Abstract
Importance:
Clinical trial sponsors rely on eligibility criteria to control the characteristics of patients in their studies, promote the safety of participants, and optimize the interpretation of results. However, in recent years, complex and often overly restrictive inclusion and exclusion criteria have created substantial barriers to patient access to novel therapies, hindered trial recruitment and completion, and limited generalizability of trial results.
Objective:
A LUNGevity Foundation working group developed a framework for lung cancer clinical trial eligibility criteria. The goals of this framework are to (1) simplify eligibility criteria, (2) facilitate stakeholders’ (patients, clinicians, and sponsors) search for appropriate trials and, (3) harmonize trial populations to support inter-trial comparisons of treatment effects.
Observations:
Clinicians, representatives from the pharmaceutical industry, the National Cancer Institute (NCI), the Food and Drug Administration (FDA), the European Medicines Agency (EMA), and LUNGevity undertook a process to identify and prioritize key items for inclusion in trial eligibility criteria. The group generated a prioritized library of terms to guide investigators and sponsors in the design of first-line, advanced non-small cell lung cancer (NSCLC) clinical trials intended to support marketing application. These recommendations address disease stage and histology, enrollment biomarkers, performance status, organ function, brain metastases, and comorbidities. This effort forms the basis for a forthcoming FDA draft Guidance for Industry.
Conclusions and Relevance:
As an initial step, the recommended cross-trial standardization of eligibility criteria may harmonize trial populations. Going forward, by connecting diverse stakeholders and providing formal opportunity for public input, the emerging FDA draft guidance may also provide an opportunity to revise and simplify longstanding approaches to trial eligibility. This work serves as a prototype for similar efforts now underway in other cancers.
Keywords: exclusion, inclusion, protocol, recruitment, sponsor
Introduction
Cancer clinical trial accrual remains a persistent challenge. Difficulties recruiting and retaining representative participants result in prolonged study duration, premature trial closure, heightened costs of clinical research, and delayed advances in the field. Many oncology trials close prematurely, and those that do finish are generally extremely costly. Multiple factors contribute to these problems, including complexity of trial protocols, lack of access to trial sites, and stringent eligibility criteria.1
Clinical trial sponsors rely on eligibility criteria to control the characteristics of study participants to generate interpretable and reproducible results. Over the last several decades, however, the number and specificity of eligibility criteria have increased substantially, further slowing accrual and limiting generalizability of study findings to real-world populations.2 In response to these trends, several multi-stakeholder efforts have sought to modernize eligibility criteria to ensure that more patients can access therapies in development.3–9 These activities focused primarily on reforming approaches to developing clinical trial eligibility criteria. LUNGevity Foundation (LUNGevity), a nonprofit patient advocacy organization committed to increasing quality of life and survivorship of people with lung cancer, formed a Scientific and Clinical Research Roundtable initiative to streamline lung cancer clinical trials. To date, this group has issued two sets of recommendations regarding eligibility criteria.10,11
To address the need for consistency in how clinical trial eligibility criteria are defined and listed in protocols, LUNGevity collaborated with the U.S. Food and Drug Administration (FDA) and the National Cancer Institute (NCI) to address three challenges arising from confusing and inconsistent eligibility criteria in clinical trials for advanced stage non-small cell lung cancer (NSCLC): (1) patients, caregivers and clinicians often face difficulties navigating trial protocols to determine eligibility because publicly available trial search engines do not standardize the listing of inclusion and exclusion criteria; (2) increasingly numerous and stringent eligibility criteria exclude a growing proportion of patients; and (3) heterogeneous study populations render cross-trial comparisons difficult.
Here we present the result of this effort: a prioritized list of recommended terms for inclusion and exclusion criteria in first-line, therapeutic clinical trials for advanced NSCLC that are intended to support marketing application. Now incorporated into a forthcoming draft FDA guidance document, this list may serve as a starting point for investigators and sponsors drafting study protocols. Although specific to lung cancer, this work may serve as a prototype for similar efforts in other cancers.
Recommendation development
Beginning in 2019, experts representing NCI, FDA, LUNGevity, and trial sponsors (Genentech, Janssen, AstraZeneca) developed a baseline eligibility criteria framework for lung cancer clinical trials. Specifically, these individuals identified and prioritized a core library of terms to provide sponsors with a recommended, consistent framework for developing study protocols. By standardizing eligibility criteria wording and order, the group aimed to assist patients and clinicians in evaluating trial enrollment opportunities, support regulatory officials in their work, and encourage trial sponsors to adopt a more consistent approach to eligibility considerations. The resulting recommendations provide the basis for a forthcoming FDA draft Guidance for Industry. The open comment period following issuance of the draft guidance will offer the public an opportunity to provide feedback on these recommendations.
The on-line figure displays the overall process for conceptualizing, developing, and reviewing the eligibility framework. As part of its Scientific and Clinical Research Roundtable, LUNGevity convened a multi-stakeholder working group consisting of four senior leaders from the FDA Oncology Center of Excellence (OCE), four members from the NCI Coordinating Center for Clinical Trials and Cancer Therapy Evaluation Program (CTEP), and three thoracic oncologists involved in cancer clinical trials. Their recommendations were reviewed by three industry sponsors. The core working group consisted of participants from the FDA, NCI, and LUNGevity. To develop recommendations for a standardized approach, the group built upon previous eligibility criteria reform recommendations developed by the ASCO-FOCR-NCI template (applicable to general oncology clinical trials) and lung cancer-specific recommendations developed through the LUNGevity Scientific and Clinical Research Roundtable (SCRT). The recommended ordering of eligibility criteria was based on CTEP trial protocols. For some criteria, language was derived from the ASCO-FOCR-NCI template. Based on feedback from international regulatory authorities (European Medicines Agency (EMA)), clinicians, and industry sponsors, the core working group revised recommendations, which were eventually considered by the FDA to produce draft Guidance.
On-Line Figure.
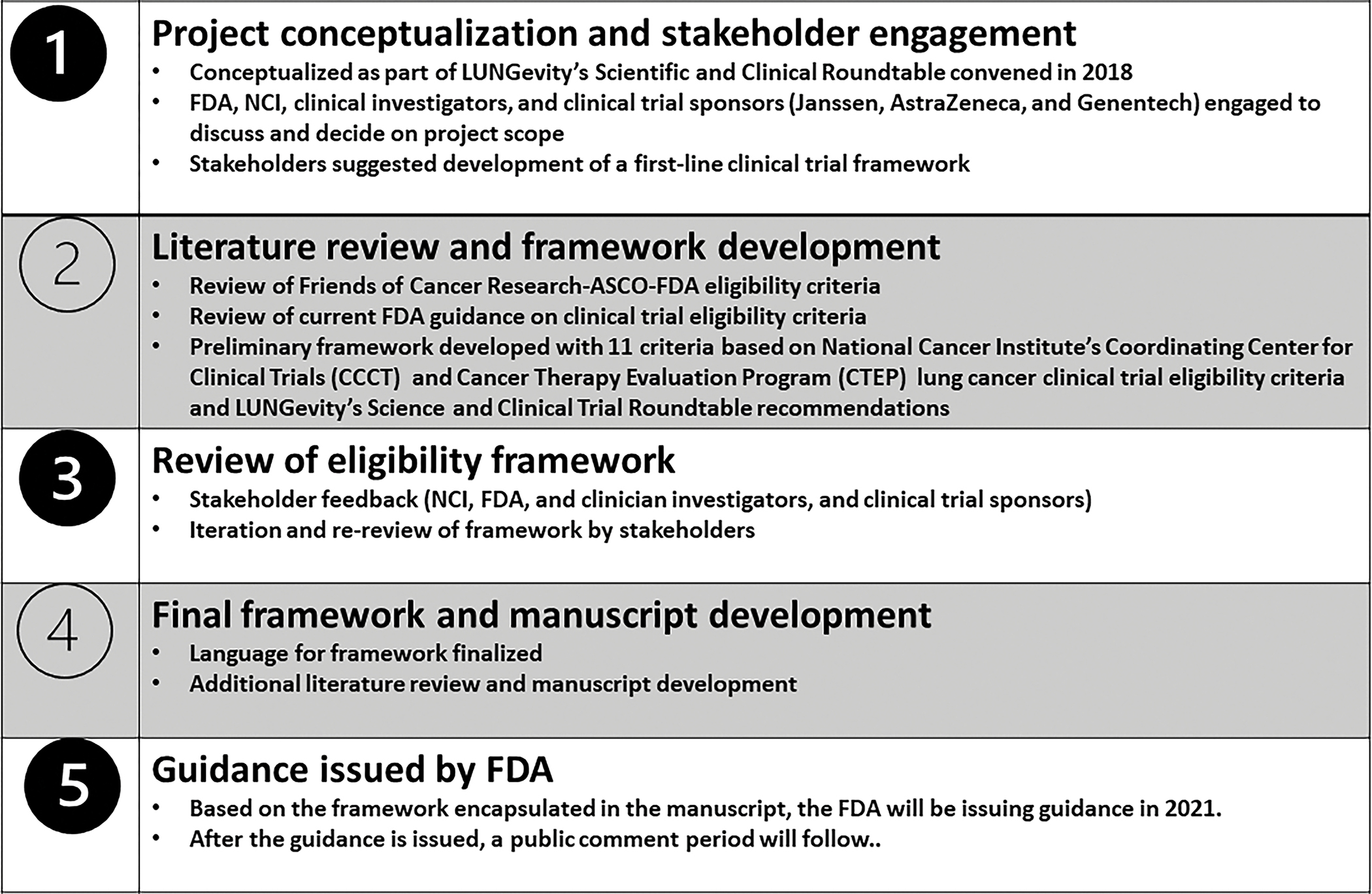
Development process for eligibility framework
Recommendations:
The forthcoming FDA draft Guidance document contains 13 eligibility categories in a recommended order (Table 1). Here we category content, as well as factors considered during their development. While discussion about some categories prompted early and widespread agreement among the experts (such as disease stage), others (such as biomarkers and organ function) featured disparate perspectives.
Table 1:
Library terms/eligibility criteria contained in the forthcoming FDA draft Guidance for Industry, “Eligibility Criteria for Non-Small Cell Lung Cancer Clinical Trials.” d
| Order | Library Term/ Eligibility Criterion | Provisional Recommendations | Considerations and Discussion Points |
|---|---|---|---|
| 1 | Stage and Histology of Disease | Stage IV non-small cell lung cell carcinoma (NSCLC) (includes M1a, M1b, M1c stage disease, American Joint Committee on Cancer [AJCC] 8th edition). | Patients with locally advanced stage IIIB disease not amenable to curative intent therapy may also be considered. Metastatic disease does not need to be demonstrated pathologically. Site of biopsy could be either the primary tumor or a metastatic site. |
| 2 | Biomarker (specific to a targeted agent) | Presence or absence of biomarker must have been appropriately demonstrated | Central performance of biomarker testing that could also be performed at enrolling clinical sites discouraged to (1) avoid unnecessary delays, (2) decrease costs, (3) optimize use of archival tissue. Some working group members also encouraged flexibility regarding source of biologic material (such as peripheral blood instead of tissue) if feasible for the biomarker(s) of interest. |
| 3 | Performance Status | Eastern Cooperative Oncology Group (ECOG) performance status 0–2. | Justification required for exclusion of performance status 2. The working group recognized that in earlier-phase, non-registrational trials, unknown safety profiles of investigational agents may require a more stringent performance status threshold. |
| 4 | Hematological parameters | At time of screening: • Absolute neutrophil count (ANC) ≥ 1500 cells/mL • Platelets ≥ 100,000 cells/mL • Hemoglobin ≥ 8.0 g/dL |
Some working group members encouraged eliminating default recommended threshold values altogether, given differences in relevance and risks according to type of treatment. For instance, for non-cytotoxic treatment regimens not expected to cause myelosuppression (e.g., most molecularly targeted therapy, immunotherapy), lower thresholds may be appropriate. |
| 5 | Brain Metastasis | • Patients with treated/stable brain metastases may be enrolled • Patients with untreated, asymptomatic brain metastasis if low likelihood of needing near-term CNS-directed therapy and CNS activity of study therapy likely may be enrolled • Patients with leptomeningeal disease if low likelihood of needing near-term CNS-directed therapy and CNS activity of study therapy likely may be enrolled |
Definition of stable brain metastases after CNS-directed therapy can be variably interpreted to mean clinical status and/or radiologic findings. Some working group members discouraged requirement to repeat CNS imaging after definitive therapy of brain metastases to (1) prevent further delay, (2) avoid unnecessary radiology procedures, (3) avoid confusion of interpreting near-term imaging studies potentially confounded by treatment effects. |
| 6 | Liver Function | Inclusion of patients with mild to moderate hepatic impairment when supported by available data | In contrast to the FDA guidance document, the LUNGevity working group recommended specific parameters as follows: bilirubin ≤ 1.5 × institutional ULN (except for patients with documented Gilbert’s syndrome), and AST/ALT ≤3 × institutional ULN (≤ 5 × ULN if liver metastases are present). However, there was considerable discussion on this topic, with some participants recommending that specific values not be provided, instead directing investigators and sponsors to base requirements on characteristics of the agent(s) under study. |
| 7 | Kidney Function | The inclusion/exclusion of patients according to renal function should be based on available data | In contrast to the FDA guidance document, the LUNGevity working group recommended a specific threshold of GFR ≥50 mL/min/1.73 m2. As with liver function, there was considerable discussion on this topic, with some participants recommending that specific values not be provided. Some working group members were reluctant to allow enrollment of patients with GFR <30 mL/min/1.73 m2 under any circumstances. |
| 8 | Cardiac Function | • For patients with known or suspected cardiac disease, or history of treatment with cardiotoxic agents, New York Heart Association Functional Classification should be assessed. • Patients with significant clinical cardiac abnormalities should be excluded. |
Some working group members urged caution around the term “significant clinical cardiac abnormalities,” given (1) the prevalence of cardiovascular comorbidities among patients with lung cancer, (2) potential confusion when interpreting, and (3) the possibility that cardiac status is not relevant to the safety or efficacy of study therapy. Instead, these working group members felt that guidance on cardiac function should resemble that on liver and kidney function, which recommends eligibility according to available data. |
| 9 | HIV Infection | Patients with CD4+ T-cell counts ≥350 cells/μL should generally be considered eligible. | HIV testing should generally not be required during eligibility screening. |
| 10 | Chronic HBV infection and/or history of HCV infection | • For HBV infection, patients should be on suppressive antiviral therapy prior to initiation of cancer therapy • For history of HCV infection, patients should have completed (or be on concurrent) curative antiviral treatment and have undetectable HCV viral load |
Some working group members raised concerns that requiring undetectable HCV viral load might exclude patients who would otherwise tolerate and potentially benefit from therapy. They noted the relatively high prevalence of chronic HCV and clinical experience suggesting feasibility of treating these individuals with a variety of systemic therapies. In general, the group felt that HBV/HCV testing requirement could be limited to agents for which clinically relevant. |
| 11 | Pneumonitis | • Patients with resolved pulmonary infections or radiation pneumonitis should be included • Eligibility of patients with chronic interstitial lung disease should be discussed |
This criterion raised considerable discussion among working group members. Points raised included the following: (1) “pneumonitis” may be an overly-broad term, particularly if applied to prior acute infections; (2) the term “pneumonitis” may be included on source documents, such as radiology reports, in the absence of a clinical syndrome; (3) pulmonary pathophysiology may be relevant to only a subset of medical cancer therapies such as immune checkpoint inhibitors and certain molecularly targeted therapies. |
| 12 | Other | Criteria specific to the investigational agent and/or mechanism of action. Examples include the following: • Metabolic panels (based on the mechanism and metabolism of the study drug) • Unique safety issues related to the mechanism of action of the therapy under study (e.g., bleeding/clotting for antiangiogenic therapies; active autoimmune disease for immunotherapy; active infections for cytotoxic therapy. • Drug-drug interactions |
Working group members recognized that investigational agents have highly diverse safety and dosing considerations. Because many of these may apply only to a small subset of therapies, it was recommended to place these criteria in a miscellaneous category and require investigators and sponsors to draft trial-specific eligibility criteria. |
| 13 | Prior or concurrent malignancy | • Include patients with prior or concurrent malignancy whose natural history or treatment does not have the potential to interfere with the safety or efficacy assessment of the investigational agent | Some working group members raised concern that the terminology “… does not have the potential to interfere …” may be overly restrictive, as it is rarely possible to rule out entirely potential events in clinical medicine. |
1. Disease stage:
A protocol’s first eligibility criterion should address disease stage and histology. The current LUNGevity working group and associated FDA draft guidance focus specifically on advanced (stage 4) NSCLC.
2. Biomarkers:
In developing this recommendation, working group participants discussed whether and how to address both required biomarker results and the test/process required to achieve it. Clinicians supported allowing locally performed testing when available, as such an approach might save time, effort, and money. They also encouraged flexibility regarding of the type of biospecimen, such as allowing results from peripheral blood testing (e.g., cell-free DNA) to identify oncogenic alterations associated with FDA-approved therapies.
Industry representatives requested the inclusion of more detail about biomarker measurements to ensure adequate rigor of testing oversight. For instance, Clinical Laboratory Improvement Amendments (CLIA)-regulated biomarker assay results are currently accepted under “enforcement discretion”—a term the FDA applies when choosing not to enforce requirements because it has determined that the risk to patients is low—if the assay is performed prior to study screening.12,13 However, if the same tests are intended to be used as part of the study screening process, an Investigational Device Exemption (IDE) application is required (and rigor of validation is expected per FDA requirements) for biomarkers associated with new molecular entities (NMEs).14 As a result of these factors, the working group indicated that use of approved companion diagnostics for patient screening, followed by central lab confirmation, may be sufficient for established biomarkers.
Because this remains an area of ongoing discussion, the current recommendations state the need for biomarker testing in lung cancer clinical trials but include relatively general language about biomarker testing requirements.
3. Performance Status
Because more cancer treatments with relatively limited toxicity profiles are being developed, clinician working group participants advocated for more frequent inclusion of patients with Eastern Cooperative Oncology Group (ECOG) performance status of 2.15 Industry participants raised concerns about potential performance status shift: a phenomenon that can occur when motivated clinicians seeking to enroll a patient on a trial might perceive and document a more favorable performance status to meet eligibility requirements. 16,17 Such a tendency could result in worse trial outcomes and potentially jeopardize the overall success of the trial.
Discussion also focused on the distinction between early-phase trials (in which it may be riskier to include more symptomatic patients, as less is known about the therapeutic agent(s) under study) and registration trials (the focus of the FDA guidance). Ultimately, the group agreed on a baseline recommendation of including ECOG performance status 0–2, with justification required for excluding performance status 2.
4. Hematological Parameters
There was extensive discussion regarding the inclusion of specific values in the baseline recommendation. Some clinicians proposed removing values altogether, instead recommending that investigators and sponsors select thresholds according to the known safety profile of the agent(s) under study. For instance, cytotoxic chemotherapy would be highly likely to result in cytopenias, so minimum blood counts would be a relevant consideration to ensure safety. Conversely, myelosuppression is extremely rare with immune checkpoint inhibitors, so lower pre-treatment hematologic parameters might be acceptable, if needed at all.18 Although the group ultimately included specific values as a starting point, participants stressed the importance of flexibility and the allowance of blood product transfusions if needed for a patient to meet a required threshold.
5. Brain metastases
For eligibility regarding brain metastases, the working group considered language from earlier FDA guidance documents.19,20 Clinician/investigator participants encouraged modeling criteria on widespread clinical practice, such as (1) not requiring pre-trial treatment of small and/or asymptomatic brain metastases; (2) not requiring confirmatory imaging after treatment of brain metastases; and (3) adjusting washout periods according to the tolerability and toxicity of brain metastasis treatment (such as a considerably shorter washout period after stereotactic radiosurgery than for whole brain radiation therapy).
Sponsors indicated the importance of relying upon clinical judgment and considering the type of mechanism of action of the agent under study. For instance, patients with untreated brain metastases might only be allowed in studies of agents expected to have a high degree of central nervous system penetration. Participants also noted that some therapies may control brain metastases without directly reaching that site,21 as may be the case with immune checkpoint inhibitors.
6. Liver function
As with hematologic parameters, there were diverse views about whether to include specific values in the recommended baseline language for organ function. Clinicians proposed omitting specific values, instead encouraging establishing minimum thresholds based on properties of the study therapy.
The working group acknowledged that eligibility criteria focused on isolated AST and/or ALT elevations (typically ≥2.5 times the institutional upper limit of normal (ULN) and occasionally ≥1.5 × ULN11) may result in exclusion of patients with adequate liver function because transaminase levels do not provide a complete picture of liver function, particularly drug metabolic capabilities. The group suggested using thresholds of bilirubin ≤ 1.5 × institutional ULN (except for patients with documented Gilbert’s syndrome), and AST/ALT ≤3 × institutional ULN for (≤ 5 × ULN if liver metastases are present). The group also supported the inclusion of patients with mild to moderate hepatic functional impairment when data supporting safety is available.
In contrast to working group recommendations, the draft FDA guidance does not contain specific threshold values for hepatic function, instead noting that patients with mild to moderate hepatic impairment may be included if available data suggest that doing so would not convey unreasonable risk. The guidance also acknowledges that patients with substantial elevations in AST and ALT (up to 20x ULN [grade 3 by NCI CTCAE]) may be asymptomatic and tolerate standard doses of many treatments.
7. Kidney function
For kidney function, sponsors noted the potential for variability across study sites depending on the geographic region, approach to measurement, and population under study. In cases where study therapy is not expected to cause renal toxicity and kidney function does not affect study therapy metabolism, the working group encouraged adoption of the most permissive level of kidney function based on prior clinical experience with the agent, including levels below institutional reference range. Ultimately, the LUNGevity working group proposed a threshold of GFR ≥50 mL/min/1.73 m2. By contrast, as with hepatic function, the draft FDA guidance does not include specific parameters, instead recommending that eligibility of patients according to renal function should be based on available data related to the agent(s) under investigation.
8. Cardiac function
For patients with known history or current symptoms of cardiac disease, or prior receipt of cardiotoxic agents, the working group and draft FDA guidance recommend an eligibility threshold of New York Heart Association (NYHA) Classification 2 (mild symptoms, slight limitation during ordinary activity) or better.22 The draft FDA guidance also recommends excluding patients with “significant clinical cardiac abnormalities,” although some working group members raised concerns that such wording could lead to confusion, particularly given the prevalence of cardiovascular comorbidities in lung cancer populations.23
9. HIV
10. HBV and HCV
For both HIV and viral hepatitis, the working group agreed that testing should only be included among study screening procedures if clinically relevant for the agent under study. Although recent FDA guidance recommends broad inclusion of patients with HIV (including those with CD4 count <350/μL for potential curable cancers or if the study drug has shown promise in earlier-phase trials),6 sponsor participants suggested a more conservative approach. Specific recommendations included requiring patients to be receiving highly active retroviral therapy, CD4 count ≥350/μL, and undetectable viral load.6
For viral hepatitis, clinician participants encouraged consideration of patients with detectable hepatitis B or C if (1) liver chemistries meet study requirements, and (2) study therapy is not expected to reactivate the virus. They also noted that, while multiple expert organizations recommend initiating antiviral therapy for hepatitis B prior to or simultaneous with anti-cancer therapy, none recommends achieving an undetectable viral load before starting cancer treatment.24
11. Pneumonitis
The inclusion of pulmonary disease in the eligibility criteria framework raised considerable discussion within the working group. All participants recognized the relevance of interstitial lung disease, chronic supplemental oxygen dependence, or pulmonary fibrosis to immune checkpoint inhibitors and selected other cancer therapies (such as brigatinib). However, because most cytotoxic agents and molecularly targeted therapies are not associated with pneumonitis or other pulmonary toxicity, clinicians suggested these eligibility considerations be placed in the “other” category to avoid a circumstance where trial protocol developers decide to exclude these conditions by default. Clinician participants also noted that radiology reports from chest imaging may include terms such as “pneumonitis” or “fibrosis” in patients without clinical lung disease, particularly after radiation therapy.11
12. Other
Recognizing that clinical trials will have inclusion/exclusion criteria specifically related to the investigational agent(s), the working group proposed that these fall under an “other” category. Examples considered by the group included the following: reproductive status; autoimmune disease for immunotherapy; bleeding/clotting for antiangiogenic therapies; active infection for cytotoxic/immunosuppressive therapies; and drug-drug interactions. Some working group participants urged caution regarding concomitant medication-related eligibility (e.g., drug-drug interactions, QTc prolongation risk) given the frequency and unclear clinical significance of these issues in clinical practice.25,26
13. Prior or concurrent malignancy
Although not covered in the initial LUNGevity working group recommendations, the draft FDA guidance recommends including patients with prior or concurrent malignancy whose natural history or treatment does not have the potential to interfere with the safety or efficacy assessment of the investigational agent. This suggestion marks a clear departure from earlier approaches to prior cancers, which may not adversely affect clinical outcomes but were previously broadly excluded from lung cancer clinical trials.27,28
Discussion:
Patients, clinicians, and regulators struggle to evaluate trials when inclusion/exclusion criteria are difficult to understand, assess, and compare. To address this challenge, our multi-stakeholder group developed a framework for standardizing the approach to defining and presenting trial protocol eligibility criteria. The process involved leveraging prior efforts to reform clinical trial eligibility criteria (including expanding eligibility by eliminating overly restrictive criteria) and rigorous consensus-building steps through multiple meetings focused on definition and presentation of criteria involving regulators, clinicians, and clinical trial sponsors.
This effort complements and is distinct from prior work because it addresses diverse categories of eligibility criteria; incorporates international input from regulatory authorities, sponsors, investigators, and patient advocacy organizations; seeks to create a common approach to presenting eligibility criteria; focuses on a specific clinical scenario (first-line systemic treatment of advanced NSCLC); has led to regulatory recommendations in the form of a forthcoming draft FDA guidance for industry; and will eventually reflect input from the general public, as provided during the upcoming open comment period. It is hoped that the FDA’s interest in addressing these topics will prompt investigators and sponsors to evaluate study protocols critically and with an eye toward standardization of eligibility criteria, ultimately leading to trials that are easier to evaluate and compare. While guidance documents represent the FDA’s current thinking on a topic, they do not create or confer any rights for or on any person, and they do not operate to bind FDA or the public. However, guidance documents may provide a starting point for sponsors to consider when designing clinical trials.29
Standardizing eligibility criteria on public-facing websites such as clinicaltrials.gov may simplify searches by patients or referring clinicians. A uniform framework might also enhance the ability to perform cross-trial evaluations. As a next step, some working group participants expressed an interested in developing an automated web-based platform for developing a clinical trial protocol. With such a tool, investigators and sponsors could rely on a dropdown menu of items listed in the framework to populate a protocol, having opportunity to justify deviation from the proposed language.
The efforts described here provide a “case study” in lung cancer, an approach that could eventually be undertaken in other malignancies. Although representing diverse stakeholder perspectives, by necessity the process to date has involved a relatively small number of participants. However, the upcoming comment period will offer the broader public an opportunity to weigh in on the draft FDA recommendations. During this time, all categories of input are welcome, ranging from addition or removal of criteria, to revision of suggested parameters, to alternative assessment approaches (such as use of validated instruments that correlate with fitness, toxicity, and outcomes to evaluate performance status30,31).
Clinical trial eligibility harmonization needs to strike a balance between being too specific (and therefore not replicable in another disease space) and overly general (thus not providing clear items that can be populated). Nor must it hinder critical discussion among trial investigators and sponsors. The selection and order of items provided in the presented recommendation is not intended to be prescriptive. Even among the relatively small number of participants in the working group process, perspectives and recommendations differed widely. We fully expect this guidance to serve as a starting point for protocol development and to evolve with experience over time.
Acknowledgements:
The authors are grateful to Gisele Sarosy, MD, Andrea Denicoff, RN, MS, ANP, Shakuntala Malik, MD, and Sheila Prindiville, MD, MPH, from the NCI for their participation in the Working Group and feedback in the development of the template, and Drs. See Phan and Barbara Gitlitz (Genentech), Dr. Nabil Chehab (AstraZeneca), and Dr. Troy Sarich (Janssen) for their feedback on the eligibility template.
References:
- 1.Tang C, Sherman SI, Price M, et al. Clinical Trial Characteristics and Barriers to Participant Accrual: The MD Anderson Cancer Center Experience over 30 years, a Historical Foundation for Trial Improvement. Clin Cancer Res. 2017;23(6):1414–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia S, Bisen A, Yan J, et al. Thoracic Oncology Clinical Trial Eligibility Criteria and Requirements Continue to Increase in Number and Complexity. J Thorac Oncol. 2017;12(10):1489–1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim ES, Bruinooge SS, Roberts S, et al. Broadening Eligibility Criteria to Make Clinical Trials More Representative: American Society of Clinical Oncology and Friends of Cancer Research Joint Research Statement. J Clin Oncol. 2017;35(33):3737–3744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.FDA. US Food and Drug Administration. Guidance for Industry: Considerations for the Inclusion of Adolescent Patients in Adult Oncology Clinical Trials Guidance for Industry. In:2019. [Google Scholar]
- 5.FDA. US Food and Drug Administration. Draft Guidance: Cancer Clinical Trial Eligibility Criteria: Patients with Organ Dysfunction or Prior or Concurrent Malignancies Guidance for Industry. In:2019. [Google Scholar]
- 6.FDA. US Food and Drug Administration. Draft Guidance: Cancer Clinical Trial Eligibility Criteria: Patients with HIV, Hepatitis B Virus, or Hepatitis C Virus Infections Guidance for Industry. In:2019. [Google Scholar]
- 7.FDA. US Food and Drug Administration. Draft Guidance: Cancer Clinical Trial Eligibility Criteria: Brain Metastases Guidance for Industry; In:2019. [Google Scholar]
- 8.FDA. US Food and Drug Administration. Draft Guidance: Cancer Clinical Trial Eligibility Criteria: Minimum Age for Pediatric Patients Guidance for Industry. In:2019. [Google Scholar]
- 9.Osarogiagbon RU, Vega DM, Fashoyin-Aje L, et al. Modernizing Clinical Trial Eligibility Criteria: Recommendations of the ASCO-Friends of Cancer Research Prior Therapies Work Group. Clin Cancer Res. 2021;27(9):2408–2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonomi P, Blumenthal G, Ferris AS, et al. Making Lung Cancer Clinical Trials More Inclusive: Recommendations for Expanding Eligibility Criteria. J Thorac Oncol. 2018;13(6):748–751. [DOI] [PubMed] [Google Scholar]
- 11.Forde PM, Bonomi P, Shaw A, et al. Expanding Access to Lung Cancer Clinical Trials by Reducing the Use of Restrictive Exclusion Criteria: Perspectives of a Multistakeholder Working Group. Clin Lung Cancer. 2020;21(4):295–307. [DOI] [PubMed] [Google Scholar]
- 12.FDA. Webinar - Clinical Laboratory Improvement Amendments (CLIA) Waiver Applications Final Guidances. In. Silver Springs, MD, USA: US Food and Drug Administration; 2020. [Google Scholar]
- 13.FDA. US Food and Drug Administration. Guidance for Industry: Framework for Regulatory Oversight of 8 Laboratory Developed Tests (LDTs). In:2014. [Google Scholar]
- 14.FDA. SUBCHAPTER H--MEDICAL DEVICES, PART 812 INVESTIGATIONAL DEVICE EXEMPTIONS. In: SERVICES DOHAH, ed. Silver Springs, MD, USA: US Food and Drug Administration; 2019. [Google Scholar]
- 15.Neeman E, Gresham G, Ovasapians N, et al. Comparing Physician and Nurse Eastern Cooperative Oncology Group Performance Status (ECOG-PS) Ratings as Predictors of Clinical Outcomes in Patients with Cancer. Oncologist. 2019;24(12):e1460–e1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320(7233):469–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow R, Chiu N, Bruera E, et al. Inter-rater reliability in performance status assessment among health care professionals: a systematic review. Ann Palliat Med. 2016;5(2):83–92. [DOI] [PubMed] [Google Scholar]
- 18.Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2016;375(19):1823–1833. [DOI] [PubMed] [Google Scholar]
- 19.FDA. Cancer Clinical Trial Eligibility Criteria: Brain Metastases Guidance for Industry. https://www.fda.gov/media/121317/download. Published 2020. Accessed September 5, 2020.
- 20.FDA. US Food and Drug Administration. Draft Guidance: Evaluating Cancer Drugs in Patients with Central Nervous System Metastases Guidance for Industry. In:2020. [Google Scholar]
- 21.Berghoff AS, Venur VA, Preusser M, Ahluwalia MS. Immune Checkpoint Inhibitors in Brain Metastases: From Biology to Treatment. Am Soc Clin Oncol Educ Book. 2016;35:e116–122. [DOI] [PubMed] [Google Scholar]
- 22.AHA. Classes of Heart Failure. https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/classes-of-heart-failure. Published 2017. Accessed October 10, 2020.
- 23.Ahn DH, Mehta N, Yorio JT, Xie Y, Yan J, Gerber DE. Influence of medical comorbidities on the presentation and outcomes of stage I-III non-small-cell lung cancer. Clin Lung Cancer. 2013;14(6):644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hwang JP, Feld JJ, Hammond SP, et al. Hepatitis B Virus Screening and Management for Patients With Cancer Prior to Therapy: ASCO Provisional Clinical Opinion Update. J Clin Oncol. 2020;38(31):3698–3715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Le T, Yang H, Rashdan S, et al. QTc Interval-Prolonging Medications Among Patients With Lung Cancer: Implications for Clinical Trial Eligibility and Clinical Care. Clin Lung Cancer. 2020;21(1):21–27 e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rashdan S, Yang H, Le T, Selby C, Gerber DE, Alvarez CA . Prevalence and Significance of Potential Pharmacokinetic Drug-Drug Interactions Among Patients with Lung Cancer: Implications for Clinical Trials. Clin Drug Investig. 2021;41(2):161–167. [DOI] [PubMed] [Google Scholar]
- 27.Gerber DE, Laccetti AL, Xuan L, Halm EA, Pruitt SL. Impact of prior cancer on eligibility for lung cancer clinical trials. J Natl Cancer Inst. 2014;106(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Laccetti AL, Pruitt SL, Xuan L, Halm EA, Gerber DE. Effect of prior cancer on outcomes in advanced lung cancer: implications for clinical trial eligibility and accrual. J Natl Cancer Inst. 2015;107(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.FDA. US Food and Drug Administration Guidances. https://www.fda.gov/industry/fda-basics-industry/guidances. Published 2021. Accessed.
- 30.Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol. 2011;29(25):3457–3465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer. 2012;118(13):3377–3386. [DOI] [PubMed] [Google Scholar]


