Summary
Background
Pregnancy is universally considered a normal physiological process. However, it has a considerable impact on the quality of mothers’ lives. This study piloted the use of the generic EuroQoL-5 Dimensions-5 Levels (EQ-5D-5L) descriptive system and the EuroQol Visual Analogue Scale (EQ-VAS) questionnaire, to assess the health-related quality of life (HRQoL) during pregnancy and its associated factors.
Methods
In this cross-sectional pilot study carried out from August to December 2019 we assessed the HRQoL and its associated factors among Moroccan pregnant women who received prenatal care at Settat's health centers. The collected data from 270 pregnant women were compared to a dataset of 289 non-pregnant women using the EQ-5D-5L instrument and socioeconomic and obstetrical questionnaires. A multiple linear regression model was used to identify associated factors. The HRQoL comparison was made using the improved RIDIT approach, which allows estimating the Absolute Risk Increase (ARI) of problems related to mobility, usual activities, and self-care and the ARI of pain/discomfort and anxiety/depression (i.e. an ARI = 10% in mobility means that pregnancy increases problems in this health dimension by 10%).
Findings
A total of 559 women were included in our study. Our results showed that the HRQoL in pregnant women was significantly lower than in non-pregnant women (EQ-5D index score = 0.71 ± 0.24 vs 0.79 ± 0.29; p < 0.0001). Similarly, the pregnancy reduced the EQ-VAS score (mean difference = −7.8 ± 17.21; p < 0.0001). The pregnancy increased the problems in mobility (ARI = 9.7% [1.7–17.6], p = 0.02), in self-care (ARI = 8% [2–14], p = 0.01), and in usual activities (ARI = 27.3% [18.9–35.7], p < 0.0001). Also, the pregnancy increased pain/discomfort (ARI = 26.5% [18–35.1], p < 0.0001) and anxiety/depression (ARI = 12% [3.2–20.9], p = 0.0112). The rural pregnant women had the worst HRQoL (EQ-5D index score = 0.57) compared to their urban peers (EQ-5D index score = 0.77). Likewise, women in the third trimester and nulliparous had the worst HRQoL (EQ-5D index score = 0.64 and 0.84 respectively).
Interpretation
The results highlighted that place of residence, parity, and gestational age are strongly associated with pregnant's HRQoL. The five EQ-5D-5L dimensions were affected during pregnancy. Consequently, there is a need to develop specific programs to monitor the HRQoL during pregnancy in order to ensure better maternal health care.
Funding
This study was funded by University Hassan First’s own fund [grant number FP/01/2018].
Keywords: Health-related quality of life, HRQoL, Pregnancy, EQ-5D-5L, VAS, RIDIT
Research in context.
Evidence before this study
We searched PubMed and Web of Science for studies published in English or French between June 2011, and June 2021, that assessed the health-related quality of life (HRQoL) of pregnant women. We used the search terms “pregnancy”, “pregnant”, “quality-of-life” and “HRQoL”. We excluded studies that focused exclusively on a specific health aspect (eg, depression) and not the quality of life across all dimensions, miscarriages, voluntary interruptions of pregnancy, childbirth, postpartum, and specific HRQoL questionnaires. The studies where HRQoL in pregnancy was assessed by generic instruments were included in the review. We identified seventy-three studies: 39% from Europe and 35% from Asia. Only two articles from Egypt and Tunisia were published representing Africa. There is no publication from Morocco during the past ten years. The category of obstetrics differed between studies; forty-four articles concern physiological pregnancies, sixteen articles concern pregnancies with gestational pathology, seven articles for pregnancies with pre-existing pathology, and six articles are dealing with In Vitro Fertilization pregnancies. The health-related quality of life among pregnant women was lower than the population norms, especially in the mental and physical domains. During pregnancy, HRQoL improved from the first to the second trimester, then declined in the second and third trimesters, most notably in physical health, mental health, and social functioning. The perceived health status was lower in the ninth month of pregnancy than in the third month. In contrast, other researchers' trials revealed no difference in HRQoL among women in different trimesters of pregnancy. A variety of factors have been linked to pregnant women's HRQoL. Improved well-being was associated, with socio-demographic characteristics (favorable economic status and social support). Similarly, improved sleep quality and moderate physical activity were linked to an increased HRQoL. Physical and psychological factors, on the other hand, were associated with a lower HRQoL.
Added value of this study
We compared the HRQoL between pregnant women and non-pregnant women using the EQ-5D-5L. To better understand the impact of pregnancy on the HRQoL, depth comparisons between both groups at each health dimension were needed. For that reason, we used the improved RIDIT approach, which allows the analysis of the five dimensions of the EQ-5D-5L separately. Our study comes with the fact that it is interesting to implement the HRQoL concept as a health promotion program to monitor HRQoL during pregnancy.
Implications of all the available evidence
This study is the first, in Africa, to evaluate the HRQoL during pregnancy without referring to a specific pathology. Our findings can be used to compare the HRQoL during pregnancy and its associated factors in several countries across the world. This is crucial information for policymakers to better understand the impact of pregnancy on women's HRQoL and therefore gear toward improving antenatal consultations program and creating supportive interventions to restore a good HRQoL and to better face the series of changes during the whole period of pregnancy. In addition, the comparison of the HRQoL between the three trimesters of pregnancy could provide evidence for developing trimester specific HRQoL management programs, as well as the recommendation to healthcare professionals to consider the age of pregnancy while designing therapeutic strategies or planned interventions for pregnant women.
Introduction
Survival and morbidity criteria are no longer sufficient to assess medical progress, hence the interest in combining them with the patient's perspective, even if it is subjective.1,2 Thus, the concept of health-related quality of life (HRQoL) has been introduced as a dimension to consider the patient's view of his health status in addition to objective clinical measures.
The World Health Organization (WHO) defines HRQoL as an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, norms, and concerns. In the field of health, the term HRQoL is frequently used, which considers aspects such as diseases, disorders, and the need for therapeutic interventions.3
In the case of pregnancy, as a physiological state with significant and interacting physical and emotional changes, quality of care and service delivery are the focus of health professionals and generally follow a medicalized and technocratic model.4 However, less attention is paid to non-clinical measures such as changes in mental health, self-esteem, and confidence, and HRQoL that are impacted even in a normal pregnancy.5 Assessment of the above factors including HRQoL in pregnant women can provide a solid foundation for maternal health promotion. The health of pregnant women must integrate HRQoL as a complementary dimension that is expressed through the program of prevention and accompaniment of pregnancy.6 In this perspective, many instruments for measuring HRQoL have been developed, which can be divided into two types. Specific instruments allow for greater sensitivity in measuring impacts but do not allow for comparison between different therapeutic areas, while generic instruments allow for comparison of the impacts of interventions in different clinical areas, but their measurement lacks sensitivity and specificity. As a generic instrument, the EuroQol EQ-5D is the one recommended by the Haute Autorité de Santé (HAS) and other foreign agencies to measure health status.7
The HRQoL of pregnant women is influenced by several factors, including social insertions, acceptance of gestation, family restructuring, the conception of the mother's role, and preparation for childbirth during pregnancy. In addition, quality of life is also influenced by physical health, psychological status, social relationships, and the relationship with important elements of the subject's environment.8 Therefore, health care professionals, in addition to traditional care, must consider changes in quality of life that are also supported by the literature.9
The assessment of HRQoL during pregnancy is a growing topic, however, in Morocco, no study in this sense has been initiated so far. The objective of this study is to highlight the evolution of the HRQoL of Moroccan pregnant women throughout pregnancy and according to gestational age, as well as the socioeconomic and obstetrical factors that influence it.
Methods
Study design and population
A cross-sectional pilot study was carried out from August to December 2019, to assess HRQoL and associated factors among Moroccan pregnant women who received prenatal care during different gestational ages at Settat's health centers. All women who gave consent subsequently responded to the questionnaire (response rate of 100%).
All pregnant women of childbearing age who had antenatal consultation visit in one of Settat health centers were the source population. The women included in the study are Moroccan, married, and pregnant, able to understand and speak Arabic, singleton, and without psychiatric and/or chronic physiological disease. The gestational age was not limited in order to compare the HRQoL during the three trimesters of pregnancy. After classifying the women according to the age of their pregnancy, which was measured according to the date of the last menstruation and confirmed by the medical examination, the consenting patients were asked to complete a questionnaire evaluating their HRQoL using the EQ-5D-5L instrument. Information regarding socioeconomic and obstetric characteristics was also collected.
Non-pregnant women of childbearing age, nulliparous, and without psychiatric and/or chronic physiological disease, and attending health centers for various consultations were admitted to the study as comparative group. They were invited to complete a questionnaire collecting information on their HRQoL and socio-demographic characteristics. Subjects matching the same socioeconomic characteristics of each case were randomly selected from the eligible participants. The questionnaire is similar to that of pregnant women sample with the exception of obstetrical characteristics.
The non-pregnant women were selected following the bellow paired algorithm including the six sociodemographic characteristics numbered (1-Age, 2-place of residence, 3-Education, 4-Employment, 5-Marital status, and 6-Socioeconomic level):
First, the interviewer asked the pregnant woman to choose a number between 1 and 6 and thereafter started the interview by asking her corresponding sociodemographic characteristic (for example, if the pregnant women choose the number 3, so the interview starts by asking her education level). Then, the interviewer notes the category response (for example, if the pregnant woman responded to primary education level, the interviewer notes this in his/her interview-book this information) and continues to ask the remaining questions. The category response was used as a paired parameter.
Second, a non-pregnant woman was selected according to the paired parameter above (the response category from the example above was “primary education level”, so the interviewer should pair on this parameter. He/she includes a non-pregnant woman with the same education level).
The interviewers were PhD students in public health and had been trained before they took part in this study.
Since we have 14.4% and 16.6% of illiterate pregnant and non-pregnant women respectively, the interviewers guided them for the questionnaire.
Before recording data, two team researchers conducted separately data quality control of the collected information by checking for the interviewer, measurement, and coding errors and for duplications (interview of the same subject twice).
Ethics statement
Ethical approval was granted by the scientific research commission of Hassan First University. Permission to conduct the study was obtained from the health delegation of the greater Casablanca region. A letter for participation and results publication was presented to the respondents. This paper forms part of the objectives set out in institutional Project FP/01/2018 which was approved by the research committee of Hassan First University. The study was conducted following the tenets of the Helsinki Declaration and was approved by the ethics committee of Hassan First University with the IRB number CERSBSS/UH1/P1/19. Both groups (pregnant and non-pregnant women) submitted their written consent form after they were ensured of the anonymity of the questionnaires, the confidentiality of their data, and their right to withdraw at any time during the interviews.
Variables
The selection of women corresponding to the inclusion criteria was based on their medical files, in order to include only pregnant women without psychiatric and/or chronic disease, and with singleton fetus. Also, we used the medical files for the gestational age. An interview of 20 min was held with the investigator to answer the questions. The first part of the questionnaire includes 11 questions on socioeconomic (age, education, marital status, employment status, home, and socioeconomic level), and obstetric characteristics (parity, gestational age, ANC visits, and gestational complications).
Regarding the HRQoL, we used the questionnaire EuroQoL 5D-5L (EQ-5D-5L) which is a standardized measure of health status developed by the EuroQol Group to provide a simple and generic measure of health for the clinical and economic evaluation, internationally validated for the measurement of the HRQoL and this questionnaire is available and validated in Moroccan dialect version.10 The questionnaire defines a respondent's health status according to five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Within each dimension, there are five severity levels corresponding to no problem, slight problem, moderate problem, severe problem, and extreme problem. A participant's response was converted into a five-digit number describing the health state, i.e, 21,534 is the health state equivalent to slight problems in mobility, no problems in self-care, extreme problems in usual activities, moderate problems in pain/discomfort, and severe problems in anxiety depression.
Using an appropriate algorithm, the five-digit health states are converted into utility scores, which are available for several countries. When utility scores are unavailable, it would be acceptable to estimate utilities using a value set from another country. As the Moroccan value set for the EQ-5D-5L has not yet been developed, we used the France value set to calculate utility scores using the EuroQol program.11
The assessment of the HRQoL, measured by the 5 dimensions, is completed by an overall assessment self-reported of health status. This assessment is obtained using a Visual Analogue Scale (EQ-VAS) which gives a subjective individual estimate of health status. It is presented as a vertical line with demarcations from 100 (best imaginable health state) to 0 (worst imaginable health state). Respondents were asked to draw a line from the bottom line 0 to the score line based on their opinion of their health status and fill the score in the blank beside.
Study size
Before starting the study, we contacted all health centers. Each center informed us of the number of pregnant women coming for ANC. A list of contact information for pregnant women attending each health center was provided. The seven lists were compiled in an Excel file. In total, there were 4100 women.
The sample size calculation was based on the EQ-VAS value. From our previous study on the HRQoL in Moroccan general population, the EQ-VAS mean was equal to 88 ± 20. In the present comparative cross-sectional study, we assume to detect at least a mean difference ΔmeanEQ-VAS = 5 between pregnant and non-pregnant women. With a study design of a ratio of pregnant to non-pregnant equal to 1, the minimum number of women of each group is calculated by:
For a 95% confidence interval (α = 0.05) and statistical power of 80% (β = 0.2) and a minimum difference to be detected of Δ = 5, the minimum number of women to interview in each group was n = 251. With an expected proportion (20%) of non-response, the total target sample was 602 (301 pregnant and 301 non-pregnant women).
The sampling was carried out by the sample random method using the Microsoft Excel function RANDBETWEEN (1; 4100) to select the 301 women to be interviewed. We called these women by phone to schedule appointments with them during their subsequent visits.
During data collection, to reach 602 participants we approached 718 eligible participants, 350 pregnant women and 368 non-pregnant women. Of these, 49 and 67 did not give consent to participate in the study, respectively. The consent rate was therefore 86% (301/350) among pregnant women and 81.8% (301/368) among non-pregnant women.
Statistical analysis
Data analysis was performed using the software Statistical Package for the Social Science (SPSS) version 19. For quantitative variables (EQ-VAS and EQ-5D-index), we tested the normality assumption by Shapiro–Wilk and Kolmogorov–Smirnov. Normally distributed continuous variables were described using the means ± standard deviations (SDs) and categorical variables were described using counts and percentages. The dependent variables were the EQ-5D index and EQ-VAS. The socio-economic and obstetrical characteristics and HRQoL of the two groups were compared using Student and ANOVA tests for continuous variables.
The effect of pregnancy on the HRQoL of women was assessed by comparing the EQ-5D-5L data of the two independent samples. This comparison was made based on the global information contained in the utility and VAS scores and EQ-5D-5L dimensions. For each EQ-5D-5L dimension characterized by an ordinal variable representing severity level, we used the improved RIDIT approach.12 This approach considers the severity level of the EQ-5D-5L dimensions, which allows estimation of Absolute Risk Reduction/Absolute Risk Increase (ARR/ARI) and ordinal Odds-Ratio. The enhanced RIDIT allows for separate analysis of the 5 dimensions of the EQ-5D-5L, which provides greater precision in understanding the effect of a circumstantial condition on health status. In our study, we evaluated the effect of pregnancy on women's HRQoL. Therefore, for each dimension of EQ-5D-5L, the effect of pregnancy was estimated by ARI and OddsOrdinal. We expect that pregnancy could increase problems in mobility, self-care and usual activities; and increase anxiety/depression and pain/discomfort among pregnant women. Then, this increase is estimated for each EQ-5D-5L dimension by ARI%. For example, if pregnancy increase anxiety/depression, we say that pregnant women are ARI% more anxious/depressive (or pregnancy increases anxiety/depression by ARI% among pregnant women). From the improved RIDIT, we also estimated the OddsOrdinal (example, pregnant women are OddsOrdinal times anxious/depressive than non-pregnant women). Analysis of behavioral changes due to pregnancy was performed using the Stuart–Maxwell test for marginal homogeneity for two dependent samples. The p-values were adjusted by Holm-Bonferroni correction.
Role of the funding
The funding source had no role in the study design, data collection, data analysis, data interpretation, access to dataset, writing of the report or decision to submit for publication. AB, SC, and AM had full access to the data in the study. IY-M had final responsibility for the decision to submit for publication.
Result
Socioeconomic and obstetrical characteristics
After data quality control, 10.2% (31) and 3.9% (12) of pregnant women and non-pregnant women were excluded respectively. A total of 579 women were included in this study (270 pregnant women and 289 non-pregnant women).
To conduct this study, the minimum sample size was 251. We added 20% expected non-response to avoid having fewer participants than the required sample (to avoid misrepresentation in the final analyzed sample). So, we interviewed 602 women, i.e., 301 in each group. After data quality control, the final analyses were conducted on 270 pregnant women and 289 non-pregnant women, which are greater than the minimum required sample size, and then do not create misrepresentation in the final analyzed sample.
The HRQoL was compared, using the EQ-5D-5L questionnaire, between pregnant and non-pregnant women matched for socioeconomic characteristics. Among them 44.1% (case) and 51.2% (control) were aged between 25 and 34 years, 73% (case) and 72.3% (control) living in urban area, 42.6% (case and control) had Middle/High school education level, 92.6% (case) and 92% (control) were unemployed, 95.6% (case) and 89.3% (control) were married, and 50% (case) and 45.7% (control) had a low socioeconomic level (Table 1).
Table 1.
Characteristics of pregnant and non-pregnant women (n = 270 vs n = 289).
| Characteristics | Pregnant women frequency (%) | Non-pregnant women frequency (%) | p-value |
|---|---|---|---|
| Age (years) | 0.274 | ||
| 15–24 | 108 (40) | 96 (33.2) | |
| 25–34 | 119 (44.1) | 148 (51.2) | |
| 35–49 | 43 (15.9) | 45 (15.6) | |
| Place of residence | 0.865 | ||
| Urban | 197 (73) | 209 (72.3) | |
| Rural | 73 (27) | 80 (27.7) | |
| Education | 0.453 | ||
| Illiterate | 39 (14.4) | 48 (16.6) | |
| Primary | 95 (35.2) | 100 (34.6) | |
| Middle/High school | 115 (42.6) | 123 (42.6) | |
| University | 21 (7.8) | 18 (6.2) | |
| Employment | 0.807 | ||
| No | 250 (92.6) | 266 (92.0) | |
| Yes | 20 (7.4) | 23 (8.0) | |
| Marital status | 0.062 | ||
| Single | 6 (2.2) | 10 (3.5) | |
| Married | 258 (95.6) | 258 (89.3) | |
| Widow | 2 (0.7) | 7 (2.4) | |
| Divorced | 4 (1.5) | 14 (4.8) | |
| Socioeconomic level | 0.327 | ||
| Low | 135 (50.0) | 132 (45.7) | |
| Intermediate | 105 (38.9) | 121 (41.9) | |
| High | 30 (11.1) | 36 (12.5) | |
| Gestational age | |||
| First trimester | 60 (22.2) | __ | __ |
| Second trimester | 114 (42.2) | __ | __ |
| Third trimester | 96 (35.5) | __ | __ |
| Parity | |||
| Nullipara | 61 (22.6) | ||
| Primipara | 101 (37.4) | __ | __ |
| Multipara | 108 (40.0) | __ | __ |
| Complications during pregnancy | |||
| Yes | 25 (9.3) | __ | __ |
| No | 245 (90.7) | __ | __ |
| Prenatal consultations | |||
| Assiduous | 257 (95.2) | __ | __ |
| Not assiduous | 13 (4.8) | __ | __ |
Assiduous: Pregnant women who have at least one antenatal consultation.
Regarding pregnant women's obstetrical characteristics, 42.2% were in the second trimester, 40% were multiparous, 90.7% had no complications during pregnancy, and 95.2% had antenatal consultations (Table 1).
Health-related quality of life
To evaluate the impact of pregnancy on the HRQoL, the collected data from 270 pregnant women were compared to a dataset of 289 non-pregnant women using the EQ-5D-5L instrument.
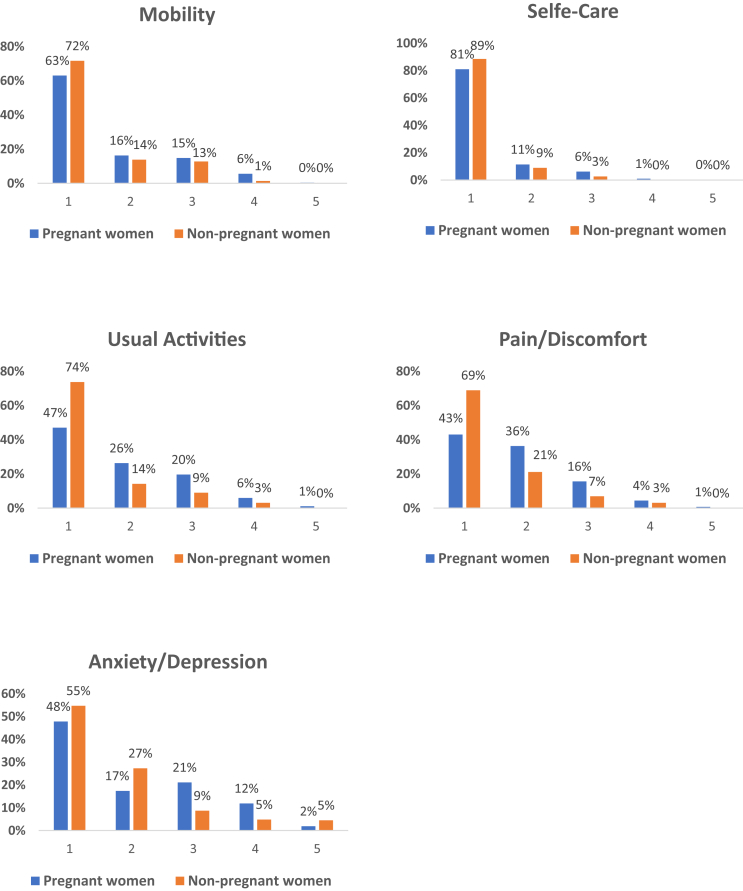
Our results demonstrated that there was a significant difference between pregnant and non-pregnant women for all the EQ-5D-5L health dimensions (p < 0.0001). In effect, pregnant women reported having more problems in mobility (37%), self-care (18%) and usual activities (53%) dimensions compared to non-pregnant women (28%, 12% and 26.2%, respectively). In addition, pregnant women were observed to have more pain/discomfort (57%) than non-pregnant women (31%). Furthermore, the anxiety/depression dimension was affected by pregnancy. In fact, the percentage of participants who reported having anxiety/depression was 52% in pregnant women compared to 46% in non-pregnant women (Fig. 1).
Fig. 1.
Profile of health-related quality of life among pregnant women and non-pregnant women. It represents the comparison between the percentages of pregnant (blue) and non-pregnant women (orange) by levels of severity (1–5) in each dimension.
Among 270 pregnant women's responses, there was 16.2% that reported to have a good health corresponding to the response pattern ‘11111’, which means these participants had no problems on all five dimensions. Regarding EQ-VAS the participants with the best possible health state (100) were 34 (12.59%).
The comparison of the EQ-5D index and EQ-VAS results showed that the EQ-5D index of pregnant women was lower than non-pregnant women 0.71 ± 0.24 and 0.79 ± 0.29, respectively (p < 0.0001), and the EQ-VAS score was 72 ± 23 and 80.2 ± 16.89, respectively (p < 0.0001).
To understand the difference between EQ-5D index of pregnant and non-pregnant women, we compared each EQ-5D-5L dimension separately using the Improved RIDIT approach (Table 2). There was a significant impact of the pregnancy on all EQ-5D-5L dimensions. The high values of ARI were observed for usual activities (ARI = 27.3%) and pain/discomfort (ARI = 26.5%) dimensions, which means that pregnancy increased by 27.3% the problems of doing usual activities, and increased pain/discomfort by 26.5%. The anxiety/depression, mobility, and self-care dimensions were less affected during pregnancy. Indeed, pregnant women were OddsOrdinal = 1.44 times more anxious/depressive (ARI = 12%) and had OddsOrdinal = 1.35 times and OddsOrdinal = 1.47 times of problems in mobility (ARI = 9.7%) and self-care (ARI = 8%) than non-pregnant women (Table 2).
Table 2.
Improved RIDIT analysis of the EQ-5D-5L HRQoL dimensions of pregnant and non-pregnant women (n = 559).
| EQ-5D dimension | ARI% [CImin%–CImax%] | OddsOrdinal [CImin–CImax] | p-value |
|---|---|---|---|
| Mobility | 9.7 [1.7–17.6] | 1.47 [1.11–1.93] | 0.02344 s |
| Self-care | 8.0 [2.0–14.0] | 1.35 [1.14–1.56] | 0.01365 s |
| Usual activities | 27.3 [18.9–35.7] | 2.68 [2.14–3.36] | <0.0001 s |
| Pain/Discomfort | 26.5 [18–35.1] | 2.51 [2.0–3.14] | <0.0001 s |
| Anxiety/Depression | 12.0 [3.2–20.9] | 1.44 [1.09–1.89] | 0.0112 s |
RIDIT: Relative to an Identified Distribution; EQ-5D-5L: EuroQol five dimensions five levels; HRQoL: Health-related Quality of Life; ARI: Absolute Risk Increase; CI: Confidence interval; s: significant after Holm-Bonferroni correction; ns: not significant after Holm-Bonferroni correction.
HRQoL associated factors
Determinants of HRQoL of pregnant women were illustrated in Table 3. The data showed no significant impact of age, marital status, education level, occupation, socioeconomic level, complications during pregnancy, and antenatal consultations on the participants’ HRQoL. However, the place of residence, gestational age, and parity were significantly associated with EQ-5D scores p < 0.0001, p < 0.0001, and p < 0.0001 respectively. The rural pregnant women had the worst HRQoL (EQ-5D index score = 0.57) compared to their urban peers (EQ-5D index score = 0.77), likewise, women in the third trimester and nulliparous had the worst HRQoL, (EQ-5D index score = 0.64 and 0.84 respectively). In addition, the EQ-5D VAS is only associated with gestational age. Women in the third trimester had the worst HRQoL (EQ-VAS = 69.42, p = 0.035) (Table 3).
Table 3.
Association between the HRQoL and the socio-demographic and clinical characteristics of pregnant women, 2019 (n = 270).
| Characteristic | EQ-5D index mean (SD) | p-value | EQ-5D VAS mean (SD) | p-value |
|---|---|---|---|---|
| Age | 0.840 | 0.708 | ||
| 15–24 | 0.71 (0.23) | 71.62 (21.88) | ||
| 25–34 | 0.72 (0.25) | 73.23 (23.56) | ||
| 34–49 | 0.73 (0.22) | 70.00 (24.59) | ||
| Marital status | 0.697 | 0.938 | ||
| Single | 0.66 (0.22) | 71.67 (25.62) | ||
| Married | 0.72 (0.24) | 72.05 (22.98) | ||
| Widow | 0.85 (0.08) | 65.00 (49.50) | ||
| Divorced | 0.63 (0.08) | 77.50 (17.08) | ||
| Home | <0.0001 | 0.302 | ||
| Urban | 0.77 (0.21) | 71.19 (23.79) | ||
| Rural | 0.57 (0.24) | 74.45 (20.77) | ||
| Education | 0.201 | 0.206 | ||
| Illiterate | 0.66 (0.24) | 70.51 (23.42) | ||
| Primary | 0.70 (0.23) | 74.47 (21.82) | ||
| Secondary | 0.74 (0.23) | 69.39 (23.58) | ||
| University | 0.76 (0.27) | 78.81 (23.55) | ||
| Occupation | 0.131 | 0.057 | ||
| Employed | 0.79 (0.24) | 79.50 (16.69) | ||
| Unemployed | 0.71 (0.24) | 71.48 (23.37) | ||
| Socioeconomic level | 0.449 | 0.363 | ||
| Low | 0.73 (0.24) | 72.85 (22.99) | ||
| Intermediate | 0.70 (0.24) | 69.90 (23.73) | ||
| High | 0.68 (0.19) | 76.17 (20.41) | ||
| Gestational age | <0.0001a | 0.035a | ||
| 1st trimester | 0.86 (0.14) | 78.29 (26.62) | ||
| 2nd trimester | 0.84 (0.18) | 75.85 (21.05) | ||
| 3rd Trimester | 0.64 (0.24) | 69.42 (22.50) | ||
| Parity | <0.0001b | 0.153 | ||
| Nullipara | 0.84 (0.15) | 77.05 (21.69) | ||
| Primipara | 0.68 (0.25) | 71.09 (24.40) | ||
| Multipara | 0.68 (0.25) | 70.18 (22.21) | ||
| Complications during pregnancy | 0.321 | 0.181 | ||
| No | 0.72 (0.24) | 72.67 (22.76) | ||
| Yes | 0.67 (0.24) | 66.20 (25.14) | ||
| ANC | 0.290 | 0.684 | ||
| Assiduous | 0.72 (0.23) | 71.94 (23.06) | ||
| Not assiduous | 0.65 (0.28) | 74.61 (22.95) |
HRQoL: Health-related quality of life; EQ-5D: EuroQol five dimensions; VAS: Visual Analogue Scale; SD: Standard Deviation; ANC: Antenatal Consultation; Assiduous: Pregnant women who have at least one antenatal consultation.
p-values ≤ 0.05 are presented in bold font.
3rd Trimester.
Nullipara.
The factors associated with HRQoL were analyzed using the linear regression model with a quality indicator R2 = 0.79, p = 0.0001, this model showed that HRQoL (EQ-5D Index) decreases by 0.262 units in rural-dwelling women, by 0.308 units from the first to the third trimester and by 0.126 units when the parity increases according to the linear equation:
The standards coefficients of the multilinear regression were negative values, which means that place of residence, gestational age and parity affected negatively the HRQoL of pregnant women. Indeed, gestational age contributed by 30.8% to lower the HRQoL, as well as place of residence by 26.2%, and parity by 12.6%.
Deep analysis of effect of gestational age on HRQoL
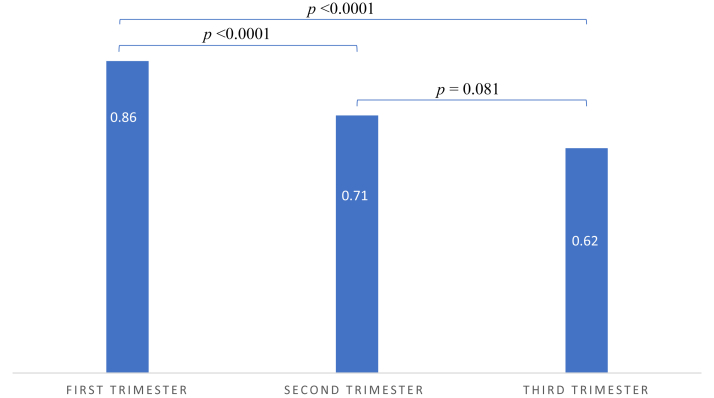
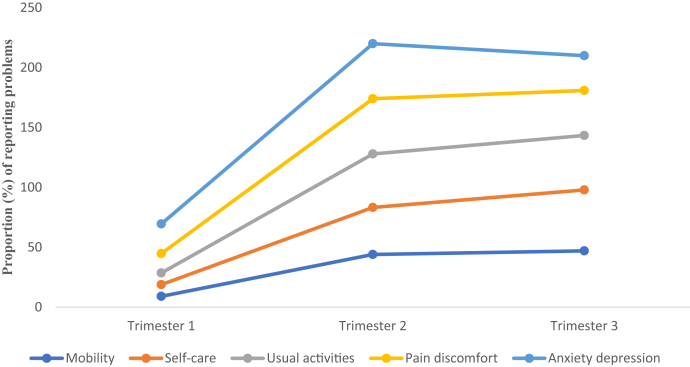
The fluctuations of the EQ-5D index value with gestational age are shown in Fig. 2. The EQ-5D index value decreases with from the first to the third trimester which means that HRQoL decreases with gestational age. We analyzed the distributions of pregnant women's responses according to each dimension separately. As shown in Fig. 3, the proportion of women reporting problems with mobility, self-care, and usual activity increases significantly with gestational age. At the same time, the proportion of women reporting problems with pain/discomfort and anxiety/depression increases from the first to the second trimester and then decreases in the third trimester.
Fig. 2.
Fluctuation of the EQ-5D index value according to gestational age. The EQ-5D index value decreases significantly from the first to the second trimester and from the second to the third trimester (p < 0.0001 and p = 0.081 respectively). EQ-5D: EuroQol five dimensions.
Fig. 3.
Profile of the proportion (%) with problems by dimension and gestational age. The proportion of women reporting problems in mobility, self-care, usual activity, pain/discomfort, and anxiety/depression increased significantly from the 1st trimester to the 2nd trimester and then increased again slightly to the third trimester, except for anxiety/depression which decreased from the 2nd to the 3rd trimester.
In order to more understand the effect of gestational age on HRQoL, we used the RIDIT analysis to assess this effect. The results of the improved RIDIT approach showed a significant impact of the gestational age on all EQ-5D-5L dimensions except anxiety and depression. Indeed, the HRQoL decreased significantly from the first to the third trimester of pregnancy. Mobility was the most affected dimension (ARI = 34% [19–54], p < 0.001) between the first and third trimester followed by usual activities (ARI = 29% [12–46], p = 0.0015), pain/discomfort (ARI = 22% [5–40], p = 0.014), and the self-care (ARI = 12% [2–22], p = 0.025) (Table 4).
Table 4.
Improved RIDIT analysis of the EQ-5D-5L HRQoL dimensions of pregnant by trimesters (n = 270).
| EQ-5D dimension | Trimester (T) | ARI% [CImin%–CImax%] | OddsOrdinal [CImin–CImax] | p-value |
|---|---|---|---|---|
| Mobility | T1/T2 | 23 [9–36] | 4.36 [2.82–6.73] | 0.0016 |
| T1/T3 | 34 [19–54] | 6.79 [4.37–10.53] | <0.0001 | |
| T2/T3 | 16 [3–30] | 1.85 [1.16–2.93] | 0.02 | |
| Self-care | T1/T2 | 6 [−2 to 14] | 2.95 [1.52–5.73] | 0.13 |
| T1/T3 | 12 [2–22] | 5.01 [2.83–8.87] | 0.025 | |
| T2/T3 | 6.1 [−2 to 15] | 1.74 [0.97–3.12] | 0.16 | |
| Usual activities | T1/T2 | 12 [−4 to 28] | 1.52 [0.94–2.45] | 0.14 |
| T1/T3 | 29 [12–46] | 2.62 [1.64–4.18] | 0.0015 | |
| T2/T3 | 19 [4–33] | 1.79 [1.14–2.79] | 0.014 | |
| Pain/Discomfort | T1/T2 | 24 [7–41] | 2.26 [1.43–3.56] | 0.008 |
| T1/T3 | 22 [5–4] | 2.11 [1.29–3.43] | 0.014 | |
| T2/T3 | 0.8 [−0.14 to 0.16] | 1.02 [0.56–1.86] | 0.39 | |
| Anxiety/Depression | T1/T2 | 2 [−0.19 to 0.15] | 1.05 [0.54–2.08] | 0.38 |
| T1/T3 | 14 [−0.03 to 0.31] | 0.67 [0.17–2.54] | 0.11 | |
| T2/T3 | 0.14 [−0.006 to 0.28] | 0.66 [0.22–1.92] | 0.07 |
RIDIT: Relative to an Identified Distribution; EQ-5D-5L: EuroQol five dimensions five levels; HRQoL: Health-related Quality of Life; ARI: absolute risk increase; CI: Confidence interval.
p-values ≤ 0.05 are presented in bold font.
Discussion
Using the EQ-5D-5L instrument, this retrospective study aimed to highlight the evolution of the HRQoL of Moroccan pregnant women throughout pregnancy and according to gestational age, as well as the socioeconomic and obstetrical factors that influence it. The primary findings were that pregnancy can negatively impact women's HRQoL, even in the case of a normal pregnancy, which is expressed by a lower EQ-5D index and EQ-5D-VAS. Furthermore, pregnant women showed the lowest EQ-5D index and EQ-5D-VAS scores in their third gestational trimester.
To our knowledge, no study has been conducted to date to assess the HRQoL of pregnant women in Morocco. The major strength of our study is its focus on HRQoL in pregnant women of different gestational ages, with a particular emphasis on comparisons across the different trimesters.
Different variables contribute to a global understanding of pregnant women's HRQoL. However, only healthy expectant women were included in the study. Therefore, the results cannot be generalized to women with any major health issues who have different levels of HRQoL. Also, prospective research would be perfect for comparing the quality of life between trimesters. This would entail delivering the questionnaire to the same women three times in the first, second, and third trimesters of pregnancy. That way, we could compare the same group of women during each pregnancy phase, and the results would be more reliable.
According to our results, the EQ-5D-5L index and the EQ-VAS were low in pregnant women than in non-pregnant women, which means that the HRQoL decreased during pregnancy. Using the RIDIT method, we noticed that pregnancy significantly decreases the mobility, usual activity, and self-care dimensions, and increases the risk of pain and discomfort, as well as anxiety and depression. It can be explained by the numerous biochemical, physiological, and anatomical changes which occur during this period. These results are comparable to those reported in other countries like Australia and Turkey.6,13 However, in Slovac Republic, Pakistan, and Greece the HRQoL during pregnancy has proven to be good and excellent.14, 15, 16
In agreement with Moghaddam Hosseini et al. (2021), socio-demographic factors (age, marital status, educational level, and occupation) were unrelated to the HRQoL.17 Likewise, socioeconomic level,18 complications during pregnancy, and antenatal care visits were not associated with the HRQoL during pregnancy. On the other hand, some researchers found lower HRQoL during pregnancy in advanced maternal age,19 in unmarried women,16,20 and in women with low educational levels.21
Like the majority of HRQoL studies conducted during pregnancy, we found that gestational age was a negative predictor of overall HRQoL.18,22, 23, 24, 25 Our findings are also consistent with the results of Morin et al. (2019) in France, where they examined the HRQoL at each month of gestation and concluded that it decreased significantly over time during pregnancy.26 Conversely, Vachkova et al. and Alzbon et al. highlighted in their studies that there was no difference in HRQoL amongst women in different trimesters.27,28
There was a correlation between the HRQoL dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression) and gestational trimesters. Similar findings were observed in international researches, mainly in physical health,9,26,29, 30, 31, 32 mental health,26,27,31 and social functioning.9,24,29 In our population, as the gestational age increased, the level of HRQoL problems simultaneously increased in mobility, self-care, and usual activities. Except for the risk of pain/discomfort dimension, which decreased slightly in the 3rd trimester, as well as the risk of anxiety/depression which also declined at the end of pregnancy. The woman's anxiety early in pregnancy might be explained by a cultural factor which is that a woman in her first trimester would tend to conceal her pregnancy until she is noticeably pregnant. This is due to the belief that if people find out about her pregnancy she would be “bewitched” or lose her baby. This cultural belief is not common only in Morocco, but in many countries. A very recent study conducted in Asante Akim Agogo, Ghana, found that fear of miscarriage as a result of bewitchment drove pregnant women to use confinement, which has implications for the early commencement of antenatal consultations.33 Also, in a study conducted in Ntcheu district, Malawi, Chimatiro & et al. found that pregnant women have beliefs regarding witch craft, so they hide their pregnancies in early months, which contributed to low antenatal consultations.34 In Cape Coast, Ghana, depressive symptoms were shown to be very frequent during pregnancy; and, similarly to our findings, this prevalence estimate declined throughout the third trimester.35 In France, the degree of anxiety/depression was also high but remained steady throughout the pregnancy.26 These results point out the importance of the antenatal care in accordance with the gestational age, in order to develop an adapted health promotion program, as well as the importance of HRQoL measurements by trimester.
In this study, urban women had higher HRQoL than rural women. No agreement exists in the literature on how HRQoL differs between rural and urban areas. Several researchers suggest that living in cities is more stressful, resulting in a higher prevalence of anxiety, depression, and other mental health issues.36,37 Other scholars have stated that rural communities are more likely to lack access to infrastructure and to be less educated, which makes it more probable that these groups will have worse HRQoL.38,39
In comparison by parity, a previous study found that nulliparous had significantly experienced poorer HRQoL compared to multiparous women.17 Further study showed that parity was not associated with the HRQoL during pregnancy.18 Contrarily, research in the literature that support the findings of our study demonstrate that pregnant women who are having their first pregnancy have best HRQoL, whereas pregnant women with high parity have worse HRQoL.5,21 These results can be explained by the influence of previous experiences of childbirth and the delivery mode40 and the increased responsibilities and delay in seeking care in multiparous women. In addition, high-parity women may use antenatal health services less frequently than low-parity women do.41
Finally, the factors explored in our study showed a significant impact of the home area, gestational age, and parity on the pregnant women's HRQoL. The results of this study provide the first database of the EQ-5D-5L questionnaire on the HRQoL in pregnant women and will help further studies on this subject. Obtaining information on the pregnant women's profiles is essential to carry out actions to promote their health and also to ensure a healthy pregnancy for the pregnant woman and her child. In the context of community medicine, when developing therapy programs or planned interventions for pregnant women, authorities and health professionals should keep the highlighted factors in mind. Despite the favorable results, it is necessary to evaluate pregnant women's health-related quality of life and to provide specific care to pregnant women with lower HRQoL.
Contributors
Conceptualization, A.B., S.C. and I.Y.-M.; methodology, A.B., S.C., A.M. and I.Y.- M.; formal analysis, A.M., A.A., E.S. and A.B.; investigation, A.B., S.C. and A.M.; data curation, A.B., S.C. and I.Y.-M.; writing—original draft preparation, A.B. and A.M.; writing—review and editing, A.B., A.A., I.Y.-M. and A.M.; visualization, A.H. and E.S.; supervision, A.M., and A.H.; project administration, I.Y.-M.; All authors had full access to all data and have read and agreed to the published version of the manuscript.
Data sharing statement
De-identified study data will be made available upon request following publication and ending three years following article publication to researchers by request to the corresponding author and at the discretion of the research team.
Declaration of interests
We declare no competing interest.
Acknowledgements
We sincerely thank the pregnant women who participated in the study, all health professionals at Settat city for their valuable support, Hassan First University, and the health delegation of the Casablanca-Settat region for granting us permission to conduct the study.
References
- 1.Armstrong D., Caldwell D. Origins of the concept of quality of life in health care: a rhetorical solution to a political problem. Soc Theory Health. 2004;2(4):361–371. [Google Scholar]
- 2.Benamouzig D. Mesures de qualité de vie en santé. Un processus social de subjectivation? Les Cahiers du Centre Georges Canguilhem. 2010;4(1):135–176. [Google Scholar]
- 3.The World Health Organization Quality of Life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41(10):1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 4.Davis-Floyd R. The technocratic, humanistic, and holistic paradigms of childbirth. Int J Gynecol Obstet. 2001;75(S1):S5–S23. doi: 10.1016/S0020-7292(01)00510-0. [DOI] [PubMed] [Google Scholar]
- 5.Boutib A., Chergaoui S., Marfak A., Hilali A., Youlyouz-Marfak I. Quality of life during pregnancy from 2011 to 2021: systematic review. Int J Womens Health. 2022;14:975–1005. doi: 10.2147/IJWH.S361643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Emmanuel E., St John W., Sun J. Relationship between social support and quality of life in childbearing women during the perinatal period. J Obstet Gynecol Neonatal Nurs. 2012;41(6):E62–E70. doi: 10.1111/j.1552-6909.2012.01400.x. [DOI] [PubMed] [Google Scholar]
- 7.HAUTE AUTORITE DE SANTE . Economique et de Santé Publique; 2018. Évaluation des technologies de santé à la HAS : place de la qualité de vie. Direction de l’Evaluation Médicale. [Google Scholar]
- 8.Jomeen J., Martin C. Perinatal quality of life: is it important for childbearing women? Pract Midwife. 2012;15(4):30–34. [PubMed] [Google Scholar]
- 9.Nascimento S.L., Surita F.G., Parpinelli M.Â., Siani S., Pinto e Silva J.L. The effect of an antenatal physical exercise programme on maternal/perinatal outcomes and quality of life in overweight and obese pregnant women: a randomised clinical trial. BJOG. 2011;118(12):1455–1463. doi: 10.1111/j.1471-0528.2011.03084.x. [DOI] [PubMed] [Google Scholar]
- 10.Khoudri I., Belayachi J., Dendane T., et al. Measuring quality of life after intensive care using the Arabic version for Morocco of the EuroQol 5 dimensions. BMC Res Notes. 2012;5:56. doi: 10.1186/1756-0500-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.EQ-5D-5L – EQ-5D [Internet] https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/ [cited 2022 May 24]. Available from:
- 12.Marfak A., Youlyouz-Marfak I., El Achhab Y., et al. Improved RIDIT statistic approach provides more intuitive and informative interpretation of EQ-5D data. Health Qual Life Outcomes. 2020;18(1):63. doi: 10.1186/s12955-020-01313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sut H.K., Asci O., Topac N. Sleep quality and health-related quality of life in pregnancy. J Perinat Neonatal Nurs. 2016;34(4):302–309. doi: 10.1097/JPN.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 14.Mazúchová L., Kelčíková S., Dubovická Z. Measuring women's quality of life during pregnancy. Kontakt. 2018 Mar 1;20(1):e31–e36. [Google Scholar]
- 15.Ishaq R., Shoaib M., Baloch N.S., et al. Profile and predictors of maternal quality of life during physiological pregnancy: a cross-sectional analysis. Front Public Health. 2022;9 doi: 10.3389/fpubh.2021.801035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saridi M., Toska A., Latsou D., Chondropoulou M.A., Matsioula A., Sarafis P. Assessment of quality of life and psycho-emotional burden in pregnant women in Greece. Eur J Midwifery. 2022;6(March):1–7. doi: 10.18332/ejm/145963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MoghaddamHosseini V., Gyuró M., Makai A., Varga K., Hashemian M., Várnagy Á. Prenatal health-related quality of life assessment among Hungarian pregnant women using PROMIS-43. Clin Epidemiol Global Health. 2021;9:237–244. [Google Scholar]
- 18.Altazan A.D., Redman L.M., Burton J.H., et al. Mood and quality of life changes in pregnancy and postpartum and the effect of a behavioral intervention targeting excess gestational weight gain in women with overweight and obesity: a parallel-arm randomized controlled pilot trial. BMC Pregnancy Childbirth. 2019;19(1):50. doi: 10.1186/s12884-019-2196-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu J., Wang S., Leng J., et al. Impacts of gestational diabetes on quality of life in Chinese pregnant women in urban Tianjin, China. Primary Care Diabetes. 2020;14(5):425–430. doi: 10.1016/j.pcd.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Hitimana R., Lindholm L., Krantz G., et al. Health-related quality of life determinants among Rwandan women after delivery: does antenatal care utilization matter? A cross-sectional study. J Health Popul Nutr. 2018;37(1):12. doi: 10.1186/s41043-018-0142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dağlar G., Bi̇lgi̇ç D., Özkan S.A. Factors affecting the quality of life among pregnant women during third trimester of pregnancy. Cukurova Med J. 2019;44(3):772–781. [Google Scholar]
- 22.Sahrakorpi N., Rönö K., Koivusalo S.B., Stach-Lempinen B., Eriksson J.G., Roine R.P. Effect of lifestyle counselling on health-related quality of life in women at high risk for gestational diabetes. Eur J Public Health. 2019;29(3):408–412. doi: 10.1093/eurpub/cky248. [DOI] [PubMed] [Google Scholar]
- 23.Ming W.K., Wu H., Wu Y., et al. Health-related quality of life in pregnancy with uterine fibroid: a cross-sectional study in China. Health Qual Life Outcomes. 2019;17(1):89. doi: 10.1186/s12955-019-1153-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen Y.H., Huang J.P., Au H.K., Chen Y.H. High risk of depression, anxiety, and poor quality of life among experienced fathers, but not mothers: a prospective longitudinal study. J Affect Disord. 2019;242:39–47. doi: 10.1016/j.jad.2018.08.042. [DOI] [PubMed] [Google Scholar]
- 25.Zarei S., Mirghafourvand M., Mohammad-Alizadeh-Charandabi S., Effati- Daryani F., Shiri-Sarand F. Predictors of quality of life in pregnant women visiting health centers of Tabriz, Iran [Internet] JMRH. 2018 doi: 10.22038/jmrh.2018.10378. [cited 2020 Jun 17];(Online First). [DOI] [Google Scholar]
- 26.Morin M., Claris O., Dussart C., et al. Health-related quality of life during pregnancy: a repeated measures study of changes from the first trimester to birth. Acta Obstet Gynecol Scand. 2019;98(10):1282–1291. doi: 10.1111/aogs.13624. [DOI] [PubMed] [Google Scholar]
- 27.Vachkova E., Jezek S., Mares J., Moravcova M. The evaluation of the psychometric properties of a specific quality of life questionnaire for physiological pregnancy. Health Qual Life Outcomes. 2013;11(1):214. doi: 10.1186/1477-7525-11-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alzboon G., Vural G. Factors influencing the quality of life of healthy pregnant women in North Jordan. Medicina. 2019;55(6):278. doi: 10.3390/medicina55060278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chang S.R., Chen K.H., Lin M.I., Lin H.H., Huang L.H., Lin W.A. A repeated measures study of changes in health-related quality of life during pregnancy and the relationship with obstetric factors. J Adv Nurs. 2014;70(10):2245–2256. doi: 10.1111/jan.12374. [DOI] [PubMed] [Google Scholar]
- 30.Moccellin A.S., Driusso P. Adjustments in static and dynamic postural control during pregnancy and their relationship with quality of life: a descriptive study. Fisioterapia. 2012;34(5):196–202. [Google Scholar]
- 31.Lau Y. The effect of maternal stress and health-related quality of life on birth outcomes among Macao Chinese pregnant women. J Perinat Neonatal Nurs. 2013;27(1):14–24. doi: 10.1097/JPN.0b013e31824473b9. [DOI] [PubMed] [Google Scholar]
- 32.Dodd J.M., Newman A., Moran L.J., et al. The effect of antenatal dietary and lifestyle advice for women who are overweight or obese on emotional well-being: the LIMIT randomized trial. Acta Obstet Gynecol Scand. 2016;95(3):309–318. doi: 10.1111/aogs.12832. [DOI] [PubMed] [Google Scholar]
- 33.Ansong J., Asampong E., Adongo P.B. Socio-cultural beliefs and practices during pregnancy, child birth, and postnatal period: a qualitative study in Southern Ghana. Cogent Public Health. 2022;9(1) [Google Scholar]
- 34.Chimatiro C.S., Hajison P., Chipeta E., Muula A.S. Understanding barriers preventing pregnant women from starting antenatal clinic in the first trimester of pregnancy in Ntcheu District-Malawi. Reprod Health. 2018;15(1):158. doi: 10.1186/s12978-018-0605-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pobee R.A., Setorglo J., Kwashie Klevor M., Murray-Kolb L.E. High levels of depressive symptoms and low quality of life are reported during pregnancy in Cape Coast, Ghana; a longitudinal study. BMC Public Health. 2022;22(1):894. doi: 10.1186/s12889-022-13299-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maia I.J.F., Marrone L.C.P., Martins M.I.M. Comparação entre a qualidade de vida, ansiedade e depressão de gestantes que vivem em zona rural e urbana em um município da Amazônia Brasileira. Res Soc Dev. 2022;11(1) [Google Scholar]
- 37.Hassan Tawfik E. Knowledge, practice and quality of life (QOL) of pregnant women: a comparison between urban and rural populations [Internet] 2020. https://papers.ssrn.com/abstract=3582231 Rochester, NY; [cited 2022 Jul 22]. Available from:
- 38.Arute J.E., Eniojukan J.F., Odili V.O. Quality of life in pregnant women attending anti-natal clinics in rural and urban areas of delta state. Value Health. 2014;17(7):A518. doi: 10.1016/j.jval.2014.08.1612. [DOI] [PubMed] [Google Scholar]
- 39.Naseem K., Khurshid S., Khan S.F., et al. Health related quality of life in pregnant women: a comparison between urban and rural populations. J Pak Med Assoc. 2011;61(3):5. [PubMed] [Google Scholar]
- 40.Ďuríčeková B., Škodová Z., Bašková M. Mode of delivery preferences among multiparous women based on previous birth experience. Cent Eur J Nurs Midw. 2021;12(4):545–554. [Google Scholar]
- 41.Alkhaldi S.M. Predictors of antenatal care utilization in Jordan: findings from a National Survey. Jordan Med J. 2016;171(3708):1–11. [Google Scholar]