Highlights
-
•
Professional interpreters result in best quality of care for patients.
-
•
Relational interpreters can provide valuable insights.
-
•
Further differentiation of interpreter types and their effect on outcome not possible.
Keywords: Interpreter services, Language interpretation, Medical setting, Language barrier, Communication, Patient outcomes
Abstract
Background
Utilization of interpreters to facilitate communication between health care providers and non-native speaking patients is essential to provide the best possible quality of care. Yet use and policy on the subject vary widely, as does knowledge on the effect of different types of interpreters. This paper systematically reviews the literature on use of interpreters in the medical setting to evaluate their effects on the quality of care.
Material and methods
We conducted a literature search of PubMed and Embase, supplemented with references from relevant previous literature. We included any report in a medical setting comparing one type of interpretation to any other, including no interpretation and measuring a patient outcome. No limit was set on time or language. Risk of bias was assessed using the Evidence Project Risk of Bias assessment tool and the CASP checklist for qualitative studies. Results were synthesized using REDCap and presented in tables.
Results
We identified 29 reports represented by five types of studies. Types of interpreter intervention examined were professional, ad hoc, relational, any and no interpreter. Outcomes measured were satisfaction, communication, utilization and clinical outcomes. Results were indicative of in-person professional interpreter resulting in highest satisfaction and communication, reaffirming that any interpreter is better than none and relational interpreters can be a valuable interpreter resource for patients in the private practice setting. To be able to further differentiate on outcome for interventions of ad-hoc or relational interpreters, further data is needed.
Discussion
In-person Professional interpreter is the interpreter type resulting in greatest satisfaction and best communication outcome for the patients. This review is limited by most data originating from one country, interpretation from mainly Spanish to English and in one cultural setting.
Funding
No funding was provided for this review.
1. Introduction
In 2018 the Danish government re-instated a law requiring residents in Denmark for more than three years to pay for interpreter services in the Danish healthcare system (Bekendtgørelse, 2018). Concerns have been voiced by healthcare professionals that this will negatively impact the quality of care and increase the cost of treatment for patients in need of interpreter services. Interpretation may thus be done more often by untrained individuals such as relatives and friends, ad hoc bilingual medical staff or not at all (Dungu et al., 2019). The importance of successful communication between provider and patient is well-known (Stewart, 1995). Mismanaged language barriers may potentially exacerbate issues of poor communication and can lead to reduced quality of care for patients (Nam et al., 2011). It was shown prior to implementation of the current law that the use of professional interpreters in Danish health care was lacking and with possible impact on quality of care (Lund Hansen MT 2013). A recent review showed a decrease in use of interpreters since implementation of the law in 2018 (Michaëlis et al., 2021), possibly reducing quality of care for patients in need of interpreter service even further.
Previous reviews show that the use of professional interpreters compared to other modes of interpretation is associated with improved patient outcomes (Karliner et al., 2007; Flores, 2005; Boylen et al., 2020). This review will attempt to update knowledge in this field and further attempt to differentiate between types of interpreters.
Danish and international studies show that there is a substantial variation in the use of interpreters in the hospital and general practitioner settings. Interpreters are not always used or available when needed, and type of interpreter varies (Hansen and Smith, 2013; Bischoff and Hudelson, 2010; Kale and Syed, 2010).
The purpose of this review is to identify the type of interpreter used; professional, ad hoc, relational, any or none and its impact on quality of care. The scope of this review is to assess the utilization and impact of different types of interpreters in healthcare settings. We hypothesized that the type of interpreter used affects the patient outcome. In other words: how does different modes of interpretation affect the treatment outcome for non-native speaking patients?
2. Methods
This paper is structured and conducted in concordance with the PRISMA guidelines for systematic reviews (Liberati et al., 2009) and based on a protocol as outlined in the PRISMA-P guidelines (Shamseer et al., 2015). A protocol was registered on the 7th of April 2021 and published on the 8th of May 2021 and has not been amended. The PROSPERO registration number for this review is: CRD42021247580 and can be accessed on the PROSPERO site.
2.1. Eligibility criteria
Inclusion and exclusion criteria were based on study design, participants, intervention, setting, outcomes, dissemination type and language. A detailed list is available in Appendix A.
Types of interpreters were defined as: (i)professional, including in-person, on-telephone, on-video or remote simultaneous– i.e., Someone paid for their service as a bilingual translator, regardless of the amount of translator training, (ii)ad hoc – i.e., bilingual medical professional or employee, (iii)relational – i.e., family, friend, or acquaintance, or (iv) any interpreter – i.e., unspecified and (v) no interpreter.
Outcomes were selected to represent quality of care. The outcome satisfaction is satisfaction with clinical care and the patients’ overall satisfaction with any part of the clinical care. Communication is comprehension and errors in communication reported both by the patient and by clinical and other staff, as well as those incidents discovered later by review of records. Utilization is utilization of clinical care, i.e., the level to which the patient can access and utilize the care offered. Clinical outcomes are a measure of the effect of the care given; compliance, progression or regression of disease, time spent to receive care, number of follow-up visits, self-reported and reported by staff.
None of the outcomes are prioritized above the other. All are deemed equally relevant to the goal of this review. Studies with outcomes within the four categories presented either qualitatively or quantitatively were included.
2.2. Information sources, searches and study selection
The databases PubMed and Embase were selected for performing database searches. Initial searches for identification of relevant MeSH and Emtree terms were done in the period from 23/3–7/4 2021. To build the searches for the databases, several iterative searches were performed, resulting in the searches seen in appendix B. Three searches were used: two in PubMed, one in Embase. The first in PubMed was using MeSH terms, the second was a similar free text search.
Eligibility assessment was done systematically by the first author, by exporting searches to spreadsheets and manually screening all titles. Next, abstracts were screened followed by full text screening for final inclusion. Reasons for exclusions are shown in results.
2.3. Data abstraction, management and assessing bias
Study data were collected and managed by REDCap electronic data capture tools hosted at Aarhus University (Harris et al., 2009; Harris et al., 2019). The rational for using REDCap for this review was to build a series of databases for continuous data extraction while reports were reviewed. These databases were built by the first author with comments and feedback on the specific data included in each instrument by the other authors. Building of data extraction instruments was an iterative process, where changes were written while data extraction was ongoing. Criteria for what data to collate and collect were those outlined in Section 2.1.
Assessment of bias were done using the Evidence Project Risk of Bias assessment tool (Kennedy et al., 2019) as the studies providing data for this review encompasses different study designs. Included qualitative reports were assessed using the CASP checklist (Skills CA 2018 [) as the recommended tool by recent reviews (Ma et al., 2020). Risk of bias assessment and assessment of qualitative reports were done by the first author.
Due to the different study designs no meta-analysis was done on the abstracted data. Instead, we present the abstracted data and risk of bias in tables as well as a short qualitative analysis of the results. Data for this review is not publicly available. Contact the authors for further information.
3. Results
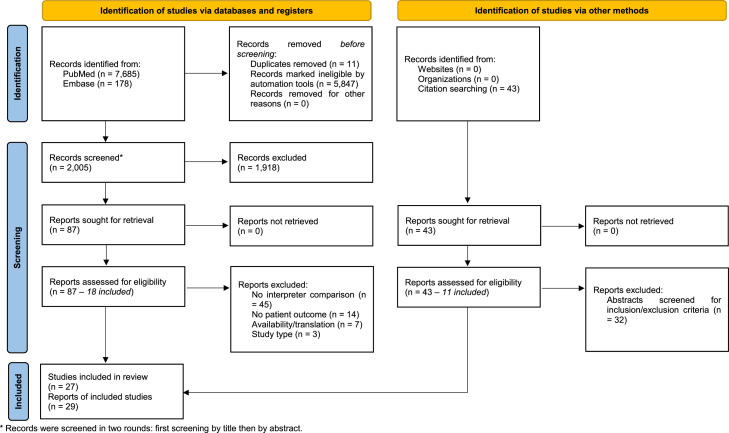
In total, 29 reports from 27 studies were included. Reasons for exclusion were: no comparison between types of interpreter use, no patient outcome, availability / translation, and study type. Searches were done in PubMed and Embase and additional records were identified through references from two previous reviews with a similar scope (Karliner et al., 2007; Flores, 2005). the flow of screening and inclusion/exclusion is outlined in the PRISMA flow diagram in Fig. A.
Fig. A.
PRISMA flow diagram. * Records were screened in two rounds: first screening by title then by abstract.
3.1. Report characteristics
Three of the reports were based on the same study. Baker(1996) (Baker et al., 1996), Baker(1998) (Baker et al., 1998), and Sarver(2000) (Sarver and Baker, 2000). All three reports were included and marked as originating from the same study.
Distribution of study design among the 29 reports were two randomized controlled trials (Bagchi et al., 2011; F Gany et al., 2007), one randomized crossover study (Xue et al., 2019), seven cohort / observational studies (Baker et al., 1996; Baker et al., 1998; Sarver and Baker, 2000; Anttila et al., 2017; Hampers and McNulty, 2002; Jacobs et al., 2007; Lindholm et al., 2012), three retrospective cohort studies (Hartford et al., 2019; López et al., 2015; Luan Erfe et al., 2017), 12 cross-sectional studies (Bernstein et al., 2002; Bischoff et al., 2003; Butow et al., 2011; Fagan et al., 2003; Flores et al., 2012; Flores et al., 2003; Gany et al., 2007; Garcia et al., 2004; Kuo and Fagan, 1999; Lee et al., 2002; Moreno and Morales, 2010; Nápoles et al., 2015) and four qualitative studies (Brooks et al., 2016; Greenhalgh et al., 2006; Hilder et al., 2017; Leanza et al., 2010). Geographical distribution were 23 reports from the USA, two from Australia and one each from Switzerland, New Zealand, Canada and the UK, respectively. Additional characteristics of included reports can be found in Table A.
Table A.
Report characteristics.
| Report | Aim of Study | Intervention comparison (interpreter) | Outcome measure | Study setting | Language(s) | Population (N) |
|---|---|---|---|---|---|---|
| Anttila et al. (2017) | To examine satisfaction and comprehension depending on interpreter type. | Professional to ad hoc Professional to relational Ad hoc to relational | Satisfaction Communication | Hospital | English, Spanish | 124 |
| Kuo et al. (1999) | To describe patient utilization and satisfaction with different types of interpretation. | Professional to ad hoc Professional to relational Ad hoc to relational | Satisfaction | Primary Care Clinic | English, Spanish | 200 |
| Lee et al. (2002) | To compare satisfaction with care for patients communicating with providers in primary language, through different interpreters. | Professional to ad hoc Professional to relational Ad hoc to relational | Satisfaction | Walk-in Clinic | English, Spanish | 536 |
| Flores et al. (2012) | To compare interpreter errors and clinical consequences in encounters with different interpreters. | Professional to ad hoc Professional to none Ad hoc to none | Communication | Emergency department/room | English, Spanish | 57 |
| Bischoff et al. (2003) | To examine language concordance (with / without interpreters) between nurses and asylum seekers. | Professional to ad hoc Professional to none Ad hoc to none | Communication | Refugee reception center | Albanian, Somali, Serbo-Croatian, Arabic, Armenian, Peul, Kurd, Lingala, Tamil, Amharic, Portuguese, French, Spanish, Russian, others | 723 |
| Fagan et al. (2003) | To compare visit lengths of patients using different types of interpreters. | Professional to none Professional to relational Relational to none | Clinical outcome | Hospital | English, Spanish, Russian, Portuguese, Cambodian, others | 613 |
| Baghci et al. (2011) | To examine effect of in-person professional interpreter on patient satisfaction. | Professional to any other | Satisfaction Communication | Emergency department/room | English, Spanish | 447 |
| Hampers et al. (2002) | To compare treatment given to patients using language concordant physician or interpreters. | Professional to any other | Utilization | Emergency department/room | English, Spanish, Polish, Russian, Vietnamese, others | 4146 |
| Jacobs et al. (2007) | To determine if improved interpreter service will reduce number of tests and post discharge events and improve satisfaction for patients. | Professional to any other | Satisfaction Utilization | Hospital | English, Spanish | 323 |
| Flores et al. (2003) | Determine frequency, categories, and potential clinical consequences of errors committed by interpreters and compare quality of interpretation by different interpreters. | Professional to ad hoc | Communication | Outpatient clinic | English, Spanish | 13 |
| Gany et al. (2007)A | To determine accuracy and speed of four different medical interpretation strategies. | Professional to ad hoc | Communication | Hospital | English, Spanish | 16 |
| Gany et al. (2007)B | To evaluate patient satisfaction with RSMI compared to usual modes of interpretation. | Professional to ad hoc | Satisfaction | Primary care clinic and emergency department. | English, Spanish, Mandarin, Cantonese | 1276 |
| Garcia et al. (2004) | To determine whether type of interpreter influences patient satisfaction and communication. | Professional to ad hoc | Satisfaction Communication | Emergency department/room | English, Spanish | 240 |
| Nápoles et al. (2015) | To assess communication and determine patient outcome based on communicative errors when comparing different interpreter types. | Professional to ad hoc | Communication | Hospital | English, Spanish | 32 |
| Butow et al. (2011) | To describe equivalence of messages conveyed by different interpreter types. | Professional to relational | Communication | Hospital | English, Arabic, Chinese, Greek | 32 |
| Xue et al. (2019) | To compare communication by comparing survey results conducted with two different types of interpreters. | Professional to relational | Communication | Post-surgery survey (out-patient clinic) | English, Arabic, Spanish, Chinese, Greek, Macedonian, Italian, Serbian, Vietnamese, Assyrian, Punjabi, Croatian, Farsi, others | 125 |
| Hartford et al. (2019) | To describe patterns of interpreter use, determine factors associated with interpreter use and differences in patient outcomes between LEP and English proficient patients. | Professional to none | Clinical outcome | Emergency department/room | English, Spanish, Mandarin, Cantonese, Vietnamese, Russian, Somali, Amharic, Arabic, Oromo, Tigrinya | 51,826 |
| López et al. (2015) | To examine if hospitalized LEP patients receive interpreter services during stay, and if use of interpreter impacts length of stay. | Professional to none | Clinical outcome Utilization | Hospital | not specified | 4224 |
| Luan Erfe et al. (2017) | To examine if professional medical interpreter had an impact on care provided for acute ischemic stroke patients. | Professional to none | Utilization | Hospital | English, Spanish, Portuguese, French, Haitian Creole, Mandarin, Cantonese, Italian, others | 259 |
| Lindholm et al. (2012) | To examine length of stay and 30-day readmission for LEP patients by access to professional interpretation. | Professional to none | Clinical outcome | Hospital | English, Spanish, Portuguese, Vietnamese, Albanian, Russian, others | 3127 |
| Baker et al. (1996)* | To examine if interpreter use affect accuracy of patients' understanding of diagnosis and treatment plan. | Any to none | Communication | Emergency department/room | English, Spanish | 530 |
| Baker et al. (1998)* | To compare satisfaction with care for patients based on need and use of interpreters. | Any to none | Satisfaction | Emergency department/room | English, Spanish | 467 |
| Bernstein et al. (2002) | To investigate impact of interpreter services on patients’ emergency department visit, utilization and charges. | Professional to none | Utilization | Emergency department/room | English, Spanish, Portuguese Creole, Haitian Creole | 500 |
| Moreno et al. (2010) | To compare satisfaction and communication between patients receiving interpreter services and not. | Any to none | Satisfaction Communication | Medical Clinics | English, Spanish | 1590 |
| Sarver et al. (2000)* | To examine association between language barriers and rates of referral for follow-up, patients’ knowledge of an appointment and compliance. | Any to none | Utilization | Hospital | English, Spanish | 1997 |
| Brooks et al. (2016) | LEP patient narratives to understand patient experiences of inadequately interpreted clinical encounters. | Professional to ad hoc | Satisfaction Communication Clinical Outcome | Any medical encounter in the last six months | English, Spanish | 22 |
| Greenhalgh et al. (2006) | To examine communication between providers, professional and relational interpreters and patients through the theories of J. Harbermas. | Professional to relational | Communication | Interviews with patients, interpreters and physicians. | Albanian, Farsi, French, Gujarati, Turkish, Bengali, Cantonese, Romanian, Somali, Spanish, Arabic, Greek, Urdu | 69 |
| Hilder et al. (2017) | To analyze interactions in consultations between physicians, patients and interpreters. | Professional to relational | Communication | Private practitioner | English, Assyrian, Gujarati, Khmer, Mandarin, Samoan, Somali, Tigrinya/Arabic, Tongan | 16 |
| Leanza et al. (2010) | To compare difference in quality of communication as per J. Habermas in consultations with a different interpreter type. | Professional to relational | Communication | Private practitioner | English, Punjabi, Vietnamese, Bengali, Tamil, Dari | 16 |
*Based on the same study: conducted at Harbor–UCLA Medical Center, a 500-bed public hospital in Torrance, California, USA.
LEP = limited English proficiency, ED = emergency department, RSMI = remote simultaneous medical interpretation.
3.2. Risk of bias in individual reports
The risk of bias in individual reports are shown in Table B. This is a bias assessment for each included report individually.
Table B.
Bias assessment of quantitative & valuation of qualitative reports.
| Report | Is this a Cohort Study? | Does report include a control or comparison group? | Does report include pre/post intervention data? | Did report randomly assign participants to the intervention? | Did report randomly select participants for assessment? | Does report have a follow-up rate of more than 80%? | Comparison groups equivalent on sociodemographics? | Comparison groups equivalent at baseline on outcome measures? | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Anttila et al. (2017) | Yes | Yes | No | No | No | Yes | Yes | NR | ||
| Kuo et al. (1999) | No | Yes | No | No | No | NA | NR | NR | ||
| Lee et al. (2002) | No | Yes | No | No | No | NA | Yes | NR | ||
| Flores et al. (2012) | No | Yes | No | NA | No | NA | NA | Yes | ||
| Bischoff et al. (2003) | No | Yes | No | No | No | NA | NR | NR | ||
| Fagan et al. (2003) | No | Yes | No | No | No | NA | NR | NR | ||
| Baghci et al. (2011) | No | Yes | No | Yes | Yes | Yes | Yes | NR | ||
| Hampers et al. (2002) | Yes | Yes | No | No | No | No | No | Yes | ||
| Jacobs et al. (2007) | Yes | Yes | No | Yes | No | No | Yes | NR | ||
| Flores et al. (2003) | No | Yes | No | No | No | NA | NA | Yes | ||
| Gany et al. (2007)A | No | Yes | No | No | No | NA | NA | NA | ||
| Gany et al. (2007)B | No | Yes | Yes | Yes | Yes | No | Yes | NR | ||
| Garcia et al. (2004) | No | Yes | No | Yes | No | NA | No | NR | ||
| Nápoles et al. (2015) | No | Yes | No | No | No | NA | NR | NR | ||
| Butow et al. (2011) | No | Yes | No | No | No | NA | NR | Yes | ||
| Xue et al. (2019) | Yes | Yes | No | Yes | No | No | Yes | NR | ||
| Hartford et al. (2019) | No | Yes | Yes | No | No | NA | NR | NR | ||
| López et al. (2015) | No | Yes | No | No | No | NA | NR | No | ||
| Luan Erfe et al. (2017) | No | Yes | No | No | No | NA | No | Yes | ||
| Lindholm et al. (2012) | Yes | Yes | No | No | No | Yes | No | Yes | ||
| Baker et al. (1996)* | Yes | Yes | Yes | No | No | No | No | NR | ||
| Baker et al. (1998)* | Yes | Yes | Yes | No | No | No | No | NR | ||
| Bernstein et al. (2002) | No | Yes | No | No | No | NA | Yes | Yes | ||
| Moreno et al. (2010) | No | Yes | No | No | No | NA | NR | NR | ||
| Sarver et al. (2000)* | Yes | Yes | Yes | No | No | No | No | NR | ||
| Report | Was there a clear statement of the aims of the research? | Is a qualitative methodology appropriate? | Was the research design appropriate to address the aims of the research? | Was the recruitment strategy appropriate to the aims of the research? | Was the data collected in a way that addressed the research issue? | Has the relationship between researcher and participants been adequately considered? | Have ethical issues been taken into consideration? | Was the data analysis sufficiently rigorous? | Is there a clear statement of findings? | How valuable is the research? |
| Brooks et al. (2016) | Yes | Yes | Yes | We don't know | We don't know | No | No | Yes | Yes | Less valuable |
| Greenhalgh et al. (2006) | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Highly valuable |
| Hilder et al. (2017) | Yes | Yes | Yes | Yes | Yes | We don't know | No | Yes | Yes | Valuable |
| Leanza et al. (2010) | No | Yes | Yes | We don't know | Yes | No | No | Yes | Yes | Valuable |
Few included reports give explicit information on equivalence of comparison groups on sociodemographics. Most provide some information on demographics. In the report by Baker et al. (1998) interviews for defining baseline outcome – satisfaction with interpretation – was performed, but results are not shown. The remainder of the reports provided no information on outcomes concerning satisfaction or communication at baseline. This is often due to a cross-sectional study design while still grouping participants in different groups for comparison.
The color-coding is to provide a quick overview of the extent of bias in each report, with green, yellow and red corresponding to low, medium and high levels of bias. The four qualitative studies were also color-coded according to valuation using red, yellow and green from lowest to highest valuation.
3.3. Results of individual reports
Results from individual reports is summarized in Table C.
Table C.
Results of individual reports.
| Report | Interventions / Outcomes | Results |
|---|---|---|
| Anttila et al. (2017) | Mode of professional interpreter, relational and ad hoc interpreter / Satisfaction and Communication. | Satisfaction was highest for prof. video interpreter > interpreter trained physician > IPPI > prof. phone interpreter (P = 0.005). Family member and ad hoc not mentioned. Communication was highest with prof. video interpreter > IPPI > interpreter trained physician > family member > prof. phone interpreter simultaneous > ad hoc > prof. phone interpreter later (P = 0.01). |
| Kuo et al. (1999) | Different types of interpreters used / Satisfaction. | Satisfaction with: Professional hospital interpreter was 92.4% (P = 0.17) Relational interpreter was 85.1% (P < 0.01) Telephone interpreter was 53.3% (P < 0.01) Ad hoc (not physician) was 40% (P = 0.05) |
| Lee et al. (2002) | Type of interpreter compared to language concordant patients / Satisfaction. | No significant difference in satisfaction between language concordant and telephone interpreted consultations. Compared to language concordant patients, use of relational and ad hoc interpreters resulted in lower satisfaction: 54% and 49% vs 77%; P < 0.01 and P = 0.007 respectively. |
| Flores et al. (2012) | Professional, ad hoc or no interpreter / Communication. | Proportion of errors of potential clinical consequence (i.e., communication) was lowest for professional interpreter vs ad hoc and no interpreter. 12% vs 22% vs 20%, respectively (P < 0.01). For mean errors per encounter, there was no significant difference. 32.7 (SD 4.9) vs 33.7 (SD 4.7) vs 32.3 (23.9), respectively. |
| Bischoff et al. (2003) | Professional, ad hoc or no interpreter / Communication. | Percentage of patients reporting physical symptoms: With professional interpreter: 25%, ad hoc interpreter: 26%, and no interpreter: 18% (P = 0.079). Percentage reporting psychological symptoms: With professional interpreter: 32%, ad hoc interpreter: 16%, no interpreter: 18% (P = 0.029). |
| Fagan et al. (2003) | Professional, relational or no interpreter / Clinical outcome. | Compared to patients with no interpreter: Professional telephone interpreter resulted in longer provider times (36.3 min vs 28.0 min (P < 0.001)). As did relational interpreter (34.4 min vs 28.0 min (P < 0.001)). In person professional interpreter did not result in significantly different provider times (26.8 min vs 28.0 min (P = 0.51). In multivariate analysis with no interpreter as reference, professional telephone and relational interpreter resulted in longer mean provider times of 8.3 min [95%CI:3.94;12.7] and 4.58 min [95%CI:1.84;7.33], respectively. |
| Baghci et al. (2011) | Professional or any interpreter / Satisfaction and communication. | Satisfaction in treatment group (i.e., professional interpreter) 96% were "very satisfied" vs. 24% in control group (i.e., any interpreter) (OR = 72 [CI:31;167], p = 0.01). Communication in treatment group 93% found understanding "very easy" vs. 18% in control group (OR = 61 [CI:23;166], p = 0.01). |
| Hampers et al. (2002) | Professional or any interpreter compared to controls / Utilization. | When compared to controls, any interpreter had adjusted results on IV use, admissions and testing (i.e., utilization) of: OR 2.2 CI95(1.2,4.3), OR 2.6 CI95(1.4,4.5), OR 1.5 CI(1.04,2.2), respectively. Professional interpreter compared to controls, on the same parameters: OR 1.2 CI95(0.7,2.1), OR 1.7 CI95(1.1,2.8), OR 0.73 CI95(0.56,0.97), respectively. |
| Jacobs et al. (2007) | Professional or any interpreter / Utilization and satisfaction. | No significant differences in outcome for the groups receiving in-person professional interpreter service, compared to the group receiving any interpreter services (i.e., telephone professional, ad hoc, relational, no interpreter). |
| Flores et al. (2003) | Professional or ad hoc interpreter / Communication. | Number of errors with potential clinical consequences were relatively higher for ad hoc than professional interpreters: 77% vs 53% respectively (P < 0.001), i.e. communication higher for professional interpreters. |
| Gany et al. (2007)A | Professional (three modes) or ad hoc interpreter / Communication. | RSMI produced fewer errors than the other modes of interpretation. Mean linguistic errors per utterance 1.139 (SD=1.737) and 0.019 (SD=0.15) medical errors. With the non-RSMI modes of interpretation there was a 12-fold greater rate of medical errors of moderate or greater significance, per utterance (p = 0.002). |
| Gany et al. (2007)B | Professional (RSMI) or ad hoc interpreter with controls / Satisfaction. | RSMI gave significantly higher Satisfaction. Linear regression of satisfaction with physician communication/care: RSMI mean 0.518, SD 0.351 vs usual methods (i.e., ad hoc interpreter) 0.436, SD 0.330, both with P < 0.05. Controls (language concordant) scored significantly higher on all parameters. |
| Garcia et al. (2004) | Professional or ad hoc interpreter compared to controls / Satisfaction and communication. | On a 100-point scale satisfaction was highest for in-person professional interpreter (mean = 79) compared to ad hoc (mean = 72) and telephone professional interpreter (mean = 74), (P < 0.001). Communication was significantly higher for the in-person professional interpreter group (mean = 78) compared to ad hoc (mean = 71) and telephone professional interpreter (mean = 63), (P < 0.001). |
| Nápoles et al. (2015) | Professional or ad hoc interpreter / Communication. | Adjusted odds of inaccurate interpretation were significantly lower for professional in person (OR=−1.25; 95%CI −1.56,−0.95) and video conferencing (OR=−1.05; 95%CI −1.26,−0.84) than for ad hoc interpreter. |
| Butow et al. (2011) | Professional or relational interpreter / Communication. | Equivalence of communication was achieved by professional interpreters 65% of the time and by relational 50% of the time (95%CI:3%−28% for the difference, P = 0.02. |
| Xue et al. (2019) | Professional or relational interpreter / Communication. | Communication presented as concordance on a scale from 0 to 100 divided in intervals. Difference in concordance when comparing professional to relational interpreter was minimal with kappa = 0.69–0.87 and ICCs above 0.74, i.e., gave equal communication results. |
| Hartford et al. (2019) | Professional or no interpreter compared to language concordant patients / Clinical outcome. | Clinical outcome may have been affected negatively for patients with no interpreter, as they had lower chance of ED admittance, but higher risk of ICU admittance within 24 h of first visit, when compared to patients with professional interpreter service or language concordant patients. |
| López et al. (2015) | Professional or no interpreter / Clinical outcome and utilization. | Patients with no interpreter or professional interpreter with a non-physician (i.e., nurse) had significantly shorter stays, OR of 0.80 and 0.77 respectively. There were no significant differences in use of ED and readmission between groups. |
| Luan Erfe et al. (2017) | Professional or no interpreter / Utilization. | Patients with no interpreter were significantly less likely to receive defect-free care (i.e., fully utilized care) compared to with a professional interpreter: 61.5% vs 73.9%, P = 0.04. After accounting for sociodemographics patients with no interpreter were half as likely to receive defect-free care, compared to with a professional interpreter: OR 0.50, 95%CI(0.27–0.90), P = 0.02. |
| Lindholm et al. (2012) | Professional or not interpreter / Clinical outcome. | Length of stay for a patient with professional interpreter at both admission and discharge was 2.57 days while 5.06 days for patients no interpreter (P<0.001). Readmission within 30 days were 24.3% for patients without interpreter present at admission and discharge compared to patients with interpreter present at both 14.9% (P<0.001). |
| Baker et al. (1996)* | Any or no interpreter / Communication. | Communication with any interpreter used: 57% with good-excellent understanding of diagnosis, 43% fair-poor (P<0.001). With interpreter not used: 38% good-excellent understanding of diagnosis, 62% fair-poor (P<0.001). |
| Baker et al. (1998)* | Any or no interpreter / Satisfaction. | On a scale from 0 to 100 patients with an interpreter at visit had an overall satisfaction score of 65 compared to those without interpreter who scored 55 (P<0.001). |
| Bernstein et al. (2002) | Professional or no interpreter with English speaking controls / Utilization. | Patients with no interpreter service provided had less utilization of care than those provided professional interpreter service. Both less than English-speaking patients. (p < 0.05) |
| Moreno et al. (2010) | Any or no interpreter / Satisfaction and communication. | Referenced against patients not needing an interpreter, patients having any interpreter when needed was independently associated with greater satisfaction and communication: 3.65 (SE=1.47) points and 6.04 (SE=1.47) points (P<0.05). Conversely needing an interpreter and not having one showed a decrease in satisfaction and communication: −2.39 (SE=1.15) points and −4.28 (SE=1.42) points (P<0.05). |
| Sarver et al. (2000)* | Any or no interpreter / Utilization. | Referenced to language concordant patients, both patients with interpreter used and not used, were more likely to be discharged without a follow-up appointment. OR 1.92 (1.11;3.33) and 1.79 (1.00;3.23) respectively. P = 0.03. |
| Brooks et al. (2016) | Professional or ad hoc interpreter / Satisfaction, communication and clinical outcome. | Importance of prof. interpreters i.e., ability to relay LEP patients’ medical needs. Barriers to interpretation i.e., time constraints or limited availability of interpreters or use of assumed effective interpreters, i.e., Portuguese interpreters for Spanish speaking patients. Perception of poor care when no interpreter is used, i.e., LEP patients miss crucial information and end up "feeling lost". |
| Greenhalgh et al. (2006) | Professional or relational interpreter / Communication. | Themes identified in relation to distinctions between professional and relational interpreters are their inherent positioning in one of two communicative spheres; 'the system' for the professional and 'the lifeworld' for the relational, sets a basis for the triadic interaction, at the outset. |
| Hilder et al. (2017) | Professional or relational interpreter / Communication. | Patients satisfied with the interpreter used, either professional or family. GPs had differing views; some for professional some for family. Themes were identified as: confidentiality, implicit understanding of the patient's situation, and ability to advocate and assist in the consultation on behalf of the patient. |
| Leanza et al. (2010) | Professional or relational interpreter / Communication. | The study found a higher number of interruptions of the voice of lifeworld (VoL) by physicians with a professional interpreter (64 total) than with a relational interpreter (2 total). VoL was interrupted by relational interpreters more often (21 total) than by professional interpreters (12 total). |
*Based on the same study: conducted at Harbor–UCLA Medical Center, a 500-bed public hospital in Torrance, California, USA.
LEP = limited English proficiency, ED = emergency department, IPPI = in-person professional interpreter, RSMI = remote simultaneous medical interpretation, GP =general practitioner.
The quantitative results of the review are nine reports on satisfaction, 12 reports on communication, six reports on utilization and four reports on clinical outcome. The total is more than the included number of reports as some reports include more than one outcome.
Of nine reports on satisfaction six found the highest positive effect of the professional interpreter intervention (Bagchi et al., 2011; Gany et al., 2007; Anttila et al., 2017; Garcia et al., 2004; Kuo and Fagan, 1999; Lee et al., 2002), two had any interpreter as the highest positive effect (Baker et al., 1998; Moreno and Morales, 2010) and one found no difference between professional interpreter and any other type/no interpreter with regards to satisfaction (Jacobs et al., 2007). In reports comparing more than two types of interpreters, the second most positive effect on satisfaction was for relational interpreter intervention (Kuo and Fagan, 1999; Lee et al., 2002).
Of twelve reports on communication eight found the highest positive effect of the professional interpreter intervention (Bagchi et al., 2011; Anttila et al., 2017; Bischoff et al., 2003; Butow et al., 2011; Flores et al., 2012; Flores et al., 2003; Gany et al., 2007; Garcia et al., 2004; Nápoles et al., 2015), two had any interpreter as the highest positive effect (Baker et al., 1996; Moreno and Morales, 2010), one found no significant differences in communication when comparing professional and relational interpreters (Xue et al., 2019). In reports comparing more than two types of interpreters, the second most positive effect for communication was for the relational interpreter intervention (Anttila et al., 2017) and no interpreter intervention (Flores et al., 2012).
Of the six reports on utilization two found the highest positive effect of the professional interpreter intervention (Hampers and McNulty, 2002; Luan Erfe et al., 2017; Bernstein et al., 2002) and one found not using an interpreter resulted in the best utilization compared to a professional interpreter (López et al., 2015). Two reports showed no better or unknown utilization when comparing professional interpreters with any/no interpreter (Sarver and Baker, 2000; Jacobs et al., 2007).
Of the four reports including clinical outcome, two found the most positive effect of the professional interpreter intervention (Hartford et al., 2019; Fagan et al., 2003), one found any interpreter having the most positive effect compared to no interpreter (Lindholm et al., 2012) and one found no difference in clinical outcome when comparing professional interpreter intervention with no interpreter intervention (López et al., 2015).
Different modes of professional interpretation are examined in some of the reports: in person professional, telephone or video interpretation, in conjunction with outcomes of satisfaction and communication. With the exception of Gany et al. (2007) examining the use of remote simultaneous medical interpreters, in person professional interpreter scored highest in the remainder of the studies (Bagchi et al., 2011; Gany et al., 2007; Anttila et al., 2017; Kuo and Fagan, 1999).
As shown by Brooks et al. (2016) patient perspectives on interpreter use in the qualitative reports showed barriers to receiving professional interpreter services in the ED or in hospital, were availability and time constraints. The effect is patients choosing to rely on relational interpreters or no interpreter. Relational interpreters will be more likely to support the perspective of the patient and their agenda or ‘lifeworld’, while the professional often acts as an advocate for the system, the ‘voice of medicine’ as shown by Greenhalgh et al. (2006). Hilder et al. (2017) showed a more complete translation were facilitated by the professional interpreter whereas the relational interpreter gave more relevant information about the patient. Leanza et al. (2010) found that physicians interrupted the patients voice of lifeworld (VoL) more often when a professional interpreter is present, and the relational interpreter interrupted the patients VoL more often than the professional (Leanza et al., 2010). Providers mention the issues of overt omissions, gate-keeping or agenda-setting by relational interpreters, and being more likely with this type of interpreter (Hilder et al., 2017). Information is at risk of being kept from providers, or pre-judged by the interpreter, when using relational interpreters.
4. Discussion
This review adds and updates to previous reviews (Karliner et al., 2007; Flores, 2005) on medical interpretation and its effect on patient outcomes. This is done by reaffirming the positive effect of interpreter assistance on health care for non-native speaking patients. When comparing different types of interpreters across the different reports this review shows a trend towards in person professional interpreter as the type of interpreter associated with the most positive outcome. The trend is most strongly supported when assessing satisfaction and communication but is present for all outcomes. Only six of 29 included reports compared more than two types of interpreters providing limited data for ranking the interventions beyond this. For those that did relational interpreters gave higher satisfaction and communication compared to ad hoc interpreters (Kuo and Fagan, 1999; Lee et al., 2002).
This is supported by the qualitative results by showing that the use of the professional interpreters garners trust from both patients (Brooks et al., 2016) and medical professionals (Leanza et al., 2010). This is however not universal as other reports have shown that both clinician and patients can have a higher degree of trust in relational interpreters (Greenhalgh et al., 2006; Hilder et al., 2017). The trust between patient and a relational interpreter comes from the relationship built between the two (Greenhalgh et al., 2006) and as such could be something to aspire to for the professional interpreter i.e., building relationships with patients. When discussing the relational interpreter the qualitative reports highlighted some potential issues of concern to healthcare professionals in form of possible ‘gate-keeping’, omissions or personal agendas outside of the patients, when using relational interpreters (Hilder et al., 2017; Leanza et al., 2010). These issues seem to demand medical professionals experienced in the interaction with the relational interpreter and patient, in order to utilize the potential for interpretation and translation, while avoiding the pitfalls mentioned above.
When assessing utilization and clinical outcome, the differentiation between types seems less clear. In this review only four reports included clinical outcome, and only six included utilization, providing limited data.
While most included reports examine in person interpretation, a few examine other media in interpretation such as telephone and video. Gany et al. (2007) examined the use of remote simultaneous medical interpreters, and found higher satisfaction among patients with this mode of professional interpretation, when compared to in-person professional interpretation. This opens the possibility of utilizing better video and audio technology to possibly have professional interpreters work from a centralized location in major modern health centres and hospitals or working remotely. Other reports examining remote audio or video interpretation still found highest satisfaction with in-person professional interpretation (Bagchi et al., 2011; Gany et al., 2007; Anttila et al., 2017; Kuo and Fagan, 1999).
This review was motivated by the legislation found in Denmark of patient-paid professional interpreters when needed. The concerns of costs are found in most countries receiving refugees or immigrants. A recent review of the literature on costs of medical interpretation showed that providing interpretation are both associated with lower and increased costs. However existing studies only look at the short term, and the pay off in the investment of high quality of care is measurable in the long term (Brandl et al., 2020), indicating the investment is worth it as supported by others (Bischoff, 2020). In addition, modern technological solutions of better and more accessible audio and video technology can alleviate some of the costs, while also providing the professional interpreter services associated with best overall quality of care for those who need it.
Our recommendations to improve interpretation for patients with limited language capabilities in their country of residence is grounded in the trends and findings of this review. In-person professional interpreters should be used in all medical settings. We further recommend considering the possibility of the use of relational interpreters, if the providers are trained in and aware of the pitfalls mentioned above (i.e., gatekeeping, omissions and non-patient agendas), or possibly as an add-on to professional interpreters.
Future research should focus on providing clearly defined baselines for both interventions and outcome. While some of the included reports defined what constitutes a professional interpreter, others did not. When looking at the interpreter intervention differentiation in types of interpreters should also be made clear. The relational interpreter differs from the ad hoc interpreter, and this should be of consideration to any future research. The lack of baselines for outcomes such as satisfaction and communication for almost all reports, outlines an important area of focus for future research into the use of interpreters and the effects on these outcomes. This could be done by providing surveys both before and after interventions, or by conducting baseline communications tests pre-intervention, with all parties: patient, interpreter and medical professional.
We also recommend that further research be done in remote interpretation. Especially video-chat technologies have taken great leaps and been introduced to larger population groups in conjunction with working during the Covid-19 pandemic. Providing remote professional interpretation with these means have the potential to improve quality of care while keeping costs low.
To add to the pool of knowledge, additional research into medical interpreter services should be carried out in other societies with different populations, cultures and languages. The interconnection between language and culture implies the consideration of cultural competency of medical professionals and professional interpreters. Incorporation of this aspect of interpretation exists to some degree in the qualitative reports included in this review but should receive further attention in future studies on medical interpretation.
4.1. Study strength and limitations
The strengths of this review is the inclusion of reports with different designs. It provides perspectives both quantitative and qualitative on the effects of interpreters in the medical setting. The randomized controlled trials are shown to provide a way of directly comparing the use of one type of interpreter to any other. The cohort and retrospective cohort studies provide strength in the temporal aspect of cause and effect, however, still faces usual issues of confounders in outcomes, such as self-reported satisfaction. Only two of five cohort studies managed a follow-up of 80% or more. The cross-sectional studies provide ways of comparing multiple interventions to multiple outcomes but does not provide any information on cause and effect, thereby limiting knowledge differentiating between intervention and outcome. The qualitative studies included provide important perspectives on the actual interaction between individuals receiving, providing and working with interpreters and interpretation. In addition, this review includes reports from six different countries and with more than 40 different languages, and as such provides a broad view of the connection between interpretation in the medical setting and patient outcomes.
Limitations of this review include the data search and selection process. Even though the process has been supervised, it was carried out by only the first author which introduces potential bias in both the search and data selection process. This was to some degree alleviated by the outline of a protocol following PRISMA-P guidelines (Shamseer et al., 2015), and the use of a database instrument in form of REDCap (Harris et al., 2009).
Most reports relate to Spanish-speaking minorities in the USA. Though methods are outlined, and biases shown for these reports, this makes the data skewed towards a specific cultural setting, i.e., the USA, and a specific sub-culture. This could be a limitation on the applicability of the findings of this review as cultural attitudes, the health care system and possibly population specific health issues are mainly representing one group in larger area.
The differences in study designs included in this review introduce issues of comparability and cross-report assessment of results. Even though the different types of interpreters and outcomes we wanted to measure are present in the reports, the differences in study design make it difficult to do direct comparisons across results from individual reports.
5. Conclusions
In conclusion, professional interpreter is the interpreter type resulting in greatest satisfaction and best communication for the patients, when compared to other types of interpretation or none, and should be used in the ER, in- and out-patient clinics or hospitals, when available. In addition, we found that the use of relational interpreters in the private practice setting can contribute to a positive outcome for the patient. This should be considered when choosing interpreters in this setting.
This review did not find enough data to rank the other types of interpreters, ad-hoc and relational, on the outcomes measured. We could not conclude which type of interpreter gave the best utilization or clinical outcome, beyond reaffirming that any interpreter is better than none.
Funding and competing interests
This review was carried out and written with no financial support and without any competing interests for any of the authors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jmh.2023.100162.
Appendix. Supplementary materials
References
- Anttila A., Rappaport D.I., Tijerino J., et al. Interpretation modalities used on family-centered rounds: perspectives of spanish-speaking families. Hosp. Pediatr. 2017;7(8):492–498. doi: 10.1542/hpeds.2016-0209. [DOI] [PubMed] [Google Scholar]
- Bagchi A.D., Dale S., Verbitsky-Savitz N., et al. Examining effectiveness of medical interpreters in emergency departments for Spanish-speaking patients with limited English proficiency: results of a randomized controlled trial. Ann. Emerg. Med. 2011;57(3):248–256. doi: 10.1016/j.annemergmed.2010.05.032. e1-4. [DOI] [PubMed] [Google Scholar]
- Baker D.W., Parker R.M., Williams M.V., et al. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275(10):783–788. [PubMed] [Google Scholar]
- Baker D.W., Hayes R., Fortier J.P. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med. Care. 1998;36(10):1461–1470. doi: 10.1097/00005650-199810000-00004. [DOI] [PubMed] [Google Scholar]
- Bekendtgørelse Om tolkebistan efter sundhedsloven, BEK nr 855 (2018).
- Bernstein J., Bernstein E., Dave A., et al. Trained medical interpreters in the emergency department: effects on services, subsequent charges, and follow-up. J. Immigr. Health. 2002;4(4):171–176. doi: 10.1023/A:1020125425820. [DOI] [PubMed] [Google Scholar]
- Bischoff A., Hudelson P. Access to healthcare interpreter services: where are we and where do we need to go? Int. J. Environ. Res. Public Health. 2010;7(7):2838–2844. doi: 10.3390/ijerph7072838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff A., Bovier P.A., Rrustemi I., et al. Language barriers between nurses and asylum seekers: their impact on symptom reporting and referral. Soc. Sci. Med. 2003;57(3):503–512. doi: 10.1016/s0277-9536(02)00376-3. [DOI] [PubMed] [Google Scholar]
- Bischoff A. The evolution of a healthcare interpreting service mapped against the bilingual health communication model: a historical qualitative case study. Public Health Rev. 2020;41:19. doi: 10.1186/s40985-020-00123-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boylen S., Cherian S., Gill F.J., et al. Impact of professional interpreters on outcomes for hospitalized children from migrant and refugee families with limited English proficiency: a systematic review. JBI Evid. Synth. 2020;18(7):1360–1388. doi: 10.11124/JBISRIR-D-19-00300. [DOI] [PubMed] [Google Scholar]
- Brandl E.J., Schreiter S., Schouler-Ocak M. Are trained medical interpreters worth the cost? A review of the current literature on cost and cost-effectiveness. J. Immigr. Minor. Health. 2020;22(1):175–181. doi: 10.1007/s10903-019-00915-4. [DOI] [PubMed] [Google Scholar]
- Brooks K., Stifani B., Batlle H.R., et al. Patient perspectives on the need for and barriers to professional medical interpretation. R I Med J. 2016;99(1):30–33. (2013) [PubMed] [Google Scholar]
- Butow P.N., Goldstein D., Bell M.L., et al. Interpretation in consultations with immigrant patients with cancer: how accurate is it? J. Clin. Oncol. 2011;29(20):2801–2807. doi: 10.1200/JCO.2010.34.3335. [DOI] [PubMed] [Google Scholar]
- Dungu K.H.S., Kruse A., Svane S.M., et al. Language barriers and use of interpreters in two Danish paediatric emergency units. Dan Med. J. 2019;66(8) [PubMed] [Google Scholar]
- Fagan M.J., Diaz J.A., Reinert S.E., et al. Impact of interpretation method on clinic visit length. J. Gen. Intern. Med. 2003;18(8):634–638. doi: 10.1046/j.1525-1497.2003.20701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores G., Laws M.B., Mayo S.J., et al. Errors in medical interpretation and their potential clinical consequences in pediatric encounters. Pediatrics. 2003;111(1):6–14. doi: 10.1542/peds.111.1.6. [DOI] [PubMed] [Google Scholar]
- Flores G., Abreu M., Barone C.P., et al. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann. Emerg. Med. 2012;60(5):545–553. doi: 10.1016/j.annemergmed.2012.01.025. [DOI] [PubMed] [Google Scholar]
- Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med. Care Res. Rev. 2005;62:255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- Gany F., Leng J., Shapiro E., et al. Patient satisfaction with different interpreting methods: a randomized controlled trial. J. Gen. Intern. Med. 2007;(2):312–318. doi: 10.1007/s11606-007-0360-8. 22 Suppl 2Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gany F., Kapelusznik L., Prakash K., et al. The impact of medical interpretation method on time and errors. J. Gen. Intern. Med. 2007:319–323. doi: 10.1007/s11606-007-0361-7. 22 Suppl 2(Suppl 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia E.A., Roy L.C., Okada P.J., et al. A comparison of the influence of hospital-trained, ad hoc, and telephone interpreters on perceived satisfaction of limited English-proficient parents presenting to a pediatric emergency department. Pediatr. Emerg. Care. 2004;20(6):373–378. doi: 10.1097/01.pec.0000133611.42699.08. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T., Robb N., Scambler G. Communicative and strategic action in interpreted consultations in primary health care: a Habermasian perspective. Soc. Sci. Med. 2006;63(5):1170–1187. doi: 10.1016/j.socscimed.2006.03.033. [DOI] [PubMed] [Google Scholar]
- Hampers L.C., McNulty J.E. Professional interpreters and bilingual physicians in a pediatric emergency department: effect on resource utilization. Arch. Pediatr. Adolesc. Med. 2002;156(11):1108–1113. doi: 10.1001/archpedi.156.11.1108. [DOI] [PubMed] [Google Scholar]
- Hansen M.T.L.N., Smith S. Tolkebrug i det danske sundhedsvæsen. Ugeskr. Laeger. 2013;175(10):5. [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartford E.A., Anderson A.P., Klein E.J., et al. The Use and impact of professional interpretation in a pediatric emergency department. Acad. Pediatr. 2019;19(8):956–962. doi: 10.1016/j.acap.2019.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilder J., Gray B., Dowell A., et al. It depends on the consultation': revisiting use of family members as interpreters for general practice consultations - when and why? Aust. J. Prim. Health. 2017;23(3):257–262. doi: 10.1071/PY16053. [DOI] [PubMed] [Google Scholar]
- Jacobs E.A., Sadowski L.S., Rathouz P.J. The impact of an enhanced interpreter service intervention on hospital costs and patient satisfaction. J. Gen. Intern. Med. 2007:306–311. doi: 10.1007/s11606-007-0357-3. 22 Suppl 2(Suppl 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kale E., Syed H.R. Language barriers and the use of interpreters in the public health services. A questionnaire-based survey. Patient Educ. Couns. 2010;81(2):187–191. doi: 10.1016/j.pec.2010.05.002. [DOI] [PubMed] [Google Scholar]
- Karliner L.S., Jacobs E.A., Chen A.H., et al. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv. Res. 2007;42(2):727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy C.E., Fonner V.A., Armstrong K.A., et al. The evidence project risk of bias tool: assessing study rigor for both randomized and non-randomized intervention studies. Syst. Rev. 2019;8(1):3. doi: 10.1186/s13643-018-0925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuo D., Fagan M.J. Satisfaction with methods of Spanish interpretation in an ambulatory care clinic. J. Gen. Intern. Med. 1999;14(9):547–550. doi: 10.1046/j.1525-1497.1999.07258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López L., Rodriguez F., Huerta D., et al. Use of interpreters by physicians for hospitalized limited english proficient patients and its impact on patient outcomes. J. Gen. Intern. Med. 2015;30(6):783–789. doi: 10.1007/s11606-015-3213-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leanza Y., Boivin I., Rosenberg E. Interruptions and resistance: a comparison of medical consultations with family and trained interpreters. Soc. Sci. Med. 2010;70(12):1888–1895. doi: 10.1016/j.socscimed.2010.02.036. [DOI] [PubMed] [Google Scholar]
- Lee L.J., Batal H.A., Maselli J.H., et al. Effect of Spanish interpretation method on patient satisfaction in an urban walk-in clinic. J. Gen. Intern. Med. 2002;17(8):641–645. doi: 10.1046/j.1525-1497.2002.10742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A., Altman D.G., Tetzlaff J., et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindholm M., Hargraves J.L., Ferguson W.J., et al. Professional language interpretation and inpatient length of stay and readmission rates. J. Gen. Intern. Med. 2012;27(10):1294–1299. doi: 10.1007/s11606-012-2041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luan Erfe B.M., Siddiqui K.A., Schwamm L.H., et al. Professional medical interpreters influence the quality of acute ischemic stroke care for patients who speak languages other than English. J. Am. Heart Assoc. 2017;6(9) doi: 10.1161/JAHA.117.006175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund Hansen MT Nielsen SS. [Interpretation in the Danish health-care system] Ugeskr. Laeger. 2013;175(10):644–648. [PubMed] [Google Scholar]
- Ma L., Wang Y.Y., Yang Z.H., et al. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: what are they and which is better? Mil Med. Res. 2020;7(1):7. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaëlis C., Krasnik A., Norredam M. Introduction of user fee for language interpretation: effects on use of interpreters in Danish health care. Eur. J. Public Health. 2021;31(4):705–707. doi: 10.1093/eurpub/ckaa254. [DOI] [PubMed] [Google Scholar]
- Moreno G., Morales L.S. Hablamos Juntos (Together We Speak): interpreters, provider communication, and satisfaction with care. J. Gen. Intern. Med. 2010;25(12):1282–1288. doi: 10.1007/s11606-010-1467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nápoles A.M., Santoyo-Olsson J., Karliner L.S., et al. Inaccurate language interpretation and its clinical significance in the medical encounters of spanish-speaking latinos. Med. Care. 2015;53(11):940–947. doi: 10.1097/MLR.0000000000000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam S., Chesla C., Stotts N.A., et al. Barriers to diabetes management: patient and provider factors. Diabetes Res. Clin. Pract. 2011;93(1):1–9. doi: 10.1016/j.diabres.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Sarver J., Baker D.W. Effect of language barriers on follow-up appointments after an emergency department visit. J. Gen. Intern. Med. 2000;15(4):256–264. doi: 10.1111/j.1525-1497.2000.06469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamseer L., Moher D., Clarke M., et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ Br. Med. J. 2015;349:g7647. doi: 10.1136/bmj.g7647. [DOI] [PubMed] [Google Scholar]
- Skills CA, Programme. CASP Qualitative Checklist https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf: critical Appraisal Skills Programme; 2018.
- Stewart M.A. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- Xue D., Churches T., Armstrong E., et al. Interpreter proxy versus healthcare interpreter for administration of patient surveys following arthroplasty: a pilot study. BMC Med. Res. Methodol. 2019;19(1):206. doi: 10.1186/s12874-019-0854-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.