Abstract
Labour induction involves helping a woman to start her labour, before labour begins on its own, for a vaginal birth with the aid of artificial methods, such as medications or other medical techniques. Labour induction is done in cases where extending the pregnancy can threaten the mother or her baby's health, and delivery should result in better outcomes than continuing the pregnancy. Currently, nearly 25% of babies are born by labour induction in economically developed countries. It is often necessary in certain situations to induce labour by using ripening techniques that not only soften the cervix but also make it thin and dilated. Mechanical or pharmacological approaches are used for the artificial induction of labour. Because research articles evaluating the safety and efficacy of various ripening techniques of the cervix vary in terms of their findings, it remains uncertain as to which is the best way to induce labour. In light of this, to find out the most popular interventions for ripening of the cervix during labour induction, we performed a review of the literature that compares the use of a Foley catheter and prostaglandins (misoprostol and dinoprostone). Our findings show that using misoprostol orally is much better than using it vaginally. Foley catheter proved to be the least effective induction technique, despite the fact that it offers the lowest risk.
Keywords: foley's catheter, dinoprostone, cervical ripening, prostaglandins, labour induction
Introduction and background
The use of artificial procedures that induce labour before the commencement of spontaneous labour and after the age of fetal viability is known as labour induction. Ripening of the cervix is crucial for successful labour induction. A sequence of biochemical processes that result in lower levels of collagen and glycosaminoglycans and an increase in water content soften and dilate the cervix throughout normal pregnancy, making it more conducive to natural labour or labour induction [1]. If this process does not succeed in a normal pregnancy, artificial ripening of the cervix is necessary. Cervical ripening and artificial labour induction have been used for centuries [2]. Currently, in more economically developed countries, nearly 25% of all babies are born by labour induction [3]. This process is chosen if the benefits of induction outweigh the risk of continuing a pregnancy [4]. In the absence of a not-so-favourable cervix, administering Pitocin or rupturing of membranes artificially is unlikely to induce labour successfully [5]. In these situations, it is often necessary to induce labour using ripening techniques that not only soften the cervix but also make it thin and dilated. Mechanical or pharmacological approaches are used for labour induction. A popular technique used for labour induction is placing a mechanical tool like a Foley catheter inside the cervical canal. This method was first described for labour induction in 1967 and is more cost-efficient than other mechanical procedures that had been used previously [6].
Examples of pharmacological techniques for inducing labour include the usage of prostaglandin, oxytocin, oestrogens, and mifepristone. In obstetrics and gynaecology, prostaglandins, which are cyclopentane derivatives of arachidonic acid, are frequently employed [7]. The only prostaglandin that the Food and Drug Administration (FDA) of the United States has approved for ripening of the cervix during labour induction is prostaglandin E2 (PGE2), also known as dinoprostone. Dinoprostone needs to be stored in cool temperatures and is expensive [8]. Misoprostol is a prostaglandin E1 (PGE1) analogue that has long been recommended to treat gastric ulcers brought on by non-steroidal anti-inflammatory drugs (NSAIDs) and is frequently used off-label to induce labour. Although the efficacy of misoprostol in the ripening of the cervix has been long established, some case reports have revealed that the frequency of significant consequences, such as uterine hyper-contractility and rupture, may be higher when compared to other techniques [9]. Because the findings of research articles evaluating the safety and efficacy of various ripening techniques of the cervix vary, it remains uncertain as to which is the best way to induce labour. Hence, in order to find out the most popular techniques for ripening the cervix during labour induction, we conducted a literature review that compares using a Foley catheter, misoprostol, and dinoprostone. Additionally, with a view to contributing to improving clinical practice and assisting with the design of the subsequent trials, we engaged in a thorough assessment of the available research [10].
Review
Methodology
Data Sources
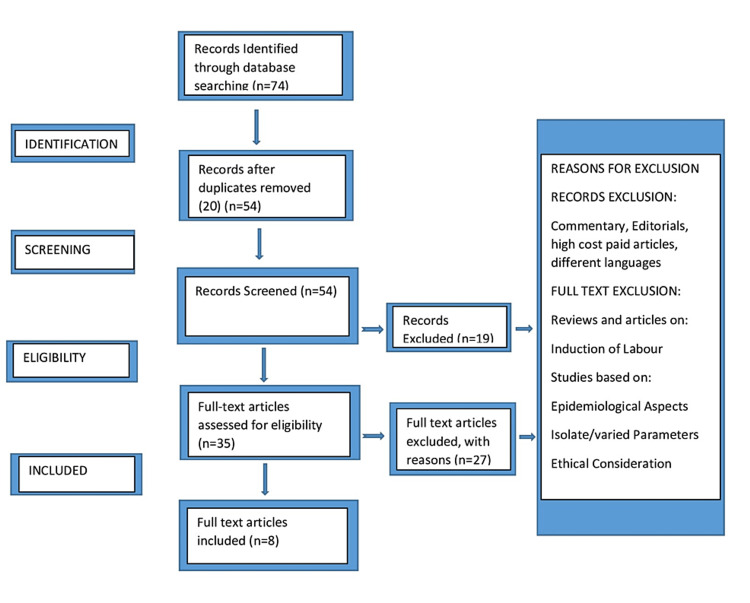
We looked for available research articles on cervical ripening or labour induction published up to 2022 with the help of keywords like "labour induction," "prostaglandin," and "foley catheter" on PubMed, Scopus, and Google Scholar databases. Around 74 articles were identified, out of which 20 articles were removed as they were duplicates. Finally, after a full-text article screening, eight articles were finalized to be reviewed. The reference list of related articles was likewise thought to be a reliable source of knowledge. No experiments were carried out to discover the unreported data (Figure 1). The exclusion criteria were as follows: a history of preterm birth, antepartum hemorrhage, placenta lying low, previous cesarean sections, current HSV infection, poly or oligohydramnios, hypertension, and any chronic illness or condition that would make the use of prostaglandin contraindicated. The procedures covered in this literature review are Foley catheter, intracervical dinoprostone, oral misoprostol, and vaginal misoprostol. We concentrated on three outcomes: induction-to-delivery interval, uterine overstimulation, and rate of cesarean delivery.
Figure 1. PRISMA flowchart depicting the study selection procedure.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Background
Labour induction starts the process of cervical thinning, uterine dilatation, and contraction, which leads to a baby being delivered artificially. When extending the pregnancy poses a risk to the health of the mother or her unborn child, it aims to end the pregnancy by a conventional vaginal delivery. The results of the delivery should be preferable to those of continuing the pregnancy. When labour is medically induced if the cervix is not mature, it will lead to challenges for the mother and fetus. Local insertion via Foley catheter, or PGE2 is regularly utilized, and numerous research has been conducted to determine the effectiveness in reducing the rate of cesarean deliveries [11-13]. The first step in the induction of labour in females with a not-so-favorable cervix is cervical ripening, which can be accomplished mechanically with a Foley catheter and, if done pharmacologically, can be achieved with PGE1 or PGE2 analogs. Over the past three decades, prostaglandins have largely replaced mechanical methods as the primary means of inducing labour in high-resource environments [13]. When asked about the delivery expectations of pregnant women, one of the main things they wanted is for their labour to be brief or short-lasting [14]. According to a questionnaire-based study that assessed how women view their birthing experiences regarding labour induction, a long induction-to-delivery interval appeared to be a significant determinant in patients' dissatisfaction with the delivery process [15]. Prolonged labour is directly linked to higher chances of postpartum fever, infections in newborns, and maternal chorioamnionitis. Therefore, when selecting a strategy for inducing labour, the induction-to-delivery interval should be considered [16]. We studied a total of eight articles, and the participants predominantly comprised singleton pregnancies in the third trimester of pregnancy with a cervix that happened to be unfavorable, intact membranes, and cephalic presentation of the fetus. And our study mainly focused on three outcomes: time between induction and delivery, uterine hyperstimulation, and frequency of cesarean delivery.
Induction-to-delivery interval
According to the studies by Mizrachi et al., Edwards et al., and Barda et al., the time between induction and delivery was lower in the Foley catheter group when compared with dinoprostone or misoprostol groups [17,18,19,20]. However, the study published by Henry et al. and Jozwiak et al. stated that the time between induction and delivery was faster with the usage of PGE2 [21]. Nevertheless, when there was a comparison between Foley+PGE2 and Foley catheter alone, the induction-to-delivery interval was shorter with the Foley+PGE2 group, as reported by Chowdhary et al. This is a significant finding as neither strategy resulted in hyperstimulation or infection but significantly decreased the induction-to-delivery interval with a similar Cesarean section rate [22,23]. Also, the time between induction and delivery was lower with Foley+PGE2 insert when compared with intravaginal PGE2 alone. We also studied a meta-analysis published by Chen et al., and it was found the time interval between induction and delivery was lower with misoprostol when compared with a Foley catheter; they reported that misoprostol is the best drug for faster induction of delivery [24]. However, none of these research articles mentioned the Foley catheter size, which we consider to be a major drawback.
Cesarean delivery rate
The study by Chen et al. reported that the probability of cesarean section was lowest with the use of oral misoprostol. All the other studies failed to show any marked difference in Cesarean delivery rate. However, among all the randomized controlled trials (RCT) we studied, Jozwiak et al.'s had the largest sample size, and in that study, they compared the use of PGE2 gel with the use of Foley catheter and found that cesarean section rate was similar in both. However, two major adverse events were also noted in the PGE2 gel group: perforation of the uterus and rupture of the uterus [18,20,23].
Uterine hyperstimulation
In the studies this article reviewed, there was a non-significant increase in the rate of uterine hyper-stimulation with the use of PGE2 when compared to Foley catheters. The survey done by Jozwiak et al. reported that the usage of a Foley catheter during induction appeared to reduce hyperstimulation of the uterus and postpartum bleeding, but this was also statistically insignificant. Also, the study by Chen et al. reported that the best method for preventing uterine hyperstimulation was the use of a Foley catheter, and the likelihood of vaginal misoprostol is considered a bad treatment method concerning hyperstimulation of the uterus and fetal heart alterations [20,23]. Another interesting study by Garg et al. stated that the hyperstimulation of the uterus was greater in the Foley+misoprostol group as compared to the Foley+dinoprostone group. But this finding was also statistically insignificant [13]. All in all, it can be suggested that the PGE1 analog misoprostol is the worst drug as far as uterine hyperstimulation is considered. However, the usage of a Foley catheter in addition to misoprostol increased the risk of chorioamnionitis. This may be due to the more frequent vaginal inspections required to administer misoprostol in repeated dosages [23]. However, the study by Garg et al. reported no such cases of chorioamnionitis, and this might be attributed to a single, one-time placement of prostaglandins, which may be intracervical or intravaginal. There are shreds of evidence to suggest that repeated doses of prostaglandins plus Foley increased the risk of chorioamnionitis, and hence the one-time placement of prostaglandin is advised [14,25,26,27,28] (Table 1).
Table 1. Studies comparing different induction techniques.
PGE2: prostaglandin E2
| Study | Statistical groups | Observed parameters | Inference |
| Mizrachi et al., Israel, 2016 [18] | 346 nulliparous females were equally divided into two study groups. The 1st group underwent induction of labour (IOL) using a Foley catheter, and the 2nd group underwent induction through PGE2 | Cesarean delivery rate, induction-delivery interval, amniotic fluid with meconium stain, oxytocin augmentation use, adverse maternal outcomes, and unfavorable neonatal outcomes | Induction to delivery was faster with a Foley catheter. Higher requirement for oxytocin augmentation in the Foley catheter group. Peripartum cord pH was slightly lesser in the PGE2 group. No change in the cesarean delivery rate |
| Garg et al., Chandigarh, India, 2021 [14] | 150 women were divided equally into two study groups. 1st group underwent IOL using misoprostol+Foley. The 2nd group underwent IOL using dinoprostone+Foley | Induction-delivery interval, change in the Bishop score, cesarean section rate, uterine hyperstimulation, and chorioamnionitis | No significant difference was observed in induction-to-delivery time and cesarean section rate. Change in the Bishop score was higher with the Foley+misoprostol group. No significant difference in uterine hyperstimulation. No cases of chorioamnionitis were observed |
| Chowdhary et al., Chandigarh, India, 2019 [23] | 110 women were divided equally into two study groups. Group 1 underwent IOL using an intracervical Foley. Group 2 underwent using Foley+PGE2 gel | Induction-delivery interval, cesarean delivery rate, uterine overstimulation, and chorioamnionitis | Induction to delivery was faster with Foley+PGE2 gel. No difference in the cesarean section rate. No uterine hyperstimulation or chorioamnionitis case was seen |
| Eser et al., Germany, 2018 [32] | 294 women were categorized into two groups. Group 1 underwent IOL using intravaginal PGE2 alone (n=148). Group 2 used Foley+PGE2 insert (n=146) | Induction-to-delivery time, duration of the latent phase | Induction to delivery was faster in group 2. The latent phase was more significant in group 1 |
| Edwards et al., Birmingham, Alabama, US, 2014 [19] | 376 women were randomized into two groups. Group 1 underwent IOL with a Foley catheter (n=185). Group2 underwent IOL with dinoprostone (n=191) | Induction-to-delivery time. The number of females delivering within 24 hours. Cesarean section rate | Induction-to-delivery time was shorter with the Foley catheter. More patients were delivered within 24 hours in the case of a Foley catheter. Cesarean delivery rate was more with dinoprostone, but the data was statistically non-significant |
| Jozwiak et al., Netherlands, 2011 [21] | 819 women were randomized into two groups. Group 1 (n=411) underwent IOL with a Foley catheter, and group 2 (n=408) underwent IOL with prostaglandin E2 | Cesarean delivery rate. The time between induction to delivery. Uterine hyperstimulation. Arterial cord pH. Oxytocin augmentation | Induction to delivery was faster with PGE2. IOL with PGE2 required lower oxytocin augmentation. No difference in the cesarean section rate |
| Barda et al., Israel, 2017 [20] | 300 women were equally randomized into two groups: n=150 for each group. The first group underwent IOL with a Foley catheter and the second group underwent IOL with dinoprostone | The time interval between induction to delivery. Induction of labour within 24 hours. Oxytocin augmentation. Cesarean delivery rate. Neonatal complications | The Foley catheter group reached active labour in a significantly shorter time. The need for oxytocin augmentation was more significant in the Foley catheter group. The difference in cesarean section rate was statistically non-significant. Both groups showed no difference in neonatal outcomes |
| Henry et al., Australia, 2013 [22] | 101 women were randomized into two groups. The first group (n=50) underwent IOL with a Foley catheter and the second group (n=51) underwent IOL with PGE2 | Vaginal delivery within 12 hours of induction. Vaginal delivery rate. Cesarean section rate. Oxytocin augmentation. The interval between the ripening of the cervix and vaginal delivery | Vaginal delivery within 12 hours was more with the usage of PGE2. The Foley catheter group required more oxytocin augmentation. The interval between the ripening of the cervix and vaginal delivery was shorter with PGE2 |
Limitations
This review has some limitations that warrant discussion. Firstly, we found that the evaluated research was quite heterogeneous. The main clinical heterogeneities pertain to the experience of inserting the research agent, the volume of the Foley catheter used, and the maximum timeframes from inserting the labour-inducing agent to removing it. Also, because relatively fewer study parameters were included in this analysis, subgroup analysis for these heterogeneities was not conducted. Moreover, we only included articles published in English and failed to discuss many other clinical scenarios such as mortality of the mother and perinatal death as these outcomes were not reported in the clinical trials. Evidence suggests that larger Foley catheters (60 or 80 ml) are more effective than smaller ones (30 ml) and that 24-hour Foley catheters are less effective than 12-hour ones [29-31].
Conclusions
In terms of the induction-to-delivery interval, the most efficient ways to induce labour in women with intact membranes after 28 weeks of pregnancy are vaginal misoprostol and dinoprostone; however, these methods are associated with an increased risk of uterine hyperstimulation and other complications like uterine perforation. The least successful induction technique is the use of a Foley catheter, but it also had the lowest risk of uterine hyperstimulation and alterations in the fetal heart rate. Oral misoprostol is a more efficient approach than vaginal misoprostol in terms of reducing the chance of a cesarean section and generating less uterine hyperstimulation with fetal heart rate variations. Additionally, it is advised that only one prostaglandin insert is used while using misoprostol in combination with Foley because repeated doses of prostaglandins in combination with Foley have been demonstrated to increase the risk of chorioamnionitis and uterine hyperstimulation. However, as described earlier, this study has a few limitations that warrant serious discussion.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.Ripening of the human uterine cervix related to changes in collagen, glycosaminoglycans, and collagenolytic activity. Uldbjerg N, Ekman G, Malmström A, Olsson K, Ulmsten U. Am J Obstet Gynecol. 1983;147:662–666. doi: 10.1016/0002-9378(83)90446-5. [DOI] [PubMed] [Google Scholar]
- 2.Combining medical and mechanical methods of cervical ripening. Does it increase the likelihood of successful induction of labor? Sullivan CA, Benton LW, Roach H, Smith LG Jr, Martin RW, Morrison JC. https://europepmc.org/article/med/8951132. J Reprod Med. 1996;41:823–828. [PubMed] [Google Scholar]
- 3.Births: preliminary data for 2010. Hamilton BE, Martin JA, Ventura SJ. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1040.8594&rep=rep1&type=pdf. Natl Vital Stat Rep. 2011;60:1–25. [PubMed] [Google Scholar]
- 4.Role of the cervix in the induction of labor. Jagani N, Schulman H, Fleischer A, Mitchell J, Randolph G. https://europepmc.org/article/med/7078845. Obstet Gynecol. 1982;59:21–26. [PubMed] [Google Scholar]
- 5.Induction of labor in the nineties: conquering the unfavorable cervix. Xenakis EM, Piper JM, Conway DL, Langer O. Obstet Gynecol. 1997;90:235–239. doi: 10.1016/S0029-7844(97)00259-7. [DOI] [PubMed] [Google Scholar]
- 6.The unfavourable cervix and induction of labour using a cervical balloon. Embrey MP, Mollison BG. J Obstet Gynaecol Br Commonw. 1967;74:44–48. doi: 10.1111/j.1471-0528.1967.tb03931.x. [DOI] [PubMed] [Google Scholar]
- 7.Non-hormonal methods for induction of labour. Lim CE, Ng RW, Xu K. Curr Opin Obstet Gynecol. 2013;25:441–447. doi: 10.1097/GCO.0000000000000027. [DOI] [PubMed] [Google Scholar]
- 8.Dinoprostone compared with misoprostol for cervical ripening for induction of labor at term. Church S, Van Meter A, Whitfield R. J Midwifery Womens Health. 2009;54:405–411. doi: 10.1016/j.jmwh.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Misoprostol for cervical ripening and labor induction: a meta-analysis. Sanchez-Ramos L, Kaunitz AM, Wears RL, Delke I, Gaudier FL. Obstet Gynecol. 1997;89:633–642. doi: 10.1016/S0029-7844(96)00374-2. [DOI] [PubMed] [Google Scholar]
- 10.Combination of direct and indirect evidence in mixed treatment comparisons. Lu G, Ades AE. Stat Med. 2004;23:3105–3124. doi: 10.1002/sim.1875. [DOI] [PubMed] [Google Scholar]
- 11.Ripening of the unfavorable cervix with extraamniotic catheter balloon: clinical experience and review. Sherman DJ, Frenkel E, Tovbin J, Arieli S, Caspi E, Bukovsky I. Obstet Gynecol Surv. 1996;51:621–627. doi: 10.1097/00006254-199610000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Pelvic scoring for elective induction. Bishop EH. https://journals.lww.com/greenjournal/Citation/1964/08000/Pelvic_Scoring_for_Elective_Induction.18.aspx. Obstet Gynecol. 1964;24:266–268. [PubMed] [Google Scholar]
- 13.A randomized trial of extra-amniotic saline infusion plus intracervical Foley catheter balloon versus prostaglandin E2 vaginal gel for ripening the cervix and inducing labor in patients with unfavorable cervices. Rouben D, Arias F. https://europepmc.org/article/med/8336880. Obstet Gynecol. 1993;82:290–294. [PubMed] [Google Scholar]
- 14.Comparison of intracervical Foley catheter combined with a single dose of vaginal misoprostol tablet or intracervical dinoprostone gel for cervical ripening: a randomised study. Garg R, Bagga R, Kumari A, Kalra J, Jain V, Saha SC, Kumar P. J Obstet Gynaecol. 2022;42:232–238. doi: 10.1080/01443615.2021.1904227. [DOI] [PubMed] [Google Scholar]
- 15.Women's expectations and experiences of childbirth. Gibbins J, Thomson AM. Midwifery. 2001;17:302–313. doi: 10.1054/midw.2001.0263. [DOI] [PubMed] [Google Scholar]
- 16.Women's perceptions, expectations and satisfaction with induced labour--a questionnaire-based study. Shetty A, Burt R, Rice P, Templeton A. Eur J Obstet Gynecol Reprod Biol. 2005;123:56–61. doi: 10.1016/j.ejogrb.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Time between membrane rupture and delivery and septicemia in term neonates. Herbst A, Källén K. Obstet Gynecol. 2007;110:612–618. doi: 10.1097/01.AOG.0000277632.36186.84. [DOI] [PubMed] [Google Scholar]
- 18.Induction of labor in nulliparous women with unfavorable cervix: a comparison of Foley catheter and vaginal prostaglandin E2. Mizrachi Y, Levy M, Bar J, Kovo M. Arch Gynecol Obstet. 2016;294:725–730. doi: 10.1007/s00404-016-4026-9. [DOI] [PubMed] [Google Scholar]
- 19.Foley catheter compared with the controlled-release dinoprostone insert: a randomized controlled trial. Edwards RK, Szychowski JM, Berger JL, Petersen M, Ingersoll M, Bodea-Braescu AV, Lin MG. Obstet Gynecol. 2014;123:1280–1287. doi: 10.1097/AOG.0000000000000238. [DOI] [PubMed] [Google Scholar]
- 20.Foley catheter versus intravaginal prostaglandins E2 for cervical ripening in women at term with an unfavorable cervix: a randomized controlled trial. Barda G, Ganer Herman H, Sagiv R, Bar J. J Matern Fetal Neonatal Med. 2018;31:2777–2781. doi: 10.1080/14767058.2017.1355906. [DOI] [PubMed] [Google Scholar]
- 21.Foley catheter versus vaginal prostaglandin E2 gel for induction of labour at term (PROBAAT trial): an open-label, randomised controlled trial. Jozwiak M, Oude Rengerink K, Benthem M, et al. Lancet. 2011;378:2095–2103. doi: 10.1016/S0140-6736(11)61484-0. [DOI] [PubMed] [Google Scholar]
- 22.Outpatient Foley catheter versus inpatient prostaglandin E2 gel for induction of labour: a randomised trial. Henry A, Madan A, Reid R, Tracy SK, Austin K, Welsh A, Challis D. BMC Pregnancy Childbirth. 2013;13:25. doi: 10.1186/1471-2393-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Comparison of intracervical Foley catheter used alone or combined with a single dose of dinoprostone gel for cervical ripening: a randomised study. Chowdhary A, Bagga R, Jasvinder Kalra, Jain V, Saha SC, Kumar P. J Obstet Gynaecol. 2019;39:461–467. doi: 10.1080/01443615.2018.1534090. [DOI] [PubMed] [Google Scholar]
- 24.A systematic review and network meta-analysis comparing the use of Foley catheters, misoprostol, and dinoprostone for cervical ripening in the induction of labour. Chen W, Xue J, Peprah MK, Wen SW, Walker M, Gao Y, Tang Y. BJOG. 2016;123:346–354. doi: 10.1111/1471-0528.13456. [DOI] [PubMed] [Google Scholar]
- 25.A prospective randomized controlled trial that compared misoprostol, Foley catheter, and combination misoprostol-Foley catheter for labor induction. Chung JH, Huang WH, Rumney PJ, Garite TJ, Nageotte MP. Am J Obstet Gynecol. 2003;189:1031–1035. doi: 10.1067/s0002-9378(03)00842-1. [DOI] [PubMed] [Google Scholar]
- 26.Cervical ripening and induction of labor with misoprostol, dinoprostone gel, and a Foley catheter: a randomized trial of 3 techniques. Barrilleaux PS, Bofill JA, Terrone DA, Magann EF, May WL, Morrison JC. Am J Obstet Gynecol. 2002;186:1124–1129. doi: 10.1067/mob.2002.123821. [DOI] [PubMed] [Google Scholar]
- 27.Combination of Foley bulb and vaginal misoprostol compared with vaginal misoprostol alone for cervical ripening and labor induction: a randomized controlled trial. Carbone JF, Tuuli MG, Fogertey PJ, Roehl KA, Macones GA. Obstet Gynecol. 2013;121:247–252. doi: 10.1097/AOG.0b013e31827e5dca. [DOI] [PubMed] [Google Scholar]
- 28.Concurrent use of Foley catheter and misoprostol for induction of labor: a randomized clinical trial of efficacy and safety. Lanka S, Surapaneni T, Nirmalan PK. J Obstet Gynaecol Res. 2014;40:1527–1533. doi: 10.1111/jog.12396. [DOI] [PubMed] [Google Scholar]
- 29.Cervical ripening: a randomized comparison between intravaginal misoprostol and an intracervical balloon catheter combined with intravaginal dinoprostone. Perry KG Jr, Larmon JE, May WL, Robinette LG, Martin RW. Am J Obstet Gynecol. 1998;178:1333–1340. doi: 10.1016/s0002-9378(98)70340-0. [DOI] [PubMed] [Google Scholar]
- 30.A randomized trial comparing a 30-mL and an 80-mL Foley catheter balloon for preinduction cervical ripening. Levy R, Kanengiser B, Furman B, Ben Arie A, Brown D, Hagay ZJ. Am J Obstet Gynecol. 2004;191:1632–1636. doi: 10.1016/j.ajog.2004.03.033. [DOI] [PubMed] [Google Scholar]
- 31.Labor induction with a Foley balloon inflated to 30 mL compared with 60 mL: a randomized controlled trial. Delaney S, Shaffer BL, Cheng YW, Vargas J, Sparks TN, Paul K, Caughey AB. Obstet Gynecol. 2010;115:1239–1245. doi: 10.1097/AOG.0b013e3181dec6d0. [DOI] [PubMed] [Google Scholar]
- 32.Transcervical Foley balloon catheter and vaginal prostaglandin E2 insert combination vs. vaginal prostaglandin E2 insert only for induction of labor at term: a randomized clinical trial. Eser A, Ozkaya E, Abide CY, et al. Arch Gynecol Obstet. 2019;299:451–457. doi: 10.1007/s00404-018-4998-8. [DOI] [PubMed] [Google Scholar]