Abstract
Objectives
To determine recognition ability and the levels of esthetic tolerance of deep bite and anterior open bite (AOB) among laypeople and investigate the factors affecting levels of tolerance.
Materials and Methods
Using a questionnaire, laypeople (N = 100) were examined, and overbite was measured. They were tested for whether they recognized deep bite and AOB. Esthetic tolerance thresholds for deep bite and AOB were selected by incremental depiction in grayscale images. Stepwise logistic regression analyses were used to quantify the effect of recognition and other factors (age, sex, education level, occupation, history of orthodontic treatment, interest in orthodontic treatment or retreatment, and overbite presence) affecting the tolerance of overbite problems (α = 0.05).
Results
Of the participants, 55% and 94% recognized deep bite and AOB, respectively. Participants with a deep bite were significantly more likely to esthetically tolerate deep bite compared with those without a deep bite (odds ratio [OR], 3.57; 95% confidence interval [CI], 1.29–9.89). Participants who recognized a deep bite problem had significantly lower esthetic tolerance to deep bite compared with participants who did not recognize a deep bite (OR, 0.17; 95% CI, 0.06–0.45). None of the other eight chosen factors significantly affected the tolerance level of AOB (P > .05).
Conclusions
Participants with a deep bite or those who did not recognize a deep bite had significantly higher esthetic tolerance of deep bite than those without or those who recognized the problem (P < .05).
Keywords: Recognition, Esthetic tolerance, Deep bite, Anterior open bite
INTRODUCTION
The level of tolerance of malocclusion is an important psychological factor influencing an individual's decision to seek orthodontic treatment.1 In general, tolerance is the minimum threshold of acceptability.2 Esthetic tolerance of a type of malocclusion can be thought of as the greatest severity of that characteristic that is esthetically acceptable to an observer. Esthetic tolerance may be affected by age, education level, social status, and cultural differences.3–5 In addition, some studies have reported higher esthetic tolerance of a deep bite and anterior open bite (AOB) than protrusion and crowding,5,6 but others found that esthetic tolerance of a deep bite and AOB were low.3,7
Studies about the effect of recognition on the tolerance of a problem have been conducted mostly in the field of socioeconomics and with varied results.8,9 In orthodontics, patient tolerance of an appliance was closely related to how informed the patient was about the purpose of the treatment.10 Previous studies on the esthetic tolerance of malocclusion assessed several characteristics of malocclusion, and the factors affecting the esthetic tolerance for each characteristic were not considered separately.5,7,11–14 The factors influencing the esthetic tolerance of more severe malocclusion may differ from or may confound the factors influencing the tolerance of less severe malocclusions. It is not known whether the recognition of one type of malocclusion affects the esthetic tolerance of that malocclusion. Therefore, the purpose of this study was to determine the level of esthetic tolerance of deep bite and AOB by laypeople and examine the effects of overbite recognition and the following seven other factors on the esthetic tolerance of those malocclusion characteristics: age, sex, education level, occupation, history of orthodontic treatment, interest in orthodontic treatment or retreatment, and overbite presence. The null hypothesis was that none of the eight chosen factors would affect the level of esthetic tolerance of the overbite problems (deep bite and AOB) among the laypeople.
MATERIALS AND METHODS
Sample Selection
This cross-sectional study was approved by the Human Research Ethics Committee of the Faculty of Dentistry, Prince of Songkla University (EC6303-008). Because eight factors varying among laypeople were included in this study, a minimum sample of 80 was determined to be required based on the recommendation of at least 10 samples per variable for multiple regression analysis.15,16 Using a consecutive sampling method, 100 participants were recruited (aged 15 to 60 years) attending the University Dental Hospital from October 2020 to January 2021. All participants were laypeople who had no background in the health sciences. All participants provided signed informed consent before data collection.
Esthetic recognition and tolerance of overbite problems were assessed by an interviewer using a questionnaire. Each participant's own overbite was evaluated in a dental chair using a sterile dental mirror and periodontal probe by the same examiner. Overbite was measured as the vertical distance between the incisal edges of the upper right central incisor and the lower right central incisor at maximum intercuspation. Deep overbite was defined as a vertical overlap of >4 mm, whereas AOB was defined as a lack of vertical overlap (overbite <0 mm).17,18
Questionnaire
The questionnaire contained three sections. Section 1 included the following demographic information: age, sex, education, occupation, history of orthodontic treatment, and interest in orthodontic treatment or retreatment. Section 2 assessed the participant's esthetic recognition of various types of malocclusions. Participants were presented with a set of pictures showing the following six types of malocclusions: deep bite, AOB, crowding, anterior crossbite, spacing, and protrusion (Figure 1). To minimize distractions that might be caused by other parts of the face, all pictures showed only anterior occlusion at maximum intercuspation in grayscale, and the color of the teeth, lips, and gingival tissue were not distractors. Participants were asked to determine which images they considered to show unesthetic occlusion. After responding, information was given to the participants regarding the definitions of each type of malocclusion and possible consequences if not corrected (Table 1).19 Section 3 assessed the participant's tolerance of overbite problems using two sets of pictures depicting varying degrees of deep bite and AOB severity. Each set contained five computer-simulated grayscale pictures, starting with normal overbite (2 mm) as a reference, followed by deep bite of 4 mm in the first picture set (for deep bite tolerance) or edge-to-edge bite (for AOB tolerance) in the second picture set, then 1-mm increments or decrements in each consecutive picture (Figures 2 and 3). Participants were informed that the variable they were assessing had pictures arranged by ascending severity, and they were asked to choose the picture in each set that they could maximally tolerate esthetically.
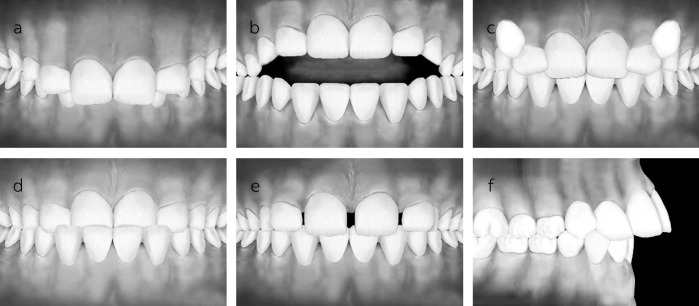
Figure 1.
Evaluation of recognition of malocclusion characteristics: (a) deep bite, (b) AOB, (c) crowding, (d) anterior crossbite, (e) spacing, and (f) protrusion.
Table 1. .
Definitions and Possible Consequences of Each Type of Malocclusion if Not Correcteda
| Malocclusion |
Explanation Script |
| Deep bite | Definition: When the bite is closed, the upper front teeth cover the bottom teeth too much. |
| Possible consequences if not corrected: Upper teeth can bite into lower gums, lower teeth can bite into the roof of the mouth, and possible gum disease and early enamel wear can develop. | |
| AOB | Definition: This occurs when the back teeth are together and the upper and lower front teeth do not overlap. This can result from excessive sucking, tongue thrusting, or mouth breathing. |
| Possible consequences if not corrected: swallowing problems, tongue pushes through teeth when swallowing, and possible speech problems. | |
| Crowding | Definition: There is insufficient space for the teeth. This can be a result of big teeth or inadequate space in the jaw or both. This may result in teeth that overlap, are rotated, or take on a crooked/staggered appearance. |
| Possible consequences if not corrected: hard to clean; possible cavities, especially between teeth; and gum disease. | |
| Anterior crossbite | Definition: The lower jaw sits in front of the upper jaw. |
| Possible consequences if not corrected: face has “bulldog” appearance, tooth wear, and stress on jaw joints. | |
| Spacing | Definition: There is too much space between teeth. It can result from missing teeth, undersized teeth, oversized jaws, or a combination of these conditions. |
| Possible consequences if not corrected: food gets stuck in open areas, possible cavities, and gum disease. | |
| Protrusion | Definition: The front teeth stick out (“buck” teeth). Teeth may appear protrusive because the upper jaw is too far forward, the lower jaw is too far back, the teeth grew in at an angle, or a combination of these conditions. Sometimes people who have protrusive front teeth also have a deep bite. |
| Possible consequences if not corrected: upper teeth are prone to accidental breaking; hard to comfortably close the mouth and lips, leading to dried-out oral tissues followed by tooth decay; speech problems; and a long, narrow face. |
Adapted from the American Association of Orthodontists.19
Figure 2.
Series of images showing increasing overbite in 1-mm increments: (a) normal overbite, (b) 4-mm overbite, (c) 5-mm overbite, (d) 6-mm overbite, and (e) 7-mm overbite.
Figure 3.
Series of images showing decreasing overbite in 1-mm increments: (a) normal overbite, (b) 0-mm overbite, (c) −1-mm overbite, (d) −2-mm overbite, and (e) −3-mm overbite.
Statistical Analysis
The content validity of the questionnaire was tested by three orthodontists with more than 5 years of experience using the Index of Item Objective Congruence (IOC).20 The IOC scores for each question ranged between 0.7 and 1.0, indicating that all experts agreed that all questions were consistent with the objectives. The same examiner remeasured the overbite in 30 randomly selected participants after an interval of 4 weeks. The intraclass correlation was 0.93, indicating strong intraexaminer reliability.
Participant demographic data and recognition and tolerance levels of deep bite and AOB were presented as descriptive statistics. Ordered logistic regression analysis was used to examine the eight chosen factor variables of the laypeople that may have affected their tolerance levels of overbite problems. Chi-square tests were initially conducted. Only exposure variables with P < .20 in the bivariate analysis were entered into the logistic regression analysis.21 Statistical analysis was carried out using SPSS (version 26.0; IBM, Chicago, Ill) at α = 0.05.
RESULTS
Characteristics of the Participants
Table 2 summarizes the demographic characteristics of the participants. The male:female ratio was 31:69. Of the participants, 47% had normal overbite, 37% had deep bite (≥4 mm), and 16% had AOB (≤0 mm). The percentages of recognition of AOB and deep bite were 94% and 55%, respectively.
Table 2. .
Demographic Characteristics of the Respondents and Percentages of Esthetic Recognition of Overbite (N = 100)
| General Characteristics |
Percentage |
| Sex | |
| Male | 31 |
| Female | 69 |
| Age, years | |
| <25 (generation Z) | 39 |
| 25–40 (generation Y) | 15 |
| 41–56 (generation X) | 44 |
| ≥57 (baby boomer) | 2 |
| Education | |
| <Bachelor's degree | 56 |
| ≥Bachelor's degree | 44 |
| History of orthodontic treatment | |
| No | 93 |
| Yes | 7 |
| Interest in orthodontic treatment or retreatment | |
| No | 53 |
| Yes | 47 |
| Overbite | |
| Normal overbite (1–3 mm) | 47 |
| Deep bite (>4 mm) | 37 |
| AOB (<0 mm) | 16 |
| Esthetic recognition of overbite problems | |
| Deep bite | 55 |
| AOB | 94 |
Percentage Esthetic Tolerance of Overbite Problems
Figure 4 shows that 14% of the participants could not esthetically tolerate any degree of deep bite (≥4 mm); 28%, 42%, 9%, and 7% could maximally tolerate deep bite to the levels of 4 mm, 5 mm, 6 mm, and 7 mm, respectively. Figure 5 shows that 12% of the participants could not esthetically tolerate any degree of AOB (≤0 mm); 43%, 28%, 14%, and 3% could maximally tolerate AOB to the levels of 0 mm, −1 mm, −2 mm, and −3 mm, respectively.
Figure 4.
Percentage of participants who could maximally esthetically tolerate each level of a deep bite (n = 100). OB indicates overbite in mm.
Figure 5.
Percentage of participants who could maximally esthetically tolerate each level of an AOB (n = 100). OB indicates overbite in mm.
Factors Related to Esthetic Tolerance of Overbite Problems
Of the eight chosen factor variables of the laypeople, participant recognition of deep bite (P < .001), history of orthodontic treatment (P = .20), education level (P = .09), and the participant having a deep bite (P = .02) passed the entrance criteria for ordered logistic regression analysis of factors affecting the esthetic tolerance of deep bite. A participant's ability to recognize deep bite was significantly associated with being less tolerant of deep bite (odds ratio [OR], 0.17; 95% confidence interval [CI], 0.06–0.45; P < .001; Table 3). However, the participant having a deep bite was significantly associated with being more tolerant of deep bite (OR, 3.57; 95% CI, 1.29–9.89; P < .01; Table 3). None of the eight chosen factor variables passed the entrance criteria for further logistic regression analysis of AOB. Therefore, the factors affecting the esthetic tolerance of AOB could not be analyzed.
Table 3. .
Ordered Logistic Regression of the Factors Relating to the Esthetic Tolerance of Deep Bite
| Variables |
Esthetic Tolerance of Deep Bite, n (%) |
OR (95% CI)a |
P Value |
|||
| 4 mm |
5 mm |
6 mm |
7 mm |
|||
| Education | ||||||
| >Bachelor's degree, reference | 16 (31.4) | 23 (45.1) | 6 (11.8) | 6 (11.8) | – | – |
| <Bachelor's degree | 12 (34.3) | 19 (54.3) | 3 (8.6) | 1 (2.9) | 1.62 (0.7–3.71) | .42 |
| History of orthodontic treatment | ||||||
| Yes, reference | 4 (57.1) | 3 (42.9) | – | – | – | – |
| No | 25 (31.6) | 39 (49.4) | 8 (10.1) | 7 (8.9) | 2.92 (0.53–15.80) | .86 |
| Participant's overbite | ||||||
| Normal overbite, 1–3 mm, reference | 18 (47.4) | 16 (42.1) | 2 (5.3) | 2 (5.3) | – | – |
| Deep bite, >4 mm | 4 (11.1) | 21 (58.3) | 6 (16.7) | 5 (13.9) | 3.57 (1.29–9.89) | .01* |
| AOB, <0 mm | 6 (50) | 5 (41.7) | 1 (8.3) | – | 1.16 (0.22–3.38) | .83 |
| Recognition of deep bite | ||||||
| Unrecognized, reference | 4 (9.3) | 27 (62.8) | 7 (16.3) | 5 (11.6) | – | – |
| Recognized | 24 (55.8) | 15 (34.9) | 2 (4.7) | 2 (4.7) | 0.17 (0.06–0.45) | <.001** |
OR > 1 indicates an increased chance of having esthetic tolerance of deep bite compared with the reference, whereas OR < 1 indicates a decreased chance of having esthetic tolerance of deep bite compared with the reference.
P < .05; ** P < .001.
DISCUSSION
This study specifically assessed the esthetic recognition and tolerance of deep bite and AOB. Laypeople recognized AOB easily but were less likely to be able to recognize a deep bite. These findings were consistent with a previous study despite differences in the study populations and data collection methods.22 When malocclusion is assessed using a combination of more than one trait, the most obvious and more easily recognized characteristic may not only dominate the participants' grading of the severity of the malocclusion but also hide the presence of the less obvious malocclusion. As the current study was centered on the recognition of a single occlusal trait (overbite: deep bite and open bite), the risk of confounding by factors introduced by the other traits was excluded to better focus on the degree of overbite.
Images of different traits of malocclusion were used without text labels to evaluate how participants visually recognized the esthetics of anterior occlusion. Eliminating the influence of labels was believed to help in more accurately determining the participants' recognition of each malocclusion characteristic. Although study models could provide more information and detail about a malocclusion, the use of models may not be suitable for studying the ability of laypeople to recognize malocclusion. This is because laypeople normally judge the esthetics of anterior occlusion by visual inspection from the frontal view and not by viewing the posterior occlusion.
The Aesthetic Component (AC) of the Index of Orthodontic Treatment Need (IOTN) was originally designed for assessing treatment need and priority by orthodontists.23,24 The AC contains 10 photographs of the anterior occlusion showing different levels of dental attractiveness ranging from best to worst appearance. Studies have used the IOTN to compare the esthetic treatment need perceptions between patients and orthodontists.24–26 However, each image of the index contains a mixture of occlusal traits, and no images include AOB. One abnormality may possibly dominate the participants' responses, whereas the other abnormalities in the image may not be recognized. Thus, the index may not accurately reflect an individual's recognition of a single type of malocclusion.
A small proportion of participants in the current study (12%–14%) could not tolerate any degree of overbite that deviated from normal. It may be implied that the majority of laypeople could esthetically accept various degrees of overbite problems, which was in agreement with another study reporting that overbite deviations only had a small influence on the oral health–related quality of life of adolescents.27 Although studies reported differences in malocclusion recognition between orthodontists and laypeople,5,28 none compared esthetic tolerance. Further study comparing the tolerance levels for malocclusion characteristics between the two groups may be useful for improving communication between orthodontists and laypeople.
The initial ability of the participants to recognize deep bite and a participant having a deep bite were identified as factors influencing the esthetic tolerance level for that characteristic. When other chosen factor variables were controlled, participants who initially did not recognize deep bite malocclusion were 5.88 times more likely to esthetically tolerate a deep bite than participants who recognized a deep bite. In addition, participants with a deep bite were 3.57 times more likely to esthetically tolerate deep bite than participants with normal overbite. These results indicated that deep bite may often not be the main reason that patients are motivated to seek orthodontic treatment. Because patient tolerance of malocclusion is important for determining demand, motivation, and cooperation during orthodontic treatment, patients should be informed about the existence of deep overbite relationships because they may result in trauma to the maxillary palatal tissue29,30 and attrition of the mandibular incisor edges.31,32 Orthodontists should also take time to explain to patients why deep bite correction is an important part of the comprehensive orthodontic treatment plan.
This study had some limitations that lead to suggestions for the improvement of future research. First, previous studies found that age, sex, education level, and socioeconomic factors were related to self-recognition of malocclusion.4,22,33,34 The lack of influence of these factors found in the current study may have been attributed to type II error. Increasing the number of samples in each stratification could help to yield more accurate results. Also, presenting a larger number of samples with a greater variety of malocclusion characteristics could provide useful information on how having a malocclusion could affect lay recognition and level of tolerance of overbite problems. Second, using facial and dental photographs may better improve visual recognition of the characteristics studied in comparison with using computer-simulated drawings of frontal occlusion only. Third, using a visual analog scale instead of a series of images ranging from normal to severe conditions may provide more precise information on an interval scale and may reduce the halo effects (a trend toward the middle)35 for esthetic tolerance determination, although participants may find it difficult to convert the amount of overbite to an abstract line.
CONCLUSIONS
Laypeople more easily recognized AOB and less easily recognized deep bite.
Esthetic tolerance was high for deep bite, but low for AOB.
Participants with a deep bite themselves were more likely to tolerate deep bite.
Participants who recognized deep bite were more likely to be less tolerant of deep bite.
None of the eight chosen factor variables (age, sex, education level, occupation, history of orthodontic treatment, interest in orthodontic treatment or retreatment, overbite presence, and recognition of overbite deviation) significantly influenced the esthetic tolerance of AOB.
REFERENCES
- 1.Albino JE, Cunat JJ, Fox RN, Lewis EA, Slakter MJ, Tedesco LA. Variables discriminating individuals who seek orthodontic treatment. J Dent Res . 1981;60(9):1661–1667. doi: 10.1177/00220345810600090501. [DOI] [PubMed] [Google Scholar]
- 2.Paravina RD, Pérez MM, Ghinea R. Acceptability and perceptibility thresholds in dentistry: a comprehensive review of clinical and research applications. J Esthet Restor Dent . 2019;31(2):103–112. doi: 10.1111/jerd.12465. [DOI] [PubMed] [Google Scholar]
- 3.Flores-Mir C, Silva E, Barriga M, Lagravere M, Major P. Lay person's perception of smile aesthetics in dental and facial views. J Orthod . 2004;31(3):204–209. doi: 10.1179/146531204225022416. [DOI] [PubMed] [Google Scholar]
- 4.Sriphadungporn C, Chamnannidiadha N. Perception of smile esthetics by laypeople of different ages. Prog Orthod . 2017;18(1):1–8. doi: 10.1186/s40510-017-0162-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soh J, Chew MT, Chan YH. Perceptions of dental esthetics of Asian orthodontists and laypersons. Am J Orthod Dentofacial Orthop . 2006;130(2):170–176. doi: 10.1016/j.ajodo.2005.05.048. [DOI] [PubMed] [Google Scholar]
- 6.Srivastava SC, Verma V, Panda S, Anita G. Perception of esthetics of different malocclusion traits by laypersons. Int J Indian Ortho Soc . 2013;47(4):474–478. [Google Scholar]
- 7.Helm S, Kreiborg S, Solow B. Psychosocial implications of malocclusion: a 15-year follow-up study in 30-year-old Danes. Am J Orthod . 1985;87(2):110–118. doi: 10.1016/0002-9416(85)90020-x. [DOI] [PubMed] [Google Scholar]
- 8.García-Castro JD, Rodríguez-Bailón R, Willis GB. Perceiving economic inequality in everyday life decreases tolerance to inequality. J Exp Soc Psychol . 2020;90:104019. [Google Scholar]
- 9.Trump KS. Income inequality influences perceptions of legitimate income differences. Br J Polit Sci . 2018;48(4):929–952. [Google Scholar]
- 10.Araújo EA, Andrade I, Jr, Brito Gde M, Guerra L, Horta MCR. Perception of discomfort during orthodontic treatment with tongue spurs. Orthodontics . 2011;12(3):260–267. [PubMed] [Google Scholar]
- 11.Tickle M, Kay EJ, Bearn D. Socio-economic status and orthodontic treatment need. Community Dent Oral Epidemiol . 1999;27(6):413–418. doi: 10.1111/j.1600-0528.1999.tb02040.x. [DOI] [PubMed] [Google Scholar]
- 12.Kim Y. Study on the perception of orthodontic treatment according to age: a questionnaire survey. Korean J Orthod . 2017;47(4):215–221. doi: 10.4041/kjod.2017.47.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pabari S, Moles DR, Cunningham SJ. Assessment of motivation and psychological characteristics of adult orthodontic patients. Am J Orthod Dentofacial Orthop . 2011;140(6):e263–e272. doi: 10.1016/j.ajodo.2011.06.022. [DOI] [PubMed] [Google Scholar]
- 14.Yamashita H, Yotsuya K, Takeuchi T, et al. Awareness of malalignment and malocclusion in children and their guardians. Bull Tokyo Dent Coll . 2008;49(1):7–13. doi: 10.2209/tdcpublication.49.7. [DOI] [PubMed] [Google Scholar]
- 15.Moons KG, de Groot JA, Bouwmeester W, et al. Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med . 2014;11(10):e1001744. doi: 10.1371/journal.pmed.1001744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pavlou M, Ambler G, Seaman SR, et al. How to develop a more accurate risk prediction model when there are few events BMJ. 2015. 351:h3868. [DOI] [PMC free article] [PubMed]
- 17.Tavares CAE, Allgayer S. Open bite in adult patients. Dental Press J Orthod . 2019;24(5):69–78. doi: 10.1590/2177-6709.24.5.069-078.bbo. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta N, Tripathi T, Rai P, Kanase AN. A comparative evaluation of bite opening by temporary anchorage devices and Connecticut intrusion arch: an in vivo study. Int J Orthod Rehabil . 2017;8(4):129–135. [Google Scholar]
- 19.American Association of Orthodontists. 7 Common bite problems in children and adults. Available at https://www3.aaoinfo.org/blog/7-common-bite-problems. Accessed December 2021.
- 20.Rovinelli RJ, Hambleton RK. On the use of content specialists in the assessment of criterion-referenced test item validity. Dutch J Educ Res . 1977;2:49–60. [Google Scholar]
- 21.Thiesen G, Gribel BF, Freitas MPM, Oliver DR, Kim KB. Mandibular asymmetries and associated factors in orthodontic and orthognathic surgery patients. Angle Orthod . 2018;88(5):545–551. doi: 10.2319/111517-785.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flores-Mir C, Silva E, Barriga MI, Valverde RH, Lagravère MO, Major PW. Laypersons' perceptions of the esthetics of visible anterior occlusion. J Can Dent Assoc . 2005;71(11):849–849d. [PubMed] [Google Scholar]
- 23.Brook PH, Shaw WC. The development of an index of orthodontic treatment priority. Eur J Orthod . 1989;11(3):309–320. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 24.Aikins EA, Dacosta OO, Onyeaso CO, Isiekwe MC. Self perception of malocclusion among Nigerian adolescents using the aesthetic component of the IOTN. Open Dent J . 2012;6:61–66. doi: 10.2174/1874210601206010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abu Alhaija ES, Al-Nimri KS, Al-Khateeb SN. Self-perception of malocclusion among north Jordanian school children. Eur J Orthod . 2005;27(3):292–295. doi: 10.1093/ejo/cjh094. [DOI] [PubMed] [Google Scholar]
- 26.Albarakati SF. Self-perception of malocclusion of Saudi patients using the aesthetic component of the IOTN index. Pak Oral Dent J . 2007;27:45–51. [Google Scholar]
- 27.Fabian S, Gelbrich B, Hiemisch A, Kiess W, Hirsch C. Impact of overbite and overjet on oral health-related quality of life of children and adolescents. J Orofac Orthop . 2018;79(1):29–38. doi: 10.1007/s00056-017-0114-0. [DOI] [PubMed] [Google Scholar]
- 28.Hamdan AM, Singh V, Rock W. Perceptions of dental aesthetics of Class III and anterior open bite malocclusions: a comparison between 10- to 11-year-old schoolchildren and orthodontists. Angle Orthod . 2012;82(2):202–208. doi: 10.2319/053111-359.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sulistiawati S, Awalia H, Zakyah AD, Putri JA. The effect of deep bite on periodontal status of anterior teeth. J Indones Dent Assoc . 2020;3(2):71–75. [Google Scholar]
- 30.Zimmer B, Seifi-Shirvandeh N. Changes in gingival recession related to orthodontic treatment of traumatic deep bites in adults. J Orofac Orthop . 2007;68(3):232–244. doi: 10.1007/s00056-007-0651-z. [DOI] [PubMed] [Google Scholar]
- 31.Khayat N, Winocur E, Kedem R, Winocur Arias O, Zaghal A, Shpack N. The prevalence of temporomandibular disorders and dental attrition levels in patients with posterior crossbite and/or deep bite: a preliminary prospective study. Pain Res Manag . 2021;2021:1–8. doi: 10.1155/2021/8827895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ritchard A, Welsh A, Donnelly C. The association between occlusion and attrition. Aust Orthod J . 1992;12(3):138–142. [PubMed] [Google Scholar]
- 33.Chia R, Allred L, Grossnickle W, Lee G. Effects of attractiveness and gender on the perception of achievement-related variables. J Soc Psychol . 1998;138(4):471–477. doi: 10.1080/00224549809600401. [DOI] [PubMed] [Google Scholar]
- 34.Reichmuth M, Greene KA, Orsini MG, Cisneros GJ, King GJ, Kiyak HA. Occlusal perceptions of children seeking orthodontic treatment: impact of ethnicity and socioeconomic status. Am J Orthod Dentofacial Orthop . 2005;128(5):575–582. doi: 10.1016/j.ajodo.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 35.Gift AG. Visual analogue scales: measurement of subjective phenomena. Nurs Res . 1989;38:286–288. [PubMed] [Google Scholar]