Abstract
The COVID-19 pandemic highlighted the need to prioritise mature digital health and data governance at both national and supranational levels to guarantee future health security. The Riyadh Declaration on Digital Health was a call to action to create the infrastructure needed to share effective digital health evidence-based practices and high-quality, real-time data locally and globally to provide actionable information to more health systems and countries. The declaration proposed nine key recommendations for data and digital health that need to be adopted by the global health community to address future pandemics and health threats. Here, we expand on each recommendation and provide an evidence-based roadmap for their implementation. This policy document serves as a resource and toolkit that all stakeholders in digital health and disaster preparedness can follow to develop digital infrastructure and protocols in readiness for future health threats through robust digital public health leadership.
Keywords: Public Health, COVID-19, Health policy, Other study design
Summary box.
The Riyadh Declaration on Digital Health articulated nine recommendations for data and digital health that need to be adopted by the global health community to address future pandemics and health threats.
We provide an evidence-based roadmap for the implementation of the nine Riyadh Declaration recommendations.
Some critical requirements for implementation include developing contextually sensitive communication strategies; instigating infoveillance (information monitoring) capabilities with fact-checking underpinned by legal standards; technology and data governance to support standardisation; a global minimum dataset to guarantee data usability and integrity based on agreed standards; and education providers and industry working closely to co-create meaningful curricula after establishing gaps in staff skills and capabilities.
The next step will be to reach a consensus on which areas to prioritise to achieve digital transformation in an equitable, inclusive and sustainable manner.
Introduction
The COVID-19 pandemic highlighted the need to prioritise mature digital health and data governance at both national and supranational levels to guarantee future health security. The Riyadh Declaration on Digital Health1 was formulated during the Riyadh Global Digital Health Summit, a landmark forum held in 2020 that highlighted the importance of digital technology, data and innovation for resilient global health and care systems. At the summit, a panel of 13 experts articulated 7 key priorities and 9 recommendations (box 1) for data and digital health that need to be adopted by the global health community to address future pandemics and health threats.
Box 1. Recommendations from the Riyadh Global Digital Health Summit.
Implement data-driven and evidence-based protocols for clear and effective communication with common messaging to build citizens’ trust.
Work with global stakeholders to confront propagation of misinformation or disinformation through social media platforms and mass media.
Implement a standard global minimum dataset for public health data reporting and a data governance structure tailored to communicable diseases.
Ensure countries prioritise digital health, particularly, improving digital health infrastructure and reaching digital maturity.
Enable health and care organisations by providing the necessary technology to collect high-quality data in a timely way and promote sharing to create health intelligence.
Cultivate a health and care workforce with the knowledge, skills and training in data and digital technologies required to address current and future public health challenges.
Ensure surveillance systems combine an effective public health response with respect for ethical and privacy principles.
Develop digital personal tools and services to support comprehensive health programmes (in disease prevention, testing, management and vaccination) globally.
Maintain, continue to fund and innovate surveillance systems as a core component of the connected global health system for rapid preparedness and optimal global responses.
The Riyadh Declaration on Digital Health was a call to action to create the infrastructure needed to share effective digital health evidence-based practices and high-quality, real-time data locally and globally to provide actionable information to more health systems and countries. Here, we expand on each recommendation and provide an evidence-based roadmap for their implementation and a toolkit to enhance global health security by preparing for future health threats through robust digital public health leadership (see table 1). The Riyadh Declaration was borne out of the COVID-19 pandemic and therefore the recommendations and solutions are applicable to communicable diseases. However, it is also important to note that the digital transformation of health applies to every area of healthcare and the threats to it, not least other impending threats such as the effects of climate change, making this roadmap also applicable and generalisable to non-communicable disease.
Table 1.
Roadmap to implementation of the Riyadh declaration on digital health recommendations
| Recommendation | Roadmap |
| Implement data-driven and evidence-based protocols for clear and effective communication with common messaging to build citizens’ trust |
|
| Work with global stakeholders to confront propagation of misinformation or disinformation through social media platforms and mass media |
|
| Implement a standard global minimum dataset for public health data reporting and a data governance structure tailored to communicable diseases |
|
| Ensure countries prioritise digital health, particularly, improving digital health infrastructure and reaching digital maturity |
|
| Enable health and care organisations by providing the necessary technology to collect high-quality data in a timely way and promote sharing to create health intelligence |
|
| Cultivate a health and care workforce with the knowledge, skills and training in data and digital technologies required to address current and future public health challenges |
|
| Ensure surveillance systems combine an effective public health response with respect for ethical and privacy principles |
|
| Develop digital personal tools and services to support comprehensive health programmes (in disease prevention, testing, management and vaccination) globally |
|
| Maintain, continue to fund and innovate surveillance systems as a core component of the connected global health system for rapid preparedness and optimal global responses |
|
Recommendation 1: implement data-driven and evidence-based protocols for clear and effective communication with common messaging to build citizens’ trust
Rationale and evidence
Data-driven initiatives could considerably improve information gathering and decision making, but there remain methodological concerns about bias, lack of transparency and misguided/misinterpreted information fuelling further infodemics.2 Clear and effective communication is necessary for more nuanced knowledge production and implementation.3 Experience from other infectious disease epidemics (eg, Zika virus, ebolavirus) demonstrated a need to develop and disseminate accurate information to successfully empower affected local communities.4 Validating those observations, the COVID-19 pandemic additionally highlighted the role of social media in the speed and penetration of misinformation, often interfering with citizens’ ability to trust and follow accurate health advice to protect individual and community health.5
Key requirements for implementation
The implementation of postpandemic protocols requires a shift towards contextually sensitive communication strategies, as effective healthcare communication is not simply about messaging. Instead, there exists an interactive, iterative process of information collection and exchange, inclusive of opinions and reactions by individuals, population groups and institutions to different risk aspects.6 7 New models must consider a context of continuously evolving technical and clinical knowledge and simultaneously acknowledge uncertainty.8 In the case of the latter, prioritising transparency and the rationale for decision making (including evidence, ie, used in decision making) can prove effective when communicated with empathy.9 Postpandemic protocols should anticipate disagreement to emerge at many levels, for example, due to the contestation of available data and/or expertise10 11; the legitimacy of decision making12–14 and competing values,6 15 16 especially in areas that can cut across a range of policy areas and disciplinary boundaries.
Data-driven and evidence-based protocols must also move beyond a static perspective of a single link between an evidence base and an optimal public health communication strategy; multiple facets might need to be considered and communications developed ongoingly. Postpandemic protocols need to acknowledge that communication delivery and message development are interdependent, impacting the eventual success of implementation and citizens’ trust. As citizens’ engagement with and response to public health information are influenced by their cultural and social identity,17 these latter factors will also determine what is perceived as a ‘trustworthy authority’ disseminating the public health information, and what type of medical leadership would be most effective.18 19
Recommendation 2: work with global stakeholders to confront propagation of misinformation or disinformation through social media platforms and mass media
Rationale and evidence
The propagation of health misinformation is gaining more attention as a significant public health concern.20–22 Given the growing popularity of different social media platforms and their potential in propagating misinformation, the ability to judge the credibility of information and what constitutes a ‘trustworthy authority’ becomes crucial.23 24 It is also becoming increasingly difficult to disentangle online news from users’ perspectives, regardless of authenticity and/or accuracy.25 Importantly, objective facts can be less influential in shaping public opinion than those appealing to emotions and personal beliefs.26
Key requirements for implementation
A multifaceted approach is necessary to combat misinformation. Using the four pillars of infodemic management recently proposed by the WHO as a basis,27 such an approach would involve: (1) the development of at different levels (organisational, national, regional) through investment in appropriate toolkits to perform such tasks (eg, extracting structured information from unstructured texts)28; (2) the development of a fact-checking culture with the appropriate reach and speed to counter misinformation29 supported by a network of related activities, such as news organisations striving to improve on their transparency and ‘findability’30; (3) greater streamlining of standards and legal frameworks, so that the above actions and activities are firmly based on grounds of legitimacy and transparency (eg, the Code of Principles from the International Fact-Checking Network https://www.ifcncodeofprinciples.poynter.org) and the 2017 Joint UN, OSCE and OAS Declaration on ‘Fake News’, Disinformation and Propaganda (https://www.osce.org/files/f/documents/6/8/302796.pdf), which help to provide a common legal understanding and (4) national efforts to improve digital literacy, as part of national development programmes, to improve citizens’ resilience to misinformation.31
Recommendation 3: implement a standard global minimum dataset for public health data reporting and a data governance structure tailored to communicable and non-communicable diseases
Rationale and evidence
The use of sophisticated tools and methodologies such as artificial intelligence (AI) in addressing pandemics relies on leveraging large amounts of rich data that must accurately capture the situations and context intended to be modelled. Collecting and sharing high-quality data for AI tasks is challenged by the many different types of data representing health, such as social determinants of health (SDOH), clinical care and behavioural patterns32 and its intrinsic heterogeneity governed by variable reporting and clinical practice. Models that do not account for this heterogeneity often fail to generalise. Overcoming this challenge requires novel approaches to capturing high-quality data, standardising disparate data and strengthening our capacity to learn from multimodal data.
Key requirements for implementation
A first key requirement is to capture complex and relevant health data. Health and healthcare are complex and multidimensional, especially in the global environment, but health mostly happens in our neighbourhood. SDOH (eg, nutritious food, employment, housing access and quality) have a significant impact and often explain more about health status than clinical factors.33 While some of these data such as real-time mobility and social interaction data can be captured from smartphones, other social determinants, such as education, change over years, so are slow to capture. SDOH data require clinical context. Healthcare data can include claims that come from administrative billing databases and electronic health records (EHRs). However, claims data are slow to capture and are limited in their ability to represent social context, and not all countries produce claims data. EHR data, when available, can provide rich clinical information, but this rich information is often stored as natural language text. The massive global variability in populations and social and environmental contexts mandates diversity in data sampling to leverage health and social data globally to address health emergencies.
A second key requirement is the technology and data governance to support standardisation. Standards are essential for sharing and exchanging health data and information. International methodologies and approaches must be supported to standardise data both in and between countries, where ‘standardising’ means the many facets of leveraging data for meaningful insights such as data structure, processes, linkage and analysis.
Standards may pertain to security, data transport, data format or structure, or the meanings of data; common data models standardise the format and representation of data as well as tools that make this transformation easier (eg, OHDSI; https://www.ohdsi.org). Data sharing can be supported through standards for electronic information exchange such as HL7 FHIR, the most common interoperability standard.34 35 A global minimum dataset specifically for pandemics would help focus data collection and standardisation efforts to ensure a basic level of data integrity and usability. Examples include minimum datasets from the European Centre for Disease Prevention (ECDC), Centers for Disease Control and Prevention (CDC) and WHO to lead to international exchange of information about outbreaks. Managing the availability, usability, integrity and security of these data also depends on data governance, which should recognise disparities between countries in their capacity to leverage health data for large-scale analytics. Furthermore, since data relevant to addressing a global pandemic comes from many different sources, public–private partnerships can help to build a global ecosystem where data is routinely collected, standardised and shared for use, for example, through the WHO Data Platform, which provides access to health-related data for all Member States monitoring global, regional and country trends (https://www.who.int/standards/classifications).
Recommendation 4: ensure countries prioritise digital health, particularly, improving digital health infrastructure and reaching digital maturity
Rationale and evidence
In 2005, the World Health Assembly, through its resolution WHA58.28 on eHealth, urged Member States ‘to consider drawing up a long-term strategic plan for developing and implementing eHealth services…to develop the infrastructure for information technologies for health…to promote equitable, affordable and universal access to their benefits’.36 This aim was reiterated in 2019 by the WHO recommendations on ‘Global strategy on digital health 2020–2025’.37 The vision is to improve healthcare globally by accelerating the development and adoption of appropriate, accessible, scalable and sustainable digital health solutions, developing infrastructure and applications that enable countries to use health data to promote health and well-being for their populations. The case for a coherent digital health strategy was amplified by the COVID-19 pandemic.
Key requirements for implementation
Building the value proposition
Digital health technology infrastructures have been a lifeline during the pandemic, providing a ‘new normal’ around engaging patients and the population using digital technologies.38–41 This momentum now needs to be consolidated through clear communication regarding the scale of investment, multidimensional outcomes, organisational impacts and value of digital health infrastructures for improving care coordination, quality, and, ultimately, the health of the population at large.42
Building the knowledge base
Leveraging the digital infrastructure to better engage with and use the information created during a patient’s healthcare journey can be achieved through research-ready clinical records.43–45 This can be achieved through the identification of a limited, standardised core of research-related components as basic elements across healthcare systems in order to facilitate individual and cooperative clinical research activities,46 47 as well as sentinel event surveillance, such as infectious disease outbreaks.48 49
Integrating data across various sources
The use of data across various sources (clinical, public health and commercial) can leverage the full range of available information and improve healthcare delivery for infectious diseases.50 For this to be successful, protocols must be developed to build interoperability as a natural and seamless element of data sources,51 including information sources outside of ‘mainstream’ healthcare such as patient-generated data.52
Creating a participative, mature culture
Digital infrastructure should be designed to strengthen the patient–clinician interactions through better patient portals, as well as the increased availability of lay-oriented, user-friendly, clinical and non-medical health data. However, this requires that participation barriers to such infrastructure remain low and complexity is incremental.53 A learning culture also incorporates the need for constant improvement through evaluation and innovation as an important component to eventually achieving digital maturity (figure 1).
Figure 1.
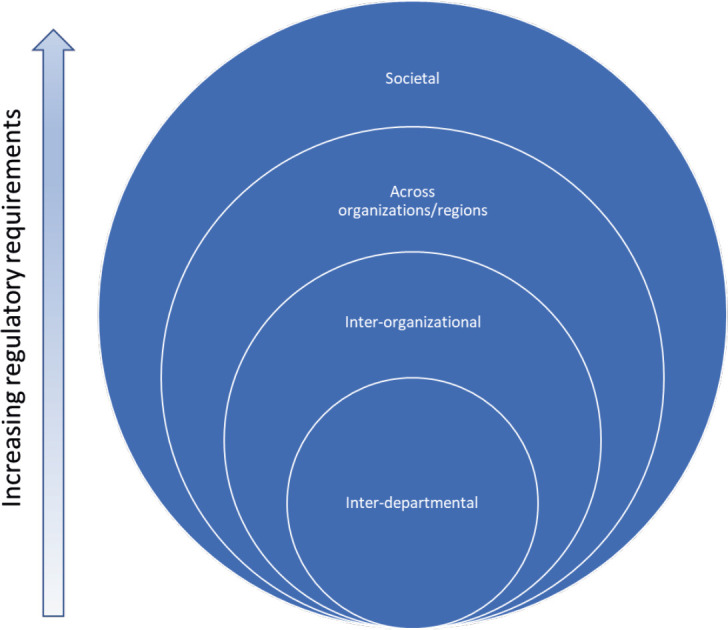
Ability to share data across domains, as a measure of digital health maturity. To reach digital health maturity, digital health infrastructure needs the following changes: (A) at the microlevel, consistent and pragmatic assessment strategies and tools for the many technologies currently implemented; (B) at the mesolevel, organisational interoperability needs to be strengthened, so that it can lead to population-level risk assessment strategies and (C) at the macrolevel, digital transformation policies that provide the political support needed to drive through the changes that will inevitable arise by the implementation of digital health infrastructures.
Building confidence in the use and security of the system
Developing secure processes for key elements including data gathering and use is an integral part of digital health infrastructure,54 while also accommodating specific needs, local innovation and evolvability,55 that is, a nuanced approach in the systems architecture while maintaining security requirements.
Recommendation 5: enable health and care organisations by providing the necessary technology to collect high-quality data in a timely way and promote sharing to create health intelligence
Rationale and evidence
Digital tools enable local and global health data gathering from a wide variety of consumer and medical devices as well as more traditional public health data sources like registries, claims data and health record data. However, ethics, privacy and security are paramount requirements that must be considered in the design of the tools and the services that they enable, such as predicting disease hotspots, planning of non-pharmaceutical interventions or vaccination scheduling.
Key requirements for implementation
Decentralised and heterogeneous health data acquisition and processing
Aggregated mobile device data enable tools that support public health decision making across the different stages of a pandemic.56 The combination of aggregate and privacy-protected mobility, health and city data through data fusion holds the promise of uncovering new insights for understanding epidemics57 58 and assisting in decision making across the different stages of a pandemic. Decentralised data processing and learning methods are important elements of the digital roadmap enabling multiscale predictions and discovery of insights. Emerging technologies and techniques, such as federated learning59 60 and differential privacy,61 can enable decentralised and privacy-aware learning over mobile devices and data registries.
Data sharing in the global environment
Sharing of aggregated and processed data and data-derived validated models is a crucial component in building regional, national and global understanding of the different stages of a pandemic. The combination of heterogeneous data sources, such as mobile phone data with social, health registry and clinical data, is critical for forecasting, planning and implementing mitigation strategies to reduce health risks.62 Use of these data sources requires trust and transparency across the healthcare ecosystem including citizens, industry and governments. Technologies that may advance the need for secure data aggregation and sharing include decentralised approaches like an internet-of-things healthcare blockchain. Scientific evaluation of technologies that enable data collection and sharing further supports trust in their use.
Ethics, privacy and security
Significant ethical issues arise in various stages when leveraging heterogeneous data sources to combat a pandemic.63 There is often tension between the need for highly detailed data and rich data with the need for individual privacy. State-of-the-art privacy solutions include data aggregation, data anonymisation and synthetic data generation techniques.64
Building trust
Scientific evaluation of technologies, methods and tools to demonstrate their value65 is essential to building trust in data sharing and aggregation.66 Rigorous evaluation of data with respect to its biases is needed to mitigate unethical use of data in applications.
Recommendation 6: cultivate a health and care workforce with the knowledge, skills and training in data and digital technologies required to address current and future public health challenges
Rationale and evidence
The rapid pace of change seen during the pandemic revealed gaps in the infrastructure, workforce skills and capabilities, and in digital education that need addressing. Developing digital leadership skills and improving the digital literacy of staff and patients have been identified as key steps in closing the digital gap in healthcare67 Pandemic response or not, health and care services lag behind other sectors in digitalisation by about a decade.68 69
Key requirements for implementation
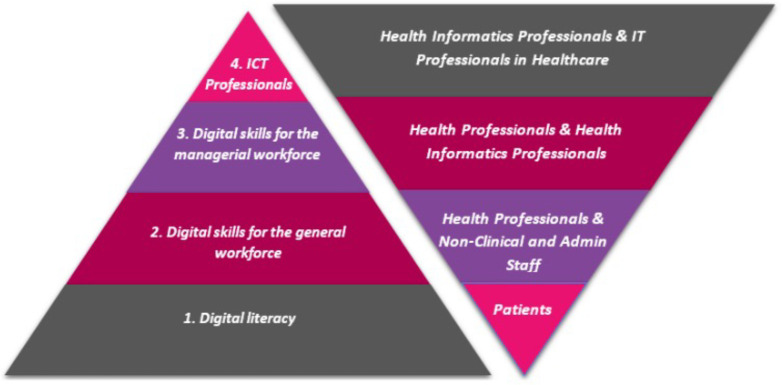
Taking time and effort to get to know the workforce and identifying knowledge and skills gaps and addressing them early on in any change process is key to securing the maximum benefit from any investment. To achieve success, it is important to understand the impact of digital transformation on the skills and capability needs of the current workforce. The level of digital proficiency required by staff in different types of jobs varies according to their role. Figure 2 provides a useful way of visualising the different digital skills and capability requirements for staff.
Figure 2.
Digital skills and capabilities spectrum versus breadth of required digital skills and capabilities per staff category in health and care. Level 1—Digital literacy (empowering individuals). Basic requirement of every citizen to become a fully ‘digitally literate’ member of society, for example, to use digital apps to communicate or engage with services, perform internet searches and being aware of cyber security matters. Level 2—Digital skills and capabilities for the general (health and care) workforce (an operational and practical skills category). Ability to use digital tools and perform digital functions in the workplace. Generally linked to using apps developed by ICT-specialists. While the digital skills required in the workplace are often context specific, there will be some minimum requirements linked to processing information that is applicable across all domains and levels of seniority. Level 3—Digital skills and capabilities for the (health and care) managerial workforce (doctors, nurses, consultants, managers, policy makers, decision makers, etc). Ability to manage digital applications and technologies and also understand them on a systems level in order to make informed decisions about issues related to digital infrastructures. These digital skills may only be relevant to designated senior staff, but again, there will be certain minimum requirements that are applicable across all areas of health and care. Level 4—Digital skills and capabilities for (health and care) ICT professionals (digitally innovative and creative individuals, organisations and businesses). Entails skills required in the IT sector, including skills linked with design and development of new digital technologies, products and services. Source: Rimpiläinen S et al.90 ICT, information and communications technology.
Ensure the education and training providers are up to date on what skills and capabilities the staff require. Developing technologies give rise to new types of occupations and reorder the types of skills and capabilities workforce needs to thrive in this new digital era.70 These changes also have an impact on the education providers. Sufficient continuing professional development provision should be on offer for educators to upskill and reskill to be able to teach relevant and up-to-date digital content and skills to their students. Furthermore, the education providers and industry should work closer together to cocreate meaningful curricula. All too often, ‘digital health’ is still provided as an optional module to future medical or health and care professionals, when it should be embedded in all the courses being taught. Engaging with the education providers in the relevant institutions to keep them updated on what the sector needs is an essential part of the digital transformation of the health and care services. By adopting these principals, it is possible to create a fertile environment that is not only receptive to considering transformational change but will embrace it.
Recommendation 7: ensure surveillance systems combine an effective public health response with respect for ethical and privacy principles
Rationale and evidence
An effective surveillance system for communicable diseases will require access to combinations of personal health data and location data, both of which are highly sensitive.1 To ensure privacy, data should ideally be anonymised by transforming the data to a form that cannot be linked to an identified or identifiable person.71 Unfortunately, this may be impossible without destroying the utility of the data. Data that are not anonymised are considered personal data and they must be managed with care.
Key requirements for implementation
Personal data can be anonymised by suitable aggregation into statistics over a larger population.71 Differential privacy provides a formal framework for proving statistical anonymity guarantees that formalise a trade-off between the degree of anonymity and data utility.72 The 2017 WHO guidelines73 outline ethical principles of surveillance, but only consider data collected in healthcare and public sources such as social media. Following these guidelines, a successful surveillance system will minimise processing and storage of personal data beyond what is necessary for their primary use. While surveillance systems are not considered to require user consent to be ethical,74 the data subjects should retain maximal level of control over the use of their personal data, especially if data collected by mobile devices or wearables are linked to their health data. Sufficient measures should be established to ensure the transparency of data processing to allow the data subjects to redefine their participation preferences.
Implementing a surveillance system that can react in a timely manner requires a global data sharing network for public health officials that supports automatic sharing of anonymised summaries as well as potentially sensitive more detailed queries according to predefined policies without human intervention. As location is important for the spread of communicable disease, an automated method for linking health data with personal location and activity data from mobile and wearable devices will be very useful. Such linking needs to be performed very carefully. In most cases, coarse locations (eg, at the city level) will be sufficient for surveillance purposes, and these are typically less sensitive than more precise data.75 Still, even city-level data can be identifiable when combining multiple locations and times,76 so user policies for personal data must be considered before their use.
Users should be able to define granular policies for the use of their personal data. These should enable specifying different privacy requirements (eg, level of anonymity or differential privacy) for different uses. Personal data should be processed in protected environments that make use of trusted computing to guarantee the data are only used for their intended purpose unless they are anonymised. To ensure transparency of data use, the data subjects should be able to follow how their data have been used and react to prevent repeating undesired uses in the future. As an additional safeguard, the system should make use of approaches such as federated learning77 to enable analysis of distributed data sets without collecting the data to a single database. Careful implementation of safeguards is important for establishing community trust on such systems.78 79
Recommendation 8: develop digital personal tools and services to support comprehensive health programs (in disease prevention, testing, management and vaccination) globally
Rationale and evidence
Recent advances in information technologies brought new opportunities for offering digital personal tools and services for disease prevention, testing, management and vaccination. Digital personal tools and services empower individuals to not only proactively engage in contact tracing,80 symptom tracking81 and vaccination,82 but also offer personal health data stores that can be accessible whenever needed for diverse purposes such as personalised care, self-reflection and data sharing for disease research.
Key requirements for implementation
First, contact tracing technologies can be categorised as people-centric or place-centric tracking.80 Wireless and location-sensing technologies such as Bluetooth, WiFi and GPS tracking are the key enablers. Second, information sharing infrastructure must be properly prepared to support interactive dashboards (disease status), contact tracing (hotspot information) and self-checking services. Timely data dissemination mandates provisioning a scalable cloud-computing infrastructure. Third, resource availability checking and resource scheduling systems (eg, for face masks, virus tests and vaccinations) should be properly supported. Fourth, mobile personal health record (mPHR) services can cover the entire process such as testing, hospitalisation and symptom tracking. Interoperability of EHRs from hospitals will increase the portability of personal health data. This includes the integration of personal health data collected from mobile and wearable devices. Fifth, mPHR can be extended to provide a basis for digital health passports that can certify a person’s proof of negative test results, vaccination or recovery from COVID-19. This requires digital accreditation systems that can be used across nations, for example, by using blockchain technologies.83
Practitioners should consider the following aspects for real-world implementation. Personal digital health tools and services must follow user-centred design principles with rapid and iterative system design.84 The design should involve various stakeholders; for example, for self-quarantine management, both end-users and local health authorities who manage them need including. Inclusive design should consider supporting alternative approaches. Old smartphones are often excluded from support, which may affect those of low socioeconomic status, necessitating either extended support for older models or employing technologies that are unlikely to become redundant, such as SMS text messaging. Non-users may not have access to digital health services due to a lack of digital literacy or their low socioeconomic status. Privacy by design needs be also considered owing to the breadth of data collection in mPHR services. Service fragmentation across multiple stakeholders, such as different government agencies and local authorities, needs coordination by offering a unified portal service or a single sign-on service for ease of access to multiple services.
Recommendation 9: maintain, continue to fund and innovate surveillance systems as a core component of the connected global health system for rapid preparedness and optimal global responses
Rationale and evidence
As cross-border mobility has grown and international and transcontinental flights are now regular, pandemics can now spread at unprecedented speeds. Many novel detection approaches are already in place, though more are needed. Even the COVID-19 pandemic was detected early by a surveillance approach called BlueDot, which goes through large quantities of information of various types including traveller information such as that from the International Air Transport Association to both detect infections and predict how they may spread.85 Early detection in the USA occurred in multiple ways, including through the Seattle Flu Study, which was performing surveillance for influenza but identified 25 cases of COVID-19 very early.86 Effective approaches for tracking COVID-19 were identified in China,87 one example being the Honghu Hybrid System, which had functions including syndromic surveillance on mobile devices, policy-making decision support, clinical decision support and follow-up tools.
Key requirements for implementation
Key requirements include access to a variety of datasets across international borders including both medical data and travel/traveller information in near real-time, as well as support for surveillance for and detection of novel viruses. Both transforming defences and enhancing situational awareness are pivotal.88
One essential enabler is central support from governments to support such evaluation over the long term. For this type of service to make a difference, it must be longitudinal. Ironically, the USA had stopped much of its standing support for pandemic preparedness shortly before the onset of COVID-19. Not surprisingly, this was one of many factors delaying the US response to this crisis. Some of this evaluation should be central, and some can be done by academic groups or private companies, but stable federal support is vital.
In terms of implementation, it will be essential to develop international consensus about what types of tracking are likely to be the most useful, and then to support the development, maintenance of and access to datasets which enable this type of tracking. Notably, access must be cross-border for this to be effective; many nations have been reluctant to make most of their data available to entities from other countries, but this is truly a global issue. By using approaches such as deidentification, it should be possible to make datasets available to qualified users from around the world. Other approaches which enable the use of data from remote sites but do not require it to move may also be attractive and should be explored.
Conclusions
The Riyadh Declaration on Digital Health, learning from the lived experiences of the COVID-19 pandemic, provided a set of recommendations on how and where digital health could help to address future pandemics and health threats. We now build on the declaration to provide a resource and toolkit for all digital health stakeholders to follow to develop digital health infrastructure and protocols at the local, national and supranational levels to prepare for future health threats.
While we have described many of the actions required for the digital transformation of health, we also recognise that such change must be fully supported with the necessary financial resources. In this regard, Transform Health, a global coalition of organisations, individuals, and institutions committed to achieving universal health coverage using digital technologies and data, recently estimated that an annual spend of US$2.5 billion will be required per year to support priority areas in digital health in low- and middle-income countries (LMICs) over the next 5 years. Given that this represents ~1% of the annual government health spending of LMICs, two-thirds of investment should be able to be met from national resources with the remainder coming from external support.89 Having established the problems, solutions and costs, the next step will be to reach a consensus on which areas to prioritise to achieve digital transformation in an equitable, inclusive and sustainable manner.
Footnotes
Handling editor: Soumitra S Bhuyan
Contributors: All authors contributed to the developing the content of the article, wrote sections of the manuscript, edited the manuscript and approved the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Al Knawy B, Adil M, Crooks G, et al. The riyadh declaration: the role of digital health in fighting pandemics. Lancet 2020;396:1537–9. 10.1016/S0140-6736(20)31978-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dinov ID. Methodological challenges and analytic opportunities for modeling and interpreting big healthcare data. Gigascience 2016;5:12. 10.1186/s13742-016-0117-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Janssen M. Situated novelty: A study on healthcare innovation and its governance. 2016.
- 4.Walker BF, Adukwu EC. The 2013-2016 Ebola epidemic: evaluating communication strategies between two affected countries in West Africa. Eur J Public Health 2020;30:118–24. 10.1093/eurpub/ckz104 [DOI] [PubMed] [Google Scholar]
- 5.Roozenbeek J, Schneider CR, Dryhurst S, et al. Susceptibility to misinformation about COVID-19 around the world. R Soc Open Sci 2020;7:201199. 10.1098/rsos.201199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyland-Wood B, Gardner J, Leask J, et al. Toward effective government communication strategies in the era of COVID-19. Humanit Soc Sci Commun 2021;8:1–11. 10.1057/s41599-020-00701-w [DOI] [Google Scholar]
- 7.Norheim OF, Abi-Rached JM, Bright LK, et al. Difficult trade-offs in response to COVID-19: the case for open and inclusive decision making. Nat Med 2021;27:10–3. 10.1038/s41591-020-01204-6 [DOI] [PubMed] [Google Scholar]
- 8.Kreps SE, Kriner DL. Model uncertainty, political contestation, and public trust in science: evidence from the COVID-19 pandemic. Sci Adv 2020;6:43. 10.1126/sciadv.abd4563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Australia GoE . COVID‐19: roadmap to recovery: a report for the nation. The Group of Eight Ltd, 2020. [Google Scholar]
- 10.Valiverronen E, Laaksonen S-M, Jauho M, et al. Liberalists and data-solutionists: redefining expertise in Twitter debates on coronavirus in Finland. JCOM 2020;19:A10. 10.22323/2.19050210 [DOI] [Google Scholar]
- 11.van Dijck J, Alinejad D. Social media and trust in scientific expertise: debating the covid-19 pandemic in the Netherlands. Social Media + Society 2020;6:205630512098105. 10.1177/2056305120981057 [DOI] [Google Scholar]
- 12.Bélanger ME, Lavenex S. Communicating mobility restrictions during the covid‐19 crisis on Twitter: the legitimacy challenge. Swiss Political Sci Review 2021;27:822–39. 10.1111/spsr.12494 [DOI] [Google Scholar]
- 13.Eliantonio M, Ştefan O. The elusive legitimacy of EU soft law: an analysis of consultation and participation in the process of adopting COVID-19 soft law in the EU. Eur J Risk Regul 2021;12:159–75. 10.1017/err.2020.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rainey S, Mormina M, Lignou S, et al. The post-normal challenges of COVID-19: constructing effective and legitimate responses. Sci Public Policy 2021;48:592–601. 10.1093/scipol/scab037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hoover AG, Heiger-Bernays W, Ojha S, et al. Balancing incomplete COVID-19 evidence and local priorities: risk communication and stakeholder engagement strategies for school re-opening. Rev Environ Health 2021;36:27–37. 10.1515/reveh-2020-0092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng H, Jiang S, Wu Q. Factors influencing COVID-19 vaccination intention: the roles of vaccine knowledge, vaccine risk perception, and doctor-patient communication. Patient Educ Couns 2022;105:277–83. 10.1016/j.pec.2021.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bavel JJV, Baicker K, Boggio PS, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav 2020;4:460–71. 10.1038/s41562-020-0884-z [DOI] [PubMed] [Google Scholar]
- 18.Ahern S, Loh E. Leadership during the COVID-19 pandemic: building and sustaining trust in times of uncertainty. Leader 2021;5:266–9. 10.1136/leader-2020-000271 [DOI] [Google Scholar]
- 19.AlKnawy B. Leadership in times of crisis. Leader 2019;3:1–5. 10.1136/leader-2018-000100 [DOI] [Google Scholar]
- 20.Iacobucci G. Vaccination: “fake news” on social media may be harming UK uptake, report warns. BMJ 2019;364:l365. 10.1136/bmj.l365 [DOI] [PubMed] [Google Scholar]
- 21.Love JS, Blumenberg A, Horowitz Z. The parallel pandemic: medical misinformation and COVID-19: primum non nocere. J Gen Intern Med 2020;35:2435–6. 10.1007/s11606-020-05897-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soltaninejad K. Methanol mass poisoning outbreak: a consequence of COVID-19 pandemic and misleading messages on social media. Int J Occup Environ Med 2020;11:148–50. 10.34172/ijoem.2020.1983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eysenbach G, Diepgen T, Lampe K, et al. EU-project medcertain: certification and rating of trustworthy and assessed health information on the net. Medical Infobahn for Europe 2000:279–83. 10.3233/978-1-60750-921-9-279 [DOI] [PubMed] [Google Scholar]
- 24.Tam J, Porter EK, Lee UJ. Examination of information and misinformation about urinary tract infections on tiktok and youtube. Urology 2022;168:35–40. 10.1016/j.urology.2022.06.030 [DOI] [PubMed] [Google Scholar]
- 25.Fernández-Luque L, Bau T. Health and social media: perfect storm of information. Healthc Inform Res 2015;21:67–73. 10.4258/hir.2015.21.2.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanekar AS, Thombre A. Fake medical news: avoiding pitfalls and perils. Fam Med Community Health 2019;7:e000142. 10.1136/fmch-2019-000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eysenbach G. How to fight an infodemic: the four pillars of infodemic management. J Med Internet Res 2020;22:e21820. 10.2196/21820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barros JM, Duggan J, Rebholz-Schuhmann D. The application of Internet-based sources for public health surveillance (infoveillance): systematic review. J Med Internet Res 2020;22:e13680. 10.2196/13680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Cock Buning M M. A multi-dimensional approach to disinformation: report of the independent high level group on fake news and online disinformation. Publications Office of the European Union, 2018. [Google Scholar]
- 30.Yang A, Shin J, Zhou A, et al. The battleground of COVID-19 vaccine misinformation on Facebook: fact checkers vs. misinformation spreaders. HKS Misinfo Review August 30, 2021. 10.37016/mr-2020-78 [DOI] [Google Scholar]
- 31.Bin Naeem S, Kamel Boulos MN. COVID-19 misinformation online and health literacy: a brief overview. Int J Environ Res Public Health 2021;18:15. 10.3390/ijerph18158091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miotto R, Wang F, Wang S, et al. Deep learning for healthcare: review, opportunities and challenges. Brief Bioinform 2018;19:1236–46. 10.1093/bib/bbx044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abrams EM, Szefler SJ. COVID-19 and the impact of social determinants of health. Lancet Respir Med 2020;8:659–61. 10.1016/S2213-2600(20)30234-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.HL7 FHIR . An agile and restful approach to healthcare information exchange. Proceedings of the 26th IEEE international symposium on computer-based medical systems; 2013; IEEE, [Google Scholar]
- 35.Saripalle RK. Fast health interoperability resources (FHIR): current status in the healthcare system. International Journal of E-Health and Medical Communications (IJEHMC) 2019;10:76–93. [Google Scholar]
- 36.World Health Organization . Fifty-eighth world health assembly: resolutions and decisions. In: Fifty-eighth world health assembly, geneva, 16-25 may 2005: resolutions and decisions, annex. Geneva, [Google Scholar]
- 37.World Health Organization . Draft global strategy on digital health 2020–2024. World Health Organization, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jazieh AR, Kozlakidis Z. Healthcare transformation in the post-coronavirus pandemic era. Front Med (Lausanne) 2020;7:429. 10.3389/fmed.2020.00429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ohannessian R, Duong TA, Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill 2020;6:e18810. 10.2196/18810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc 2020;27:853–9. 10.1093/jamia/ocaa037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pérez Sust P, Solans O, Fajardo JC, et al. Turning the crisis into an opportunity: digital health strategies deployed during the COVID-19 outbreak. JMIR Public Health Surveill 2020;6:e19106. 10.2196/19106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kolasa K, Kozinski G. How to value digital health interventions? A systematic literature review. Int J Environ Res Public Health 2020;17:2119. 10.3390/ijerph17062119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dalal AK, Piniella N, Fuller TE, et al. Evaluation of electronic health record-integrated digital health tools to engage hospitalized patients in discharge preparation. J Am Med Inform Assoc 2021;28:704–12. 10.1093/jamia/ocaa321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Milinovich A, Kattan MW. Extracting and utilizing electronic health data from EPIC for research. Ann Transl Med 2018;6:42. 10.21037/atm.2018.01.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.World Health Organization . Digital health platform handbook: building a digital information infrastructure (infostructure) for health. 2020.
- 46.Eklund N, Andrianarisoa NH, van Enckevort E, et al. Extending the minimum information about Biobank data sharing terminology to describe samples, sample donors, and events. Biopreserv Biobank 2020;18:155–64. 10.1089/bio.2019.0129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marshall JC, Murthy S, Diaz J. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis 2020;20:e192–7. 10.1016/S1473-3099(20)30483-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Group EMTMDSW . Minimum data set for reporting by emergency medical teams. World Health Organization, 2017. [Google Scholar]
- 49.Ibrahim NK. Epidemiologic surveillance for controlling covid-19 pandemic: types, challenges and implications. J Infect Public Health 2020;13:1630–8. 10.1016/j.jiph.2020.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Davidson JA, Anderson LF, Adebisi V, et al. Creating a web-based electronic tool to aid tuberculosis (TB) cluster investigation: data integration in TB surveillance activities in the united kingdom, 2013 to 2016. Euro Surveill 2018;23:44. 10.2807/1560-7917.ES.2018.23.44.1700794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abdolkhani R, Gray K, Borda A, et al. Patient-generated health data management and quality challenges in remote patient monitoring. JAMIA Open 2019;2:471–8. 10.1093/jamiaopen/ooz036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dash S, Shakyawar SK, Sharma M, et al. Big data in healthcare: management, analysis and future prospects. J Big Data 2019;6:1–25. 10.1186/s40537-019-0217-0 [DOI] [Google Scholar]
- 53.Lavallee DC, Lee JR, Austin E, et al. Mhealth and patient generated health data: stakeholder perspectives on opportunities and barriers for transforming healthcare. Mhealth 2020;6:8. 10.21037/mhealth.2019.09.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kulynych J, Greely HT. Clinical genomics, big data, and electronic medical records: reconciling patient rights with research when privacy and science collide. J Law Biosci 2017;4:94–132. 10.1093/jlb/lsw061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hathaliya JJ, Tanwar S. An exhaustive survey on security and privacy issues in healthcare 4.0. Computer Communications 2020;153:311–35. 10.1016/j.comcom.2020.02.018 [DOI] [Google Scholar]
- 56.Oliver N, Lepri B, Sterly H, et al. Mobile phone data for informing public health actions across the covid-19 pandemic life cycle. Sci Adv 2020;6:eabc0764. 10.1126/sciadv.abc0764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cori A, Donnelly CA, Dorigatti I, et al. Key data for outbreak evaluation: building on the ebola experience. Philos Trans R Soc Lond B Biol Sci 2017;372:1721. 10.1098/rstb.2016.0371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Drew DA, Nguyen LH, Steves CJ, et al. Rapid implementation of mobile technology for real-time epidemiology of COVID-19. Science 2020;368:1362–7. 10.1126/science.abc0473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rieke N, Hancox J, Li W, et al. The future of digital health with federated learning. NPJ Digit Med 2020;3:119. 10.1038/s41746-020-00323-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vaid A, Jaladanki SK, Xu J, et al. Federated learning of electronic health records to improve mortality prediction in hospitalized patients with COVID-19: machine learning approach. JMIR Med Inform 2021;9:e24207. 10.2196/24207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Differential privacy: A survey of results . International conference on theory and applications of models of computation; Springer, 2008 [Google Scholar]
- 62.Weissman GE, Crane-Droesch A, Chivers C, et al. Locally informed simulation to predict Hospital capacity needs during the COVID-19 pandemic. Ann Intern Med 2020;173:680–1. 10.7326/L20-1062 [DOI] [PubMed] [Google Scholar]
- 63.Athey S. Beyond prediction: using big data for policy problems. Science 2017;355:483–5. 10.1126/science.aal4321 [DOI] [PubMed] [Google Scholar]
- 64.Goncalves A, Ray P, Soper B, et al. Generation and evaluation of synthetic patient data. BMC Med Res Methodol 2020;20:108. 10.1186/s12874-020-00977-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wynants L, Van Calster B, Collins GS, et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ 2020;369:m1328. 10.1136/bmj.m1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Park Y, Jackson GP, Foreman MA, et al. Evaluating artificial intelligence in medicine: phases of clinical research. JAMIA Open 2020;3:326–31. 10.1093/jamiaopen/ooaa033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Taylor K, Properzi F. Closing the digital gap: shaping the future of UK healthcare. united kingdom, deloitte centre for health services. 2019: 62. [Google Scholar]
- 68.Imison C, Castle-Clarke S, Watson R, et al. Delivering the benefits of digital health care: 2016. [Google Scholar]
- 69.Landi H. Study: healthcare lags other industries in digital transformation, customer engagement tech. healthcare informatics. Available: https://wwwhealthcare-informaticscom/news-item/patientengagement/study-healthcare-lags-other-industries-digital-transformationcustomer [Accessed 20 Jun 2018].
- 70.Rimpiläinen S, Morrison C, Nielsen SL, et al. Spotlight on careers in digital health and care: addressing future workforce development needs in digital health and care. 2019. [Google Scholar]
- 71.Graham C. Anonymisation: managing data protection risk code of practice. Information Commissioner’s Office, 2012. [Google Scholar]
- 72.Calibrating noise to sensitivity in private data analysis . Theory of cryptography conference. Springer, 2006. [Google Scholar]
- 73.Fairchild AL, Haghdoost AA, Bayer R, et al. Ethics of public health surveillance: new guidelines. Lancet Public Health 2017;2:e348–9. 10.1016/S2468-2667(17)30136-6 [DOI] [PubMed] [Google Scholar]
- 74.Lee LM, Heilig CM, White A. Ethical justification for conducting public health surveillance without patient consent. Am J Public Health 2012;102:38–44. 10.2105/AJPH.2011.300297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Geo-indistinguishability . Differential privacy for location-based systems. Proceedings of the 2013 ACM SIGSAC conference on Computer & communications security; 2013 [Google Scholar]
- 76.de Montjoye Y-A, Hidalgo CA, Verleysen M, et al. Unique in the crowd: the privacy bounds of human mobility. Sci Rep 2013;3:1376. 10.1038/srep01376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kairouz P, McMahan HB, Avent B. Advances and open problems in federated learning foundations and trends® in machine learning. 2021: 1–210. 10.1561/9781680837896 [DOI] [Google Scholar]
- 78.Degeling C, Carter SM, van Oijen AM, et al. Community perspectives on the benefits and risks of technologically enhanced communicable disease surveillance systems: a report on four community juries. BMC Med Ethics 2020;21:31. 10.1186/s12910-020-00474-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Degeling C, Chen G, Gilbert GL, et al. Changes in public preferences for technologically enhanced surveillance following the COVID-19 pandemic: a discrete choice experiment. BMJ Open 2020;10:e041592. 10.1136/bmjopen-2020-041592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lee U, Kim A. Benefits of mobile contact tracing on COVID-19: tracing capacity perspectives. Front Public Health 2021;9:586615. 10.3389/fpubh.2021.586615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 2020;5:e475–83. 10.1016/S2468-2667(20)30164-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Malik AA, McFadden SM, Elharake J, et al. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020;26:100495. 10.1016/j.eclinm.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Angelopoulos CM, Damianou A, Katos V. n.d. DHP framework: digital health passports using blockchain--use case on international tourism during the COVID-19 pandemic. ArXiv Preprint:arXiv:200508922 2020. 10.48550/arXiv.2005.08922 [DOI] [Google Scholar]
- 84.Schnall R, Rojas M, Bakken S, et al. A user-centered model for designing consumer mobile health (mhealth) applications (apps). J Biomed Inform 2016;60:243–51. 10.1016/j.jbi.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bogoch II, Watts A, Thomas-Bachli A, et al. Potential for global spread of a novel coronavirus from China. J Travel Med 2020;27:taaa011. 10.1093/jtm/taaa011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chu HY, Englund JA, Starita LM, et al. Early detection of covid-19 through a citywide pandemic surveillance platform. N Engl J Med 2020;383:185–7. 10.1056/NEJMc2008646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gong M, Liu L, Sun X, et al. Cloud-Based system for effective surveillance and control of COVID-19: useful experiences from hubei, China. J Med Internet Res 2020;22:e18948. 10.2196/18948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lander E, Sullivan J. American pandemic prepardness: transforming our capabilities. Washington, DC, USA: The White House, 2021. [Google Scholar]
- 89.Health T. Closing the divide: more and better funding for digital health 2022. Available: https://www.ictworks.org/wp-content/uploads/2022/12/Funding-Digital-Transformation-Health.pdf [Accessed 30 Jan 2023].
- 90.Rimpiläinen S, Morrison C, Rooney L. Review and analysis of the digital health sector and skills for scotland: digital health and care institute. Glasgow: University of Strathclyde, [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are available.