Abstract
Aims
Same-day discharge is increasingly common after catheter ablation for atrial fibrillation (AF). However, the impact of same-day discharge on healthcare utilization after ablation and whether this differs by ablation modality remains uncertain. We examined the safety, efficacy, and subsequent healthcare utilization of a same-day discharge protocol for AF ablation, including radiofrequency (RF) and cryoballoon ablation, in a contemporary cohort.
Methods and results
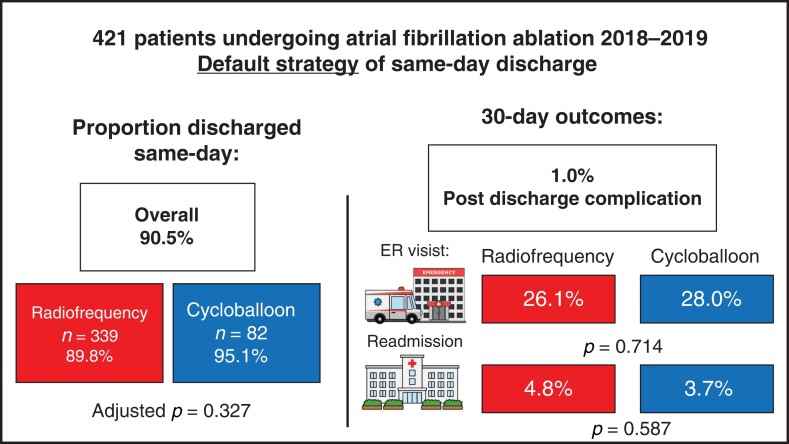
All consecutive patients for whom full healthcare utilization data were available at two centres and who underwent AF ablation from 2018 to 2019 were included. Same-day discharge was the default strategy for all patients. The efficacy and safety outcomes were proportions of same-day discharge and readmission/emergency room (ER) visits, and post-discharge complications, respectively. Of the 421 patients who underwent AF ablation (mean 63.3 ± 10.2 years, 33% female), 90.5% (381/421) achieved same-day discharge with no difference between RF and cryoballoon ablation (89.8 vs. 95.1%, adjusted P = 0.327). Readmission ≤30 days occurred in 4.8%, with ER visits ≤30 days seen in 26.1% with no difference between ablation modalities (P = 0.634). Patients admitted overnight were more likely to present to the ER (40.0 vs. 24.7% with same-day discharge, P = 0.036). The overall post-discharge complication rate was low at 4/421 (1.0%), with no difference between ablation modality (P = 0.324) and admission/same-day discharge (P = 0.485).
Conclusion
Same-day discharge can be achieved in a majority of patients undergoing RF or cryoballoon ablation for AF. Healthcare utilization, particularly ER visits, remains high after AF ablation, regardless of ablation modality or same-day discharge.
Keywords: Catheter ablation, Atrial fibrillation, Outcomes, Radiofrequency, Cryotherapy
Graphical Abstract
Graphical Abstract.
What’s new?
When employed as the default strategy, same-day discharge after atrial fibrillation (AF) ablation can be achieved for a vast majority of patients (90%).
Complications identified after same-day discharge are rare (1%).
Readmission to hospital and emergency room visits are high after AF ablation, but same-day discharge does not result in increased admission/visits after ablation.
Introduction
Catheter ablation of atrial fibrillation (AF) is the most common ablation procedure performed in many electrophysiology centres.1 It is an effective therapy for AF and superior to antiarrhythmic agents for both initial/primary or secondary treatment of AF.2 However, the increasing volume of AF ablation has placed increasing demands on healthcare resource utilization. As the procedure of AF ablation has evolved, with a reduction in procedure time and complication rates,3–5 same-day discharge for AF ablation has increasingly been implemented to minimize the impact of AF ablation on hospital resources.6–11 The adoption of same-day discharge has risen dramatically, particularly in the past 2 years of the global coronavirus pandemic, during which hospital beds have become scarce resources. Yet, despite the increasing body of evidence, same-day discharge after AF ablation is still not performed in a majority of centres.12
Our group has previously demonstrated that a strategy of routine same-day discharge for radiofrequency (RF) AF ablation is safe and can be achieved in a vast majority of patients undergoing ablation.7 However, there remains several unanswered questions. First, can same-day discharge be achieved for all ablation modalities? Cryoballoon ablation is generally shorter than RF ablation, thereby potentially facilitating same-day discharge, yet requiring a larger bore venous sheath, which may result in more difficult haemostasis.13 Existing studies evaluating the impact of ablation modality on same-day discharge have been mixed,6,9,14,15 although selection bias has favoured the use of cryoballoon for same-day discharge patients. Second, although same-day discharge does not increase re-admission to hospital, does it result in increased emergency room (ER) visits? The purpose of this study was to examine the safety, efficacy, and subsequent healthcare utilization of a same-day discharge protocol for AF ablation in a contemporary cohort including RF and cryoballoon ablation.
Methods
This was a multicentre cohort study of consecutive patients undergoing catheter ablation for AF at St Paul’s Hospital and Vancouver General Hospital (Vancouver, Canada) from 2018 to 2019. All consecutive index and repeat procedures in adults ≥19 years of age were eligible. For the current analysis, we restricted the cohort to include only those patients residing in the Vancouver Coastal Health Region (as determined by residential address), for whom complete post-procedure hospitalization and ER visit data were available.
Same-day discharge was the default strategy for the overall cohort, and pre-planned overnight admission could be requested by the treating physician in cases of medical complexity or lack of social supports.
This study complied with the Declaration of Helsinki and was approved by the institutional ethics review boards at each site. Waiver of consent was obtained based on minimal risk.
Detailed baseline and procedural characteristics were obtained from the procedural databases and supplemented by chart review. Intraprocedural complications and reasons for hospital admission were adjudicated by two physicians (M.W.D. and K.H.). These data were then merged with Vancouver Coastal Health Authority administrative data that captures death, hospital admission, and ER visits, as well as associated diagnoses, for all facilities within the health authority region.
Same-day discharge protocol
Our same-day discharge protocol has been published previously.7 Our institutions have implemented a default same-day discharge strategy for all patients undergoing AF ablation since the inception of the programmes (2010 for Vancouver General and 2005 for St Paul’s Hospital). Same-day discharge was the default strategy for all patients, unless a pre-planned overnight admission was requested by the treating physician in cases of medical complexity or lack of social supports (physician discretion). There were no pre-specified clinical criteria for choosing which patients would have a pre-planned admission overnight.
All patients were admitted to a cardiac short stay unit prior to ablation. Both sites performed up three complex ablations (including AF ablation) per lab, per day during the study period. Peri-procedural anticoagulation, ultrasound-guided vascular access, and ablation modality/strategy were at the discretion of the operator. General anaesthesia was used in all cases. Intraprocedural heparin was reversed using protamine in the majority of cases. The femoral venous sheaths were removed in the electrophysiology laboratory. Femoral arterial sheaths were not employed. Following ablation, haemostasis was obtained through manual pressure for a minimum of 10 min. Sutures or vascular closure devices were not routinely employed. Urinary catheters were not routinely placed. Patients were transported back to the cardiac short stay unit where bed rest was maintained for 3 h and extended if haemostasis was not obtained. Patients could remain in the recovery unit for up to 8 h and could be transferred to inpatient wards after recovery unit closure (2000 h). Patients could still be discharged after 2000 h if all discharge criteria, including patient/support person agreement, were met.
Standard nursing post-anaesthesia recovery protocols were used. After completion of bed rest, patients were ambulated. If ambulation was well tolerated with no access site bleeding and stable vital signs, patients were discharged into the care of a family member or support person. Interrupted anticoagulation was resumed 6 h after sheath removal. Written education material and discharge instructions were provided to the patient. The decision to admit a patient for overnight monitoring was left to the discretion of the treating physician and nursing team. Post-procedure care was provided by interdisciplinary AF clinics with telephone visits at 7–10 days and in-person visits at 3, 6, and 12 months.
Outcomes
The primary efficacy outcome of interest was the proportion of patients achieving same-day discharge. The primary healthcare utilization outcomes of interest were hospitalization and ER visits within 30 days. The primary safety outcome was a composite of death, stroke/transient ischaemic attack or embolism, and bleeding requiring hospitalization, within 30 days of discharge after ablation (excluding intraprocedural and immediate post-procedure complications during the procedural hospital stay).
For all outcomes, we pre-specified a comparison between the RF and cryoballoon groups. Furthermore, we also examined the difference in these outcomes between those discharged on the same day and those admitted to hospital post-procedure (with or without complications).
Statistical analysis
Baseline characteristics of study patients were summarized in terms of frequencies and percentages. Descriptive statistics for categorical variables were reported as frequency and percentage; continuous variables were reported as mean (standard deviation). Differences between the RF and cryoballoon groups were compared using χ2 for categorical variables and t-test for continuous variables.
To account for differences between the RF and cryoballoon ablation groups, we considered baseline patient characteristics and clinically relevant variables for inclusion in the efficacy and healthcare utilization models. Stepwise logistic regression models were used to evaluate the independent relationships between the outcomes and potential risk factors. For the efficacy analysis, successful same-day discharge after AF ablation was the binary outcome. For the healthcare utilization analysis, all-cause hospital readmission/ER visit within 30 days after discharge was the binary outcome. All tests were conducted at the 0.05 level, all confidence limits were two-sided, and all analyses were conducted in Stata version 16.1 (StataCorp, College Station, TX, USA).
Results
During the study period from January 2018 to October 2019, a total of 427 AF ablations were performed on patients residing in the Vancouver Coastal Health Authority, for whom full healthcare utilization data were available. Six of 427 patients (1.4%) had a pre-planned overnight admission due to the absence of a caregiver for support upon discharge. Of the remaining 421 patients for whom same-day discharge was the default strategy, 339 (80.5%) underwent RF ablation and 82 (19.5%) underwent cryoballoon ablation (reflecting local practice).
The baseline characteristics are summarized in Table 1. There were notable differences in baseline characteristics between the RF and cryoballoon groups, with more paroxysmal AF and less repeat procedures in the cryoballoon group. There were more patients with heart failure in the RF group, and this was also reflected by a higher proportion of patients with reduced left ventricular function in this group. All patients had general anaesthesia, but the procedure times (room entry to exit) were shorter in the cryoballoon group (median 138 vs. 211 min in the RF group), and the cryoballoon group had fewer cases ending after 1600 h, reflecting local scheduling practices.
Table 1.
Baseline characteristics
| Baseline characteristic | Radiofrequency ablation (N = 339) | Cryoballoon ablation (N = 82) | P-value for comparison |
|---|---|---|---|
| Age (years), mean (SD) | 63.5 (10.2) | 62.2 (10.0) | 0.280 |
| Female sex, N (%) | 112 (33.0) | 29 (35.4) | 0.823 |
| Type of AF, N (%) | |||
| ȃParoxysmal | 172 (50.7) | 66 (80.5) | <0.001 |
| ȃPersistent | 167 (49.3) | 16 (19.5) | |
| Repeat procedure, N (%) | 110 (32.4) | 1 (1.2) | <0.001 |
| Prior stroke, N (%) | 25 (7.4) | 3 (3.7) | 0.226 |
| Valvular diseasea,N (%) | 23 (6.8) | 6 (7.3) | 0.860 |
| Heart failure, N (%) | 101 (29.8) | 9 (11.0) | 0.001 |
| Hypertension, N (%) | 105 (31.0) | 34 (41.5) | 0.070 |
| Diabetes mellitus, N (%) | 37 (10.9) | 6 (7.3) | 0.334 |
| Coronary artery disease, N (%) | 65 (19.2) | 16 (19.5) | 0.944 |
| Pacemaker/defibrillator, N (%) | 32 (9.4) | 3 (3.7) | 0.134 |
| Obstructive sleep apnoea, N (%) | 66 (19.5) | 15 (18.3) | 0.808 |
| Smoker or pulmonary disease, N (%) | 13 (3.8) | 8 (9.8) | 0.027 |
| Chronic kidney disease, N (%) | 48 (14.2) | 11 (13.4) | 0.862 |
| Echocardiographic parameters | |||
| LA diameter (mm), mean (SD) | 42.4 (6.8) | 41.6 (6.3) | 0.333 |
| LA volume (mL/m2), mean (SD) | 41.4 (12.1) | 39.6 (12.2) | 0.241 |
| LVEF <50%, N (%) | 61 (18.0) | 6 (7.3) | 0.017 |
| Procedural characteristics | |||
| Periprocedural anticoagulation | |||
| ȃWarfarin | 25 (7.4) | 4 (4.9) | 0.909 |
| ȃDabigatran | 29 (8.6) | 6 (7.3) | |
| ȃRivaroxaban | 120 (35.4) | 31 (37.8) | |
| ȃApixaban | 152 (44.8) | 37 (45.1) | |
| ȃOtherb | 13 (3.8) | 4 (4.9) | |
| General anaesthesia, N (%) | 339 (100.0) | 82 (100.0) | 1.000 |
| Transoesophageal echocardiography | 336 (99.1) | 81 (98.8) | 0.779 |
| Cardioversion (intraprocedure), N (%) | 75 (22.1) | 16 (19.5 | |
| Intraprocedural complication, —N (%) | |||
| ȃAny | 11 (3.2) | 1 (1.2) | 0.324 |
| ȃAccess site complication | 1 (0.3) | 1 (1.2) | 0.458 |
| ȃPericardial effusion | 3 (0.9) | 0 (0.0) | |
| ȃStroke or embolism | 5 (1.5) | 0 (0.0) | |
| ȃPhrenic nerve palsy | 0 (0.0) | 0 (0.0) | |
| ȃOther | 2 (0.6) | 0 (0.0) | |
| Procedure duration (room entry to exit) in minutes, median (range) | 211 (87–404) | 138 (104–183) | <0.001 |
| Procedure finish time, N (%) | |||
| ȃ09:00–12:59 h | 105 (31.0) | 38 (46.3) | 0.004 |
| ȃ13:00–15:59 h | 96 (28.3) | 26 (31.7) | |
| ȃ≥16:00 h | 138 (40.7) | 18 (22.0) | |
AF, atrial fibrillation; LA, left atrium; LVEF, left ventricular ejection fraction; SD, standard deviation.
Valvular disease was defined as any valve prosthesis or native valve disease (stenosis or regurgitant) of at least moderate severity.
Other anticoagulants typically consisted of patients switching anticoagulants at the time of ablation because of preference or side effects.
Efficacy of same-day discharge
For the overall cohort, same-day discharge was achieved in 90.5% (381/421—Table 2). Same-day discharge was achieved in 89.4% (303/339) of the RF group, and in 95.1% (78/82) in the cryoballoon group (unadjusted P = 0.112 for comparison). The most common reasons for admission were intraprocedural complications, late procedure finish, and access site bleeding (Table 2). For reference, the rate of same-day discharge for the whole cohort of 652 patients (including those living outside the Vancouver Coastal Health Region) was 87.5% (569/652).
Table 2.
Efficacy of same-day discharge and reasons for admission
| Radiofrequency ablation (N = 339) | Cryoballoon ablation (N = 82) | P-value for comparison, unadjusted | |
|---|---|---|---|
| Same-day discharge, N (%) | 303 (89.4) | 78 (95.1) | 0.112 |
| Admission post-procedure, N (%) | 36 (10.6) | 4 (4.9) | |
| ȃAccess site problem | 4 (1.2) | 2 (2.4) | 0.782 |
| ȃAnaesthesia-related problem | 3 (0.9) | 1 (1.2) | |
| ȃIntra-procedural complication | 10 (2.9) | 1 (1.2) | |
| ȃObstructive sleep apnoea monitoring | 1 (0.3) | 0 (0.0) | |
| ȃArrhythmia-related | 1 (0.3) | 0 (0.0) | |
| ȃHeart failure/respiratory problem | 1 (0.3) | 0 (0.0) | |
| ȃLate procedure finish | 10 (2.9) | 0 (0.0) | |
| ȃOther | 6 (1.8) | 0 (0.0) |
In examining predictors of failure of same-day discharge (see Supplementary material online, Table S1). A history of congestive heart failure or left ventricular dysfunction was strongly associated with a requirement for admission, even after multivariable adjustment [adjusted odds ratio for failure of same-day discharge [odds ratio (OR) 2.08 (1.02–4.17), P = 0.044]. After adjustment, ablation modality remained non-significant as a predictor of failure of same-day discharge [adjusted OR 0.55 (0.16–1.85), P = 0.327]. No other baseline variable, such as age or persistent AF, was predictive of failure of same-day discharge. Among procedural variables, the strongest independent predictor of failure of same-day discharge was a procedure finish after 1600 h [adjusted OR for same-day discharge 6.25 (2.04–20.00), P = 0.002]. Overnight admission was not mandatory for procedure finish after 1600 h, and 81.7% of patients in this group were discharged on the same day.
Hospital admission and emergency room visits
The healthcare utilization outcomes and safety outcomes are presented in Table 3. In the 30 days after procedural discharge, 4.8% of patients (20/421) had unplanned admissions to hospital (2 patients had 2 separate admissions, for a total of 22 admissions). The most common reasons for admission were recurrent atrial arrhythmias (7/22–31.8%), pericarditis (3/22–13.6%), access site complications (2/22–9.0%), bradycardia (2/22–9.0%), and shortness of breath without heart failure (2/22–9.0%). However, 26.1% of patients (110/421) had an ER visit within 30 days, with 18.2% (20/110) adjudicated to be unrelated to the ablation procedure. Of those determined to be potentially related to ablation, the most common reasons for ER visits were atrial arrhythmias (36/110–32.7%), chest pain/pericarditis (16/110–14.6%), other arrhythmias such as bradycardia (12/110–10.9%), and access site bleeding (10/110–9.1%).
Table 3.
Healthcare utilization and safety outcomes
| Overall (N = 421) | Radiofrequency ablation (N = 339) | Cryoballoon ablation (N = 82) | P-value for comparison, unadjusted | Same-day discharge (N = 381) | Admitted to hospital (N = 40) | P-value for comparison, unadjusted | |
|---|---|---|---|---|---|---|---|
| Healthcare utilization | |||||||
| Readmission or ER visit within 30 days, N (%) | 113 (26.8%) | 89 (26.2%) | 24 (29.2%) | 0.634 | 97 (25.5%) | 16 (40.0%) | 0.048 |
| ER visit within 30 days | 110 (26.1%) | 87 (25.7%) | 23 (28.0%) | 0.714 | 94 (24.7%) | 16 (40.0%) | 0.036 |
| Readmission within 30 days | 20 (4.8%) | 17 (5.0%) | 3 (3.7%) | 0.587 | 17 (4.5%) | 3 (7.5%) | 0.390 |
| Safety outcomes (post discharge), N (%) | |||||||
| Composite | 4 (1.0%) | 4 (1.2%) | 0 (0.0%) | 0.324 | 4 (1.1%) | 0 (0.0%)a | 0.485 |
| Death | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Stoke/TIA/embolism | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Bleeding/effusionb | 4 (1.0%) | 4 (1.2%) | 0 (0.0%) | 4 (1.1%) | 0 (0.0%) | ||
ER, emergency room; TIA, transient ischemic attack.
Twenty-nine per cent of those admitted to hospital immediately after their ablation had experienced an intra-procedural or immediate post-procedural complication, see Table 1 for details of intraprocedural complications.
Bleeding/effusion outcomes included access site bleeding requiring admission for intervention or pericardial effusion/tamponade.
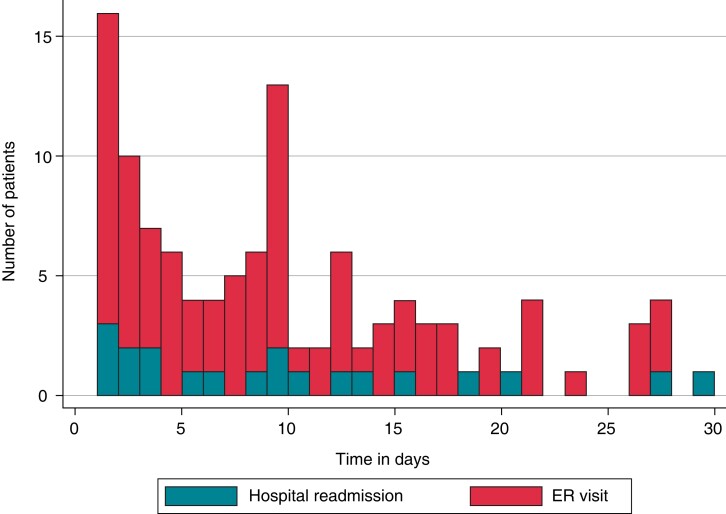
The median time to either ER visit or readmission (Figure 1) was 8 days (interquartile range 3–14 days). Of these, 3.8% occurred within 24 h, 22% occurred within 48 h, and 46% occurred within 7 days.
Figure 1.
Timing of ER visits and rehospitalization. The graph shows the timing of any readmission to hospital or ER visit after discharge and up to 30 days. ER, emergency room.
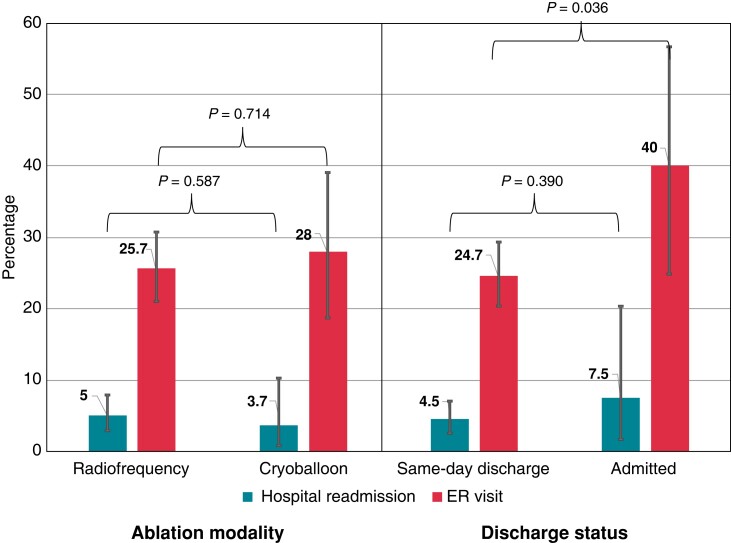
There was no difference in the rate of readmission between RF and cryoballoon ablation modalities (5.0 vs. 3.7%, respectively, unadjusted P = 0.587, Figure 2). Similarly, there was no difference in the rate of ER visits between RF and cryoballoon ablation (25.7 vs. 28.0%, respectively, P = 0.714, Figure 2).
Figure 2.
Hospital readmission and ER visits by ablation modality and by same-day discharge. The rates of rehospitalization and ER visits are presented by ablation modality, and whether the patient was discharged on the same-day or kept overnight after ablation. Abbreviation as in Figure1.
Furthermore, there was no difference in the unadjusted rate of readmission between patients with same-day discharge or those kept in hospital (4.5 vs. 7.5%, respectively, P = 0.390, Figure 2). There was significantly lower ER visits in the same-day discharge group (24.7%) than in those admitted to hospital post-procedure (40.0%, P = 0.036, Figure 2). In the multivariate analysis (see Supplementary material online, Table S2), cryoballoon ablation was not significantly associated with any admission/ER visit; however, same-day discharge was associated with a decrease in admission/hospitalization [adjusted OR 0.44 (0.22–0.88), P = 0.021].
Safety outcomes
The primary safety outcome (composite of death, stroke/transient ischaemic attack or embolism, and bleeding requiring hospitalization) after discharge but within 30 days of after ablation, occurred in 4 of 421 (0.47%) patients, all of which were in the same-day discharge group and received RF ablation (Table 3). Two of these patients had access site bleeding complications requiring intervention, one within 24 h of discharge and the other at 8 days. The other two patients had late presentation of a pericardial effusion (at 8 days), and one was subsequently diagnosed with an atrioesophageal fistula that was successfully treated surgically (at 13 days). No death or stroke/embolism was observed within 30 days of discharge.
Discussion
In this multicentre cohort of patients undergoing AF ablation, we achieved a very high rate of same-day discharge, at over 90%, using a standard clinical protocol with same-day discharge as the default strategy. There was no difference in the ability to achieve same-day discharge between RF and cryoballoon ablation. Rehospitalization within 30 days of same-day discharge was relatively low at just over 5%, however ER visits within 30 days occurred in a quarter of patients. The rates of rehospitalization and ER visits did not differ between those discharged on the same day and those kept overnight for observation. The rate of serious complications identified after same-day discharge was very low, at 1%, with only one complication occurring within 24 h of discharge.
This work adds to our previous experience demonstrating the safety and feasibility of same-day discharge for AF ablation.7 This contemporary analysis observed an improvement in the proportion of patients discharged on the same-day with modern ablation technologies. Furthermore, this was a more contemporary cohort with predominantly direct oral anticoagulant use perioperatively and a higher proportion of patients undergoing cryoballoon ablation.
In examining the current findings in the context of the prior literature, it is important to distinguish observational studies using same-day discharge as the default strategy,7,16 including the current study and those that used a selective strategy for identifying appropriate patients for same-day discharge.6,8–10,14,15 The most important limitation of analyses using selective same-day discharge is that immense selection bias prevents a rigorous comparison of outcomes between same-day discharge and overnight admission. These selective studies are still important as ‘proof of concept,’ however. Employing a default strategy of same-day discharge removes much, though not all, of the selection bias, enabling a reasonable comparison of outcomes.
Among the previous studies evaluating ablation modality and same-day discharge, Ignacio et al.15 reported no impact of ablation modality on the feasibility of same-day discharge, and Bartoletti et al.6 demonstrated similar findings. The studies by Reddy et al.9 and He et al.14 showed higher rates of same-day discharge with cryoballoon ablation vs. standard RF ablation, though cryoballoon ablation patients were preferentially selected for same-day discharge in both studies. Our experience, with same-day discharge as the default strategy, showed no difference between ablation modalities.
We achieved a rate of same-day discharge of just over 90% in this cohort, again with same-day discharge as the default strategy. Previous studies that have employed a selective strategy of same-day discharge have reported rates from 18 to 47%.6,9–11,15 Prior studies that have employed a same-day discharge protocol as the default strategy have shown that this is successful in 79–90% of cases.7,16 The only study to have reported a higher rate of same-day discharge was that of Opel et al.,8 which examined highly selected patients chosen for cryoballoon ablation at a non-tertiary centre.8 In this series, 98.6% were discharged on the same-day.
Compared with our previous experience,7 using the same methodology for tracking outcomes, we showed a decrease in readmission rates at 30 days to 5.2% in the current cohort (2018–19) compared with 7.7% in our previous work (2010–14). This likely represents advances in the safety and efficacy of catheter ablation. The prior work from He et al.14 showed similar readmission rates, but Bartoletti et al.6 showed a reduced readmission rate at 2.1%; however, it was unclear whether admissions to other hospitals were accounted for.
We did observe a high rate of ER visits at 30 days, at over 25%, despite having access to telehealth support from nurses in the AF clinics. Our experience was similar to that of Ignacio et al.15, who reported between 16 and 31% ER visits within 30 days. Although the rates of readmission and ER visits are not higher with same-day discharge in the current or prior studies, the rates remain higher than desired. This likely reflects the unique aspects of AF ablation, particularly the occurrence of post-procedure pericarditis and associated arrhythmia recurrence. Although beyond the scope of this analysis, many of these visits could have been prevented through better perioperative care and education, in order to minimize healthcare utilization after AF ablation in general.
Limitations
The most notable limitation of the current analysis was that we had to restrict our cohort to a subset of patients in whom we had full data with respect to ER visits. This may have introduced some bias as these patients were all from the Vancouver Coastal Region, which is predominantly urban, who may have a higher socioeconomic status than their rural counterparts. However, in a subgroup analysis of our previous work,7 we showed similar readmission rates between the Vancouver Coastal Region and the rest of British Columbia. As with all observational studies, patients were not randomized to RF or cryoballoon therapy, and we attempted to account for differences between the groups with multivariable analysis. Nonetheless, residual bias and confounding may have masked a true difference between the groups. Finally, given the observational nature of the study, this analysis could not establish whether same-day discharge has a meaningfully different rate of healthcare utilization than routine overnight admissions.
Conclusions
Routine same-day discharge was feasible in the vast majority of patients who underwent AF ablation. We observed no difference in the rates of same-day discharge between RF and cryoballoon ablation, and both modalities had similar readmission and ER visit rates at 30 days. Complications after same-day discharge were low. However, ER visit rates in the first month after ablation were high, regardless of same-day discharge or overnight stay, and more work is needed to prevent unnecessary healthcare utilization post ablation.
Supplementary Material
Acknowledgements
This work would not have been possible without the tireless efforts of Kathy Big-Gee Lee BSN, who was tragically taken from this world too soon. May her soul rest in peace.
Contributor Information
Marc W Deyell, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7; Centre for Cardiovascular Innovation, University of British Columbia, 2775 Laurel Street, 9th Floor, Vancouver, BC, Canada V5Z 1M9.
Kurt Hoskin, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7.
Jacqueline Forman, St. Paul's Hospital, Providence Health Care, 1081 Burrard Street, Vancouver, BC, Canada V6Z 1Y6.
Zachary W Laksman, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7; Centre for Cardiovascular Innovation, University of British Columbia, 2775 Laurel Street, 9th Floor, Vancouver, BC, Canada V5Z 1M9.
Nathaniel M Hawkins, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7; Centre for Cardiovascular Innovation, University of British Columbia, 2775 Laurel Street, 9th Floor, Vancouver, BC, Canada V5Z 1M9.
Matthew T Bennett, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7; Centre for Cardiovascular Innovation, University of British Columbia, 2775 Laurel Street, 9th Floor, Vancouver, BC, Canada V5Z 1M9.
John A Yeung-Lai-Wah, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7.
Santabhanu Chakrabarti, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7.
Andrew D Krahn, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7; Centre for Cardiovascular Innovation, University of British Columbia, 2775 Laurel Street, 9th Floor, Vancouver, BC, Canada V5Z 1M9.
Jason G Andrade, Division of Cardiology, Department of Medicine, University of British Columbia, #200-1033 Davie Street, Vancouver, BC, Canada V6E 1M7; Centre for Cardiovascular Innovation, University of British Columbia, 2775 Laurel Street, 9th Floor, Vancouver, BC, Canada V5Z 1M9.
Supplementary material
Supplementary material is available at Europace online.
Funding
This work was supported in part by the Division of Cardiology Academic Practice Plan, Faculty of Medicine, University of British Columbia (M.W.D.).
Data Availability
The data from this study are available from the corresponding author, upon reasonable request.
References
- 1. Kaoutskaia A, Shurrab M, Amit G, Parkash R, Exner D, Toal Set al. . Canadian national electrophysiology ablation registry report 2011–2016. BMC Health Serv Res 2021;21:435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Andrade JG, Wazni OM, Kuniss M, Hawkins NM, Deyell MW, Chierchia GBet al. . Cryoballoon ablation as initial treatment for atrial fibrillation: JACC state-of-the-art review. J Am Coll Cardiol 2021;78:914–30. [DOI] [PubMed] [Google Scholar]
- 3. Tripathi B, Arora S, Kumar V, Abdelrahman M, Lahewala S, Dave Met al. . Temporal trends of in-hospital complications associated with catheter ablation of atrial fibrillation in the United States: an update from Nationwide Inpatient Sample database (2011–2014). J Cardiovasc Electrophysiol 2018;29:715–24. [DOI] [PubMed] [Google Scholar]
- 4. Noseworthy PA, Kapa S, Haas LR, Van Houten H, Deshmuk AJ, Mulpuru SKet al. . Trends and predictors of readmission after catheter ablation for atrial fibrillation, 2009–2013. Am Heart J 2015;170:483–9. [DOI] [PubMed] [Google Scholar]
- 5. Andrade JG, Champagne J, Dubuc M, Deyell MW, Verma A, Macle Let al. . Cryoballoon or radiofrequency ablation for atrial fibrillation assessed by continuous monitoring: a randomized clinical trial. Circulation 2019;140:1779–88. [DOI] [PubMed] [Google Scholar]
- 6. Bartoletti S, Mann M, Gupta A, Khan AM, Sahni A, El-Kadri Met al. . Same-day discharge in selected patients undergoing atrial fibrillation ablation. Pacing Clin Electrophysiol 2019;42:1448–55. [DOI] [PubMed] [Google Scholar]
- 7. Deyell MW, Leather RA, Macle L, Forman J, Khairy P, Zhang Ret al. . Efficacy and safety of same-day discharge for atrial fibrillation ablation. JACC Clin Electrophysiol 2020;6:609–19. [DOI] [PubMed] [Google Scholar]
- 8. Opel A, Mansell J, Butler A, Schwartz R, Fannon M, Finlay Met al. . Comparison of a high throughput day case atrial fibrillation ablation service in a local hospital with standard regional tertiary cardiac centre care. Europace 2018;21:440–4. [DOI] [PubMed] [Google Scholar]
- 9. Reddy SA, Nethercott SL, Chattopadhyay R, Heck PM, Virdee MS. Safety, feasibility and economic impact of same-day discharge following atrial fibrillation ablation. Heart Lung Circ 2020;29:1766–72. [DOI] [PubMed] [Google Scholar]
- 10. Creta A, Ventrella N, Providência R, Earley MJ, Sporton S, Dhillon Get al. . Same-day discharge following catheter ablation of atrial fibrillation: a safe and cost-effective approach. J Cardiovasc Electrophysiol 2020;31:3097–103. [DOI] [PubMed] [Google Scholar]
- 11. Kowalski M, Parikh V, Salcido JR, Chalfoun N, Albano A, O’Neill PGet al. . Same-day discharge after cryoballoon ablation of atrial fibrillation: a multicenter experience. J Cardiovasc Electrophysiol 2021;32:183–90. [DOI] [PubMed] [Google Scholar]
- 12. König S, Svetlosak M, Grabowski M, Duncker D, Nagy VK, Bogdan Set al. . Utilization and perception of same-day discharge in electrophysiological procedures and device implantations: an EHRA survey. Europace 2020;23:149–56. [DOI] [PubMed] [Google Scholar]
- 13. Andrade JG, Champagne J, Dubuc M, Deyell MW, Verma A, Macle Let al. . Cryoballoon or radiofrequency ablation for atrial fibrillation assessed by continuous monitoring. Circulation 2019;140:1779–88. [DOI] [PubMed] [Google Scholar]
- 14. He H, Datla S, Weight N, Raza S, Lachlan T, Aldhoon Bet al. . Safety and cost-effectiveness of same-day complex left atrial ablation. Int J Cardiol 2021;322:170–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ignacio DM, Jarma DJJ, Nicolas V, Gustavo D, Leandro T, Milagros Cet al. . Current safety of pulmonary vein isolation in paroxysmal atrial fibrillation: first experience of same day discharge. J Atr Fibrillation 2018;11:2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Akula DN, Mariam W, Luthra P, Edward F, Katz DJ, Levi S Aet al. . Safety of same day discharge after atrial fibrillation ablation. J Atr Fibrillation 2020;12:2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data from this study are available from the corresponding author, upon reasonable request.