Abstract
Disparities in cancer research persist around the world. This is especially true in global health research, where high-income countries (HICs) continue to set global health priorities further creating several imbalances in how research is conducted in low and middle-income countries (LMICs). Cancer research disparities in Africa can be attributed to a vicious cycle of challenges in the research ecosystem ranging from who funds research, where research is conducted, who conducts it, what type of research is conducted and where and how it is disseminated. For example, the funding chasm between HICs and LMICs contributes to inequities and parachutism in cancer research. Breaking the current cancer research model necessitates a thorough examination of why current practices and norms exist and the identification of actionable ways to improve them. The cancer research agenda in Africa should be appropriate for the African nations and continent. Empowering African researchers and ensuring local autonomy are two critical steps in moving cancer research towards this new paradigm.
Keywords: Health policies and all other topics, Health policy, Health services research, Cancer, Review
Summary box.
Cancer research disparities in Africa have been the topic of many publications.
However, most are siloed to one particular issue of the cancer research ecosystem.
This study highlights a vicious cycle of disparities that contribute to the current state of cancer research in Africa.
Recommendations suggested in this study can be used as a roadmap for African researchers and policy makers to train, fund and shape the national cancer research agenda.
Background
Global health is a field riddled with disparities in clinical care, funding opportunities and research. In many cases, global health priorities continue to be set by high-income countries (HIC), while the Global South continues to bear the most significant burden of disease. This reality will be further accentuated in the coming years amidst the anticipated health pressures from climate change.1 The disproportionate burden of illness has transitioned from the historic paradigm of communicable diseases to non-communicable diseases (NCD).2 Additionally, this transition is readily apparent in the rapid rise of cancer in low and middle-income countries (LMICs), including those in sub-Saharan Africa (SSA).3
By 2040, it is estimated that there will be nearly 30 million new cancer diagnoses and over 16 million cancer-related deaths annually in LMICs.4 5 Despite this high cancer burden in LMICs, less than 4% of the total global annual cancer research output as measured by publications is coauthored by individuals from these countries.6 Further, low-income countries, most of which are from Africa, have the lowest proportion of corresponding authors.7 8 Africa is home to 15% of the global population; however, it shoulders a quarter of the global disease burden and produces only 2% of the world’s research output.6 9
The global oncology research pendulum continues to be extraordinarily imbalanced, with near-total domination by the Global North.10 One of these imbalances—the continued lack of African representation in research done in Africa—is arguably unethical and linked with epistemic wrongs and injustices. This imbalance has been characterised by the non-collaborative style of research activities involving some researchers predominantly from HICs, who fly in and out of LMICs for short periods of time.11 While these researchers will receive access to local African research data, they often publish these data without acknowledging or sharing authorship with local investigators, this perpetuates the ongoing under-representation of African scientists in global health.12 13 Under-representation of African researchers and authorship parachutism are not uncommon problems in global health, but few have described this phenomenon as it relates to cancer research in Africa.13 14
A recent review of global oncology publications found that among studies done in and about SSA, African investigators were the first and last authors in only 45% and 41% of publications, respectively.15 This was further confirmed by a comparative bibliometric analysis of cancer research across Africa over a 12-year period (2009–2020), which found that for a total of 5303 papers from SSA, African researchers were likely to be the first author in only 42% and the last author in 30%.16 As evidenced by these two reviews, the lack of research leadership among African researchers spans all research types from clinical trials to observational studies—majority of the studies in these reports are observational. Additionally, there is clear evidence of major imbalances in global cancer research priorities. A review of contemporary clinical trials that enrolled patients from LMICs showed that only 8% of all oncology randomised clinical trials are led by investigators in LMICs, highlighting a strong mismatch between the global burden of diseases and global cancer research leadership. This is important to note given the fact that studies enrolling in LMICs tend to identify large benefits for patients.17 18 Africa cancer research priorities are parallel to those of funding agencies in high-income Western nations, lacking palliative care, implementation science and qualitative research domains which are relevant to African context.16 Some types of cancer, such as oesophageal cancer, cervix, prostate and liver cancers, which are common in Africa, are underfunded and understudied in Africa.16
Cancer research parachutism in LMICs has presented itself in various ways. Most frequently, it manifests as unequal authorship distribution.11 14 19 Second, an often unacknowledged ethical problem is the lack of post-trial access to study drugs and products for local study participants.15 20 21 The Helsinki Declaration mandates trial investigators continue to supply beneficial study drugs to study participants after the trial conclusion.20 However, there are no systems in place to ensure that this enduring access to beneficial treatments is granted to study participants in LMICs.18
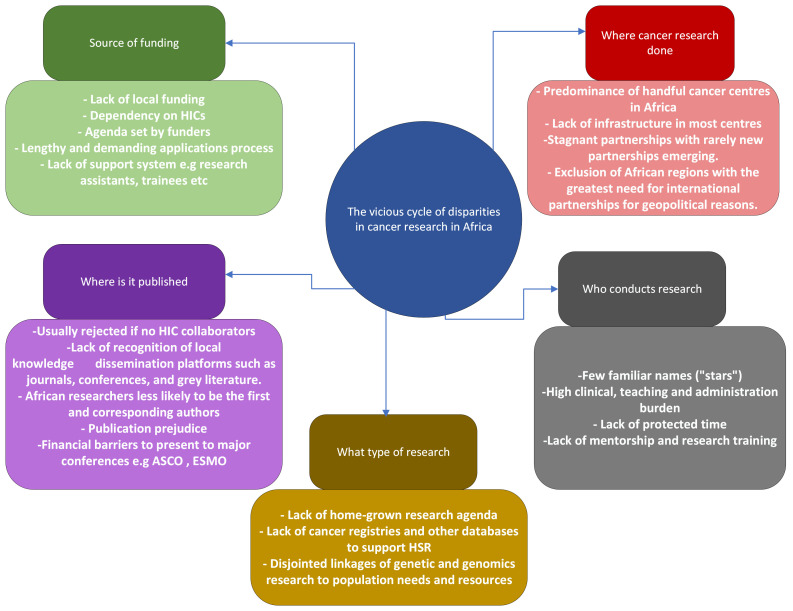
Current disparities in cancer research in Africa can be attributed to a vicious cycle of challenges in the research ecosystem (figure 1). It is therefore critical that the under-representation of African cancer researchers is not viewed in isolation but is rather understood as part of a broader issue of global research disparities. To address this imbalance in cancer research, we describe the current cancer research ecosystem and highlight disparities related to research funding, where research is done, who does it, what type of research is performed, as well as where and how results are disseminated. We also attempt to provide high-level solutions to address these striking disparities.
Figure 1.
The vicious cycle of disparities in Africa’s cancer research ecosystem. ASCO, American Society of Clinical Oncology; HIC, high-income country; ESMO, European Society for Medical Oncology; HSR, Health Service Research.
Source of cancer research funding in Africa
In 2007, African Union (AU) member states committed to investing at least 1% of their gross domestic product in research and development.22 Fifteen years later, no country has achieved this goal.23 Lack of internal funding poses a significant barrier for African countries looking to invest in cancer, especially when faced with a plethora of competing priorities in the health sector and beyond. Given these limitations, African researchers are forced to turn to international funding agencies.24 Accordingly, international funding bodies hold enormous autonomy and power in setting global cancer research priorities. Most cancer research funding agencies and governments are located in HICs, despite funding programmes that are designed for African settings.25 To access these funds, Africa-based researchers must submit lengthy applications which align with the demands and priorities of the funding body rather than those of the local population. Some applications may also stipulate that African researchers collaborate with researchers from HICs to be eligible for funding. The funding chasm between HICs and LMICs contributes to inequities and parachutism in cancer research.26 27
Moreover, the burdensome nature of the lengthy and complex funding applications presented by these bodies poses significant challenges for African researchers. These researchers are already overwhelmed with clinical work, teaching and administrative duties, and lack the preaward administrative support that is often available to HIC-based investigators. This gives an upper hand to Global North applicants, who frequently have access to research assistants, graduate students and support staff that facilitate the execution of grant applications. This perpetuates the trend of institutions based in HICs receiving funding for work in Africa, some without the inclusion of any African researchers, as has been seen in the financing of malaria initiatives.28 Even when African malaria researchers are included, the majority of funding goes to institutions in the funding countries, leaving only about 1% of funding for local LMIC institutions.28 Our experience with collaborative grants for cancer research demonstrates that, due to their low base salaries, African researchers are always compensated less for their full-time equivalent on collaborative research grants. When international funding bodies based in HICs do collaborate with African researchers, it is often a quasipartnership, given the inherent power imbalance created by the funding source.13 Thus, to access funding and establish a seat at the metaphorical table, African researchers are left to seek out often inequitable collaborations with HIC researchers and institutions, further exacerbating the trends of power imbalance and research parachutism.29
Another barrier relates to the fact that most international funding agencies implicitly, and occasionally explicitly, require a demonstration of prior publications or prior partnerships. This practice places many African researchers at significant disadvantages, particularly if their countries are not considered as ‘favourable’ within the ranking scale of partnerships with HICs.
National funding is mandatory for successful and sustainable cancer research in Africa as it addresses local needs and priorities and facilitates autonomy for local experts. International grants may help advance certain projects, but complete dependence ultimately erodes the local relevance of the African cancer research agenda.27 African governments, cancer societies, organisations and local academic institutions should aim to develop competitive grants and fellowship schemes administered by African institutions. There are several African-based initiatives to fund African research agenda; these include the AU member states’ pledge of allocating 1% of national budget to research, creation of African centre for disease control, the signed memorandum of understanding between the American Society of Clinical Oncology and the African Organization for Research and Training in Cancer and the recent signed agreement between the US and African leaders to fund cancer research.22 30–32 In addition, local ethics committees should develop frameworks which require sponsors and research collaborators from HICs to incorporate local authors and researchers before the research is approved.
Where in Africa is cancer research done?
A recent bibliometric analysis of cancer research across Africa showed that SSA contributes only 22% (5281/23 679 papers), of which 42% is from South Africa.16 Together, South Africa and Egypt contribute 62% of cancer research papers from Africa.16 As most research from Africa is a result of north–south collaboration, researchers from HICs tend to prioritise collaborations with countries and hospitals where there is a large patient population or where they have previously conducted research.33 However, the conduct of research at such centres may put a greater burden on the clinicians whose capacity for research is already limited due to existing research projects and overwhelming clinical duties. Additionally, if these collaborations are successful, there is a risk of continued support to these few centres only with limited expansion of collaborative research with other new centres. Conversely, new research partnerships between HICs and other institutions with smaller patient populations are often hindered by a lack of expertise or may have competing priorities or inadequate infrastructure for high-quality cancer research.34 35 Therefore, the result is a system in which an exclusive group of institutions receive a disproportionate number of resources and opportunities, perpetuating inequity.
As many African countries have made significant strides in controlling infectious diseases, there may be an opportunity for them to leverage the skills, and infrastructure towards NCDs including cancer.36 To facilitate this change, African governments and partners must prioritise cancer research. As well, funding bodies should attempt to broaden the network of beneficiaries in Africa. Finally, investing in the education and training of African researchers is critical to generate a more diverse pool of African cancer researchers and ensuring that research expertise is not centralised in a few cancer centres.
Who conducts research in Africa?
Challenges to conducting research in Africa continue to exist. There is very little emphasis on research in undergraduate, postgraduate medical and nursing education, and hardly any clinician-investigator programmes. The resultant lack of research exposure and mentorship leads most clinicians to focus mainly on clinical, administrative and education duties with nominal time devoted to research—if any.37 Full-time clinicians are overburdened with high clinical and teaching workloads, coupled with the realities of unprotected research time and low salaries.38 Despite these significant limitations, African ‘stars’ in cancer research have emerged over time. These impressive clinicians have garnered significant global attention, increasing their likelihood of receiving funding, promotions and authorship opportunities. While their acclaim is well deserved, the pool of African ‘stars’ remains limited, with researchers from HICs turning to the same few Africans over and over again for collaborations. This approach puts an immense burden on the shoulders of a narrow few and reduces opportunities for others to achieve similar achievements in cancer research.
One strategy to address this challenge is to invest in the mentorship and training of early-career researchers in Africa. To do this, urgent and concerted efforts are needed to identify trainees interested in cancer research at an early stage and create attractive cancer research-focused career pathways. These can start at a junior level during medical training and extend to master’s, PhD and postdoctoral levels. Funding for these scholars can be secured from local governments or philanthropic efforts to ensure retention and job security while avoiding potential poaching from international institutions in HICs. To protect this research pipeline, clinicians who wish to conduct research must be supported through the provision of protected time. Unlike their counterparts in HICs, securing local or international grants often does not translate into protected time for African oncologists. Policies need to be formulated and implemented to address this inequity by local and international funding bodies.
African researchers need access to opportunities to strengthen their research skills. Higher learning institutions, professional bodies and societies should avail learning opportunities such as research methods workshops similar to the Collaboration for Research Methods Development in Oncology course offered by the Tata Memorial Centre (Mumbai, India) and clinical research mentorship programme for radiation oncology residents in Africa organised by Princes Margaret Cancer Centre (Toronto, Canada).39 40
Type of cancer research
While HICs pursue moonshot initiatives, LMICs are still struggling to implement basic evidence-based medicine.41–44 Interventions that are funded in HICs are often related to high-tech, high-cost innovations, including those related to precision medicine and genetic counselling.45
To address this profound gap in cancer research and care, Pramesh et al highlight that cancer research in LMICs should focus on reducing the burden of patients presenting with late-stage cancer, improving access to cancer treatments including surgery, chemotherapy and radiotherapy, and integrating value-based cancer care.46 This can be achieved through supporting initiatives such as Choosing Wisely, which advocates for value-based cancer care, advancing the implementation of science and quality improvement research and leveraging technology to improve cancer treatment outcomes and clinical trials conducted in Africa.47 It is important to prioritise health system strengthening and health services research, as this will be the basis for improving cancer outcomes.48 This can be achieved through concerted and deliberate efforts to establish an African cancer research agenda that is developed for Africa by Africans.
Cancer research dissemination
African researchers are robustly engaged in local conferences and social platforms, and produce important work in grey literature and local journals that are largely not indexed in major databases.49 Despite these important contributions, a documented publication bias against studies from LMICs, including those in Africa,17 has limited African researchers from being published in high-impact journals based in HICs. Rather than integrating global health/oncology as a mainstay feature, many high-impact factor journals have created sister journals dedicated to these topics, and most articles from African researchers can be found in these lower impact affiliate journals.17 When African researchers are published in high-impact journals, it is rarely the first author, as this position is commonly reserved for a ‘renowned’ collaborating author from an HIC.15 Additionally, a large number of researchers from Africa who are unfunded by HIC-based funding agencies will not be able to attend the major oncology conferences where researchers have opportunities to publish, network and establish collaborations. Costs associated with travel, registration and accommodation, as well as logistical challenges related to visa approval, make participation in these large events difficult for researchers in Africa.50
Models of funding, training, publication and infrastructure should therefore be developed to stimulate and support research in Africa. There is an unmet need to have dedicated cancer journals which empower LMICs and compete with existing high-impact journals. Given the existing power differentials in global oncology, structured reflexivity tools such as transparency matrices that situate every person involved in a collaborative research project should be filled by each author and attached to manuscripts submitted for publication.51 52
Conclusion
Dismantling the current model of cancer research requires a complete interrogation of the current practices and norms and identifying tangible strategies for improvement. This approach should proceed with consideration of the importance of lived experiences and local interpretive tools, and with an inclusive approach that values the voices of those who have historically been disadvantaged due to economic status, gender or other minority identities.
In this effort, a critical look at the current limitations to executing cancer research projects in Africa is also required. These include the timelines set by HICs, pitted against the limited local resources, intense workload, lack of training and limited research infrastructure available. Western eligibility criteria for research grants must also be examined more closely. For example, prioritising publication records without looking at local experience and knowledge puts African researchers at a disadvantage due to the lack of established research career development pathways in most African settings. If we are to truly work towards a decolonised global cancer research agenda, new tools and approaches must be embraced to decolonise academic publishing in global oncology, including the implementation of structured reflexivity statements and the transparency matrix.51 52 This paradigm shift will require a collaborative global effort in pursuit of a more equitable and locally empowered vision of cancer research in Africa.
Though disparities in cancer research are severe and of great concern, numerous strategies can and should be implemented to achieve a more equitable vision of global cancer research (table 1). Empowering African researchers and ensuring local autonomy are two critical steps in the move towards this new paradigm in cancer research.
Table 1.
Actionable steps to reduce cancer research disparities in Africa
| 1 | African governments, cancer societies, organisations and local academic institutions should develop and administer competitive grants and fellowship schemes. |
| 2 | Local ethics committees to develop a framework which will obligate research sponsors and partners from HICs to incorporate local researchers in the design, conduct and dissemination of research findings. |
| 3 | African countries to establish and scale up cancer research centres of excellence. |
| 4 | Investing in the education, training and mentorship of early-career African researchers to generate a more diverse pool of African cancer researchers. |
| 5 | Produce incentives to retain competent clinicians and medical educators who wish to conduct research. This can be through the provision of protected time and offered training opportunities to strengthen their professional skills. |
| 6 | Concerted and deliberate efforts to establish an African cancer research agenda that is developed by Africa and led by adequately equipped and funded African scholars, clinicians and researchers. |
| 7 | Prioritise local journals for the dissemination of Africa-based research. |
| 8 | Adopt new tools for decolonising academic publishing in cancer research such as transparency matrix and structured reflexivity statement. |
| 9 | African research institutions should make sure to promote gender equality and equity in the conduct of cancer research for both participants and researchers. |
| 10 | Strengthening and encouraging South–South collaborations to address common challenges and increase capacity especially in countries traditionally excluded from international attention. |
HICs, high-income countries.
bmjgh-2022-011338supp001.pdf (20.2KB, pdf)
Footnotes
Handling editor: Seye Abimbola
Twitter: @rubagumyaf, @ChemtaiMungo
Contributors: FR and NH conceptualised the article. FR drafted the first draft with input from LC. All other authors provided inputs and comments on the last two final drafts. FR incorporated all coauthors’ comments and inputs. All authors approved the final version of the manuscript before submission. FR is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Author note: The reflexivity statement for this paper is linked as an online supplemental file 1.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Mordecai EA, Ryan SJ, Caldwell JM, et al. Climate change could shift disease burden from malaria to arboviruses in Africa. Lancet Planet Health 2020;4:e416–23. 10.1016/S2542-5196(20)30178-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fenollar F, Mediannikov O. Emerging infectious diseases in Africa in the 21st century. New Microbes New Infect 2018;26:S10–8. 10.1016/j.nmni.2018.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dalal S, Beunza JJ, Volmink J, et al. Non-communicable diseases in sub-saharan Africa: what we know now. Int J Epidemiol 2011;40:885–901. 10.1093/ije/dyr050 [DOI] [PubMed] [Google Scholar]
- 4.Shah SC, Kayamba V, Peek RM, et al. Cancer control in low- and middle-income countries: is it time to consider screening? J Glob Oncol 2019;5:1–8. 10.1200/JGO.18.00200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Global Cancer Observatory . Cancer (IARC)TIA for R. 2022. Available: https://gco.iarc.fr/
- 6.Anyangwe SCE, Mtonga C. Inequities in the global health workforce: the greatest impediment to health in sub-Saharan Africa. Int J Environ Res Public Health 2007;4:93–100. 10.3390/ijerph2007040002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mukherji D, Murillo RH, Van Hemelrijck M, et al. Global cancer research in the post-pandemic world. Lancet Oncol 2021;22:1652–4. 10.1016/S1470-2045(21)00602-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourlon MT, Jiménez Franco B, Castro-Alonso FJ, et al. Global oncology authorship and readership patterns. JCO Glob Oncol 2022;8:e2100299. 10.1200/GO.21.00299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schemm Y. Africa doubles research output over past decade, moves towards a knowledge-based economy. 2013: 3.
- 10.Van Hemelrijck M, Lewison G, Fox L, et al. Global cancer research in the era of COVID-19: a bibliometric analysis. Ecancermedicalscience 2021;15:1264. 10.3332/ecancer.2021.1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.University MJB l Njala . We need to end “parachute” research which sidelines the work of African scientists [Quartz]. 2019. Available: https://qz.com/africa/1536355/african-scientists-are-sidelined-by-parachute-research-teams/
- 12.Smith J. Parasitic and parachute research in global health. Lancet Glob Health 2018;6:e838. 10.1016/S2214-109X(18)30315-2 [DOI] [PubMed] [Google Scholar]
- 13.Smith E, Hunt M, Master Z. Authorship ethics in global health research partnerships between researchers from low or middle income countries and high income countries. BMC Med Ethics 2014;15:42. 10.1186/1472-6939-15-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheel M, Kirk MD. Parasitic and parachute research in global health. Lancet Glob Health 2018;6:e839. 10.1016/S2214-109X(18)30310-3 [DOI] [PubMed] [Google Scholar]
- 15.Tuyishime H, Hornstein P, Lasebikan N, et al. Authorship distribution and under-representation of sub-Saharan African authors in global oncology publications. JCO Glob Oncol 2022;8:e2200020. 10.1200/GO.22.00020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mutebi M, Lewison G, Aggarwal A, et al. Cancer research across Africa: a comparative bibliometric analysis. BMJ Glob Health 2022;7:e009849. 10.1136/bmjgh-2022-009849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wells JC, Sharma S, Del Paggio JC, et al. An analysis of contemporary oncology randomized clinical trials from low/middle-income vs high-income countries. JAMA Oncol 2021;7:379–85. 10.1001/jamaoncol.2020.7478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rubagumya F, Hopman WM, Gyawali B, et al. Participation of lower and upper middle-income countries in clinical trials led by high-income countries. JAMA Netw Open 2022;5:e2227252. 10.1001/jamanetworkopen.2022.27252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Lancet Global Health . Closing the door on parachutes and parasites. Lancet Glob Health 2018;6. 10.1016/S2214-109X(18)30239-0 [DOI] [PubMed] [Google Scholar]
- 20.World Medical Association . World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191–4. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 21.Dal-Ré R, Ndebele P, Higgs E, et al. Protections for clinical trials in low and middle income countries need strengthening not weakening. BMJ 2014;349:g4254. 10.1136/bmj.g4254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simpkin V, Namubiru-Mwaura E, Clarke L, et al. Investing in health R & D: where we are, what limits us, and how to make progress in Africa. BMJ Glob Health 2019;4:e001047. 10.1136/bmjgh-2018-001047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Data, The World Bank . Research and development expenditure (% of GDP). 2022. Available: https://data.worldbank.org/indicator/GB.XPD.RSDV.GD.ZS
- 24.Dimitris MC, Gittings M, King NB. How global is global health research? A large-scale analysis of trends in authorship. BMJ Glob Health 2021;6:e003758. 10.1136/bmjgh-2020-003758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmutz A, Salignat C, Plotkina D, et al. Mapping the global cancer research funding landscape. JNCI Cancer Spectr 2019;3:pkz069. 10.1093/jncics/pkz069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gimbel S, Chilundo B, Kenworthy N, et al. Donor data vacuuming:audit culture and the use of data in global health partnerships. MAT 2018;5. 10.17157/mat.5.2.537 [DOI] [Google Scholar]
- 27.Noor AM, Robinson J. Country ownership in global health. PLOS Glob Public Health 2022;2:e0000113. 10.1371/journal.pgph.0000113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Erondu NA, Aniebo I, Kyobutungi C, et al. Open letter to international funders of science and development in Africa. Nat Med 2021;27:742–4. 10.1038/s41591-021-01307-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Desai A, Kuderer NM, Lyman GH. Aligning cancer clinical trials with cancer burden: need for greater global leadership, resources, and vision. JAMA Oncol 2021;7:357–8. 10.1001/jamaoncol.2020.7293 [DOI] [PubMed] [Google Scholar]
- 30.ASCO . ASCO and the african organisation for research and training in cancer announce innovative collaboration to advance cancer research in africa. 2022. Available: https://old-prod.asco.org/news-initiatives/policy-news-analysis/asco-and-aortic-sign-mou-clinical-trials-research
- 31.The White House . FACT SHEET: cancer moonshot announces new actions aimed to reduce the cancer burden in africa as part of the U.S.-africa leaders summit | OSTP. 2022. Available: https://www.whitehouse.gov/ostp/news-updates/2022/12/14/fact-sheet-cancer-moonshot-announces-new-actions-aimed-to-reduce-the-cancer-burden-in-africa-as-part-of-the-u-s-africa-leaders-summit/
- 32.Africa CDC . Home. 2022. Available: https://africacdc.org/
- 33.Regional Office for Africa, WHO . Handbook for cancer research in africa. 2022. Available: https://www.afro.who.int/publications/handbook-cancer-research-africa
- 34.Zeigler-Johnson CM, Gueye SM, Rebbeck TR. Building infrastructure for cancer research in Africa. J Afr Cancer 2011;3:52–8. 10.1007/s12558-010-0112-2 [DOI] [Google Scholar]
- 35.Ngwa W, Addai BW, Adewole I, et al. Cancer in sub-saharan Africa: a lancet oncology commission. Lancet Oncol 2022;23:e251–312. 10.1016/S1470-2045(21)00720-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piot P, Caldwell A, Lamptey P, et al. Addressing the growing burden of non-communicable disease by leveraging lessons from infectious disease management. J Glob Health 2016;6:010304. 10.7189/jogh.06.010304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rubagumya F, Nyagabona SK, Msami KH, et al. Attitudes and barriers to research among oncology trainees in East Africa. Oncologist 2019;24:e864–9. 10.1634/theoncologist.2018-0805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vanderpuye V, Hammad N, Martei Y, et al. Cancer care workforce in Africa: perspectives from a global survey. Infect Agent Cancer 2019;14:11. 10.1186/s13027-019-0227-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ranganathan P, Chinnaswamy G, Sengar M, et al. The International collaboration for research methods development in oncology (CReDo) workshops: shaping the future of global oncology research. Lancet Oncol 2021;22:e369–76. 10.1016/S1470-2045(21)00077-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong RK, Vanderpuye V, Yarne J, et al. Clinical research mentorship programme (CRMP) for radiation oncology residents in Africa-building capacity through mentoring. Ecancermedicalscience 2021;15:1210. 10.3332/ecancer.2021.1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Horgan D. Personalised medicine and healthcare for an immediate future; 28.
- 42.Cancer moonshot research initiatives - NCI. 2017. Available: https://www.cancer.gov/research/key-initiatives/moonshot-cancer-initiative/implementation
- 43.Mutebi M, Dehar N, Nogueira LM, et al. Cancer groundshot: building a robust cancer control platform in addition to launching the cancer moonshot. Am Soc Clin Oncol Educ Book 2022:100–15. 10.1200/EDBK_359521 [DOI] [PubMed] [Google Scholar]
- 44.Queen’s University, Queen’s Gazette . Cancer groundshot: access to proven treatments must parallel development of new therapies. 2022. Available: https://www.queensu.ca/gazette/stories/cancer-groundshot-access-proven-treatments-must-parallel-development-new-therapies
- 45.Brant JM, Mayer DK. Precision medicine: accelerating the science to revolutionize cancer care. Clin J Oncol Nurs 2017;21:722–9. 10.1188/17.CJON.722-729 [DOI] [PubMed] [Google Scholar]
- 46.Pramesh CS, Badwe RA, Bhoo-Pathy N, et al. Priorities for cancer research in low- and middle-income countries: a global perspective. Nat Med 2022;28:649–57. 10.1038/s41591-022-01738-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rubagumya F, Mitera G, Ka S, et al. Choosing wisely Africa: ten low-value or harmful practices that should be avoided in cancer care. JCO Glob Oncol 2020;6:1192–9. 10.1200/GO.20.00255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aggarwal A, Lievens Y, Sullivan R, et al. What really matters for cancer care-health systems strengthening or technological innovation? Clin Oncol (R Coll Radiol) 2022;34:430–5. 10.1016/j.clon.2022.02.012 [DOI] [PubMed] [Google Scholar]
- 49.Hofman KJ, Kanyengo CW, Rapp BA, et al. Mapping the health research landscape in sub-Saharan Africa: a study of trends in biomedical publications. J Med Libr Assoc 2009;97:41–4. 10.3163/1536-5050.97.1.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mwareya R. Canada’s restrictive visa policies casting a shadow over IAC 2022. 2022. Available: https://www.aljazeera.com/opinions/2022/7/24/canadas-restrictive-visa-policies-casting-a-shadow-over-iac-2022
- 51.Saleh S, Masekela R, Heinz E, et al. Equity in global health research: a proposal to adopt author reflexivity statements. PLOS Glob Public Health 2022;2:e0000160. 10.1371/journal.pgph.0000160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khan SA. Decolonising global health by decolonising academic publishing. BMJ Glob Health 2022;7:e007811. 10.1136/bmjgh-2021-007811 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2022-011338supp001.pdf (20.2KB, pdf)
Data Availability Statement
No data are available.