Abstract
Background
The association between fine particular matter (PM2.5) and frailty is less studied, and the national burden of PM2.5-related frailty in China is unknown.
Objective
To explore the association between PM2.5 exposure and incident frailty in older adults, and estimate the corresponding disease burden.
Design
Chinese Longitudinal Healthy Longevity Survey from 1998 to 2014.
Setting
Twenty-three provinces in China.
Subjects
A total of 25,047 participants aged ≥65-year-old.
Methods
Cox proportional hazards models were performed to evaluate the association between PM2.5 and frailty in older adults. A method adapted from the Global Burden of Disease Study was used to calculate the PM2.5-related frailty disease burden.
Results
A total of 5,733 incidents of frailty were observed during 107,814.8 person-years follow-up. A 10 μg/m3 increment of PM2.5 was associated with a 5.0% increase in the risk of frailty (Hazard Ratio = 1.05, 95% confidence interval = [1.03–1.07]). Monotonic, but non-linear exposure-response, relationships of PM2.5 with risk of frailty were observed, and slopes were steeper at concentrations >50 μg/m³. Considering the interaction between population ageing and mitigation of PM2.5, the PM2.5-related frailty cases were almost unchanged in 2010, 2020 and 2030, with estimations of 664,097, 730,858 and 665,169, respectively.
Conclusions
This nation-wide prospective cohort study showed a positive association between long-term PM2.5 exposure and frailty incidence. The estimated disease burden indicated that implementing clean air actions may prevent frailty and substantially offset the burden of population ageing worldwide.
Keywords: fine particular matter (PM2.5), frailty, older adults, Chinese Longitudinal Healthy Longevity Survey (CLHLS), disease burden, older people
Key Points
This nation-wide prospective cohort study showed a positive association between long-term fine particular matter (PM2.5) exposure and frailty.
Monotonic, but non-linear exposure-response associations were observed, and slopes were steeper at concentrations ≥50 μg/m3.
Considering rapid population ageing and significant decrease in fine particular matter (PM2.5), the disease burden was almost unchanged in 2010–2030.
Introduction
Frailty is an emerging global disease burden that has a significant impact on clinical practice and public health [1]. With the rapid ageing population, the prevalence of frailty is expected to increase [2]. More studies are required to provide suggestions on modifiable factors and develop effective strategies that target the prevention and management of frailty in the ageing population [3].
Fine particular matter (PM2.5) is an environmental exposure leading to ageing-related health outcomes [4–7]. Three studies in China have concluded that PM2.5 may increase the incidence of frailty [8–10]. Due to the cross-sectional nature and the lack of individualized PM2.5 exposure, current evidence was insufficient to support the casual relationship between PM2.5 and frailty. Furthermore, no study has been conducted to estimate the national burden of PM2.5-related frailty in China.
We conducted a comprehensive investigation on the longitudinal association between PM2.5 and incident frailty among older adults using detailed personal PM2.5 at 1 km × 1 km, and estimated the national burden of PM2.5-related frailty at 2010, 2020 and 2030 in consideration of different scenarios of PM2.5 pollution and population ageing in China [11–13].
Methods
Study design and participants
The Chinese Longitudinal Healthy Longevity Survey (CLHLS) was conducted from 1998 to 2014 [14] with 3–5 years’ follow-up intervals. Recruited were 42,037 participants aged ≥65-year-old. We excluded participants who lost-to-follow-up in the first follow-up survey (n = 6,324), with < 50% indicators to calculate Frailty Index (FI) (n = 702), with prevalent frailty at baseline (n = 6,210), and with uncertain addresses (n = 3,754). Finally, 25,047 participants were included in the analysis (Supplementary Figure 1). The study was approved by the Biomedical Ethics Committee of Peking University (IRB00001052–13074).
Individualized ambient PM2.5 exposure
Estimates of ground-level concentrations of PM2.5 at 1 km × 1 km resolution were obtained from the Atmospheric Composition Analysis Group [15], which were highly consistent (R2 = 0.81) with out-of-sample cross-validated PM2.5 concentrations from monitors [16]. We calculated personal exposures of PM2.5 by linking residential locations to the nearest PM2.5 grids.
Frailty assessment
Frailty status were measured by FI including multiple dimensions of cumulative health deficits such as body functions and other physiological systems [17]. As previously reported [17], the FI which was calculated using 39 health-related deficits of various dimensions collected from baseline and follow-up surveys by self-report and physical measurements (Supplementary Table 1).
Covariates
We categorised the education level as illiterate and literate; categorised residence as rural or urban; categorised marital status as married or unmarried, divorced, or widowed; categorised income as pension or other; categorised occupation before 60-year-old as intellectual, labour or others; categorised living arrangement as living with family members, alone or in a nursing home; divided the current statuses of regular exercising, smoking, and alcohol drinking into yes or no.
Statistical analysis
The missing data (<2%) were imputed using multiple imputation methods (N imputation = 5) [18]. Cox proportional hazards models were performed to evaluate the association between PM2.5 exposure and incident frailty with controlling for potential covariates. We modelled PM2.5 as (i) a simple continuous variable [with hazard ratios (HRs) and 95% confidence intervals (CIs) estimated for each 10 μg/m3 increment]; (ii) ordinal variables by quartiles; (iii) categorical variables according to Chinese guidelines (<35, 35–75 and ≥ 75 μg/m3).
We used the HR estimates from the Cox proportional hazards models to calculate the PM2.5-related disease burden in China, using a method adapted from the Global Burden of Disease Study [19]. On the hypothesis that the frailty rate would remain stable if PM2.5 concentrations were reduced to 10 μg/m3. We calculated, for each county (i), the frailty (Fi) in the population aged ≥65-year-old that is attributable to ambient PM2.5 (Supplementary Formulae 1A and 1B, Supplementary Tables 2 and 3).
Results
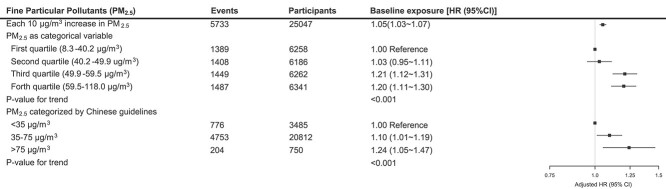
During 107,814.8 person-years follow-up, 5,733 incidents of frailty were observed. In the fully adjusted cox proportional hazards model, each 10 μg/m3 increase in PM2.5 was associated with a 5.0% increase in the risk of frailty (HR = 1.05, 95% CI = [1.03–1.07]). Compared with the lowest quartile of PM2.5, the HRs (95% CI) of the second, third and fourth quartiles were 1.03 (0.95–1.11), 1.21 (1.12–1.31) and 1.20 (1.11–1.30), respectively. Categorised by Chinese guidelines, adjusted HRs (95% CI) were 1.10 (1.01–1.19) and 1.24 (1.05–1.47) for participants with PM2.5 concentrations at 35–75 and ≥ 75 μg/m3, respectively, compared with those <35 μg/m3 (Figure 1). Monotonic, but non-linear exposure-response relationships of long-term PM2.5 exposure with risk of frailty were observed, and slopes were steeper at concentrations ≥50 μg/m3 (Supplementary Figures 4A and 5B). Results remained stable in sensitive analyses (Supplementary Figure S5).
Figure 1.
Long-term personal fine particular pollutants (PM2.5) exposure and incident frailty in Chinese older adults. Model adjusted for age, sex, education level, residence, marital, income, previous occupation and living status, current smoking, current drinking and regular exercising.
Considering the interaction between population ageing and mitigation of PM2.5, the cases of PM2.5-related frailty were 664,097, 730,858 and 665,169 for 2010, 2020 and 2030, respectively. With the population ageing and unimproved air quality, the PM2.5-related incident frailty cases were estimated to be 1,041,760 in 2020 and 1,341,428 in 2030. As the population ageing is usually irreversible, compared with the disease burden without considering improved air quality, the significant decreases of PM2.5-related frailty incidents (310,902 in 2020 and 676,259 in 2030) in the scenario with improved air quality were primarily benefited from the substantial mitigation of PM2.5 (Figure 2).
Figure 2.
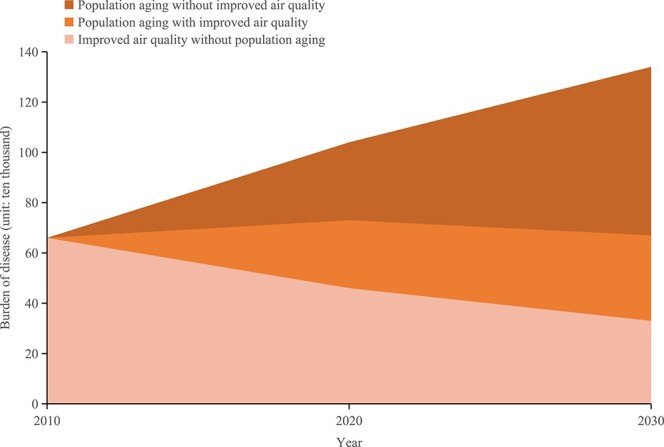
Estimated incident frailty related to PM2.5 exposure in adults aged ≥65-year-old in China in 2010, 2020 and 2030 with respect to the interaction between population ageing and air quality improvement
Discussion
Through this nation-wide prospective cohort study, we found a stable positive association between long-term PM2.5 exposure and frailty in Chinese older adults. As the population ageing is usually irreversible, the significant decreases of PM2.5-related frailty burden were primarily benefited from the mitigation of PM2.5.
This study shared several common findings with the previous two studies on the association between air quality and frailty. Compared to Hu et al.’s study [10] using city-level air pollution data without individualized PM2.5, our study established the association between PM2.5 and frailty with personal exposure at 1 km × 1 km, and further explored the non-linear dose–response relationship between them. Lee et al. reported the relationship between PM2.5 and frailty in Asians [9], but limited by the lack of national representative samples. Therefore, our findings provided new hints for larger-scale epidemiological studies to uncover the landscape of air pollution’s impact on healthy ageing.
We further estimated the PM2.5-related frailty disease burden in China. The ageing population increased more than 50% in 2020 compared with 2010, while the incident frailty cases attributable to PM2.5 in older adults increased by <3%. The plausible explanation may be that PM2.5 levels in China decreased (from 49.9 to 33.1 μg/m3) over the decade for the stringent air quality control policy since 2013. The interaction between population ageing and mitigation of PM2.5 in this study emphasised that the importance of taking actions to reduce air pollution.
Frailty is an emergent state of dysregulations in a compromised complex dynamical system that consists of the musculoskeletal system, metabolic system and stress-response system. Previous epidemiological and animal-based studies have shown that PM2.5 and other air pollutants could manifest such age-related biological vulnerability to stressors and harmed physiological reserves [20]. In mice studies, long-term exposure to PM2.5 impaired the function of brown adipose tissue and changed the gene expression from brown to white adipocyte specific patterns [21, 22], which are specialised for fatty acid metabolism, energy expenditure and heat generation. Also, long-term exposure to PM2.5 could cause inflammatory reaction [23, 24]. We thus speculate that the arguments of systemic inflammation, insulin resistance and oxidative stress resulting from PM2.5 would first cause mild disorders of the three systems to incubate frailty [25].
The major strengths of this study include the following: (i) it is the first long-term cohort study to investigate the causal association between PM2.5 and frailty; (ii) we first estimated the national-wide burden of PM2.5-related frailty among Chinese older adults under several different scenarios. The study also has limitations. Although we estimated individualized ambient PM2.5 exposures at 1 km × 1 km for all participants, the unmeasured exposures and time spend indoors might still limit us to generate the real-world exposures. Participants in our study were Chinese older adults, which limits the generalisation of the results to other ethnic groups.
Conclusion
In conclusion, we added evidence to the relationship between PM2.5 exposure and frailty incidence in a nation-wide prospective cohort study at community setting. We provided reliable risk estimations with the accurate individualized ambient PM2.5 exposures and inclusion of numerous covariates. Although faced with a rapid ageing in recent decades, China’s actions on air clean significantly decreased the concentration of PM2.5 and correspondingly contributed to the reduction of frailty related disease burdens. Considering population ageing and mitigation of PM2.5, the PM2.5-related frailty cases were almost unchanged in 2010, 2020 and 2030. Evidence suggested that the benefit of air quality improvement was likely to offset the frailty-related disease burden aggravated by population ageing.
Supplementary Material
Acknowledgments
We sincerely thank the provincial and county Centers for Disease Control and Prevention staff for carrying out the fieldwork and the participants of the CLHLS study.
Contributor Information
Yuebin Lv, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China.
Ze Yang, Beijing Institute of Geriatrics, Beijing Hospital, National Center of Gerontology, Beijing, China; Institute of Geriatric Medicine, Chinese Academy of Medical Sciences, Beijing, China.
Lihong Ye, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; School of Population Medicine and Public Health, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China.
Meijie Jiang, Department of Occupational and Environmental Health Sciences, School of Public Health, Peking University, Beijing, China.
Jinhui Zhou, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China.
Yanbo Guo, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; Department of Epidemiology and Biostatistics, School of Public Health, Jilin University, Changchun, Jilin, China.
Yidan Qiu, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; Department of Big Data in Health Science, School of Public Health, Zhejiang University, Hangzhou, Zhejiang, China.
Xinwei Li, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; Department of Epidemiology and Biostatistics, School of Public Health, Jilin University, Changchun, Jilin, China.
Chen Chen, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China.
Aipeng Ju, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; Department of Epidemiology and Biostatistics, School of Public Health, Jilin University, Changchun, Jilin, China.
Jun Wang, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China.
Chenfeng Li, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; Department of Occupational Health and Environment Health, School of Public Health, Anhui Medical University, Hefei, Anhui, China.
Yang Li, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China.
Jiaonan Wang, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; Center for Global Health, School of Public Health, Nanjing Medical University, Nanjing, Jiangsu, China.
Juan Zhang, School of Population Medicine and Public Health, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, China.
John S Ji, Vanke School of Public Health, Tsinghua University, Beijing, China.
Tiantian Li, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China.
Andrea A Baccarelli, Laboratory of Environmental Precision Health, Mailman School of Public Health, Columbia University, New York, NY, USA.
Xu Gao, Department of Occupational and Environmental Health Sciences, School of Public Health, Peking University, Beijing, China.
Xiaoming Shi, China CDC Key Laboratory of Environment and Population Health, National Institute of Environmental Health, Chinese Center for Disease Control and Prevention, Beijing, China; Center for Global Health, School of Public Health, Nanjing Medical University, Nanjing, Jiangsu, China.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
The work was supported by National Natural Sciences Foundation of China (grant numbers 82025030, 81941023 and 82222063) and China CDC Key Laboratory of Environment and Population Health (grant number 2022-CKL-03).
Data Availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
- 1. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet 2019; 394: 1365–75. [DOI] [PubMed] [Google Scholar]
- 2. Mousa A, Savva GM, Mitnitski A et al. Is frailty a stable predictor of mortality across time? Evidence from the cognitive function and ageing studies. Age Ageing 2018; 47: 721–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet 2019; 394: 1376–86. [DOI] [PubMed] [Google Scholar]
- 4. Newman JD, Bhatt DL, Rajagopalan S et al. Cardiopulmonary impact of particulate air pollution in high-risk populations: JACC state-of-the-art review. J Am Coll Cardiol 2020; 76: 2878–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim HB, Shim JY, Park B, Lee YJ. Long-term exposure to air pollutants and cancer mortality: a meta-analysis of cohort studies. Int J Environ Res Public Health 2018; 15: 2608. 10.3390/ijerph15112608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cristaldi A, Fiore M, Oliveri Conti G et al. Possible association between PM(2.5) and neurodegenerative diseases: a systematic review. Environ Res 2022; 208: 112581. 10.1016/j.envres.2021.112581. [DOI] [PubMed] [Google Scholar]
- 7. Crouse DL, Peters PA, Hystad P et al. Ambient PM2.5, O₃, and NO₂ exposures and associations with mortality over 16 years of follow-up in the Canadian Census Health and Environment Cohort (CanCHEC). Environ Health Perspect 2015; 123: 1180–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Myers V, Broday DM, Steinberg DM, Yuval DY, Gerber Y. Exposure to particulate air pollution and long-term incidence of frailty after myocardial infarction. Ann Epidemiol 2013; 23: 395–400. [DOI] [PubMed] [Google Scholar]
- 9. Lee WJ, Liu CY, Peng LN, Lin CH, Lin HP, Chen LK. PM(2.5) air pollution contributes to the burden of frailty. Sci Rep 2020; 10: 14478. 10.1038/s41598-020-71408-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hu K, Keenan K, Hale JM, Börger T. The association between city-level air pollution and frailty among the elderly population in China. Health Place 2020; 64: 102362. [DOI] [PubMed] [Google Scholar]
- 11. Huang J, Pan X, Guo X, Li G. Health impact of China's air pollution prevention and control action plan: an analysis of national air quality monitoring and mortality data. Lancet Planet Health 2018; 2: e313–23. [DOI] [PubMed] [Google Scholar]
- 12. Zheng Y, Xue T, Zhang Q, Geng G, He K, Air quality and health benefits of China's recent stringent environmental policy. American Geophysical Union, Agu Fall Meeting; 2016.
- 13.World Health Organization. WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide: executive summary. Geneva: World Health Organization, 2021; Licence: CC BY-NC-SA 3.0 IGO. [PubMed]
- 14. van Donkelaar A, Martin RV, Brauer M, Boys BL. Use of satellite observations for long-term exposure assessment of global concentrations of fine particulate matter. Environ Health Perspect 2015; 123: 135–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fried LP, Cohen AA, Xue QL, Walston J, Bandeen-Roche K, Varadhan R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging 2021; 1: 36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lv YB, Gao X, Yin ZX et al. Revisiting the association of blood pressure with mortality in oldest old people in China: community based, longitudinal prospective study. BMJ 2018; 5: k2158. 10.1136/bmj.k2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gu D, Dupre ME, Sautter J, Zhu H, Liu Y, Yi Z. Frailty and mortality among Chinese at advanced ages. J Gerontol B Psychol Sci Soc Sci 2009; 64: 279–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zeng Y, Feng Q, Hesketh T, Christensen K, Vaupel JW. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet 2017; 389: 1619–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the global burden of disease study 2019: a systematic analysis for the global burden of disease study 2019. Lancet 2021; 396: 2006–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lin H, Guo Y, Ruan Z et al. Association of Indoor and outdoor air pollution with hand-grip strength among adults in six low- and middle-income countries. J Gerontol A Biol Sci Med Sci 2020; 75: 340–7. [DOI] [PubMed] [Google Scholar]
- 21. Xu Z, Xu X, Zhong M et al. Ambient particulate air pollution induces oxidative stress and alterations of mitochondria and gene expression in brown and white adipose tissues. Part Fibre Toxicol 2011; 11: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Xu X, Liu C, Xu Z et al. Long-term exposure to ambient fine particulate pollution induces insulin resistance and mitochondrial alteration in adipose tissue. Toxicol Sci 2011; 124: 88–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pan B, Chen M, Zhang X et al. Hypothalamic-pituitary-adrenal axis mediates ambient PM(2.5) exposure-induced pulmonary inflammation. Ecotoxicol Environ Saf 2021; 15: 111464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu C, Yang J, Guan L, Zhu Y, Geng X. Filtered air intervention reduces inflammation and hypothalamus-pituitary-adrenal axis activation in adult male and female rats after PM 2.5 exposure. Environ Sci Pollut Res Int 2020; 27: 35341–8. [DOI] [PubMed] [Google Scholar]
- 25. Peters A, Nawrot TS, Baccarelli AA. Hallmarks of environmental insults. Cell 2021; 184: 1455–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.