Abstract
The purpose of this study is to investigate preeclampsia. It used the visualization tools of CiteSpace, VOSviewer, Gunnmap, Bibliometrix®, and Carrot2 to analyze 3,754 preeclampsia studies from 1985 to 2020 in Obstetrics and Gynecology areas. Carrot2 was used to explain each cluster in extra detail. The results found that there is an increasing trend in many publications related to preeclampsia from 1985 to 2020. The number of studies on preeclampsia has increased significantly in the last century. Analysis of the keywords found a strong relationship with preeclampsia concepts and keywords classified into five categories. Co-citation analysis was also performed which was classified into six categories. Reading the article offers important to support not only to grind the context of preeclampsia challenges but also to design a new trend in this field. The number of studies on preeclampsia has substantially improved over the decades ago. The findings of documents published from 1985 to 2020 showed three stages in research on this subject: 1985 to 1997 (a seeding stage), 1997–2005 (rapid growth stage), and 2005 onwards (development stage).
Keywords: bibliometric; preeclampsia; web of science database; co-citation; co-occurrence, theme evolution
Introduction
As one of the multisystem diseases during pregnancy, pre-eclampsia is a considerable cause of maternal and infant morbidity and mortality worldwide (Steegers et al., 2010). Over the past century, the term pre-eclampsia has evolved from a kidney-specific disease causing chronic nephritis to a state of toxaemia caused by circulating toxins (Phipps et al., 2016), characterized by hypertension and proteinuria appearing after 20 weeks of gestation. Pre-eclampsia affects approximately 5–7% of pregnancies (Witlin & Sibai, 1998). Recently, it has been redefined as de novo hypertension that manifests after 20 weeks of pregnancy and is accompanied by proteinuria (N300 mg/day), maternal organ dysfunction (including renal insufficiency, liver involvement, neurological or haematological problems), or uteroplacental dysfunction (potential cause of fetal growth restriction) (Tranquilli et al., 2014).
Bibliometric or citation analysis evaluates frequently cited articles in various disciplines, reviews the redundancy of the literature, assesses the quality of publications, highlights trends in research interest, and/or the evolution of scholarly publications over time. It is widely used in different medical fields and several studies using this approach have been published (Lee et al., 2019; Yadava et al., 2019), such as traumatic brain injury (Karydakis et al., 2019), artificial intelligence in the treatment of cerebrovascular disease and heart disease (Tran et al., 2019), IUGR (Kazemi Aski et al., 2020), and oral leukoplakia (Liu W et al., 2019).
To the best of our knowledge, no bibliometric research on preeclampsia has been performed. This study was therefore designed as a bibliometric analysis to evaluate pre-eclampsia articles from 1985 to 2020. To examine the data present in the WoS database, a quantitative literature search was employed. The relationships and impacts of key publications and related factors in this field were assessed using literature metrics, article ratings, and institutional and country ratings.
Our article makes several contributions to the advancement of literature. To uncover thinking flows, essential concepts, and developing issues with the potential to be included in future studies, we first utilized the quantitative bibliometric analysis method, which enables many numerous robust structured, and thorough inspections of this research subject. Subsequently, in order to demonstrate how the preeclampsia domain’s bounds have changed over time and give readers an immediate understanding of the deftly constructed increasing. Finally, we connected evolutionary paths with upcoming study directives to promote new preeclampsia study flows in the Obstetrics and Gynecology field.
Methods
Bibliometrics method
Bibliometrics is a systematic method that is broadly defined as a quantitative examination of published documents (Broadus, 1987; De Bellis, 2009). Using approaches such as content analysis, text analysis, citation analysis, keyword co-occurrence, co-citation analysis, or co-authoring analysis, Pritchard described bibliometrics as the application of mathematics and statistical methodologies to books and other media of communication (Pritchard, 1969; Dias, 2019). By highlighting the most significant articles, the bibliometric analysis might help the scholar avoid becoming overwhelmed by the massive amount of publications (Karydakis et al., 2019). Utilizing citation data, citation analysis quantifies the study’s influence as a reflection of the volume of citations a publication accumulates over time (Yadava et al., 2019). Additionally, citation analysis is employed to assess academic impacts (Liu et al., 2013). The papers with a high citation count are assumed to contain insightful suggestions for further studies (Jeung et al., 2011) and their authors are regarded as significant figures in the field (Butt et al., 2019).
The majority of bibliometric studies used citation analysis to determine the most popular papers, authors, journals, countries, co-authorship of authors, and keyword co-occurrences (Alarcon-Ruiz et al., 2019; Lee et al., 2019). Citation analysis has been applied in a variety of fields to identify the most significant publications (States et al., 2019). The frequency with which a text has been cited by other researchers can be determined using techniques of citation analysis (Xu et al., 2015). Citation analysis methods have recently made their way into the medical studies (Chen, 2004; Gupta et al., 2019).
Eligibility requirements, study selection, and data extraction
The study had nothing to do with the approval of ethical committees. The WoS database was used to retrieve the data for our study. Data were gathered in December 2020 utilizing the WoS database’s internet search engine. In this study, the authors conducted a comprehensive search of all papers using the term “Preeclampsia” as the search query. Only the “TITLE” was the subject of keyword searches. As a result, a group of 3754 papers written between 1985 and 2020 were gathered. Then, this collection was fixed as the foundation for all ensuing VOSviewer analyses. The application CiteSpace and VOSviewer (1.6.11) was used to create bibliometric network visualizations (Chen, 2004; Van Eck & Waltman, 2009).
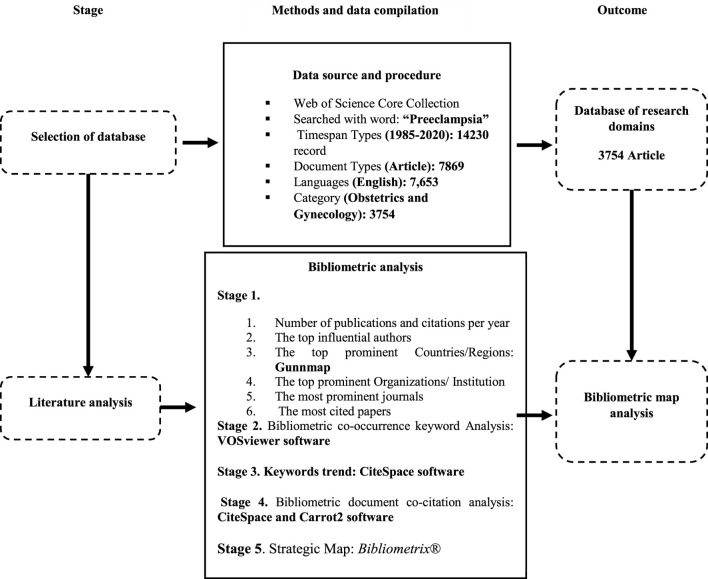
A review of the literature revealed that 14,230 publications about preeclampsia were published between 1985 and 2020. Article (3,754), Proceedings Paper (221), Early Access (62), and book chapter are among these publications (13). In this study, 7,653 of the 7,869 English-language papers that fall under the category of obstetrics and gynaecology were examined. The total number of articles eventually decreased to 3,754 (Figure 1).
FIGURE 1.
Methodological approach (Author’s Presentation).
Data synthesis
Country maps were created using Gunnmap. VOSviewer software was used to examine the bibliometric co-occurrence keyword analysis, CiteSpace for the analysis of keywords trends, Carrot2 for the analysis of bibliometric document co-citations, and Bibliometrix® for the analysis of the strategic map.
Results
Distribution of published preeclampsia papers per year
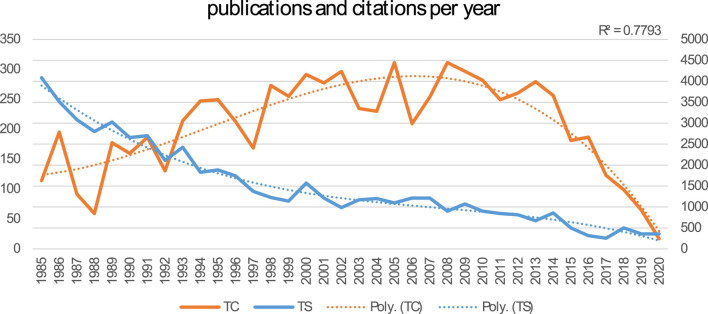
A total of 3,495 papers were included. Figure 2 shows the growth in preeclampsia research from 1985 to 2020 in terms of publications (total studies/TS) and citations (total citations/TC) each year. Over half of the articles (51% of them) were published within the last 10 years.
FIGURE 2.
Number of publications and citations per year from 1985 to 2020.
Authors with the most publications in the preeclampsia discipline
The top 20 document-producing authors, nations/regions, and organizations/institutions are recognized. The ranked authors who reproduced preeclampsia articles between 1985 and 2020 were Sibai, B.M. (TS = 98); Roberts, J.M. (TS = 64); Romero, R. (TS = 55); Nicolaides, K.H. (TS = 48); Martin, JN (TS = 32); Chaiworapongsa, T (TS = 30); Hassan, S.S. (TS = 29); Steegers EAP (TS = 28); Baker PN (TS = 27); Saade GR (TS = 27); Staff, A.C. (TS = 28); Dekker, G.A. (TS = 26); Erez O (TS = 26); Van Pampus MG (TS = 26); Nisell H (TS = 25); Karumanchi, S.A. (TS = 24); Redman CWG (TS = 24); Von Dadelszen P (TS = 24); Wang YP (TS = 24); and Franx A (TS = 22).
Countries/regions with the most publications in the preeclampsia discipline
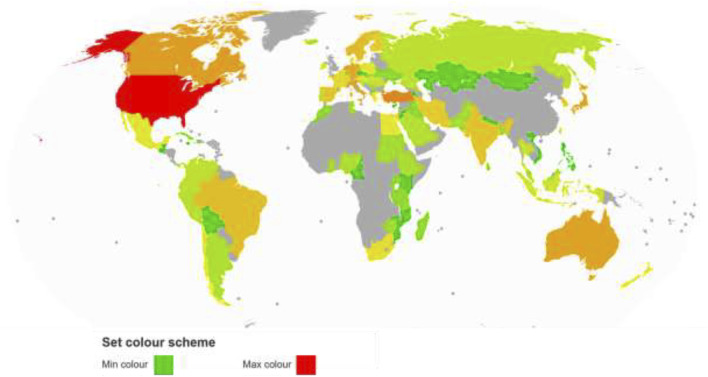
The number of articles generated by each region and the total number of citations each country has on the examined study area define the impact of the most productive regions. We select the top 20 document-producing areas in the preeclampsia field of research. The “United States” is the first dominant region (TS = 1200, TC = 49,692), and after that “Peoples R China” (TS = 311, TC = 3307) and “England” (TS = 262, TC = 12,342). Another region with a high number of publications is Turkey (TS = 232), followed by the Netherlands (TS = 196), Canada (TS = 162), Italy (TS = 152), Japan (TS = 149), Australia (TS = 145), Israel (TS = 131), Germany (TS = 130), Norway (TS = 101), Sweden (TS = 93), Brazil (TS = 91), India (TS = 80), Spain (TS = 79), South Korea (TS = 72), Iran (TS = Figure 3 displays a map of the study-based regions in red (highest) and green (lowest) colours.
FIGURE 3.
Regions map based on documents.
Organizations/institutions with the most publications in the preeclampsia discipline
The study includes 2359 institutions from various geographical areas. The top 20 organisations with the most publications are listed below. The impact of the most productive organisations in the preeclampsia discipline is determined by the total number of documents printed by each organisation and the total number of citations. The three most significant universities are the “University of Texas system” (TS = 108, TC = 3845), “Harvard University” (TS = 104, TC = 4124), and “The Pennsylvania Commonwealth System of Higher Education/PCSHE” (TS = 99, TC = 5616). Other institutions with the highest publications include, ‘The University of London’ (TS = 97, TC = 97), ‘The University of Pittsburgh’ (TS = 95, TC = 5463); ‘NIH USA’ (TS = 92, TC = 5949), ‘The University of Tennessee system’ (TS = 86, TC = 6219), ‘University of Tennessee health science center’ (TS = 84, TC = 6150), ‘NIH Eunice Kennedy Shriver national institute of child health human development NICHD’ (TS = 79, TC = 5448), ‘University of California system’ (TS = 78, TC = 4319); ‘Wayne State University’ (TS = 76, TC = 4518); ‘Magee Women’s research institute’ (TS = 69, TC = 4082), and ‘Kings College London’ (TS = 67, TC = 3426), ‘University of Oslo’ (TS = 59, TC = 2117); ‘Karolinska Institutet’ (TS = 57, TC = 1320), and ‘Erasmus university Rotterdam’ (TS = 54, TC = 1248); ‘The University of Cincinnati’ (TS = 52, TC = 3118), ‘The University of Groningen’ (TS = 52, TC = 1361), ‘King S College Hospital’ (TS = 51, TC = 2435), and ‘King S college hospital NHS foundation trust’ (TS = 51, TC = 2435).
Journals with the most publications in the preeclampsia discipline
This section introduces the 20 top Journals in order. The ‘AJOG’ is the most influential journal, with 41,991 total citations (TS = 622). The ‘Hypertension in Pregnancy’ (7247 citations, TS = 447), the ‘Journal of Maternal Fetal and Neonatal Medicine’ (3911 citations, TS = 297), the ‘Pregnancy hypertension an international journal of Womens cardiovascular health’ (1691 citations, TS = 280), the ‘Obstetrics and Gynecology’ (15,156 citations, TS = 267), the ‘Placenta’ (6038 citations, TS = 209), the ‘European journal of obstetrics gynecology and reproductive biology’ (3599 citations, TS = 152), the ‘Acta Obstetricia et Gynecologica Scandinavica’ (2763 citations, TS = 113), the ‘Reproductive sciences’ (1988 citations, TS = 113), the ‘Gynecologic and obstetric investigation’ (1948 citations, TS = 109), the ‘Archives of gynecology and obstetrics’ (1077 citations, TS = 88), the ‘American Journal of Perinatology’ (1029 citations, TS = 82), the ‘BMC Pregnancy and Childbirth’ (826 citations, TS = 79), the ‘Journal of Perinatal Medicine’ (1295 citations, TS = 79), the ‘Prenatal diagnosis’ (1377 citations, TS = 52), the ‘Clinical and Experimental Obstetrics Gynecology’ (277 citations, TS = 47), the ‘Fetal diagnosis and therapy’ (1159 citations, TS = 44), the ‘Journal of Reproductive Medicine’ (451 citations, TS = 43), the ‘British Journal of Obstetrics and Gynaecology’ (BJOJ) (3928 citations, TS = 41), the ‘Journal of the society for gynecologic investigation’ (1048 citations, TS = 40).
Most-cited documents in preeclampsia discipline
The most cited documents involved Roberts et al. (1989) (N = 1466); Khong et al. (1986) (N = 1247); Sacks et al. (1998) (N = 607) and Walsh (1985) (N = 546) respectively (Table 1). Also, the results found that 24 (out of 30 most cited) of the documents were clinical and research papers and 6 of the documents were literature reviews. About 18 articles were published in ‘AJOG’. Table 2.
TABLE 1.
The most cited authors, countries, organizations, and journals in the preeclampsia discipline.
| Authors | TS | TC | Countries/Regions | TS | TC | Organizations/Institution | TS | TC | Journals | TS | TC | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | SibaiB.M. | 98 | 7420 | United States of America | 1200 | 49,708 | University of Texas System | 108 | 3845 | AJOG | 622 | 41,991 |
| 2 | RobertsJ.M. | 64 | 5824 | Peoples R China | 311 | 3311 | Harvard University | 104 | 4124 | Hypertension in Pregnancy | 447 | 7247 |
| 3 | Romero, R | 55 | 3900 | England | 262 | 12,347 | PCSHE | 99 | 5616 | Journal of Maternal-Fetal and Neonatal Medicine | 297 | 3911 |
| 4 | NicolaidesK.H. | 48 | 2154 | Turkey | 232 | 3163 | University of London | 97 | 4191 | Pregnancy hypertension an international journal of Women’s cardiovascular health | 280 | 1691 |
| 5 | Martin, JN | 32 | 1414 | Netherlands | 196 | 6583 | University of Pittsburgh | 95 | 5463 | Obstetrics and Gynecology | 267 | 15,156 |
| 6 | Chaiworapongsa, T | 30 | 2108 | Canada | 162 | 5922 | NIH United States of America | 92 | 5949 | Placenta | 209 | 6038 |
| 7 | HassanS.S. | 29 | 1612 | Italy | 152 | 3712 | University of Tennessee system | 86 | 6219 | European journal of obstetrics gynaecology and reproductive biology | 152 | 3599 |
| 8 | Steegers EAP | 28 | 701 | Japan | 149 | 3545 | University of Tennessee health science center | 84 | 6150 | Acta Obstetricia et Gynecologica Scandinavica | 113 | 2763 |
| 9 | Baker PN | 27 | 990 | Australia | 145 | 3019 | NIH Eunice Kennedy Shriver national institute of child health human development NICHD | 79 | 5448 | Reproductive sciences | 113 | 1988 |
| 10 | Saade GR | 27 | 1052 | Israel | 131 | 3490 | University of California system | 78 | 4319 | Gynecologic and obstetric investigation | 109 | 1948 |
| 11 | StaffA.C. | 27 | 1087 | Germany | 130 | 3148 | Wayne State University | 76 | 4518 | Archives of gynaecology and obstetrics | 88 | 1077 |
| 12 | DekkerG.A. | 26 | 1719 | Norway | 101 | 4276 | MAGEE Womens research institute | 69 | 4082 | American Journal of Perinatology | 82 | 1029 |
| 13 | Erez O | 26 | 1167 | Sweden | 93 | 2715 | Kings College London | 67 | 3426 | BMC Pregnancy and Childbirth | 79 | 826 |
| 14 | Van Pampus MG | 26 | 548 | Brazil | 91 | 1148 | University of Oslo | 59 | 2117 | Journal of Perinatal Medicine | 79 | 1295 |
| 15 | Nisell H | 25 | 622 | India | 80 | 696 | Karolinska Institutet | 57 | 1320 | Prenatal diagnosis | 52 | 1377 |
| 16 | KarumanchiS.A. | 24 | 1254 | Spain | 79 | 1631 | ERASMUS University Rotterdam | 54 | 1248 | Clinical and Experimental Obstetrics Gynecology | 47 | 277 |
| 17 | Redman CWG | 24 | 1838 | South Korea | 72 | 1708 | University of Cincinnati | 52 | 3118 | Fetal diagnosis and therapy | 44 | 1159 |
| 18 | Von Dadelszen P | 24 | 1401 | Iran | 69 | 491 | University of Groningen | 52 | 1361 | Journal of Reproductive Medicine | 43 | 451 |
| 19 | Wang YP | 24 | 1149 | Finland | 65 | 2423 | King S College Hospital | 51 | 2435 | British Journal of Obstetrics and Gynaecology | 41 | 3928 |
| 20 | Franx A | 22 | 632 | France | 53 | 967 | King S College hospital NHS foundation trust | 51 | 2435 | Journal of the society for gynecologic investigation | 40 | 1048 |
TABLE 2.
The top studies within the preeclampsia discipline.
| References | Source | Citation | Citation per year | Research type |
|---|---|---|---|---|
| Roberts et al. (1989) | AJOG | 1466 | 44.42 | Literature review |
| Khong et al. (1986) | BJOJ | 1247 | 34.64 | Literature review |
| Sacks et al. (1998) | AJOG | 607 | 25.29 | Clinical |
| Walsh (1985) | AJOG | 546 | 14.76 | Clinical |
| Gilstrap & Ramin (2002) | Obstetrics and Gynecology | 534 | 26.7 | Clinical |
| von Dadelszen et al. (2003) | Hypertension in Pregnancy | 475 | 25 | Literature review |
| Romero et al. (2008) | Journal of Maternal-Fetal & Neonatal Medicine | 454 | 32.43 | Clinical |
| Sibai et al. (1986b) | AJOG | 445 | 12.36 | Clinical |
| Roberts & Hubel (2009) | Placenta | 441 | 33.92 | Literature review |
| Dekker, et al. (1995) | AJOG | 424 | 15.7 | Clinical |
| MacKay et al. (2001) | Obstetrics and Gynecology | 414 | 19.71 | Clinical |
| Kurki et al. (2000) | Obstetrics and Gynecology | 390 | 17.73 | Clinical |
| Ness & Roberts (1996) | AJOG | 382 | 14.69 | Literature review |
| Ishihara et al. (2002) | AJOG | 380 | 19 | Clinical |
| Sibai et al. (1995) | AJOG | 362 | 13.41 | Clinical |
| Sibai et al. (1997) | AJOG | 361 | 14.44 | Clinical |
| Saftlas et al. (1990) | AJOG | 358 | 11.19 | Clinical |
| Lisonkova & Joseph (2013) | AJOG | 347 | 38.56 | Clinical |
| Vince et al. (1995) | BJOJ | 338 | 12.52 | Clinical |
| Yallampalli & Garfield (1993) | AJOG | 330 | 11.38 | Clinical |
| Pineles et al. (2007) | AJOG | 322 | 21.47 | Clinical |
| Allaire et al. (2000) | Obstetrics and Gynecology | 320 | 14.55 | Clinical |
| Seligman et al. (1994) | AJOG | 314 | 11.21 | Clinical |
| Villar et al. (2006) | AJOG | 307 | 19.19 | Clinical |
| Sibai et al. (1994) | AJOG | 301 | 10.75 | Clinical |
| Akolekar et al. (2013) | Fetal Diagnosis and Therapy | 287 | 31.89 | Clinical |
| Ødegård et al. (2000) | Obstetrics and Gynecology | 281 | 12.77 | Clinical |
| Sibai et al. (1986a) | AJOG | 276 | 7.67 | Clinical |
| Rodgers et al. (1988) | AJOG | 270 | 7.94 | Clinical |
| Burton et al. (2009) | Placenta | 269 | 20.69 | Literature review |
Hot topics in the preeclampsia research
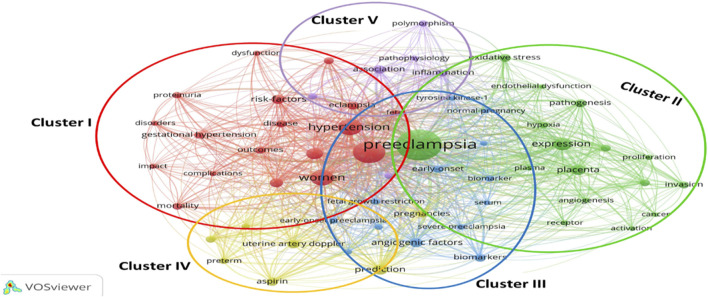
One of the best bibliometrics methods is keyword analysis. The evolution of a scientific domain is discovered using the co-occurrence method (Zhu et al., 2019). The co-occurrence technique is reliable and useful for selecting the most beneficial themes over time (Wang et al., 2018). Figure 4 shows the five clusters that were created from the 60 keywords (minimum keywords, 10 times): cluster one (n = 18 items), cluster two (n = 16), cluster three (n = 13), cluster four (n = 7), and cluster five (n = 6 things). The material for each cluster is displayed in Table 3.
FIGURE 4.
Co-occurrence map.
TABLE 3.
Classification of keywords based on clusters.
| Cluster | Keywords |
|---|---|
| Cluster 1: 18 items Management of Preeclampsia |
Cardiovascular-Disease, Complications, Disease, Disorders, Dysfunction, Eclampsia, Fetal, Gestational Hypertension, Hypertension, Hypertensive Disorders, Impact, Management, Mortality, Outcomes, Pregnancy, Proteinuria, Risk-Factors, Women |
| Cluster 2: 16 items Diagnosis of Preeclampsia |
Activation, Angiogenesis, Cancer, Endothelial Dysfunction, Expression, Hypoxia, Invasion, Migration, Oxidative Stress, Pathogenesis, Placenta, Plasma, Preeclampsia, Proliferation, Receptor, Trophoblast |
| Cluster 3: 13 items The role of Biomarkers in Preeclampsia |
Angiogenic Factors, Biomarker, Biomarkers, Early-Onset, Early-Onset Preeclampsia, Fetal, Growth Restriction, Late-Onset Preeclampsia, Normal-Pregnancy, Plgf, Serum, Severe, Preeclampsia, Soluble Endoglin, Tyrosine Kinase-1 |
| Cluster 4: 7 items The role of Asprin in Preeclampsia |
Aspirin, Growth Restriction, Low-Dose Aspirin, Prediction, Pregnancies, Preterm, Uterine Artery Doppler |
| Cluster 5: 6 items Preeclampsia and IUGR |
Association, Blood-Pressure, Inflammation, Intrauterine Growth Restriction, Pathophysiology, Polymorphism |
Keywords trend
Topics that are expanding quickly in the field of preeclampsia were found by analyzing the frequency of keywords in subject categories. In Table 4, there are a few thematic groups with bursts and thorough details on the 25 thematic groups with the most powerful citation bursts. Preeclampsia, prostacyclin, endothelium, and thromboxane are identified by CiteSpace’s burst detection as the five topic areas with the most intense citation bursts. During a specific time, these topics were active research areas. Table 5 displays every colour section according to a timeline. A red line segment showing the beginning and finish of the burst duration is used to denote the length of a burst in a subject category. Pregnancy-induced hypertension, for instance, revealed a time of burst from 1992 to 2006 with a burst strength of 39.91 at the top of the list. The number of documents in the “pregnancy-induced hypertension” domain increased significantly between 1992 and 2006, indicating that preeclampsia research in this field was active at the time. Preeclampsia research has recently focused on topics including “cardiovascular disease,” “diagnosis,” “early onset,” “fetal growth restriction,” and “aspirin”.
TABLE 4.
Top keywords with the strongest citation bursts.
| Keywords | Year | Freq | Burst | Degree | Centrality | Strength | Begin | End | 1992–2020 |
|---|---|---|---|---|---|---|---|---|---|
| Pregnancy Induced Hypertension | 1992 | 123 | 39.91 | 24 | 0.14 | 36.9 | 1992 | 2006 |

|
| Preeclampsia | 1992 | 64 | 33.83 | 15 | 0.02 | 31.25 | 1992 | 2003 |

|
| Prostacyclin | 1992 | 42 | 22.15 | 19 | 0.06 | 20.35 | 1992 | 2003 |

|
| Endothelium | 1992 | 24 | 12.63 | 12 | 0.01 | 11.41 | 1992 | 2004 |

|
| Thromboxane | 1992 | 23 | 12.10 | 12 | 0.01 | 11.29 | 1992 | 2003 |

|
| Endothelial Cell | 1992 | 44 | 19.22 | 22 | 0.06 | 15.51 | 1993 | 2003 |

|
| Rat | 1992 | 27 | - | 17 | 0.04 | 12.51 | 1994 | 2000 |

|
| Nitric Oxide | 1992 | 59 | 24.35 | 20 | 0.06 | 18.51 | 1995 | 2007 |

|
| Activation | 1992 | 74 | 21.53 | 21 | 0.06 | 18.81 | 1996 | 2009 |

|
| Lipid Peroxidation | 1992 | 42 | 18.22 | 14 | 0.02 | 11.86 | 1996 | 2005 |

|
| Insulin Resistance | 1992 | 42 | 17.61 | 9 | 0.01 | 13.25 | 2005 | 2012 |

|
| Soluble Endoglin | 1992 | 66 | 17.93 | 12 | 0.01 | 15.37 | 2007 | 2014 |

|
| Gene Expression | 1992 | 40 | 11.75 | 4 | 0.00 | 12.05 | 2009 | 2015 |

|
| Circulating Angiogenic Factor | 1992 | 39 | 12.59 | 14 | 0.02 | 13.44 | 2010 | 2014 |

|
| Placental Growth Factor | 1992 | 100 | 14.61 | 15 | 0.02 | 12.95 | 2012 | 2020 |

|
| Angiogenic Factor | 1992 | 170 | 16.46 | 18 | 0.03 | 19.15 | 2013 | 2017 |

|
| Biomarker | 1992 | 103 | 16.65 | 15 | 0.02 | 18.06 | 2013 | 2020 |

|
| Prediction | 1992 | 200 | 4.44 | 19 | 0.05 | 13.77 | 2013 | 2020 |

|
| Uterine Artery Doppler | 1992 | 136 | 11.33 | 14 | 0.01 | 11.08 | 2013 | 2016 |

|
| Prevention | 1992 | 119 | 18.43 | 14 | 0.03 | 14.97 | 2014 | 2020 |

|
| Cardiovascular Disease | 1992 | 75 | 12.58 | 6 | 0.00 | 13.42 | 2014 | 2020 |

|
| Diagnosis | 1992 | 93 | 18.33 | 13 | 0.02 | 21.72 | 2015 | 2020 |

|
| Early Onset | 1992 | 40 | 16.56 | 2 | 0.00 | 14.1 | 2016 | 2020 |

|
| Fetal Growth Restriction | 1992 | 63 | 14.97 | 6 | 0.00 | 13.5 | 2016 | 2020 |

|
| Aspirin | 1992 | 54 | 16.81 | 13 | 0.02 | 14.1 | 2017 | 2020 |

|
TABLE 5.
The first five authors contribute to selected clusters.
| Freq | Burst | Centrality | Source | References | Cluster | Carrot analysis |
|---|---|---|---|---|---|---|
| 32 | 19.57 | 0.17 | Lancet | Roberts and Redman (1993) | 0 |
|
| 24 | 13.98 | 0.06 | Am J Obstet Gynecol | Dekker and Sibai (1998) | 0 | |
| 23 | 14.13 | 0.19 | Am J Obstet Gynecol | Dekker et al. (1995) | 0 | |
| 22 | 12.23 | 0.19 | New Engl J Med | Kupferminc et al. (1999) | 0 | |
| 17 | 10.20 | 0.00 | New Engl J Med | Schobel et al. (1996) | 0 | |
| 25 | 16.41 | 0.10 | Am J Obstet Gynecol | Roberts et al. (1989) | 1 |
|
| 20 | 12.03 | 0.35 | Am J Obstet Gynecol | Seligman et al. (1994) | 1 | |
| 13 | 8.15 | 0.00 | Clin Perinatol | Friedman et al. (1991) | 1 | |
| 12 | 7.52 | 0.05 | Am J Obstet Gynecol | Pinto et al. (1991) | 1 | |
| 11 | 6.89 | 0.01 | Am J Hypertens | Roberts et al. (1991) | 1 | |
| 70 | 36.46 | 0.15 | New Engl J Med | Levine et al. (2004) | 2 |
|
| 55 | 29.76 | 0.54 | J Clin Invest | Maynard et al. (2003) | 2 | |
| 52 | 31.12 | 0.03 | Am J Obstet Gynecol | AuthorAnonymous (2000) | 2 | |
| 40 | 23.39 | 0.59 | Am J Obstet Gynecol | Redman et al. (1999) | 2 | |
| 33 | 18.93 | 0.25 | Lancet | Roberts & Cooper (2001) | 2 | |
| 186 | 93.38 | 0.20 | Obstet Gynecol | Roberts JM et al. (2013) | 3 |
|
| 63 | 00.00 | 0.02 | Pregnancy Hypertens | Tranquilli et al. (2014) | 3 | |
| 62 | 29.47 | 0.09 | New Engl J Med | Rolnik et al. (2018) | 3 | |
| 51 | 23.56 | 0.05 | Lancet | Mol et al. (2016) | 3 | |
| 49 | 22.62 | 0.03 | New Engl J Med | Zeisler et al. (2016) | 3 | |
| 82 | 41.70 | 0.02 | Lancet | Steegers et al. (2010) | 4 |
|
| 50 | 27.55 | 0.03 | Semin Perinatol | Duley (2009) | 4 | |
| 45 | 18.83 | 0.27 | Am J Obstet Gynecol | Lisonkova & Joseph (2013) | 4 | |
| 45 | 16.07 | 0.08 | Fetal Diagn Ther | Akolekar et al. (2013) | 4 | |
| 43 | 21.53 | 0.01 | Obstet Gynecol | Bujold et al. (2010) | 4 | |
| 73 | 39.03 | 0.00 | Lancet | Sibai et al. (2005) | 5 |
|
| 67 | 35.74 | 0.00 | Science | Redman & Sargent (2005) | 5 | |
| 62 | 31.23 | 0.23 | New Engl J Med | Levine et al. (2006) | 5 | |
| 47 | 23.53 | 0.20 | Nat Med | Venkatesha et al. (2006) | 5 | |
| 47 | 22.53 | 0.76 | J Matern-Fetal Neo M | Romero et al. (2008) | 5 |
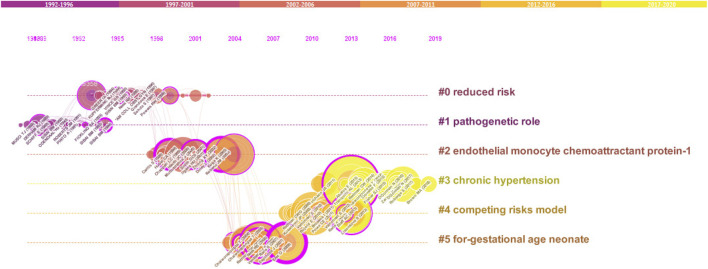
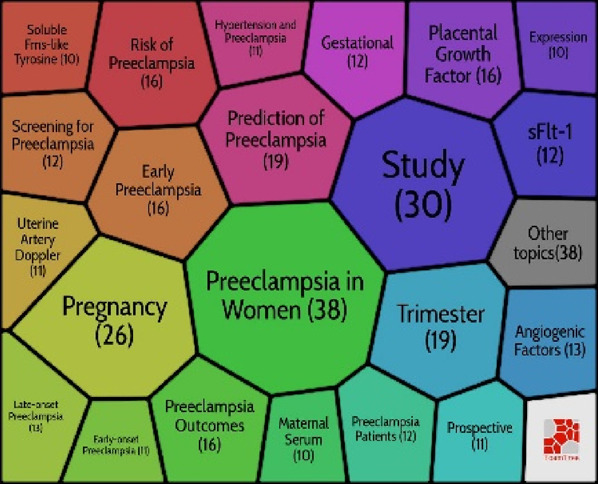
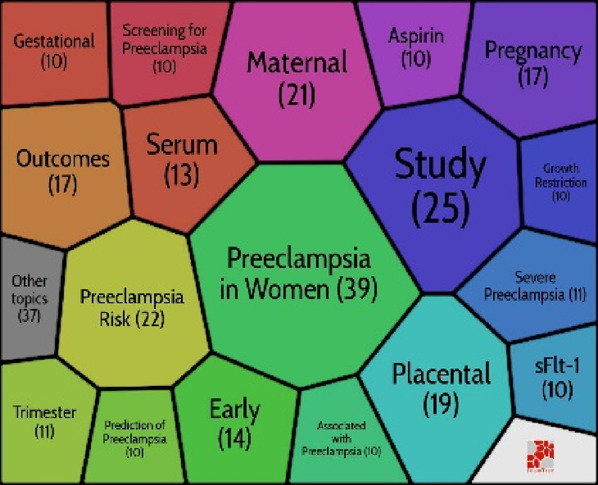
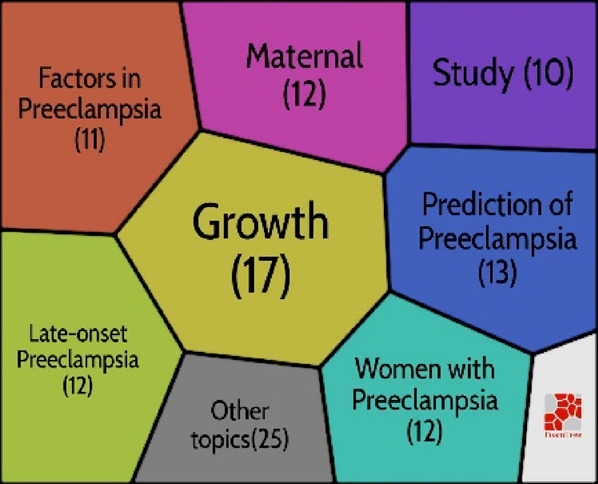
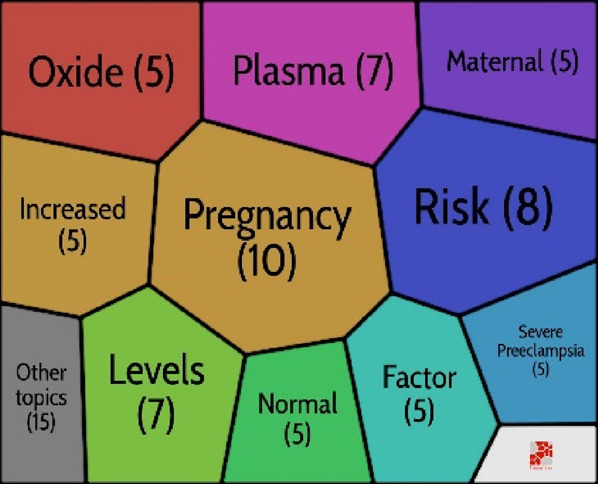
Co-citation network
Co-citation analysis is an effective technique that has gained widespread acceptance in several fields for accurately defining and visualising the intellectual structure of a study topic. In light of this, we decided to analyse the discipline’s structure using co-citation network analysis. Citespace software was used to investigate the preeclampsia discipline, which has its intellectual foundation in particular in the cited references. A network with 187 nodes and 598 edges was generated using document co-citation reference analysis in Citespace and the parameter settings: Slice length = 5; pruning: pathfinder; top N per slice: 30; top N%: 10%. (Figure 5). The LLR algorithm and title were used to cluster articles. Six clusters were ultimately procured, and Citespace gave them names automatically.
FIGURE 5.
Co-citation grid of cited references.
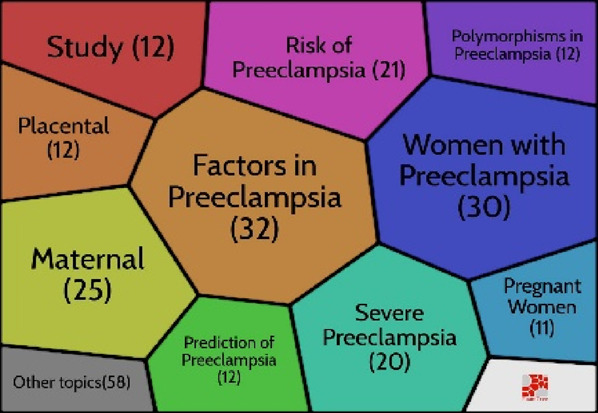
By using Carrot2, the clusters were deduced. To discover more about these clusters, the Carrot2 using the lingo algorithm was utilised on each cluster. The results showed that clusters #3 and #4 were the most recent clusters, while cluster #0 was the largest and oldest. Silhouette values of all clusters are bigger than 0.93. With 34 articles spread across 16 years, from 1985 to 2001, Cluster #0 is the largest cluster. Cluster #0 has a high degree of consistency, as evidenced by its Silhouette value of 0.936. Considering that Cluster #0 is the main cluster, its themes have been spread very widely. Carrot2 is capable of algorithmically managing the primary themes that are gleaned from the titles, keywords, and abstracts of cited documents (Table 5). The second-largest cluster, Cluster #1, contains 33 articles over the 10 years of 1985–1995 (Silhouette = 0.952). Cluster #3 is the most recent cluster (Silhouette = 0.992), and replicates significant events related to the risk of preeclampsia, placenta, sFlt-1, trimester, and growth restriction. Clusters #2, #4, and #5 all have silhouette values of 0.957, 0.949, and 0.935, respectively.
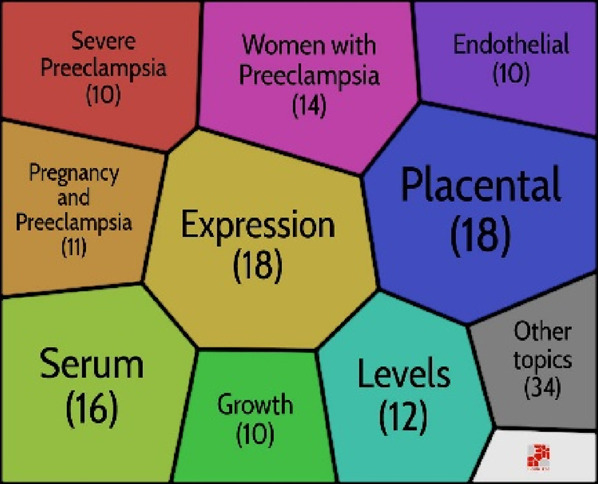
Theme evolution: Strategic map in preeclampsia
Many keywords only occasionally appeared, therefore they undoubtedly had a significant impact on the key topic of preeclampsia. We involved the study’s title keywords. Using Bibliometrix®, a strategic map is created to examine the most important highlighted keywords in the preeclampsia field. The highly related keywords are gathered into clusters, and the themes are named using the most highly related terms (Wang et al., 2019). The strategic map is divided into four sections (Cobo et al., 2011), as indicated by Callon et al. (1991) including the basic themes (bottom right), emerging themes (bottom left), motor themes (top right), and highly developed themes (right-left). Motor themes have strong relationships and are quite determined. Themes that are thoroughly developed and isolated have strong internal connections but weak external links. Themes that are developing or declining have a slight density and concentration, signifying weak interior and outer relations. Finally, basic and transversal themes, which are represented by topics with weak internal ties but large exterior links, have a high concentration and low density (Cobo et al., 2011). The first five keywords and the number of times they appeared were as follows:
Highly developed and isolated themes: Hypertensive Disorders (249), Angiogenic Factors (149), Uterine Artery Doppler (122), Tyrosine Kinase-1 (86), and Soluble Endoglin (86).
Motor themes: Expression (355), Normal-Pregnancy (168), Plasma (164), Oxidative Stress (146), and Pathogenesis (142).
Emerging or declining themes: Pregnancy-induced hypertension (152), Pre-eclampsia (101), Elevated liver enzymes (84), Hemolysis (49), and Therapy (33).
Basic and transversal themes: Pregnancy (1084), Women (798), Hypertension (590), Risk (516), and Eclampsia (168).
Discussion
In this study, by using bibliometric analysis, our research has explored and studied the trend of preeclampsia discipline between 1985 and 2020. The paper has valued the study and articles’ performance of authors, journals, organizations, and regions. To better recognize the configuration of the preeclampsia discipline, the authors advanced and studied co-citation, co-occurrence, strategic, and keywords maps. The chronological distribution displays three times in the publication movements in the preeclampsia discipline. The most cited document, ‘preeclampsia - an endothelial-cell disorder’ was published in the ‘AJOG’ (Roberts et al., 1989). The article’s from the ‘BJOJ’ was the second-most quoted piece of writing (Khong et al., 1986). Sacks article’s ‘AJOG’, which received the third-highest number of citations, was authored (Sacks et al., 1998). Sibai, Roberts, and Romero had the most preeclampsia-related documents among the authors. The United States, China, and England were the three most productive countries. The most effective institutions were ‘the University of Texas system’, ‘Harvard University’, and ‘PCSHE’. In terms of the number of articles, the overall number of citations, and productive organisations, the United States comes out on top. The ‘AJOG’, ‘Hypertension in Pregnancy’, and ‘Journal of Maternal-Fetal and Neonatal Medicine’ are the journals with the greatest impact.
We discovered that preeclampsia is a developing but still challenging field of medicine, particularly obstetrics and gynaecology. The results of documents released between 1985 and 2020 revealed three stages in this field’s research: a seeding stage from 1985 to 1997, a rapid growth stage from 1997 to 2005, and a post-2005 stage (development stage). An examination of the keywords revealed a close connection to preeclampsia themes. As a result, the findings regarding the primary structuring of the mentioned sources were made clear by the keywords. This stability suggests that an appropriate study on this topic was developed along the progress process. Investigating the keywords revealed a network of keywords with five clusters in the study. According to this finding, the management, diagnosis, biomarker’s involvement in preeclampsia, aspirin’s role in preeclampsia, and the relationship between preeclampsia and IUGR are the primary areas of investigation in the preeclampsia field. The strategic keyword map’s findings revealed that a number of the keywords represent fundamental themes. The majority of motor topics have focused on expression, healthy pregnancy, plasma, oxidative stress, and pathophysiology, as shown in Figure 6 pregnancy-induced hypertension, preeclampsia prostacyclin, endothelium, and thromboxane were also the keywords with the greatest spikes in citations, but more recently, the focus of preeclampsia articles has shifted to include aspirin, cardiovascular disease, and early-onset, and fetal growth restriction. In other words, these areas have received more focus to evaluate the fetal and maternal impact of preeclampsia. Even though in previous years, these areas have received virtually little attention.
FIGURE 6.
Strategic map in preeclampsia.
Six clusters were identified based on the results of co-citation, with clusters #3 and #4 being the most recent clusters and cluster #0 being the largest and oldest. Recently, the themes of chronic hypertension and conflicting risk models were studied. As a result, research on chronic hypertension and the competing risks model was focused on, along with studies on preeclampsia from lowered risks and the pathogenetic function. Researchers have been working on the chronic hypertension (Banala et al., 2020; Bramham et al., 2020; Hernández-Pacheco et al., 2020) as well as the competing risks model (Larroca et al., 2014; O’Gorman et al., 2016; Tsiakkas et al., 2016) in recent years.
Conclusions and implications
The main cause of maternal and neonatal morbidity and mortality is preeclampsia (Liu T et al., 2019). Preeclampsia is a complication in pregnancy mainly described by the occurrence of hypertension, and proteinuria after ≥20 weeks of gestation, edema in pregnancy and accompanied by signs of damage to other organ systems (Moghaddami Tabrizi et al., 2001; Roberts et al., 2013). It is associated with a higher risk of impending death, cardiovascular disease, cerebrovascular illness, and persistent hypertension (Leslie & Briggs, 2016). Acute renal failure, liver rupture, pulmonary edema, and cerebrovascular accidents are among the preeclampsia complications that can cause maternal death (Adu-Bonsaffoh et al., 2013). Preeclampsia is managed by preventing seizures, reducing maternal hypertension, and having the fetus delivered on schedule (Yeo et al., 2014). Although the pathogenesis of this significant obstetric condition is still unknown (Chaiworapongsa et al., 2014; Burton et al., 2019; Phipps et al., 2019). Every study in our research is significant and deserving of examination by obstetricians and gynecologists in active practice. According to a bibliometric examination of highly referenced works in the field, the AJOG is the best leading journal in the preeclampsia discipline. More than 60% of these articles were published in the AJOG. Despite these constraints, many of the most popular articles in other fields are supported by the top-cited papers, co-citations, and co-occurrence maps. All scholars in the field of healthcare can use the bibliometric method to examine the trend in the chosen field.
Contribution
This work makes a variety of contributions to theory and practice. The finding of this study was that the group of recently hot topics in this field that emerged from our research can serve as the foundation for future research. This study makes a significant contribution for researchers involved in preeclampsia because not only we shape, structure, and recognize the key universities, journals, documents and authors to be taken into consideration when conducting future research on preeclampsia but also to design a new trend in this field.
Strengths and limitations
This study has several restrictions. The WoS database is the only one that may be used for this research. Although it is the source with the most documentation, the information it contains is limited. This database does not index certain journals. As a result, other sources like PubMed, Google Scholar, and Scopus are available for use by other researchers. The second restriction is that an author could only have a minimum of 10 documents and a maximum of 10 keyword phrases. Third, this bibliometric analysis only considers publications in the fields of obstetrics and gynecology; other researchers may look into the fields of reproductive biology, physiology, general internal medicine, developmental biology, and biochemistry molecular biology. This study’s greatest asset was the thorough review of articles from the very beginning to the present.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranted or endorsed by the publisher.
References
- Adu-Bonsaffoh K., Oppong S. A., Binlinla G., Samuel O. A. (2013). Maternal deaths attributable to hypertensive disorders in a tertiary hospital in Ghana. Int. J. Gynecol. Obstetrics 123 (2), 110–113. 10.1016/j.ijgo.2013.05.017 [DOI] [PubMed] [Google Scholar]
- Akolekar R., Syngelaki A., Poon L., Wright D., Nicolaides K. H. (2013). Competing risks model in early screening for preeclampsia by biophysical and biochemical markers. Fetal Diagnosis Ther. 33 (1), 8–15. 10.1159/000341264 [DOI] [PubMed] [Google Scholar]
- Alarcon-Ruiz C. A., Diaz-Barrera M. E., Vera-Monge V. A., Alva-Diaz C., Metcalf T. (2019). A bibliometric analysis of the Latin American research on stroke 2003–2017. World Neurosurg. 129, e545–e554. 10.1016/j.wneu.2019.05.212 [DOI] [PubMed] [Google Scholar]
- Allaire A. D., Ballenger K. A., Wells S. R., McMahon M. J., Lessey B. A. (2000). Placental apoptosis in preeclampsia. Obstetrics Gynecol. 96 (2), 271–276. 10.1016/S0029-7844(00)00895-4 [DOI] [PubMed] [Google Scholar]
- AuthorAnonymous (2000). Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am. J. Obstetrics Gynecol. 183 (1), s1–s22. 10.1067/mob.2000.107928 [DOI] [PubMed] [Google Scholar]
- Banala C., Moreno S., Cruz Y., Boelig R. C., Saccone G., Berghella V., et al. (2020). Mothers with long QT syndrome are at increased risk for fetal death: Findings from a multicenter international study. Am. J. Obstetrics Gynecol. 223 (3), e1–e263. 10.1016/j.ajog.2019.09.004 [DOI] [PubMed] [Google Scholar]
- Bramham K., Villa P. M., Joslin J. R., Laivuori H., Hämäläinen E., Kajantie E., et al. (2020). Predisposition to superimposed preeclampsia in women with chronic hypertension: Endothelial, renal, cardiac, and placental factors in a prospective longitudinal cohort. Hypertens. Pregnancy 39 (3), 326–335. 10.1080/10641955.2020.1769643 [DOI] [PubMed] [Google Scholar]
- Broadus R. N. (1987). Toward a definition of “bibliometrics. Scientometrics 12 (5), 373–379. 10.1007/BF02016680 [DOI] [Google Scholar]
- Bujold E., Roberge S., Lacasse Y., Bureau M., Audibert F., Marcoux S., et al. (2010). Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy A meta-analysis. Obstetrics Gynecol. 116, 402–414. 10.1097/AOG.0b013e3181e9322a [DOI] [PubMed] [Google Scholar]
- Burton G. J., Redman C. W., Roberts J. M., Moffett A. (2019). Pre-eclampsia: Pathophysiology and clinical implications. Bmj 366, l2381. 10.1136/bmj.l2381 [DOI] [PubMed] [Google Scholar]
- Burton G. J., Yung H.-W., Cindrova-Davies T., Charnock-Jones D. S. (2009). Placental endoplasmic reticulum stress and oxidative stress in the pathophysiology of unexplained intrauterine growth restriction and early onset preeclampsia. Placenta 30, S43–S48. 10.1016/j.placenta.2008.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butt I., Iqbal T., Zohaib S. (2019). Healthcare marketing: A review of the literature based on citation analysis. Health Mark. Q. 0 (0), 271–290. 10.1080/07359683.2019.1680120 [DOI] [PubMed] [Google Scholar]
- Callon M., Courtial J. P., Laville F. (1991). Co-word analysis as a tool for describing the network of interactions between basic and technological research: The case of polymer chemsitry. Scientometrics 22 (1), 155–205. 10.1007/BF02019280 [DOI] [Google Scholar]
- Chaiworapongsa T., Chaemsaithong P., Yeo L., Romero R., Services H. (2014). Pre-eclampsia part 1: Current understanding of its pathophysiology. Nat. Rev. Nephrol. 10 (8), 466–480. 10.1038/nrneph.2014.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen C. (2004). Searching for intellectual turning points: Progressive knowledge domain visualization. Proc. Natl. Acad. Sci. U. S. A. 101 (1), 5303–5310. 10.1073/pnas.0307513100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobo M. J., López-Herrera A. G., Herrera-Viedma E., Herrera F. (2011). An approach for detecting, quantifying, and visualizing the evolution of a research field: A practical application to the fuzzy sets theory field. J. Inf. 5 (1), 146–166. 10.1016/j.joi.2010.10.002 [DOI] [Google Scholar]
- De Bellis N. (2009). Bibliometrics and citation analysis: From the science citation index to cybermetrics. Lanham, MD: scarecrow press. [Google Scholar]
- Dekker G. A., Devries J. I. P., Doelitzsch P. M., Huijgens P. C., Vonblomberg B. M. E., Jakobs C., et al. (1995). Underlying disorders associated with severe early-onset preeclampsia. Am. J. Obstetrics Gynecol. 173 (4), 1042–1048. 10.1016/0002-9378(95)91324-6 [DOI] [PubMed] [Google Scholar]
- Dekker G. A., Sibai B. M. (1998). Etiology and pathogenesis of preeclampsia: Current concepts. Am. J. Obstetrics Gynecol. 179 (5), 1359–1375. 10.1016/s0002-9378(98)70160-7 [DOI] [PubMed] [Google Scholar]
- Dias G. P. (2019). Fifteen years of e-government research in ibero-America: A bibliometric analysis. Gov. Inf. Q. 36 (3), 400–411. 10.1016/j.giq.2019.05.008 [DOI] [Google Scholar]
- Duley L. (2009). The global impact of pre-eclampsia and eclampsia. Seminars Perinatology 33 (3), 130–137. 10.1053/j.semperi.2009.02.010 [DOI] [PubMed] [Google Scholar]
- Friedman S. A., Taylor R. N., Roberts J. M. (1991). Pathophysiology of preeclampsia. Clin. Perinatology 18 (4), 661–682. 10.1016/S0095-5108(18)30490-1 [DOI] [PubMed] [Google Scholar]
- Gilstrap L. C., Ramin S. M. (2002). Diagnosis and management of preeclampsia and eclampsia. ACOG Pract. Bull. 33, 1–9. [Google Scholar]
- Gupta A., Kennedy B., Meriwether K. V., Francis S. L., Cardenas-Trowers O., Stewart J. R. (2019). Citation classics: The 100 most cited articles in urogynecology. Int. Urogynecology J. 31, 249–266. 10.1007/s00192-019-04021-9 [DOI] [PubMed] [Google Scholar]
- Hernández-Pacheco J. A., Rosales-Zamudio C. I., Borboa-Olivares H., Espejel-Núñez A., Parra-Hernández S., Estrada-Gutiérrez G., et al. (2020). The sFlt-1/PlGF ratio as a triage tool to identify superimposed preeclampsia in women with chronic hypertension in emergency rooms. Pregnancy Hypertens. 21, 38–42. 10.1016/j.preghy.2020.04.014 [DOI] [PubMed] [Google Scholar]
- Ishihara N., Matsuo H., Murakoshi H., Laoag-Fernandez J. B., Samoto T., Maruo T. (2002). Increased apoptosis in the syncytiotrophoblast in human term placentas complicated by either preeclampsia or intrauterine growth retardation. Am. J. Obstetrics Gynecol. 186 (1), 158–166. 10.1067/mob.2002.119176 [DOI] [PubMed] [Google Scholar]
- Jeung C.-W., Yoon H. J., Park S., Jo S. J. (2011). The contributions of human resource development research across disciplines: A citation and content analysis. Hum. Resour. Dev. Q. 22 (1), 87–109. 10.1002/hrdq.20062 [DOI] [Google Scholar]
- Karydakis P., Giakoumettis D., Themistocleous M. (2019). The 100 most cited papers about pediatric traumatic brain injury: A bibliometric analysis. Ir. J. Med. Sci. 189, 315–325. 10.1007/s11845-019-02085-6 [DOI] [PubMed] [Google Scholar]
- Kazemi Aski S., Akbari R., Hantoushzadeh S., Ghotbizadeh F. (2020). A bibliometric analysis of Intrauterine Growth Restriction research. Placenta 95, 106–120. 10.1016/j.placenta.2020.03.010 [DOI] [PubMed] [Google Scholar]
- Khong T. Y., De Wolf F., Robertson W. B., Brosens I. (1986). Inadequate maternal vascular response to placentation in pregnancies complicated by pre‐eclampsia and by small‐for‐gestational age infants. BJOG Int. J. Obstetrics Gynaecol. 93 (10), 1049–1059. 10.1111/j.1471-0528.1986.tb07830.x [DOI] [PubMed] [Google Scholar]
- Kupferminc M. J., Eldor A., Steinman N., Many A., Bar-Am A., Jaffa A., et al. (1999). Increased frequency of genetic thrombophilia in women with complications of pregnancy. N. Engl. J. Med. 340 (1), 9–13. 10.1056/NEJM199901073400102 [DOI] [PubMed] [Google Scholar]
- Kurki T., Hiilesmaa V., Raitasalo R., Mattila H., Ylikorkala O. (2000). Depression and anxiety in early pregnancy and risk for preeclampsia. Obstetrics Gynecol. 95 (4), 487–490. 10.1016/S0029-7844(99)00602-X [DOI] [PubMed] [Google Scholar]
- Larroca S. G.-T., Tayyar A., Poon L. C., Wright D., Nicolaides K. H. (2014). Competing risks model in screening for preeclampsia by biophysical and biochemical markers at 30-33 Weeks’ gestation. FETAL DIAGNOSIS Ther. 36 (1), 9–17. 10.1159/000362518 [DOI] [PubMed] [Google Scholar]
- Lee A., Ramstein J., Cohen A. J., Agochukwu-Mmonu N., Patino G., Breyer B. N. (2019). The top 100 cited articles in urethral reconstruction. Urology 135, 139–145. 10.1016/j.urology.2019.08.052 [DOI] [PubMed] [Google Scholar]
- Leslie M. S., Briggs L. A. (2016). Preeclampsia and the risk of future vascular disease and mortality: A review. J. Midwifery & Women’s Health 61 (3), 315–324. 10.1111/jmwh.12469 [DOI] [PubMed] [Google Scholar]
- Levine R. J., Lam C., Qian C., Yu K. F., Maynard S. E., Sachs B. P., et al. (2006). Soluble endoglin and other circulating antiangiogenic factors in preeclampsia. N. Engl. J. Med. 355 (10), 992–1005. 10.1056/NEJMoa055352 [DOI] [PubMed] [Google Scholar]
- Levine R. J., Maynard S. E., Qian C., Lim K.-H., England L. J., Yu K. F., et al. (2004). Circulating angiogenic factors and the risk of preeclampsia. N. Engl. J. Med. 350 (7), 672–683. 10.1056/NEJMoa031884 [DOI] [PubMed] [Google Scholar]
- Lisonkova S., Joseph K. S. (2013). Incidence of preeclampsia: Risk factors and outcomes associated with early-versus late-onset disease. Am. J. Obstetrics Gynecol. 209 (6), e1–e544. 10.1016/j.ajog.2013.08.019 [DOI] [PubMed] [Google Scholar]
- Liu T., Zhang M., Guallar E., Wang G., Hong X., Wang X., et al. (2019). Trace minerals, heavy metals, and preeclampsia: Findings from the boston birth cohort. J. Am. Heart Assoc. 8 (16), e012436. 10.1161/JAHA.119.012436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Zhang Y., Wu L., Yang X., Shi L. (2019). Characteristics and trends of oral leukoplakia research: A bibliometric study of the 100 most cited articles. Medicine 98 (27), e16293. 10.1097/MD.0000000000016293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Zhang J., Guo C. (2013). Full-text citation analysis: A new method to enhance scholarly networks. J. Am. Soc. Inf. Sci. Technol. 64, 1852–1863. 10.1002/asi.22883 [DOI] [Google Scholar]
- MacKay A. P., Berg C. J., Atrash H. K. (2001). Pregnancy-related mortality from preeclampsia and eclampsia. Obstetrics Gynecol. 97 (4), 533–538. 10.1016/S0029-7844(00)01223-0 [DOI] [PubMed] [Google Scholar]
- Maynard S. E., Min J.-Y., Merchan J., Lim K.-H., Li J., Mondal S., et al. (2003). Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J. Clin. Investigation 111 (5), 649–658. 10.1172/JCI17189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghaddami Tabrizi N., Eazadi Mood N., Tahmasbi M. (2001). Midtrimester serum B-subunit human chorionic gonadotropin levels and the subsequent development of preeclampsia. Tehran Univ. Med. J. 59 (4), 63–66. http://tumj.tums.ac.ir/article-1-1312-fa.html. [Google Scholar]
- Mol B. W. J., Roberts C. T., Thangaratinam S., Magee L. A., de Groot C. J. M., Hofmeyr G. J. (2016). Pre-eclampsia. Lancet 387 (10022), 999–1011. 10.1016/S0140-6736(15)00070-7 [DOI] [PubMed] [Google Scholar]
- Ness R. B., Roberts J. M. (1996). Heterogeneous causes constituting the single syndrome of preeclampsia: A hypothesis and its implications. Am. J. Obstetrics Gynecol. 175 (5), 1365–1370. 10.1016/S0002-9378(96)70056-X [DOI] [PubMed] [Google Scholar]
- Ødegård R. A., Vatten L. J., Nilsen S. T., Salvesen K. Å., Austgulen R. (2000). Preeclampsia and fetal growth. Obstetrics Gynecol. 96 (6), 950–955. 10.1016/S0029-7844(00)01040-1 [DOI] [PubMed] [Google Scholar]
- O’Gorman N., Wright D., Syngelaki A., Akolekar R., Wright A., Poon L. C., et al. (2016). Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 11-13 weeks gestation. Am. J. Obstetrics Gynecol. 214 (1), e1–e103. 10.1016/j.ajog.2015.08.034 [DOI] [PubMed] [Google Scholar]
- Phipps E. A., Thadhani R., Benzing T., Karumanchi S. A. (2019). Pre-eclampsia: Pathogenesis, novel diagnostics and therapies. Nat. Rev. Nephrol. 15 (5), 275–289. 10.1038/s41581-019-0119-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps E., Prasanna D., Brima W., Jim B. (2016). Preeclampsia: Updates in pathogenesis, definitions, and guidelines. Clin. J. Am. Soc. Nephrol. 11 (6), 1102–1113. 10.2215/CJN.12081115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pineles B. L., Romero R., Montenegro D., Tarca A. L., Han Y. M., Kim Y. M., et al. (2007). Distinct subsets of microRNAs are expressed differentially in the human placentas of patients with preeclampsia. Am. J. Obstetrics Gynecol. 196 (3), 261–e6. 10.1016/j.ajog.2007.01.008 [DOI] [PubMed] [Google Scholar]
- Pinto A., Sorrentino R., Sorrentino P., Guerritore T., Miranda L., Biondi A., et al. (1991). Endothelial-derived relaxing factor released by endothelial cells of human umbilical vessels and its impairment in pregnancy-induced hypertension. Am. J. Obstetrics Gynecol. 164 (2), 507–513. 10.1016/S0002-9378(11)80010-4 [DOI] [PubMed] [Google Scholar]
- Pritchard A. (1969). Statistical bibliography or bibliometrics. J. Documentation 25 (4), 348–349. [Google Scholar]
- Redman C. W. G., Sacks G. P., Sargent I. L. (1999). Preeclampsia: An excessive maternal inflammatory response to pregnancy. Am. J. Obstetrics Gynecol. 180 (2), 499–506. 10.1016/s0002-9378(99)70239-5 [DOI] [PubMed] [Google Scholar]
- Redman C. W., Sargent I. L. (2005). Latest advances in understanding preeclampsia. Science 308 (5728), 1592–1594. 10.1126/science.1111726 [DOI] [PubMed] [Google Scholar]
- Roberts J. M., Pa A., Bakris G., Barton J. R., Im B. (2013). Hypertension in pregnancy. Report of the American college of obstetricians and gynecologists’ task force on hypertension in pregnancy. Obstetrics Gynecol. 122 (5), 1122–1131. 10.1097/01.AOG.0000437382.03963.88 [DOI] [PubMed] [Google Scholar]
- Roberts J. M., Cooper D. W. (2001). Pathogenesis and genetics of pre-eclampsia. Lancet 357 (9249), 53–56. 10.1016/s0140-6736(00)03577-7 [DOI] [PubMed] [Google Scholar]
- Roberts J. M., Hubel C. A. (2009). The two stage model of preeclampsia: Variations on the theme. PLACENTA 30, S32–S37. 10.1016/j.placenta.2008.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts J. M., Redman C. W. G. (1993). Pre-eclampsia: More than pregnancy-induced hypertension. Lancet 341 (8858), 1447–1451. 10.1016/0140-6736(93)90889-O [DOI] [PubMed] [Google Scholar]
- Roberts J. M., Taylor R. N., Goldfien A. (1991). Clinical and biochemical evidence of endothelial cell dysfunction in the pregnancy syndrome preeclampsia. Am. J. Hypertens. 4 (8), 700–708. 10.1093/ajh/4.8.700 [DOI] [PubMed] [Google Scholar]
- Roberts J. M., Taylor R. N., Musci T. J., Rodgers G. M., Hubel C. A., McLaughlin M. K. (1989). Preeclampsia: An endothelial cell disorder. Am. J. Obstetrics Gynecol. 161 (5), 1200–1204. 10.1016/0002-9378(89)90665-0 [DOI] [PubMed] [Google Scholar]
- Rodgers G. M., Taylor R. N., Roberts J. M. (1988). Preeclampsia is associated with a serum factor CYTO-toxic to human-endothelial cells. Am. J. Obstetrics Gynecol. 159 (4), 908–914. 10.1016/S0002-9378(88)80169-8 [DOI] [PubMed] [Google Scholar]
- Rolnik D. L., Wright D., Poon L. C., O’Gorman N., Syngelaki A., de Paco Matallana C., et al. (2018). Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. Obstetrical Gynecol. Surv. 73 (1), 11–12. 10.1097/01.ogx.0000528015.09400.25 [DOI] [PubMed] [Google Scholar]
- Romero R., Nien J. K., Espinoza J., Todem D., Fu W., Chung H., et al. (2008). A longitudinal study of angiogenic (placental growth factor) and anti-angiogenic (soluble endoglin and soluble vascular endothelial growth factor receptor-1) factors in normal pregnancy and patients destined to develop preeclampsia and deliver a small for gestational age neonate. J. Maternal-Fetal Neonatal Med. 21 (1), 9–23. 10.1080/14767050701830480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks G. P., Studena K., Sargent I. L., Redman C. W. G. (1998). Normal pregnancy and preeclampsia both produce inflammatory changes in peripheral blood leukocytes akin to those of sepsis. Am. J. Obstetrics Gynecol. 179 (1), 80–86. 10.1016/s0002-9378(98)70254-6 [DOI] [PubMed] [Google Scholar]
- Saftlas A. F., Olson D. R., Franks A. L., Atrash H. K., Pokras R. (1990). Epidemiology of preeclampsia and eclampsia in the united-states, 1979-1986. Am. J. Obstetrics Gynecol. 163 (2), 460–465. 10.1016/0002-9378(90)91176-D [DOI] [PubMed] [Google Scholar]
- Schobel H. P., Fischer T., Heuszer K., Geiger H., Schmieder R. E. (1996). Preeclampsia - a state of sympathetic overactivity. N. Engl. J. Med. 335 (20), 1480–1485. 10.1056/NEJM199611143352002 [DOI] [PubMed] [Google Scholar]
- Seligman S. P., Buyon J. P., Clancy R. M., Young B. K., Abramson S. B. (1994). The role of nitric-oxide in the pathogenesis of preeclampsia. Am. J. Obstetrics Gynecol. 171 (4), 944–948. 10.1016/S0002-9378(94)70064-8 [DOI] [PubMed] [Google Scholar]
- Sibai B., Dekker G., Kupferminc M. (2005). Pre-eclampsia. Lancet 365 (9461), 785–799. 10.1016/S0140-6736(05)17987-2 [DOI] [PubMed] [Google Scholar]
- Sibai B. M., Elnazer A., Gonzalezruiz A., el-Nazer A., GonzAlez-Ruiz A. (1986a). Severe preeclampsia-eclampsia in young primigravid women - subsequent pregnancy outcome and remote prognosis. Am. J. Of Obstetrics And Gynecol. 155 (5), 1011–1016. 10.1016/0002-9378(86)90336-4 [DOI] [PubMed] [Google Scholar]
- Sibai B. M., Ewell M., Levine R. J., Klebanoff M. A., Esterlitz J., Catalano P. M., et al. (1997). Risk factors associated with preeclampsia in healthy nulliparous women. The Calcium for Preeclampsia Prevention (CPEP) Study Group. Am. J. Of Obstetrics And Gynecol. 177 (5), 1003–1010. 10.1016/S0002-9378(97)70004-8 [DOI] [PubMed] [Google Scholar]
- Sibai B. M., Gordon T., Thom E., Caritis S. N., Klebanoff M., Mcnellis D., et al. (1995). Risk factors for preeclampsia in healthy nulliparous women: A prospective multicenter study. The national institute of child health and human development network of maternal-fetal medicine units. Am. J. Of Obstetrics And Gynecol. 172 (21), 642–648. 10.1016/0002-9378(95)90586-3 [DOI] [PubMed] [Google Scholar]
- Sibai B. M., Mercer B. M., Schiff E., Friedman S. A. (1994). Aggressive versus expectant management of severe preeclampsia at 28 to 32 weeks gestation - a randomized controlled trial. Am. J. Of Obstetrics And Gynecol. 171 (3), 818–822. 10.1016/0002-9378(94)90104-X [DOI] [PubMed] [Google Scholar]
- Sibai B. M., Taslimi M. M., El-Nazer A., Amon E., Mabie B. C., Ryan G. M. (1986b). Maternal-perinatal outcome associated with the syndrome of hemolysis, elevated liver enzymes, and low platelets in severe preeclampsia-eclampsia. Am. J. Obstetrics Gynecol. 155 (3), 501–509. 10.1016/0002-9378(86)90266-8 [DOI] [PubMed] [Google Scholar]
- States U., Shah R., Kashkoush J., Kashkoush A., Patel T. (2019). Analysis of the top 100 most influential papers in benign prostatic hyperplasia. Can. Urological Assoc. J. = J. de l’Association Des Urologues Du Can. 14. 10.5489/cuaj.5831 [DOI] [PubMed] [Google Scholar]
- Steegers E. A. P., Von Dadelszen P., Duvekot J. J., Pijnenborg R. (2010). Pre-eclampsia. Lancet 376 (9741), 631–644. 10.1016/S0140-6736(10)60279-6 [DOI] [PubMed] [Google Scholar]
- Tran B. X., Latkin C. A., Vu G. T., Nguyen H. L. T., Nghiem S., Tan M.-X., et al. (2019). The current research landscape of the application of artificial intelligence in managing cerebrovascular and heart diseases: A bibliometric and content analysis. Int. J. Environ. Res. Public Health 16 (15), 2699. 10.3390/ijerph16152699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tranquilli A., Dekker G., Magee L., Roberts J., Sibai B. M., Steyn W., et al. (2014). The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens. 4 (2), 97–104. 10.1016/j.preghy.2014.02.001 [DOI] [PubMed] [Google Scholar]
- Tsiakkas A., Saiid Y., Wright A., Wright D., Nicolaides K. H. (2016). Competing risks model in screening for preeclampsia by maternal factors and biomarkers at 30-34 weeks’ gestation. Am. J. Obstetrics Gynecol. 215 (1), e1–e87. 10.1016/j.ajog.2016.02.016 [DOI] [PubMed] [Google Scholar]
- Van Eck N. J., Waltman L. (2009). Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 84 (2), 523–538. 10.1007/s11192-009-0146-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venkatesha S., Toporsian M., Lam C., Hanai J., Mammoto T., Kim Y. M., et al. (2006). Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat. Med. 12 (6), 642–649. 10.1038/nm1429 [DOI] [PubMed] [Google Scholar]
- Villar J., Carroli G., Wojdyla D., Abalos E., Giordano D., Ba’aqeel H., et al. (2006). Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am. J. Of Obstetrics And Gynecol. 194 (4), 921–931. 10.1016/j.ajog.2005.10.813 [DOI] [PubMed] [Google Scholar]
- Vince G. S., Starkey P. M., Austgulen R., Kwiatkowski D., Redman C. W. G. (1995). Interleukin-6, tumour necrosis factor and soluble tumour necrosis factor receptors in women with pre-eclampsia. Br. J. Of Obstetrics And Gynaecol. 102 (1), 20–25. 10.1111/j.1471-0528.1995.tb09020.x [DOI] [PubMed] [Google Scholar]
- von Dadelszen P., Magee L. A., Roberts J. M. (2003). Subclassification of preeclampsia. Hypertens. Pregnancy 22 (2), 143–148. 10.1081/PRG-120021060 [DOI] [PubMed] [Google Scholar]
- Walsh S. W. (1985). Preeclampsia: An imbalance in placental prostacyclin and thromboxane production. Am. J. Obstetrics Gynecol. 152 (3), 335–340. 10.1016/s0002-9378(85)80223-4 [DOI] [PubMed] [Google Scholar]
- Wang C., Lim M. K., Zhao L., Tseng M.-L., Chien C.-F., Lev B. (2019). The evolution of omega-the international journal of management science over the past 40 years: A bibliometric overview. Omega 93, 102098. 10.1016/j.omega.2019.08.005 [DOI] [Google Scholar]
- Wang P., Zhu F. W., Song H. Y., Hou J. H., Zhang J. L. (2018). Visualizing the academic discipline of knowledge management. Sustain. Switz. 10 (3), 682. 10.3390/su10030682 [DOI] [Google Scholar]
- Witlin A., Sibai B. (1998). Magnesium sulfate therapy in preeclampsia and eclampsia. Obstetrics Gynecol. 92 (5), 883–889. 10.1016/s0029-7844(98)00277-4 [DOI] [PubMed] [Google Scholar]
- Xu J., Zhang Y., Wu Y., Wang J., Dong X., Xu H. (2015). Citation sentiment analysis in clinical trial papers. AMIA Annu. Symp. Proc. 2015, 1334–1341. https://www.ncbi.nlm.nih.gov/pubmed/26958274. [PMC free article] [PubMed] [Google Scholar]
- Yadava S. M., Patrick H. S., Ananth C. V., Rosen T., Brandt J. S. (2019). Top-cited articles in the journal: A bibliometric analysis. Am. J. Obstetrics Gynecol. 220 (1), 12–25. 10.1016/j.ajog.2018.11.1091 [DOI] [PubMed] [Google Scholar]
- Yallampalli C., Garfield R. E. (1993). Inhibition of nitric-oxide synthesis in rats during pregnancy produces signs similar to those of preeclampsia. Am. J. Of Obstetrics And Gynecol. 169 (5), 1316–1320. 10.1016/0002-9378(93)90299-X [DOI] [PubMed] [Google Scholar]
- Yeo L., Romero R., Sci D. M., Romero R. (2014). Pre-eclampsia part 2: Prediction, prevention and management. Nat. Rev. Nephrol. 10 (9), 531–540. 10.1038/nrneph.2014.103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeisler H., Llurba E., Chantraine F., Vatish M., Staff A. C., Sennström M., et al. (2016). Predictive value of the sFlt-1: PlGF ratio in women with suspected preeclampsia. N. Engl. J. Med. 374, 13–22. 10.1056/NEJMoa1414838 [DOI] [PubMed] [Google Scholar]
- Zhu J., Song L. J., Zhu L., Johnson R. E. (2019). Visualizing the landscape and evolution of leadership research. Leadersh. Q. 30 (2), 215–232. 10.1016/j.leaqua.2018.06.003 [DOI] [Google Scholar]