In 2014, national emergency medicine and geriatrics societies released joint, standardized guidelines for Geriatric Emergency Department (GEDs) [1] One guideline recommendation is for assistive devices, which included cognitive engagement tools, walking aids/devices, and hearing amplifiers, to be incorporated in GEDs [1]. This recommendation for assistive devices was based on expert consensus and data from non-ED settings, and the effects of providing these types of equipment on ED patients and staff have not been explored. The primary aim of this qualitative study was to evaluate GED equipment use and the impact on patient experience. The secondary aim was to determine specific needs of ED staff and ideas for changes or improvements.
The setting is an academic, tertiary care Level 1 GED in the Midwest with 82,000 patient visits a year. The GED program and equipment have been previously described [2,3]. Equipment remains with the patient for use throughout their ED stay (Fig. 1). We conducted semistructured interviews with a convenience sample of patients ≥65 years old and ED staff using interview guides developed by our team. Briefly, we collected participant background, experience with the GED assistive devices, and the overall GED experience (interview guides available as Supplementary File S.1 and S.2). The study was approved by the site’s Institutional Review Board.
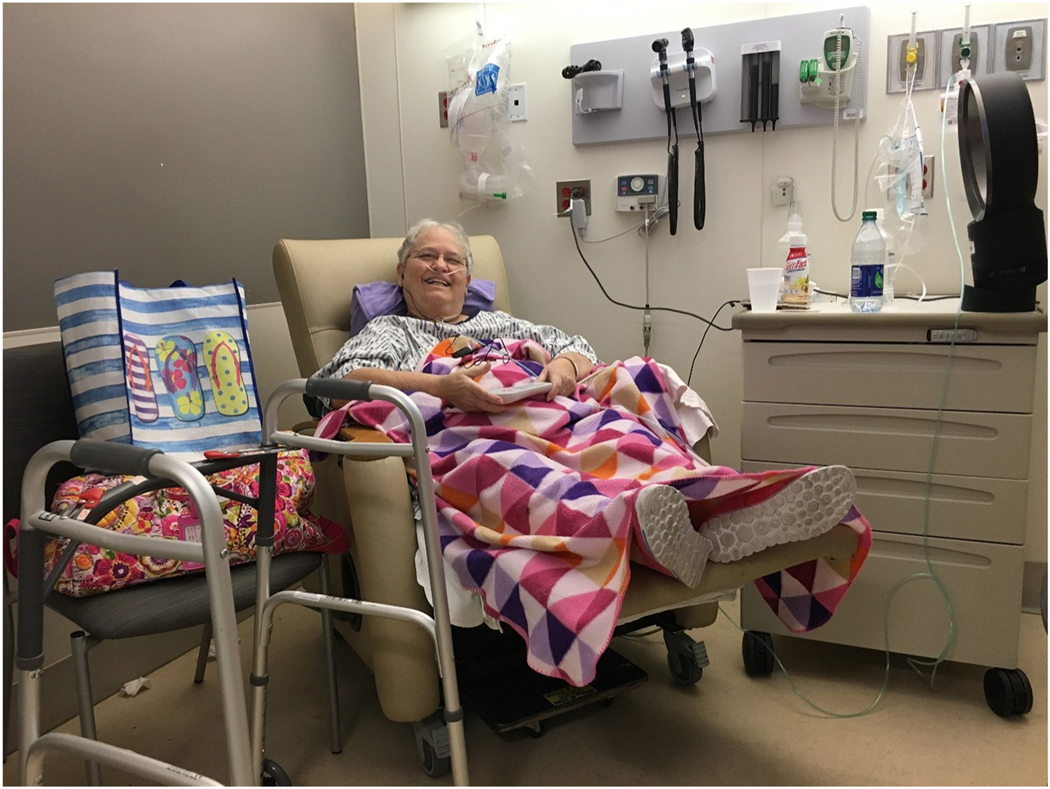
Fig. 1.
One study patient displays her use of the hearing amplifiers (black earbuds leading to a black box resting on her lap) and walker.
ED care providers (nurses, physicians, therapists, and nursing techs) participated in in-person interviews which took place during their workday (four hour timeframes across two days). Patients ≥65 years who had used any of the GED equipment were identified by ED staff. Exclusion criteria included non-English speaking patients and those in skilled nursing facilities or incarcerated. Patients and their caregivers when present were asked if someone from the study staff could give them a call after their discharge to ask questions regarding their experience with the assistive device as part of a research study. Participants were mailed a $25 gift card upon completion of the interview.
Consistent with rigorous qualitative methods [4], the transcribed interviews were inductively and deductively analyzed. We first developed a preliminary coding dictionary based on the questions asked in the interviews [5]. Three research team members engaged in coding the transcripts using ATLAS.ti qualitative data analysis software (Scientific Software Development Gmbh, Berlin, Germany) in order to refine the coding dictionary and explore the emergence of new codes in the data. The refined dictionary was used by the same members to code all remaining transcripts. Frequent meetings were held throughout the coding process to ensure reliability of coding and agreement about the creation and definitions of new codes as they emerged, consistent with a grounded theory approach [6]. We achieved saturation of the themes as reflected by a consistency of comments reported by patients and providers around key, emergent concepts.
Twenty two patients agreed to be contacted for the study and nine were able to be interviewed. Fifteen care providers were interviewed (Table 1). The most common devices used by the patients were mobility devices (walkers and canes), followed by sensory aids (hearing aids and glasses) and cognitive (puzzles and fidget toys). Study participants also mentioned mobility aids most (30 mentions), followed by sensory aids (16 mentions), cognitive aids (10 mentions) and personal care items such as shower chairs and bedside commodes (7 mentions).
Table 1.
Summary statistics on demographic information about study participants.
| Care provider role (n=15) | Frequency or mean | Mean tenure at institution (Years) |
|---|---|---|
|
| ||
| Registered nurses n (%) | 6 (40) | 8 |
| Physicians n (%) | 3 (20) | 3 |
| Occupational therapists n (%) | 3 (20) | 1 |
| Paramedics n (%) | 3 (20) | 7 |
| Patient (n=9) | ||
| Female n (%) | 4 (45) | |
| Age M (SD) | 78 (10) | |
All participants felt access to assistive devices in the GED was beneficial. Patients noted that they were offered assistive items without having to request them. Among providers, we identified three major themes: impact of assistive devices on patients, impact on the care team, and barriers to use. Table 2 presents sample quotations related to our identified themes and subthemes. Themes were consistent across the disciplines and staff members identified. Detailed quotes for providers are available in the Supplementary Tables S1–S3.
Table 2.
Example provider quotes by theme and subtheme.
| Impact on patients | |
| Empowering | “The more that you can actually show them concretely this is how it improves your quality of life, your functioning… if you are only verbally telling them this will help you the follow through is not going to be there. But if you can actually show them with that equipment, whether it be to show them how it improves or like Lauren said if they are in denial show them look you can’t do this.” [OT/PT 1] |
| “I always let them do what they can themselves and they can at least feel like they have, you know, I am strong enough to do this part. Like yes we have balance, whatever but you are not dependent you are still—because people don’t want to lose independence and all that so let them do what they can do safely.” [OT/PT 4] | |
| “…a lot of them they come in via EMS and they don’t have the ability to bring any of their walkers or their canes or anything with them and so in their mind they are kind of bed bound, unless they are a fall risk but…they basically kind of just, you know, they don’t have as much independence and they kind of feel it when they come in here. But if we have the equipment available I had a patient that was boarding in the ED for over 24 hours and when I came on shift they said “Well we have a walker available” and they were able to get up and down from the bed, over the chairs, kind of move about the room a little bit and it made their stay a lot more pleasant because they didn’t feel like they were just trapped in one spot. They had their independence and they were very grateful for that.” [Paramedic 2] | |
| “Well if they come here and they have a hard time reading discharge instructions we have the readers. If they can’t hear very well then we have that. You know it is just anything that they have a disability with anytime that we can help with that disability to make it more functional for them and…an ease of walking…everything. …We had a woman come in who didn’t have her hearing aids, was extremely hard of hearing, the conversation was like everybody out here could hear it and we just happened to have like, I don’t know, like a sound amplifying device. And hooked it up with her and really turned around the ability…she could really hear, she was impressed with how that worked so it kind of helped with the care.” [RN 4] | |
| Better education | “A lot of it is just the ease and a lot of it is just what they are used to or maybe it is a new diagnosis and something that they are going to need trained on too.” [RN 6] |
| “I had a patient who was waiting for a bed in the James who had been there over a day. And I guess he was geriatric, I think he was 65. And he was having acute on chronic right side weakness. I recommended a platform wheeled walker. When he had the wheeled walker from home we had the platform here. Put the platform on his walker, showed his daughter how to use it, he was able to go home and avoid admission, got the equipment, did the family teaching which was great. They were really appreciative.” [RN 3] | |
| Improve patient experience | “In the sense that now I feel like they are more connected in terms of what our recommendations are, what we are doing. It is very isolating when you can’t hear. So the amplifiers I have found to be very positive.” [OT/PT 1] |
| “Helps them feel more secure and if they are used to having a cane or whatever to use to get around it makes it much easier and makes them more mobile too. They don’t even need us if they have that device. I think it is an extension to our healthcare and helping patients. An extension to making things better for them and more independent too, so. It is a nice thing to have for that reason.” [Paramedic 1] | |
| “You know, when they are here in the ER they are out of their comfort zone just like any patient normally is. But you know they are just a more vulnerable population and just to be able to assist them, you know if you normally do use a walker it is nice to see they can still use that walker while they are here.” [RN 1] | |
| Impact on providers | |
| Improved ability to assess patient | “…so that if we have amplifiers or if we know that they are deaf in the left ear and we—and its good because then we are not saying that they have cognitive problems, they just couldn’t hear us. Put them in or see us. And they are like “Oh” and now you can hear us, now you can follow commands and you are oriented. But sometimes we are going to label you as cognitively impaired but in reality you don’t have your hearing aids. You know? So even having the amplifiers and that, it gives us a better baseline to make better discharge recommendations.” [PT/OT 3] |
| “I feel like the overall treatment session is going to be…the quality is going to be better for a couple of reasons. Not only they are going to hear what I have to say in terms of information that I am providing, recommendations, but also often times you are asking questions and they don’t even know what you are asking so you are getting misinformation about what a home set up is, what kind of support they have. Is it a regular support every day? Or is it just somebody coming in once a week? So you can get misinformation back if they are not hearing what your questions are.” [RN 1] | |
| “I think it gives me more opportunity during the interviewing process because instead of having 10 minutes to focus on trying to get my message across and have them answer the question, we can at least—they can hear me from the upfront and they can answer the question right away and then we can kind of move on to other things.” [Physician 1] | |
| “For example we will have patients who are coming in short of breath or maybe have pneumonia and kind of a criteria for whether they can go home is if they can ambulate with medical oxygen. And I could just have the nurse walk them around but if they maybe—I know I have had patients who use a cane or walker for mobility. So you want to test what they will actually be using so we will get them a cane or walker to use.” [Physician 3] | |
| Improve workflow | “I think sometimes it might be able to save time and resources that if someone is that borderline saying “Well they are quite independent they just don’t have a walker”, that we have a walker that the nursing staff will walk them to the bathroom and be like do they need to have therapy? And possibly think about … do they just need that walker because that is what they rely on at home and their baseline is fine.” [OT/PT 4] |
| “…they are accessible to us but the walkers and canes you know, if you didn’t have those you are just, you are just…take a lot longer. So you would have to go find a walker, you would have to find a cane.” [RN 6] | |
| “I think for me it allows me to spend more time with them because I have that equipment instead of just verbally saying this will be great. It helps me do my job better. I can do far better education when I have the equipment if it is available. And it saves me time. Productivity, I can see more people because it is right here. I don’t have to run to another floor to grab something and bring it back down.” [RN 1] | |
| Safety | “I think for safety and like physical safety issue for us even like you don’t have to hold them, carry them, try to help ambulate them to the bathroom. Now they have like a way to kind of do it independent with some stand by assistance versus manual— helping them walk so I think that is good for us as well.” [RN 3] |
| “The walkers and canes, so most of the time we don’t have our geriatric patients walking just because I don’t want them to fall and I am not that big of a person to catch them.” [Physician 1] | |
| Barriers | |
| Equipment-related barriers | “All the gate belts disappeared once I told PT where they were.” [RN 4] |
| “Well we have our ER people too, our staff, it’s good for them but sometimes they keep it and don’t bring it back” Paramedic 1 “..the size of our rooms are so small. You put all of this equipment in these rooms and then you have an elderly person trying to maneuver a walker around and it just adds that much more.” [RN 6] | |
| Reminders to use items | “...a lot of us don’t do it regularly but maybe if we could have some sort of more streamlined way that that gets done.” RN 4 “I don’t have a reminder of like hey this is a geriatric patient, could they benefit from hearing aids or walker or…most of the time it is kind of on the backend.” [RN 5] |
|
“I think it is just remembering to do the assessment part that I was talking about. And the flow sheet. Like, especially between handoff.” [RN 3] “We are like oh yeah I remember we have that thing. But then you forget and then you’re like “Oh wait. I couldn’t go do it.” [Physician 1] |
|
| “The nurses knowing we have them as resources and where to find them would be fantastic.” Physician 2 | |
| Lack of EHR integration | “But if there is a geriatric patient and maybe a flag or something, Hey. Do they need a resource?” [Physician 1] |
| “So there is a documentation flowsheet for patient rounding note. But the GEDI assessment in and of itself does not exist separately. So it only exists within the rounding note.” [RN 3] |
Note: OT/PT = Occupational Theraphy/Physical Theraphy; RN = Registered Nurse; ED = Emergency Department; ER = Emergency Room; GEDI = Geriatric Emergency Department Intake
Providers in our study described ways in which incorporating assistive devices into GED care empowers patients to be more engaged in their care. Older adults report more fear and difficulty navigating the ED system and understanding how to call the nurse or provider [7]. GED equipment may assist with these difficulties as we found that these devices helped the patient directly by affording them greater independence during their GED stay as well as indirectly by facilitating communication between the patient and provider. Tools that allow the patient to more fully participate in their care can be an important facilitator to patient engagement in the ED setting.
Study limitations include cognitive recall of the patients, as some participants had to be prompted that they were given the device in the ED. Additionally, we did not have the opportunity to review results with the participants which could potentially result in further suggestions for improvement. In the case of patients, the results were uniformly positive but this could have resulted in additional conclusions from staff.
Supplementary Material
Funding Details
Funding for this study was partially covered, specifically LTS and BMR’s efforts, by the National Institute on Aging: NIA K23AG06128401.
Footnotes
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajem.2020.07.073.
Disclosure Statement
All authors declare no commercial associations or conflicts of interest.
Contributor Information
Naleef Fareed, CATALYST – The Center for the Advancement of Team Science, Analytics, and Systems Thinking, College of Medicine, The Ohio State University, Institute for Behavioral Medicine Research, 460 Medical Center Drive, Columbus, OH 43210, United States of America; Department of Biomedical Informatics, College of Medicine, The Ohio State University, 1585 Neil Ave., Columbus, OH 43210, United States of America.
Lauren T. Southerland, Department of Emergency Medicine, College of Medicine, The Ohio State University, 410 W 10th Ave., Columbus, OH 43210, United States of America
Brian M. Rao, Department of Emergency Medicine, College of Medicine, The Ohio State University, 410 W 10th Ave., Columbus, OH 43210, United States of America
Cynthia J. Sieck, CATALYST – The Center for the Advancement of Team Science, Analytics, and Systems Thinking, College of Medicine, The Ohio State University, Institute for Behavioral Medicine Research, 460 Medical Center Drive, Columbus, OH 43210, United States of America Department of Family Medicine, College of Medicine, The Ohio State University, 2231 N High St., Columbus, OH 43210, United States of America.
References
- [1].ACoE Physicians, Society AG, Association EN, SfAE Medicine, GEDGT Force. Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7–25. [DOI] [PubMed] [Google Scholar]
- [2].Southerland LT, Savage EL, Muska Duff K, et al. Hospital costs and reimbursement model for a Geriatric Emergency Department. Acad Emerg Med. 2020. 10.1111/acem.13998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Southerland LT, Lo AX, Biese K, et al. Concepts in practice: Geriatric emergency departments. Ann Emerg Med. 2020;75(2):162–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Miles M, Huberman A. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- [5].Crabtree B, Miller W. Using Codes and Code Manuals: A Template Organizing Style of Interpretation. , 2Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- [6].Kennedy M, Enander RA, Tadiri SP, Wolfe RE, Shapiro NI, Marcantonio ER. Delirium risk prediction, healthcare use and mortality of elderly adults in the emergency department. J Am Geriatr Soc. 2014;62(3):462–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Liu B, Taylor DM, Ling SL, MacGibbon P. Non-medical needs of older patients in the emergency department. Australas J Ageing. 2016;35(3):174–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.