Abstract
With the extensive use of mobile phones globally, some people engage in excessive or problematic phone use behaviors. However, little is known regarding the latent structure of problematic mobile phone use. The current study employed the Chinese versions of the Nomophobia Questionnaire, Mobile Phone Addiction Tendency Scale, and Depression-Anxiety-Stress Scale-21 to explore the latent psychological structure of problematic mobile phone use and nomophobia and their associations with mental health symptoms. Results showed that a bifactor latent model best fit nomophobia, which contained a general factor and four unique factors involving the fear of being unable to access information, losing convenience, losing contact, and losing one’s Internet connection. Results also showed significant correlations among latent factors of nomophobia, problematic mobile phone use, and mental health symptoms. Through these findings, we can conclude that two problematic mobile phone use behaviors share a common factor concerning excessive use, and nomophobia has independent unique factors concerning usable function. This study clarifies the structure of problematic mobile phone use, and it implies that we can distinguish problematic mobile phone use from functional use; further investigation of problematic mobile phone use is warranted.
Keywords: Bifactor model, High-order CFA, Problematic mobile phone use, Nomophobia, Mental health
Introduction
In contemporary times, mobile phones have become the most important and commonly used devices for people around the world (Poushter et al., 2018). According to data from Statista, there were 6.92 billion smartphone users globally as of 2022, which is approximately 86.41% of the global population. Mobile phones are so popular among users because they provide convenience to daily life, including communicating with families at any place and time, paying online, listening to music, taking photographs, watching movies, playing games, editing documents, getting medical services, and much more (Sun et al., 2022). There are, however, some negative effects of mobile phones, such as wasting daily time, impairing concentration, and thus reducing performance by inducing task-irrelevant thoughts and mind wandering (Kates et al., 2018; Soror et al., 2015). Even more, for some individuals, excessive mobile phone use is a substantial problem with serious adverse consequences. In particular, problematic mobile phone use and nomophobia have been discussed (Bartwal & Nath, 2019; Billieux et al., 2015).
Problematic Mobile Phone Use
Early researchers conceptualized problematic mobile phone use (PMPU) as an addictive behavior, also known as “smartphone addiction” and “smartphone use disorder” (Kardefelt-Winther, 2014; Lachmann et al., 2018). This concept was defined as the symptoms of addiction associated with excessive mobile phone use, such as tolerance, withdrawal, and loss of control (Su et al., 2014; Harris et al., 2020). These symptoms matched the criteria for internet gaming disorder (IGD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) fifth edition. However, some researchers believed that excessive use of technology should be characterized as problematic use (Bianchi & Phillips, 2005; Liu et al., 2022) rather than addiction in order to not over-pathologize everyday behaviors. Therefore, it has been commonly accepted that PMPU more recently, while distressing for some people, is not an addictive behavior (Panova & Carbonell, 2018), nor is it considered a diagnosis in the DSM-5 or ICD-11. Therefore, PMPU is defined as psychological dependence on an individual’s mobile phone that can result in compulsive or improper use behavior and affects daily lives (Liu et al., 2022; Bartwal & Nath, 2019; Park & Lee, 2011). Nonetheless, for some individuals PMPU can result in dangerous health consequences such as traffic accidents (Delgado et al., 2016), physical pain (Lee et al., 2015), and sleep problems (Sahin et al., 2013).
Nomophobia
In recent years, a newer PMPU-related notion, nomophobia, has been proposed and widely studied (Kaviani et al., 2020), due to the introduction of the fear of missing out (FOMO) construct (Elhai et al., 2020b). Although PMPU and nomophobia have some behavioral similarities, such as excessive mobile phone usage, their basic psychological concepts are different (Tran, 2016; Ren et al., 2021). PMPU highlights the physical, mental, and social dysfunction resulting from excessive mobile phone use (De-Sola Gutierrez et al., 2016; Lu et al., 2021), while nomophobia is defined as distress or anxiety when losing access to one’s mobile phone, for example from battery drain or inability to use while in class (Rodriguez-Garcia et al., 2020), and it is a by-product of emerging technologies in the 21st century (King et al., 2013). Studies showed that nomophobia was more common among college students (King et al., 2014). Furthermore, nomophobia is associated with numerous problems for some individuals, such as physical pain (Gao et al., 2020) and mental health symptoms (Rahme et al., 2021), including anxiety (Kara et al., 2021) and depression (Copaja-Corzo et al., 2022). Therefore, nomophobia is an important construct worth investigating.
There is an abundance of research focused on the impact of nomophobia. However, little data exist on the latent symptom structure of nomophobia, and results are inconsistent. To date, most research on nomophobia has supported a four-factor structure involving the inability to access information, inability to communicate, losing connectedness, and giving up convenience, initially proposed by Yildirim and Correia (2015). In addition, the Pakistani and Turkish versions of the Nomophobia Questionnaire both supported this four-factor structure (Nawaz et al., 2017; Yildirim et al., 2016). Also, in China, a revised version of this scale yielded adequate fit for the four-factor model (Ren et al., 2020). However, when Adawi and his colleagues (2019) translated this scale into Italian, they found three factors through exploratory factor analysis: not being able to access information, not being able to communicate, and a single factor merging convenience and losing connectedness. Yet commonalities between four factors can be found in these and many other studies. For example, Ma and Liu’s study (2018) showed that the correlations nomophobia factors were higher than 0.5. These findings implied that the structure of nomophobia had not been well-defined in previous studies, prompting us to further investigate its structure.
In a systematic review article, Kamolthip and his colleagues (2022) argued that mobile phone users should be divided into two groups: adaptable or functional users, and problematic users. Adaptive (functional) users use mobile phones for a variety of reasons in a normal time range, including communication and socializing. However, problematic users use their phones in ways that are out of control and unhealthy, spending a lot of time online (such as excessive gaming or online shopping) feeling unable to stop using, even if their bodies are uncomfortable. It suggests that mobile phone dependency is triggered not only by the exhibition of problematic mobile phone use (Chen et al., 2020; Pancani et al., 2020), but also by the functional use of mobile phones (Van Deursen et al., 2015). However, existing research on nomophobia did not differentiate between problematic and functional mobile phone use. In other words, nomophobia was treated as pure problematic mobile phone use by ignoring its functional use features. Consequently, it might lead to an exaggeration of the impact of problematic mobile phone use. Moreover, it was impossible to directly distinguish problematic use features and functional use features when nomophobia has been measured as a manifest variable. Therefore, he latent variable method could provide a possible solution.
The Relationship Between PMPU, Nomophobia and Mental Health Symptoms
Despite the fact that both PMPU and nomophobia belong to the category of problematic mobile phone use, we found significant differences between them according to their basic definition and typical symptoms (Tran, 2016; Luo et al., 2021). Typical symptoms of PMPU are withdrawal symptoms, salience, social comfort, and mood changes (Su et al., 2014; Chen et al., 2017), while typical manifestations of nomophobia include fear of being unable to access information, losing convenience, losing contact, and losing connection to the internet (Yildirim & Correia, 2015; Ren et al., 2020). Notably, these symptoms of nomophobia are all relevant to the functional context of the mobile phone. In addition, PMPU emphasizes the health and social impairments caused by problematic use of mobile phones (De-Sola Gutierrez et al., 2016; Lu et al., 2021), whereas nomophobia highlights a pathological fear and anxiety when people lose phone access (Rodriguez-Garcia et al., 2020; Ren et al., 2020). Thus, there seem to be some commonalities, as well as differences, between PMPU and nomophobia. This prompts us to more comprehensively explore their relationship.
Although PMPU and nomophobia are unique, they are both similarly related to mental health symptoms. PMPU is related to symptoms of depression (Chen et al., 2019), anxiety (Elhai et al., 2019a; Zhang et al., 2018), stress (Liu et al., 2018), and low self-esteem (Elhai et al., 2019b). Similarly, nomophobia has shown relations with mental health symptoms. For instance, Kara et al. (2019) discovered individuals with a higher level of nomophobia had greater loneliness and anxiety. Tams et al. (2018) also found that individuals with a higher level of nomophobia had higher stress scores.
However, we do not mean to suggest that mobile phone use will necessarily exacerbate negative emotions and mental health issues. Some researchers discovered that mobile phone use could also relive negative moods, such as in the Interaction of Person-Affect-Cognition-Execution (I-PACE) model. The I-PACE model (Brand et al., 2016) describes the psychological and neurobiological processes underlying the development and maintenance of problematic mobile phone use, and it is the most commonly accepted theoretical framework for modelling PMPU and nomophobia (Dempsey et al., 2019). It is proposed that a person’s specific problematic mobile phone use would be interactively influenced by their core characteristics, perception of external and internal triggers, affective and cognitive responses, and internet use decisions (Brand et al., 2019). Notably, the I-PACE model also claimed that there were some negative consequences but also some positive impacts on daily life from internet and mobile phones. The theory reviewed a great number of articles on the relationship between mobile phone use and mental health symptoms and concluded that some mobile phone use (e.g., playing an online game, communicating with relatives, and listening to music) might lead to feelings of gratification or relief from negative emotions (Laier & Brand, 2017; Kuss et al., 2018; Laier et al., 2018), while if a person is dependent on their mobile phones for a long period of time (Wegmann et al., 2018), he or she is more likely to suffer from more negative mental health symptoms (e.g., depression, anxiety, and stress in this study). It can be found that the relationship between PMPU, nomophobia, and negative mood or mental health symptoms was inconsistent based on the aforementioned literature, and thus it needed to be investigated further.
Presentation of Issues
According to the literature review above, we found that there are still several gaps in the literature that remain unexplored. First, the structure of nomophobia has not been well defined in previous studies. Previous studies have not distinguished the difference between problematic mobile use and functional mobile phone use. These mixed findings would lead us to have a misunderstanding of nomophobia. Thus, it prompted us to comprehensively explore the structure of nomophobia. In addition, the structure of nomophobia is not well defined, leading to an unclear relationship with PMPU. Third, current research indicates that mobile phone use might both alleviate or aggravate negative mental health symptoms. Such inconsistent findings are due to the fact that the previous studies failed to differentiate between problematic and functional mobile phone use. It indicates that the relationship between PMPU, nomophobia, and mental health symptoms is unclear. We needed to further investigate the latent psychological structures among them.
Therefore, the current study examines two issues: the latent structure of nomophobia and the association among PMPU, nomophobia, and mental health symptoms. Consequently, the following article is organized as two studies. Study 1 compared higher-order and bifactor models on the basis of confirmatory factor analysis (CFA) in order to further explore the structure of nomophobia, which was the novelty of this study. Study 2 examines the latent associations between PMPU, nomophobia, anxiety, depression, and stress by using a structural equation model (SEM). It was hypothesized that (1) nomophobia is not a conventional first-order CFA structure and it might fit a bifactor model including a factor concerning problematic mobile phone use and some factors regarding functional mobile phone use (2) there would be a positive association between problematic mobile phone use and mental health symptoms, rather than with functional mobile phone use.
Method
Participants
We recruited 945 participants to complete an 8-10-minute survey through online and paper-pencil questionnaires in 2019, prior to the outbreak of COVID-19. All participants were college students and graduate students in Tianjin, a large city in China. We administered paper-and-pencil measures to 90 persons at a time. We also used the Wen Juan Xing App (http://www.wjx.cn/) to complete online surveys for other participants outside the classroom. Participant consent was required. In our study, one participant was deemed invalid and deleted due to a lack of response to more than 20 items. And 37 participants were also deleted because their grades were higher than a master’s degree or missing. y Finally, the sample comprised 907 participants, which included 312 men (34.40%) and 595 women (65.60%). Age ranged from 19 to 26 years (M = 20.175, SD = 1.966). The participants provided their written informed consent to participate in this study.
Before data analysis, three measurement invariance tests on nomophobia were conducted. Firstly, a measurement invariance test between males and females was supported by a multi-group CFA. In the meantime, two measurement invariance tests-a two-group CFA and a three-group CFA-were conducted across different ages. Results supported measurement invariance. Measurement invariance tests indicated that neither gender nor age would influence the construct of nomophobia. Additionally, because gender and age effects on nomophobia were not central to this paper’s research purpose, we do not discuss this issue further in the paper. It is shown in the “Appendix” section of this paper. Besides that, the formula for calculating sampling error was used to calculate the sampling error of each variable:
 |
Finally, results showed that the sampling error of variables in our study ranged from 0.007 to 0.045 for a 95% confidence level.
Measures
Chinese Version of the Nomophobia Scale
Ren et al. (2020) formed a Chinese version of the Nomophobia Scale (NMP-C) by using exploratory structural equation modelling (ESEM) and item response theory model (IRT) based on the Nomophobia Questionnaire of Yildirim and Correia (2015). The NMP-C contains four dimensions, including the fear of being unable to access information, losing convenience, losing contact, and losing connection to the internet. The scale consists of 16 items in total, with 4 items in each dimension. An example item is “I would feel anxious without checking in on my QQ, WeChat, and email through my smartphone.” It is scored using a 7-point Likert scale, ranging from 1 (“Not at all”) to 7 (“Completely in conformity with”), and a higher score indicates a higher level of nomophobia. The scale has good reliability and validity (Ren et al., 2020). Cronbach’s α for the whole scale was 0.948 and for the four dimensions ranged from 0.834 to 0.915 in this study. The coefficient ω for the whole scale was 0.948 and the ωs for the four dimensions ranged from 0.836 to 0.915 in this study. The reliability of the NMP-C scale was good.
Mobile Phone Addiction Tendency Scale
The Chinese Mobile Phone Addiction Tendency Scale (MPATS) was developed by Xiong et al. (2012). It is the most widely cited scale to measure the PMPU of Chinese participants (Jiang & Bai, 2014; Ye et al., 2017; Liu et al., 2022). The MPATS is composed of 16 items and four factors/subscales, including withdrawal symptoms (6 items), salience (4 items), social comfort (3 items), and mood changes (3 items). An example item is “I often have the illusion that my phone is ringing or vibrating.” The MPATS uses a 5-point Likert scale, ranging from 1 (“Extremely inconsistent”) to 5 (“Extremely consistent”), and higher scores indicate higher levels of PMPU. Cronbach’s α of the whole scale was 0.900 and the four dimensions ranged from 0.568 to 0.829 in this study. And the coefficient ω for the whole scale was 0.900 and the ωs for the four dimensions ranged from 0.594 to 0.834 in this study. The reliability of the MPATS was good.
Depression, Anxiety, and Stress Scale
The Depression-Anxiety-Stress Scale (DASS) was developed by Lovibond and Lovibond (1995), along with a short version (DASS-21). The DASS-21 is a widely cited scale that contains three subscales (Li et al., 2022; Wang et al., 2020), including depression, anxiety, and stress. The scale consists of 21 items in total, with 7 items in each dimension. An example item is “I feel depressed and frustrated.” The DASS-21 uses a 4-point Likert scale, ranging from 1 (“Did not apply to me at all”) to 4 (“Applied to me very much”). In this study, we used the Chinese version (Lu et al., 2020), which is reliable and valid. Cronbach’s α of the whole scale was 0.910 and Cronbach’s α of four dimensions ranged from 0.752 to 0.835 in this study. The coefficient ω of the whole scale was 0.912 and the ωs of four dimensions ranged from 0.754 to 0.833 in this study.
Software and Statistical Methods
SPSS 25.0 was used in this study for data preprocessing and reliability analysis. Mplus 8.0 was used to conduct bifactor and structural equation modelling (SEM). All variables were treated as continuous variables, and mean substitution was used to impute missing data. The skewness of all items in three scales ranged from − 0.630 to 1.918 (SE = 0.081), and item kurtosis ranged from − 1.269 to 3.824 (SE = 0.162). Maximum likelihood parameter estimates with standard errors and a mean-adjusted chi-square test statistic (MLM) were used, since the data were non-normally distributed. In SEM, we used a Pearson covariance matrix with linear regression for factor and path coefficients, to explore relationships among nomophobia, PMPU and mental health symptoms.
In the CFA model, factors that are directly connected to the indicators or items are called first-order factors. Above the first-order factor, factors affecting the lower-order factors are called second-order or higher-order factors. CFA models with higher-order factors are called higher-order CFA models (Bollen, 1989). Bifactor models assume that there will be both a general factor and unique factors - a general factor that explains the common variation of all items, and unique factors explains the common variation after controlling for the general factor. To assess goodness-of-fit, the Akaike information criterion (AIC; Akaike, 1974) and Bayesian information criterion (BIC; Schwarz, 1978) were employed. A lower AIC or a lower BIC is preferred. Besides that, we also provide other indices of model fit, such as the root mean square error of approximation (RMSEA), standardized root-mean-square residual (SRMR), comparative fit index (CFI), and Tucker-Lewis index (TLI). As suggested by Kline (2016) and Wen et al. (2004), RMSEA and SRMR values should be below 0.08. CFI and TLI values greater than 0.90 are acceptable, while values greater than 0.95 are excellent.
Results
Latent Structure of Nomophobia
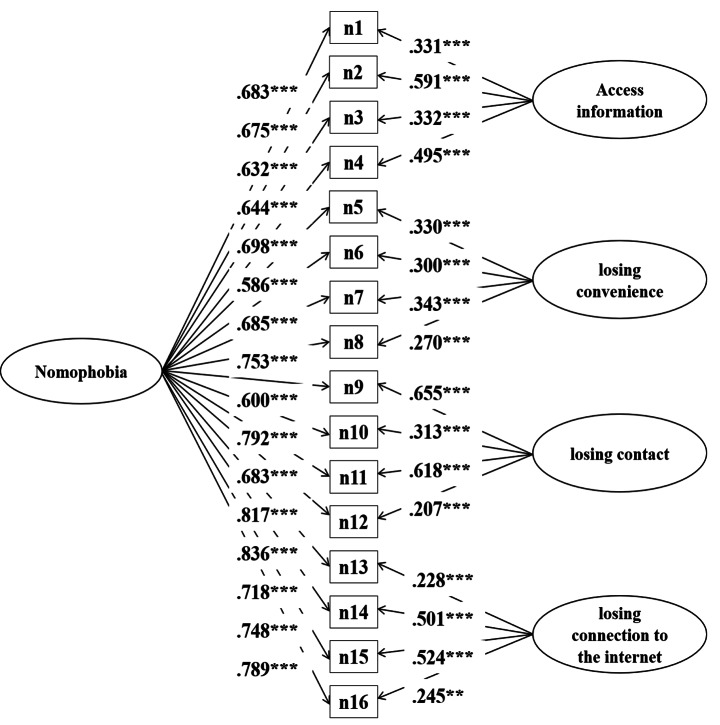
First, CFA was conducted on the Nomophobia scale. Good model fit was demonstrated (χ2 = 546.830, p < .001, df = 98, TLI = 0.929, CFI = 0.942, SRMR = 0.044, RMSEA = 0.071), and factor loadings ranged from 0.651 to 0.879. Correlations between the four factors were moderately strong (higher than 0.714). These results further indicated that a general factor may explain the latent factors. As a result, we conducted second-order CFA model and bifactor modeling. All goodness of fit indices supported the bifactor model when comparing the first-order CFA, second-order CFA, and bifactor model, because the bifactor model has more excellent indicator including smallest AIC = 47205.728, BIC = 47513.578, SRMR = 0.026, RMSEA = 0.043 and largest CFI = 0.974, TLI = 0.981. Detailed results can be seen in Table 1. The general factor of the bifactor model presented the principal variation of nomophobia. And fear of being unable to access information, fear of losing convenience, fear of losing contact and fear of losing connection to the internet were four unique factors consistent with nomophobia’s four dimensions. The specific model can be seen in Fig. 1.
Table 1.
Model Fit indicator for each model of nomophobia
| Model | AIC | BIC | χ 2 | p | df | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|---|---|---|
| First-Order CFA | 47648.907 | 47908.655 | 546.830 | < 0.001 | 98 | 0.942 | 0.929 | 0.071 | 0.044 |
| s-Order CFA | 47646.225 | 47896.352 | 549.527 | < 0.001 | 100 | 0.942 | 0.931 | 0.070 | 0.045 |
| Bifactor | 47205.728 | 47513.578 | 238.954 | < 0.001 | 88 | 0.981 | 0.974 | 0.043 | 0.026 |
NOTE. AIC = Akaike information criterion; BIC = Bayesian information criterion; df = degrees of freedom; CFI = comparative fit index; TLI = Tucker–Lewis index; RMSEA = root mean square error of approximation; SRMR = Standardized Root Mean Square Residual
Fig. 1.
The bifactor model of Nomophobia
We computed the ω_H of the general factor which was 0.895. This value means that 89.5% of the variance of unit-weighted total scores can be attributed to the individual differences on the general factor. In addition, we also computed the explained common variance (ECV). Results showed that the computed explained common variance was 0.745, meaning that the general factor explains 74.5% of the common variance extracted with 25.5% of the common variance spread across group factors. And the results also showed that the value of percent uncontaminated correlations (PUC) was 80%, which means, in an applied sense, that the overwhelming majority of correlations inform directly on the general factor, which is the target trait that the instrument was designed to assess.
The Associations Between Nomophobia and Mental Health Symptoms
Before building the SEM model of PMPU, nomophobia, and three mental health symptom scores including depression, anxiety, and stress, we needed to construct a generalized factor that can represent PMPU from the first-order CFA structure of PMPU. Consequently, we built a bifactor model and a second-order CFA model for PMPU. However, we discovered that there was a contradiction in the first-order CFA data fit for the 16-item version of PMPU in building the model. Some evidence was found for adequate fit, such as SRMR = 0.051, RMSEA = 0.084, but also some evidence for inadequate fit which included χ2 = 723.206, p < .001, df = 98, CFI = 0.865, TLI = 0.890.Then, four items (items 1, 8, 9, and 10) were deleted from the original scales since high correlations among the residuals were observed in the results. CFA was computed again and the data fit the four-factor structure well (χ2 = 272.446, p < .001, df = 48, TLI = 0.928, CFI = 0.948, SRMR = 0.036, RMSEA = 0.072). After that, bifactor and second-order models were conducted on PMPU to extract a generalized factor that could represent the PMPU. Bifactor modeling of PMPU did not converge, and thus the high-order CFA model was employed to denote the generalized factor of PMPU (χ2 = 251.572, p < .001, df = 49, TLI = 0.936 CFI = 0.953, SRMR = 0.036, RMSEA = 0.068). The second-order factor presented the sum variation of four factors of MPATS, which was named “PMPU”. Details can be seen in Table 2.
Table 2.
Model Fit indicator of PMPU
| Model | AIC | BIC | χ2 | Sig. | df | CFI | TLI | RMSEA | SRMR |
|---|---|---|---|---|---|---|---|---|---|
| Second-Order CFA | 28611.435 | 28808.651 | 251.572 | < 0.001 | 49 | 0.953 | 0.936 | 0.068 | 0.036 |
| Bifactor | - | - | - | - | - | - | - |
NOTE. “-” Means the model did not converge. AIC = Akaike information criterion; BIC = Bayesian information criterion; df = degrees of freedom; CFI = comparative fit index; TLI = Tucker–Lewis index; RMSEA = root mean square error of approximation; SRMR = Standardized Root Mean Square Residual
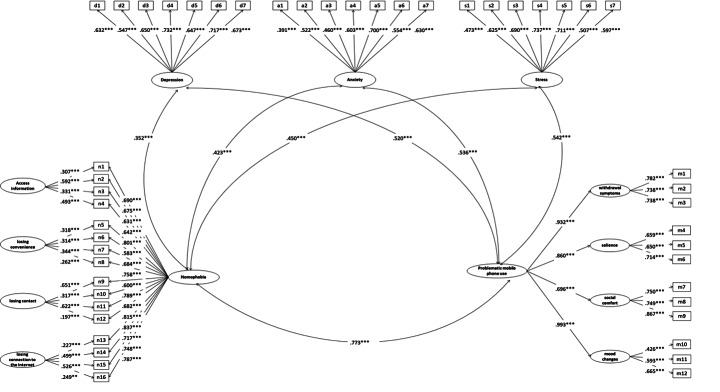
Based on the bifactor structure (nomophobia) and high-order structure (PMPU), we further explored the associations between these two constructs and three mental health variables in the SEM model. The overall SEM for the nomophobia constructs and relations with another PMPU and mental health symptoms is shown in Fig. 2. The results of SEM fit indices were good (χ2 = 2387.460, p < .001, df = 1081, TLI = 0.926, CFI = 0.932, SRMR = 0.041, RMSEA = 0.037). Specifically, the correlation coefficient between the second-order factor of mobile phone overuse and the general factor of nomophobia was high (r = .773, p < .001). However, the correlations between the four unique factors of nomophobia and the second-order factor of mobile phone overuse were very low, coefficients ranged from − 0.119 to 0.117 (p < .05).
Fig. 2.
The Model for Nomophobia, PMPU and Mental health
In addition, SEM results showed that both the latent factors for PMPU (MPAT) and nomophobia had significant correlations with the three mental health variables. Importantly, the correlations between four unique factors of nomophobia and three mental health factors were very low, with coefficient values ranging from − 0.024 to 0.017. In Fig. 2, we only display the significant paths in the SEM.
Discussion
Bifactor Structure of Nomophobia and Relationship to Mental Health
First, this study investigated the latent psychological structure of nomophobia in a sample of Chinese university students by model comparison. The present results showed that the structure of nomophobia fitted a bifactor model well rather than a second-order model (see Table 1), including a general factor concerning problematic mobile phone use and four unique factors concerning functional use. Next, we used the bifactor structure to distinguish problematic mobile phone use from functional mobile phone use, and then we examined the relationship among PMPU, nomophobia, and mental health symptoms using the SEM model. Results showed that the general factor of nomophobia was highly associated with PMPU (r = .773, p < .001) (see Fig. 2). It is inferred that either PMPU or nomophobia share a common component concerning mental health. Both the second-order factor in PMPU and the general factor in nomophobia showed moderate correlations with depression, anxiety, and stress (see Fig. 2).
This finding corroborates previous work on relationships among mental health, nomophobia, and mobile phone overuse (Tams et al., 2018). The related results showing depression, anxiety, and stress associated with nomophobia fit within the I-PACE theoretical model developed by Brand and colleagues (Brand et al., 2019). It confirmed that the general factor of nomophobia concerning would be related to mental health symptoms (Throuvala et al., 2020). Similarly, the findings of the current study have also been supported by other researchers’ studies. For instance, Kara et al. (2019) confirmed that the level of nomophobia was significantly related to anxiety, and other scholars also discovered that nomophobia was significantly related with depression, stress, and other mental health problem (Rodriguez-Garcia et al., 2020). In the meantime, some studies discovered that PMPU was significantly associated with anxiety, depression, and stress symptoms (Zhang et al., 2020; Elhai et al., 2020a).
Notably, after the general factor was extracted from nomophobia, the unique factors were no longer related to the PMPU (MPAT) factor or mental health factors. It can also explain the distinction between nomophobia and PMPU. Moreover, the four unique factors of nomophobia are functional rather than problematic. In other words, the bifactor model structurally separated nomophobia into two distinct parts. One presented dependence on functionality of the mobile phone, while the other presented fear and anxiety about mobile phone use. However, several factor loadings on unique factors in the bifactor model were not very high, though they were significant. It indicates that discrimination of these items from their corresponding unique factors was not very strong. In addition, the current study employed a bifactor model to separate fear and anxiety from the functional overuse of a mobile phone, and then employed the general factor from the bifactor model to explore the relationship between nomophobia and other psychological variables, which may be more accurate than using a total score of nomophobia. Such information could help advance our understanding of the factors that influence college students’ nomophobia.
Structure of MPAT
Our study also found that the structure of the MPAT represented a second-order rather than a bifactor model (see Table 2), while nomophobia retained a bifactor structure. Distinct latent structures indicated that these two problematic mobile phone use constructs are unique from each other. MPAT emphasizes the psychological, physical, and social functions resulting from the use of mobile phones (Xiong et al., 2012), while NMP emphasizes a pathological fear after one’s loss of mobile phone access (Yildirim & Correia, 2015).
In the majority of previous studies, PMPU has been treated as a first-order multifactor model (Pasquale et al., 2017; Csibi et al., 2018). However, MPAT was a second-order CFA structure in this study. According to the present study, we found that the latent factor conceptualizations of PMPU are varied. For instance, some scholars have discovered four factors of PMPU (Kim et al., 2014), while other scholars have proposed six factors (Pasquale et al., 2017). There seem to be some commonalities, but also differences, between conceptualizations. Thus, conclusions about the latent symptom structure of PMPU were inconsistent and needed to be investigated. We used a second-order factor as an indicator of overuse degree in this study. Results showed that a second-order CFA structure in this study may be more appropriate for mobile phone overuse. Correlations for the second-order factor with depression (r = .520, p < .001), anxiety (r = .536, p < .001) and stress (r = .542, p < .001) were further supportive of the higher-order factor as a more likely representative indicator of individual mobile phone overuse. Theoretically, it further demonstrates that there is a strong commonality among several factors. That is, individuals with PMPU may have some degree of expression on all dimensions, not just a single dimension or a few dimensions.
Implications and Limitations
The purpose of this study was to explore the structure of nomophobia, and SEM was used to verify the bifactor structure. It has several theoretical implications. Firstly, previous studies found that the structure of nomophobia was first-order, including four dimensions (Nawaz et al., 2017; Yildirim et al., 2016), while we found that nomophobia was a bifactor model. This structure distinguished problematic mobile phone use from functional use by using the bifactor structure and then concluded that nomophobia shared a common factor concerning mobile phone overuse, and it has independent unique factors concerning usable function. The findings provided more information to advance our understanding of nomophobia. Secondly, this study found that individuals’ nomophobia significantly correlated with anxiety, depression, and stress. It provides compelling evidence for assumptions of the I-PACE model by using empirical data. In addition to the theoretical contributions, this study confirmed that the mobile phone is a double-edged sword. On the one hand, mobile phones provide us with a lot of functional convenience. On the other hand, there will be more risk from overuse if individuals spend excessive time on mobile phones. The bifactor model distinguished these two components from a statistical perspective. In future practical use and empirical research, the general and unique factor scores based on the bifactor model will provide a way to quantify functional and overused components.
There were also several limitations to this study. First, the conclusion about the bifactor structure of nomophobia was drawn from a sample of Chinese university students, and thus it should be generalized to other groups with caution. More evidence from other populations could be used to test model invariance across the populations in the future. Besides that, problematic mobile phone use of youth and the elderly may perform differently. More participants at different ages would further verify the psychological structure of nomophobia. Third, the current study mainly focused on the structure of nomophobia, and distinguished problematic mobile phone use from functional use by using the bifactor structure. It would be worthwhile to investigate the associations among problematic mobile phone use, functional mobile phone use, and other psychological factors based on this bifactor structure.
Conclusion
We concluded that the bifactor model was the best model for nomophobia that contained a general factor concerning mobile phone overuse and four unique factors concerning usable function use. The general factor concerning mobile phone overuse was significantly related to the mental health symptoms, while the functional factors were not correlated to the mental health symptoms. That is, some problematic cell phone use, rather than functional cell phone use, is associated with an individual’s negative psycho-emotional performance.
Acknowledgements
The authors would like to express their gratitude to all participants in this study.
Appendix
Firstly, a measurement invariance test between the males and females was supported by a multi-group confirmatory factor analysis (CFA). (Results can be seen in Table S1). In the meantime, two measurement invariance tests, a two-group CFA and a three-group CFA were conduct across different ages. Participants were divided into two groups (Group 1: Their age were smaller than the mean age (17–20 years old, 611 participants); Group 2: Their age were higher than the mean age (21–26 years old, 296 participants)). (Results can be seen in Table S2). Also we tried dividing participants into three groups (Group 1: Their age were smaller than the mean age (17–19 years old, 431 participants); Group 2: Their age were equal to the mean age (20 years old, 180 participants); Group 3: Their age were higher than the mean age (21–26 years old, 296 participants)). Results showed that measurement invariance was supported among different groups of age (Results of three groups can be seen in Table S3). According to these results, we can conclude that that neither gender nor age would influence the construct of nomophobia.
Table S1.
Measurement invariance about gender of nomophobia
| Overall fit indices | Comparative fit indices | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | S-Bχ 2 | Df | CFI | TLI | SRMR | RMSEA (90% CI) | compare | Δχ 2 | Δdf | ΔCFI | ΔTLI | ΔSRMR | ΔRMSEA |
| Model A | 983.182*** | 196 | 0.925 | 0.908 | 0.050 | 0.094 (0.088, 0.100) | |||||||
| Model B | 983.182*** | 196 | 0.925 | 0.908 | 0.050 | 0.094 (0.088, 0.100) | A vs. B | 0.000 | 0 | 0.000 | 0.000 | 0.000 | 0.000 |
| Model C | 1016.758*** | 220 | 0.924 | 0.917 | 0.053 | 0.089 (0.084, 0.095) | B vs. C | 33.576 | 24 | 0.001 | 0.009 | 0.003 | 0.005 |
| Model D | 1099.182*** | 236 | 0.918 | 0.917 | 0.057 | 0.090 (0.084, 0.095) | C vs. D | 82.424 | 16 | 0.006 | 0.000 | 0.004 | 0.001 |
| Model E | 1022.468*** | 224 | 0.924 | 0.919 | 0.058 | 0.089 (0.083, 0.094) | D vs. E | 76.714 | 12 | 0.006 | 0.002 | 0.001 | 0.001 |
| Model F | 1027.554*** | 230 | 0.924 | 0.921 | 0.059 | 0.087 (0.082, 0.093) | E vs. F | 5.086 | 6 | 0.000 | 0.002 | 0.001 | 0.002 |
| Model G | 1095.566*** | 234 | 0.918 | 0.916 | 0.082 | 0.090 (0.085, 0.096) | F vs. G | 68.012 | 4 | 0.006 | 0.005 | 0.023 | 0.003 |
Table S2.
Measurement invariance about gender of nomophobia (two groups)
| Overall fit indices | Comparative fit indices | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | S-Bχ 2 | Df | CFI | TLI | SRMR | RMSEA (90% CI) | compare | Δχ 2 | Δdf | ΔCFI | ΔTLI | ΔSRMR | ΔRMSEA |
| Model A | 1021.226*** | 196 | 0.923 | 0.906 | 0.048 | 0.096 (0.091, 0.102) | |||||||
| Model B | 1021.226*** | 196 | 0.923 | 0.906 | 0.048 | 0.096 (0.091, 0.102) | A vs. B | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Model C | 1040.824*** | 220 | 0.924 | 0.917 | 0.049 | 0.091 (0.085, 0.096) | B vs. C | 19.598 | 24 | 0.001 | 0.011 | 0.001 | 0.005 |
| Model D | 1081.291*** | 236 | 0.922 | 0.920 | 0.051 | 0.089 (0.084, 0.094) | C vs. D | 40.467 | 16 | 0.002 | 0.003 | 0.002 | 0.002 |
| Model E | 1044.600*** | 224 | 0.924 | 0.918 | 0.054 | 0.090 (0.084, 0.095) | D vs. E | 36.691 | 12 | 0.002 | 0.002 | 0.003 | 0.001 |
| Model F | 1053.911*** | 230 | 0.924 | 0.920 | 0.053 | 0.089 (0.083, 0.094) | E vs. F | 9.311 | 6 | 0.000 | 0.002 | 0.001 | 0.001 |
| Model G | 1076.172*** | 234 | 0.922 | 0.920 | 0.071 | 0.089 (0.084, 0.095) | F vs. G | 22.261 | 4 | 0.002 | 0.000 | 0.018 | 0.000 |
Table S3.
Measurement invariance about gender of nomophobia (three groups)
| Overall fit indices | Comparative fit indices | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model | S-Bχ 2 | Df | CFI | TLI | SRMR | RMSEA (90% CI) | compare | Δχ 2 | Δdf | ΔCFI | ΔTLI | ΔSRMR | ΔRMSEA |
| Model A | 1171.207*** | 306 | 0.920 | 0.906 | 0.051 | 0.097 (0.091, 0.103) | |||||||
| Model B | 1171.207*** | 306 | 0.920 | 0.906 | 0.051 | 0.097 (0.091, 0.103) | A vs. B | 0.000 | 0 | 0.000 | 0.000 | 0.000 | 0.000 |
| Model C | 1205.102*** | 342 | 0.920 | 0.916 | 0.054 | 0.091 (0.086, 0.097) | B vs. C | 33.895 | 36 | 0.000 | 0.010 | 0.003 | 0.006 |
| Model D | 1272.446*** | 374 | 0.917 | 0.920 | 0.057 | 0.089 (0.084, 0.095) | C vs. D | 70.334 | 32 | 0.003 | 0.004 | 0.003 | 0.002 |
| Model E | 1214.150*** | 350 | 0.920 | 0.918 | 0.064 | 0.090 (0.086, 0.096) | D vs. E | 60.296 | 24 | 0.003 | 0.002 | 0.007 | 0.001 |
| Model F | 1230.516*** | 362 | 0.920 | 0.920 | 0.062 | 0.089 (0.084, 0.095) | E vs. F | 16.366 | 12 | 0.000 | 0.002 | 0.002 | 0.001 |
| Model G | 1258.412*** | 370 | 0.918 | 0.920 | 0.082 | 0.089 (0.084, 0.095) | F vs. G | 17.896 | 8 | 0.002 | 0.000 | 0.020 | 0.000 |
Author Contributions
All authors contributed to the study conception and design. Shixiu Ren: Conceptualization, Methodology, Software, Writing-Original draft, Writing-Reviewing and Editing. Tour Liu: Conceptualization, Methodology, Writing-Reviewing and Editing. Xinlu Zhao: Data collection, Investigation. Haibo Yang: Data collection, Investigation. Jon D. Elhai: Methodology, Writing- Reviewing and Editing.
Funding
This research was supported by the National Natural Science Foundation of China. (Grant number 31800945).
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Conflict of Interest
Shixiu Ren, Tour Liu, Xinlu Zhao, Haibo Yang, and Jon D. Elhai declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Tianjin Normal University, China) and with the Helsinki Declaration of 1975, as revised in 2000 (5) (Ethical review number: XL2020-08).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adawi M, Bragazzi NL, Argumosa-Villar L, Boada-Grau J, Vigil-Colet A, Yildirim C, Watad A. Translation and validation of the nomophobia questionnaire in the italian language: exploratory factor analysis. JMIR mHealth and uHealth. 2019;6(1):1–24. doi: 10.2196/mhealth.9186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19(6):716–723. doi: 10.1109/TAC.1974.1100705. [DOI] [Google Scholar]
- Bartwal J, Nath B. Evaluation of nomophobia among medical students using smartphone in north India. Medical Journal Armed Forces India. 2019;76(4):451–455. doi: 10.1016/j.mjafi.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billieux J, Maurage P, Lopez-Fernandez O, Kuss DJ, Griffiths MD. Can disordered mobile phone use be considered a behavioral addiction? An update on current evidence and a comprehensive model for future research. Current Addiction Reports. 2015;2(1):156–162. doi: 10.1007/s40429-015-0054-y. [DOI] [Google Scholar]
- Bianchi A, Phillips JG. Psychological predictors of problem mobile phone use. Cyberpsychology & behavior. 2005;8(1):39–51. doi: 10.1089/cpb.2005.8.39. [DOI] [PubMed] [Google Scholar]
- Bollen, K. A. (1989). Structural equations with latent variables. John Wiley & Sons, Inc. 10.1002/9781118619179
- Brand M, Wegmann E, Stark R, Muller A, Wolfling K, Robbins TW, Potenza MN. The interaction of person-affect-cognition-execution (I-PACE) model for addictive behaviors: Update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neuroscience and Biobehavioral Reviews. 2019;104(1):1–10. doi: 10.1016/j.neubiorev.2019.06.032. [DOI] [PubMed] [Google Scholar]
- Brand M, Young KS, Laier C, Wolfling K, Potenza MN. Integrating psychological and neurobiological considerations regarding the development and maintenance of specific internet-use disorders: an Interaction of person-affect-cognition-execution (I-PACE) model. Neuroscience and Biobehavioral Reviews. 2016;71(1):252–266. doi: 10.1016/j.neubiorev.2016.08.033. [DOI] [PubMed] [Google Scholar]
- Chen CY, Lian SK, Yang C, Zhou ZK. Effect of mobile phone addiction on college students’ depression: mediation and moderation analyses. Chinese Journal of Clinical Psychology. 2019;27(4):746–749. doi: 10.16128/j.cnki.1005-3611.2019.04.021. [DOI] [Google Scholar]
- Chen IH, Pakpour AH, Leung H, Potenza MN, Su JA, Lin CY, Griffiths MD. Comparing generalized and specific problematic smartphone/internet use: longitudinal relationships between smartphone application-based addiction and social media addiction and psychological distress. Journal of behavioral addictions. 2020;9(2):410–419. doi: 10.1556/2006.2020.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Wang L, Qiao NN, Cao PY, Zhang YL. Preliminary development of adult smartphone addiction scale. Chinese Journal of Clinical Psychology. 2017;25(4):645–649. doi: 10.16128/j.cnki.1005-3611.2017.04.012. [DOI] [Google Scholar]
- Copaja-Corzo C, Aragon-Ayala CJ, Taype-Rondan A, Nomotest-Group Nomophobia and its associated factors in peruvian medical students. International Journal of Environmental Research and Public Health. 2022;19(9):1–11. doi: 10.3390/ijerph19095006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csibi S, Griffiths MD, Cook B, Demetrovics Z, Szabo A. The psychometric properties of the smartphone application-based addiction scale (SABAS) International Journal of Mental Health and Addiction. 2018;16(1):393–403. doi: 10.1007/s11469-017-9787-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delgado MK, Wanner KJ, Mcdonald C. Adolescent cell phone use while driving: an overview of the literature and promising future directions for prevention. Media and communication. 2016;4(3):79–89. doi: 10.17645/mac.v4i3.536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey A, O’Brien E, Tiamiyu KD, Elhai JD. Fear of missing out (FoMO) and rumination mediate relations between social anxiety and problematic Facebook use. Addictive Behaviors Reports. 2019;9(1):1–7. doi: 10.1016/j.abrep.2018.100150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De-Sola Gutierrez J, Rodríguez de Fonseca F, Rubio G. Cell-phone addiction: a review. Frontiers in Psychiatry. 2016;7(175):1–15. doi: 10.3389/fpsyt.2016.00175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Levine JC, Hall BJ. The relationship between anxiety symptom severity and problematic smartphone use: a review of the literature and conceptual frameworks. Journal of Anxiety Disorders. 2019;62(1):45–52. doi: 10.1016/j.janxdis.2018.11.005. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Levine JC, Hall BJ. Problematic smartphone use and mental health problems: current state of research and future directions. Dusunen Adam: The Journal of Psychiatry and Neurological Sciences. 2019;32(1):1–3. doi: 10.14744/DAJPNS.2019.00001. [DOI] [Google Scholar]
- Elhai JD, Yang HB, Fang JW, Bai XJ, Hall BJ. Depression and anxiety symptoms are related to problematic smartphone use severity in chinese young adults: fear of missing out as a mediator. Addictive Behaviors. 2020;101(1):1–7. doi: 10.1016/j.addbeh.2019.04.020. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Yang HB, Rozgonjuk D, Montag C. Using machine learning to model problematic smartphone use severity: the significant role of fear of missing out. Addictive Behaviors. 2020;103(1):1–7. doi: 10.1016/j.addbeh.2019.106261. [DOI] [PubMed] [Google Scholar]
- Gao Y, Dai H, Jia G, Liang C, Tong T, Zhang Z, Zhu Y. Translation of the chinese version of the nomophobia questionnaire and its validation among college students: factor analysis. JRMI mHealth and uHealth. 2020;8(3):1–5. doi: 10.2196/13561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang YZ, Bai XL. College students rely on mobile internet making impact on alienation: the role of society supporting systems. Psychological Development and Education. 2014;30(5):540–549. [Google Scholar]
- Kates AW, Wu H, Coryn CL. The effects of mobile phone use on academic performance: a meta-analysis. Computers & Education. 2018;127(1):107–112. doi: 10.1016/j.compedu.2018.08.012. [DOI] [Google Scholar]
- Kamolthip R, Chirawat P, Ghavifekr S, Gan WY, Tung SE, Nurmala I, Nadhiroh SR, Pramukti I, Lin CY. Problematic internet use (PIU) in youth: a brief literature review of selected topics. Current Opinion in Behavioral Sciences. 2022;46(1):1–9. doi: 10.1016/j.cobeha.2022.101150. [DOI] [Google Scholar]
- Kara M, Baytemir K, Inceman-Kara F. Duration of daily smartphone usage as an antecedent of nomophobia: exploring multiple mediation of loneliness and anxiety. Behavior & Information Technology. 2019;40(1):85–98. doi: 10.1080/0144929X.2019.1673485. [DOI] [Google Scholar]
- Kardefelt-Winther D. A conceptual and methodological critique of internet addiction research: towards a model of compensatory internet use. Computers in Human Behavior. 2014;31(1):351–354. doi: 10.1016/j.chb.2013.10.059. [DOI] [Google Scholar]
- Kaviani F, Robards B, Young KL, Koppel S. Nomophobia: is the fear of being without a smartphone associated with problematic use? International Journal of Environmental Research and Public Health. 2020;17(1):1–19. doi: 10.3390/ijerph17176024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D, Lee Y, Lee J, Nam JK, Chung Y. Development of korean smartphone addiction proneness scale for youth. PloS One. 2014;9(5):1–8. doi: 10.1371/journal.pone.0097920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AL, Valenca AM, Silva AC, Sancassiani F, Machado S, Nardi AE. “Nomophobia”: impact of cell phone use interfering with symptoms and emotions of individuals with panic disorder compared with a control group. Clinical Practice & Epidemiology in Mental Health. 2014;10(1):28–35. doi: 10.2174/1745017901410010028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AL, Valenca AM, Silva AC, Baczynski T, Carvalho MR, Nardi AE. Nomophobia: dependency on virtual environments or social phobia? Computers in Human Behavior. 2013;29(1):140–144. doi: 10.1016/j.chb.2012.07.025. [DOI] [Google Scholar]
- Kline, R. B. (2016). Principles and practice of structural equation modeling (3rd ed.). Guilford Press.
- Kuss DJ, Pontes HM, Griffiths MD. Neurobiological correlates in internet gaming disorder: a systematic literature review. Frontiers in psychiatry. 2018;9(166):1–12. doi: 10.3389/fpsyt.2018.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachmann B, Sindermann C, Sariyska RY, Luo R, Melchers MC, Becker B, Cooper AJ, Montag C. The role of empathy and life satisfaction in internet and smartphone use disorder. Frontiers in Psychology. 2018;9(398):398. doi: 10.3389/fpsyg.2018.00398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laier C, Brand M. Mood changes after watching pornography on the internet are linked to tendencies towards internet-pornography-viewing disorder. Addictive behaviors reports. 2017;5(1):9–13. doi: 10.1016/j.abrep.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laier C, Wegmann E, Brand M. Personality and cognition in gamers: avoidance expectancies mediate the relationship between maladaptive personality traits and symptoms of internet-gaming disorder. Frontiers in Psychiatry. 2018;9(304):1–8. doi: 10.3389/fpsyt.2018.00304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M, Hong Y, Lee S, Won J, Yang J, Park S, Chang KT, Hong Y. The effects of smartphone use on upper extremity muscle activity and pain threshold. Journal of physical therapy science. 2015;27(6):1743–1745. doi: 10.1589/jpts.27.1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li P, Yang J, Zhou Z, Zhao Z, Liu T. The influence of college students’ academic stressors on mental health during COVID-19: the mediating effect of social support, social well-being, and self-identity. Frontiers in public health. 2022;10(1):1–13. doi: 10.3389/fpubh.2022.917581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, Zhang D, Yang X, Zhang C, Fan C, Zhou Z. Perceived stress and mobile phone addiction in chinese adolescents: a moderated mediation model. Computers in Human Behavior. 2018;87(1):247–253. doi: 10.1016/j.chb.2018.06.006. [DOI] [Google Scholar]
- Liu XR, Lu H, Zhou Z, Chao M, Liu T. Development of a computerized adaptive test for problematic mobile phone use. Frontiers in Psychology. 2022;13(1):1–13. doi: 10.3389/fpsyg.2022.892387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck Depression and anxiety inventories. Behavior Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- Lu GL, Ding YM, Zhang YM, Huang HT, Liang YP, Chen CR. The correlation between mobile phone addiction and coping style among chinese adolescents: a meta-analysis. Child and adolescent psychiatry and mental health. 2021;15(60):1–11. doi: 10.1186/s13034-021-00413-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu S, Duan XY, Qiu MY. Longitudinal measurement invariance of the chinese versions of DASS-21 in college students. Chinese Journal of Clinical Psychology. 2020;28(5):950–953. doi: 10.16128/j.cnki.1005-3611.2020.05.019. [DOI] [Google Scholar]
- Luo J, Ren SX, Li YX, Liu T. The effect of college students’ adaptability on nomophobia: based on Lasso regression. Frontiers in Psychiatry. 2021;12(1):1–9. doi: 10.3389/fpsyt.2021.641417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Liu C. Evaluation of the factor structure of the chinese version of the Nomophobia Questionnaire. Current Psychology. 2018;40(1):1367–1373. doi: 10.1007/s12144-018-0071-9. [DOI] [Google Scholar]
- Nawaz I, Sultana I, Amjad MJ, Shaheen A. Measuring the enormity of nomophobia among youth in Pakistan. Journal of Technology in Behavioral Science. 2017;2(1):149–155. doi: 10.1007/s41347-017-0028-0. [DOI] [Google Scholar]
- Pancani L, Preti E, Riva P. The psychology of smartphone: the development of the smartphone impact scale (SIS) Assessment. 2020;27(6):1176–1197. doi: 10.1177/1073191119831788. [DOI] [PubMed] [Google Scholar]
- Panova T, Carbonell X. Is smartphone addiction really an addiction? Journal of Behavioral Addictions. 2018;7(2):252–259. doi: 10.1556/2006.7.2018.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park BW, Lee KC. The effect of users’ characteristics and experiential factors on the compulsive usage of the smartphone. Ubiquitous Computing & Multimedia Applications. 2011;151(1):438–446. doi: 10.1007/978-3-642-20998-7_52. [DOI] [Google Scholar]
- Pasquale CD, Sciacca F, Hichy Z. Italian validation of smartphone addiction scale short version for adolescents and young adults (SAS-SV) Psychology. 2017;8(10):1513–1518. doi: 10.4236/psych.2017.810100. [DOI] [Google Scholar]
- Poushter, J., Bishop, C., & Chwe, H. (2018). Social media use continues to rise in developing countries but plateaus across developed ones. Pew Research Center. https://assets.pewresearch.org/wp-content/uploads/sites/2/2018/06/15135408/Pew-Research-Center_Global-Tech-Social-Media-Use_2018.06.19.pdf
- Rahme C, Hallit R, Akel M, Chalhoub C, Hachem M, Hallit S, Obeid S. Nomophobia and temperaments in Lebanon: results of a national study. Perspectives in Psychiatric Care. 2021;1(1):1–6. doi: 10.1111/ppc.12968. [DOI] [PubMed] [Google Scholar]
- Ren SX, Guli GN, Liu T. Revisement of Nomophobia Scale for Chinese. Psychological Exploration. 2020;40(3):247–253. [Google Scholar]
- Rodriguez-García AM, Moreno-Guerrero AJ, López Belmonte J. Nomophobia: an individual’s growing fear of being without a smartphone: a systematic literature review. International Journal of Environmental Research and Public Health. 2020;17(2):580–599. doi: 10.3390/ijerph17020580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin S, Ozdemir K, Unsal A, Temiz N. Evaluation of mobile phone addiction level and sleep quality in university students. Pakistan Journal of Medical Sciences. 2013;29(4):913–918. doi: 10.12669/pjms.294.3686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. The Annals of Statistics. 1978;6(2):461–464. doi: 10.1214/aos/1176344136. [DOI] [Google Scholar]
- Soror AA, Hammer BI, Steelman ZR, Davis FD, Limayem MM. Good habits gone bad: explaining negative consequences associated with the use of mobile phones from a dual-systems perspective. Information Systems Journal. 2015;25(4):403–427. doi: 10.1111/isj.12065. [DOI] [Google Scholar]
- Su S, Pan TT, Liu QX, Chen XW, Wang YJ, Li MY. Preliminary development of Smartphone Addiction Scale for college students. Chinese Mental Health Journal. 2014;28(5):392–397. [Google Scholar]
- Sun YC, Yang JQ, Liu T. The Association between neuroticism and nomophobia: Chain mediating effect of attachment and loneliness. International Journal of Mental Health and Addiction. 2022;1(1):1–18. doi: 10.1007/s11469-022-00897-9. [DOI] [Google Scholar]
- Tams S, Legoux R, Leger P. Smartphone withdrawal creates stress: a moderated mediation model of nomophobia, social threat, and phone withdrawal context. Computers in Human Behavior. 2018;81(1):1–9. doi: 10.1016/j.chb.2017.11.026. [DOI] [Google Scholar]
- Throuvala MA, Griffiths MD, Rennoldson M, Kuss DJ. Mind over Matter: testing the efficacy of an online randomized controlled trial to reduce distraction from Smartphone Use. International Journal of Environmental Research and Public Health. 2020;17(13):1–30. doi: 10.3390/ijerph17134842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran D. Classifying nomophobia as smart-phone addiction disorder. UC Merced Undergraduate Research Journal. 2016;9(1):1–23. doi: 10.5070/M491033274. [DOI] [Google Scholar]
- Van Deursen AJAM, Bolle CL, Hegner SM, Kommers PAM. Modeling habitual and addictive smartphone behavior: the role of smartphone usage types, emotional intelligence, social stress, self-regulation, age, and gender. Computers in Human Behavior. 2105;45(1):411–420. doi: 10.1016/j.chb.2014.12.039. [DOI] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain behavior and immunity. 2020;87(1):40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegmann E, Müller SM, Ostendorf S, Brand M. Highlighting internet-communication disorder as further internet-use disorder when considering neuroimaging studies. Current Behavioral Neuroscience Reports. 2018;5(4):295–301. doi: 10.1007/s40473-018-0164-7. [DOI] [Google Scholar]
- Wen ZL, Hou JT, Marsh HW. Structural equation model testing: cutoff criteria for goodness of fit indices and chi-square test. Acta Psychological Sinica. 2004;36(2):186–194. [Google Scholar]
- Xiong J, Zhou ZK, Chen W, You ZQ, Zhai ZY. Development of the mobile phone addiction tendency scale for college students. Chinese mental health journal. 2012;26(3):222–225. doi: 10.3969/j.issn.1000-6729.2012.03.013. [DOI] [Google Scholar]
- Ye BJ, Fang XT, Yang Q, Zheng Q, Liu LL, Guo SY. The effects of difficulties in emotional regulation on college students’ mobile phone addiction: the chain mediating effect of facial negative physical self and social avoidance and distress. Psychological Development and Education. 2017;30(2):249–256. [Google Scholar]
- Yildirim C, Correia AP. Exploring the dimensions of nomophobia: development and validation of a self-reported questionnaire. Computers in Human Behavior. 2015;49(1):130–137. doi: 10.1016/j.chb.2015.02.059. [DOI] [Google Scholar]
- Yildirim C, Sumuer E, Adnan M, Yildirim S. A growing fear: prevalence of nomophobia among turkish college students. Information Development. 2016;32(5):1322–1331. doi: 10.1177/0266666915599025. [DOI] [Google Scholar]
- Zhang Y, Zhang DJ, Xiong L, Gu CH. Effects of mobile phone addiction on depression and anxiety: mediation and moderation analyses. Chinese Journal of Clinical Psychology. 2018;26(6):1086–1090. doi: 10.16128/j.cnki.1005-3611.2018.06.008. [DOI] [Google Scholar]
- Zhang G, Yang X, Tu X, Ding N, Lau J. Prospective relationships between mobile phone dependence and mental health status among chinese undergraduate students with college adjustment as a mediator. Journal of affective disorders. 2020;260(1):498–505. doi: 10.1016/j.jad.2019.09.047. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.