Abstract
Transurethral enucleation and resection of prostate (TUERP), as one of the conventional surgical methods for patients with benign prostatic hyperplasia (BPH), usually resulted in pseudo urinary incontinence after surgery. The present study was thereby conducted to evaluate the feasibility of anterior lobe-preserving transurethral enucleation and resection of prostate (ALP-TUERP) on reducing the incidence rate of urinary incontinence after surgery in patients with BPH. Patients diagnosed with BPH underwent surgical treatment were enrolled in the present study within the inclusion criteria. Characteristics including age, prostate volume (before surgery), PSA level, maximum free flow rate, international prostate symptom score, and quality of life were reviewed and compared between the groups of ALP-TUERP and TUERP. Incidence rate of urinary incontinence on 24 hours, 3 days, 7 days, and 14 days after catheter drawing was deemed as main outcome, which was compared between the groups. In addition, secondary outcomes including surgery time, difference value of hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, catheter flushing time, and incidence rate of recurrent bleeding were also compared between the groups. There were 81 patients included in the present study within the inclusion criteria. There was no statistical difference on the baseline characteristics including age, prostate volume (before surgery), PSA level, maximum free flow rate (before surgery), international prostate symptom score, or quality of life between the 2 groups. Statistical superiority was observed on the incidence rate of urinary incontinence on day 1 (χ2 = 9.375, P = .002), and day 3 (χ2 = 4.046, P = .044) in the group ALP-TUERP, when comparing to group TUERP. However, the difference was not observed anymore after 7 days after catheter drawing (P = .241 for day 7, P = .494 for day 14) between them. In addition, no statistical differences were observed on surgery time, difference value of hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, or catheter flushing time between the group ALP-TUERP and TUERP (all P > .05). Results of the present study demonstrated a potentially statistical superiority of ALP-TUERP on the reduction of incidence rate of urinary incontinence comparing to conventionally TUERP.
Keywords: anterior lobe, benign prostatic hyperplasia, retrospective, transurethral enucleation and resection of prostate, urinary incontinence
1. Introduction
Benign prostatic hyperplasia (BPH), as the nonmalignant growth or hyperplasia of the prostate tissue, which has emerged as the most common benign clinical progressive disease causing urination disorders in middle-aged and elderly men.[1] The incidence rate of BPH in men older than fifty years is as high as 50%, and remaining increasing with age.[2,3] Histologically, BPH is mainly presented as hyperplasia of prostatic interstitial and glandular components. In anatomy, the main manifestation is the enlargement of the prostate, within the main manifestation of urinary flow mechanics being bladder outlet obstruction. In patients with severe BPH, the progress of the disease usually leads to significant lower urinary tract symptoms (LUTS) including frequent urination, urgency to urinate, incontinence, and thereby resulted in renal impairment or even renal failure.[4,5]
There have been several therapeutic measures including watchful waiting, eating behavior adjustment, medication, and surgery recommended as treatment strategies for BPH.[6,7] Among those, surgery of prostatectomy has been considered as the most effective choice for patients with severe BPH. Among the various surgical methods including open prostatectomy, laser transurethral resection of prostate, bipolar transurethral enucleation of the prostate, photoselective vaporization of the prostate, and prostatic artery embolization, transurethral resection of the prostate (TURP) was recommended as the gold standard for surgical treatment of BPH, because it provided a significant improvement in symptoms.[8–10] However, TURP causes several common complications including urinary tract infection, bleeding, and postoperative urinary retention.[10] In addition, there is little advantage on the improvement of the urine flow rate for TURP comparing to open prostatectomy. In recent years, a novel surgical method named transurethral enucleation and resection of prostate (TUERP) has been reported by Liu et al, and frequently used in clinical practice in China.[11] The most significant feature of the surgical method is that it changes the way to remove the prostate. Specifically speaking, the lens sheath of the electroscope is used to imitate the finger movements in open surgery, with the middle and left glands of the hyperplasia of the prostate being bluntly separated step by step along the prostate surgical capsule with the verumonum and bladder neck as markers. The gland is met at 12 o’clock, with the exact hemostasis been obtained under the direct vision of electroscope. With that manner, there is no communication between the gland under blunt dissection and the vessels supplying the gland with the surgical envelope, thereby the amount of blood loss was greatly reduced, and the absorption of lavage fluid also been greatly reduced. Finally, the removed prostate was chopped up in vivo and flushed out.[11] However in clinical practice, it was found that a majority patients suffered urinary incontinence, especially pseudo urinary incontinence several days after surgery, which influenced quality of life (QoL) significantly. The potentially mechanism has been considered that blunt separation during enucleation may cause injury to the urethral sphincter, especially urethral sphincter in front of the anterior lobe of the prostate, and thereby resulted in temporary dysfunction of the urethral sphincter.
Hence in the present study, we conducted the retrospective cohort study, aiming to evaluate the feasibility of anterior lobe-preserving transurethral enucleation and resection of prostate (ALP-TUERP) on improving urinary incontinence in patients with BPH.
2. Patients and methods
2.1. Data source and patient selection
Patients diagnosed with BPH underwent surgical treatment from January 1st 2020 to June 30th, 2022 in People’s Hospital of Xiangxiang were reviewed and screened with the inclusion criteria. All the included patients received the operation procedure of ALP-TUERP (Groups research) or TUERP (Group control) as surgical treatment. Clinical characteristics including age, prostate volume (before surgery), PSA level, maximum free flow rate (Qmax, before surgery), international prostate symptom score (IPSS), and QoL were extracted and compared between the groups. The inclusion criteria adopted in the present study were presented as below: Male patients diagnosed as BPH within the age between 60 and 85 years old; Recurrent urinary retention (inability to urinate after at least one removal of catheter); Maximum free flow rate (less than 15 mL/s) before surgery. The exclusion criteria adopted in the present study were presented as below: BPH accompanied with central system disease or neurogenic bladder; Urethral stricture; Inability to tolerate surgery by any reasons; Prostate cancer patients; Bladder stones cannot be cleared through the urethra. The resection method was chosen by patients themselves, within an informed consent form of the operation signed by patients or their relatives. Specifically, patients included in the present study had received either a prostate ultrasound or a prostate MRI examination to evaluate the volume of prostates before the surgery. For prostates larger than 80 mL, 2/3 of the anterior lobe was retained during the surgery. However, for prostates less than 80 mL, 1/3 of the anterior lobe was retained. In addition, age is also considered as an important factor before surgery. In patients over 70, the retaining of anterior lobe should be much more than that in patients less than 70 years old, which depends on the experience of the surgeon (Xin Huang). This study was approved by the ethical committee of the People’s Hospital of Xiangxiang. All investigations in the present study were performed in accordance with the Declaration of Helsinki (Revised in 2013). Written informed consent was obtained from the patients or their families before the study. All personal information of included patients was de-identified in the preparation and presentation of the present study. The reporting of the research conforms to the STROBE guidelines.
2.2. Surgical procedure
Surgical operations of all the included patients were performed by a same surgeon (HX). Patients have completed all routine examinations before surgery. Combined spinal-epidural anesthesia was adopted during the whole management of the resection, with ECG monitoring and blood oxygen saturation monitoring been performed during the procedure.
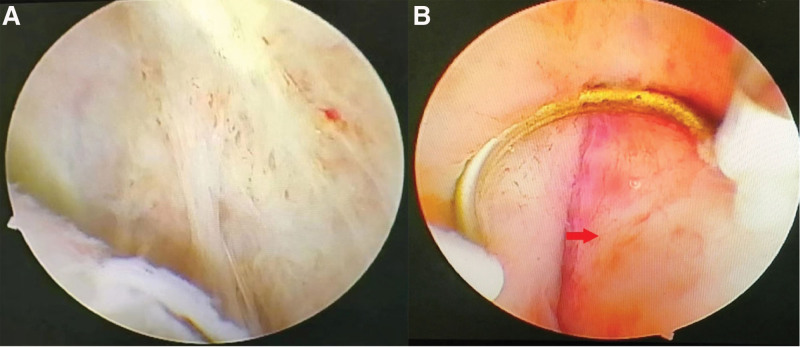
The electric microscope sheath was extended to the prostate capsule in an arc from the proximal verumoncus to the left lobe, with the capsule plane expanding counterclockwise to the 12 o ‘clock direction. Partial distal gland was retained during the expansion of the plane. Bladder neck was cut off by electricity. Subsequently, the electric microscope sheath was extended to the prostate capsule in the proximal verumoncus to the right lobe in an arc, with the capsule plane expanding clockwise. Meanwhile, the bladder neck at 7 o ‘clock was retained. Finally, the gland is removed, chopped up in vivo and flushed out. The principle of anterior lobe retention is depended on the age of the patient and the size of the patient’s prostate, details of which have been described above. The surgical operation of ALP-TUERP was presented in Figure 1.
Figure 1.
Surgical operation of ALP-TUERP. (A) Transurethral enucleation and resection of prostate. (B) Preserved anterior lobe (red arrow). ALP-TUERP = anterior lobe-preserving transurethral enucleation and resection of prostate.
2.3. Outcome measures
The primary outcome in the present study was the incidence rate of urinary incontinence, which was evaluated at the time points on 24 hours, 3 days, 7 days, and 14 days after catheter drawing. The incidence rate of urinary incontinence was assessed by 1-hour pad test, of which testing protocol has been standardized by International Continence Society (ICS-pad test).[12] The bladder must be emptied (urination) before the test. Patients should drink 500 mL of warm water within 15 minutes at the beginning of the test. The procedure was conducted as following. The test is started by putting 1 pre-weighted pad without patient voiding; Patient walks for 30 minutes, including climbing 1 flight of stairs (up and down); Patient performs the following activities: standing up from sitting (10×), coughing vigorously (10×), running on the spot for 1 minute, bending to pick up an object from the floor (5×), and washing hands in running water for 1 minute (this activity program may be modified according to the patient’s physical fitness); The total amount of urine leaked is determined by weighing the pad; If a moderately full bladder cannot be maintained through the hour (if the patient must void), the test has to be started again. At the end of the 1-hour test, the urine pad was weighed. The weight of the dry pad was subtracted, which was deemed as the weight of urine leakage. If the pad gained more than 1 gram, the result was positive, otherwise being negative. The secondary outcomes in the present study included surgery time, difference value of Hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, catheter flushing time, and incidence rate of recurrent bleeding between the 2 groups. Catheter flushing time refers to the duration from the ending of the operation to the ending of bladder irrigation. The procedure of continuous bladder irrigation is a necessary progress after surgery for all the included patients, aiming to avoiding catheter obstruction by blood clot. The procedure of continuous bladder irrigation should be continued until the emerging of urine clean (first time), without gross hematuria (first time). Catheter retaining time refers to the time from the end of the operation to the removal of the catheter. At the time of the emerging of urine clean without gross hematuria (first time), the continuous bladder irrigation is terminated. However, without continuous bladder irrigation, the gross hematuria would be recurrent. In consideration of that, we suggested the included patients to drink water at a dose of more than 2000 mL a day to relieve gross hematuria. During that time, the catheter was retained for hemostasis by compression, as well as drainage of urine. The catheter removal was performed until the emerging of urine clean without gross hematuria at second time. Then the catheter would be removed. Baseline characteristics included age, prostate volume (before surgery), PSA level, Qmax (before surgery), IPSS, and QoL were assessed 1 week before the surgery performed.
2.4. Statistical analysis
Descriptive data including prostate volume (before surgery), PSA level, Qmax (before surgery), IPSS, and QoL were presented with mean ± standard deviation, which were compared with independent-samples t test. Age of the included patients was described as median and range. The comparative incidence rate of urinary incontinence between the groups was performed with chi-square test, or Fisher exact test if necessary. Secondary clinical outcomes including surgery time, difference value of Hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, and catheter flushing time were also presented with mean ± standard deviation, and compared within independent-samples t test. Comparison of incidence rate of recurrent bleeding between the 2 groups was conducted in Fisher exact test. All statistical analyses were performed with IBM SPSS 23.0 software (IBM Corp., Armonk, NY). P values <.05 were considered significant.
3. Results
During January 1, 2020 to June 30, 2022 in People’s Hospital of Xiangxiang, there were 81 patients included in the present study within the inclusion criteria. Forty-one patients were treated with ALP-TUERP and the other forty patients been treated with conventional TUERP in the control group. There was no statistical difference on the baseline characteristics including age, prostate volume (before surgery), PSA level, Qmax (before surgery), IPSS, or QoL between the 2 groups (Table 1).
Table 1.
Baseline characteristics of patients with benign prostatic hyperplasia.
| ALP-TUERP (n = 41) | TUERP (n = 40) | P value | |
|---|---|---|---|
| Age | 70 (56, 88) | 71 (58, 84) | .912 |
| Prostate volume (mL3) | 76.63 ± 38.44 | 83.25 ± 30.17 | .258 |
| PSA (μg/L) | 3.62 ± 1.77 | 3.06 ± 1.39 | .677 |
| Qmax (mL/s) | 7.52 ± 2.64 | 7.78 ± 2.12 | .513 |
| IPSS | 24.71 ± 3.12 | 25.19 ± 2.84 | .473 |
| QoL | 4.39 ± 1.15 | 4.22 ± 1.07 | .825 |
ALP-TUERP = anterior lobe-preserving transurethral enucleation and resection of prostate, IPSS = international prostate symptom score, Qmax = maximum free flow rate, QoL = quality of life, TUERP = transurethral enucleation and resection of prostate.
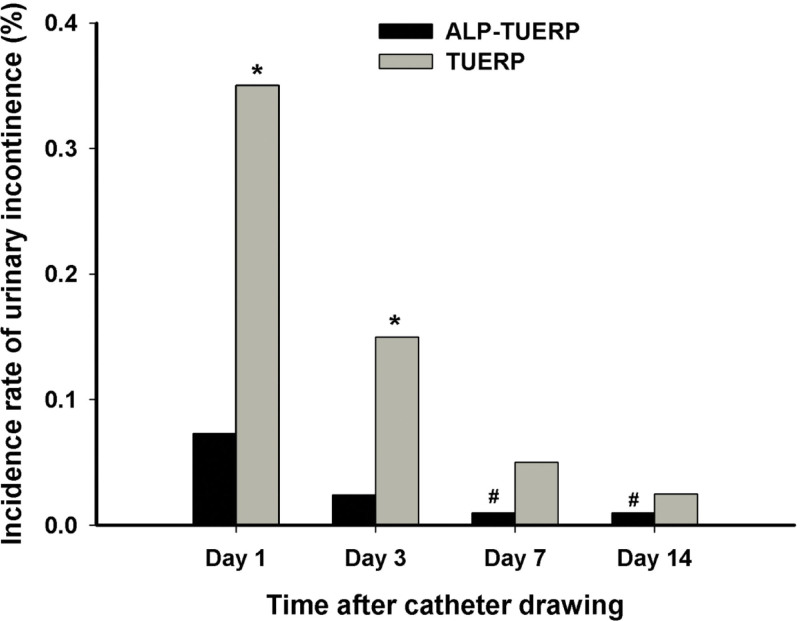
All the included patients were discharged successfully after the surgery. One-hour past test was performed at the time points of 24 hours (Day 1), 3 days, 7 days, and 14 days after the catheter drawing. There was statistical difference observed on the incidence rate of urinary incontinence on day 1 (χ2 = 9.375, P = .002), and day 3 (χ2 = 4.046, P = .044) between the group ALP-TUERP and group TUERP, respectively. However, the difference was not observed anymore after 7 days after catheter drawing (P = .241 for day 7, P = .494 for day 14) between them. The results were presented in Figure 2.
Figure 2.
Incidence rate of urinary incontinence on days 1, 3, 7, and 14 after the catheter drawing of ALP-TUERP or TUERP. *P < .05. # there was no patient in the group ALP-TUERP suffering urinary incontinence any more. The value here was assigned artificially as 0.001 to show the histogram for good understanding. ALP-TUERP = anterior lobe-preserving transurethral enucleation and resection of prostate, TUERP = transurethral enucleation and resection of prostate.
In terms to secondary outcomes, there was no statistical difference observed on surgery time, difference value of hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, or catheter flushing time between the group ALP-TUERP and TUERP (all P > .05). The descriptive data of surgery time, difference value of hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, and catheter flushing time were presented with Mean ± SD, which were showed in Table 2. The comparative results with 95% CI were also demonstrated in the Table 2.
Table 2.
Secondary clinical outcomes for the included patients between the groups (n = 81).
| ALP-TUERP (mean ± SD) | TUERP (mean ± SD) | P value | 95% CI | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Surgery time (min) | 57.15 + 8.946 | 56.58 + 8.311 | .101 | −0.917 | 0.0819 |
| ∆Hemoglobin | 7.105 + 2.699 | 7.491 + 3.095 | .221 | −1.006 | 0.234 |
| Catheter retaining (d) | 6.846 + 1.226 | 6.729 + 0.073 | .265 | −0.885 | 0.321 |
| Catheter flushing (d) | 2.612 + 0.782 | 2.832 + 0.852 | .057 | −0.445 | 0.006 |
| Recurrent bleeding | N/A | N/A | .512* | N/A | N/A |
∆Hemoglobin = Difference value of hemoglobin before and after surgery, ALP-TUERP = anterior lobe-preserving transurethral enucleation and resection of prostate, N/A = not applicable, TUERP = transurethral enucleation and resection of prostate.
Fisher exact test was adopted.
Postoperative adverse events were evaluated with the parameters of incidence rate of recurrent bleeding, which was also presented in the Table 2. There was no significant difference observed on the incidence rate of recurrent bleeding between the groups (P = .512). Otherwise, there was no other complication reported among the enrolled patients.
4. Discussion
Postoperative urinary incontinence, especially short-term urinary incontinence has been emerged as one of the most common complications after the surgery of BPH, which comes to be the main reason of postoperative anxiety and fear of surgery. The present retrospective cohort study was thereby conducted to evaluate the feasibility and efficacy of ALP-TUERP on reducing the incidence rate of urinary incontinence in patients with BPH. Accordingly, results of the present study demonstrated a statistical superiority of ALP-TUERP on the reduction of incidence rate of urinary incontinence, especially in 3 days after catheter drawing when compared to conventionally TUERP. In addition, there was no disadvantage observed on the comparison including surgery time, difference value of hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, or catheter flushing time between the group ALP-TUERP and TUERP. To the best of our knowledge, this is the first research conducted to investigate the feasibility of ALP-TUERP on improving urinary incontinence in patients with BPH. We expected that the presentation of the research would provide clinical thought for physicians in practice.
As a chronic progressive disease, BPH usually presents a long disease course, with its incidence increasing gradually with age. BPH initially occurs after age forty years old, within more than half of men suffering BPH after 60 years of age, and at the age of 80 the ratio reached 83%.[13] A majority of patients diagnosed with BPH usually presented with LUTS including dysuresia, frequent urination, urgent urination, and painful urination. Approximately a quarter of patients with LUTS need surgical treatment of BPH finally.[14] In recent years, with the improvement of patients’ requirements for QoL postoperatively, postoperative urinary incontinence, especially pseudo urinary incontinence, has emerged as a main reason leading to patients’ fear of surgery. In terms of postoperative urinary incontinence prevention, we believe that the key problem during the operation procedure is how to protect the urethral sphincter, which also becomes the main problem to delay the postoperative recovery of patients. Because the anterior lobe of the prostate is adjacent to the urethral sphincter and connected by the urethral mucosal tissue, excessive resection during the operation may directly lead to postoperative urethral sphincter function impairment and urinary incontinence symptoms.[15] In addition, BPH mainly occurs in the transitional region of the prostate, with its clinical manifestations mainly being hyperplasia in the bilateral lobe and middle lobe. However, there exist few glands in anterior lobe, which is close to the half-moon urethral sphincter. Electrical and thermal stimulation or blunt separation and pulling generated during the operation of electric incision or ensnusion may lead to urethral sphincter injury directly. In addition, the symptom of pseudo incontinence also results from the traction of the urethral sphincter during the surgery or physical inadaptation after the sudden removal of the prostate. Hence, the preservation of the anterior lobe might avoid the risks, and the posterior urethra length preserving during surgery may also stands as the main strategy to avoid postoperative incontinence.[16,17] Therefore, we considered that it might be particularly important to retain the anterior lobe of the prostate and the relevant urethral mucosa during the operation procedure.
During the resection procedure of ALP-TUERP in the present study, anterior lobe of the prostate was retained, rather than total resection in the group TUERP. Accordingly, the incidence rate of postoperative urinary incontinence in group ALP-TUERP was significant lower than that in group TUERP (3/41 vs 14/40, P = .002). Most of the patients who received the operation of ALP-TUERP discharged rapidly after catheter drawing. They were satisfactory with the superior outcomes of the surgical method of ALP-TUERP, when compared to the conventional TUERP. In addition, there were no additional adverse events including surgery time, difference value of hemoglobin before and after surgery (∆Hemoglobin), catheter retaining time, catheter flushing time, or incidence rate of recurrent bleeding observed between the groups. In addition in the present study, rehabilitation therapy including pelvic floor muscle function exercise and lifestyle adjustment, which has been recommend as standard operation after surgery of prostate, was also adopted among all the included patients.[17,18] We believe that the comprehensive application of surgical method, as well as the postoperative rehabilitation therapy, may systematically contribute to the recovery of BPH patients after surgery, which is also in line with the concept of enhanced recovery after surgery in recent years.[19–21] As mentioned before, the clinical application of TUERP was widely used in China, rather than western countries in recent years, which lead to the deficiency of relative literatures published. Even so, we hope the presentation of the preliminary research might be meaningful for urologists.
There exist several limitations in the present study described as below. Firstly, observation period of the present study was only for 4 weeks after surgery. Long-term dynamic evaluation for a longer period, especially to identify the recurrence status of BPH between the groups is required. Secondly, the research was performed in a single center within the nature of retrospective cohort study. Further demonstration in a larger sample, with prospective design might be necessary to identify the feasibility further.
5. Conclusion
Totally, the present retrospective cohort study was conducted to evaluate the feasibility and efficacy of ALP-TUERP on reducing the incidence rate of urinary incontinence in patients with BPH. Accordingly, results of the present study demonstrated a statistical superiority of ALP-TUERP on the reduction of incidence rate of urinary incontinence when compared to conventionally TUERP.
Acknowledgments
The authors thank the patients for their participation and agreement to publication of the study.
Author contributions
Conceptualization: Xin Huang.
Data curation: Xin Huang, Liang Wang.
Formal analysis: Xin Huang.
Investigation: Xu Chen.
Software: Xi Xiang Chen.
Validation: Qiao Zhi Chen.
Visualization: Cang Li.
Writing – original draft: Xin Huang.
Writing – review & editing: Jin Lian Tian.
Abbreviations:
- ALP-TUERP
- anterior lobe-preserving transurethral enucleation and resection of prostate
- BPH
- benign prostatic hyperplasia
- IPSS
- international prostate symptom score
- LUTS
- lower urinary tract symptoms
- QoL
- quality of life
- TUERP
- transurethral enucleation and resection of prostate
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
The publication of the present study details was approved by the ethical committee of the People’s Hospital of Xiangxiang.
Written informed consent was obtained from the patients or their relatives for publication of this study and any accompanying images.
The study was funded by a project supported by Scientific Research Fund of Hunan Provincial Education Department (20C0207).
The authors have no conflicts of interest to disclose.
How to cite this article: Huang X, Chen XX, Chen X, Chen QZ, Wang L, Li C, Tian JL. Feasibility of anterior lobe-preserving transurethral enucleation and resection of prostate on improving urinary incontinence in patients with benign prostatic hyperplasia: A retrospective cohort study. Medicine 2023;102:7(e32884).
Contributor Information
Xi Xiang Chen, Email: 1586542369@qq.com.
Xu Chen, Email: 1586542369@qq.com.
Qiao Zhi Chen, Email: 1586542369@qq.com.
Liang Wang, Email: 22541943@qq.com.
Cang Li, Email: licang0928@sina.com.
Jin Lian Tian, Email: 2240618896@qq.com.
References
- [1].Bushman W. Etiology, epidemiology, and natural history of benign prostatic hyperplasia. Urol Clin North Am. 2009;36:403–15, v. [DOI] [PubMed] [Google Scholar]
- [2].Verhamme KM, Dieleman JP, Bleumink GS, et al. Incidence and prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in primary care--the Triumph project. Eur Urol. 2002;42:323–8. [DOI] [PubMed] [Google Scholar]
- [3].Langan RC. Benign prostatic hyperplasia. Prim Care. 2019;46:223–32. [DOI] [PubMed] [Google Scholar]
- [4].Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013;64:118–40. [DOI] [PubMed] [Google Scholar]
- [5].Berges R, Oelke M. Age-stratified normal values for prostate volume, PSA, maximum urinary flow rate, IPSS, and other LUTS/BPH indicators in the German male community-dwelling population aged 50 years or older. World J Urol. 2011;29:171–8. [DOI] [PubMed] [Google Scholar]
- [6].Netto NR, Jr., de Lima ML, Netto MR, et al. Evaluation of patients with bladder outlet obstruction and mild international prostate symptom score followed up by watchful waiting. Urology. 1999;53:314–6. [DOI] [PubMed] [Google Scholar]
- [7].Yap T, Emberton M. Behaviour modification and benign prostatic hyperplasia: replacement for medications. Curr Opin Urol. 2010;20:20–7. [DOI] [PubMed] [Google Scholar]
- [8].Zwergel U, Wullich B, Lindenmeir U, et al. Long-term results following transurethral resection of the prostate. Eur Urol. 1998;33:476–80. [DOI] [PubMed] [Google Scholar]
- [9].McVary KT, Roehrborn CG, Avins AL, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185:1793–803. [DOI] [PubMed] [Google Scholar]
- [10].Wasson JH, Reda DJ, Bruskewitz RC, et al. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med. 1995;332:75–9. [DOI] [PubMed] [Google Scholar]
- [11].Chunxiao L. Research progress on transurethral enucleation and resection of prostate. J Minim Invasive Med. 2015;10:263–8. [Google Scholar]
- [12].Krhut J, Zachoval R, Smith PP, et al. Pad weight testing in the evaluation of urinary incontinence. Neurourol Urodyn. 2014;33:507–10. [DOI] [PubMed] [Google Scholar]
- [13].Mostafa MM, Khallaf A, Khalil M, et al. Efficacy and safety of transurethral resection of the prostate, holmium laser enucleation of the prostate, and photoselective vaporization of the prostate in management of overactive bladder symptoms complicating benign prostatic hyperplasia in patients with moderately enlarged prostates: a comparative study. Can Urol Assoc J. 2022. [Google Scholar]
- [14].Al Demour SH, Abuhamad M, Santarisi AN, et al. The effect of transurethral resection of the prostate on erectile and ejaculatory functions in patients with benign prostatic hyperplasia. Urol Int. 2022;106:997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Zhang J, Wang Y, Li S, et al. Efficacy and safety evaluation of transurethral resection of the prostate versus plasmakinetic enucleation of the prostate in the treatment of massive benign prostatic hyperplasia. Urol Int. 2021;105:735–42. [DOI] [PubMed] [Google Scholar]
- [16].Grechenkov AS, Glybochko PV, Alyaev YG, et al. [Risk factors for anterior urethral strictures after transurethral resection of benign prostatic hyperplasia]. Urologiia. 2015:62–5. [PubMed] [Google Scholar]
- [17].Goyal NK, Goel A, Sankhwar S, et al. Transurethral resection of prostate abscess: is it different from conventional transurethral resection for benign prostatic hyperplasia? ISRN Urol. 2013;2013:109505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Goode PS, Burgio KL, Johnson TM, 2nd, et al. Behavioral therapy with or without biofeedback and pelvic floor electrical stimulation for persistent postprostatectomy incontinence: a randomized controlled trial. JAMA. 2011;305:151–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Lone Z, Zhang A, Benidir T, et al. The role of enhanced recovery after surgery protocols in the development of acute kidney injury following radical cystectomy. Urol Oncol. 2022;40:453 e1–e7. [DOI] [PubMed] [Google Scholar]
- [20].Developed by the Joint Writing Group of the International Urogynecological Association and the American Urogynecologic Society. AUGS-IUGA Joint clinical consensus statement on enhanced recovery after urogynecologic surgery. Int Urogynecol J. 2022;33:2921–40. [DOI] [PubMed] [Google Scholar]
- [21].Latthe P, Panza J, Marquini GV, et al. AUGS-IUGA Joint Clinical Consensus Statement on Enhanced Recovery After Urogynecologic Surgery: Developed by the Joint Writing Group of the International Urogynecological Association and the American Urogynecologic Society. Individual writing group members are noted in the Acknowledgements section. Urogynecology (Hagerstown). 2022;28:716–34. [DOI] [PubMed] [Google Scholar]