Abstract
Background:
Evidence on the relationship between exposure to greenness and adolescent mental health is limited. The purpose of this study was to examine the association between greenness throughout childhood and mental health at age 12 years.
Methods:
We assessed greenness using the satellite-based measure of Normalized Difference Vegetation Index (NDVI) within 200m, 400m, and 800m of home address at birth, age 12 years, and across childhood (averaged for each year from birth to age 12) among the Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS) cohort. Self-reported symptoms of anxiety and depression were assessed at age 12 years using the Spence Children’s Anxiety Scale (SCAS) and Children’s Depression Inventory 2 (CDI 2), respectively. Associations were estimated using linear regression, adjusting for covariates including traffic-related air pollution, neurological hazard exposure, blood lead level, household income, and community deprivation.
Results:
In adjusted models, NDVI was largely not associated with self-reported anxiety and depression symptoms, except for the SCAS separation anxiety subscale at 400m and 800m (0.1 unit increase mean NDVI 400m: β = −0.97, 95% CI: −1.86, −0.07; 800m: β = −1.33, 95% CI: −2.32, −0.34).
Conclusion:
While we found no direct relationship between greenness and overall symptoms of anxiety and depression in adolescents upon adjustment for relevant covariates at the 200m distance, greenness may lesson symptoms of separation anxiety within 400m and 800m distance from the home address at age 12 years. Future research should examine mechanisms for these relationships at the community- and individual-level.
Keywords: Pediatric, Nature, Environment, Green space, Mental health
1. Introduction
Mental health disorders, including anxiety and depression, affect as many as 1 in 5 Americans (National Institute of Mental Health [NIMH], 2019). Individuals living with mental health disorders face an increased risk for chronic medical conditions (Colton and Manderscheid, 2006) and may die on average 25 years earlier than those without mental health disorders (National Association of State Mental Health Program Directors Council, 2006).
Many mental health disorders begin during adolescence (Patel et al., 2007; World Health Organization [WHO], 2019), with as many as half of all chronic mental health disorders beginning by age 14 years (Kessler et al., 2005). However, due to inadequate recognition and treatment, these disorders often are not diagnosed until later in life. One in every 4–5 youth in the U.S. will meet criteria for a mental health disorder during their lifetime (Merikangas et al., 2010). Anxiety and depressive disorders are among the most common, with the anxiety prevalence over 30% (Merikangas et al., 2010) and depression affecting approximately 13% of adolescents (Federal Interagency Forum on Child and Family Statistics, 2017).
Adolescence, defined by the American Academy of Pediatrics as ages 11 through 21 years (Hagan et al., 2008) and by the World Health Organization as ages 10 through 19 years, presents unique challenges and opportunities for mental health (WHO, 2019). This time of life is characterized by the biological changes of puberty and crucial milestones related to intellectual, social, and emotional development (American Academy of Pediatrics, 2012). Mental health disorders can profoundly affect the way adolescents think, feel, learn, and relate to others, potentially disrupting daily functions such as schoolwork, sleeping, and eating (NIMH, 2018). Such disruption further complicates reaching expected developmental milestones, resulting in lower educational achievements, higher levels of substance abuse, experiences of violence, and poor reproductive and sexual health (Patel et al., 2007). Developing interventions for prevention of mental health disorders in adolescence could have beneficial impacts into adulthood and across the lifespan, as the health and behavioral patterns established during this age determine both current and future health status (Nishida et al., 2016; WHO, 2019).
Greenness, generally defined as vegetation such as trees and grasses, has shown promise for positively contributing to mental and physical health (Browning and Lee, 2017; Fong et al., 2018; Hartig et al., 2014). While a larger body of evidence supports greenness positively influencing mental health in adults, there is limited evidence regarding the association between greenness and mental health during adolescence (Gascon et al., 2015). A landmark study of 345,000 Dutch participants of various ages found those living in the greenest environments were diagnosed with fewer mental and physical health disorders, with strongest associations between greenness and decreased mental health disorders in youth (Maas et al., 2009a). While an early systematic review of literature exploring the relationship between greenness and mental health found inadequate evidence to support an association among children and adolescents (Gascon et al., 2015), a subsequent review of 11 quantitative and one qualitative study found access to green space associated with overall health, wellbeing, and cognitive development among children aged 0–18 years (McCormick, 2017). Most recently, exposure to greenness was found to be beneficial for adolescent depression but with limited evidence (Vanaken and Danckaerts, 2018), finding two studies indicating decreased depressive symptoms in adolescents exposed to greenness in cross-sectional (Bezold et al., 2018a) and longitudinal analyses (Bezold et al., 2018b). Additionally, Mavoa et al. (2019) found decreased depressive symptoms significantly associated with increased greenness for adolescents in New Zealand, while Madzia et al. (2019) found exposure to greenness was associated with reduced parent-reported anxiety scores and depression scores in adolescents in the United States.
The purpose of this study was to examine the association between greenness and self-reported symptoms of anxiety and depression among adolescent participants of a longitudinally followed pediatric cohort.
2. Materials and methods
2.1. Study population
The Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS) is a longitudinal cohort of children recruited during infancy in Cincinnati, Ohio, USA. Eligibility for study enrollment required a birth record address either far (>1500m) or near (<400m) a major highway or interstate (Ryan et al., 2005). Enrolled infants also must have had at least one atopic parent defined as having a positive skin prick test to at least one aeroallergen (Ryan et al., 2005). The study was conducted with approval of the University of Cincinnati and Cincinnati Children’s Hospital Institutional Review Boards with written informed consent of parents and assent of participants.
The CCAAPS cohort included 762 infants born between October 2001 and July 2003 in seven counties within southwest Ohio (Butler, Clermont, Hamilton, and Warren counties) and northern Kentucky (Boone, Campbell, and Kenton counties) (Gernes et al., 2019). Participants were evaluated at ages 1, 2, 3, 4, 7, and 12 years on various health and demographic characteristics including addresses. For years without a study visit, addresses were collected retrospectively at the age 7 and 12 year visits (Brunst et al., 2015). All addresses were geocoded using EZLocate software from TeleAtlas for the ArcView Geographic Information System 3.2 (Environmental Systems Research Institute, Redlands, CA) (Ryan et al., 2005).
2.2. Exposure and health assessments
2.2.1. Greenness
Normalized Difference Vegetation Index (NDVI) is extracted using satellite imagery to measure visible and near-infrared light reflection from chlorophyll (GIS Geography, 2020). NDVI provides a continuous variable for greenness, with values ranging from −1 to +1. Negative values are associated with water, near-zero values are associated with barrenness such as deserts, and positive values range from grassland to rainforests (GIS Geography, 2020). In this analysis, we extracted NDVI values using Landsat 7, Enhanced Thematic Mapper Plus (ETM+) imagery at 30 m × 30 m resolution from cloud-free days in June of 2000 and 2010. Because water bodies have NDVI values less than 0, we excluded negative values from assessment.
To estimate the amount of greenness surrounding the child at close range, at the street level, and at the community level, three nested buffer radii were used: 200 m, 400 m, and 800 m. For each annual study visit, the closest of the two NDVI scenes (2000 or 2010) to the time of data collection were used to calculate the average NDVI value within a fixed radius distance (200m, 400m, and 800m) from each participant’s geocoded home address. This was calculated for three time periods: birth, address at the age 12 study visit, and averaged across childhood, calculated from the mean of NDVI values ascertained for all home addresses from birth to age 12 years.
2.2.2. Mental health
Instruments measuring self-reported symptoms of anxiety and depression were administered via trained examiner. Participants were given instructions prior to completing instruments, and the examiner was available to assist if needed. Instruments were scored according to publisher guidelines. Resources and assistance with referrals were offered to both participant and caregiver for elevated scores (Yolton et al., 2019).
2.2.2.1. Anxiety.
Self-reported symptoms of anxiety were ascertained using the Spence Children’s Anxiety Scale (SCAS; Spence, 1998). The SCAS contains 44 items measuring self-reported symptoms of anxiety, each scoring between 0 (never) and 3 (always) points. Six domains of anxiety are assessed: Panic and Agoraphobia, Separation Anxiety, Social Phobia, Obsessive Compulsive Disorder, Physical Injury Fears, and Generalized Anxiety Disorder. Points are summed to produce a score for each of the six subscales, and a Total Anxiety score is calculated ranging from 0 to 132. Scoring is converted to T-scores standardized for age and gender, with a mean of 50 and standard deviation of 10. The SCAS has high internal consistency reliability (α = 0.87–0.94; Ramme, n.d.).
2.2.2.2. Depression.
Self-reported symptoms of depression were collected using the Children’s Depression Inventory 2 (CDI 2; Kovacs, 2011) Short-Form. The CDI 2 contains 12 items assessing self-reported, affective and behavioral signs of depression in children and adolescents. Each item contains three statements, from which the child selects one answer that best describes his or her feelings over the past two weeks, each scoring 0 (absence of symptoms), 1 (mild symptoms), or 2 (definite symptoms). The CDI 2 yields a total depression score, converted to a T-score standardized for age and gender, with a mean of 50 and standard deviation of 10. Psychometric testing of the tool found reliability coefficients ranging from 0.82 (test) to 0.84 (retest) in the community sample, and 0.85 (test) to 0.81 (retest) in the clinical sample (Figueras et al., 2010).
2.2.3. Covariates
Possible confounding pathways were identified and visualized through a directed acyclic graph (DAG). DAGs are tools for making a priori causal inferences based on theorized relationships (Suttorp et al., 2015). Our DAG for adolescent mental health and greenness is provided in Fig. 1, created with dagitty.net software (Textor et al., 2016). Based on our hypothesized DAG, statistical models were adjusted for household income, traffic-related air pollution, neurological hazard exposure, blood lead, and community deprivation.
Fig. 1.
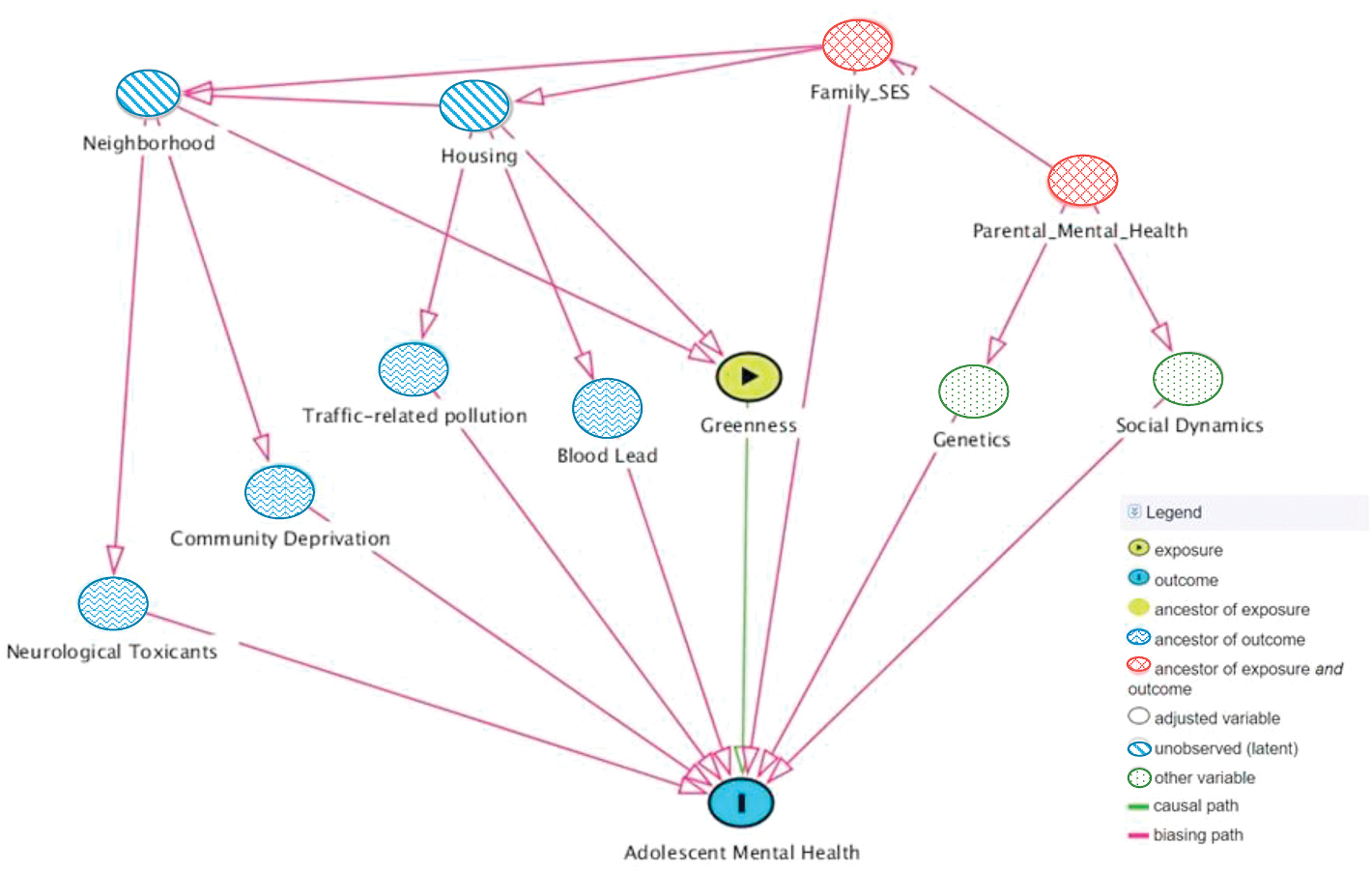
Directed acyclic graph (DAG) of adolescent mental health and greenness. Model covariates identified were household income, traffic-related air pollution, neurological toxics, community deprivation, and lead. Created with daggity.net software (Textor et al., 2016).
2.2.3.1. Household income.
Household income was reported by parents at the age 1 and 12 year study visits. Income was queried in nine categories and considered as ordered factors (Table 1). Income at age 1 year was used in “birth” models, income at age 12 years was used in “Age 12” models, and the two values were averaged for “across childhood” models.
Table 1.
Characteristics, Health Outcomes, and Covariates by Age.
| Characteristics, Health Outcomes, and Exposures | ||
|
| ||
| n (%) | ||
|
| ||
| Sex | Male | 191 (56) |
|
|
||
| Female | 153 (44) | |
|
|
||
| Race | White | 268 (78) |
| Non-White | 76 (22) | |
| Household Income at Age 12 | Under $10K | 21 (6.1) |
| $10K to under $20K | 18 (5.2) | |
| $20K to under $30K | 23 (6.7) | |
| $30K to under $40K | 18 (5.2) | |
| $40K to under $50K | 14 (4.1) | |
| $50K to under $70K | 49 (14.2) | |
| $70K to under $90K | 43 (12.5) | |
| $90 to under $110K | 36 (10.5) | |
| Over $110K | 105 (30.5) | |
| Did not respond | 17 (4.9) | |
| M (SD) | ||
| Anxiety | Physical Injury Fears | 49.53 (8.19) |
| Social Phobia | 46.74 (7.98) | |
| Generalized Anxiety Disorder | 46.38 (6.63) | |
| Panic and Agoraphobia | 46.86 (7.38) | |
| Obsessive Compulsive Disorder | 45.98 (7.45) | |
| Separation Anxiety | 45.45 (6.51) | |
| Total Score | 44.18 (8.17) | |
| Depression | Total Score | 52.7 (10.7) |
| Blood Lead Level (μg/dL) | Age 12 | 0.567 (0.37) |
| ECAT (μg/m3) | 6 Months of Age | 0.401 (0.15) |
| Age 12 | 0.376 (0.12) | |
| Across childhood | 0.377 (0.10) | |
| Community Deprivation Index | Birth | 0.459 (0.16) |
| Age 12 | 0.333 (0.14) | |
| Across childhood | 0.386 (0.14) | |
| National Neurological Hazard Index | 6 Months of Age | 0.056 (0.01) |
| Age 12 | 0.053 (0.01) | |
| Across childhood | 0.054 (0.01) | |
dL = deciliter; M = mean; m3 = meter cubed; SD=Standard Deviation; μg = microgram.
2.2.3.2. Traffic-related air pollution.
A marker of air pollution, elemental carbon attributable to traffic (ECAT) was estimated as a continuous variable using a previously established land use regression model based on ambient air sampling from 24 sites within the study area (Ryan et al., 2007). ECAT was estimated at the birth record address in “birth” models, at the age 12 home address for “Age 12” models, and estimates using home address for each year of life were averaged for “across childhood” models.
2.2.3.3. Community deprivation.
Community deprivation was quantified as an index of six census tract-level variables related to material deprivation (fraction over age 25 with at least high school diploma or general educational development equivalent, fraction of households in poverty, median household income, fraction of population with no health insurance coverage, fraction of population receiving public assisted income or supplemental nutritional assistance, fraction of houses that are vacant), using the 2015 5-year American Community Survey (Brokamp et al., 2016). Values were calculated for three time periods (birth, age 12 years, and averaged across childhood) from the mean of index values from each year between birth and age 12 years. Community deprivation index yields a continuous value between zero and one, with higher values indicating more deprivation.
2.2.3.4. Neurological hazard.
Neurological hazards present at the census-tract level were estimated using data from the United States Environmental Protection Agency’s (EPA) 2014 National Air Toxics Assessment (EPA, 2018). The National Neurological Hazard Index (NNHI) is a census-tract level total score based on the sum of hazard quotients for 24 toxics affecting the neurological system. A continuous index value was assigned based on the census tract corresponding to participant addresses at birth and at age 12 years. Resultant values were used for modeling exposures at birth and age 12 years, then averaged for modeling exposures across childhood. An index <1 indicates air toxics are unlikely to adversely affect neurological health (EPA, 2018).
2.2.3.5. Blood lead.
A known neurotoxicant adversely associated with mental health outcomes (Bouchard et al., 2009; Liu et al., 2014), blood samples collected from participants at the age 12 visit were analyzed for lead concentrations obtained by inductively coupled plasma mass spectrometry at the Laboratory for Inorganic and Nuclear Chemistry at the New York State Department of Health’s Wadsworth Center (Dantzer et al., 2020). Blood lead levels were expressed as a continuous variable.
2.3. Statistical analysis
Analyses were performed using R (R Core Team, 2019). Relationships between NDVI in three buffer distances (200m, 400m, 800m) at birth, age 12 years, and averaged across childhood (annually between birth and age 12 years) and self-reported symptoms of anxiety and depression were examined. Linear regression modeling was used to estimate the association between NDVI and CDI 2 total score and SCAS total and subscale scores while adjusting for household income, ECAT, neurological hazard index, community deprivation index, and blood lead level. Reported model parameter estimates represent effect per 0.1 unit change in NDVI.
3. Results
3.1. Study population characteristics
Of the 762 children enrolled in CCAAPS, 344 (45%) completed the age 12 study visits. Five participants did not complete the mental health instruments as the study visit was completed by mail; our policy for mailed visits was to omit these instruments since support could not be offered if depression or anxiety scores were elevated (Yolton et al., 2019). Thus, 339 participants were included in this analysis. Of these, 56% (n = 191) of participants were male (Table 1). The percentage of minority participants (n = 83, 24%) was slightly higher than in the sample region population (20%; Ohio-Kentucky-Indiana Regional Council of Governments, 2016). There were no statistically significant differences in demographic characteristics between participants who completed the age 12 study visit and those who did not (Yolton et al., 2019). No participants met the threshold for elevated NNHI (≥1; EPA, 2018) or blood lead levels (≥5 μg/dL; Centers for Disease Control and Prevention, 2019).
3.2. Mental health outcomes
The prevalence of elevated SCAS scores (T ≥ 65) among the cohort was less than 3% for Total Anxiety (M = 44.2, SD = 8.2; Table 2). The prevalence of elevated Total Depression score (T ≥ 65) was 9.7% (M = 52.7, SD = 10.2; Table 2).
Table 2.
Spence Children’s Anxiety Score results for total anxiety and anxiety sub-scales; Children’s Depression Inventory 2 results for total depression score.
| SCAS | |||
|
| |||
| M (SD) | n (%) T-score >65 | ||
|
| |||
| panic and agoraphobia | 46.9 (7.4) | 7 (2.1) | |
| separation anxiety | 45.4 (6.5) | 4 (1.2) | |
| social phobia | 46.7 (8.0) | 5 (1.5) | |
| obsessive compulsive disorder | 46.0 (7.5) | 9 (2.6) | |
| physical injury fears | 49.5 (8.2) | 9 (2.6) | |
| generalized anxiety disorder | 46.4 (6.6) | 1 (0.3) | |
| total anxiety score | 44.2 (8.2) | 3 (0.9) | |
|
| |||
| CDI 2 | |||
|
| |||
| Category | T-Score | n (%) | |
|
| |||
| CDI 2 Category | Low | <40 | 32 (9.3) |
| Average | 40–59 | 222 (64.5) | |
| High Average | 60–64 | 52 (15.1) | |
| Elevated | 65–69 | 14 (4.1) | |
| Very Elevated | ≥70 | 19 (5.6) | |
| N/A | N/A | 5 (1.4) | |
CDI 2, Child Depression Inventory 2; M, mean; SCAS, Spence Children’s Anxiety Score; SD, standard deviation.
CDI 2 categories based on Kovacs (2011); 339 participants completed instruments.
3.3. Greenness exposure
Mean NDVI increased across all buffer radii from the home address between birth and age 12 (Table 3), indicating participants’ surrounding greenness increased as they aged, either through increased greenness around the home or by changing residence to an area with more greenness. Averaging NDVI estimates at all recorded participant addresses provided a measure of lifetime exposure to greenness, referred to as “across childhood”. NDVI range (0.095–0.775) for all buffer radii and all ages is reported in Table 3.
Table 3.
Exposure to greenness by buffer distance.
| NDVI BUFFER | AGE | Mean (Standard Deviation) | Range |
|---|---|---|---|
|
| |||
| 200m | Birth | 0.505 (0.11) | 0.111–0.772 |
| Age 12 | 0.565 (0.10) | 0.111–0.722 | |
| Across Childhood | 0.535 (0.08) | 0.230–0.710 | |
| 400m | Birth | 0.526 (0.10) | 0.167–0.775 |
| Age 12 | 0.573 (0.10) | 0.095–0.765 | |
| Across Childhood | 0.559 (0.08) | 0.272–0.734 | |
| 800m | Birth | 0.533 (0.10) | 0.161–0.742 |
| Age 12 | 0.597 (0.10) | 0.131–0.754 | |
| Across Childhood | 0.564 (0.08) | 0.230–0.743 | |
3.4. Greenness and anxiety
Significant negative correlations (r = −0.12 to −0.16, p < 0.05) were observed between greenness and Total Anxiety score and the Generalized Anxiety subscale in 400m and 800m buffer radii at all time points (birth, age 12 years, and average across childhood; Supplementary Table 1). No significant correlation was noted between NDVI at any age or buffer radius and subscales for Panic and Agoraphobia, Physical Injury Fears, or Social Phobia. In the Obsessive-Compulsive Disorder subscale, statistically significant correlation with NDVI was noted in the 200m radius averaged across childhood (r = −0.13, p = 0.016), at 400 m at age 12 and averaged across childhood (age 12: r = −0.14, p = 0.008; average: r = −0.16, p = 0.003), and at 800 m at all three time points (birth: r = −0.17, p = 0.002; age 12: r = −0.16, p = 0.003; average: r = −0.17, p = 0.002). In the Separation Anxiety Disorder subscale, statistically significant correlation with NDVI was noted at age 12 and averaged across childhood in the 400m and 800m radii (400m age 12: r = −0.14, p = 0.012; 400m average: r = −0.11, p = 0.044, 800m age 12: r = −0.17, p = 0.002; 800m average: r = −0.11, p = 0.040).
In models controlling for community deprivation, ECAT, blood lead, NNHI, and household income, NDVI remained statistically significant only for Separation Anxiety (Fig. 2, Supplementary Table 1), with a significant inverse association between NDVI at age 12 and Separation Anxiety for the 400m and 800m radii (400m: β = −0.97, 95% CI: −1.86, −0.07; 800m: β = −1.33, 95% CI: −2.32, −0.34).
Fig. 2.
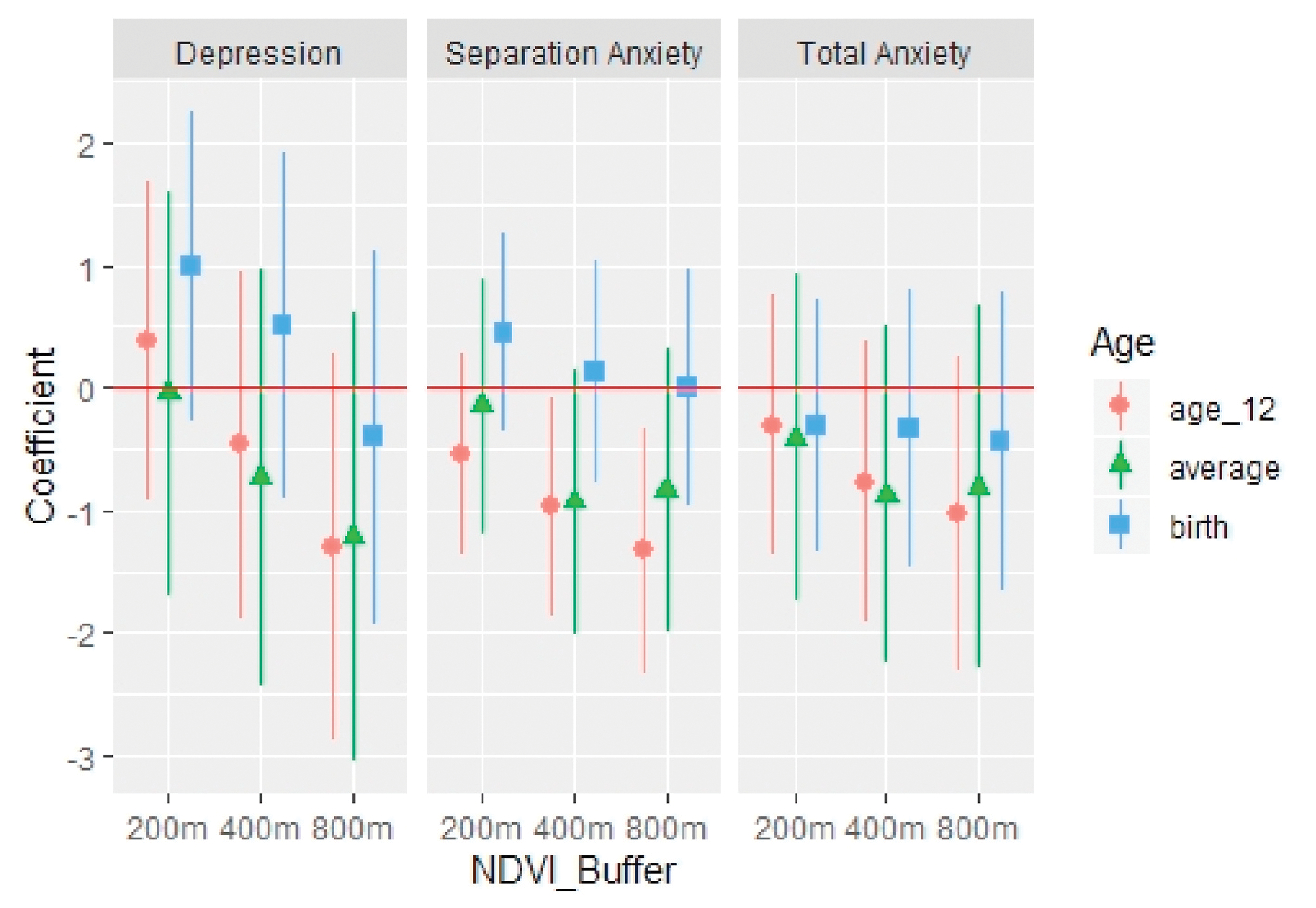
Estimates and confidence intervals of change in self-reported mental health outcomes (total depression score, separation anxiety subscale, and total anxiety score) per 0.1 change in NDVI in three buffer radii (200m, 400m, and 800m) from participant home address at birth, age 12, and averaged across childhood. Models included neurological toxics, community deprivation, traffic-related air pollution, blood lead level, and household income.
3.5. Greenness and depression
There were statistically significant, negative correlations between greenness and self-reported symptoms of depression in the 400m radius from the home address averaged across childhood (r = −0.15, p = 0.007) and 800m radius at all time points (birth: r = −0.17, p = 0.002; age 12 years: r = −0.17, p = 0.001; across childhood: r = −0.18, p = 0.001; Supplementary Table 2). However, after controlling for community deprivation, ECAT, blood lead, NNHI, and household income, NDVI was not associated with depression symptoms for any buffer radius or time period (Fig. 2).
4. Discussion
We examined the association between greenness and adolescent mental health in a birth cohort with complete address history to age 12 years. After adjusting for possible confounding pathways, we did not observe a significant relationship between greenness and self-reported depression. A previous analysis in a longitudinal study (Bezold et al., 2018b) found increased greenness associated with lower odds of self-reported depressive symptoms in adolescents. Possible causes for the discrepancy between that study and ours include higher NDVI resolution in our study (30 m × 30 m versus 1 km × 1 km) and smaller sample size (n = 339 versus n = 11,346) potentially hindering the ability to detect relationships between variables after covariate adjustment. With regard to anxiety, greenness was correlated with decreased scores for Generalized Anxiety Disorder, Obsessive-Compulsive Disorder, and Separation Anxiety in 400m and 800m radii. While we did not observe associations between NDVI in the 200 m radius at any age and anxiety outcomes, NDVI at 400 and 800 m radii were significantly associated with separation Anxiety after covariate adjustment.
Greenness has been found to be beneficial for social cohesion (de Vries et al., 2013; Dadvand et al., 2016; Maas, van Winsum-Westra, Verheij, de Vries and Groenewegen, 2009b), which in the context of the neighborhood contributes to mental well-being (Rios et al., 2012; Fone et al., 2014). It is plausible that greenness in these buffer distances may equate to communal areas such as parks, offering opportunity for social interaction. Such interaction is particularly relevant to adolescence as a developmental time for seeking connection to peers (McElhaney et al., 2008), potentially lessening symptoms of separation anxiety.
Although not associated with greenness in our findings, fear of physical injury was the anxiety subscale with the highest mean score and most participants meeting the threshold for elevation. Previous literature has suggested that fear is important for understanding how we interact with greenness. Louv (2005), when introducing the concept of nature deficit disorder in children, suggested lack of time spent outside may in part be due to parent and child fear of harm from strangers, violence, kidnapping, traffic, etc. Maas et al. (2009b) found green spaces generally enhance feelings of safety, but the opposite may be true in the urban core. When considering the context of neighborhood parks, perceptions of safety can be a concern (Groshong et al., 2020), and parents are less likely to encourage their adolescent children to engage with green spaces perceived as unsafe (Christian et al., 2015). However, when youth are able to share safe public green spaces, they are more likely able to build relationships and lessen separation anxiety. Therefore, our findings support the development and maintenance of safe public green spaces where adolescents can benefit from decreased anxiety.
Greenness in larger distances may also reflect greater opportunity for physical activity (Markevych et al., 2017). Previous research has found physical activity to be protective against anxiety and depression through alleviation of stress (Anderson and Shivakumar, 2013; van Minnen et al., 2010). Stress reduction theory (SRT; Ulrich et al., 1991) suggests the natural features of greenness generate positive feelings that can block negative thoughts and emotions, disrupting the stress response. Additionally, exercise is known to reduce the stress hormones adrenaline and cortisol while stimulating production of endorphins. Thus, correlation between greenness in 400m and 800m distances, but not in the 200m distance, may be explained by greater opportunity for physical activity that lowers stress.
Future research should assess how adolescents interact with greenspaces, whether they are used for physical activity or enhancing social cohesion, and the role of fear in perceptions of green spaces. Future studies of greenness and adolescent mental health should also consider which types of vegetation may confer most benefit for supporting mental health.
4.1. Strengths and limitations
This study contributes to a growing body of evidence examining the influence of greenness on self-reported symptoms of anxiety and depression in adolescents and is unique in examining greenness in three distinct developmental time periods. A major strength of this study is the longitudinal design. Because address history had been recorded for participants from birth through age 12 years, it was possible to assess exposure to greenness in three time periods: at birth, at age 12 years, and cumulatively, averaged across each year of life. As evidence regarding greenness and adolescent mental health grows, establishing the most beneficial timeframes of exposure is necessary. In this study, exposure to greenness at age 12 years was most beneficial for separation anxiety, an association that remained significant after adjustment for relevant covariates.
Another strength of this study is the measurement of symptoms of anxiety and depression in adolescents via self-report. Adolescent mental health disorders are often unrecognized (Cicchetti and Toth, 1998; Stein and Fazel, 2015), and parent report of adolescent internalizing behavior underestimates adolescent self-report (Chen et al., 2017). While parent report is valuable, particularly for measuring externalizing behaviors, self-report is more valid for measuring internalizing behaviors such as symptoms of anxiety and depression in adolescents (Aebi et al., 2017).
Limitations of this study include attrition within the cohort over the 12-year data collection period. While loss to follow-up did occur, participants at age 12 years did not differ significantly from those who did not participate. Additionally, the presence of potential unmeasured covariates in the relationship between greenness and adolescent mental health is a limitation of this work, although a causal inference approach was employed to minimize this limitation. Although many factors influence mental health, through comprehensive assessment only covariates associated with the outcome variable were included in regression models, thereby minimizing additional confounding. We acknowledge, however, that our DAGs and subsequent analyses represent our model of relationships between variables based on previous literature and potential alternative DAGs may be put forth. We analyzed only direct effects for this study; future studies may consider factors mediating the relationship between greenness and adolescent mental health. Lastly, because every participant had an atopic parent, we are not able to determine if this characteristic influenced our results.
Use of NDVI to estimate surrounding greenness is a strength, as this measure is used in the majority of current literature on the topic and may allow for comparisons across studies. However, estimating NDVI on cloud-free days in June approximates maximum exposure to leafy vegetation which may not be representative of average vegetation throughout the year. NDVI does not capture vegetation diversity, which may have differing effects on mental well-being.
4.2. Conclusion
The development of mental health disorders is complex, and the role of environmental exposures is not well understood. Because adolescent mental health disorders have lasting effects into adulthood, there is an urgent need for preventative interventions and proper screening. Our findings suggest residential surrounding greenness does not directly contribute to decreased symptoms of anxiety and depression overall but may decrease symptoms of separation anxiety in adolescents. Public health interventions at the neighborhood level, such as the provision of safe green spaces, may provide benefit for the entire community, independent of medical diagnosis or treatment.
Supplementary Material
Funding
This work was supported by the Robert Wood Johnson Foundation, Princeton, NJ, through the Future of Nursing Scholarship, Grant #74334, in partnership with the University of Cincinnati and Cincinnati Children’s Hospital Medical Center. Funding for the Cincinnati Childhood Allergy and Air Pollution Study is provided by the National Institute of Environmental Health Sciences (R01ES11170 and ES019890). Funders had no role in study design, collection, analyses, interpretation of data, writing of the report, or decision to submit the article for publication.
Abbreviations:
- CDI 2
Children’s Depression Inventory 2
- CCAAPS
Cincinnati Childhood Allergy and Air Pollution Study
- DAG
Directed Acyclic Graph
- ECAT
Elemental Carbon Attributable to Traffic
- NNHI
National Neurological Hazard Index
- NDVI
Normalized Difference Vegetation Index
- SCAS
Spence Children’s Anxiety Scale
Footnotes
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Credit author statement
Kim Hartley: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing, Funding acquisition, Joseph Perazzo: Conceptualization, Writing – review & editing, Cole Brokamp: Conceptualization, Writing – review & editing, Formal analysis, Methodology, Data curation. Gordon Lee Gillespie: Conceptualization, Writing – review & editing. Kim M. Cecil: Conceptualization, Writing – review & editing. Grace LeMasters: Conceptualization, Writing – review & editing. Kimberly Yolton: Conceptualization, Writing – review & editing. Patrick Ryan: Conceptualization, Writing – review & editing, Methodology, Data curation.
Human subjects protection
This work was determined to be non-human subjects research, not requiring oversight by the combined institutional review board of the affiliate organizations.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.110628.
References
- Aebi M, Kuhn C, Banaschewski T, Grimmer Y, Poustka L, Steinhausen HC, Goodman R, 2017. The contribution of parent and youth information to identify mental health disorders or problems in adolescents. Child Adolesc. Psychiatr. Ment. Health 11 (23). 10.1186/s13034-017-0160-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics, 2012, November 16. Stages of Adolescence from. https://www.healthychildren.org/English/ages-stages/teen/Pages/Stages-of-Adolescence.aspx. (Accessed 27 October 2020).
- Anderson E, Shivakumar G, 2013. Effects of exercise and physical activity on anxiety. Front. Psychiatr. 4 (27), 1–4. 10.3389/fpsyt.2013.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezold CP, Banay RF, Coull BA, Hart JE, James P, Kubzansky LD, Missmer SA, Laden F, 2018a. The association between natural environments and depressive symptoms in adolescents living in the United States. J. Adolesc. Health 62 (4), 488–495. 10.1016/j.jadohealth.2017.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezold CP, Banay RF, Coull BA, Hart JE, James P, Kubzansky LD, Missmer SA, Laden F, 2018b. The relationship between surrounding greenness in childhood and adolescence and depressive symptoms in adolescence and early adulthood. Ann. Epidemiol. 28 (4), 213–219. 10.1016/j.annepidem.2018.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchard MF, Bellinger DC, Weuve J, Matthews-Bellinger J, Gilman SE, Wright RO, Schwartz J, Weisskopf MG, 2009. Blood lead levels and major depressive disorder, panic disorder, and generalized anxiety disorder in US young adults. Arch. Gen. Psychiatr. 66 (12), 1313–1319. 10.1001/archgenpsychiatry.2009.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brokamp C, LeMasters G, Ryan P, 2016. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J. Expo. Sci. Environ. Epidemiol. 26 (4), 428–434. 10.1038/jes.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning M, Lee K, 2017. Within what distance does “greenness” best predict physical health? A systematic review of articles with GIS buffer analyses across the lifespan. Int. J. Environ. Res. Publ. Health 14 (7), 675. 10.3390/ijerph14070675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunst Kelly J., Ryan Patrick H., Brokamp Cole, Bernstein David, Reponen Tiina, Lockey James, Hershey Khurana, Gurjit K, Levin Linda, Grinshpun Sergey A., LeMasters Grace, 2015. Timing and duration of traffic-related air pollution exposure and the risk for childhood wheeze and asthma. Am. J. Respir. Crit. Care Med. 192 (4), 421–427. 10.1164/rccm.201407-1314OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2019. Blood Lead Levels in Children from. https://www.cdc.gov/nceh/lead/prevention/blood-lead-levels.htm. (Accessed 27 October 2020).
- Chen YY, Ho SY, Lee PC, Wu CK, Gau SS, 2017. Parent-child discrepancies in the report of adolescent emotional and behavioral problems in Taiwan. PloS One 12 (6), e0178863. 10.1371/journal.pone.0178863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christian HE, Klinker CD, Villanueva K, Knuiman MW, Foster SA, Zubrick SR, Divitini M, Wood L, Giles-Corti B, 2015. The effect of the social and physical environment on children’s independent mobility to neighborhood destinations. J. Phys. Activ. Health 12 (s1), S84–S93. 10.1123/jpah.2014-0271. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL, 1998. The development of depression in children and adolescents. Am. Psychol. 53 (2), 221–241. 10.1037//0003-066x.53.2.221. [DOI] [PubMed] [Google Scholar]
- Colton CW, Manderscheid RW, 2006. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev. Chronic Dis.: Public Health Res. Pract. Pol. 3 (2), 1–14. [PMC free article] [PubMed] [Google Scholar]
- Dadvand P, Bartoll X, Basagaña X, Dalmau-Bueno A, Martinez D, Ambros A, Cirach M, Triguero-Mas M, Gascon M, Borrell C, Nieuwenhuijsen MJ, 2016. Green spaces and general health: roles of mental health status, social support, and physical activity. Environ. Int. 91, 161–167. 10.1016/j.envint.2016.02.029. [DOI] [PubMed] [Google Scholar]
- Dantzer J, Ryan P, Yolton K, Parsons PJ, Palmer CD, Cecil K, Unrine JM, 2020. A comparison of blood and toenails as biomarkers of children’s exposure to lead and their correlation with cognitive function. Sci. Total Environ. 700, 134519. 10.1016/j.scitotenv.2019.134519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Interagency Forum on Child and Family Statistics, 2017. America’s Children: Key National Indicators of Well-Being, 2017: Adolescent Depression from. https://www.childstats.gov/americaschildren/depression.asp. (Accessed 27 October 2020).
- Figueras MA, Amador-Campos JA, Gomez-Benito J, del Barrio GV, 2010. Psychometric properties of the Children’s Depression Inventory in community and clinical sample. Spanish J. Psychol. 13 (2), 990–999. 10.1017/s1138741600002638. [DOI] [PubMed] [Google Scholar]
- Fone D, White J, Farewell D, Kelly M, John G, Lloyd K, Williams G, Dunstan F, 2014. Effect of neighbourhood deprivation and social cohesion on mental health inequality: a multilevel population-based longitudinal study. Psychol. Med. 44 (11), 2449–2460. 10.1017/S0033291713003255. [DOI] [PubMed] [Google Scholar]
- Fong KC, Hart JE, James P, 2018. A review of epidemiologic studies on greenness and health: updated literature through 2017. Curr. Environ. Health Rep. 5 (1), 77–87. 10.1007/s40572-018-0179-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gascon M, Triguero-Mas M, Martinez D, Dadvand P, Forns J, Plasencia A, Nieuwenhuijsen M, 2015. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int. J. Environ. Res. Publ. Health 12 (4), 4354–4379. 10.3390/ijerph120404354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gernes Rebecca, Brokamp Cole, Rice Glenn E., Wright J. Michael, Kondo Michelle C., Michael Yvonne L., Donovan Geoffrey H., Gatziolis Demetrios, Bernstein David, LeMasters Grace K., Lockey James E., Khurana Hershey Gurjit K, Ryan Patrick H., 2019. Using high-resolution residential greenspace measures in an urban environment to assess risks of allergy outcomes in children. Sci. Total Environ. 668, 760–767. 10.1016/j.scitotenv.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GIS Geography, 2020. What Is NDVI? from. https://gisgeography.com/ndvi-normalized-difference-vegetation-index/. (Accessed 27 October 2020).
- Groshong L, Wilhelm Stanis SA, Kaczynski AT, Hipp JA, 2020. Attitudes about perceived park safety among residents in low-income and high minority Kansas City, Missouri neighborhoods. Environ. Behav. 52 (6), 579–610. 10.1177/0013916518814291. [DOI] [Google Scholar]
- Hagan JF., Shaw JS., Duncan P. (Eds.). Bright Futures: Guidelines for the Health Supervision of Infants, Children, and Adolescents (third ed.). American Academy of Pediatrics. [Google Scholar]
- Hartig T, Mitchell R, de Vries S, Frumkin H, 2014. Nature and health. Annu. Rev. Publ. Health 35, 207–228. 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE, 2005. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatr. 62 (6), 617–627. 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M, 2011. Children’s Depression Inventory CDI2: Technical Manual, second ed. Multi-Health Systems, Inc, North Tonawanda, NY. [Google Scholar]
- Liu J, Liu X, Wang W, McCauley L, Pinto-Martin J, Wang Y, Li L, Yan C, Rogan WJ, 2014. Blood lead concentrations and children’s behavioral and emotional problems: a cohort study. JAMA Pediatrics 168 (8), 737–745. 10.1001/jamapediatrics.2014.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Louv R, 2005. Last Child in the Woods: Saving Our Children from Nature Deficit Disorder. Algonquin Books of Chapel Hill, Chapel Hill, NC. [Google Scholar]
- Maas J, Verheij R, De Vries S, Spreeuwenberg P, Schellevis F, Groenewegen P, 2009a. Morbidity is related to a green living environment. J. Epidemiol. Community 63 (12), 967–973. 10.1136/jech.2008.079038. [DOI] [PubMed] [Google Scholar]
- Maas J, van Winsum-Westra M, Verheij RA, de Vries S, Groenewegen PP, 2009b. Is green space in the living environment associated with people’s feelings of social safety? Environ. Plann.: Econ. Space 41, 1763–1777. 10.1068/a4196. [DOI] [Google Scholar]
- Madzia J, Ryan P, Yolton K, Percy Z, Newman N, LeMasters G, Brokamp C, 2019. Residential greenspace association with childhood behavioral outcomes. J. Pediatr. 207, 233–240. 10.1016/j.jpeds.2018.10.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markevych I, Schoierer J, Hartig T, Chudnovsky A, Hystad P, Dzhambov A, de Vries S, Triguero-Mas M, Brauer M, Nieuwenhuijsen M, Lupp G, Richardson EA, Astell-Burt T, Dimitrova D, Feng X, Sadeh M, Standl M, Heinrich J, Fuertes E, 2017. Exploring pathways linking greenspace to health: theoretical and methodological guidance. J. Environ. Res. 158, 301–317. 10.1016/j.envres.2017.06.028. [DOI] [PubMed] [Google Scholar]
- Mavoa S, Lucassen M, Denny S, Utter J, Clark T, Smith M, 2019. Natural neighbourhood environments and the emotional health of urban New Zealand adolescents. Landsc. Urban Plann. 191, 103638. 10.1016/j.landurbplan.2019.103638. [DOI] [Google Scholar]
- McCormick R, 2017. Does access to green space impact the mental well-being of children: a systematic review. J. Pediatr. Nurs. 37, 3–7. 10.1016/j.pedn.2017.08.027. [DOI] [PubMed] [Google Scholar]
- McElhaney KB, Antonishak J, Allen JP, 2008. “They like me, they like me not”: popularity and adolescents’ perceptions of acceptance predicting social functioning over time. Child Dev. 79 (3), 720–731. 10.1111/j.1467-8624.2008.01153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J, 2010. Lifetime prevalence of mental disorders in U.S. Adolescents: results from the national comorbidity survey replication-adolescent supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatr. 49 (10), 980–989. 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Minnen A, Hendriks L, Olff M, 2010. When do trauma experts choose exposure therapy for PTSD patients? A controlled study of therapist and patient factors. Behav. Res. Ther. 48 (4), 312–320. 10.1016/j.brat.2009.12.003. [DOI] [PubMed] [Google Scholar]
- National Association of State Mental Health Program Directors Council, 2006. Morbidity and Mortality in People with Serious Mental Illness. NASMHPD Medical Directors Council Publications and Reports, Alexandria, VA. [Google Scholar]
- National Institute of Mental Health, 2018. Teen Depression from. https://www.nimh.nih.gov/health/publications/teen-depression/index.shtml. (Accessed 27 October 2020).
- National Institute of Mental Health, 2019, February. Mental Illness from. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml. (Accessed 27 October 2020).
- Nishida A, Richards M, Stafford M, 2016. Prospective associations between adolescent mental health problems and positive mental wellbeing in early old age. Child Adolesc. Psychiatr. Ment. Health 10, 12. 10.1186/s13034-016-0099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohio-Kentucky-Indiana Regional Council of Governments, 2016. Demographics from. https://2040.oki.org/demographics/. (Accessed 27 October 2020).
- Patel V, Flisher AJ, Hetrick S, McGorry P, 2007. Mental health of young people: a global public-health challenge. Lancet 369 (9569), 1302–1313. 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- R Core Team, 2019. R: A Language and Environment for Statistical Computing. Foundation for Statistical Computing, R Vienna, Austria. [Google Scholar]
- Ramme R (n.d.) Spence Children’s Anxiety Scale: an Overview of Psychometric Findings. Retrieved October 27, 2020 from http://www.scaswebsite.com/docs/Ramme%20SCAS%20Psychomet%20evidence.pdf.
- Rios R, Aiken LS, Zautra AJ, 2012. Neighborhood contexts and the mediating role of neighborhood social cohesion on health and psychological distress among Hispanic and non-Hispanic residents. Ann. Behav. Med. 43 (1), 50–61. 10.1007/s12160-011-9306-9. [DOI] [PubMed] [Google Scholar]
- Ryan Patrick H., LeMasters Grace, Biagini Jocelyn, Bernstein David, Grinshpun Sergey A., Shukla Rakesh, Wilson Kimberly, Villareal Manuel, Burkle Jeff, Lockey James, 2005. Is it traffic type, volume, or distance? Wheezing in infants living near truck and bus traffic. J. Allergy Clin. Immunol. 116 (2), 279–284. 10.1016/j.jaci.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Ryan P, LeMasters GK, Biswas P, Levin L, Hu S, Lindsey M, Bernstein DI, Lockey J, Villareal M, Khurana Hershey GK, Grinshpun SA, 2007. A comparison of proximity and land sue regression traffic exposure models and wheezing in infants. Environ. Health Perspect. 115 (2), 278–284. 10.1289/ehp.9480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spence SH, 1998. A measure of anxiety symptoms among children. Behav. Res. Ther. 36 (5), 545–566. 10.1016/s0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- Stein K, Fazel M, 2015. Depression in young people often goes undetected. Practitioner 259 (1782), 17–22. [PubMed] [Google Scholar]
- Suttorp MM, Siegerink B, Jager KJ, Zoccali C, Dekker FW, 2015. Graphical presentation of confounding in directed acyclic graphs. Nephrol. Dial. Transplant. 30 (9), 1418–1423. 10.1093/ndt/gfu325. [DOI] [PubMed] [Google Scholar]
- Textor J, van der Zander B, Gilthorpe MK, Liskiewicz M, Ellison GTH, 2016. Robust causal inference using directed acyclic graphs: the R package ‘dagitty’. Int. J. Epidemiol. 45 (6), 1887–1894. 10.1093/ije/dyw341. [DOI] [PubMed] [Google Scholar]
- Ulrich RS, Simon RF, Losito BD, Fiorito E, Miles MA, Zelson M, 1991. Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 11 (3), 201–230. 10.1016/S0272-4944(05)80184-7. [DOI] [Google Scholar]
- United States Environmental Protection Agency, 2018. 2014 NATA Assessment Results from. https://www.epa.gov/national-air-toxics-assessment/2014-nata-assessment-results. (Accessed 27 October 2020).
- Vanaken GJ, Danckaerts M, 2018. Impact of green space exposure on children’s and adolescents’ mental health: a systematic review. Int. J. Environ. Res. Publ. Health 15 (12), EE2668. 10.3390/ijerph15122668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries S, van Dillen SME, Groenewegen PP, Spreeuwenberg P, 2013. Streetscape greenery and health: stress, social cohesion and physical activity as mediators. Soc. Sci. Med. 94, 26–33. 10.1016/j.socscimed.2013.06.030. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2019. Coming of Age: Adolescent Health from. https://www.who.int/news-room/spotlight/coming-of-age-adolescent-health#:~:text=Coming%20of%20age%3A%20adolescent%20health&text=The%20world%20now%20has%20more,between%2010%20and%2019%20years. (Accessed 27 October 2020).
- Yolton K, Khoury JC, Burkle J, LeMasters G, Cecil K, Ryan P, 2019. Lifetime exposure to traffic-related air pollution and symptoms of depression and anxiety at age 12 years. Environ. Res. 173, 199–206. 10.1016/j.envres.2019.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


