Abstract
For many years, surgical treatment of buried penis in children has been researched by several scholars, and numerous methods exist. This study aimed to explore the clinical effect of a modified fixation technique in treating buried penis in children. Clinical data of 94 patients with buried penis who were treated using the modified penile fixation technique from March 2017 to February 2019 in Fujian Maternity and Child Health Hospital (Fuzhou, China) were retrospectively collected, compared, and analyzed. Clinical data of 107 patients with buried penis who were treated using traditional penile fixation technique from February 2014 to February 2017 were chosen for comparison. The results showed that at 6 months and 12 months after surgery, the penile lengths in the modified penile fixation group were longer than those in the traditional penile fixation group (both P < 0.05). The incidence of postoperative skin contracture and penile retraction in the modified penile fixation group was less than that in the traditional penile fixation group (P = 0.034 and P = 0.012, respectively). When the two groups were compared in terms of parents’ satisfaction scores, the scores for penile size, penile morphology, and voiding status in the modified penile fixation group were higher than those in the traditional penile fixation group at 2-week, 6-month, and 12-month follow-ups after surgery (all P < 0.05). We concluded that the modified penile fixation technique could effectively reduce the incidence of skin contracture and penile retraction and improve the penile length and satisfaction of patients’ parents.
Keywords: buried penis, modified fixation technique, penile retraction
INTRODUCTION
Buried penis is a common congenital penile dysplasia in children. It has an incidence of 0.68% in China.1–3 Different causes have been proposed, including the following: abnormal fibrous bands between the dartos and deep fascias, deficiency of shaft skin, lack of skin attachment to the penile shaft, excessive prepubic fat, and abnormal displacement of the penis in the ventral direction.4–6 The penis appears to be fused to the scrotum, and the penile shaft is entrapped within the subcutaneous tissue. The penis might be partially visible with a “stumpy-looking” and “dome-shaped” appearance or completely invisible with only the glans covered by a protruding prepuce. Buried penis can lead to several conditions, e.g., phimosis, difficulties in maintaining hygiene leading to balanitis, urinary tract infections, urine spreading, urinary retention, erectile dysfunction obstruction, penile cancer, and psychological illness.7,8 Additionally, the longer the penis is hidden, the greater is the risk. Therefore, patients with buried penis must be diagnosed early and receive surgical treatment.
For many years, several scholars have conducted research on the surgical treatment of buried penis, and various surgical methods are available, e.g., Sugita’s, Shiraki’s, Borsellino’s, Brisson’s, and Hadidi’s surgeries, which have their respective advantages and disadvantages.4,9–12 We advocated as much simplification of the surgery and reduction of postoperative complications as possible to obtain a relatively good postsurgical appearance. This study aimed to introduce a modified fixation technique developed for buried penis treatment and explore its clinical effectiveness.
PARTICIPANTS AND METHODS
This study was approved by the ethics committee of Fujian Maternity and Child Health Hospital, Fuzhou, China (2019 Ethics Application No. 163; September 27, 2019) and strictly adhered to the tenets of the Declaration of Helsinki (2008). Additionally, all the parents or guardians of the children provided written consent regarding study participation for their respective minors.
Participants
Between February 2014 and February 2017, 107 patients with buried penis were treated using the traditional penile fixation technique in Fujian Maternity and Child Health Hospital. Between March 2017 and February 2019, 94 patients with buried penis were treated using the modified penile fixation technique. According to the surgery method, the patients were divided into the modified penile fixation group (n = 94) and the traditional penile fixation group (n = 107). The clinical data of two groups were retrospectively collected, compared, and analyzed. All surgeries were performed by a surgeon with extensive surgical experience.
Children who were definitively diagnosed with buried penis were included. The exclusion criteria were as follows: (1) children combined with severe active balanitis; (2) children combined with buried penis associated with other penile deformities; (3) the clinical data were incomplete; (4) patients undergoing reoperation; or (5) study participation was not approved by patients’ guardians.
Modified fixation method
First, the distal end of the foreskin was lifted using pliers. Then, the narrow end of the prepuce was removed from the ventral side to the dorsal side using scissors such that the inner plate of the prepuce was separated from the outer plate. A F6-F8 silica gel catheter was preserved, and the left and right sides of the inner plate of the prepuce were symmetrically clamped using two mosquito pliers. Hemostatic forceps were used for the initial segment of the inner plate at 12 o’clock, 5 o’clock, and 7 o’clock positions on the penis; the initial segment was longitudinally attached to the Buck’s fascia and stretched along the penile shaft up to the penile root. Simultaneously, the assistant held the undamaged forceps and clamped the outer plate of the foreskin to form a separation surface. The surgeon gently dissociated the abnormal fibrotic tissue bound to the Buck’s fascia until the penis was completely exposed. The attachment band around the crura of the penis was removed to ensure that both the dorsally fixed planes were flat.
The Scarpa’s fascia was pulled down using hemostatic forceps to fully expose the fixed point. Needles (#12) were penetrated into the skin at approximately 2 o’clock and 10 o’clock positions between the penis and scrotal skin. Next, a 4-0 prolene suture was punctured through the pinhole at a distance of approximately 0.3 cm away from the dorsal nerve and vascular plexus of the penis and was passed through the Buck’s fascia at the root of the separated plate. Then, the needle was penetrated through the pinhole at the original position of the Scarpa’s fascia layer. The knot was tied and buried into the dermis of the skin. Longitudinal cutting was performed at 12 o’clock, 5 o’clock, and 7 o’clock positions on the inner plate to remove the stenosis ring and excess inner plate tissue. The incision was sutured using a 5-0 single absorbable suture. The operative penile length was measured, and a dressing was applied to the penis (Figure 1).
Figure 1.
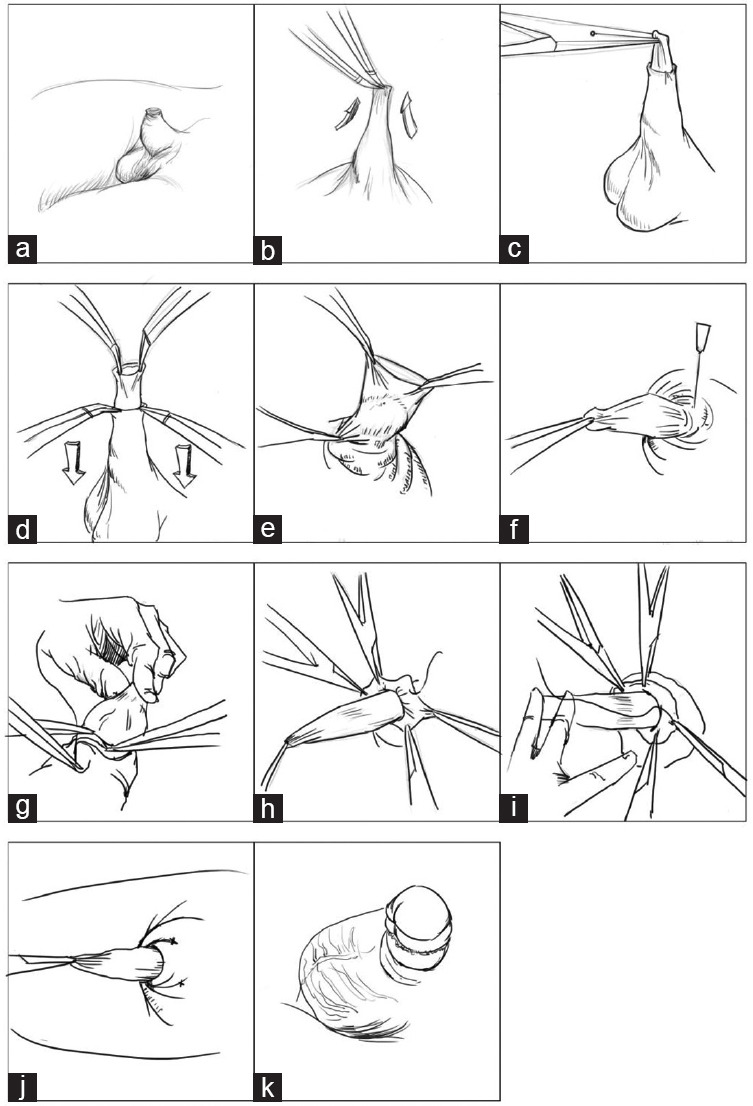
The surgical procedure. (a) The preoperative appearance. (b) Remove the narrow end of the prepuce. (c) Clamp and drag the prepuce with the mosquito pliers. (d) The undamaged forceps clamped the outer plate of the foreskin to form a separation surface. (e) Dissect the tethering ligament along the penile shaft closed to the Buck’s fascia. (f) Needles (#12) were penetrated into the skin at about 2 o’clock and 10 o’clock position. (g) The 4-0 prolene suture was punctured through the pinhole. (h) The 4-0 prolene line was sutured across the Buck’s fascia next to the dorsal penile vascular nerve plexus. (i) The needle was penetrated through the pinhole at the original position of the Scarpa’s fascia layer. (j) The knot was fixed in the dermis. (k) The postoperative appearance.
Traditional fixation method
The procedure of traditional fixation was similar to that of the modified one. The difference was that the dermis and Scarpa’s and Buck’s fascias were sewn directly using silk thread at 10 o’clock and 2 o’clock positions on the dorsal side of the penis instead of perforating the skin.
Evaluation of parents’ satisfaction and postoperative complications
Conducting follow-ups at 2 weeks, 6 months, and 12 months after surgery was recommended. At all follow-ups conducted after surgery, the following complications were recorded: incision infection, scrotum hematoma, penile retraction, and preputial skin necrosis. A questionnaire regarding penile size, morphology, and voiding status was administered to evaluate parents’ satisfaction. The degree of satisfaction was determined on a scale of 1–5 (grade 1: very unsatisfactory; grade 2: unsatisfactory; grade 3: neither satisfactory nor unsatisfactory; grade 4: satisfactory; and grade 5: very satisfactory).13 The questionnaire was administered at the 6- and 12-month follow-ups after surgery.
Penile length measurement method
Penile length was measured from the tip to the root of the penis above the pubic symphysis.14
Diagnosis of skin contracture
There are keloids or hard blocks in the anastomosis, which affect the elasticity of the outer plate and cause hardening of the inner plate or adhesion of the glans head.4
Statistical analyses
SPSS version 19 (IBM, Armonk, NY, USA) was used to perform statistical analysis. Continuous data were presented as the mean ± standard deviation and range. Because the two cohorts are unevenly distributed, a nonparametric analysis was performed. The χ2 or Fisher’s test was used to categorize the variables. P < 0.05 was defined as statistically significant.
RESULTS
General preoperative data of all patients are shown in Table 1. There were no statistically significant differences between the modified penile fixation group and traditional penile fixation group in terms of age, weight, and preoperative penile length distribution (all P > 0.05; Table 1), which indicated that the two groups were homogeneous and comparable.
Table 1.
Comparison of preoperative general data between modified penile fixation group and traditional penile fixation group
| Item | Modified penile fixation group | Traditional penile fixation group | P |
|---|---|---|---|
| Patients (n) | 94 | 107 | |
| Age (year), mean±s.d. | 4.3±2.1 | 4.9±2.5 | 0.563 |
| Weight (kg), mean±s.d. | 22.7±9.5 | 23.5±11.6 | 0.427 |
| Preoperative penis length (cm), mean±s.d. | 1.7±0.2 | 1.8±0.3 | 0.883 |
s.d.: standard deviation
All surgeries were successfully completed, and a total of 201 patients were successfully followed up. There were no differences between the two groups in terms of surgery time, postoperative hospital stay, catheter retention time, and postoperative penile length (all P > 0.05). The penile lengths at 6 months and 12 months after surgery in the modified penile fixation group were longer than those in the traditional penile fixation group (P = 0.036 and P = 0.029, respectively; Table 2).
Table 2.
Comparison of the postoperative clinical data between modified penile fixation group and traditional penile fixation group
| Item | Modified penile fixation group | Traditional penile fixation group | P |
|---|---|---|---|
| Operating time (min), mean±s.d. | 49.4±4.0 | 54.2±6.8 | 0.235 |
| Postoperative hospital stay (day), mean±s.d. | 3.3±0.9 | 3.5±1.3 | 0.308 |
| Catheter retention time (day), mean±s.d. | 3.1±0.8 | 3.4±1.1 | 0.526 |
| Postoperative penis length (cm), mean±s.d. | 3.6±0.5 | 3.5±0.6 | 0.879 |
| Penis length at 6 months after surgery (cm), mean±s.d. | 3.4±0.6 | 3.1±0.7 | 0.036 |
| Penis length at 12 months after surgery (cm), mean±s.d. | 3.9±0.8 | 3.5±0.7 | 0.029 |
s.d.: standard deviation
The incidence of postoperative skin contracture and penile retraction in the modified penile fixation group was lower than that in the traditional penile fixation group (0 vs 4.8%, P = 0.034; and 0 vs 6.5%, P = 0.012, respectively). There were no clinical symptoms in the children with penile retraction. Because the children were young and had no clinical symptoms, a second surgery was not performed, and they were closely followed up. There was no difference between the two groups in terms of the incidence of lymphedema, incision infection, or scrotal hematoma (all P > 0.05). There were no complications of skin necrosis or a second surgery in both the groups (Table 3).
Table 3.
Comparison of the complications between modified penile fixation group and traditional penile fixation group
| Item | Modified penile fixation group | Traditional penile fixation group | P |
|---|---|---|---|
| Lymphedema (n) | 90 | 105 | 0.321 |
| Incision infection, n (%) | 2 (2.2) | 2 (1.9) | 0.896 |
| Scrotal hematoma, n (%) | 2 (2.2) | 5 (4.8) | 0.326 |
| Skin contracture, n (%) | 0 (0) | 5 (4.8) | 0.034 |
| Penis retraction, n (%) | 0 (0) | 7 (6.7) | 0.012 |
| Skin necrosis, n (%) | 0 (0) | 0 (0) | 1.0 |
| Second operation, n (%) | 0 (0) | 0 (0) | 1.0 |
Three aspects of parents’ satisfaction were evaluated, including penile size, penile morphology, and voiding status. The results of comparing the satisfaction scores received by the parents of the two groups showed that the scores for penile size, penile morphology, and voiding status in the modified penile fixation group were higher than those in the traditional penile fixation group at the 2-week, 6-month, and 12-month follow-ups after surgery (all P < 0.05; Table 4).
Table 4.
Comparison of the satisfaction score of the parents between modified penile fixation group and traditional penile fixation group
| Item | Modified penile fixation group | Traditional penile fixation group | P |
|---|---|---|---|
| 2 weeks after surgery (mean ± s.d.) | |||
| Penile size | 4.3±0.8 | 3.8±0.9 | 0.043 |
| Penile morphology | 4.2±0.7 | 3.7±0.7 | 0.041 |
| Voiding status | 4.2±0.9 | 3.6±1.0 | 0.039 |
| 6 months after surgery (mean ± s.d.) | |||
| Penile size | 4.3±0.9 | 3.5±1.0 | 0.032 |
| Penile morphology | 4.4±0.8 | 3.6±1.1 | 0.033 |
| Voiding status | 4.2±0.7 | 3.5±0.9 | 0.035 |
| 12 months after surgery (mean ± s.d.) | |||
| Penile size | 4.4±1.1 | 3.3±0.9 | 0.025 |
| Penile morphology | 4.5±1.0 | 3.5±1.2 | 0.027 |
| Voiding status | 4.3±0.9 | 3.4±0.9 | 0.030 |
s.d.: standard deviation
DISCUSSION
Buried penis is a common congenital malformation of the penis in children, which affects not only penile development but also psychological and behavioral aspects of children. If this condition is left untreated, teenage boys often develop anxiety regarding their penile size. It may affect self-esteem and gender identification and can cause social embarrassment. Some authors have named this condition “small penis syndrome”.15 Small penis syndrome is not only a problem wherein the penis itself looks small physically but, more importantly, it also seriously affects boys’ self-confidence and causes psychological development-related problems, e.g., anxiety, depression, being not good at showing ourselves, behavior lack of male sexual characteristics, and issues related to social integration ability. This would in turn develop severe psychosocial problems that require more attention.16 Additionally, buried penis will increase the risk of infection.7,8 Therefore, early diagnosis and treatment of buried penis is crucial.17
Various surgical methods for treating buried penis are available, e.g., Johnson’s, Shiraki’s, and Devine’s surgeries and other modified surgeries, and they have their respective advantages and disadvantages.18-22 Johnson’s surgery employs a circular incision at the root of the penis. Although its postoperative fixation effect is good, the patient’s subcutaneous blood and lymphatic vessels are blocked, resulting in postoperative penile skin swelling and preputial edema.18 Shiraki’s surgery solves the problem of insufficient outer foreskin by retaining more inner foreskin; however, too much inner foreskin affects the appearance of the penis.19 Devine’s surgery solves the cause and the problem of penile skin deficiency, but because the skin of the penile scrotum horn is not treated, the appearance of the buried penis with webbed skin does not remarkably improve.20 Because Devine’s surgery only cuts and releases the narrow ring of the foreskin from the dorsal side of the penis, this creates a narrow field of vision and makes the exposure of the surgical area extremely difficult.
Scholars worldwide have performed substantial research and attempted to simplify the surgical procedure, improve the short-term and long-term appearances of the penis after surgery, reduce the occurrence of postoperative complications, and improve the satisfaction of children with buried penis and their parents. Srinivasan et al.23 summarized the basic steps of buried penis treatment. Han et al.13 used the transferred scrotal flap to fill the vacancy of the ventral external plate of the penile shaft. Yu et al.24 attempted a minimally invasive treatment that only fixed the dorsal root of the penis. Chin et al.25 simplified the steps of the surgery – the inner plate was trimmed and the narrow ring of the outer plate was removed, but the ventral side was not modified, and the dorsal dermis and Buck’s fascia of the penis were fixed with two stitches.
After years of clinical practice, it was found that for buried penis surgery, fixation of the penile base is very important, and it directly relates to the success or failure of the surgery. If the penile base is improperly fixed, it will cause skin contracture and penile retraction, affecting the appearance of the penis after surgery, and it may even lead to a second surgery. The traditional penile base fixation method involves suturing the Scarpa’s and Buck’s fascias directly to the dermis using a silk thread. Because the dermis tends to slip easily, if there is little suture tissue, it cannot provide sufficient pulling force, and penile base fixation is unstable after surgery, easily leading to penile retraction after surgery. Moreover, if there is too much suture tissue, skin contracture appears easily after surgery. To reduce postoperative complications, the penile fixation technique was modified. The Scarpa’s and Buck’s fascias were firmly fixed using 4-0 Prolene thread through the skin, which provided sufficient pulling force and prevented postoperative complications such as skin contracture and penile retraction. In this study, the incidence of complications such as skin contracture and penile retraction was lower in the modified fixation group (P < 0.05).
A good penile appearance is very important for children’s confidence and mental health. Parents’ satisfaction was evaluated via three aspects, including penile size, penile morphology, and voiding status. The results showed that at 2 weeks, 6 months, and 12 months after surgery, all the satisfaction scores of the modified fixation group were higher than those of the traditional fixation group (all P < 0.05). Furthermore, the penile appearance was better when the modified fixation technique was used; this could be attributed to the provision of a more stable fixation effect, effectively reducing the deformation of the penis after surgery and ensuring the effect of surgical shaping.
This study has several limitations. First, this was a retrospective study. Second, this was a single-center study with a small sample size. Third, the follow-up time was brief. In future, we plan to conduct a multi-center prospective randomized controlled study and follow up the long-term results to more objectively evaluate the effect of this procedure.
CONCLUSIONS
The modified penile fixation technique is simple and easy to perform. It can also effectively reduce the incidence of skin contracture and penile retraction as well as improve penile length and satisfaction of patients’ parents.
AUTHOR CONTRIBUTIONS
XC, BJG, and CMZ conceptualized and designed the study, and they also assisted with drafting or revision of the manuscript. XC and WHH wrote the manuscript and collected the data. XC, BJG, and LC performed data analysis and assisted with proofreading. All authors have read and approved the final manuscript.
COMPETING INTERESTS
All authors declared no competing interests.
ACKNOWLEDGMENTS
We acknowledge the contributions of the doctors of Yi-Fan Fang, Dian-Ming Wu, and Ming-Kun Liu in Fujian Maternity and Child Health Hospital.
REFERENCES
- 1.Maizels M, Zaontz M, Donovan J, Bushnick PN, Firlit CF. Surgical correction of the buried penis: description of a classification system and a technique to correct the disorder. J Urol. 1986;136:268–71. doi: 10.1016/s0022-5347(17)44837-3. [DOI] [PubMed] [Google Scholar]
- 2.Liu X, He DW, Hua Y, Zhang DY, Wei GH. Congenital completely buried penis in boys: anatomical basis and surgical technique. BJU Int. 2013;112:271–5. doi: 10.1111/j.1464-410X.2012.11719.x. [DOI] [PubMed] [Google Scholar]
- 3.Yan XM, Zhou Y. Effect of modified penile detrophication in the treatment of congenital occult penis. J Clin Urol. 2012;27:687–8. [Google Scholar]
- 4.Sugita Y, Ueoka K, Tagkagi S, Hisamatsu E, Yoshino K, et al. A new technique of concealed penis repair. J Urol. 2009;182:1751–4. doi: 10.1016/j.juro.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 5.Cromie WJ, Ritchey ML, Smith RC, Zagaja GP. Anatomical alignment for the correction of buried penis. J Urol. 1998;160:1482–4. [PubMed] [Google Scholar]
- 6.Shenoy MU, Srinivasan J, Sully L, Rance CH. Buried penis: surgical correction using liposuction and realignment of skin. BJU Int. 2000;86:527–30. doi: 10.1046/j.1464-410x.2000.00798.x. [DOI] [PubMed] [Google Scholar]
- 7.Lei J, Luo C, Wang X, Su X. A novel “six stitches”procedures for pediatric and adult buried penis. Int Braz J Urol. 2019;45:190–1. doi: 10.1590/S1677-5538.IBJU.2017.0688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murakami H, Yazaki Y, Seo S, Ochi T, Okawada M, et al. A single surgeon's experience of 65 cases of penoplasty for congenital megaprepuce, with special reference to mid- to long-term follow-up. Pediatr Surg Int. 2015;31:89–92. doi: 10.1007/s00383-014-3627-2. [DOI] [PubMed] [Google Scholar]
- 9.Shiraki IW, Shirai RS. Congenital micropenile skin sleeve. J Urol. 1975;114:469–72. doi: 10.1016/s0022-5347(17)67060-5. [DOI] [PubMed] [Google Scholar]
- 10.Borsellino A, Spagnoli A, Vallasciani S, Martini L, Ferro F. Surgical approach to concealed penis: technical refinements and outcome. Urology. 2007;69:1195–8. doi: 10.1016/j.urology.2007.01.065. [DOI] [PubMed] [Google Scholar]
- 11.Brisson P, Patel H, Chan M, Feins N. Penoplasty for buried penis in children: report of 50 cases. J Pediatr Surg. 2001;36:421–5. doi: 10.1053/jpsu.2001.21605. [DOI] [PubMed] [Google Scholar]
- 12.Hadidi AT. Buried penis: classification surgical approach. J Pediatr Surg. 2014;49:374–9. doi: 10.1016/j.jpedsurg.2013.09.066. [DOI] [PubMed] [Google Scholar]
- 13.Han DS, Jang H, Youn CS, Yuk SM. A new surgical technique for concealed penis using an advanced musculocutaneous scrotal flap. BMC Urol. 2015;15:54. doi: 10.1186/s12894-015-0044-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu F, Lin T, He D, Wei G, Liu J, et al. New technique for the treatment of buried penis in children. Urology. 2016;88:166–9. doi: 10.1016/j.urology.2015.09.031. [DOI] [PubMed] [Google Scholar]
- 15.Wylie KR, Eardley I. Penile size and the 'small penis syndrome'. BJU Int. 2007;99:1449–55. doi: 10.1111/j.1464-410X.2007.06806.x. [DOI] [PubMed] [Google Scholar]
- 16.Cytryn L, Cytryn E, Rieger RE. Psychological implications of cryptorchism. J Am Acad Child Psychiatry. 1967;6:131–65. doi: 10.1016/s0002-7138(09)61294-2. [DOI] [PubMed] [Google Scholar]
- 17.Herndon CD, Casale AJ, Cain MP, Rink RC. Long-term outcome of the surgical treatment of concealed penis. J Urol. 2003;170:1695–7. doi: 10.1097/01.ju.0000083911.59937.c6. [DOI] [PubMed] [Google Scholar]
- 18.Li BY, Zhang GF, Wang H. Effect comparison of different surgical methods for concealing penis. Chin J Urol. 2010;31:128–30. [Google Scholar]
- 19.Li XL, Gong YB, Lin T. Diagnosis and surgical treatment of buried penis in children. Chin J Pediatr Surg. 1996;17:215–7. [Google Scholar]
- 20.Xu JG, Lv C, Wang YC, Zhu J, Xue CY. Management of concealed penis with modified penoplasty. Urology. 2015;85:698–702. doi: 10.1016/j.urology.2014.06.044. [DOI] [PubMed] [Google Scholar]
- 21.Gao ZX, Liu XL. [Progress in diagnosis and treatment of occult penis. Chin J Androl. 2021;35:73–80. [Article in Chinese] [Google Scholar]
- 22.Frenkl TL, Agarwal S, Caldamone AA. Results of a simplified technique for buried penis repair. J Urol. 2004;171:826–8. doi: 10.1097/01.ju.0000107824.72182.95. [DOI] [PubMed] [Google Scholar]
- 23.Srinivasan AK, Palmer LS, Palmer JS. Inconspicuous penis. ScientificWorldJournal. 2011;11:2559–64. doi: 10.1100/2011/238519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu W, Cheng F, Zhang X, Ruan Y, Yang S, et al. Minimally invasive technique for the concealed penis lead to longer penile length. Pediatr Surg Int. 2010;26:433–7. doi: 10.1007/s00383-010-2576-7. [DOI] [PubMed] [Google Scholar]
- 25.Chin TW, Tsai HL, Liu CS. Modified prepuce unfurling for buried penis: a report of 12 years of experience. Asian J Surg. 2015;38:74–8. doi: 10.1016/j.asjsur.2014.04.006. [DOI] [PubMed] [Google Scholar]


