This Letter to the Editor refers to article: ‘Prognostic value of right ventricular refractory period heterogeneity in Type-1 Brugada electrocardiographic pattern’ by Rossi et al. https://doi.org/10.1093/europace/euac168.
A response to this letter is available ‘Prognostic value of right ventricular refractory period heterogeneity in Brugada syndrome. Independent predictor or part of something more complex?—Authors’ response’ by Alberto Giannoni et al. https://doi.org/10.1093/europace/euac249.
We have recently read with great interest the article by Rossi et al.1 entitled ‘Prognostic value of right ventricular refractory period heterogeneity in Type-1 Brugada electrocardiographic pattern’.
A prognostic stratification with electrophysiological study (EPS) was performed in 198 patients of a cohort of 372 Brugada syndrome (BrS) patients with spontaneous or drug-induced type-1 electrocardiogram (ECG) with symptoms. The primary endpoint of the study was a composite of sudden cardiac death (SCD), resuscitated cardiac arrest, or appropriate intervention by the implantable cardioverter-defibrillator. Family history of SCD, syncope, and a spontaneous Type-1 ECG pattern were univariate predictors of the primary endpoint in the whole population. From results obtained by the authors, in patients undergoing EPS, the primary endpoint was not only predicted by ventricular tachycardia (VT)/ventricular fibrillation (VF) inducibility but also by a difference in the refractory period between right ventricular outflow tract (RVOT) and right ventricle apex (ΔRPRVOT-apex) > 60 ms. For the authors, the eterogeneity of right ventricular refractory periods represents a strong, independent predictor of life-threatening arrhythmias in BrS patients, beyond VT/VF inducibility at EPS and common clinical predictors.1
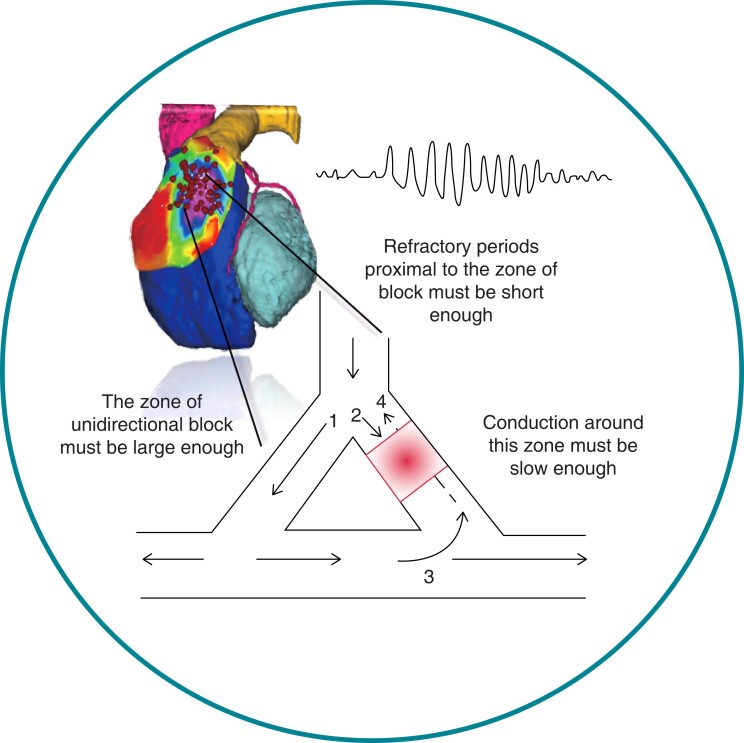
As reported in some research, differences between shortest and longest refractory periods are not the sole indicators of the risk of developing re-entry, and the shape of the blocked zone may also be important.2 The combined effect of three variables must compete together and exceed a threshold: the zone of unidirectional block must be large enough, conduction around this zone must be slow enough, and refractory periods proximal to the zone of block must be short enough (Figure 1). Even in the presence of large disparities in refractory periods but when the size of sites of prolonged refractory period is small, re-entry will not occur unless conduction is also significantly slowed.3,4 Considering that the electrogenic alterations at the base of BrS are mainly epicardial and that EPS provide data about endocardial refractory periods is interesting to know by the authors what is in their cohort of patients the role of the other two variables listed above, so that right ventricular refractory period heterogeneity may be considered ‘a strong independent predictor of life-threatening arrhythmias’. Dispersion of refractory period is a necessary but not sufficient condition for initiation of re-entry.3
Figure 1.
The combined effect of three variables that must compete together and exceed a threshold for the initiation of re-entry.
References
- 1. Rossi A, Giannoni A, Nesti M, Notarstefano P, Castiglione V, Solarino G, et al. Prognostic value of right ventricular refractory period heterogeneity in type-1 Brugada electrocardiographic pattern. Europace 2022:euac168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Allessie MA, Bonke FI, Schopman FJ. Circus movement in rabbit atrial muscle as a mechanism of tachycardia. II. The role of nonuniform recovery of excitability in the occurrence of unidirectional block, as studied with multiple microelectrodes. Circ Res 1976;39:168–77. [DOI] [PubMed] [Google Scholar]
- 3. Burton FL, Cobbe SM. Dispersion of ventricular repolarization and refractory period. Cardiovasc Res 2001;50:10–23. [DOI] [PubMed] [Google Scholar]
- 4. Dendramis G, Antzelevitch C, Brugada P. Brugada syndrome: diagnosis, clinical manifestations, risk stratification and treatment. New York: Nova Science Publishers; 2015. [Google Scholar]