Abstract
Sibling donation in pediatric hematopoietic stem cell transplant (HSCT) can be emotionally distressing for children, but may simultaneously evoke positive emotions, and has the potential to facilitate personal growth. We conducted a narrative review of sibling donor experiences, which included an analysis of psychosocial distress and post-traumatic growth (PTG). We searched the following databases: MEDLINE, CINAHL, PsycInfo, and SCOPUS. Search concepts used to develop key terms included HSCT, siblings, children, and psychosocial outcomes. Specific inclusion criteria included a) research articles published in English in peer-reviewed journals until September 2020, and b) reported trauma symptoms and PTG characteristics of sibling donation experiences. Four themes were identified: fear and anxiety related to HLA testing, overwhelming pressure to donate, guilt and blame when the ill child died, as well as emotional and physical isolation following donation. Sibling responses also included evidence of PTG, articulated as a deepened appreciation for life, closer relationships with the ill child and other family members, increased personal strength, and spiritual growth. These results highlight a critical need for future research approaches that further empower sibling donor voices, such as those found in participatory, arts-based methodologies.
Keywords: pediatric, sibling hematopoietic stem cell donor, sibling donor, experience, narrative review, psychosocial oncology
Introduction
Hematopoietic stem cell transplantation (HSCT) has increasingly become a treatment modality used for pediatric cancers, hematological, and genetic disorders (Pelletier et al., 2015). A large percentage of pediatric HSCT treatments rely on a donation of bone marrow or stem cells from siblings because of their close genetic match at the human leukocyte antigen loci (HLA) (D’Auria et al., 2015). Although the success rate of HSCT is high, a small but growing body of literature suggests that there are significant but often overlooked psychosocial risks for pediatric siblings before, during, and after donation (D’Auria et al., 2015; Erden et al., 2019; Gizli Coban et al., 2017; Hoag et al., 2018; Hutt et al., 2015; MacLeod et al., 2003; Packman et al., 1997a, 1997b; Pelletier et al., 2014; Pentz et al., 2012; 2014; Pot-Mees and Zeitlin, 1987; Stegenga et al., 2019; Switzer et al. 2016; White et al., 2017; Wiener et al., 2008; Wilkins and Woodgate, 2007; Zajac-Spychala et al., 2020). Even less research attention has been focused on potential positive gains for sibling donors, such as post-traumatic growth (PTG) which has been defined by Tedeschi and Calhoun (2004) as positive psychological change gained through the struggle of facing highly challenging circumstances.
Aim
To provide insight into what is currently known about sibling donor experiences of pediatric HSCT and to provide key recommendations to guide future research, practice, and policy.
Review design
A narrative review was selected as opposed to a systematic review as we aimed to critique, describe, interpret, and gain a deeper understanding of the broad spectrum of literature (Greenhalgh et al., 2018) that focused on pediatric sibling donation experiences before, during, and after pediatric HSCT, using a post-traumatic stress (PTS) (Substance Abuse and Mental Health Administration, 2014) and PTG theoretical framework (Tedeschi and Calhoun, 2004). The congruence of a PTS/PTG theoretical framework for this integrative review is supported by a growing application of PTS theory (Kazak and Baxt, 2007; Stuber et al., 2010), and PTG theory (Tobin et al., 2018) in the childhood cancer literature over the last 10–20 years (Kazak and Baxt, 2007; Stuber et al., 2010), and Packman‘s (1999) previous adoption of a psychosocial model for exploring PTS symptoms (Green et al., 1985) in pediatric HSCT. This review was guided by the following research question: What are the experiences, including symptoms of trauma and characteristics of PTG, reported by pediatric sibling donors for HSCT?
Inclusion and exclusion criteria were developed based on the research question. To be included in the analysis, articles needed to be: a) an original research article, b) published in a peer-reviewed journal until September 2020, c) published in the English language, d) report on psychosocial experiences of sibling HSCT donors, and e) the donor population must have been under 18 years of age at the time of donation.
Search methods
An academic librarian (JW) developed the literature search. Based on the research question, four search concepts were developed: HSCT, siblings, children, and psychosocial experiences. The search concept for “children” was adapted for Medline from a validated search filter developed for PubMed (Leclercq et al., 2013). An initial set of target articles was used to identify relevant keywords and subject headings. This search was initially developed in MEDLINE (Ovid), and subsequently translated into CINAHL (Ebsco), PsycInfo (Ovid), and Scopus. Subject headings (e.g., MeSH) were used for each of the concepts and combined with keywords using Boolean operators. Appropriate search histories have been included for each database as a supplementary file.
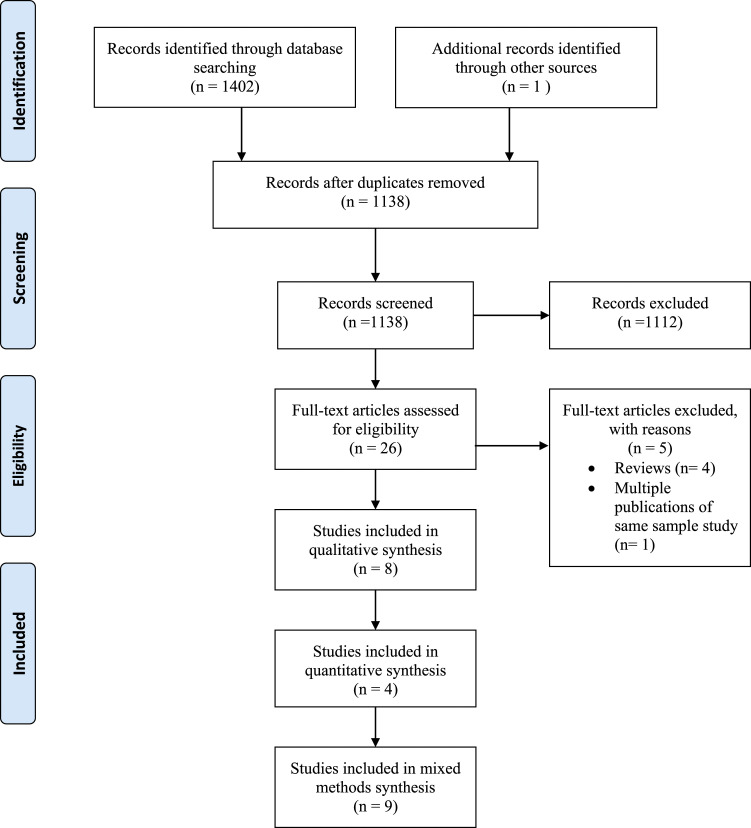
Final searches were run on July 30, 2020, producing a total of 1402 results, which were exported to EndNote, version X9.3.3 (Clarivate Analytics), where they were deduplicated using a simplified version of the method described by Bramer et al. (2016). Following deduplication, there were 1137 results.
Data extraction
The search results were uploaded to Rayyan for title and abstract screening (Ouzzani et al., 2016). Additionally, one article was identified through the reference list of a relevant article, increasing the total number of results to 1138. Two authors, AWK and CW screened titles and abstracts to identify articles that met all five inclusion criteria, and 1112 publications that did not meet inclusion criteria were excluded during this screening stage. In cases where it was unclear if publications met inclusion criteria, they proceeded to full text screening. Conflicts were resolved through discussion.
Twenty six results proceeded to full text review and were screened by the first author (AWK). Four were excluded due to their research method (reviews), but these articles are addressed in the discussion. One was excluded based on reporting data from the same study.
A PRISMA diagram is presented in Figure 1 to visually represent this process.
Figure 1.
Flow diagram (Moher et al., 2009) to display study selection process of literature exploring the psychosocial experiences of pediatric hematopoietic stem cell donors.
Search outcome
The final review sample included 21 studies: eight employed qualitative methodology, four quantitative, and nine articles used mixed methods. Six studies focused solely on sibling donors, while the remaining studies explored sibling donor, sibling nondonor, and/or parent and patient perspectives. All articles had child participants within their sample. Detailed information regarding each of the 21 studies, including the sample size, participant age, methodology, and measures are found in Table 1.
Table 1.
General characteristics of studies exploring pediatric sibling donors of HSCT.
| Author | Country | Sample size (transplant status) | Study design | Measures |
|---|---|---|---|---|
| D’Auria et al. (2015) | Canada | 8 sibling donors aged 10–30 years (successful) | Qualitative, grounded theory | Semi-structured, open-ended interviews |
| Erden et al. (2019) | Turkey | 30 HSCT recipients; 20 donors aged 6–18 years; 30 nondonors aged 6–18 years | Cross-sectional study, descriptive, quantitative | Kiddie Schedule for Affective Disorders and
Schizophrenia (K-SADS) Children’s Depression Inventory State-Trait Anxiety Inventory for Children State-Trait Anxiety Inventory Rosenberg Self-Esteem Scale Hollingshead-Redlich Scale |
| Gizli Coban et al. (2017) | Turkey | 35 mothers and siblings (donor and nondonor)
aged 5–18 years; 35 healthy peers aged 5–18 years and mothers |
Cross-sectional study, descriptive, quantitative | CPTSD-RI PCL-C (mothers) PedsQL 4.0 |
| Hoag et al. (2018) | USA | 9 sibling donors aged 9–21 years (6 successful; 3 unsuccessful) | Mixed methods, longitudinal study | Semi-structured
interview The Child Behavior Checklist (ages 6–18) Youth Self-Report (ages 11–18) Adult Self-Report (age 18–59) The Ways of Coping Questionnaire The Network of Relationships Inventory The Faces of Pain Scale Revised |
| Hutt et al. (2015) | Israel | 36 sibling donors median age 13 at time of donation, 50 parents of pediatric patients | Cross-sectional, descriptive, quantitative | Questionnaires: Donor’s attitude questionnaire regarding stem cell transplant Parent’s attitude questionnaire regarding the sibling donor experience |
| MacLeod et al. (2003) | Canada | 15 sibling donors aged 7–20 years (8 successful; 7 unsuccessful) | Qualitative, grounded theory | Interviews |
| Packman et al. (1997a; 1997b, 1998, 2003, 2004) | USA | 44 siblings; 21 donors, 23 nondonors aged 6–18 years (all successful) | Mixed methods with a cross-sectional description component | Semi-structured, forced-choice and open-ended
interviews using: The Revised Children’s Manifest Anxiety Scale The Child Depression Inventory The Rosenberg Self-Esteem Scale Child Post-Traumatic Stress Reaction Scale; Kinetic Family Drawing Revised Human Figure Drawing |
| Pelletier et al. (2014) | USA and Canada | 58 parents and surrogates; 19 patients; 16 donor siblings aged 9–17 years; 39 nondonor siblings, half-siblings and cousins | Qualitative, exploratory study (semantic content analysis); secondary analysis | Semi-structured, open-ended interviews |
| Pentz et al. (2014) | USA and Canada | T1= 12 sibling donors T2= 12 sibling donors T3= 10 sibling donors aged 9–18 years |
Mixed methods, cross-sectional description component | Interviews The Satisfaction with Decision Scale Decision Regret Scale |
| Pentz et al. (2012) | USA and Canada | 15 patients aged 11–18 years; 22 mothers; 2 step-mothers; 1 grandmother; 19 fathers; 3 stepfathers; 1 grandfather; 13 sibling donors aged 9–17 years; nondonor siblings aged 9–22 years | Qualitative grounded theory; secondary analysis | Qualitative Interviews |
| Pot-Mees and Zeitlin (1987) | England | 15 patients; 9 sibling donors; 10 sibling nondonors; 15 mothers; 8 fathers | Mixed methods, cross-sectional, pilot study | Semi-structured interview The Richmond BCL Rutter A Scale Ruth Griffiths Developmental Scales (younger children) British Abilities Scales (older children) General Health Questionnaire (parents) |
| Stegenga et al. (2019) | USA and Canada | 47 parents and surrogates; 17 patients; 16 donor siblings; 39 nondonor siblings; half-siblings; cousins | Qualitative, exploratory study (semantic content analysis); secondary analysis | Semi-structured, open-ended interviews |
| Switzer et al. (2016) | USA | 105 pediatric
donors: 5–7 years= 19; 8–12 years= 45; 13–18 years= 41 |
Quantitative, longitudinal | The Pediatric Quality of Life Inventory Health Related Quality of Life Open-ended question (parents) |
| White et al. (2017) | USA and Canada | 109 family members 56 parent/surrogates; 18 patients; 24 nondonor siblings; 11 donor siblings; 15 health care providers |
Qualitative, exploratory study (semantic content analysis); secondary analysis | Semi-structured, open-ended interviews |
| Wiener et al. (2008) | USA | 14 sibling donors: 11 siblings living (3 recipients deceased) aged 9–28 years | Qualitative, exploratory study (content analysis) | Retrospective interviews |
| Wilkins and Woodgate (2007) | Canada | 8 siblings: 3 donors; 5 nondonors (all recipients living) aged 11–24 years | Qualitative, hermeneutic phenomenology | Semi-structured, open-ended interviews |
| Zajac-Spychala et al. (2020) | Poland | 45 recipients median age 11.9 at time of donation; 45 sibling donors median age 15.5 at time of donation | Mixed methods, cross-sectional | Demographic
Survey Functional Assessment of Chronic Illness Therapy-Bone Marrow Transplant Functional Assessment of Cancer Therapy (FACT) (general) FACT T01 Adult Siblings Relationship Questionnaire |
Integrative synthesis and analysis
The sample of research articles was analyzed using narrative review methodology (Torraco, 2005; Whittemore and Knafl, 2005). The analysis explored the trajectory of pediatric sibling donation experiences through two main lenses: trauma symptoms and characteristics of PTG reported by siblings before, during, or after donation. For this review, trauma symptoms were defined as resulting from “an event, series of events or circumstances” experienced “by an individual as physically or emotionally harmful or life threatening and that has long lasting adverse effects on this individual’s functioning and mental, social, emotional or spiritual wellbeing” (Substance Abuse and Mental Health Administration, 2014: 7). Post-traumatic growth can occur in the aftermath of traumatic events, and recent research has demonstrated that PTS symptoms and growth can and do coexist (Shah and Mishra, 2021). While identified studies did not address PTG specifically, sibling reports were found to include characteristics of personal growth from the donation process. Post-traumatic growth was defined as “an increased appreciation for life,” “more intimate relationships with others,” “gains in personal strength,” and “spiritual growth” (Tedeschi and Calhoun, 2004: 6). Articles were manually reviewed by AWK for sibling donor descriptions of PTS and PTG experiences that matched chosen PTS and PTG definitions. These descriptions of PTS and PTG within the literature were then manually sorted into more descriptive narrative themes within each lens, and described in detail within the findings Mays, Pope, & Popay (2005).
Findings
Donor-related trauma symptoms
While a wide range of traumatic stress symptoms are possible (Galatzer-Levy et al., 2018), within this review trauma symptoms reported by sibling donors included: PTS symptoms, anxiety, depression, stress, guilt, blame, and general emotional distress. Four distinct themes were identified from the reviewed literature including: 1) psychological distress, including fear and anxiety related to HLA testing, 2) an overwhelming pressure to donate, 3) guilt and blame following the death of the ill child, and 4) emotional/physical isolation from parents following donation. These four themes mapped closely onto a specific timeline for sibling donors, which began with blood testing to find the closest HLA match, learning they were an HLA match, making the decision to donate, becoming a patient themselves during the donation procedure, and waiting to find out if the transplant was successful.
The distress of HLA testing
Learning that the ill child would need HSCT treatment signaled the beginning of a distressing period for the entire family (D’Auria et al., 2015). At this time, family members underwent blood tests to determine if they were an HLA match for donation. The HLA testing process created stress for siblings; many children expressed fear and anxiety about the needles that would be used to draw blood (D’Auria et al., 2015; Pot-Mees and Zeitlin, 1987; Wilkins and Woodgate, 2007). In one study that used retrospective, structured interviews with adults, 64% of donors stated, regardless of their age at the time of donation, that needle pokes were their primary concern (Weiner et al., 2008). After the HLA test, siblings reported a high degree of anxiety while waiting to find out if they would be the closest match (Hoag et al., 2018). For example, one sibling expressed the immense pressure they felt to “be the perfect match” (D’Auria et al., 2015: 449). This sibling was also scared they might not be a match:
When they took my blood I was so scared I passed out. I mean I was so terrified because the pressure was just so overwhelming (D’Auria et al., 2015: 449).
Once a decision to donate had been made, siblings experienced fear and anxiety about the actual donation procedure, specifically around any physical pain they might experience (Hoag et al., 2018; MacLeod et al., 2003; Packman et al., 1997a, 1997b; Wiener et al., 2008; Wilkins and Woodgate, 2007). One sibling (8 years) described their emotional state on the day of donation:
When I entered the hospital, I was so scared…I didn’t want to die or anything. I was so nervous, I thought I was going to get sick (Packman et al., 1998: 182).
Similarly, an adolescent sibling indicated that they felt their body was “violated” during blood draws and other medical procedures (Packman et al., 1997a: 251).
The overwhelming pressure to donate
Once identified as the most appropriate HLA match, siblings felt pressure and responsibility to go through with the donation procedure. Their decision to donate was predominantly made from an obligation to their family, and siblings did not always feel they had a voice in the decision-making process (Hoag et al., 2018; Hutt et al., 2015; MacLeod et al., 2003; Packman et al., 1997a, 1998; Pentz et al., 2014; Stegenga et al., 2019). For instance, one sibling recalled being told by their father that if they did not donate there would be horrible consequences:
My dad came to me and said, ‘you’re doing this’. I told him I didn’t want to. He said ‘Fine then, he’ll die’…so it wasn’t my choice (Packman et al., 1998: 180).
Another sibling echoed a similar sentiment stating:
You do have a choice but it’s really either you do it or something really bad is going to happen (D’Auria et al., 2015: 449).
Pentz et al. (2014) interviewed parents of pediatric HSCT patients to explore family decision-making processes. The majority of parents (77%) felt that there was “no choice” in the decision about whether or not siblings would donate (Pentz et al., 2014: e1156). From the same study sample, 31% of sibling donors felt there was “no decision to be made” (Pentz et al., 2012: 882). Even when siblings were offered a choice, many still reported feeling pressured by their parents to donate (Hutt et al., 2015; Pentz et al., 2014). One sibling shared:
There are fears and memories, it was traumatic because of the pressure. The donation was forced because of the situation (Hutt et al., 2015: 1339).
Some sibling donors indicated that they wanted to have the autonomy to make the final decision (D’Auria et al., 2015; Hoag et al., 2018; MacLeod et al., 2003; Packman et al., 1997a; Pentz et al., 2014), although many felt overwhelming pressure and responsibility to save their brother’s or sister’s life through their HSCT donation (D’Auria et al., 2015; MacLeod et al., 2003). One sibling described this pressure:
I hope I’m not the one to do my brother in…it would have killed me (D’Auria et al.,2015: 450).
Feelings of guilt and blame
A 14-year-old sibling donor expressed fear that something might go wrong with the transplant and believed that would be their fault (Wallace et al., 2014). Further, donation pressure was exacerbated by the siblings’ belief that the donation would take immediate effect; they did not understand that it would take weeks or months for their ill sibling to recover from HSCT (D’Auria et al., 2015). If the HSCT treatment was unsuccessful, and their brother/sister died, sibling donors felt guilt and blame (MacLeod et al., 2003; Packman et al., 1997a, 1997b). MacLeod et al. (2003) reported that these feelings intensified over time, especially if children did not have an opportunity to speak with someone about the unsuccessful HSCT and death of their brother or sister. One sibling recalled:
I knew that was the last chance and knowing that it didn’t work, I felt guilty… It was something that built up and nobody probably even realized that I felt that way (MacLeod et al., 2003: 228)
Emotional and physical isolation from parents
When interviewed about concerns they faced during HSCT, sibling donors reported “feeling negative effects of separation from the parent and caregiver” (White et al., 2017: 4). Similarly, Hoag et al. (2018) found that 40% of sibling donors felt they were not provided with adequate support post-donation. The critical need for emotional support throughout HSCT and psychosocial follow-up after HSCT was similarly echoed in other studies (D’Auria et al., 2015; Pentz et al., 2014; Wilkins and Woodgate, 2007; Zajac-Spychala et al., 2020).
Packman et al. (1997a) asked donor and nondonor siblings to complete three self-report measures during hospital follow-up visits or at home. These included an anxiety scale (Reynolds and Richmond, 1992), a traumatic stress symptom scale (Frederick et al., 1992), and a self-esteem scale for children aged 12 years and older (Rosenberg, 1965). Donor siblings reported significantly higher anxiety and significantly lower self-esteem as compared to nondonor siblings. Furthermore, both donor and nondonor siblings reported moderate-to-severe levels of PTS symptoms following HSCT (Packman et al., 1997a).
Additionally, Gizli Coban, Surer Adanir, and Ozatalay (2017) retrospectively compared the Child PTSD Reaction Index (Pynoos et al., 1987) scores of siblings of pediatric bone marrow transplant (BMT) survivors including sibling donors to a healthy control group, revealing that siblings of BMT survivors experienced significantly higher levels of PTSD (Gizli Coban et al., 2017). Interestingly, when comparing scores of donor to nondonor siblings, nondonor siblings’ PTSD scores were higher (Gizli Coban et al., 2017). Donor siblings may experience anxiety as they prepare for and anticipate donation, while nondonor siblings may be grappling with the emotional stress of not only having a seriously ill sibling, but also seeing another sibling become a patient through the donation process (Gizli Coban et al., 2017; Packman et al., 1997a). Packman et al. (1997a) attributed lower self-esteem scores reported by sibling donors to the physical and emotional isolation they experienced once the focus returned to the patient after the donation procedure was complete.
Once their ill brother/sister’s health improved and their parents were home more, sibling donors experienced difficulty opening up emotionally to their parents. Siblings continued to struggle with the physical and emotional separation from parents that had occurred during HSCT. An adolescent sibling donor expressed this experience:
I’m sorry, you don’t even care enough to be home…I don’t see why I should talk to you about how much you’re ignoring me (Packman et al., 1998: 180).
For some adolescent sibling donors who had withdrawn inward emotionally, the return home of the patient and other family members proved to be a stressful experience (Packman et al., 1997a). Many sibling donors indicated that neither their parents nor clinicians had asked about their psychosocial well-being post-donation (Packman et al., 1997a). One donor sibling shared the following:
No one really asked me…I didn’t have anyone to talk to about it. In fact, you are the first person I’ve talked to about this (Packman et al., 1997a: 251).
Post-traumatic growth
These review findings call attention to how complex the HSCT process is for sibling donors. In addition to experiences of distress, many sibling donors described personal gains and growth post-donation. These growth experiences were framed within the characteristics of PTG, which included “an increased appreciation for life,” “more intimate relationships with others,” “gains in personal strength,” and “spiritual growth” (Tedeschi and Calhoun, 2004: 6).
Appreciation for life
Within the research reviewed, sibling donors described a sense of purpose concerning what they perceived as a direct contribution to their brother/sisters’ recovery (Hutt et al., 2015). One sibling remarked six years post-donation:
You are giving life to someone else. You are not just one of those people just standing there trying to help them, you’re actually the one who is doing it. You’re the one who is saving him (Packman et al., 1998: 182).
Another sibling spoke to this experience:
You’re basically giving them a second chance…I found it as, uh, as a wonderful thing to help my brother out (Hoag et al., 2018: 372).
Some sibling donors were puzzled as to why an individual would choose not to donate if they matched and were offered a chance to save their sibling’s life (D’Auria et al., 2015). Even though they had previously expressed fear about the procedure and the possibility of physical pain, they also recognized how important their donation was to their sibling’s recovery and maintained this mindset years following donation. The donation experience appeared to contribute to gaining a greater sense of purpose in life.
Closer relationships with their ill sibling and parents
In the aftermath of HSCT, sibling donors felt they gained a closer relationship with their sibling and other family members (D’Auria et al., 2015; Hoag et al., 2018; Hutt et al., 2015; MacLeod et al., 2003; Packman et al., 1997b; Pelletier et al., 2014; Pentz et al., 2014; Wilkins and Woodgate, 2007). Hoag et al. (2018) found that by 6 months post-donation, most sibling donors felt that their family was closer than they had been pre-donation. Siblings described an intensified bond and a strengthened sense of loyalty to their ill brother or sister, as one sibling shared:
When I say we’re closer than brothers, whatever it is, if there’s a word for closer than brothers, that’s the word we are (D’Auria et al., 2015: 450).
Sibling donors expected that their ill sibling would be there for them when needed in the future (D’Auria et al., 2015). Sibling donors felt the entire family was closer after HSCT and that the traumatic experience of HSCT had encouraged family members to lean on each other for support, creating closer relationships within the family system (Hutt et al., 2015; Weiner et al., 2008).
Increased sense of personal strength
Many sibling donors described feeling happy and relieved that they were a match for their ill sibling and valued being able to actively contribute to their sibling’s treatment (D’Auria et al., 2015; Hoag et al., 2018; Hutt et al., 2015; MacLeod et al., 2003; Pentz et al., 2014). Within the literature we reviewed, only two siblings expressed regret over their decision post-donation. One sibling donor expressed shock after their sibling died and grappled with the post-donation realization that death was a possibility (Hoag et al., 2018) and the other sibling described the donation as “painful” (Pentz et al., 2014: e1160).
Most siblings felt proud and happy about their donation decision (Hoag et al., 2018; Packman et al., 1997b) or experienced increased self-esteem and felt good about themselves (Erden et al., 2019; Hutt et al., 2015). Sibling donors also shared that they felt they had grown as a person after donating. One sibling reflected, three years post-donation:
I do feel like a better person after giving bone marrow to my brother and I would do it again…you can save somebody’s life (Packman et al., 1998: 179).
Sibling donors also showed gains in personal and social growth in their school environment post-donation. In one study, teachers of both donor and nondonor siblings assessed behavioral problems and social competencies in school two and a half years post-donation (Packman et al., 1997a). Donor siblings scored higher in terms of adaptive skills, leadership qualities, and social skills when compared with nondonor siblings (Packman et al., 1997a). The authors hypothesized that school might provide a positive distraction for donor siblings, by providing a place where they can practice mastery, receive support, and gain distance from the trauma of their donation experience.
Many sibling donors were also able to set aside their fears and anxieties of the procedural pain, while ruminating over the pain that their ill sibling was still enduring (D’Auria et al., 2015; MacLeod et al., 2003). This compassion for their sibling’s pain in the midst of their own donation experience may also set in motion processes leading toward PTG.
Spiritual growth
The domain of spiritual growth was only mentioned in one study reviewed (Wilkins and Woodgate, 2007), where sibling donors referred to their spirituality and religious beliefs as a coping response to HSCT. Prayer was the most common coping response which helped sibling donors process their experience (Wilkins and Woodgate, 2007).
Taken together, the experiences of traumatic stress symptoms and personal growth expressed by pediatric sibling HSCT donors highlights the complexity of the donation process for donor siblings; they simultaneously need to process fear, anxiety, and isolation along with experiences of greater meaning, personal growth, and enhanced relationships. A small but growing body of literature clearly demonstrates that a better understanding of the multifaceted experience of pediatric HSCT donation from the unique perspective of pediatric sibling donors themselves is needed. Further understanding about sibling donors’ perspectives of distress and growth will facilitate the development of supports and resources to minimize the trauma experienced and foster the potential for personal growth and meaning.
Discussion
The aim of this narrative review was to gain a nuanced understanding of the range of psychosocial experiences of pediatric sibling donors within the literature. All 21 studies reviewed reported that pediatric sibling donors express some form of psychosocial distress across the donation process. Only three studies in this review explicitly measured trauma symptoms experienced by donors and nondonors, which included anxiety (Erden et al., 2019; Packman et al., 1997a), depression (Erden et al., 2019; Packman et al., 1997a), and PTS symptoms (Gizli Coban et al., 2017; Packman et al., 1997a). However, within the remaining articles, siblings did express experiences of distress, fear, overwhelming pressure, guilt and blame, as well as emotional and social isolation. These reports also fit within the Substance Abuse and Mental Health Administration (2014) trauma framework used to guide this review.
The term “post-traumatic growth” was not explicitly used in the studies analyzed in this review; however, sibling donors described personal gains and growth post-donation in 48% of studies reviewed (D’Auria et al., 2015; Erden et al., 2019; Hoag et al., 2018; Hutt et al., 2015; MacLeod et al., 2003; Packman et al., 1997b; Pelletier et al., 2014; Pentz et al., 2014; Weiner et al., 2008; Wilkins and Woodgate, 2007), suggesting that a PTG lens was an appropriate fit. This novel analysis provides an increased understanding of the potential for growth during sibling donation, which may contribute to the development of new approaches to psychosocial intervention in the future.
The findings from previous reviews (Bauk et al., 2013; Packman, 1999; Packman et al., 2010; Weiner et al., 2007) are consistent with the PTS symptoms and distress described within our findings. Also, congruent with previous reviews, was our identification of intensified psychological distress of sibling donors in the context of unsuccessful transplants (Bauk et al., 2013; Packman et al., 2010; Weiner et al., 2007). Earlier reviews briefly underlined the growth experienced by sibling donors, primarily describing that growth as “positive effects” (Bauk et al., 2013: 240). The improved family cohesion experienced by all family members (Bauk et al., 2013; Weiner et al., 2007; Packman et al., 2010) was also highlighted.
It is also worth noting that only two previous reviews (Bauk et al., 2013; Weiner et al., 2007) exclusively focused on the pediatric sibling donor perspective. It is important that researchers, clinicians, and parents understand children’s donor experiences from their perspective, so they are able to effectively engage in the ethically sensitive process of respecting children’s voices, autonomy, and well-being during HSCT (Hoag et al., 2018).
Limitations
The research studies included in this review were limited by the use of primarily cross-sectional and descriptive research designs and small samples. We were only able to include English language articles because of time and translation costs. Additionally, most studies explored the experience of pediatric HSCT from the perspective of multiple family members, rather than exclusively focusing on sibling donor perspectives. This created a challenge when attempting to tease apart the unique experiences of pediatric sibling donors from other findings; however, these experiences were separated by headings which aided in differentiation. In addition, it was not possible to use a developmental lens to examine potential differences in PTG in siblings who were children or adolescents, given the wide variety of ages across studies. Despite these limitations, this review presented critical information about symptoms of trauma and characteristics of PTG experienced by pediatric sibling donors from their own perspective.
Recommendations for practice and policy
We identified a critical need for siblings to receive ongoing psychosocial support across the donation process. Comprehensive psychosocial support for sibling donors begins with providing accurate, developmentally appropriate information about the donation procedure at different time points: pre-donation, post-donation, and during recovery (D’Auria et al., 2015). In the reviewed literature, it was clear that some sibling donors experienced distress due to a lack of knowledge about the donation procedure, but they also lacked understanding about the HSCT recovery trajectory (D’Auria et al., 2015).
When it is recognized that pediatric sibling donors have the potential to develop PTG characteristics stemming from their donation experiences, support services can be re-conceptualized to a strength-based perspective. Additionally, it is important to recognize that the PTS/PTG experienced by sibling donors is occurring in the context of a complex set of traumatic experiences for multiple family members, as well as the family system (Berger and Weiss, 2009; Van Schoors et al., 2015). Knowledge development focused on how these complex traumatic processes interact and influence one another is also central to understanding how to address PTS and facilitate PTG in sibling donors in practice.
An additional recommendation for practice is that sibling donors receive support that focuses on their well-being throughout HSCT. Health care professionals can use tools such as play therapy or expressive arts approaches to help siblings understand the treatment process, and to assist them in authentically expressing their fears and anxieties (Heiney et al., 2002). This level of care should continue post-donation, as sibling donors have indicated they wanted follow-up visits to monitor their adjustment in the months and years after donation (D’Auria et al., 2015; Packman et al., 1997b; Pentz et al., 2014; Wilkins and Woodgate, 2007).
Given the challenges and concerns reported by sibling donors, it is further recommended that a professional within the HSCT donation team be identified to act as an independent advocate for donor siblings, to assist them in navigating the complex decision-making process of donation. Many siblings indicated that they felt they were not given a choice about whether or not to donate, and they experienced traumatic symptoms around a lack of informed consent and autonomy in decision-making. A donor advocate could assist potential sibling donors in making decisions based on their personal values and assisting them to navigate the complex decision-making process (Hoag et al., 2018; Weaver et al., 2015).
Recommendations for future research
Based on our review findings, one clear gap identified in the literature was limited data on the short and long-term psychosocial effects of sibling HSCT donation (D’Auria et al., 2015). There is a critical need for longitudinal studies about how siblings adjust post-donation and throughout their lives. Longitudinal studies could not only identify and explore differing sibling trajectories post-donation but would also assist in identifying factors that facilitate or hinder PTS recovery, personal growth, and impacts on family relationships over time. Additionally, studies which explicitly focus on sibling donors that utilize both quantitative and qualitative methodology, as well as larger study samples are needed.
Future studies also need to examine the sibling donor experience of PTS/PTG in the context of the PTS/PTG experienced by the family system (Berger and Weiss, 2009; Van Schoors et al., 2015). The experiences of trauma and growth reported by sibling donors across the reviewed studies may have been significantly impacted by relational processes within the family (Berger and Weiss, 2009; Van Schoors et al., 2015). Gaining a stronger understanding of sibling donor PTS/PTG through a family systems perspective may provide further insight into how to support sibling donors, and the entire family during HSCT (Berger and Weiss, 2009; Van Schoors et al., 2015).
In this review, there were eight studies that adopted qualitative methodologies, including grounded theory (D’Auria et al., 2015; MacLeod et al., 2003; Pentz et al., 2012), hermeneutic phenomenology (Wilkins and Woodgate, 2007), and content analysis (Pelletier et al., 2014; Stegenga et al., 2019; White et al., 2017; Wiener et al., 2008). These studies consistently used the method of narrative interviews. Given the ongoing emotional and cognitive development of child sibling donors, it may be helpful to explore the addition of art-based qualitative methods to assist children to communicate these complex experiences with HSCT donation.
The adoption of participatory, arts-based research methodologies would add further developmental sensitivity to the research evidence currently available. Children recall and communicate information more easily through hands-on, interactive and creative activities that use their senses such as painting, drawing, symbolic play, or digital storytelling (Linder et al., 2018). In the literature we reviewed, only one study included arts-based methods of data collection, which complemented rating scales and interviews (Packman et al., 1998). We suggest that further engagement with qualitative, arts-based, participatory methodologies would facilitate relationship, dialogue, and sibling voice within the research process (Coyne and Carter, 2018; Horgan, 2017). Pediatric sibling donors may feel more comfortable sharing their psychosocial distress or growth through expressive arts methods where they can be creative and feel in control of how they share their experiences (McNiff, 2018; Sourkes, 2018).
Conclusion
Sibling donors are important stakeholders within the pediatric HSCT treatment process. In this narrative review, we analyzed the literature on psychosocial experiences of pediatric sibling donors, exploring traumatic stress symptoms including fear and anxiety, an overwhelming pressure to donate, feelings of guilt and blame, as well as physical and emotional isolation from their family following a donation procedure. Sibling donors also reported PTG characteristics, such as a greater appreciation for life, more intimate family relationships, a greater sense of personal strength and spiritual growth (Tedeschi and Calhoun, 2004). Our findings confirm that although HSCT is psychologically distressing for pediatric sibling donors, it can also be the catalyst for rich personal growth and development on an individual and relational level. If pediatric HSCT sibling donation is approached with support for traumatic stress symptoms as well as the potential for growth in mind, the experience may be significantly and fundamentally improved for donor siblings.
Acknowledgments
The first author would like to acknowledge the Department of Community Services, Red River College, for PhD tuition support.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Andrea Winther Klippenstein is supported by a 2021-2022 Research Manitoba-Children's Hospital Research Institute of Manitoba PhD in Health Research Studentship Award.
Ethical concerns: The authors acknowledge there are no ethical concerns.
ORCID iDs
Andrea D Winther Klippenstein https://orcid.org/0000-0002-7212-9538
Christina H West https://orcid.org/0000-0001-8265-5737
References
- Bauk K, D’Auria JP, Andrews A, et al. (2013) The pediatric sibling donor experience in hematopoietic stem cell transplant: an integrative review of the literature. Journal of Pediatric Nursing 28: 235–242. DOI: 10.1016/j.pedb.2012.09.004 10.1016/j.pedb.2012.09.004. [DOI] [PubMed] [Google Scholar]
- Berger R, Weiss T. (2009) The posttraumatic growth model: an expansion to the family system. Traumatology 15: 63–74. DOI: 10.1177/1534765608323499. [DOI] [Google Scholar]
- Bramer WM, Giustini D, De Jonge GB, et al. (2016) De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association 104(3). DOI: 10.5195/JMLA.2016.24 10.5195/JMLA.2016.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne I, Carter B. (eds) (2018) Being Participatory: Researching with Children and Young People. Switzerland: Springer. [Google Scholar]
- D’Auria JP, Fitzgerald TM, Presler CM, et al. (2015) Through the eyes of young sibling donors: the hematopoietic stem cell donation experience. Journal of Pediatric Nursing 30: 447–453. DOI: 10.1016/j.pedn.2014.12.012. [DOI] [PubMed] [Google Scholar]
- Erden S, Kuşkonmaz BB, Çetinkaya DU, et al. (2019) Pediatric bone marrow transplantation: psychopathologic features in recipients along with siblings. Psychooncology 28(10): 1995–2001. DOI: 10.1080/08880018.2019.1648619. [DOI] [PubMed] [Google Scholar]
- Gizli Çoban Ö, Sürer Adanır A, Özatalay E. (2017) Post-traumatic stress disorder and health-related quality of life in the siblings of the pediatric bone marrow transplantation survivors and post-traumatic stress disorder in their mothers. Pediatric Transplantation 21: 1–7. DOI: 10.1111/petr.13003. [DOI] [PubMed] [Google Scholar]
- Green BL, Wilson JP, Lindy JD. (1985) Conceptualizing post-traumatic stress disorder: a psychosocial framework. In: Figley CR. (ed) Trauma and Its Wake: The Study and Treatment of Post-Traumatic Stress Disorder. New York: Brumer/Mazel, 53–69. [Google Scholar]
- Frederick CJ, Pynoos RS, Nadar K. (1992) Child Post-Traumatic Stress Reaction Index. Los Angeles, CA: University of California. [Google Scholar]
- Galatzer-Levy IR, Huang SH, Bonanno GA. (2018) Trajectories of resilience and dysfunction following potential trauma: a review and statistical evaluation. Clinical Psychology Review 63: 41–55. DOI: 10.1016/j.cpr.2018.05.008. [DOI] [PubMed] [Google Scholar]
- Greenhalgh T, Thorne S, Malterud K. (2018) Time to challenge the spurious hierarchy of systematic over narrative reviews? European Journal of Clinical Investigation 48(6): e12931. DOI: 10.1111/eci.12931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heiney SP, Bryant LH, Godder K, et al. (2002) Preparing children to be bone marrow donors. Oncology Nursing Forum 29(10): 1485–1489. DOI: 10.1188/02.ONF.1485-1489. [DOI] [PubMed] [Google Scholar]
- Hoag J, Igler E, Karst J, et al. (2018) Decision-making, knowledge, and psychosocial outcomes in pediatric siblings identified to donate hematopoietic stem cells. Journal of Psychosocial Oncology 37: 367–382. DOI: 10.1080/07347332.2018.1489443. [DOI] [PubMed] [Google Scholar]
- Horgan D. (2017) Child participatory research methods: attempts to go ‘deeper’. Childhood 24(2): 245–259. DOI: 10.1177/0907568216647787. [DOI] [Google Scholar]
- Hutt D, Nehari M, Munitz-Shenkar D, et al. (2015) Hematopoietic stem cell donation: psychological perspectives of pediatric sibling donors and their parents. Bone Marrow Transplantation 50: 1337–1342. DOI: 10.1038/bmt.2015.152. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Baxt C. (2007) Families of infants and young children with cancer: a post-traumatic stress framework. Pediatric Blood & Cancer 49: 1109–1113. DOI: 10.1002/pbc.21345. [DOI] [PubMed] [Google Scholar]
- Leclercq E, Leeflang MMG, van Dalen EC. and et al. (2013) Validation of search filters identifying pediatric studies in PubMed. The Journal of Pediatrics 162(3): 629–634.e2. DOI: 10.1016/j.jpeds.2012.09.012 10.1016/j.jpeds.2012.09.012. [DOI] [PubMed] [Google Scholar]
- Linder L, Bratton H, Nguyen A, et al. (2018) Symptoms and self-management strategies identified by children with cancer using draw-and-tell interviews. Oncology Nursing Forum 45(3): 290–300. DOI: 10.1188/18.ONF.290-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLeod KD, Whitsett SF, Mash EJ, et al. (2003) Pediatric sibling donors of successful and unsuccessful hematopoietic stem cell transplants (HSCT): a qualitative study of their psychosocial experience. Journal of Pediatric Psychology 28(4): 223–230. DOI: 10.1093/jpepsy/jsg010. [DOI] [PubMed] [Google Scholar]
- Mays N, Pope C, Popay J. (2005) Systematically reviewing qualitative and quantitative evidence to inform management and policy‐making in the health field. Journal of Health Services Research & Policy 10(Suppl 1): 6–20. [DOI] [PubMed] [Google Scholar]
- McNiff S. (2018) Philosophical and practical foundations of artistic inquiry: creating paradigms, methods, and presentations based in art. In: Leavy P. (ed) Handbook of Arts-Based Research. New York, NY: Guilford Press, 22–36. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6(7): e1000097. DOI: 10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouzzani M, Hammady H, Fedorowicz Z, et al. (2016) Rayyan—A web and mobile app for systematic reviews. Systematic Reviews 5(1): 210. DOI: 10.1186/s13643-016-0384-4 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Packman W. (1999) Psychosocial impact of BMT on pediatric siblings. Bone Marrow Transplantation 24: 701–706. [DOI] [PubMed] [Google Scholar]
- Packman WL, Beck VL, VanZutphen KH, et al. (2003) The human figure drawing with donor and nondonor siblings of pediatric bone marrow transplant patients. Art Therapy 20(2): 83–91. [Google Scholar]
- Packman WL, Crittenden MR, Rieger Fischer JB, et al. (1998) The kinetic family drawing with donor and nondonor siblings of pediatric bone marrow transplant patients. Art Therapy 15(3): 177–184. [Google Scholar]
- Packman WL, Crittenden MR, Schaeffer E, et al. (1997. a) Psychosocial consequences of bone marrow transplantation in donor and nondonor siblings. Journal of Developmental & Behavioral Pediatrics 18(4): 244–253. [PubMed] [Google Scholar]
- Packman WL, Crittenden MR, Rieger Fischer JB, et al. (1997. b) Siblings’ perceptions of the bone marrow transplantation process. Journal of Psychosocial Oncology 15(3–4): 81–105. DOI: 10.1300/J077v15n03_04. [DOI] [Google Scholar]
- Packman W, Gong K, VanZutphen K, et al. (2004) Psychosocial adjustment of adolescent siblings of hematopoietic stem cell transplant patients. Journal of Pediatric Oncology Nursing 21(4): 233–248. DOI: 10.1177/1043454203262698. [DOI] [PubMed] [Google Scholar]
- Packman WL, Weber S, Wallace J, et al. (2010) Psychological effects of hematopoietic SCT on pediatric patients, siblings and parents: a review. Bone Marrow Transplantation (italics), 45: 1134–1146. [DOI] [PubMed] [Google Scholar]
- Pelletier W, Hinds PS, Alderfer MA, et al. (2014) Themes reported by families as important when proceeding with pediatric hematopoietic stem cell transplantation. Pediatric Blood & Cancer 61: 1625–1631. DOI: 10.1002/pbc.25075. [DOI] [PubMed] [Google Scholar]
- Pelletier W, Schulte F, Guilcher GM. (2015) Pediatric hematopoietic stem cell donors: need for longitudinal medical and psychosocial surveillance. Pediatric Blood & Cancer 62: 737–738. DOI: 10.1002/pbc.25375. [DOI] [PubMed] [Google Scholar]
- Pentz RD, Alderfer MA, Pelletier W, et al. (2014) Unmet needs of siblings of pediatric stem cell transplant recipients. Pediatrics 133(5): e1156–e1162. DOI: 10.1542/peds.2013-3067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pentz RD, Pelletier W, Alderfer MA, et al. (2012) Shared decision‐making in pediatric allogeneic blood and marrow transplantation: what if there is no decision to make? The Oncologist 17: 881–885. DOI: 10.1634/theoncologist.2011-0446 10.1634/theoncologist.2011-0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pot-Mees CC, Zeitlin H. (1987) Psychosocial consequences of bone marrow transplantation in children: a preliminary communication. Journal of Psychosocial Oncology 5(2): 73–81. DOI: 10.1542/peds.2016-1057. [DOI] [Google Scholar]
- Pynoos RS, Frederick C, Nade K, et al. (1987) Life threat and posttraumatic stress in school-age children. Archives of General Psychiatry 44: 1057–1063. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Richmond BO. (1992) Revised Children’s Manifest Anxiety Scale. Los Angeles, CA: University of California. [Google Scholar]
- Rosenberg M. (1965) Society and the adolescent self-image. Princeton, NJ: Princeton University Press. [Google Scholar]
- Shah H, Mishra AK. (2021) Trauma and children: exploring posttraumatic growth among school children impacted by armed conflict in Kashmir. American Journal of Orthopsychiatry 91(1): 132–148. DOI: 10.1037/ort0000523 10.1037/ort0000523. [DOI] [PubMed] [Google Scholar]
- Sourkes BM. (2018) Children’s artwork. Child and adolescent psychiatric clinics of North America 27: 551–565. DOI: 10.1016/j.chc.2018.05.004 10.1016/j.chc.2018.05.004. [DOI] [PubMed] [Google Scholar]
- Stegenga K, Pentz RD, Alderfer MA, et al. (2019) Child and parent access to transplant information and involvement in treatment decision making. Western Journal of Nursing Research 41(4): 576–591. DOI: 10.1170/0193945918770440. [DOI] [PubMed] [Google Scholar]
- Stuber ML., Meeske KA, Krull KR, et al. (2010) Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics 125(5): e1124–e1134. DOI: 10.1542/peds.2009-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2014) SAMHSA’s concept of trauma and guidance for a trauma informed approach. MD Rockville: HHS Publication No.Substance Abuse and Mental Health Services Administration. (SMA) 14-4884. [Google Scholar]
- Switzer GE, Bruce J, Kiefer DM, et al. (2016) Health-related quality of life among pediatric hematopoietic stem cell donors. The Journal of Pediatrics 178: 164–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. (2004) TARGET ARTICLE: “Posttraumatic growth: conceptual foundations and empirical evidence”. Psychological Inquiry 15(1): 1–18. DOI: 10.1207/s15327965pli1501_01. [DOI] [Google Scholar]
- Tobin J, Allem J-P, Slaughter R, et al. (2018) Posttraumatic growth among childhood cancer survivors: associations with ethnicity, acculturation, and religious service attendance. Journal of Psychosocial Oncology 36(2): 175–188. DOI: 10.1080/07347332.2017.1365799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torraco RJ. (2005) Writing integrative literature reviews: guidelines and examples. Human Resource Development Review 4(3): 356–367. DOI: 10.1177/1534484305278283. [DOI] [Google Scholar]
- Van Schoors M, Caes L, Verhofstadt LL, et al. (2015) Systematic review: family resilience after pediatric cancer diagnosis: figure 1. Journal of Pediatric Psychology 40(9): 856–868. DOI: 10.1093/jpepsy/jsv055. [DOI] [PubMed] [Google Scholar]
- Wallace J, Packman W, Huffman LC, et al. (2014) Psychosocial changes associated with participation in art therapy interventions for siblings of pediatric hematopoietic stem cell transplant patients. Art Therapy 31(1): 4–11. DOI: 10.1080/07421656.2014.873685. [DOI] [Google Scholar]
- Weaver MS, Diekema DS, Carr A, et al. (2015) Matched marrow, sibling shadow: the epidemiology, experience, and ethics of sibling donors of stem cells. Journal of Adolescent and Young Adult Oncology 4(3): 100–104. DOI: 10.1089/jayao.2014.0051 10.1089/jayao.2014.0051. [DOI] [PubMed] [Google Scholar]
- White TE, Hendershot KA, Dixon MD, et al. (2017) Family strategies to support siblings of pediatric hematopoietic stem cell transplant patients. Pediatrics 139(2): e20161057. DOI: 10.1542/peds.2016-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whittemore R, Knafl K. (2005) The integrative review: updated methodology. Journal of Advanced Nursing 52(5): 546–553. [DOI] [PubMed] [Google Scholar]
- Wiener LS, Steffen-Smith E, Battles HB, et al. (2008) Sibling stem cell donor experiences at a single institution. Psychooncology 17: 304–307. DOI: 10.1002/pon.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener LS, Steffen-Smith E, Fry T, et al. (2007) Hematopoietic stem cell donation in children. Journal of Psychosocial Oncology 25(1): 45–66. DOI: 10.1002/pon.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins KL, Woodgate RL. (2007) An interruption in family life: siblings’ lived experience as they transition through the pediatric bone marrow transplant trajectory. Oncology Nursing Forum 34(2): e28–e35. DOI: 10.1188/07.ONF.E28-E35. [DOI] [PubMed] [Google Scholar]
- Zajac-Spychala O, Pieczonka A, Baranska M, et al. (2020) Long-term recipient health-related quality of life and donor-recipient relationship following sibling pediatric hematopoietic stem cell transplantation. Biology of Blood and Marrow Transplantation 26: 401–406. DOI: 10.1016/j.bbmt.2019.10.009 10.1016/j.bbmt.2019.10.009. [DOI] [PubMed] [Google Scholar]