH,12,21 but there are many pertinent disease-specific differences that need to be further elucidated regarding optimal ICP-treatment thresholds and optimal treatment options and their order of escalation. MMM tools may carry a role to determine when cerebral decompensation occurs due to high ICP and to evaluate successful effects of treatments, but the evidence to support this approach is very limited.
3.1.2. Carbon dioxide management: a balance between intracranial pressure and cerebral blood flow optimization
Several studies of aSAH support normo- and even hypercapnia in order to counteract ischemic CBF,32 increase brain tissue oxygenation,32 reduce DCI,33 and improve clinical outcome.33, 34, 35 However, the literature is not completely consistent, as others have rather found that mild hyperventilation (pCO2 4.0–5.1 kPa) may be the optimal balance to avoid last-tier ICP treatments, DCI, and poor outcome.36 Particularly, one fear with too generous hypercapnia is steal phenomemen, i.e. CBF augmentation only in pCO2-reactive brain regions that were already non-ischemic, while vasospastic and ischemic brain regions with lost pCO2-reactivity instead exhibit a CBF decrease.37 On balance, a pCO2 between 4.5 and 5.5 kPa may be an adequate balance among high ICP, low CBF, and the risk of steal. Radiological imaging such as xenon-enhanced computed tomography38, 39, 40 and MMM-tools including btO2/jugular bulb and microdialysis may be of value to better determine the cerebral net effects of therapy changes in pCO2-ventilation, although spatial constraints to focal brain regions may limit the sensitivity of btO2 or mircrodialysis to detect the any potential negative steal effect in distant, vulnerable brain regions.
3.1.3. ABP-,CPP-, and cerebral autoregeulation monitoring, thresholds, and treatments
ABP- and, in the aSAH cases with an EVD, CPP-monitoring are very important during NIC.41 In aSAH care, there is a biphasic approach to target ABP and CPP. Re-bleeding is a severe early complication and the highest risk is estimated to occur within the first 24 h post-ictus.42 Elevated ABP is thought to be an important risk factor for re-bleeding, although more aggressive ABP-lowering management has not shown any definite outcome benefit.43 Currently, AHA recommends avoiding systolic bood pressure (sBP) above 160 mmHg3 and NCC recommends that mean arterial blood pressure (MAP) above 110 mmHg should be avoided until aneurysm occlusion.4
After a successful aneurysm occlusion, the risk/benefit ratio of high ABP/CPP changes, since the re-bleeding risk is almost obviated, whereas there is a gradual increase in the risk of cerebral vasospasm, delayed cerebral ischemia (DCI), and brain infarctions during the following 10–14 days. Both AHA and the NCC recommend to maintain euvolemia to prevent cerebral ischemia and to induce arterial hypertension in case of DCI, but without any strict ABP-/CPP-threshold.3,4 Due to the lack of strict guideline recommendations in ABP-/CPP-targets,3,4 many centers extrapolate the CPP-targets from TBI protocols and keep the lower threshold target at 60 mmHg.5,11 However, current evidence support that much higher CPP-targets may be warranted in aSAH (Fig. 3). Findings from retrospective studies by our as well as other groups have demonstrated that CPP closer to 70–90 mmHg is associated with better brain tissue oxygenation,14 cerebreal energy metabolism,12,14 and favorable outcome6,21 in aSAH.
Fig. 3.
CPP in relation to clinical outcome in TBI and SAH.
The figure illustrates the combined effect of “insult” duration and intensity on clinical outcome.6 Red and blue color indicate unfavorable and favorable clinical outcome, respectively, in a subset of TBI (n = 441) and aSAH (n = 449) patients treated at our center. The patients were managed with similar treatment targets (CPP ≥60 mmHg) and the graphs illustrate that aSAH patients may benefit from much higher CPP-targets than TBI patients.
aSAH = aneurysmal subarachnoid hemorrhage. CPP = Cerebral perfusion pressure. TBI = Traumatic brain injury.
However, the role of fixed CPP-targets for all patients has also been questioned, due to differences in cerebral autoregulation between patients and throughout the temporal course in the acute phase (Fig. 4). For example, many aSAH patients exhibit co-morbidities such as chronic arterial hypertension, leading to a chronic right-shifted autregulation curve. This means that the lower and upper limit of autoregulation are pushed towards higher baseline ABP-/CPP-values, predisposing for greater susceptibility for cerebral ischemia at ABP-/CPP-values that healthier patients would tolerate.44 Additionally, aSAH patients exhibit various degrees of cerebral vasopasm thoughout the vascular tree, which may also vary over time in the acute phase. The importance of an individual and temporally dynamic cerebral pressure autoregulatory status has encouraged the development of MMM tools to assess this function, including pressure reactivity index (PRx), mean flow index (Mx), and oxygen reactivity index (ORx).44 Particularly, when PRx is plotted against CPP, an autoregulation curve with the optimal plateau phase of stable CBF can oftentimes be estimated (denoted as CPPopt). CPPopt as a treatment target has shown promising results in TBI studies,45 in which CPP close to CPPopt has been associated with optimal btO2,46 cerebral energy metabolism,47 and clinical outcome.47, 48, 49, 50, 51 However, the evidence to support CPPopt in aSAH is less clear. Some studies have found that CPP below CPPopt is associated with lower CBF8,52 and precedes DCI,53 whereas CPP above CPPopt seems to provoke hyperemia and seizures,54 but it does not correlate with cerebral energy metabolism12 or unfavorable outcome.21
Fig. 4.
A–B. Key concepts in cerebral pressure autoregulation and autoregulatory-oriented therapy.
Fig. 4A illustrates four examples of different cerebral pressure autoregulatory status. The blue curve shows the classic “Lassen curve” with a plateau of stable CBF over a broad range of CPPs. Cerebral ischemia occurs at the lower end of autoregulation when the cerebral vessels are already maximally dilated and then become pressure passive below this CPP-value. Similarly, cerebral hyperemia occurs as CPP surpasses the upper end of the autoregulatory plateau, when the capacity for further cerebral vasoconstriction is exceeded, and CBF again follows CPP passively. The yellow curve shows a right-shifted curve with preserved plateau range, which could be the case for patients with pre-ictal chronic arterial hypertension. The green curve illustrates a case with right-shifted and narrowed plateau, which may occur with cerebral vasospasm with increased vasoconstriction and reduced capacity for vasodilation. Hence, both the yellow and green curves illustrate two cases with increased susceptibility for cerebral ischemia despite “normal” CPP. The red curve illustrates a case with totally lost capacity to autoregulate, where CBF completely depends on CPP. Fig. 4B illustrates how the capacity for cerebral pressure autoregulation curve may be continuously monitored with PRx plotted against CPP for the last 4 h, in order to detect CPPopt. CPPopt reflects the plateau phase of CBF, i.e. the nadir of the U-shaped PRx/CPP curve. However, in cases with lost capacity to autoregulate, e.g. with high PRx and without the U-shaped curve, CPPopt cannot be detected.
CBF = Cerebral blood flow, CPP = Cerebral perfusion pressure, CPPopt = Optimal CPP, PRx = Pressure reactivity index.
Altogether, several retrospective studies support that aSAH patients may benefit from much higher CPP-targets closer to 70–90 mmHg, but there is a need for prospective studies to validate this and determine the best methods to reach these targets, e.g. ABP augmentation by fluids and vasopressors and/or different methods of ICP-lowering. There are preliminary reports of individualized autoregulatory CPP-targets, but their role in aSAH remains to be determined.
3.2. Oxygenation – arterial content, cerebral delivery, and cerebral tissue oxygenation
Previous sections have focused on CBF and this section will discuss the variables responsible for the arterial oxygen content (CaO2), with the ultimate goal to optimize CDO2. The hemoglobin (HgB) level is the main contributing factor for CaO2 in case of near maximal oxygen saturation (SaO2), whereas the freely dissolved oxygen only make up a small proportion of the CaO2. Anemia therefore drastically reduces CDO2. At the same time, hemodilution is one of the components in HHH-therapy to improve blood rheology and increase CBF,8 although the net benefit on CDO2 could be questioned.8 The definition of anemia and the threshold for red blood cell transfusion (RBCT) during NIC, the net cerebral effects of hemodilution, and the role of arterial hyperoxia have received great interest in acute brain injuries in general as well as in aSAH, as discussed below.
3.2.1. The role of hemoglobin
Regarding the definition of significant anemia in aSAH, several retrospective studies demonstrate an increased risk of developing brain tissue hypoxia,55,56 cerebral energy metabolic disturbances,55,56 and poor neurological outcome57 when HgB falls below 9–10 g/dL. However, general management to avoid and when to treat anemia remains controversial. NCC recommends at first hand to minimize all necessary blood loss (e.g. from lab tests) and at second hand to give RBCT to keep HgB above 8–10 g/dL and that patients with DCI might benefit from even higher levels.4 AHA is more vague and states that RBCT may be beneficial for aSAH patients at risk of cerebral ischemia, although any threshold for treatment is not defined.3 Hence, the most crucial question has remained if and when aSAH patients benefit from RBCT. Similar to the anemia-threshold, RBCT seems to improve cerebral oxygenation and energy metabolism and clinical outcome when HgB has fallen below 9–10 g/dL,57,58 but not in all studies.59 One important concern has been if the potential improvement in cerebral oxygenation from RBCT, in effect, outweighs the treatment risks. The potential negative effects of RBCT are not fully understood, but may include a worsening in cerebral pressure autoregulation,60 increased inflammatory response, as well as cardiac and respiratory dysfunction.61,62 The risks of RBCT have led to explorations of “restricted” (HgB 7 g/dL) rather than “liberal” (10 g/dL) thresholds for RBCT, where the more restricted approach appears safe and even favorable at least in general ICU patients.63 However, it has been questioned if this is valid for aSAH since these patients exhibit a reduced reserve for any CBF and CDO2 deterioration, predisposing for a lower tolerance for low HgB-levels. Thus, MMM-tools could then be useful to determine when cerebral decompensation occurs and when higher HgB by means of RBCT could be warranted to individualize care. For example, RBCT might be beneficial for subnormal HgB with concurrent brain tissue hypoxia, but not in case of normal brain tissue oxygenation. Otherwise, as a solution to any potential negative effect of RBCT, other oxygen-carrying agents (e.g. SANGUINATE) have been suggested as treatments to improve cerebral oxygenation in aSAH.64
Interestingly, hemodilution, which is part of HHH-therapy, may seem contradictory to the RBCT-approach. The idea of hemodilution is CBF augmentation to improve CDO2, but it occurs at the expense of a lower CaO2, and from a mechanistic point of view it is not fully clear if the CBF augmentation occurs due to improved blood rheology or is a partial compensation to counteract an increased tissue hypoxia.65 Most aSAH studies have confirmed that hemodilution leads to higher CBF, but that it does not translate into any CDO2 improvement.8,66 Consequently, hemodilution does not benefit cerebral oxygenation, but there are perhaps other advantages of the CBF augmentation.67 Specifically, higher CBF may increase CDGlc and in theory also clearance of cerebral waste products.
To conclude, controversy remains regarding how to optimize CaO2 in aSAH. Both RBCT and hemodilution remain two apparanetly contradictory treatment approaches for DCI. However, in theory, it may be that RBCT is beneficial in case of brain tissue hypoxia to improve CDO2, whereas the CBF augmentation may be more relevant when the predominant pathomechanism is mitochondrial dysfunction in order to drive anerobic energy metabolism. MMM-protocols could then be of value to further diagnose the cause of energy metabolic disturbance in order to individualize CBF- and CaO2-oritented treatments.
3.2.2. Arterial oxygenation
As already outlined, changes in the partial pressure of oxygen (pO2) has a great influence on CaO2 when the SaO2 is low, but not under normal settings with near full saturation. Otherwise, the effects of supranormal pO2 on the freely dissolved oxygen content is neglible for CaO2. Although NCC and AHA do not provide any guidelines for pO2,3,4 most centers aim for normoxia.5,35 There has also been an interest in normobaric hyperoxia as a way to compensate for cerebral ischemia and diffusion limitations to improve cerebral oxygenation and aerobic energy metabolism. In effect, increasing FiO2 to hyperoxic levels in order to treat low btO2 has shown promise in TBI,68,69 however hyperoxic pO2-levels may also exert adverse effects including cerebral vasoconstriction70,71 and induction of reactive oxygen species.72 In aSAH, the negative effects of hyperoxia seem to predominate, as hyperoxia has been associated with cerebral vasospasm,73 DCI,74,75 and unfavorable outcome.74, 75, 76 Altogether, normoxia around 12 kPa with near maximal oxygen saturation seems most beneficial. However, it remains to be determined if hyperoxia is only negative or may be beneficial in certain clinical states of e.g. diffusion limitations due to edema or to overcome mitochondrial dysfunction, based on MMM-analysis.
3.3. Cerebral delivery of nutrients
The content of the arterial nutrients glucose and lactate together with CBF determine the CDGlc and CDLac. In this section, optimization of the arterial content of glucose and lactate are discussed in detail.
3.3.1. Arterial glucose thresholds and management
The arterial glucose content is under normal conditions regulated within a narrow interval, but aSAH typically induces an acute and often persistent elevation in arterial glucose post-ictus due to activation of the hypothalamic-pituitary-adrenal (HPA)-axis, hypothalamic damage/dysfunction, and systemic inflammation.35,77, 78, 79 Stress-induced hyperglycemia may compensate for eventual low CBF in order to attenuate neuroglucpoenia, but hyperglycemia may also exert several negative systemic and cerebral effects. Particularly, hyperglycemia increases the risk of systemic complications including infections, disturbed wound healing, and respiratory dysfunction.77,80,81 In addition, hyperglycemia is associated with disturbed cerebral energy metabolism82 and development of DCI,82, 83, 84 possibly due to more vasospasm, microvascular thrombi, increased systemic inflammation, and excacerbated reperfusion injury.77 Several studies have also established an association between hyperglycemia and unfavorable clinical outcome in aSAH.35,79,82,83 Consequently, optimizing arterial glucose is of great importance and this subject has received much interest and also led to great controversy both in general intensive care unit populations80,81 as well as after acute brain injury85, 86, 87, 88 including aSAH.89,90 Specifically, intensive insulin therapy (IIT) to keep arterial glucose within a tight interval (e.g. 4.4–6.1 mM) leads to a significant reduction in mean arterial glucose-levels, but also increases the incidence of hypoglycemia.90 Patients with aSAH are very vulnerable to hypoglycemia and the gain in avoiding hyperglycemia is likely off-set by the corresponding increase in hypoglycemic events from IIT.90 Systemic continuous glucose monitoring could facilitate IIT by earlier detection of imminent hypoglycemia, but the reliability of these continuous monitors has been questioned.91 In addition, as a way to individualize care, it has been suggested to guide arterial glucose management based on microdialysis monitoring of cerebral glucose, e.g. by administration of intravenous glucose infusion in cases of low MD-glucose.92 However, this has not been sufficiently studied to implement in clinical practice.
Currently, a more loose and less intense arterial glucose management is generally favored, as NCC recommends to keep it between 4.4 and 11.1 mM and possibly to adjust this based on low microdialysis-levels,4 whereas AHA generally recommends avoiding hypoglycemia.3 A combination of a more reliable technique to continuously measure systemic glucose combined with cerebral microdialysis-glucose monitoring could perhaps further refine arterial glucose management.
3.3.2. Arterial lactate
The role of lactate as a cerebral fuel has gradually gained acceptance and interest. Lactate is transported via monocarboxylate transporters into endothelial cells and astrocytes via MCAT1 and into neurons via MCAT2.93 In the astrocyte-neuron-lactate-shuttle (ANLS), astrocytes metabolize glucose into lactate, which is shuttled to neurons and is there used for oxidative phosphorylation.93, 94, 95, 96, 97 Under normal conditions, the arterial contribution to cerebral lactate is low around 10%, but increases to 60% at 5 mM.98 However, the cerebral lactate uptake can be upregulated following acute brain injury.97 As the cerebral lactate increases, more is used as cerebral energy fuel, which spares glucose.95,99,100 Still, the use of exogenous lactate as a supplementary cerebral energy fuel remains exploratory at the moment. However, it is worth mentioning that lactate solutions may exert additional cerebral effects. High arterial lactate may induce cerebral vasodilation and augment CBF,99,101 although possibly at the expense of a worse pressure autoregulation.35,102 Furthermore, lactate in hypertonic solutions may be beneficial to reduce brain edema and thereby reduce ICP.95 Altogether, further MMM studies are needed to better determine the role of exogenous lactate infusions on cerebral physiology.
3.4. Cerebral energy metabolism
CaO2, CaGlc, CaLac, and CBF are important variables to optimize the cerebral energy metabolic supply for neuronal survival. However, there are several additional variables that interfere with the capacity to generate energy as well as the requirements of energy metabolic turnover, as described below.
3.4.1. Hypo- and hyperthermia – temperature management
The body has under normal conditions a tightly regulated set-temperature around 37 °C. There is controversy over the exact definitions of hypo-, normo-, and hyperthermia in the literature, however, T < 36 °C, 36 °C ≤ T ≤ 38, and T > 38 °C would be one example applied by our institution.21,103 In addition, systemic and brain temperature are usually highly correlated, but brain temperature may be up to 1–2 °C higher following acute brain injury,104 secondary to elevated heat production from increased energy metabolism.
The natural course of body temperature follows a biphasic pattern after aSAH. Particularly in poor-grade cases with transient global ischemia, body temperature initially falls, possibly as a neuroprotective mechanism, the first hours and then hyperthermia usually gradually develops.105 Major drivers of hyperthermia are infectious complications during NIC and neurogenic mechanisms. Neurogenic fever is common in poor-grade cases with a greater burden of SAH and IVH106 and the underlying explanation is a change in temperature set point due to toxic and inflammatory effects of the SAH/IVH and/or ischemic complications in the brainstem and hypothalamus.107
Several previous studies demonstrate an association between hyperthermia and negative outcomes in aSAH, including worse cerebral energy metabolism,108 development of DCI,106,109 and poor neurological recovery.21,106,109,110 One explanation is that hyperthermia, per se, induces negative cerebral effects including increased cerebral energy metabolism, cerebral hyperemia, blood–brain-barrier disruption and cerebral edema, intracranial hypertension, and excitotoxicity.111 However, the direction of the association between hyperthermia and poor aSAH outcomes is not always clear and hyperthermia is to a great extent also an epiphenomenon of a worse primary and secondary brain injury. Current guidelines recommend avoiding hyperthermia, although the treatment threshold and therapeutic approaches remain largely varied among guidelines and centers. AHA provides a recommendation to avoid hyperthermia in general by using standard treatments, without any further specifications.3 NCC recommends avoiding hyperthermia (without any strict threshold), particularly in the vasospasm phase, by using acetaminophen and NSAIDs at first hand and surface cooling and intravascular devices at second hand, while avoiding shivering.4 The level of evidence for these treatments is low. Specifically, among the pharmacological agents, NSAIDs may reduce fever, but could simultaneously induce cerebral vasoconstriction, and worsen CPP and btO2, predisposing for negative net effects on the brain, in addition to risks of systemic complications (kidney injury).112 Among the various cooling techniques, intravascular cooling shows some promise at least in TBI, as initiation of cooling improves cerebral energy metabolism.113 A major concern with this approach is the risk of inflicting stress and shivering, which may rather worsen cerebral physiology.114 Furthermore, therapeutic hypothermia has received great interest as a potential neuroprotective treatment in acute brain injuries, however, so far, any true benefit on outcome remains unclear in general as well as in aSAH. Specifically, in aSAH, therapeutic hypothermia has been mostly studied as an intraoperative neuroprotective adjunct during surgery for ruptured intracranial aneurysms, which was shown to be safe, but did not improve neurological outcomes.115,116 AHA does currently not recommend it on a general basis, but holds it as an option.3 Otherwise therapeutic hypothermia has been used to treat DCI117 and elevated ICP118 in case series, but without any conclusive evidence for its use. Similarly, although therapeutic hypothermia initially seemed promising in TBI,119 recent studies have shown that hypothermia neither improves outcome if used to reduce intracranial hypertension prophylactically120 or therapeutically.121 Similarly, after cardiac arrest, initial studies found promising neurological results with therapeutic hypothermia,122 whereas more recent studies indicate that this treatment does not improve functional outcomes.123
Altogether, hyperthermia is common during the late acute phase of aSAH and is associated with negative outcomes, but the causality remains obscure. Currently, hyperthermia is chiefly treated on a symptomatic physiological basis. Particularly in non-infectious, neurogenic hyperthermia, the underlying mechanism is not addressed. It is possible that more granular studies based on protein biomarkers from CSF-/MD-samples9,10 may provide a better understanding of underlying processes such as neuroinflammation and may provide a mechanistic basis for future treatments.
3.4.2. Seizures and cortical spreading depolarizations
Epileptic activity is common following acute brain injures in general as well as after aSAH. This may manifest as focal or generalized convulsive and non-convulsive seizures. Seizures occasionally occur immediately after ictus or re-bleeding and in case of cerebral ischemia and brain herniation.124 Convulsive seizures are typically easy to identify, whereas non-convulsive seizures are rather detected with electroencephalography (EEG) in patients in a poor neurological condition without any other clear explanation.125 The rate of seizures based on clinical criteria has been estimated to occur in between 4 and 26% of the cases,124 whereas the rate of epileptic activity may be much higher as evaluated with EEG and in particular with the more sensitive method electrocorticography.126 Seizures may increase ICP and energy metabolic turnover leading to neuronal cell death.127 Both AHA and NCC state that short-term seizure prophylaxis may be considered in the acute phase,3,4 although NCC points out that phenytoin has been associated with worsened long-term outcome and should be avoided.4 NCC also suggests the use of continuous EEG to assess for non-convulsive seizures in patients who fail to improve.4
A distinct, but akin neuroelectric phenomenom is cortical spreading depolarization (CSD), characterized by a moving gradient of cortical membrane depolarization with subsequent electrical depression and associated CBF disturbances (inverse neurovascular coupling).127, 128, 129 This may ultimately result in disturbed cerebral energy metabolism and cell death. There are currently no specific treatments for CSD, but it has generally been suggested beneficial to optimize systemic and cerebral physiology. Furthermore, glutamate seems to be a major contributor to CSD and various pharmacological agents targeting glutamate synthesis and receptor-antagonists have also been suggested.127
In conclusion, this is an emerging areas of NIC, studies of CSD, and the role of the newer generation of antiepileptic agents with better tolerance profiles are much warranted.
3.4.3. Mitochondrial dysfunction
Energy is produced via anaerobic glycolysis and aerobic oxidative phosphorylation, in which the former only generates a small proportion of the total energy production. Functioning mitochondrias are therefore key for energy production. In recent years, the understanding of mitochondrial dysfunction as a pathophysiological mechanism in acute brain injuries including aSAH has gained increased understanding and interest.67,130,131 Microdialysis studies indicate that mitochondrial dysfunction is common after aSAH67,132 and is associated with poor clinical outcome.133 It has been speculated if arterial hyperoxia could improve oxidative aerobic energy metabolism in the mitochondria.134 Pharmacological agents such as cyclosporin have been tried as potential neuroprotective agents to ameliorate this pathological energy metabolic state in TBI studies,135 but there are otherwise no current available therapies during NIC. This is also an emerging field that needs better understanding and therapeutic agents.
4. Cellular and molecular injury processes and the role of neuroprotective agents
Cerebral physiology as well as cellular and molecular injury patterns compromise a very complex area that currently remains insufficiently understood. There have been several attempts to develop and implement neuroprotective agents in aSAH, but with limit success, similar to the case in severe TBI. Some explanations for the disappointing results may be animal/patient heterogeneity and differences in therapeutic windows between animal models and human trials. A deeper understanding of the cellular and molecular injury patterns together with MMM-tools to monitor these processes bedside could potentially solve this problem, as discussed below.
4.1. Neuroprotective agents
There are a number of clinical trials that have evaluated different pharmacological agents to address various aspects of aSAH pathophysiology.136 First, nimodipine is a calcium-channel blocker, which reduces DCI and improves outcome, and is the only neuroprotective agent that is integrated in current management guidelines.3,4,137 The mechanism of action was initially thought to counteract cerebral vasospasm, which proved not to be the case,137 and other important but less understood mechanisms may be more important. Second, endothelin-receptor antagonists have proven to counteract cerebral vasospasm, but without any benefit on clinical outcome, possibly as a consequence of associated adverse effects such as anemia, arterial hypotension, and respiratory failure.138 Third, other agents with a potential beneficial effect on cerebral vasospasm and DCI include statins139,140 and magnesium sulphate,141 which, so far, are promising but need further validation.3,4 Fourth, mitochondrial dysfunction is common after aSAH67 and as outlined above, cyclosporin has been used to treat this condition in TBI,135 but it remains to be tested in aSAH. Fifth, there are several emerging agents such as cilostazol that may exert broad-spectrum beneficial neuroprotective effects that need to be further explored in future randomized controlled trials.140 Sixth, although tranexamic acid is not directly neuroprotective, it could be viewed as that in one sense, since administration after ictus until aneurysm occlusion may reduce the rate of re-bleedings and thereby secondary brain injury. However, concerns have also been raised regarding increased risk of thromboembolic complications with this treatment136,142,143 and with modern management including early aneurysm occlusion it does not seem to add any benefit on long-term outcome.142
4.2. Online bedside monitoring of molecular injury patterns – the next step in precision medicine?
The development of large-pore microdialysis catheters has paved the way to monitor and analyze complex molecular cascades in the interstitial tissue of the brain bedside.144, 145, 146, 147, 148 Together with the newly developed technique proximity extension assay (PEA),9,10,149 which is a very sensitive tool to detect small quantities of protein while using only small volumes of fluid, it is now also possible to efficaciously detect and study numerous brain protein biomarkers from patients with acute brain injury such as TBI and aSAH.150, 151, 152 This may enable a deeper understanding of ongoing pathophysiological processes and refine indications and time windows of treatments for neuroprotective pharmacological agents. However, due to the complexity of these data, there will most likely be a need to analyze the dynamics of these biomarkers with artificial intelligence to understand their complex patterns, in future NIC units.
5. Concluding remarks
Although the level of evidence in aSAH management in general is poor, we do know several ways to improve outcome, such as early aneurysm occlusion to prevent re-bleeding, CSF drainage in case of increased ICP and/or acute hydrocehpauls, and CBF augmentation in case of DCI. In addition, NIC with the aim to avoid secondary insults has succefully improved clinical outcome after aSAH. However, as outlined in this review, it has been very challenging to prove which specific NIC targets and treatments that are most optimal. This is not surprising, considering the challenges in conducting research in such a severe disease as aSAH which is often associated with a heterogeneous and complex NIC course. Most likely, CPP above 60 mmHg, ICP below 20 mmHg, and oxygen saturation above 95% are good rough estimates to optimize cerebral physiology, but we argue that NIC management could be further fine tuned. Below, we highlight four future perspectives, escalated from what hopefully lies just next-door (short-term) to what may be discerned a bit farer away on the horizon (long-term).
-
i)
NIC management of aSAH is currently to a large degree extrapolated from TBI care. However, we need to proceed with basic aSAH-specific prospective studies on high-frequency data analyses of ICP, CPP, Hgb, and body temperature etc. to better understand general, “epidemiological (for all patients)” pathophysiology and treatment effects in this disease.
-
ii)
The approach above is still limited to the one-size-fits-all concept and the next step is to individualized care. This can be done by integrating more systemic and cerebral physiology from MMM-tools into NIC management, such as autoregulatory-oriented therapy with CPPopt.
-
iii)
The major challenges of implementing MMM tools in management are their limitations regarding reliability and validity. We need to proceed to study cerebral physiology in relation to these inherent limitations of MMM tools and proceed with methodological innovation. Artificial intelligence may prove to be beneficial in this attempt.
-
iv)
A major step towards MMM development and individualized treatments is to go from the physiological to the cellular and molecular level of cerebral injury mechanisms. Large-pore cerebral microdialysis with bedside online measurements of biomarkers related to neuroinflammation, neurodegeneration, and neurorepair may be one solution in this direction. Specifically, this may be of great importance in order to optimize the indication and time window for future neuroprotective pharmacological agents.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgement
The study was supported by the Department of Medical sciences, Uppsala University.
Abbreviatipons
- ABP =
Arterial blood pressure
- AHA =
American Heart Association
- ANLS =
Astrocyte-neuron-lactate-shuttle
- aSAH =
Aneurysmal SAH
- BtO2 =
Brain tissue oxygenation
- CaO2 =
Arterial oxygen content
- CBF =
Cerebral blood flow
- CDGlc =
Cerebral delivery of glucose
- CDLac =
Cerebral delivery of lactate
- CDO2 =
Cerebral delivery of oxygen
- CPP =
Cerebral perfusion pressure
- CPPopt =
The optimal CPP, i.e. with the most optimal autoregulatory status (lowest PRx)
- CSD =
Cortical spreading depolarization
- CSF =
Cerebrospinal fluid
- DC =
Decompressive craniectomy
- DCI =
Delayed cerebral ischemia
- EEG =
Electroencephalography
- EVD =
External ventricular drainage
- Hgb =
Hemoglobin
- HHH =
Hypervolemia, hemodilution, and hypertension
- HPA =
Hypothalamic-pituitary-adrenal
- ICH =
Intracerebral hemorrhage
- ICP =
Intracranial pressure
- IIT =
Intensive insulin therapy
- IMPACT =
International mission for prognosis and analysis of clinical trials in TBI
- IVH =
Intraventricular hemorrhage
- MMM =
Multimodality monitoring
- NCC =
Neurocritical Care Society
- NIC =
Neurointensive care
- NSAID =
Non-steroidal anti-inflammatory drugs
- PEA =
Proximity extension assay
- PRx =
Pressure reactivity index
- RBCT =
Red blood cell transfusion
- SAH =
Subarachnoid hemorrhage
- SaO2 =
Arterial oxygen saturation
- sBP =
Systolic blood pressure
- TBI =
Traumatic brain injury
References
- 1.Svedung Wettervik T.M., Lewén A., Enblad P. Fine tuning of traumatic brain injury management in neurointensive care-indicative observations and future perspectives. Front Neurol. 2021;12 doi: 10.3389/fneur.2021.638132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cesarini K.G., Hårdemark H.G., Persson L. Improved survival after aneurysmal subarachnoid hemorrhage: review of case management during a 12-year period. J Neurosurg. 1999;90(4):664–672. doi: 10.3171/jns.1999.90.4.0664. [DOI] [PubMed] [Google Scholar]
- 3.Connolly E.S., Jr., Rabinstein A.A., Carhuapoma J.R., et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. 2012;43(6):1711–1737. doi: 10.1161/STR.0b013e3182587839. [DOI] [PubMed] [Google Scholar]
- 4.Diringer M.N., Bleck T.P., Claude Hemphill J., 3rd, et al. Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the Neurocritical Care Society's Multidisciplinary Consensus Conference. Neurocritical Care. 2011;15(2):211–240. doi: 10.1007/s12028-011-9605-9. [DOI] [PubMed] [Google Scholar]
- 5.Ryttlefors M., Howells T., Nilsson P., et al. Secondary insults in subarachnoid hemorrhage: occurrence and impact on outcome and clinical deterioration. Neurosurgery. 2007;61(4):704–714. doi: 10.1227/01.Neu.0000298898.38979.E3. ; discussion 714-5. [DOI] [PubMed] [Google Scholar]
- 6.Wettervik T.S., Hånell A., Howells T., et al. ICP, CPP, and PRx in traumatic brain injury and aneurysmal subarachnoid hemorrhage: association of insult intensity and duration with clinical outcome. J Neurosurg. 2022;1(aop):1–8. doi: 10.3171/2022.5.JNS22560. [DOI] [PubMed] [Google Scholar]
- 7.Svedung Wettervik T., Engquist H., Hånell A., et al. Cerebral microdialysis monitoring of energy metabolism: relation to cerebral blood flow and oxygen delivery in aneurysmal subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2022 doi: 10.1097/ana.0000000000000854. [DOI] [PubMed] [Google Scholar]
- 8.Svedung Wettervik T., Engquist H., Hånell A., et al. Cerebral blood flow and oxygen delivery in aneurysmal subarachnoid hemorrhage: relation to neurointensive care targets. Neurocritical Care. 2022 doi: 10.1007/s12028-022-01496-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dyhrfort P., Shen Q., Clausen F., et al. Monitoring of protein biomarkers of inflammation in human traumatic brain injury using microdialysis and proximity extension assay technology in neurointensive care. J Neurotrauma. 2019 doi: 10.1089/neu.2018.6320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vlachogiannis P., Hillered L., Enblad P., et al. Temporal patterns of inflammation-related proteins measured in the cerebrospinal fluid of patients with aneurysmal subarachnoid hemorrhage using multiplex Proximity Extension Assay technology. PLoS One. 2022;17(3) doi: 10.1371/journal.pone.0263460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carney N., Totten A.M., O'Reilly C., et al. Guidelines for the management of severe traumatic brain injury, Fourth edition. Neurosurgery. 2017;80(1):6–15. doi: 10.1227/neu.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 12.Svedung Wettervik T., Hånell A., Howells T., et al. Intracranial pressure- and cerebral perfusion pressure threshold-insults in relation to cerebral energy metabolism in aneurysmal subarachnoid hemorrhage. Acta Neurochir. 2022 doi: 10.1007/s00701-022-05169-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen H.I., Stiefel M.F., Oddo M., et al. Detection of cerebral compromise with multimodality monitoring in patients with subarachnoid hemorrhage. Neurosurgery. 2011;69(1):53–63. doi: 10.1227/NEU.0b013e3182191451. ; discussion 63. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt J.M., Ko S.B., Helbok R., et al. Cerebral perfusion pressure thresholds for brain tissue hypoxia and metabolic crisis after poor-grade subarachnoid hemorrhage. Stroke. 2011;42(5):1351–1356. doi: 10.1161/strokeaha.110.596874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Winberg J., Holm I., Cederberg D., et al. Cerebral microdialysis-based interventions targeting delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Neurocritical Care. 2022;37(1):255–266. doi: 10.1007/s12028-022-01492-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bohman L.E., Pisapia J.M., Sanborn M.R., et al. Response of brain oxygen to therapy correlates with long-term outcome after subarachnoid hemorrhage. Neurocritical Care. 2013;19(3):320–328. doi: 10.1007/s12028-013-9890-6. [DOI] [PubMed] [Google Scholar]
- 17.Alotaibi N.M., Wang J.Z., Pasarikovski C.R., et al. Management of raised intracranial pressure in aneurysmal subarachnoid hemorrhage: time for a consensus? Neurosurg Focus. 2017;43(5):E13. doi: 10.3171/2017.7.Focus17426. [DOI] [PubMed] [Google Scholar]
- 18.Bordoni L., Li B., Kura S., et al. Quantification of capillary perfusion in an animal model of acute intracranial hypertension. J Neurotrauma. 2021;38(4):446–454. doi: 10.1089/neu.2019.6901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zoerle T., Lombardo A., Colombo A., et al. Intracranial pressure after subarachnoid hemorrhage. Crit Care Med. 2015;43(1):168–176. doi: 10.1097/ccm.0000000000000670. [DOI] [PubMed] [Google Scholar]
- 20.Elf K., Nilsson P., Enblad P. Outcome after traumatic brain injury improved by an organized secondary insult program and standardized neurointensive care. Crit Care Med. 2002;30(9):2129–2134. doi: 10.1097/01.Ccm.0000025893.73582.52. [DOI] [PubMed] [Google Scholar]
- 21.Svedung Wettervik T., Howells T., Lewén A., et al. Temporal dynamics of ICP, CPP, PRx, and CPPopt in high-grade aneurysmal subarachnoid hemorrhage and the relation to clinical outcome. Neurocritical Care. 2021 doi: 10.1007/s12028-020-01162-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sorrentino E., Diedler J., Kasprowicz M., et al. Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocritical Care. 2012;16(2):258–266. doi: 10.1007/s12028-011-9630-8. [DOI] [PubMed] [Google Scholar]
- 23.Svedung Wettervik T., Howells T., Hillered L., et al. Mild hyperventilation in traumatic brain injury-relation to cerebral energy metabolism, pressure autoregulation, and clinical outcome. World neurosurgery. 2020;133:e567–e575. doi: 10.1016/j.wneu.2019.09.099. [DOI] [PubMed] [Google Scholar]
- 24.Alotaibi N.M., Elkarim G.A., Samuel N., et al. Effects of decompressive craniectomy on functional outcomes and death in poor-grade aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Neurosurg. 2017;127(6):1315–1325. doi: 10.3171/2016.9.Jns161383. [DOI] [PubMed] [Google Scholar]
- 25.Veldeman M., Weiss M., Daleiden L., et al. Decompressive hemicraniectomy after aneurysmal subarachnoid hemorrhage-justifiable in light of long-term outcome? Acta Neurochir. 2022 doi: 10.1007/s00701-022-05250-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wettervik T.S., Lenell S., Nyholm L., et al. Decompressive craniectomy in traumatic brain injury: usage and clinical outcome in a single centre. Acta Neurochir. 2018;160(2):229–237. doi: 10.1007/s00701-017-3418-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kolias A.G., Adams H., Timofeev I.S., et al. Evaluation of outcomes among patients with traumatic intracranial hypertension treated with decompressive craniectomy vs standard medical care at 24 Months: a secondary analysis of the RESCUEicp randomized clinical trial. JAMA Neurol. 2022 doi: 10.1001/jamaneurol.2022.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooper D.J., Rosenfeld J.V., Murray L., et al. Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med. 2011;364(16):1493–1502. doi: 10.1056/NEJMoa1102077. [DOI] [PubMed] [Google Scholar]
- 29.Hutchinson P.J., Kolias A.G., Timofeev I.S., et al. Trial of decompressive craniectomy for traumatic intracranial hypertension. N Engl J Med. 2016;375(12):1119–1130. doi: 10.1056/NEJMoa1605215. [DOI] [PubMed] [Google Scholar]
- 30.Lazaridis C., DeSantis S.M., Smielewski P., et al. Patient-specific thresholds of intracranial pressure in severe traumatic brain injury. J Neurosurg. 2014;120(4):893–900. doi: 10.3171/2014.1.Jns131292. [DOI] [PubMed] [Google Scholar]
- 31.Zeiler F.A., Ercole A., Cabeleira M., et al. Patient-specific ICP epidemiologic thresholds in adult traumatic brain injury: a CENTER-TBI validation study. J Neurosurg Anesthesiol. 2021;33(1):28–38. doi: 10.1097/ana.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 32.Westermaier T., Stetter C., Kunze E., et al. Controlled hypercapnia enhances cerebral blood flow and brain tissue oxygenation after aneurysmal subarachnoid hemorrhage: results of a phase 1 study. Neurocritical Care. 2016;25(2):205–214. doi: 10.1007/s12028-016-0246-x. [DOI] [PubMed] [Google Scholar]
- 33.Solaiman O., Singh J.M. Hypocapnia in aneurysmal subarachnoid hemorrhage: incidence and association with poor clinical outcomes. J Neurosurg Anesthesiol. 2013;25(3):254–261. doi: 10.1097/ANA.0b013e3182806465. [DOI] [PubMed] [Google Scholar]
- 34.Lång M., Raj R., Skrifvars M.B., et al. Early moderate hyperoxemia does not predict outcome after aneurysmal subarachnoid hemorrhage. Neurosurgery. 2016;78(4):540–545. doi: 10.1227/neu.0000000000001111. [DOI] [PubMed] [Google Scholar]
- 35.Svedung Wettervik T., Hånell A., Howells T., et al. Association of arterial metabolic content with cerebral blood flow regulation and cerebral energy metabolism-A multimodality analysis in aneurysmal subarachnoid hemorrhage. J Intensive Care Med. 2022 doi: 10.1177/08850666221080054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Darkwah Oppong M., Wrede K.H., Müller D., et al. PaCO2-management in the neuro-critical care of patients with subarachnoid hemorrhage. Sci Rep. 2021;11(1) doi: 10.1038/s41598-021-98462-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reiff T., Barthel O., Schönenberger S., et al. High-normal P(a)CO(2) values might be associated with worse outcome in patients with subarachnoid hemorrhage - a retrospective cohort study. BMC Neurol. 2020;20(1) doi: 10.1186/s12883-020-1603-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Engquist H., Lewén A., Hillered L., et al. CBF changes and cerebral energy metabolism during hypervolemia, hemodilution, and hypertension therapy in patients with poor-grade subarachnoid hemorrhage. J Neurosurg. 2021;134(2):555–564. doi: 10.3171/2019.11.Jns192759. [DOI] [PubMed] [Google Scholar]
- 39.Engquist H., Rostami E., Enblad P. Temporal dynamics of cerebral blood flow during the acute course of severe subarachnoid hemorrhage studied by bedside xenon-enhanced CT. Neurocritical Care. 2019;30(2):280–290. doi: 10.1007/s12028-019-00675-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Engquist H., Rostami E., Ronne-Engström E., et al. Effect of HHH-therapy on regional CBF after severe subarachnoid hemorrhage studied by bedside xenon-enhanced CT. Neurocritical Care. 2018;28(2):143–151. doi: 10.1007/s12028-017-0439-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Le Roux P., Menon D.K., Citerio G., et al. Consensus summary statement of the international multidisciplinary consensus conference on multimodality monitoring in neurocritical care. Neurocritical Care. 2014;21(2):1–26. doi: 10.1007/s00134-014-3369-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Larsen C.C., Sørensen B., Nielsen J.D., et al. Reduced clot-stability during the first 6 hours after aneurysmal subarachnoid haemorrhage--a prospective case-control study. Thromb Res. 2012;129(5):e229–e232. doi: 10.1016/j.thromres.2012.01.016. [DOI] [PubMed] [Google Scholar]
- 43.Calviere L., Gathier C.S., Rafiq M., et al. Rebleeding after aneurysmal subarachnoid hemorrhage in two centers using different blood pressure management strategies. Front Neurol. 2022;13 doi: 10.3389/fneur.2022.836268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wettervik T.S., Fahlström M., Enblad P., et al. Cerebral pressure autoregulation in brain injury and disorders - a review on monitoring, management, and future directions. World neurosurgery. 2021 doi: 10.1016/j.wneu.2021.11.027. [DOI] [PubMed] [Google Scholar]
- 45.Tas J., Beqiri E., van Kaam R.C., et al. Targeting autoregulation-guided cerebral perfusion pressure after traumatic brain injury (COGiTATE): a feasibility randomized controlled clinical trial. J Neurotrauma. 2021;38(20):2790–2800. doi: 10.1089/neu.2021.0197. [DOI] [PubMed] [Google Scholar]
- 46.Jaeger M., Dengl M., Meixensberger J., et al. Effects of cerebrovascular pressure reactivity-guided optimization of cerebral perfusion pressure on brain tissue oxygenation after traumatic brain injury. Crit Care Med. 2010;38(5):1343–1347. doi: 10.1097/CCM.0b013e3181d45530. [DOI] [PubMed] [Google Scholar]
- 47.Wettervik T.S., Howells T., Hillered L., et al. Autoregulatory or fixed cerebral perfusion pressure targets in traumatic brain injury: determining which is better in an energy metabolic perspective. J Neurotrauma. 2021 doi: 10.1089/neu.2020.7290. [DOI] [PubMed] [Google Scholar]
- 48.Svedung Wettervik T.M., Howells T., Enblad P., et al. Temporal neurophysiological dynamics in traumatic brain injury: role of pressure reactivity and optimal cerebral perfusion pressure for predicting outcome. J Neurotrauma. 2019;36(11):1818–1827. doi: 10.1089/neu.2018.6157. [DOI] [PubMed] [Google Scholar]
- 49.Aries M.J., Czosnyka M., Budohoski K.P., et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40(8):2456–2463. doi: 10.1097/CCM.0b013e3182514eb6. [DOI] [PubMed] [Google Scholar]
- 50.Steiner L.A., Czosnyka M., Piechnik S.K., et al. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med. 2002;30(4):733–738. doi: 10.1097/00003246-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 51.Svedung Wettervik T., Howells T., Lewén A., et al. Blood pressure variability and optimal cerebral perfusion pressure-new therapeutic targets in traumatic brain injury. Neurosurgery. 2020;86(3):E300–e309. doi: 10.1093/neuros/nyz515. [DOI] [PubMed] [Google Scholar]
- 52.Johnson U., Engquist H., Lewén A., et al. Increased risk of critical CBF levels in SAH patients with actual CPP below calculated optimal CPP. Acta Neurochir. 2017;159(6):1065–1071. doi: 10.1007/s00701-017-3139-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weiss M., Albanna W., Conzen C., et al. Optimal cerebral perfusion pressure during delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Crit Care Med. 2022;50(2):183–191. doi: 10.1097/ccm.0000000000005396. [DOI] [PubMed] [Google Scholar]
- 54.Alkhachroum A., Megjhani M., Terilli K., et al. Hyperemia in subarachnoid hemorrhage patients is associated with an increased risk of seizures. J Cerebr Blood Flow Metabol : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2020;40(6):1290–1299. doi: 10.1177/0271678x19863028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kurtz P., Schmidt J.M., Claassen J., et al. Anemia is associated with metabolic distress and brain tissue hypoxia after subarachnoid hemorrhage. Neurocritical Care. 2010;13(1):10–16. doi: 10.1007/s12028-010-9357-y. [DOI] [PubMed] [Google Scholar]
- 56.Oddo M., Milby A., Chen I., et al. Hemoglobin concentration and cerebral metabolism in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2009;40(4):1275–1281. doi: 10.1161/strokeaha.108.527911. [DOI] [PubMed] [Google Scholar]
- 57.Ayling O.G.S., Ibrahim G.M., Alotaibi N.M., et al. Anemia after aneurysmal subarachnoid hemorrhage is associated with poor outcome and death. Stroke. 2018;49(8):1859–1865. doi: 10.1161/strokeaha.117.020260. [DOI] [PubMed] [Google Scholar]
- 58.Dhar R., Zazulia A.R., Derdeyn C.P., et al. RBC transfusion improves cerebral oxygen delivery in subarachnoid hemorrhage. Crit Care Med. 2017;45(4):653–659. doi: 10.1097/ccm.0000000000002266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kramer A.H., Gurka M.J., Nathan B., et al. Complications associated with anemia and blood transfusion in patients with aneurysmal subarachnoid hemorrhage. Crit Care Med. 2008;36(7):2070–2075. doi: 10.1097/CCM.0b013e31817c1095. [DOI] [PubMed] [Google Scholar]
- 60.Sekhon M.S., Griesdale D.E., Czosnyka M., et al. The effect of red blood cell transfusion on cerebral autoregulation in patients with severe traumatic brain injury. Neurocritical Care. 2015;23(2):210–216. doi: 10.1007/s12028-015-0141-x. [DOI] [PubMed] [Google Scholar]
- 61.Clevenger B., Kelleher AJCEiA Critical Care, Pain. Hazards of blood transfusion in adults and children. Cont Educ Anaesth Crit Care Pain. 2014;14(3):112–118. doi: 10.1093/bjaceaccp/mkt042. [DOI] [Google Scholar]
- 62.Marik P.E. The risks of blood transfusion in patients with subarachnoid hemorrhage. Neurocritical Care. 2012;16(2):343–345. doi: 10.1007/s12028-011-9654-0. ; author reply 346-9. [DOI] [PubMed] [Google Scholar]
- 63.Dupuis C., Sonneville R., Adrie C., et al. Impact of transfusion on patients with sepsis admitted in intensive care unit: a systematic review and meta-analysis. Ann Intensive Care. 2017;7(1):5. doi: 10.1186/s13613-016-0226-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dhar R., Misra H., Diringer M.N. SANGUINATE™ (PEGylated carboxyhemoglobin bovine) improves cerebral blood flow to vulnerable brain regions at risk of delayed cerebral ischemia after subarachnoid hemorrhage. Neurocritical Care. 2017;27(3):341–349. doi: 10.1007/s12028-017-0418-3. [DOI] [PubMed] [Google Scholar]
- 65.Hoiland R.L., Bain A.R., Rieger M.G., et al. Hypoxemia, oxygen content, and the regulation of cerebral blood flow. Am J Physiol Regul Integr Comp Physiol. 2016;310(5):R398–R413. doi: 10.1152/ajpregu.00270.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ekelund A., Reinstrup P., Ryding E., et al. Effects of iso- and hypervolemic hemodilution on regional cerebral blood flow and oxygen delivery for patients with vasospasm after aneurysmal subarachnoid hemorrhage. Acta Neurochir. 2002;144(7):703–712. doi: 10.1007/s00701-002-0959-9. ; discussion 712-3. [DOI] [PubMed] [Google Scholar]
- 67.Jacobsen A., Nielsen T.H., Nilsson O., et al. Bedside diagnosis of mitochondrial dysfunction in aneurysmal subarachnoid hemorrhage. Acta Neurol Scand. 2014;130(3):156–163. doi: 10.1111/ane.12258. [DOI] [PubMed] [Google Scholar]
- 68.Wettervik T.S., Engquist H., Howells T., et al. Arterial oxygenation in traumatic brain injury-relation to cerebral energy metabolism, autoregulation, and clinical outcome. J Intensive Care Med. 2020 doi: 10.1177/0885066620944097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Okonkwo D.O., Shutter L.A., Moore C., et al. Brain oxygen optimization in severe traumatic brain injury phase-II: a phase II randomized trial. Crit Care Med. 2017;45(11):1907–1914. doi: 10.1097/ccm.0000000000002619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kety S.S., Schmidt C.F. The effects of altered arterial tensions of carbon dioxde and oxygen on cerebral blood flow and cerebral oxygen consumption of normal young men. J Clin Invest. 1948;27(4):484–492. doi: 10.1172/jci101995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Menzel M., Doppenberg E.M., Zauner A., et al. Cerebral oxygenation in patients after severe head injury: monitoring and effects of arterial hyperoxia on cerebral blood flow, metabolism and intracranial pressure. J Neurosurg Anesthesiol. 1999;11(4):240–251. doi: 10.1097/00008506-199910000-00003. [DOI] [PubMed] [Google Scholar]
- 72.Vidal-Jorge M., Sánchez-Guerrero A., Mur-Bonet G., et al. Does normobaric hyperoxia cause oxidative stress in the injured brain? A microdialysis study using 8-iso-prostaglandin F2α as a biomarker. J Neurotrauma. 2017;34(19):2731–2742. doi: 10.1089/neu.2017.4992. [DOI] [PubMed] [Google Scholar]
- 73.Reynolds R.A., Amin S.N., Jonathan S.V., et al. Hyperoxemia and cerebral vasospasm in aneurysmal subarachnoid hemorrhage. Neurocritical Care. 2020 doi: 10.1007/s12028-020-01136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fukuda S., Koga Y., Fujita M., et al. Hyperoxemia during the hyperacute phase of aneurysmal subarachnoid hemorrhage is associated with delayed cerebral ischemia and poor outcome: a retrospective observational study. J Neurosurg. 2019:1–8. doi: 10.3171/2019.9.Jns19781. [DOI] [PubMed] [Google Scholar]
- 75.Jeon S.B., Choi H.A., Badjatia N., et al. Hyperoxia may be related to delayed cerebral ischemia and poor outcome after subarachnoid haemorrhage. J Neurol Neurosurg Psychiatr. 2014;85(12):1301–1307. doi: 10.1136/jnnp-2013-307314. [DOI] [PubMed] [Google Scholar]
- 76.Yokoyama S., Hifumi T., Kawakita K., et al. Early hyperoxia in the intensive care unit is significantly associated with unfavorable neurological outcomes in patients with mild-to-moderate aneurysmal subarachnoid hemorrhage. Shock. 2019;51(5):593–598. doi: 10.1097/shk.0000000000001221. [DOI] [PubMed] [Google Scholar]
- 77.Kruyt N.D., Biessels G.J., DeVries J.H., et al. Hyperglycemia in aneurysmal subarachnoid hemorrhage: a potentially modifiable risk factor for poor outcome. J Cerebr Blood Flow Metabol : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2010;30(9):1577–1587. doi: 10.1038/jcbfm.2010.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zetterling M., Engström B.E., Hallberg L., et al. Cortisol and adrenocorticotropic hormone dynamics in the acute phase of subarachnoid haemorrhage. Br J Neurosurg. 2011;25(6):684–692. doi: 10.3109/02688697.2011.584638. [DOI] [PubMed] [Google Scholar]
- 79.Frontera J.A., Fernandez A., Claassen J., et al. Hyperglycemia after SAH: predictors, associated complications, and impact on outcome. Stroke. 2006;37(1):199–203. doi: 10.1161/01.STR.0000194960.73883.0f. [DOI] [PubMed] [Google Scholar]
- 80.Van den Berghe G., Wilmer A., Hermans G., et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449–461. doi: 10.1056/NEJMoa052521. [DOI] [PubMed] [Google Scholar]
- 81.van den Berghe G., Wouters P., Weekers F., et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345(19):1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 82.Schlenk F., Vajkoczy P., Sarrafzadeh A. Inpatient hyperglycemia following aneurysmal subarachnoid hemorrhage: relation to cerebral metabolism and outcome. Neurocritical Care. 2009;11(1):56–63. doi: 10.1007/s12028-009-9222-z. [DOI] [PubMed] [Google Scholar]
- 83.van Donkelaar C.E., Dijkland S.A., van den Bergh W.M., et al. Early circulating lactate and glucose levels after aneurysmal subarachnoid hemorrhage correlate with poor outcome and delayed cerebral ischemia: a two-center cohort study. Crit Care Med. 2016;44(5):966–972. doi: 10.1097/ccm.0000000000001569. [DOI] [PubMed] [Google Scholar]
- 84.Otite F., Mink S., Tan C.O., et al. Impaired cerebral autoregulation is associated with vasospasm and delayed cerebral ischemia in subarachnoid hemorrhage. Stroke. 2014;45(3):677–682. doi: 10.1161/strokeaha.113.002630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bilotta F., Caramia R., Cernak I., et al. Intensive insulin therapy after severe traumatic brain injury: a randomized clinical trial. Neurocritical Care. 2008;9(2):159–166. doi: 10.1007/s12028-008-9084-9. [DOI] [PubMed] [Google Scholar]
- 86.Coester A., Neumann C.R., Schmidt M.I. Intensive insulin therapy in severe traumatic brain injury: a randomized trial. Journal of Trauma and Acute Care Surgery. 2010;68(4):904–911. doi: 10.1097/TA.0b013e3181c9afc2. [DOI] [PubMed] [Google Scholar]
- 87.Oddo M., Schmidt J.M., Carrera E., et al. Impact of tight glycemic control on cerebral glucose metabolism after severe brain injury: a microdialysis study. Crit Care Med. 2008;36(12):3233–3238. doi: 10.1097/CCM.0b013e31818f4026. [DOI] [PubMed] [Google Scholar]
- 88.Svedung Wettervik T., Howells T., Ronne-Engstrom E., et al. High arterial glucose is associated with poor pressure autoregulation, high cerebral lactate/pyruvate ratio and poor outcome following traumatic brain injury. Neurocritical Care. 2019;31(3):526–533. doi: 10.1007/s12028-019-00743-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Latorre J.G., Chou S.H., Nogueira R.G., et al. Effective glycemic control with aggressive hyperglycemia management is associated with improved outcome in aneurysmal subarachnoid hemorrhage. Stroke. 2009;40(5):1644–1652. doi: 10.1161/strokeaha.108.535534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kramer A.H., Roberts D.J., Zygun D.A. Optimal glycemic control in neurocritical care patients: a systematic review and meta-analysis. Crit Care. 2012;16(5):R203. doi: 10.1186/cc11812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Salinas P.D., Mendez C.E. Glucose management technologies for the critically ill. Journal of diabetes science and technology. 2019;13(4):682–690. doi: 10.1177/1932296818822838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hutchinson P.J., Jalloh I., Helmy A., et al. Consensus statement from the 2014 international microdialysis forum. Intensive Care Med. 2015;41(9):1517–1528. doi: 10.1007/s00134-015-3930-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Simpson I.A., Carruthers A., Vannucci S.J. Supply and demand in cerebral energy metabolism: the role of nutrient transporters. J Cerebr Blood Flow Metabol : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2007;27(11):1766–1791. doi: 10.1038/sj.jcbfm.9600521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Pellerin L., Magistretti P.J. Glutamate uptake into astrocytes stimulates aerobic glycolysis: a mechanism coupling neuronal activity to glucose utilization. Proc. Natl. Acad. Sci. U.S.A. 1994;91(22):10625–10629. doi: 10.1073/pnas.91.22.10625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bouzat P., Sala N., Suys T., et al. Cerebral metabolic effects of exogenous lactate supplementation on the injured human brain. Intensive Care Med. 2014;40(3):412–421. doi: 10.1007/s00134-013-3203-6. [DOI] [PubMed] [Google Scholar]
- 96.Gallagher C.N., Carpenter K.L., Grice P., et al. The human brain utilizes lactate via the tricarboxylic acid cycle: a 13C-labelled microdialysis and high-resolution nuclear magnetic resonance study. Brain : J Neurol. 2009;132(Pt 10):2839–2849. doi: 10.1093/brain/awp202. [DOI] [PubMed] [Google Scholar]
- 97.Jalloh I., Helmy A., Shannon R.J., et al. Lactate uptake by the injured human brain: evidence from an arteriovenous gradient and cerebral microdialysis study. J Neurotrauma. 2013;30(24):2031–2037. doi: 10.1089/neu.2013.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boumezbeur F., Petersen K.F., Cline G.W., et al. The contribution of blood lactate to brain energy metabolism in humans measured by dynamic 13C nuclear magnetic resonance spectroscopy. J Neurosci : the official journal of the Society for Neuroscience. 2010;30(42):13983–13991. doi: 10.1523/jneurosci.2040-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Carteron L., Solari D., Patet C., et al. Hypertonic lactate to improve cerebral perfusion and glucose availability after acute brain injury. Crit Care Med. 2018;46(10):1649–1655. doi: 10.1097/ccm.0000000000003274. [DOI] [PubMed] [Google Scholar]
- 100.Quintard H., Patet C., Zerlauth J.B., et al. Improvement of neuroenergetics by hypertonic lactate therapy in patients with traumatic brain injury is dependent on baseline cerebral lactate/pyruvate ratio. J Neurotrauma. 2016;33(7):681–687. doi: 10.1089/neu.2015.4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Attwell D., Buchan A.M., Charpak S., et al. Glial and neuronal control of brain blood flow. Nature. 2010;468(7321):232–243. doi: 10.1038/nature09613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Svedung Wettervik T., Engquist H., Howells T., et al. Arterial lactate in traumatic brain injury–Relation to intracranial pressure dynamics, cerebral energy metabolism and clinical outcome. J Crit Care. 2020;60:218–225. doi: 10.1016/j.jcrc.2020.08.014. [DOI] [PubMed] [Google Scholar]
- 103.Svedung Wettervik T.M., Engquist H., Lenell S., et al. Systemic hyperthermia in traumatic brain injury-relation to intracranial pressure dynamics, cerebral energy metabolism, and clinical outcome. J Neurosurg Anesthesiol. 2020 doi: 10.1097/ana.0000000000000695. [DOI] [PubMed] [Google Scholar]
- 104.Rossi S., Zanier E.R., Mauri I., et al. Brain temperature, body core temperature, and intracranial pressure in acute cerebral damage. J Neurol Neurosurg Psychiatr. 2001;71(4):448–454. doi: 10.1136/jnnp.71.4.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Takagi K., Tsuchiya Y., Okinaga K., et al. Natural hypothermia immediately after transient global cerebral ischemia induced by spontaneous subarachnoid hemorrhage. J Neurosurg. 2003;98(1):50–56. doi: 10.3171/jns.2003.98.1.0050. [DOI] [PubMed] [Google Scholar]
- 106.Fernandez A., Schmidt J.M., Claassen J., et al. Fever after subarachnoid hemorrhage: risk factors and impact on outcome. Neurology. 2007;68(13):1013–1019. doi: 10.1212/01.wnl.0000258543.45879.f5. [DOI] [PubMed] [Google Scholar]
- 107.Hocker S.E., Tian L., Li G., et al. Indicators of central fever in the neurologic intensive care unit. JAMA Neurol. 2013;70(12):1499–1504. doi: 10.1001/jamaneurol.2013.4354. [DOI] [PubMed] [Google Scholar]
- 108.Oddo M., Frangos S., Milby A., et al. Induced normothermia attenuates cerebral metabolic distress in patients with aneurysmal subarachnoid hemorrhage and refractory Fever. Stroke. 2009;40(5):1913–1916. doi: 10.1161/strokeaha.108.534115. [DOI] [PubMed] [Google Scholar]
- 109.Oliveira-Filho J., Ezzeddine M.A., Segal A.Z., et al. Fever in subarachnoid hemorrhage: relationship to vasospasm and outcome. Neurology. 2001;56(10):1299–1304. doi: 10.1212/wnl.56.10.1299. [DOI] [PubMed] [Google Scholar]
- 110.Naidech A.M., Bendok B.R., Bernstein R.A., et al. Fever burden and functional recovery after subarachnoid hemorrhage. Neurosurgery. 2008;63(2):212–217. doi: 10.1227/01.Neu.0000320453.61270.0f. ; discussion 217-8. [DOI] [PubMed] [Google Scholar]
- 111.Meier K., Lee K. Neurogenic fever. J Intensive Care Med. 2017;32(2):124–129. doi: 10.1177/0885066615625194. [DOI] [PubMed] [Google Scholar]
- 112.Schiefecker A.J., Pfausler B., Beer R., et al. Parenteral diclofenac infusion significantly decreases brain-tissue oxygen tension in patients with poor-grade aneurysmal subarachnoid hemorrhage. Crit Care. 2013;17(3):R88. doi: 10.1186/cc12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chmayssani M., Stein N.R., McArthur D.L., et al. Therapeutic intravascular normothermia reduces the burden of metabolic crisis. Neurocritical Care. 2015;22(2):265–272. doi: 10.1007/s12028-014-0076-7. [DOI] [PubMed] [Google Scholar]
- 114.Oddo M., Frangos S., Maloney-Wilensky E., et al. Effect of shivering on brain tissue oxygenation during induced normothermia in patients with severe brain injury. Neurocritical Care. 2010;12(1):10–16. doi: 10.1007/s12028-009-9280-2. [DOI] [PubMed] [Google Scholar]
- 115.Todd M.M., Hindman B.J., Clarke W.R., et al. Mild intraoperative hypothermia during surgery for intracranial aneurysm. N Engl J Med. 2005;352(2):135–145. doi: 10.1056/NEJMoa040975. [DOI] [PubMed] [Google Scholar]
- 116.Anderson S.W., Todd M.M., Hindman B.J., et al. Effects of intraoperative hypothermia on neuropsychological outcomes after intracranial aneurysm surgery. Ann Neurol. 2006;60(5):518–527. doi: 10.1002/ana.21018. [DOI] [PubMed] [Google Scholar]
- 117.Seule M.A., Muroi C., Mink S., et al. Therapeutic hypothermia in patients with aneurysmal subarachnoid hemorrhage, refractory intracranial hypertension, or cerebral vasospasm. Neurosurgery. 2009;64(1):86–92. doi: 10.1227/01.Neu.0000336312.32773.A0. discussion 92-3. [DOI] [PubMed] [Google Scholar]
- 118.Karnatovskaia L.V., Lee A.S., Festic E., et al. Effect of prolonged therapeutic hypothermia on intracranial pressure, organ function, and hospital outcomes among patients with aneurysmal subarachnoid hemorrhage. Neurocritical Care. 2014;21(3):451–461. doi: 10.1007/s12028-014-9989-4. [DOI] [PubMed] [Google Scholar]
- 119.Chen H., Wu F., Yang P., et al. A meta-analysis of the effects of therapeutic hypothermia in adult patients with traumatic brain injury. Crit Care. 2019;23(1):396. doi: 10.1186/s13054-019-2667-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cooper D.J., Nichol A.D., Bailey M., et al. Effect of early sustained prophylactic hypothermia on neurologic outcomes among patients with severe traumatic brain injury: the POLAR randomized clinical trial. JAMA. 2018;320(21):2211–2220. doi: 10.1001/jama.2018.17075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Andrews P.J., Sinclair H.L., Rodriguez A., et al. Hypothermia for intracranial hypertension after traumatic brain injury. N Engl J Med. 2015;373(25):2403–2412. doi: 10.1056/NEJMoa1507581. [DOI] [PubMed] [Google Scholar]
- 122.Group HaCAS. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 123.Dankiewicz J., Cronberg T., Lilja G., et al. Hypothermia versus normothermia after out-of-hospital cardiac arrest. N Engl J Med. 2021;384(24):2283–2294. doi: 10.1056/NEJMoa2100591. [DOI] [PubMed] [Google Scholar]
- 124.Lanzino G., D'Urso P.I., Suarez J. Seizures and anticonvulsants after aneurysmal subarachnoid hemorrhage. Neurocritical Care. 2011;15(2):247–256. doi: 10.1007/s12028-011-9584-x. [DOI] [PubMed] [Google Scholar]
- 125.Bögli S.Y., Wang S., Romaguera N., et al. Impact of seizures and status epilepticus on outcome in patients with aneurysmal subarachnoid hemorrhage. Neurocritical Care. 2022;36(3):751–759. doi: 10.1007/s12028-022-01489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kondziella D., Friberg C.K., Wellwood I., et al. Continuous EEG monitoring in aneurysmal subarachnoid hemorrhage: a systematic review. Neurocritical Care. 2015;22(3):450–461. doi: 10.1007/s12028-014-0068-7. [DOI] [PubMed] [Google Scholar]
- 127.Suzuki H., Kawakita F., Asada R. Neuroelectric mechanisms of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Int J Mol Sci. 2022;23(6) doi: 10.3390/ijms23063102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kramer D.R., Fujii T., Ohiorhenuan I., et al. Cortical spreading depolarization: pathophysiology, implications, and future directions. J Clin Neurosci : official journal of the Neurosurgical Society of Australasia. 2016;24:22–27. doi: 10.1016/j.jocn.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 129.Dreier J.P. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med. 2011;17(4):439–447. doi: 10.1038/nm.2333. [DOI] [PubMed] [Google Scholar]
- 130.Verweij B.H., Muizelaar J.P., Vinas F.C., et al. Impaired cerebral mitochondrial function after traumatic brain injury in humans. J Neurosurg. 2000;93(5):815–820. doi: 10.3171/jns.2000.93.5.0815. [DOI] [PubMed] [Google Scholar]
- 131.Svedung Wettervik T., Hånell A., Howells T., et al. Females exhibit better cerebral pressure autoregulation, less mitochondrial dysfunction, and reduced excitotoxicity after severe traumatic brain injury. J Neurotrauma. 2022 doi: 10.1089/neu.2022.0097. [DOI] [PubMed] [Google Scholar]
- 132.Wettervik T.S., Howells T., Hånell A., et al. Intracranial pressure variability: a new potential metric of cerebral ischemia and energy metabolic dysfunction in aneurysmal subarachnoid hemorrhage? J Neurosurg Anesthesiol. 2022 doi: 10.1097/ANA.0000000000000816. ePub ahead of print. [DOI] [PubMed] [Google Scholar]
- 133.Kofler M., Gaasch M., Rass V., et al. The importance of probe location for the interpretation of cerebral microdialysis data in subarachnoid hemorrhage patients. Neurocritical Care. 2020;32(1):135–144. doi: 10.1007/s12028-019-00713-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Diringer M.N., Zazulia A.R., Powers W.J. Does ischemia contribute to energy failure in severe TBI? Translational stroke research. 2011;2(4):517–523. doi: 10.1007/s12975-011-0119-8. [DOI] [PubMed] [Google Scholar]
- 135.Kelsen J., Karlsson M., Hansson M.J., et al. Copenhagen head injury ciclosporin study: a phase IIa safety, pharmacokinetics, and biomarker study of ciclosporin in severe traumatic brain injury patients. J Neurotrauma. 2019;36(23):3253–3263. doi: 10.1089/neu.2018.6369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Young A.M., Karri S.K., Helmy A., et al. Pharmacologic management of subarachnoid hemorrhage. World neurosurgery. 2015;84(1):28–35. doi: 10.1016/j.wneu.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 137.Pickard J.D., Murray G.D., Illingworth R., et al. Effect of oral nimodipine on cerebral infarction and outcome after subarachnoid haemorrhage: British aneurysm nimodipine trial. BMJ (Clinical research ed) 1989;298(6674):636–642. doi: 10.1136/bmj.298.6674.636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Macdonald R.L., Higashida R.T., Keller E., et al. Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haemorrhage undergoing surgical clipping: a randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2) Lancet Neurol. 2011;10(7):618–625. doi: 10.1016/s1474-4422(11)70108-9. [DOI] [PubMed] [Google Scholar]
- 139.Bohara S., Gaonkar V.B., Garg K., et al. Effect of statins on functional outcome and mortality following aneurysmal subarachnoid hemorrhage - results of a meta-analysis, metaregression and trial sequential analysis. Clin Neurol Neurosurg. 2021;207 doi: 10.1016/j.clineuro.2021.106787. [DOI] [PubMed] [Google Scholar]
- 140.Chen J., Tang P., Fu X. Cilostazol administration for subarachnoid hemorrhage: a meta-analysis of randomized controlled trials. J Clin Neurosci : official journal of the Neurosurgical Society of Australasia. 2021;89:305–310. doi: 10.1016/j.jocn.2021.04.044. [DOI] [PubMed] [Google Scholar]
- 141.Reddy D., Fallah A., Petropoulos J.A., et al. Prophylactic magnesium sulfate for aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. Neurocritical Care. 2014;21(2):356–364. doi: 10.1007/s12028-014-9964-0. [DOI] [PubMed] [Google Scholar]
- 142.Post R., Germans M.R., Tjerkstra M.A., et al. Ultra-early tranexamic acid after subarachnoid haemorrhage (ULTRA): a randomised controlled trial. Lancet (London, England) 2021;397(10269):112–118. doi: 10.1016/s0140-6736(20)32518-6. [DOI] [PubMed] [Google Scholar]
- 143.Hillman J., Fridriksson S., Nilsson O., et al. Immediate administration of tranexamic acid and reduced incidence of early rebleeding after aneurysmal subarachnoid hemorrhage: a prospective randomized study. J Neurosurg. 2002;97(4):771–778. doi: 10.3171/jns.2002.97.4.0771. [DOI] [PubMed] [Google Scholar]
- 144.Hillman J., Aneman O., Anderson C., et al. A microdialysis technique for routine measurement of macromolecules in the injured human brain. Neurosurgery. 2005;56(6):1264–1268. doi: 10.1227/01.neu.0000159711.93592.8d. ; discussion 1268-70. [DOI] [PubMed] [Google Scholar]
- 145.Hutchinson P.J., O'Connell M.T., Nortje J., et al. Cerebral microdialysis methodology--evaluation of 20 kDa and 100 kDa catheters. Physiol Meas. 2005;26(4):423–428. doi: 10.1088/0967-3334/26/4/008. [DOI] [PubMed] [Google Scholar]
- 146.Mellergård P., Aneman O., Sjögren F., et al. Changes in extracellular concentrations of some cytokines, chemokines, and neurotrophic factors after insertion of intracerebral microdialysis catheters in neurosurgical patients. Neurosurgery. 2008;62(1):151–157. doi: 10.1227/01.Neu.0000311072.33615.3a. ; discussion 157-8. [DOI] [PubMed] [Google Scholar]
- 147.Mellergård P., Sjögren F., Hillman J. The cerebral extracellular release of glycerol, glutamate, and FGF2 is increased in older patients following severe traumatic brain injury. J Neurotrauma. 2012;29(1):112–118. doi: 10.1089/neu.2010.1732. [DOI] [PubMed] [Google Scholar]
- 148.Helmy A., Carpenter K.L., Menon D.K., et al. The cytokine response to human traumatic brain injury: temporal profiles and evidence for cerebral parenchymal production. J Cerebr Blood Flow Metabol : official journal of the International Society of Cerebral Blood Flow and Metabolism. 2011;31(2):658–670. doi: 10.1038/jcbfm.2010.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dyhrfort P., Svedung Wettervik T., Clausen F., et al. A dedicated 21-plex proximity extension assay panel for high-sensitivity protein biomarker detection using microdialysis in severe traumatic brain injury: the next step in precision medicine? Neurotrauma reports. 2023;4(1):25–40. doi: 10.1089/neur.2022.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Hillered L., Dahlin A.P., Clausen F., et al. Cerebral microdialysis for protein biomarker monitoring in the neurointensive care setting–a technical approach. Front Neurol. 2014;5:245. doi: 10.3389/fneur.2014.00245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Landegren U., Vänelid J., Hammond M., et al. Opportunities for sensitive plasma proteome analysis. Anal Chem. 2012;84(4):1824–1830. doi: 10.1021/ac2032222. [DOI] [PubMed] [Google Scholar]
- 152.Darmanis S., Gallant C.J., Marinescu V.D., et al. Simultaneous multiplexed measurement of RNA and proteins in single cells. Cell Rep. 2016;14(2):380–389. doi: 10.1016/j.celrep.2015.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]