Abstract
Background
In many countries, national, regional and local inter‐ and intra‐agency collaborations have been introduced to improve health outcomes. Evidence is needed on the effectiveness of locally developed partnerships which target changes in health outcomes and behaviours.
Objectives
To evaluate the effects of interagency collaboration between local health and local government agencies on health outcomes in any population or age group.
Search methods
We searched the Cochrane Public Health Group Specialised Register, AMED, ASSIA, CENTRAL, CINAHL, DoPHER, EMBASE, ERIC, HMIC, IBSS, MEDLINE, MEDLINE In‐Process, OpenGrey, PsycINFO, Rehabdata, Social Care Online, Social Services Abstracts, Sociological Abstracts, TRoPHI and Web of Science from 1966 through to January 2012. 'Snowballing' methods were used, including expert contact, citation tracking, website searching and reference list follow‐up.
Selection criteria
Randomized controlled trials (RCTs), controlled clinical trials (CCTs), controlled before‐and‐after studies (CBAs) and interrupted time series (ITS) where the study reported individual health outcomes arising from interagency collaboration between health and local government agencies compared to standard care. Studies were selected independently in duplicate, with no restriction on population subgroup or disease.
Data collection and analysis
Two authors independently conducted data extraction and assessed risk of bias for each study.
Main results
Sixteen studies were identified (28,212 participants). Only two were considered to be at low risk of bias. Eleven studies contributed data to the meta‐analyses but a narrative synthesis was undertaken for all 16 studies. Six studies examined mental health initiatives, of which one showed health benefit, four showed modest improvement in one or more of the outcomes measured but no clear overall health gain, and one showed no evidence of health gain. Four studies considered lifestyle improvements, of which one showed some limited short‐term improvements, two failed to show health gains for the intervention population, and one showed more unhealthy lifestyle behaviours persisting in the intervention population. Three studies considered chronic disease management and all failed to demonstrate health gains. Three studies considered environmental improvements and adjustments, of which two showed some health improvements and one did not.
Meta‐analysis of three studies exploring the effect of collaboration on mortality showed no effect (pooled relative risk of 1.04 in favour of control, 95% CI 0.92 to 1.17). Analysis of five studies (with high heterogeneity) looking at the effect of collaboration on mental health resulted in a standardised mean difference of ‐0.28, a small effect favouring the intervention (95% CI ‐0.51 to ‐0.06). From two studies, there was a statistically significant but clinically modest improvement in the global assessment of function symptoms score scale, with a pooled mean difference (on a scale of 1 to 100) of ‐2.63 favouring the intervention (95% CI ‐5.16 to ‐0.10).
For physical health (6 studies) and quality of life (4 studies) the results were not statistically significant, the standardised mean differences were ‐0.01 (95% CI ‐0.10 to 0.07) and ‐0.08 (95% CI ‐0.44 to 0.27), respectively.
Authors' conclusions
Collaboration between local health and local government is commonly considered best practice. However, the review did not identify any reliable evidence that interagency collaboration, compared to standard services, necessarily leads to health improvement. A few studies identified component benefits but these were not reflected in overall outcome scores and could have resulted from the use of significant additional resources. Although agencies appear enthusiastic about collaboration, difficulties in the primary studies and incomplete implementation of initiatives have prevented the development of a strong evidence base. If these weaknesses are addressed in future studies (for example by providing greater detail on the implementation of programmes; using more robust designs, integrated process evaluations to show how well the partners of the collaboration worked together, and measurement of health outcomes) it could provide a better understanding of what might work and why. It is possible that local collaborative partnerships delivering environmental Interventions may result in health gain but the evidence base for this is very limited.
Evaluations of interagency collaborative arrangements face many challenges. The results demonstrate that collaborative community partnerships can be established to deliver interventions but it is important to agree goals, methods of working, monitoring and evaluation before implementation to protect programme fidelity and increase the potential for effectiveness.
Plain language summary
Collaboration between local health and local government agencies for health improvement
Since the 1980s, national and international health organisations have promoted partnerships between health and other public services at a local level to improve the health of the population. This review looked for evidence on whether collaboration does or does not work when compared to standard services.
Of the two good quality studies identified, one showed no evidence that collaboration between local services improved health and the other showed a modest improvement in some areas. Of the remaining studies, where health benefits were reported these were often modest, inconsistent with other findings and could have been the result of additional funding or resources. Two out of three studies looking at environmental changes reported some health benefits.
These findings show that when comparing local collaborative partnerships between health and government agencies with standard working arrangements, there is generally no difference in health outcomes.
Summary of findings
Summary of findings for the main comparison. Overview of studies.
| Interventions for health improvement in all populations | ||||||
| Outcomes | Intervention and Comparison intervention | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Comments | |
| Assumed risk | Corresponding risk | |||||
| With comparator | With intervention | |||||
| Mortality | ||||||
| Mortality/health improvement | Study population | RR 1.04 (0.92 to 1.17) | 1994 (3) | |||
| 347 per 1000 | 352 per 1000 | |||||
| Mental Health | ||||||
| Morbidity/health improvement | The mean mental health score in the intervention groups was 0.28 standard deviations lower, a small effect favouring intervention (95% CI: 0.52 to 0.04 lower). | 12060 (5) | Standard Mean Difference ‐0.28 (‐0.52 to ‐0.04) | |||
| Physical Health | ||||||
| Morbidity/health improvement | The mean physical health score in the intervention groups was
0.01 standard deviations lower (95% CI: 0.1 lower to 0.07 higher). |
11388 (5) | Standard Mean Difference ‐0.01 (‐0.1 to 0.07) | |||
| Quality of Life | ||||||
| Morbidity/health improvement | The mean quality of life in the intervention groups was 0.08 standard deviations lower (95% CI 0.44 lower to 0.27 higher). | 797 (3) | Standard Mean Difference ‐0.08 (‐0.44 to 0.27) | |||
| Global Assessment of Function symptoms score | ||||||
| Morbidity/health improvement | The mean global assessment of function symptoms score in the intervention groups was 2.63 lower, a small effect favouring intervention (95% CI: 5.16 to 0.1 lower). | 600 (2) | ||||
Background
The level of health within a given population is affected not only by its health services but also by factors as diverse as environmental, social, cultural and economic influences (Benzeval 1995). These factors are addressed by many publicly funded organisations, including local government and local health authorities. The recognition of the role that social determinants play in the health of the population makes it clear that health cannot be the responsibility of just one agency and, over the last three decades, collaboration has been an increasing focus of health promotion internationally (Marmot 2005).
The need for collaborative working was highlighted in the 1986 Ottawa Charter for Health Promotion, produced during the First International Conference on Health Promotion. The Charter stated that “the prerequisites and prospects for health cannot be ensured by the health sector alone. More importantly, health promotion demands coordinated action by all concerned: by governments, by health and other social and economic sectors, by nongovernmental and voluntary organizations, by local authorities, by industry and by the media. People in all walks of life are involved as individuals, families and communities. Professional and social groups and health personnel have a major responsibility to mediate between differing interests in society for the pursuit of health" (WHO 1986).
In 1997 the Jakarta Declaration identified partnerships for health and social development between different sectors as one of its five key priorities. It stressed the need to strengthen existing partnerships and urged the development of new partnerships (Jakarta 1997). These priorities were further highlighted in 2005 when the Bangkok Charter stated that “partnerships, alliances, networks and collaborations provide exciting and rewarding ways of bringing people and organizations together around common goals and joint actions to improve the health of populations" (WHO 2005).
In his report "Fair Society, Healthy Lives" Marmot advised that tackling health inequalities also requires action across the social determinants of health, including education, occupation, employment, income, home and community. He emphasised the key role of local government along with national government departments, the voluntary and private sectors (Marmot 2010).
The World Health Organization (WHO) has documented the success that can be achieved when people, agencies, governments and industry work together to tackle international public health challenges such as smallpox, dehydration, poor mental health, tobacco, AIDS, tuberculosis and outbreaks (WHO 2011). The reports are encouraging but all involved national and international effort. It is not clear if collaborations between local health and local government agencies are equally successful.
In many countries national, regional and local inter‐ and intra‐agency collaborations have been introduced in order to improve health outcomes; often in disadvantaged groups. Agencies involved include primary and secondary healthcare providers, social services, housing, transport, leisure and library services, education and training departments and a range of voluntary bodies. Currently, there are a number of examples where collaborative programmes have been funded at national or state level but delivered locally through interagency partnerships. The WISEWOMAN Project was developed in the USA to prevent or control cardiovascular and other chronic diseases in low income and under‐ or uninsured women. The project comprises 15 state‐based partnerships across a range of agencies working within existing breast and cervical cancer screening programmes to provide screening and lifestyle interventions (CDC 2007). The Victoria Primary Care Partnerships in Australia have drawn together over 800 agencies in 13 partnerships to improve the efficiency and efficacy of health resources and to improve health and wellbeing (Primary 2004; Primary 2005; Primary 2009).
In the United Kingdom, interdepartmental working has been signalled as the way forward since the reorganisation of health and social services that took place during the 1970s (Great Britain 1970; Great Britain 1972; Great Britain 1973). Despite a split in responsibilities, close collaborative working between local health and local government agencies was identified as essential to improve the standards of services being delivered (Laws Statutes 1973a; Laws Statutes 1973b; Laws Statutes 1974). Collaboration was expected to be wide‐ranging, involving the sharing of resources, information, responsibilities and power. Since that time, successive UK governments have created a number of committee and team structures to facilitate partnerships. These have included bodies with statutory functions, such as Joint Commissioning Committees, and others established in accordance with governmental guidance, such as drug and alcohol action teams (Great Britain 1977; Great Britain 1999; HM Government 1995; HM Government 1998). The focus on collaboration has continued with successive governments. For example, the SureStart programme brought together early education, childcare, health and family support with the aim of delivering the best start in life for every child via a mix of universal and targeted programmes for young children and their parents (Sure Start 2004). These bodies address local problems and may have a very different set of priorities from those of their individual partner agencies. The question of whether better health outcomes are achieved as a result of such collaborative arrangements is not clearly answered.
Rationale of the review
In 2000, an unpublished systematic review by the current authors examined the research evidence related to the health effect of collaboration between local health and local government agencies (Wales Office 2001). The review found no evidence that interagency collaborative working necessarily led to improved health. In light of the continued emphasis on local collaborative working, the authors felt it was appropriate to update the review. As in the original review, the focus is on locally‐based initiatives. These could include initiatives arising from a national or state agenda as long as there was local flexibility in how they were developed and implemented. Collaboration at state and national levels often involves coordination of large scale planning and represents a different model of strategic alliances and relationship‐building from partnerships configured at the community level (Padgett 2004). Evidence is needed on the effectiveness of locally‐developed partnerships which target changes in individual health outcomes and behaviours.
Objectives
Primary research objective
To critically assess and summarise the effects of interagency collaboration between local health and local government agencies on health outcomes.
Secondary research objectives
1. To document and describe methods and models of collaboration between local health service agencies and local government authorities.
2. To assess the best methods of collaboration for producing measurable health improvement, if any such methods exist.
3. To develop guidance for future research and research methods if insufficient evidence is identified to address the primary research objective.
Methods
Criteria for considering studies for this review
Types of studies
Included studies were randomized or quasi‐randomized controlled trials (RCTs) including cluster RCTs; controlled clinical trials (CCTs); controlled before‐and‐after studies (CBAs) with a minimum of two study and two control sites; interrupted time series (ITS) with a minimum of three points both before and after the intervention. Studies which were solely economic evaluations were excluded. For included studies, authors were asked for information on partnership or process evaluations related to their collaborative arrangements, and for clarification of study design or missing data as appropriate. Studies or phases of studies where follow‐up rates were less than 60% were excluded. Where studies reported sequential results, they were included up to the point where follow‐up fell below 60%.
Types of participants
All population types and all age groups were included.
Types of interventions
Any interventions of interagency collaboration and partnership between statutory health and local government agencies where the level of partnership between collaborators could be clearly determined (for example, who are the partner agencies and what are their roles within the partnership) and where the interventions were aimed at improving health. For each intervention, comparator care was the mainstream care provided in the area and at the time the intervention was being tested (standard care).
Interventions could be delivered by a wide range of partner agencies but needed to include personnel funded or hosted by a local health agency (for example, doctors, nurses, therapists, midwives, health visitors, dieticians, school nurses, clinical psychologists, health promotion practitioners including public health units) and personnel funded or hosted by a local government agency (for example, social workers, teachers, educational psychologists, housing support workers, library and leisure staff, transport staff, environmental health officers). Multi‐partner collaborations could include education authorities and health agencies, departments for transportation or housing and health agencies, or a mix of these. Interventions where another organisation, for example a voluntary organisation, had been contracted to act on behalf of one of those agencies were also considered for inclusion.
Collaboration was defined as 'two or more parties that pursue an agreed set of goals and work cooperatively toward a set of shared health outcomes', adapted from that used by Gillies (1998) in describing alliances and partnerships for health promotion. Partnerships for health promotion focus on health outcomes rather than specific health promotion goals (Gillies 1998). Local collaboration was judged to have taken place if there was evidence that the partners had agreed local joint working arrangements and shared objectives.
Studies with the following types of interventions were excluded.
Studies which evaluated the effect of collaborative training initiatives between, for example, medical and social work undergraduates.
Studies that included a collaboration designed to enhance one agency's effectiveness in accessing other agencies, as these studies would not be reporting on the outcomes of the collaboration itself but the degree of involvement of the parent agency.
Studies where local government collaborated with the police, probation and prison services or the church but not with a health agency.
Studies where health agencies collaborated with the police, probation and prison services or the church but not with a local government agency.
Types of outcome measures
The primary outcomes of interest were limited to those which were either direct measures of improved health, health status, survival; or lifestyle factors where evidence indicates these have an effect on those direct measures. Studies were included where there were data for any measure of the following endpoints, and where a validated tool was used (see Appendix 1).
Mortality e.g., all‐cause death within period of study; probability of survival.
Morbidity e.g., quality of life measures, incidence rates, measures of symptoms and functionality, birth weight.
Behavioural change was included as a lifestyle change measure when it was known to directly affect levels of health risk or provide health protection e.g., measures of physical activity, smoking status and history, alcohol consumption, dietary change.
Where studies reported more than one relevant outcome, each was captured and reported in narrative form. Where outcomes were provided at multiple follow‐up points, each outcome was reported for the longest available follow‐up period where attrition was 40% or less.
Search methods for identification of studies
Electronic searches
The following electronic databases were searched from January 1966 (or the database start date if later than January 1966) to December 2011 without language, publication or geographical restrictions. The search strategies were based on the strategy developed for Ovid MEDLINE. All search strategies for the electronic databases are provided in Appendix 2.
AMED (Allied and Complementary Medicine) 1966 to 2011.
ASSIA (Applied Social Sciences Index and Abstracts) 1966 to 2011.
CINAHL (Cumulative Index to Nursing & Allied Health Literature) 1966 to 2011.
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library) 2012, Issue 1.
Cochrane Public Health Group Specialized Register 25 January 2012.
DoPHER (Database of promoting health effectiveness reviews) 2004 to 2011.
EMBASE (Excerpta Medica) 1980 to 2011.
ERIC (Education Resources Information Center) 1966 to 2011.
HMIC (Health Management Information Consortium) 1979 to 2011.
International Bibliography of the Social Sciences (IBSS) 1979 to 2011.
MEDLINE 1966 to 2011.
MEDLINE In‐Process & Other Non‐Indexed Citations 1966 to 2011.
PsycINFO 1966 to 2011.
Rehabdata 1966 to 2011.
OpenGrey (formerly OpenSIGLE) 1980 to 2011.
Social Care Online 1970 to 2011.
Social Services Abstracts 1979 to 2011.
Sociological Abstracts 1996 to 2011.
TRoPHI (The Trials Register of Promoting Health Interventions) 2004 to 2011.
Web of Science ‐ Science Citation Index 1979 to 2011.
Web of Science ‐ Social Sciences Citation Index 1979 to 2011.
Searching other resources
Reference lists of included studies and systematic reviews identified in the search were checked for additional citations, and citation tracking of identified RCTs was conducted using Scopus. In addition, experts were contacted directly and via mail lists, and the following websites were searched for publications and unpublished research.
The Association of Public Health Observatories (APHO): http://www.apho.org.uk/.
International Public Health Forum (IPHF): http://www.iphfonline.org/.
Local Government Association: http://www.lga.gov.uk/lga/core/page.do?pageId=1.
NHS Evidence ‐ National Library for Public Health: http://www.library.nhs.uk/publichealth/.
The World Federation of Public Health Associations: http://www.wfpha.org/.
World Health Organization: http://www.who.int/en/.
The UK Public Health Association: http://www.ukpha.org.uk/.
Conference proceedings via the British Library's ZETOC service: http://zetoc.mimas.ac.uk/.
Dissertation and Theses and Index to Theses database: http://proquest.umi.com/login.
Mail lists
Equity, Health & Human Development
EAHIL
Evidence Based Health
LIS Medical
PUBLIC‐HEALTH
PUBLIC‐HEALTH‐INTELLIGENCE
Social Policy
LIS Research Support
Study identification and selection
The titles and abstracts of all search results were reviewed independently by two authors to select potentially relevant studies using pre‐defined inclusion criteria. Studies that appeared to meet the inclusion criteria were independently reviewed in full text by two authors. Where there was a difference of opinion, a third review author also reviewed the paper and a consensus was reached.
Data collection and analysis
Assessment of risk of bias
Each eligible study was independently assessed for risk of bias by two review authors using a modified Cochrane Effective Practice and Organisation of Care Review Group (EPOC) risk of bias assessment (EPOC 2007a) and Chapter 8 (assessing risk of bias) in the Cochrane Handbook (Higgins 2008). Questions for RCTs, CCTs, CBAs and ITS study designs were incorporated into a modified version of the EPOC data abstraction form (EPOC 2007b) (see Figure 1, 'Risk of bias summary' for the categories). Where authors disagreed, a third author assessed the study and discrepancies were resolved by consensus.
1.
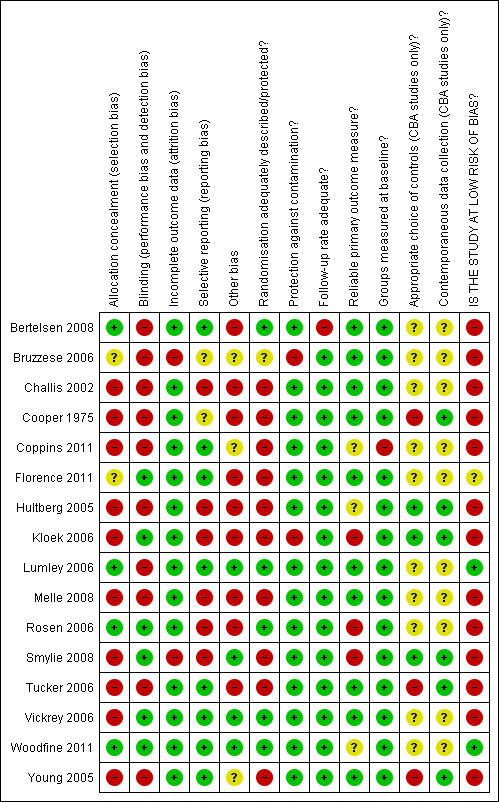
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
All included studies met the minimum standard of the EPOC checklist and were assessed and reported in a ‘Risk of bias' table (Higgins 2008). Where studies reported sequential results, those where follow‐up fell below 60% were excluded.
Studies were defined as having a low risk of bias if they demonstrated the following: an adequate randomisation methodology; a process of allocation concealment; blinding (of participants, investigators and for outcome assessment); non‐selective outcome reporting and a follow‐up response rate greater than 80% (or incomplete outcome data less than 20%) (Burger 2005; Higgins 2008).
Studies that did not fulfil the criteria for demonstrating a low risk of bias were reported as having an unclear or high risk of bias after considering all the items in the checklist.
Data extraction
A modified version of the EPOC data abstraction form was developed. It included questions to capture health equity data based on those used in the draft Cochrane Health Equity Field checklist for review authors (Morris 2007). The revised form was piloted by the authors before use. Data were extracted for all studies that met the quality and inclusion criteria. Two review authors independently completed a form for each study. Data were also extracted for included studies that reported a formal evaluation of the intervention, including the use of any specific partnership assessment tool (PAT) (Dickinson 2006; Hardy 2003; Victorian Health Promotion Foundation 2005).
Where studies reported more than one endpoint per outcome, the primary endpoint identified by study authors was extracted. Where no primary endpoint was identified by the study authors, the measures with the longest follow‐up and with attrition rates under 40% were reported.
Data analysis
Reporting results
Continuous outcomes were reported, where possible, on the original scale. Dichotomous outcomes were presented with odds ratios. All outcome effects were shown with their associated 95% confidence intervals.
Meta‐analysis
Meta‐analyses were conducted where trials reported similar outcomes. Random‐effects models were used for all analyses due to the expected differences in intervention, settings and outcomes. Relative risks were used to summarise dichotomous outcomes and standardised mean differences for continuous outcomes, except where the exact same outcome measure was used in different studies when mean differences were used.
Subgroup analysis
The number of studies with similar outcomes was not deemed sufficient to investigate subgroup analysis by population group or type of intervention.
Asssessment of heterogeneity
Heterogeneity was formally evaluated using the I2 statistic, as well as graphically using the forest plots.
Assessment of publication bias
Funnel plots to assess for publication bias were not presented due to the small number of studies in each meta‐analysis (maximum of five).
Incomplete outcome data (non‐response follow‐up rate)
As stated in the protocol, studies with attrition greater than 40% were excluded.
Summary of findings table
The Table 1 was completed to present brief information about the three categories of health outcomes. It was decided that the inclusion of evidence quality for each group of outcomes (based on the GRADE approach) was not feasible given the heterogeneity and range of study designs.
Results
Description of studies
Results of the search
Electronic searches yielded 19,064 references in the original search and an additional 11,001 references in the search for the updated review; 416 full‐text articles were assessed for eligibility from the original search and 92 from the updated search. Sixteen studies met the inclusion criteria for the narrative synthesis, of which 11 contributed data to meta‐analyses.
Excluded studies
Four hundred and ninety‐one studies were excluded. Most were excluded because of the nature of the collaboration, for example, partners coming from either health or local government agencies but not both, or prescriptive collaborations set up under national or international programmes. Other studies did not report relevant health outcomes or had inappropriate study designs. The Characteristics of excluded studies table lists the 491 studies with reasons for exclusion.
Ongoing studies
One ongoing study was identified (see Characteristics of ongoing studies).
| Lead author | Study design | Population | Intervention | Health outcomes |
| Bertelsen 2008 | RCT | 547 patients with first diagnosis within schizophrenia spectrum in Copenhagen and Aarhus, Denmark | The lead agency was mental health. Collaboration was between psychiatrists, psychologists, nurses, vocational therapists, social workers, family therapists working in multidisciplinary teams following agreed protocols. They delivered an intensive early intervention programme of Assertive Community Treatment, family treatment and social skills training. |
Primary health outcomes: Symptoms on the Scale for Assessment of Psychotic Symptoms (SAPS), Scale for Assessment of Negative Symptoms (SANS) and the Global Assessment of Functioning (GAF) scores for symptoms and for function |
| Bruzzese 2006 | Cluster RCT | 591 children in kindergarten to Grade 5, New York City, USA | The lead agency was the Local Education Authority. Collaboration was between school nurses, community and primary care physicians, school educators, public health assistants and university staff. They established Preventive Care Networks for each intervention school and delivered training for health and educational professionals. |
Primary health outcomes: Asthma symptoms in past 2 weeks and past 6 months, number of nights woken in past 2 weeks and past 6 months Number of days restricted activity in past 2 weeks and past 6 months Paediatric Asthma Caregiver's Quality of Life Questionnaire (PACQLQ) |
| Challis 2002 | CCT | 95 elderly adults with dementia in Lewisham, UK | The lead agency was community mental health. Collaboration was between social services case managers and mental health teams. They delivered an intensive case management scheme with structured care plans. Case managers had protected case loads and control of a devolved budget. They had access to health and social care resources. |
No primary outcomes were stated Health outcomes included: Depression measured by the Comprehensive Assessment and Referral Evaluation (CARE) schedule, disability measured through Clifton Assessment Procedures for the Elderly (CAPE) behaviour rating scale Physical disability, social disturbance, communication disorder and apathy measured through CAPE Patients' overall level of risk Carers' health assessed for strain and malaise |
| Cooper 1975 | CCT | 189 patients with chronic neurotic illness in primary care practice in a metropolitan area, UK | The lead agency was primary care. Collaboration was between general practitioners and health visitors in a primary care practice, a social worker and research psychiatrists. They established multidisciplinary coordination and evaluation of patients' care through fortnightly meetings. |
Primary health outcomes: Change in psychiatric rating (scale now known as GHQ 30) |
|
Coppins 2011 NEW |
RCT | 65 participants aged 6 to 14 years with a BMI above the 91st centile, living in Jersey, UK |
The lead agency was the local community health service. Collaboration was between a dietician, physical activity health promotion officer, educational and clinical psychologists, physical activity instructors. They ran workshops and physical activity sessions in school settings. Siblings aged 6 to 14 years and parents/guardians were encouraged to participate. |
Change in BMI standard deviation score. Change in weight, waist circumference, sum of skinfolds % body fat |
|
Florence 2011 NEW |
ITS | Resident populations and visitors to Cardiff and selected control cities in the UK | The lead agency was health. Collaboration was between city government (education, transport, licensing regulators) police, an emergency department consultant and an oral and maxillofacial surgeon, ambulance service and local licensees. They worked together in the Cardiff Violence Prevention Programme to share data between agencies and use the information for violence prevention through targeted policing and other strategies. |
Hospital admissions after violence, police recorded woundings, police recorded common assaults |
| Hultberg 2005 | CBA | 138 patients with musculoskeletal disorder in Goteburg, Sweden | The lead agency was primary care. Collaboration was between health centre physicians, nurses, occupational therapists, physiotherapists, social workers and social insurance officers working in co‐financed multidisciplinary teams based in the health centres. They had access to a joint budget provided by one common administrative body. They attended weekly team meetings to discuss and intensify the rehabilitation of individual patients. |
Primary health outcomes: Pain level measured by the Visual Analogue Scale (VAS) Health‐related quality of life measured through EuroQol 5 dimensions instrument (EQ‐5D) |
| Kloek 2006 | CBA | 2781 residents in Eindhoven, Netherlands | The lead agency was municipal health. Collaboration consisted of multi‐agency coalitions between municipal health services and representatives from social work, social welfare, city development department, neighbourhood residents organisation, general practice and researchers. They assessed neighbourhood health needs, developed action plans to improve health‐related behaviour and delivered a range of activities in schools, small community groups and public events. |
Primary outcome was to improve health‐related behaviours, measured by impact on fruit and vegetable consumption, physical activity, smoking and alcohol consumption |
| Lumley 2006 | Cluster RCT |
11,305 women giving birth in Victoria, Australia | The lead agency was local authority. Collaboration in each intervention area consisted of key stakeholders from local government, GPs, Maternal and Child Health nurses, community and consumer organisations and a community development officer forming local steering committees to deliver a Program of Resources, Information and Support for Mothers (PRISM). Interventions included components for primary care and for local community services. Clinical audits were conducted. |
Primary health outcome: EPDS, a 10‐item scale for use in the postnatal period to identify probable depression SF36 physical and mental component scores |
| Melle 2008 | CCT | 281 patients with first episode psychosis in four catchment areas in Norway and Denmark | The lead agency was mental health. Collaboration was between mental health clinicians, nurses, psychologists, GPs, school staff and social workers. Specialist integrated teams delivered an Early Detection Programme for rapid assessment of possible first episode psychosis patients and community information campaigns in schools and the local media to raise awareness of mental health issues. |
Primary outcome was the duration of untreated first episode psychosis Secondary health outcomes included symptom levels assessed through the Positive and Negative Syndrome Scale (PANSS) scores and level of functioning through the Global Assessment of Functioning scores |
|
Rosen 2006 NEW |
Cluster RCT randomized at the level of preschool |
40 public religious and secular preschools with 1029 children aged 3 and 4 years old. Additional support for children from 469 families who were in the intervention preschools. Set in Jerusalem region, Israel |
The lead agency was public health. Collaboration was between public health officers, Ministry of Education officials, teachers, preschools, school nurses, doctors and educational experts. They delivered an intervention consisting of educational lectures and resources, play materials, video and puppetry, along with ensuring environmental facilities were adequate to support good hand hygiene. The home component consisted of educational resources sent to families, chosen by computer‐generated random numbers, of children attending the intervention preschools. Control preschools had no intervention until the study was over. Home component control families received an educational pack on toothbrushing. |
Illness‐related absenteeism, handwashing behaviour before lunch and after using the bathroom |
|
Smylie 2008 NEW |
CBA | 240 Grade Nine students in six public schools in Windsor‐Essex County, Ontario, Canada | The lead agency was public health. Collaboration was between public health nurses, health promoters, social workers, teachers, a teen mother, a teen father and an HIV positive individual. They delivered a five session class‐based learning programme, a newsletter and workshops to help parents communicate effectively on sexual health issues with their children. |
Forty‐six items on knowledge, birth control attitudes, contraceptive agency (the degree to which students felt comfortable accessing and using birth control), communication, awareness of sexual response, sex role attitudes and sexual interaction values |
| Tucker 2006 | CBA | 8703 secondary school children, median age 14 years 6 months, in Lothian and Grampian regions, UK | The lead agency was the local health board. Collaboration was between health, education and the voluntary sector working in 10 schools. As part of the Healthy Respect programme, they established a partnership to implement the SHARE (Sexual Health and Relationships Education) project of multidisciplinary staff training, multidisciplinary delivery in classroom lessons and drop‐in sexual health services. |
Primary health outcomes: Self‐reported sexual intercourse at <16 years, and knowledge, attitudes and intentions about sexually transmitted diseases and condom use |
| Vickrey 2006 | Cluster RCT |
408 dementia patient and carer dyads, Southern California, USA | The lead agency was primary care. Collaboration was between physicians, leaders from community agencies, a community caregiver, the researchers and care managers. They formed a steering committee to identify existing guidelines as care goals. They introduced a disease management programme promoting care guidelines, care coordination and referral protocols. Community agency care managers and healthcare care managers received the same formal education and training programme. Health and community agency staff collaborated to provide support to patients with dementia and their carers. |
Primary outcome, extent of adherence to guidelines, was not relevant to this review Secondary health outcomes: Health‐related quality of life (HRQoL) for patients and carers |
|
Woodfine 2011 NEW |
RCT | 192 asthmatic children aged 5‐14 years, who had been in receipt of ≥3 prescriptions of corticosteroid inhalers in previous 12 months. Set in Wrexham, UK |
The lead agency was public health. The collaborators were local public health, primary care, Wrexham County Borough Council and academia. Vent‐Axia HR200XL ventilation systems were installed in the roof space and improvement/replacement of central heating system was undertaken if required. |
Primary: Parental assessment of the child's asthma‐specific quality of life (PedQL asthma module) 4 and 12 months after randomisation Secondary: General health‐related quality of life (PedQL core module), school attendance and the use of health care including medication Cost effectiveness of intervention |
| Young 2005 | CCT | 1648 vulnerable elderly patients in the Leeds area, UK | The lead agency was the health authority. Collaboration was between Leeds Health Authority and Leeds City Council. They developed a commissioning framework to provide support and rehabilitation to older patients following a health crisis at home or in hospital. A multi‐agency joint care management team commissioned care from a multidisciplinary Intermediate Care Team comprising nurses, therapists and social services staff. |
Primary health outcome: Independence measured by Nottingham Extended Activities of Daily Living Index |
Table 1. Outlines of included studies
Included studies
Characteristics of studies
Sixteen studies were included in the narrative synthesis, of which seven were RCTs or cluster RCTs (Bertelsen 2008; Bruzzese 2006; Coppins 2011; Lumley 2006; Rosen 2006; Vickrey 2006; Woodfine 2011), four studies were CCTs (Challis 2002; Cooper 1975; Melle 2008; Young 2005), four studies were CBAs (Hultberg 2005; Kloek 2006; Smylie 2008; Tucker 2006) and one was an ITS (Florence 2011). Eleven were included in the meta‐analyses (Figure 2). A brief outline of each included study can be found in Table 1. More details are presented in the 'Characteristics of included studies' table for each study (see Characteristics of included studies).
2.
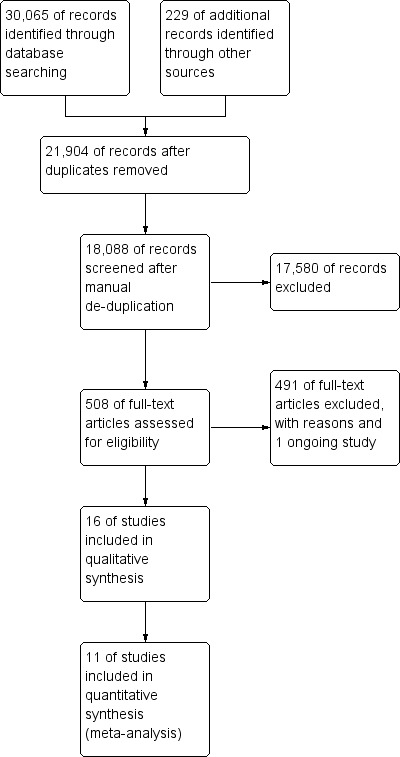
Study flow diagram.
Of the 16 studies meeting the inclusion criteria (Figure 1), 15 reported information on 28,212 participants although not all participants contributed outcome data as many participants were lost to follow‐up. One study monitored rates of violence in a population of 324,800 (Florence 2011). The largest number of participants (11,305) was from a study (Lumley 2006) that aimed to reduce depression and improve the physical health of mothers six months after giving birth. The next largest study (Tucker 2006) surveyed 8703 school children in two different cohorts.
Seven studies were conducted in the UK (Challis 2002; Cooper 1975; Coppins 2011; Florence 2011; Tucker 2006; Woodfine 2011; Young 2005), one in Denmark (Bertelsen 2008), one in Sweden (Hultberg 2005), one in both Norway and Denmark (Melle 2008), one in the Netherlands (Kloek 2006), two in US states (Bruzzese 2006; Vickrey 2006), one in Canada (Smylie 2008), one in Israel (Rosen 2006) and one in Australia (Lumley 2006). While reports on interventions in low or middle income countries were identified by the search strategy, many of them reflected work by international aid agencies delivering internationally agreed programmes with local partners rather than by local partnerships working to locally agreed goals.
Eight studies were delivered through community and primary care services (Bertelsen 2008; Challis 2002; Cooper 1975; Hultberg 2005; Lumley 2006; Vickrey 2006; Woodfine 2011; Young 2005), five were delivered in schools (Bruzzese 2006; Coppins 2011; Rosen 2006; Smylie 2008; Tucker 2006) and three were set in the wider community (Florence 2011; Kloek 2006; Melle 2008). No studies were based in hospitals but two (Bertelsen 2008; Young 2005) recruited participants from hospital‐based services.
Bertelsen 2008, Melle 2008, Rosen 2006, Tucker 2006, Woodfine 2011 and Young 2005 succeeded in recruiting the sample sizes required by their power calculations. Lumley 2006 identified that they were not recruiting enough participants and extended the recruitment period until the required number had been recruited to the intervention group though not to the control group. Vickrey 2006 aimed to recruit 438 dyads but failed to achieve this. Hultberg 2005 did not conduct a power calculation but aimed to recruit 450 patients, which they failed to achieve despite extending the recruitment period by eight months. The remaining studies did not provide power calculations and did not state their desired sample size (Bruzzese 2006; Challis 2002; Cooper 1975; Coppins 2011; Florence 2011; Kloek 2006; Smylie 2008).
Primary outcomes
Few studies reported one primary outcome, although several had one overarching goal for which there was a range of measures. Coppins 2011 aimed to produce a change in the body mass index standard deviation score (BMI SDS) (or BMI z‐score), a measure demonstrating the deviation of children's BMI from the average of a child of the same age and sex. Kloek 2006 aimed to improve health‐related behaviours measured through self‐reported diet, exercise, smoking and alcohol behaviours. Melle 2008 aimed to reduce the duration of untreated first episode psychosis in order to improve mental health outcomes in the longer term. The primary outcome for Vickrey 2006 was adherence to care guidelines on the understanding that this should improve quality of life for dementia patients and their carers. Young 2005 aimed to protect the independence of vulnerable elderly patients in order to minimise hospitalisations and institutionalisation. The primary outcome for Rosen 2006 was a reduction in illness absenteeism but reliable data were hard to collect. Smylie 2008 wanted to support actual change in sexual behaviour in under 16s but it was thought inappropriate to ask school students about this so proxies relating to knowledge, attitudes, communication and self‐awareness were used. All studies measured multiple outcomes and Bruzzese 2006, Challis 2002 and Vickrey 2006 included measures of carer health. The primary outcome for Bertelsen 2008 was stated to be at five years but at that point follow‐up rates for symptom and function assessments were below 60% in both arms. Follow‐up rates at two years were above 60%, unequal in the two arms, and assessment was not blinded.
Characteristics of participants
Seven studies delivered interventions to individual participants (Bertelsen 2008; Challis 2002; Cooper 1975; Coppins 2011; Hultberg 2005; Woodfine 2011; Young 2005). Six studies delivered interventions to populations defined by: area of residence (Kloek 2006; Melle 2008); school attended (Rosen 2006; Smylie 2008; Tucker 2006); or registered primary care clinic (Vickrey 2006). Bruzzese 2006, Florence 2011 and Lumley 2006 used a variety of interventions, some aimed at the general population and others at individuals. Two studies targeted deprived communities (Bruzzese 2006; Kloek 2006) and all but five studies (Coppins 2011; Melle 2008; Smylie 2008; Woodfine 2011; Young 2005) reported measures of deprivation. The targets of the educational programmes and public information campaigns in Melle 2008 were school children and households in the intervention areas. However, the target group to benefit were people with first episode psychosis who, if the programme was successful, would have assessment, diagnosis and treatment earlier in the course of their illness due to increased awareness and support in their community. In Kloek 2006 the programmes were delivered to children as well as adults but the outcomes were only measured in adults. Bruzzese 2006, Challis 2002 and Vickrey 2006 included measures to support carers.
Four of the five studies identified in the 2012 update were targeted at children (Coppins 2011; Rosen 2006; Smylie 2008; Woodfine 2011). The fifth study (Florence 2011) was aimed at the population of a city, particularly but not solely people making use of a city centre's night‐time facilities.
Characteristics of interventions
Collaboration was delivered through a range of multidisciplinary teams working to agreed programmes. Partners included primary and secondary healthcare workers, public health officers, health promotion officers, local authority staff including social workers and care staff, teaching professionals, environmental health officers, sports and leisure officers, police and voluntary agencies.
Seven studies reported on interventions to improve the care or treatment of patients (Bertelsen 2008; Bruzzese 2006; Challis 2002; Cooper 1975; Hultberg 2005; Vickrey 2006; Young 2005) through multidisciplinary team work. Nine studies reported health education, health promotion or disease prevention initiatives (Coppins 2011; Florence 2011; Kloek 2006; Lumley 2006; Melle 2008; Rosen 2006; Smylie 2008; Tucker 2006; Woodfine 2011). Examples of health education and promotion included Melle 2008, which aimed to raise community awareness of psychosis to encourage early referrals and so decrease the duration of untreated psychosis; and Kloek 2006, which ran nutrition projects in primary schools, quit smoking courses and large annual community events related to health along with other activities such as walking events.
Six studies related to mental health initiatives (Bertelsen 2008; Challis 2002; Cooper 1975; Lumley 2006; Melle 2008; Vickrey 2006), including one focused on preventing depression and improving the physical health of mothers in the first six months after giving birth (Lumley 2006). Of the remaining five studies, two related to chronic disease management (Bruzzese 2006; Hultberg 2005), two were aimed at encouraging healthy lifestyles (Kloek 2006; Tucker 2006) and one was aimed at improving support for the frail elderly (Young 2005).
Defined at‐risk populations were targeted in five studies, two in children (Bruzzese 2006; Tucker 2006) and three in the elderly (Challis 2002 ; Vickrey 2006; Young 2005).
One study followed longitudinal incident rates of violent assault in a defined population (Florence 2011).
Evaluation of partnerships and processes
Some authors included comments on the extent to which participants had taken part in or received interventions. For instance Smylie 2008 captured how many classroom sessions students had attended. Of the 10 authors who responded to requests for information on partnership evaluations, six studies had been formally evaluated (Challis 2002; Kloek 2006; Lumley 2006; Rosen 2006; Tucker 2006; Vickrey 2006) although data were not available for the Lumley 2006 intervention. Additionally, for Woodfine 2011 a cost effectiveness analysis was performed. However, many authors had not conducted partnership evaluations.
Risk of bias in included studies
Of the seven RCTs, only two were considered to be at low risk of bias (Lumley 2006; Woodfine 2011) and one was at unclear risk of bias (Vickrey 2006). Of the non‐randomised studies, Melle 2008 and Florence 2011 were judged to be at unclear risk of bias and all the others were deemed to be at high risk of bias.
For detailed information on the risk of bias of individual studies see the risk of bias tables for each study and the risk of bias summary (Figure 1).
Adequate randomisation methodology
Most RCTs and cluster RCTs reported appropriate methods for randomisation. Bertelsen 2008, Rosen 2006, Vickrey 2006 and Woodfine 2011 used various independent methods to generate random allocation. Lumley 2006 generated a random set of eight matched pairs of areas from a stratified set of 21 eligible areas. Bruzzese 2006 and Coppins 2011 did not give a description of how participants were randomised.
Contamination of the control group
Controlling conditions in population or area level intervention studies can be hard. People are free to move between areas and there may be family or social ties between intervention and control arms which are unknown to the researchers. Three studies reported on probable contamination in the control groups of their studies. One study appeared to have been conducted to a high standard (Bruzzese 2006) but a similar intervention was introduced to the wider community, including the whole study population, part way through the study thereby contaminating the control group and reducing the potential to demonstrate a true effect from the intervention. Lumley 2006 reported that they had looked for evidence of contamination in the control areas and found that some members of the control group had received the leaflets designed for the intervention group. They concluded that as the overall intervention consisted of many additional components this was unlikely to have led to bias in the results. Kloek 2006 identified low levels of contamination in control neighbourhoods, which was to be expected as they were in the same city as the intervention neighbourhoods. For the remaining studies contamination of the control group appeared unlikely.
Allocation concealment
Based on the author report, only four studies were able to conceal allocation (Bertelsen 2008; Florence 2011; Lumley 2006; Rosen 2006).
Selective outcome reporting
Selective outcome reporting appeared to be more common in the non‐randomised studies. Some studies reported follow‐up results linked to previous work. For example, Melle 2008 reported two year follow‐up results on a study that had started recruiting participants eight to 10 years previously and which had been extensively reported by other authors. There were differences in the way the various reports described the same study, making it difficult to understand exactly what had been done and raising the possibility that some data were not being fully reported. Challis 2002 reported different sets of outcomes at different follow‐up periods. Smylie 2008 captured full follow‐up data on 22 students who had not attended any sexual health sessions and omitted to include these results in their analysis. It was not possible to establish whether Cooper 1975 had used selective outcome reporting because a protocol was not available.
Level of blinding
We assessed blinding of participants and researchers. The participants and researchers in population or public health Interventions often cannot be blinded because there are clear differences between receiving the intervention and not. Rosen 2006 used an interesting technique to blind families as they gave the intervention families information and equipment related to handwashing and for the control families they gave information on toothbrushing. Most studies were unable to achieve blinding of outcome assessment. Of the studies that reported blinding, Vickrey 2006 used a variety of ways to achieve as high a level of blinding as possible. Participants were blinded at baseline and they were not reminded of status at follow‐up. Data abstractors were blinded. Carers were blinded at the baseline survey. Bruzzese 2006, Lumley 2006 and Smylie 2008 did not use blinding in assessments but the outcomes were judged unlikely to have been influenced by this. In Cooper 1975 there was no evidence to suggest assessment had been blind, although assessment of individuals was not performed by the psychiatrist involved in their care.
Incomplete outcome data
Only studies where outcome data appeared to be adequately accounted for were included in this review. Outcome data available for less than 60% of participants at any time‐point were excluded.
Unit of analysis errors
Four studies employed cluster randomisation (Bruzzese 2006; Lumley 2006; Rosen 2006; Vickrey 2006). All used methods to account for the clustering and none of these studies were re‐analysed. Bruzzese 2006 used Generalised Estimating Equations (GEE) models to account for clustering. Lumley 2006 used a multilevel model reporting that the intracluster correlation coefficient (ICC) was 0.0012. Rosen 2006 used mixed linear models and reported an ICC of 0.06 for overall absenteeism and 0.07 for illness absenteeism. Vickrey 2006 used multilevel modelling to account for clustering, however this study contributed uncorrected dichotomous information to the mortality meta‐analysis. Using the design effect of 1.57 reported in their sample size calculation (based on an ICC of 0.03) the sample size of both control and intervention groups were scaled down from 238 and 170 to 152 and 108 for the intervention and control groups respectively. Numbers of events were selected that produced proportions of events closest to the observed proportions. The effect of this design effect scaling was very small.
Interrupted time series (ITS) studies
Only one interrupted time series study (Florence 2011) was identified and this has been reported separately.
Effects of interventions
See: Table 1
Randomized controlled trials (RCTs)
Lumley 2006 (a cluster RCT with low risk of bias) conducted a community randomized trial using the PRISM (Program of Resources, Information and Support for Mothers) approach to reduce depression and improve women's physical health after giving birth. Power calculations suggested that questionnaires needed to be sent to 9600 women in each arm and, as birth rates were lower than anticipated, data collection was extended to generate the required sample size. A total of 6248 women out of 10,144 women (61.6%) in the intervention arm and 5057 out of 8411 women (60.1%) in the control arm completed postal questionnaires six months after giving birth. The intervention and control groups appeared comparable at baseline. The mean Edinburgh Postnatal Depression Score (EPDS) was 6.91 (SE adjusted (adj) 0.11) in 6163 women in the intervention communities and 6.83 (SE adj 0.11) in 4969 women in the control communities (P = 0.61, mean difference 0.08, SE adj 0.09, 95% confidence interval (CI) ‐0.25 to 0.40). Mean SF‐36 physical component scores were 50.24 (SE adj 0.10) for 5917 women in the intervention communities and 50.26 (SE adj 0.16) for 4761 women in the control communities (P = 0.91, mean difference ‐0.02, SEadj 0.19, 95% CI ‐0.43 to 0.39). Mean SF‐36 mental component scores were 47.58 (SE adj 0.15) in 5917 women in the intervention communities and 47.91 (SE adj 0.19) in 4761 women in the control communities (P = 0.20, mean difference ‐0.32, SE adj 0.24, 95% CI ‐0.83 to 0.18). None of these findings were significant. There was no difference between intervention and control communities in the mothers' rating of partners' practical and emotional support, with mean scores derived from a set of six questions being 6.9 in both groups.
Evaluation of the intervention
An interorganisational analysis has being conducted. It has not yet been published and a copy could not be obtained.
Summary: there were no significant differences between the two groups in any of the measures at six‐months follow‐up.
Woodfine 2011 (an RCT with a low risk of bias) aimed to evaluate the effectiveness of tailored packages of home improvements, providing adequate heating and ventilation in order to reduce mould spores, for children with moderate or severe asthma. They aimed to recruit 200 children to yield 80% power to detect, at 5% significance level, a change in asthma‐specific quality of life of at least 0.4 of the standard deviation of the parent‐completed asthma‐specific module of PedsQL, a validated quality of life measure for children.
At month 12 (11 months post‐intervention): 169 (88%) responded (intervention group (I) = 88; control group (C) = 89). The mean difference in PedsQL asthma scale adjusted for baseline was 7.1 (95% CI 2.8 to 11.4); standardised effect size 0.42. There were no significant differences in physical scale (4.5, 95% CI ‐0.2 to 9.1; standardised effect size 0.22) or psychosocial functioning (2.2, 95% CI ‐1.9 to 6.4; standardised effect size 0.11). The overall psychosocial scale at 12 months was 74.6 in the intervention group (n = 69) and 68.3 in the control group (n = 70) (mean adjusted difference 2.7, 95% CI ‐1.8 to 7.2) favouring the intervention arm. There was no significant difference in parent‐reported school absence over 12 months: mean 9.2 days in intervention group versus 13.2 days in control group (Mann‐Whitney U test P = 0.091); and mean 3.9 days in intervention group versus 6.4 days in control group for asthma‐related absences (Mann‐Whitney U test P = 0.053).
There was no significant difference in healthcare costs over 12 months between groups. The authors reported a shift from ‘severe’ to ‘moderate’ asthma in 17% of the intervention group and 3% of the control group.
Cost effectiveness of the intervention: the mean cost of modifications was £1718 per child treated or £12,300 per child shifted from ‘severe’ to ‘moderate’ asthma. ‘Bootstrapping’ gave an incremental cost‐effectiveness ratio (ICER) of £234 per point improvement on the 100‐point PedsQL™ asthma‐specific scale (95% CI £140 to £590). The ICER fell to £165 (95% CI £84 to £424) for children with ‘severe’ asthma. The authors concluded that the intervention had been cost effective.
Evaluation of the intervention
The authors did not undertake a formal evaluation, although some information on the delivery of the programme was provided in a cost‐effectiveness analysis.
Summary: the impact of asthma on childrens' lives, as measured by the asthma subscale of the parent‐completed PedsQL, was significantly lessened in the intervention group 11 months after home modification. No significant improvement was seen in overall physical or psychosocial quality of life at 12 months. School absences were not statistically significantly different between groups.
Bertelsen 2008 (an RCT with high risk of bias) aimed to determine the long‐term effects of an intensive early‐intervention programme for first‐episode psychotic patients. They assessed 547 participants at baseline before randomization and the two groups appeared well matched and representative of the client group. At two years the independent assessment was unblinded and at five years the independent assessment was blinded. (Note: the mean differences are based on a repeated model to impute missing data.)
The follow‐up rate at two years was 75% in the intervention group (n = 205) and 60% in the control group (n = 164). The mean symptom score on the Scale for Assessment of Psychotic Symptoms (SAPS) was 1.06 (SD 1.26) in the intervention group and 1.27 (SD 1.40) in the control group, estimated mean difference ‐0.32 (95% CI ‐0.58 to ‐0.06, P = 0.02). The mean symptom score on the Scale for Assessment of Negative Symptoms (SANS) was 1.41 (SD 1.15) in the intervention group and 1.82 (SD 1.23) in the control group, estimated mean difference ‐0.45 (95% CI ‐0.67 to ‐0.22, P < 0.001). The mean Global Assessment of Functioning (GAF) symptom score was 51.18 (SD 15.01) in the intervention group and 48.67 (SD 15.92) in the control group, estimated mean difference 2.45 (95% CI ‐0.32 to 5.22, P = 0.08). The mean GAF function score was 55.16 (SD 15.15) in the intervention group and 51.13 (SD 15.92) in the control group, estimated mean difference 3.12 (95% CI 0.37 to 5.88, P = 0.03).
The primary endpoint of the study was at five years but as follow‐up was below 60%, with 56% in the intervention group and 57% in the control group, and below 60% in both arms when deaths were taken into account, it is not reported here.
Evaluation of the intervention
No process evaluation has been identified.
Summary: interim results at two‐year unblinded follow‐up showed that the SAPS and SANS symptom scores and the GAF score for function were statistically significantly improved in the intervention group although the size of these effects was very modest (‐0.32, ‐0.45 for SAPS and SANS respectively, both on a 6‐point scale; and 2.45 on the GAF, a 100‐point scale). There was no difference in the GAF score for symptoms between the two groups.
Vickrey 2006 (a cluster RCT with medium risk of bias) tested the effectiveness of a dementia guideline‐based disease management programme on quality of care and outcomes for patients with dementia. Primary outcomes related to the level of adherence to 23 guidelines and were not relevant to this review. Secondary outcomes were assessed through a caregiver survey. At baseline assessment the intervention and control groups did not differ in patient and caregiver characteristics. At 18‐months follow‐up the mean patient health‐related quality of life score had decreased from 0.17 (SD 0.30) to 0.10 (SD 0.30) in the intervention group and from 0.16 (SD 0.32) to 0.03 (SD 0.29) in the control group. The adjusted analysis for intervention versus control group between‐group difference was 0.06 (95% CI 0.005 to 0.11, P = 0.034). Caregiver health‐related quality of life, measured using EuroQol‐5D, changed from a mean of 0.83 (SD 0.17) at baseline to 0.81 (SD 0.16) at 18‐months follow‐up for carers of patients in the intervention group and from 0.80 (SD 0.22) at baseline to 0.77 (SD 0.23) at 18‐month follow‐up for carers of patients in the control group. The adjusted analysis for intervention versus control between‐group difference was 0.02 (95% CI ‐0.01 to 0.06, P = 0.127).
By the 12‐month follow‐up 34 out of 238 patients had died in the intervention group and 20 out of 170 patients had died in the control group.
Evaluation of the intervention
All care management communications and encounters with the participants were recorded on an electronic database. Subsequent analysis of the impact of the three agencies demonstrated that contact with healthcare organisation care managers was associated with improved quality. Further, statistically and clinically significant incremental gains in quality were seen with the addition of the other provider types (community agency care managers and healthcare organisation primary care providers). It was noted that the three groups of staff may have recorded their interventions differently. Factors associated with accepting case management were also analysed and were found to include cohabitation of the caregiver, lesser severity of dementia and higher patient co‐morbidity.
Summary: at 18‐month follow‐up the caregivers reported that quality of life had deteriorated for the intervention and control groups but the intervention group had a better health‐related quality of life score than the control group. There was no difference in the health‐related quality of life for the carers of the two groups.
Bruzzese 2006 (a cluster RCT with high risk of bias) established a preventive network of school nurses, teachers and primary care providers to improve elementary school childrens' control of asthma. Randomization was at the school level. Intervention and control groups were assessed at baseline and found to be comparable apart from the control group children waking more nights due to asthma in the previous two weeks. For every 50 children known by the school nurse to have asthma, the network identified another 25 children with an asthma diagnosis and another 20 children with symptoms suggestive of asthma. Follow‐up at two years by telephone interview of caregivers was 64% in the intervention group (n = 195) and 61% in the control group (n = 173). The mean number of days with symptoms in the past two weeks was 2.9 (SD 3.7) in the intervention group and 2.6 (SD 3.4) in the control group; mean number of days with symptoms in the last six months was 32.1 (SD 44.9) in the intervention group and 32.0 (SD 45.6) in the control group. The mean number of nights woken in the past two weeks was 1.6 (SD 2.6) in the intervention group and 2.2 (SD 3.4) in the control group; mean number of nights woken in the last six months was 26.3 (SD 40.6) in the intervention group and 26.8 (SD 42.3) in the control group. The mean number of days with restricted activity in the past two weeks was 1.5 (SD 2.45) in the intervention group and 1.5 (SD 2.8) in the control group; mean number of days with restricted activity in the past six months was 25.4 (SD 41.3) in the intervention group and 23.6 (SD 41.0) in the control group. Caregivers' quality of life assessed using the Paediatric Asthma Caregiver's Quality of Life Questionnaire was mean 5.5 (SD 1.5) in the intervention group and 5.5 (SD 1.6) in the control group. None of these outcomes were significantly different.
Evaluation of the intervention
No process evaluation has been carried out.
Summary: the network identified more children with diagnosed and undiagnosed asthma than were known to the school nurses. There were no differences in outcomes between the children in the two groups or between the two groups of carers at two‐year follow‐up.
Coppins 2011 (an RCT with a high risk of bias) aimed to treat overweight and obese children through a multi‐component family focused education package. Workshops were conducted on healthy eating, physical activity, psychological well‐being and behaviour change, including reducing sedentary activity; and offered regular physical activity sessions for obese and overweight children aged 6 to 14 years, their siblings aged 6 to 14 years, and their parents. Outcomes were measured at six‐month intervals for 24 months but the intervention was given to the intervention‐control group in the first 12 months and to the control‐intervention group in the second 12 months, so the point of comparison was taken to be at 12 months for the purpose of this review. There were some differences between the groups at baseline with the intervention group being on average 16.5 months older than the control group.
The primary outcome was change in BMI SDS. At 12 months the change in the intervention group BMI SDS was ‐0.17 (95% CI ‐0.26 to ‐0.08) and the adjusted difference was ‐0.13 (95% CI ‐0.26 to ‐0.008). The change for the control group BMI SDS was ‐0.08 (95% CI ‐0.24 to 0.07) and the adjusted difference was ‐0.14 (95% CI 0.28 to ‐0.001). The mean difference between the intervention and control groups was ‐0.09 (95% CI ‐0.26 to 0.09, F = 0.99, P = 0.32).
Evaluation of the intervention
The corresponding author reported that no information relating to process or partnership evaluations has been published.
Summary: the multi‐component intervention to help overweight and obese children adopt healthier lifestyles and normalise their BMI was not effective compared to the wait‐list control group.
Rosen 2006 (an RCT with a high risk of bias) evaluated the effects of a comprehensive hand hygiene programme, including improving environmental facilities where indicated, on preschool children aged 3 and 4 years in 40 preschools (20 intervention, 20 control). They also nested an RCT within the intervention group to test a home education component. Sample size was calculated to detect a 25% drop in illness absenteeism with a power of 80% and a two‐sided alpha level of 0.05, given a control group illness absenteeism rate of 6% per child day (36 preschools, rounded up to 40). A planned 60‐day study period was extended to 66 days during the trial. Sample size for the home intervention was similarly calculated to detect an illness absenteeism reduction from 4.5% to 3.0%. The required sample size was 204 families per arm. The main outcome measures were overall absenteeism and illness absenteeism from preschool. For the purposes of this review the outcome measure of illness absence was used. The researchers also measured handwashing behaviours.
The average per day percentage of illness absenteeism was 3.40 days (489 children) and 3.11 days (540 children) for the intervention and control preschools respectively: intraclass correlation coefficient 0.0747, between day correlation 0.0417, adjusted RR of 1.00 (95% CI 0.81 to 1.32, P = 0.97). For the home component, illness absenteeism was 2.92 (n = 237) in the intervention group and 3.04 (n = 232) in the control group, adjusted RR of 0.94 (95% CI 0.76 to 1.23, P = 0.57).
Evaluation of the intervention
The corresponding author reported a detailed survey of the teachers', parents' and childrens' reactions to the programme and there were comments made on the activity of the partners delivering the intervention. The feedback was extremely positive and other schools have taken up the programme several years after completion of the study. There were descriptions of the partnership in the published papers but there does not appear to have been a formal evaluation of the partnership itself.
Summary: neither the joint handwashing and environmental intervention in preschools nor the home education component had an effect on childrens' illness absenteeism.
Controlled clinical trials (CCTs)
Melle 2008 (a controlled clinical trial with medium risk of bias) investigated the effectiveness of community and health professional educational campaigns to reduce the duration of untreated psychosis through early referral and prompt assessment and treatment of those affected. Patients were recruited over a four‐year period and followed up for two years after recruitment. Power calculations suggested they needed to recruit 100 patients in each group. The researchers invited 186 patients in the intervention area and 194 patients in the control area to join the study: 141 and 140 patients agreed, respectively (74% of all eligible patients). At recruitment the mean duration of untreated psychosis in the intervention group (n = 118) was five weeks (range 0 to 1196) and in the control group (n = 113) it was 16 weeks (range 0 to 966) (P < 0.01, Mann‐Whitney U test). Symptomatic and functional status was measured at two years in 118 patients from the intervention areas and 113 patients from the control areas. The mean Positive and Negative Syndrome Scale for schizophrenia (PANSS) positive component was 9.13 (SD 4.97) in the intervention group and 9.06 (SD 4.02) in the control group. The mean PANSS negative component was 15.54 (SD 6.48) in the intervention group and 19.19 (SD 9.06) in the control group. The mean Global Assessment of Function (GAF) symptoms score was 53.64 (SD 17.68) in the intervention group and 50.81 (SD 14.54) in the control group. The mean GAF functioning score was 53.80 (SD 17.32) in the intervention group and 49.47 (SD 14.78) in the control group. Only the PANSS negative component score was statistically significant (P < 0.001, t test), in favour of the intervention group, after correcting for multiple testing.
Evaluation of the intervention
No process evaluation was identified.
Summary: the mean duration of untreated psychosis was significantly shorter in the intervention area but this is an intermediate outcome and it is not clear if it resulted in lasting health benefit. The intervention group had lower scores for the negative component of the PANSS scale than the control group at two‐year follow‐up and the difference was statistically significant. There were no significant differences between the two groups for the positive component of the PANSS scale or for the GAF function and symptom scores. The authors noted that clinical ratings of the PANSS scale had not been masked and there was therefore the possibility of assessment bias.
Challis 2002 (a controlled clinical trial with high risk of bias) evaluated the Lewisham Case Management Scheme. This intensive scheme integrated social service case managers into a Community Mental Health Team for the Elderly; caring for a target population of older people with dementia. They had control over a devolved budget and had access to all relevant health and social care resources. The 45 patients in the intervention group and 50 in the control group appeared to be comparable at baseline. Follow‐up rates were different for each measure and only health measures with greater than 60% follow‐up are reported here. At six months the mean CAPE Behaviour Rating Scale score for disability, a composite measure of physical disability, social disturbance, communication disorder and apathy, increased from 14.94 (SD 5.11) to 15.83 (SD 5.60), mean change of 0.89, for the intervention group (n = 35); and decreased from 16.07 (SD 4.67) to 15.33 (SD 5.30) (n = 43), mean change of ‐0.74, for the control group: F = 2.87 (95% CI for the group difference ‐0.29 to 3.55, P value not significant). The mean level of risk to the cases decreased from 1.94 (SD 1.17) to 1.30 (SD 1.21), mean change of ‐0.64 in the intervention group (n = 33); and increased from 1.42 (SD 1.26) to 1.47 (SD 1.24), mean change 0.05 in the control group (n = 43) (95% CI for the group difference ‐1.30 to ‐0.07, P < 0.05). From the 43 matched pairs, 12 deaths were recorded in the intervention group and 15 in the control group at 24‐month follow‐up but the total number of deaths from the 95 participants was not reported. The study reported that around 80% of participants had carers, implying there were 75 carers in total. At 12 months the mean overall strain on carers decreased from 4.00 (SD 1.62) to 3.00 (SD 1.57), mean change of ‐1.0 in the carers for the intervention group (n = 26); and from 4.09 (SD 1.28) to 2.91 (SD 1.80), mean change of ‐1.18 in the carers for the control group (n = 32): F = 0.17 (95% CI for group difference ‐0.74 to 1.11, P value not significant). Malaise decreased from a mean of 5.92 (SD 5.28) to 4.32 (SD 4.34), mean change ‐1.60 in the carers for the intervention group (n = 25); and from 6.68 (SD 3.99) to 6.32 (SD 3.60), mean change ‐0.35 in the carers for the control group (n = 34): F = 2.84 (95% CI for group difference ‐2.73 to 0.23, P value not significant).
Evaluation of the intervention
The author supplied some additional information which reported progress of the project rather than formally evaluating the collaborative partnership. It demonstrated that the model had been highly valued and staff particularly appreciated having control over relatively small budgets. Local commissioners of health and social care jointly agreed to maintain the service and it has since become mainstream, recognised as providing good practice in terms of its integration and co‐location of staff.
Summary: the researchers' unblinded assessment of patients' overall level of risk indicated a decrease in the intervention group and an increase in the control group at six months. There was no difference in the CAPE Behaviour Rating Score between the intervention and control group patients at six months and no differences in strain or malaise between carers of the intervention and control patients at 12 months.
Cooper 1975 (a controlled clinical trial with high risk of bias) assessed the therapeutic value of attaching a social worker to a metropolitan primary care practice for the management of chronic neurotic illness. Participants were assessed at baseline and were broadly similar in demographic profiles. There were some differences between the groups in diagnoses but the paper reports the differences as being of doubtful significance to the findings. The psychiatric mean score at one‐year follow‐up decreased from 26.9 to 16.6, mean change ‐10.3 (SD 10.2) in the intervention group (n = 92); and from 26.1 to 19.7, mean change ‐6.4 (SD 9.9) in the control group (n = 97): test of significance t = 2.68, P < 0.01. The team analysed the impact various professional groups may have had on the ratings and concluded that the therapeutic effect of the experimental service was not confined to any one member or professional group in the team but a result of the group interaction.
Evaluation of the intervention
No process evaluation has been identified.
Summary: the psychiatric score of both groups decreased at one‐year follow‐up suggesting decreased clinical severity in both groups, more so in the intervention group than in the control group.
Young 2005 (a controlled clinical trial with high risk of bias) compared a group of older people before and after the introduction of intermediate care services for older people. The primary outcome was independence at six months measured by the Nottingham Extended Activities of Daily Living Score (NEADL). The patients (848 in the intervention group and 800 in the control group) were assessed at baseline and were similar, though the control group were recruited in two blocks between November 1998 and November 2000 and the intervention group were recruited in two blocks between January 2001 and October 2001. At 12‐month follow‐up the mean NEADL score decreased by ‐2.23 (SD 3.69) for the intervention group patients (n = 483) and by ‐2.51 (SD 3.65) for the control group patients (n = 490). The difference of the means was 0.28 (95% CI ‐0.18 to 0.74). By 12 months 333 patients (39%) had died in the intervention group and 301 patients (38%) had died in the control group.
Evaluation of the intervention
The corresponding author reported that no evaluation was performed.
Summary: the level of independence decreased by a similar amount in the two groups by the six‐month follow‐up.
Controlled before‐and‐after studies (CBAs)
Hultberg 2005 (a controlled before‐and‐after study with high risk of bias) assessed whether intensifying services through co‐financed teams with personnel from primary care, social insurance and social services would have any effect on the health status of patients attending rehabilitation services for musculoskeletal disorders in primary care health centres. Despite extending recruitment by eight months the study managed to recruit less than half the targeted sample size, with 107 in the intervention group and 31 in the control group. Participants were assessed at baseline and were similar for lifestyle and clinical characteristics. Demographic distributions were similar but there were differences in socio‐economic distribution, with a higher proportion of white collar workers in the intervention group. At 12‐month follow‐up 57% (61/107) of intervention patients and 58% (18/31) of control patients had an increased perceived pain level (P = 0.712). A further 24% (26/107) of intervention patients and 29% (9/31) of control patients had a decreased perceived pain level at this point (P value not given). The mean changes in EuroQol 5 dimensions (EQ‐5D) index values between baseline and one‐year follow‐up were +0.145 for the intervention patients and +0.069 for the controls but the difference was not significant (P = 0.27).
Evaluation of the intervention
The corresponding author reported that no evaluation was performed.
Summary: there were no statistically significant differences in pain levels or quality of life between the intervention and control groups at follow‐up.
Kloek 2006 (a controlled before‐and‐after study with high risk of bias) investigated the impact of a two‐year community intervention on health‐related behaviour among adults aged 18 to 65 years living in deprived neighbourhoods. At baseline 2781 participants, of 4800 who were eligible, completed a postal questionnaire (1426 in the intervention neighbourhoods and 1355 in the control neighbourhoods) and the characteristics of the respondents in the two groups were similar. Two‐year follow‐up data were collected from 69% (n = 1929) of the respondents to the baseline survey but not all people completed all the data fields. From baseline to two‐year follow‐up, mean vegetable consumption (g/day) changed from 100 (SD 51) g/day to 99 (SD 52) g/day for 953 people in the intervention neighbourhoods and from 99 (SD 52) g/day to 100 (SD 51) g/day for 851 people in the control neighbourhoods. Mean fruit consumption had changed from 125 (SD 105) g/day to 130 (SD105) g/day for 958 people in the intervention neighbourhoods and from 130 (SD 106) g/day to 125 (SD 101) g/day for 856 people in the control neighbourhoods. Physical activity was estimated as METs/week, where MET is the metabolic energy expenditure calculated as the total minutes of physical activity per week multiplied by the intensity. Mean physical activity had changed from 7253 (SD 5443) METs/week to 6898 (SD 5358) METs/week for 953 people in the intervention neighbourhoods and from 6931 (SD 4945) METs/week to 6817 (SD 4677) METs/week for 832 people in the control neighbourhoods. The percentage of people who were current smokers changed from 41% to 40% for 938 people in the intervention neighbourhoods and from 41% to 39% for 853 people in the control neighbourhoods. The percentage of people who had excessive alcohol consumption changed from 5% to 4% for 964 people in the intervention neighbourhoods and from 8% to 7% for 853 people in the control neighbourhoods. Analysis of covariance of 15 comparisons within and between the groups showed that none of these changes were significant apart from fruit consumption, which attained borderline significance (P = 0.044).
Evaluation of the intervention
A formal process evaluation was conducted. Data were gathered prospectively though the programme using documentation of meetings and activities. A postal questionnaire was conducted at the end of the intervention asking questions about programme awareness and programme participation. The number of activities run (dose delivered), the number of people who took part (dose received) and the reach of the programme across the intervention areas were all analysed. An organisational chart was produced showing the involvement of the participating organisations in the development of community plans and implementation of the programme.
For dose delivered: of 53 planned activities, 10 could not be delivered due to low participation rates of neighbourhood residents. Dose received: across the intervention neighbourhoods, 69% to 71% of the survey respondents were aware of one or more large‐scale programme activities and 11% to 13% had taken part in at least one of the activities. Reach: the programme was thought to have reached around 2500 residents altogether, 21% of one neighbourhood and 62% of the other. The authors found a difference in goals and priorities. The Municipal Health Services wanted to use evidence‐based methods for the purposes of research; whilst the neighbourhood coalition wanted to use intuitively reasonable methods to promote behaviour change. They also found that most funding came from external sources and the Municipal Health Service, raising concerns about sustainability of future community coalitions. They concluded that it is feasible to deliver a community intervention in deprived neighbourhoods but that the intervention they used may not have been strong enough or achieved sufficient exposure to attain community‐wide health behaviour change. They also concluded that practitioners and researchers should agree beforehand on what the realistic goals are and valid outcomes for any proposed community health programme.
Summary: there were no significant differences between the two groups in four of the five outcomes at follow‐up. There was a small statistically significant improvement in self‐reported fruit consumption but this could have been a chance finding as so many comparisons were analysed. It is not clear how important this improvement would be for individuals' overall health levels.
Smylie 2008 (a controlled before‐and‐after study with a high risk of bias) evaluated an extended sex education programme for grade nine students in six (three intervention) public schools in Windsor‐Essex County, Canada. The intervention consisted of in‐school class‐based student learning, videos and discussions on dating and healthy relationships, teen panel discussion, a teens interacting with parents newsletter and parent workshops. There was no primary outcome as it was thought to be inappropriate to ask about sexual behaviours in under 16s, but a range of knowledge, values, attitudes, perceived risk, communication about sex, self‐efficacy and skills were measured through self‐completed questionnaires in class. The authors point out that given the large number of tests for significance, confidence should only be placed in results at P = 0.01 or lower.
The mean percentage of all questions answered correctly at baseline was 78% (n = 240). At follow‐up this was 87% for the intervention group (n = 95) and 79% for the control group (n = 116) (P < 0.001). Birth control attitudes changed from 7.00 at baseline (n = 240) to 6.55 for the intervention group (n = 6.55) and 7.59 for the control group (n = 116), where lower values represented more positive attitudes towards birth control. The difference was not significant. For contraceptive agency (the degree to which students felt comfortable accessing and using birth control) responses had changed from 7.41 (n = 240) to 6.72 for the intervention group (n = 95) and 6.86 for the control group (n = 116), where lower values represented higher contraceptive agency. These differences were not significant. Communication with others about sexuality had changed from baseline 13.28 (n = 240) to 12.86 for the intervention group (n = 95) and 11.96 for the control group (n = 116), where lower values represented more comfort talking about sexuality with the named party. The differences were not significant. Awareness of own sexual responses changed from 7.27 at baseline (n = 240) to 6.81 for the intervention group (n = 95) and 6.49 for the control group (n = 116), where lower values represented more sex comfort. The change for the control group was not significant at the 0.01 level, nor for the intervention group. Sex role attitudes changed from 8.05 at baseline (n = 240) to 7.11 in the intervention group (n = 95) and 8.95 in the control group (n = 116), where higher values represented stronger traditional sex role values. The difference between intervention and control groups was significant at follow‐up (P < 0.001). Sexual interaction values changed from 8.56 at baseline (n = 240) to 8.23 for the intervention group (n = 95) and 9.86 for the control group (n = 116), where lower values represented greater acceptance of a partner's rejection of sexual activity. The difference between the intervention and control group at follow‐up was not significant at the 0.01 level.
Evaluation of the intervention
The corresponding author reported that no evaluation was performed.
Summary: there were some changes in knowledge and attitudes of the students from this intervention but these measures were taken only one month after completion of the programme and did not necessarily lead to change in actual behaviour of the students. However, the statistics were not fully reported, particularly any differences between intervention and control groups at baseline.
Tucker 2006 (a controlled before‐and‐after study with high risk of bias) evaluated the effect of the Sexual Health and Relationships Education (SHARE) project. SHARE was part of a national demonstration programme Healthy Respect on teenage sexual health behaviour. The team evaluated project outcomes through surveys of year three and four pupils (average age 14 years 6 months) in 2001 and again in 2003, two years after implementation of the project. They used a standardised 12‐part questionnaire (the SHARE questionnaire) to test for changes in the proportion of pupils reporting sexual intercourse at age < 16 years, and changes in knowledge, attitudes and intentions related to sexually transmitted infections (STI) and condom use. Children in the intervention schools were similar to those in the control schools for gender, family composition and ethnicity but there were differences in parental house ownership, educational attainment and employment. These variables were included in the multivariate models for adjustment. In the intervention schools 2760 children completed the questionnaire at baseline and 2796 at the two‐year follow‐up. In the control schools, 1564 children completed the questionnaire at baseline and 1583 at follow‐up.
At baseline 665 children (24%) in the intervention schools reported sexual intercourse compared to 287 children (19%) in the control schools, adjusted OR of 1.29 (95% CI 1.10 to 1.52, P = 0.002). At two‐year follow‐up 629 (23%) of children in the intervention schools reported sexual intercourse compared to 280 (18%) in the control schools. The statistically significant differences between the intervention and control schools at baseline for reported sexual intercourse were maintained at two‐year follow‐up, with the intervention schools still reporting higher levels than the control schools (OR 1.35, 95% CI 1.15 to 1.60, P < 0.001).
Knowledge: at baseline 1845 children in the intervention schools (69%) knew that STIs may be asymptomatic compared to 1066 children (72%) in the control schools, adjusted OR of 0.95 (95% CI 0.82 to 1.10, P = 0.51). At follow‐up there was no significant change: 1966 children (74%) in the intervention schools knew that STIs may be asymptomatic compared to 1151 children (74%) in the control schools (OR 1.00, 95% CI 0.86 to 1.17, P = 0.96).
At baseline 972 children in the intervention schools (37%) believed that condom use reduced the chance of contracting an STI compared to 627 children (42%) in control schools, adjusted OR of 0.85 (95% CI 0.74 to 0.98, P = 0.02). At follow‐up the difference had disappeared: 1089 children (41%) in the intervention schools believed that condom use reduced their chance of contracting an STI compared to 647 children (42%) in the control schools (OR 1.00, 95% CI 0.88 to 1.14, P = 0.99).
At baseline 1667 children in the intervention schools (63%) believed that condoms are effective in preventing HIV/AIDS compared to 1040 children (70%) in the control schools, adjusted OR of 0.78 (95% CI 0.67 to 0.90, P = 0.001). At follow‐up the difference was smaller but still significant: 1739 children (65%) in the intervention schools believed that condoms are effective in preventing HIV/AIDS compared to 1082 children (70%) in the control schools (OR 0.85, 95% CI 0.73 to 0.98, P = 0.03).
Attitude: at baseline 2090 children in the intervention schools (79%) agreed with planning protection from STIs before sex compared with 1220 children (82%) in the control schools, adjusted OR of 0.88 (95% CI 0.74 to 1.05, P = 0.15). At follow‐up 2186 children in the intervention schools (82%) agreed with planning protection from STIs before sex compared with 1301 children (84%) in the control schools, adjusted OR of 0.92 (95% CI 0.77 to 1.10, P = 0.34).
Intention: at baseline 1737 children in the intervention schools (66%) intended to obtain their own condoms compared with 983 (66%) in the control schools, adjusted OR of 1.0 (95% CI 0.86 to 1.15, P = 0.98). At follow‐up 1825 children (69%) in the intervention schools intended to obtain their own condoms compared with 1061 children (69%) in the control schools, adjusted OR of 1.03 (95% CI 0.89 to 1.19, P = 0.73).
Evaluation of the intervention
This study was a demonstration project conducted in 2001 to 2003 as part of the Healthy Respect programme. A formal independent evaluation was conducted using inventories of services associated with sexual health provision, interviews with professional staff and young people, and from scrutiny of committee documentation and project reports. They found evidence of extensive partnership working and new forms of service delivery. Partnership development was not uniform and some key agencies were under‐represented, particularly community education and social work. They commented that young people were not well engaged in the development of services. Consultation exercises about drop‐in centres demonstrated young people wanted longer opening hours, services at weekends, access to contraceptives and a holistic approach; but few of these were met. There were also many concurrent initiatives in the intervention and control areas aimed at improving life chances of young people. These could have masked or magnified the effect of the intervention. However, the researchers concluded that valuable sustainable partnerships had been established which would help develop sexual health services for young people over a longer time period. A second phase of Healthy Respect has since been run.
Summary: children in the intervention area were more likely to report sexual intercourse than the children in the control area and the difference was statistically significant at baseline and two years after implementation of the programme. The children in the intervention school were as likely as those in the control schools to know that STIs can be asymptomatic and this did not change after two years. Children in the intervention schools were less likely to believe that use of condoms reduced the chance of contracting STIs at baseline but the difference had disappeared at follow‐up. However, fewer children in the intervention schools knew that condoms are effective at preventing HIV/AIDS than in the control schools at baseline and after two years. The attitudes and intentions in the two groups remained similar.
Interrupted time series (ITS)
Florence 2011 (an interrupted time series study with a low risk of bias) evaluated the impact of anonymised information sharing between agencies to prevent injury related to violence. The Cardiff Violence Prevention Programme developed a data sharing strategy. Information (location, time, day and type of weapon) from all patients reporting injury in a violent incident was captured electronically in hospital emergency departments. The personal identifiers were deleted and the information shared with the partnership crime analyst, who combined it with police intelligence data to generate maps of violence hotspots. This allowed specific risks and patterns to be observed by the partnership and led to new strategies by police and the local authority to minimise the risk of further violence. There were 33 months of observation before the programme was implemented and 51 months after implementation.
Florence reported incidence rates of hospital admissions related to violence before and after intervention in the control and intervention cities (Cardiff being the intervention city compared to 14 cities designated 'most similar' by the Home Office in England and Wales).
Monthly average counts of hospital admissions after violence changed from 21.03 before implementation to 16.89 after implementation in the intervention city and from 21.20 to 33.35 in control cities. The population adjusted rate of violence per 100,000 population changed from 6.71 to 5.39 in the intervention city and from 5.33 to 8.39 in the control cities. An adjusted analysis indicated this was statistically significant (incidence ratio 0.79, 95% CI 0.73 to 0.85).
Police recorded that wounding assaults changed from 168.52 to 256.76 in the intervention city and from 181.03 to 382.48 in the control cities. Population adjusted rates per 100,000 population for police recorded wounding assaults changed from 53.79 to 81.96 in the intervention city and from 53.86 to 113.80 in the control cities. An adjusted analysis indicated this was statistically significant (incidence ratio 0.68, 95% CI 0.61 to 0.75).
Police recorded common assaults changed from 47.79 to 61.14 in the intervention city and from 142.65 to 110.88 in the control cities, with population adjusted rates per 100,000 population changing from 15.25 to 19.51 in the intervention city and from 42.44 to 32.99 in the control cities. An adjusted analysis indicated this was statistically significant (incidence ratio 1.38, 95% CI 1.13 to 1.70).
This is consistent with the intervention successfully downgrading woundings to less serious assaults in the intervention group.
Evaluation of the intervention
No process evaluation has been identified.
Summary: the partnership based on information sharing and redirecting resources to tackle violence hotspots led to a substantial reduction in violent injury.
Outcomes by study design
Summarising the evidence from the seven RCTs, evidence of health benefit was extremely weak. Lumley 2006, a study at low risk of bias, showed no evidence of health gain. Woodfine 2011 found parents reported that asthma had less impact on their children's lives following home modification but there was no improvement in overall physical or psychosocial quality of life. In Vickrey 2006 the carers reported health benefits for patients but not for themselves. Bertelsen 2008 showed inconsistent results with benefits in three out of four measures following unblinded intermediate assessment. The fourth study (Bruzzese 2006) showed no health benefits for patients or their carers. Coppins 2011 and Rosen 2006 found no health benefits.
Looking at the four CCTs, Melle 2008, a study at medium risk of bias, showed a reduced duration of untreated psychosis in the experimental group but this did nor appear to translate into longer‐term benefit: only one of the four mental health scores showed a significant difference and this measurement was possibly biased due to unblinded clinical assessment. Of the remaining CCTs, Cooper 1975 showed clear benefits in both intervention and control groups, although the benefit was higher in the former. Challis 2002 showed benefit in just one measure out of many and Young 2005 showed no health benefits. Challis 2002 recognised the burden on carers but the intervention did not improve carers' health.
Of the CBAs, Kloek 2006 conducted several analyses and found one positive measure that was of doubtful clinical significance (self‐reported fruit consumption). Hultberg 2005 showed no health benefits in any measures. The results of the study by Tucker 2006 were that the intervention group's worse health behaviour at baseline, a higher rate of sexual intercourse under the age of 16 years, remained at follow‐up two years later. Smylie 2008 reported some short‐term changes in knowledge and attitudes but there was no longer term follow‐up to see if the benefits were sustained or led to changes in behaviour.
The only ITS identified (Florence 2011) entailed a long‐term partnership with continuing dialogue between partners resulting in multiple collaborative interventions. It appeared to lead to a significant reduction in violent injury.
Interventions to improve care or treatment of individual patients
Of the seven interventions designed to improve the management of individual patients, two showed clear health benefits (Cooper 1975; Vickrey 2006), two showed benefits in some measures (Bertelsen 2008; Challis 2002) and three showed no benefits from the interventions (Bruzzese 2006; Hultberg 2005; Young 2005).
Health education, health promotion or disease prevention initiatives
Of the seven population‐level interventions, one showed a decreased rate of violent injuries (Florence 2011) and four showed improvement in one or more of the many health outcomes measured (Kloek 2006; Melle 2008; Smylie 2008; Woodfine 2011). Two studies showed no benefits (Lumley 2006; Tucker 2006).
Mental health initiatives
The largest study in the review, and the only mental health intervention rated as low risk of bias (Lumley 2006), identified no health benefits. Cooper 1975 suggested a real improvement for the intervention group and Vickrey 2006 reported health benefits for the patients but not the carers. Bertelsen 2008 showed inconsistent results with some but not all measures of symptoms improved. Melle 2008 and Challis 2002 showed a mixed picture, with benefits in a small proportion of the many outcomes measured.
Healthy lifestyle initiatives
Kloek 2006 failed to show any health benefit arising from a wide‐ranging community intervention apart from a minimal increase in self‐reported fruit consumption. In Tucker 2006 the children in the intervention group had worse outcomes than the control group for reported sexual intercourse under the age of 16 years. Both studies were at high risk of bias. Rosen 2006 and Coppins 2011 also found no health benefits from their interventions.
Chronic disease management
Bruzzese 2006, Hultberg 2005 and Young 2005 all failed to demonstrate any health benefit from their interventions. All these studies were at high risk of bias.
Resource implications
Resource data presented in the reports were captured and, where no quantitative data were available, qualitative conclusions were made by the review authors on the level of resources which would be required to deliver the intervention being tested (see Table 2).
| Study | Observations on resources needed to deliver the intervention |
| Bertelsen 2008 | Significant additional resource required to deliver intervention. |
| Bruzzese 2006 | Substantial support needed to deliver the intervention. |
| Challis 2002 | Mean costs per annum: £23,402 for intervention group, £19,053 for control group. Additional resources required could account for any benefits achieved. |
| Cooper 1975 | Additional resources in intervention group included a social worker allocated to GP practice and involvement of two research team psychiatrists. |
|
Coppins 2011 NEW |
Cost per child was estimated at £403 compared with £45 for usual care of 1.5 hours of individual dietetic consultations. |
|
Florence 2011 NEW |
Additional resource was a data analyst to combine health and police data. |
| Hultberg 2005 | The total healthcare cost for an average patient in the intervention was EUR 1979 and EUR 1286 for controls. |
| Kloek 2006 | Expensive programme to implement and additional service could explain any improvements rather than the collaboration itself. |
| Lumley 2006 | Additional resource requirements included employment and training of community development officers and the production and distribution of information packs. |
| Melle 2008 | Additional resources would be required to replicate this service. (USD 390 for awareness raising strategies ‐ unclear whether this is per patient) |
|
Rosen 2006 NEW |
Additional resources included medical and epidemiological lectures given to the teachers, environmental equipment for the preschools, educational resource packs and puppet theatre visits. For the home intervention there were information packages. Teachers needed to spend time reinforcing hand hygiene messages with the children in class. |
|
Smylie 2008 NEW |
The routine sex education curriculum was usually delivered by physical education teachers and varied in time spent and style of delivery. The intervention programme was highly structured and included several specialists: sexual health worker, social worker from a sexual assault crisis centre, public health nurse. Plus a newsletter and several three‐hour parent workshops. |
| Tucker 2006 | Exact costs unclear though additional costs incurred for training and new drop‐in centres. |
| Vickrey 2006 | Significant extra resources appeared to be used in the intervention group, although it is unclear what costs were associated with this. |
|
Woodfine 2011 NEW |
Significant additional resource required. Cost effectiveness of intervention: Shift from ‘severe’ to ‘moderate’ asthma: I = 17%; C =3%. Mean cost of modifications: £1718 per child treated or £12,300 per child shifted from ‘severe’ to ‘moderate’. No significant difference in healthcare costs over 12 months between groups. ‘Bootstrapping’ gave an incremental cost‐effectiveness ratio (ICER) of £234 per point improvement on the 100‐point PedsQL™ asthma‐specific scale (95% CI £140 to £590). ICER fell to £165 (95% CI £84 to £424) for children with ‘severe’ asthma. |
| Young 2005 | Appears to be reorganisation of existing resource rather than utilising additional resources. |
Table 2: Resources required to deliver the interventions in the included studies.
Several studies specifically reported the additional costs incurred by the intervention arm as compared to the control, and the team working with Woodfine 2011 conducted a formal cost‐effectiveness study alongside the RCT. Whilst costs were not provided for all studies, it was clear that in most studies the interventions required additional resources. Young 2005, the only study which appeared to require no additional resources, failed to demonstrate any benefits arising from the intervention.
Meta‐analysis of the effects of interventions
Mortality
Three studies were included in a meta‐analysis investigating the impact of collaboration on mortality (Challis 2002; Vickrey 2006; Young 2005) as shown in Analysis 1.1. The pooled relative risk was 1.04 in favour of control (95% CI 0.92 to1.17). The I2 statistic was 0%. There was no difference in the relative risk of mortality in the intervention population compared to the control population. These three studies all investigated older patients: Challis 2002 and Vickrey 2006 were conducted in patients with dementia; and Young 2005 was conducted in patients presenting to emergency admission elderly care departments with falls, confusion, incontinence or immobility. This last study was the largest included in this meta‐analysis, contributing over 90% of the weight. Excluding it did not change the results (RR 0.95, 95% CI 0.61 to 1.48).
1.1. Analysis.
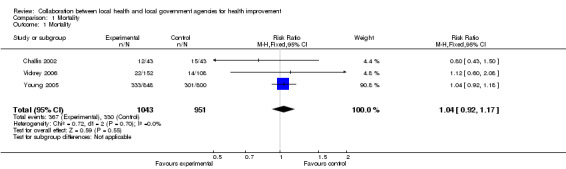
Comparison 1 Mortality, Outcome 1 Mortality.
Morbidity
Morbidity was addressed under four headings: mental health, physical health, quality of life and the Global Assessment of Function symptoms scale.
Mental health
Five studies were included in a meta‐analysis investigating the impact of collaboration on mental health (Bertelsen 2008; Cooper 1975; Lumley 2006; Melle 2008; Woodfine 2011; Woodfine 2011a) as shown in Analysis 2.1. The pooled standardised mean difference was ‐0.28, favouring intervention (95% CI ‐0.51 to ‐0.06). The I2 statistic was 84%, indicating that these results need to be interpreted cautiously. From a visual inspection of the forest plot the studies appear reasonably consistent, with only Lumley 2006 favouring control. Removing this study did not substantially alter the pooled relative risk (RR ‐0.36, 95% CI ‐0.52 to ‐ 0.19). The populations investigated in these studies were quite different: Bertelsen 2008 was conducted in patients with schizophenia; Cooper 1975 in patients with chronic neurotic illness; Lumley 2006 in pregnant women; Melle 2008 in patients with a diagnosed episode of psychosis; and Woodfine 2011 in children with asthma. The interventions were also very different.
2.1. Analysis.
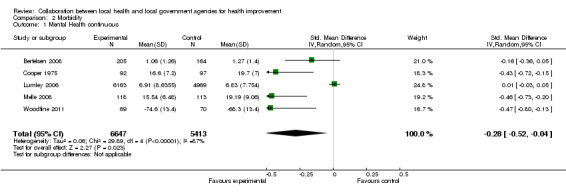
Comparison 2 Morbidity, Outcome 1 Mental Health continuous.
Physical health
Five studies were included in a meta‐analysis investigating the impact of collaboration on physical health (Bruzzese 2006; Coppins 2011; Hultberg 2005; Lumley 2006; Woodfine 2011; Woodfine 2011a) as shown in Analysis 2.2. The pooled standardised mean difference was statistically different from zero (SMD ‐0.07 in favour of intervention, 95% CI ‐0.20 to 0.07). There was no evidence of improved physical health in the intervention arm versus the control arm. Although the I2 statistic was only 16% the forest plot revealed some heterogeneity between the studies. This is to be expected as the study populations were quite different: kindergarten children with asthma (Bruzzese 2006); children aged 6 to 14 years old in the top 10% of BMI (Coppins 2011); adults with musculoskeletal disorders (Hultberg 2005); pregnant women (Lumley 2006); and children aged 5 to 14 years with asthma (Woodfine 2011). Most of the weight was assigned to Lumley 2006, being the largest paper, but excluding this study does not greatly alter the pooled relative risk (RR ‐0.08, 95% CI ‐0.28 to 0.12).
2.2. Analysis.
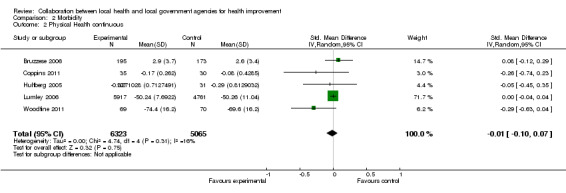
Comparison 2 Morbidity, Outcome 2 Physical Health continuous.
Quality of life
Three studies were included in a meta‐analysis investigating the impact of collaboration on quality of life (Bruzzese 2006; Vickrey 2006; Woodfine 2011; Woodfine 2011a) as shown in Analysis 2.3. The pooled standardised mean difference was not statistically different from zero (SMD ‐0.08 favouring intervention, 95% CI ‐0.44 to 0.27). The intervention effect was not large. The I2 statistic was 83%, and visual inspection of the forest plot did not indicate substantial heterogeneity. There was no significant difference in quality of life for the intervention arm compared to the control arm. Bruzzese 2006 was conducted in kindergarten children with asthma, Vickrey 2006 in patients with dementia, and Woodfine 2011 in children aged 5 to 14 years with asthma.
2.3. Analysis.
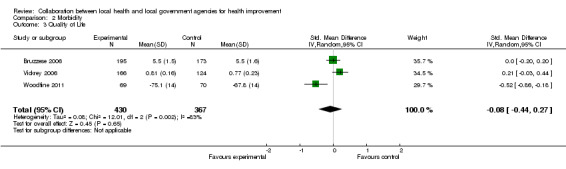
Comparison 2 Morbidity, Outcome 3 Quality of Life.
Global assessment of function symptoms score scale
Two studies were included in a meta‐analysis investigating the impact of collaboration on function measured by the Global Assessment of Function symptoms score (GAFSS) scale (Bertelsen 2008; Melle 2008) as shown in Analysis 2.4. The pooled mean difference was ‐2.63, favouring intervention (95% CI ‐5.16 to ‐0.10). The GAFSS scale ranges from 1 to 100 and so a difference of just over two and half should be considered a small effect. The I2 statistic was 0% and visual inspection of the forest plot indicated that the two studies were not substantially different. There was an improvement in the symptoms, as measured by the GAFSS, in the intervention arm versus the control arm and the improvement was statistically significant. Bertelsen 2008 was conducted in patients with schizophenia and Melle 2008 was conducted in patients with a diagnosed episode of psychosis.
2.4. Analysis.
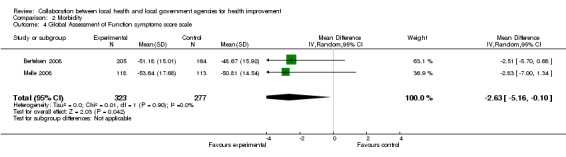
Comparison 2 Morbidity, Outcome 4 Global Assessment of Function symptoms score scale.
Rosen 2006 investigated the impact of the intervention on sickness absence, but the results were not included in any of the outcomes.
Behaviour change
Ony two studies addressed behaviour change outcomes (Kloek 2006; Smylie 2008). However the outcomes measured were very different: Kloek 2006 included exercise, diet, smoking status and alcohol consumption as outcomes whilst Smylie 2008 measured knowledge. Therefore no meta‐analysis was performed. One study investigated the impact of an intervention on handwashing (Rosen 2006), but data extraction could not be performed due to the lack of reported information.
In addition to Kloek 2006 and Smylie 2008, three other studies were not included in any meta‐analysis: Rosen 2006, Florence 2011 and Tucker 2006.
Since most studies included in the meta‐analyses were at high risk of bias, a sensitivity analysis was not performed.
Discussion
This review explores the health impact of local interagency collaborations between health and local government agencies compared to standard services, measured by changes in health outcomes.
The aim was to examine the effectiveness of collaborative interventions between agencies, and not disciplines. The routine services delivered to control groups in included studies were often coordinated between agencies but did not include staff members working outside their usual professional roles or their employing agencies. We found studies where individuals collaborated at the personal level or health organisations employed professionals who might traditionally work in local government, but we did not include them as the aim of the review was to examine studies where the agencies themselves established partnerships. This is a more sustainable solution than relying on individuals to maintain working practices outside their own organisation’s traditional boundaries.
From over 500 papers looked at in full text, only 16 studies were eligible for inclusion in the review and, overall, there was little or no reliable evidence of health benefits from the interventions.
Two possibilities need to be considered for this lack of effect. First, the process of collaboration may not have been optimal, leading to interventions not being fully delivered. There was evidence from the reports that some teams had not fully implemented the intervention (Bruzzese 2006; Young 2005) and this may have contributed to the lack of success in some studies.
Second, the process of collaboration was optimal but the desired outcomes were not achieved. Lumley 2006, the study with the highest number of participants, reported extensive activity directed at primary care and local community agencies to improve postnatal outcomes. Collaboration appeared to be effective and the interventions were delivered as planned but no health benefits were achieved. This would support the hypothesis that locally‐based collaboration is not associated with additional health benefits when compared to routine services.
Analysing evaluations linked to the included studies in this review may help answer why these interventions failed to make an impact on peoples' health, but few studies reported formal process of partnership evaluations. Where the research teams reported evaluations, or where they stated they had encountered difficulties, the details were captured.
The difficulties of delivering interventions at a population level
Conducting interventions at the population level requires different approaches from studies that assess the impact of interventions on individuals. Population‐level interventions are not conducted in isolation so control over settings and service delivery is harder to achieve, as demonstrated by the evaluation of Tucker's study of school students (Tucker 2006) which identified a number of other initiatives operating concurrently across the study area.
Whilst our searches identified initiatives from national programmes such as Sure Start 2004, no studies met the inclusion criteria.
Florence 2011, an ITS study, combined several sets of routinely collected data to identify potential trouble areas which could then be policed differently and could have environmental modifications. The partnership was established in 1997 and the programme was implemented in full from 2001, demonstrating the length of time it can take to develop working in effective partnership. Results are reported up to 2007 so the partnership was sustained over a number of years. The resulting trends in violent assault rates suggested substantial improvement for the intervention area compared to other similar cities.
Young 2005 reported that the implementation of intermediate care services coincided with the introduction of Primary Care Trusts, although they did not think this had an effect on the intervention as community services were not changed.
Lumley 2006 had the largest sample size. It reported a complex intervention, combining personal support to the target group of new mothers, educational support to the fathers of their respective babies, and environmental adjustments to encourage new mothers to socialise. The study failed to demonstrate any differences between intervention and control groups. In the five years that the study was being planned, changes were implemented in local government which included dismissing elected local councillors, appointing commissioners and amalgamating 210 local councils into 78. Half of all municipal services were put out to tender, including the maternal and child health programmes in most municipalities. It might be hard to maintain strong partnerships in the face of such disruption though the researchers still managed to deliver the intervention.
Some interventions may be applied to the whole population in order to deliver benefits to at‐risk groups or individuals within the population. This was the case for Melle 2008, where awareness‐raising information campaigns were designed for the general public, school children, teachers and health professionals to encourage early identification of individuals with possible psychosis, and so encourage prompt access to specialist assessment and treatment.
Kloek 2006 recognised that the results of their intervention might have reflected secular trends in the population of the Netherlands at that time. They assessed the potential impact of population movements on their results. Study authors estimated that 11% of respondents to their baseline survey had moved outside the intervention area at two‐year follow‐up. Those coming into the area after the start of the trial would have been less exposed to the intervention overall. Some of those moving out of the intervention area may have moved into a control area, potentially introducing contamination. The effect of these movements could be to mask the true size of effect that could be achieved by the intervention in a more controlled environment.
Randomization may only be possible at the organisational level, such as school, primary care clinic or area of residence, as many of the studies showed. It is particularly challenging for multi‐agency collaborative interventions to be implemented as RCTs as they are often, by necessity, implemented within organisational boundaries to conceal allocation. It has often been proposed that cohort studies or ITS studies should be used to research interventions at a population level but very few of these studies were found.
Achieving consistency in the intervention can be challenging. Young 2005 reported that the intervention was not delivered to the whole arm as planned. Where it was delivered there were delays in engaging with many of the cases.
Bertelsen 2008 demonstrated that it can be hard to maintain high follow‐up rates with long‐running studies.
The aim of the interventions was not always directly focused on improving the health of patients or the population. Young 2005 investigated the impact of intermediate care services for frail elderly patients following emergency admission. The explicit aim was to reduce long‐term care and hospital use, with the intermediate outcome being to improve patients' level of independence. It is possible that many other studies had similar underlying motives that were not acknowledged in the papers but which had been the driving force for setting up the intervention. Outcomes such as hospitalisation and other service use were not accepted as health outcomes for this review because the direction for health benefit is not always clear. Sometimes increased service use is a beneficial outcome, reflecting better access to an appropriate level of care, but in other instances it reflects more episodes of deterioration in health.
Effects of different models of collaboration
As much information as possible was captured on the levels at which collaboration was being developed, identifying strategic, commissioning and operational involvement of partners and the ways they worked together in teams (for example agreed strategies and protocols, multidisciplinary teams, joint training, evaluation and financing arrangements). This information is presented in a narrative form in the 'Characteristics of included studies' tables. The intention had been to explore the effect on health outcomes of different types of collaboration. However, as so many of the studies were at high risk of bias this analysis was not performed.
The impact of additional resources being used in the interventions
The focus of the review is health outcomes and not costs, cost effectiveness or cost benefits of experimental services. Therefore economic evaluations were excluded. Nonetheless, cost data were collected where reported, and where increased funding or resources were required to deliver the intervention this has been identified. The only formal cost‐effectiveness study, performed by Edwards 2011, was of Woodfine 2011. It demonstrated that a programme of environmental improvements to homes had led to improved quality of life. Although it had cost more than routine services, the analysis concluded that the programme was cost effective.
Many interventions consisted of enhanced services compared to the routine services available for the control groups. Despite the additional use of resources, few studies showed a significant impact on patient outcomes. If there had been a significant benefit for the intervention groups it would have been difficult to separate out the impact of collaboration from the impact of simply providing more care, more benefits or more support.
Unintended consequences
The narrative synthesis and the limited meta‐analyses of outcomes suggest the interventions lead to no or very weak health benefits, but there was no suggestion that collaboration was directly causing harm to participants.
Overall completeness and applicability of evidence
A large number of surveys and case studies were found, but no studies of collaborative interventions by local government and health agencies working together to tackle obesity prevention, drug and alcohol abuse or smoking cessation were identified. Of the included studies, mental health issues are covered in six studies (Bertelsen 2008; Cooper 1975; Lumley 2006; Melle 2008; Vickrey 2006; Woodfine 2011), musculoskeletal disorders in one (Hultberg 2005) and frail older people by one (Young 2005). The update has broadened the range, with additional studies looking at injury prevention (Florence 2011), the impact of hand washing programmes (Rosen 2006), obesity management (Coppins 2011), asthma (Bruzzese 2006; Woodfine 2011) and sexual knowledge and attitudes (Smylie 2008; Tucker 2006), and one on more general healthy lifestyles (Kloek 2006). Many interventions had broad aims to tackle a variety of lifestyles and environmental stresses rather than focusing on single issues. From a public health perspective, it is important to take this broad approach but it poses challenges to research as it makes the investigation complex and will generate multiple outcomes, where the significance of improvement in a single variable may be difficult to interpret.
Three studies addressed environmental facilities and resources to bring about improvements (Florence 2011; Rosen 2006; Woodfine 2011). Of these, two appear to have been successful, which is plausible as it is recognised that health is influenced by environmental factors (Marmot 2010).
Some studies based in low and middle income countries were identified but none met the inclusion criteria for this review. Studies were excluded for a variety of reasons, most notably study design or the lack of one or other partner (health or local authority). In addition, some presented collaborative work where the lead partner was an international agency and the level of local flexibility was limited.
Most studies included in this review were conducted in high income countries (UK, Australia, USA, Scandinavia, Canada and the Netherlands). They compared the outcomes of collaboration between local health and local government services with those achieved by local services routinely working together with clearly defined roles and responsibilities. The results may not be relevant where local services are still evolving, or where there are extreme shortages of staff and resources.
This review did not set out to examine how collaboration between partners can improve processes such as service planning, capacity building or service development. Equally the aim was not to look at collaboration taking place in response to acute incidents or disease outbreaks. Such collaborations are in effect the local routine services working together in planned ways to manage unusual events. They tend to be reported post hoc and to focus on lessons learned for all partners.
Inadequate reporting of study design
Some potentially relevant studies were reported incompletely and did not present enough information to allow assessment of collaboration, study design or potential for bias. We attempted to contact authors for clarification but those studies which remained unclear were excluded (see Characteristics of excluded studies).
Quality of evidence
Many of the identified studies were investigating relevant partnerships but were of poor quality or failed to implement the intended service (see Characteristics of excluded studies). All the included studies except Lumley 2006 and Woodfine 2011 had methodological weaknesses with the potential for bias. Common problems included lack of allocation concealment, blinded outcome assessment and either a lack of information on study power or a failure to recruit sufficient participants. Some included studies examined how fully the interventions they were investigating had been implemented. Young 2005 found only 29% of patients in the intervention group received the care package; and of that group 44% not doing so until 10 days or more after discharge. Kloek 2006 reported that 53 activities had been planned as part of their community‐wide programme to improve health‐related behaviours but only 43 programmes ran.
Many studies reported that the period of follow‐up was too short to demonstrate the anticipated benefits, but the one study reporting five‐year results had follow‐up rates below 60% (Bertelsen 2008) and another study planning five and 10‐year follow‐up only presented patients' results at two‐year follow‐up despite being published 11 years after the start of the programme (Melle 2008).
This review has generated a picture of some scattered statistically significant health benefit outcomes but the overall distribution of positive findings is inconsistent within and between studies. Where studies used composite measures to assess health outcomes (such as SF‐36 and PANSS) they tended to report the measures in their component parts, for example as SF‐36 physical component score (PCS) and SF‐36 mental health component score (MCS), rather than reporting the overall measure. In such instances the possibility of selective outcome reporting cannot be excluded. Generally where there may be some statistically significant differences for component scores the clinical impact of these scores is less than that of the overall measure.
Agreements and disagreements with other studies or reviews
There is a huge volume of literature documenting collaborative interventions where benefits have been claimed, but we did not find any other recent systematic reviews addressing this overarching question. A similar systematic review looking at the impact of multi‐agency partnerships on public health outcomes, which excluded studies measuring impact on individuals, reported that evidence was partial and it was difficult to ascertain any health effects attributable to partnership working, despite the costs associated with establishing these public health partnerships (Smith 2009).
In the context of few rigorously designed and conducted studies on this topic, it is not clear that collaborative arrangements are more beneficial to the health of the participants than standard care. Even if collaboration could improve health outcomes, there are insufficient data to determine which models are most likely to be successful. The literature identified on improving lifestyles is based largely on subjective measures, including attitudes, but there is little evidence of meaningful benefits resulting from such changes. In the area of chronic disease management the literature was dominated by case studies and small single centre studies, which do not generate strong evidence of benefit or harm. Included mental health studies reported positive outcomes in component scores but the overall outcomes do not indicate that collaboration confers health benefits at either patient or population level. There is no evidence of clinically important benefit from the studies we identified in health promotion and health education interventions or in chronic disease management.
Authors' conclusions
Implications for practice.
Despite decades of research on the impact of enhanced collaboration between local health and local government services there is no reliable evidence that it necessarily improves health outcomes when compared to standard services.
This review only identified two methodologically sound, high quality studies. One of these showed modest improvements in some aspects of health, the other found no health improvements. Some studies reported a few positive outcomes but these were not reflected in the overall outcome measures and the positive results may have been due to the additional funding or resources that were made available for the collaboration.
It is possible that local collaborative partnerships making environmental changes may succeed in improving health but the evidence base is still too weak to be confident that this is the case.
Multi‐agency collaborative initiatives are hard to implement, usually more expensive than standard services, and may be subject to external changes outside the control of the partnership. New partnerships should be clear about the outcomes they aim to achieve and these outcomes should be relevant to all partners. They should monitor outcomes, ideally starting well before any intervention is initiated, and evaluate how well they are delivering any new service.
When considering changes in service provision, evaluation needs to be included in the planning phase and before the implementation of the service in order to demonstrate whether the services are being delivered as designed and if they are working as well as intended. There needs to be a distinction between how well the service is being delivered and what outcomes the service is achieving.
Implications for research.
Although agencies and individual professionals appear enthusiastic about collaboration, methodological problems in the primary studies and incomplete implementation of initiatives have prevented the development of a strong evidence base to understand what, if anything, works and why. We will continue to look for evidence on how well collaborations work for future updates, particularly searching for process and partnership evaluations of our included studies. We welcome comments and information on potentially relevant papers and studies.
High quality population‐level research is hard to conduct and there are many questions still unanswered about partnership working. Our review has demonstrated that RCT designs for population studies are possible, though challenging to conduct with sufficient rigour. Consideration needs to be given to designing studies using methods in line with best practice before the intervention is implemented. Research studies need to have comparable intervention and control groups and the partnership being tested needs to be clearly described in terms of agencies engaged, what their roles are, what resources are being shared, whether any joint documents such as plans and protocols are being used and whether any training, audit or evaluation is undertaken. Clear results need to be presented in a timely fashion and in sufficient detail to support critical appraisal.
Service development in low and middle income countries is often supported by international aid agencies but there is little evidence of how to establish effective local partnerships. A systematic review looking at outcomes from international agencies working with multi‐agency local partnerships in low and middle income countries would add valuable evidence in this area.
Further research is needed to understand how to influence behaviour for public health gain in the context of challenging global secular changes. Further attention should be given to exploring the potential health gains that can be achieved through collaborating to implement environmental changes.
What's new
| Date | Event | Description |
|---|---|---|
| 30 August 2012 | New citation required but conclusions have not changed | The evidence base remains weak and results are largely unchanged from previous version. |
| 22 August 2012 | New search has been performed | Update search was performed from January 2008 to 31 December 2011 and five new studies were identified. Information on process or partnership evaluations has been included where available. Meta‐analysis was performed using studies with comparable outcomes. Summary of findings table was added. The evidence base remains weak and results are largely unchanged. |
History
Protocol first published: Issue 2, 2009 Review first published: Issue 6, 2011
| Date | Event | Description |
|---|---|---|
| 22 August 2012 | New search has been performed | Update search was performed from January 2008 to 31 December 2011 and five new studies were identified. Information on process or partnership evaluations has been included where available. Meta‐analysis was performed using studies with comparable outcomes. Summary of findings table was added. The evidence base remains weak and results are largely unchanged. |
| 26 July 2011 | Amended | Response rate exclusion criteria made more explicit. Five year assessment data for Bertelsen have been excluded as response rate was less than 60%. More detailed reasons for exclusion have been given in the characteristics of excluded studies table. Lumley 2006 reference corrected. |
| 11 August 2010 | New search has been performed | Final draft submitted for editorial approval |
Acknowledgements
The authorship team would like to thank Clair Stansfield for searching the Database of Promoting Health Effectiveness Reviews (DoPHER) and Dr Helen Morgan for searching the Cochrane Public Health Group Specialized Register. Also thanks to all the authors who provided additional data to be used in this review. Thanks go to Dr Laurie Anderson, Professor Elizabeth Waters, Professor Mark Petticrew and Jodie Doyle for their editorial support during the update of this review. We would like to acknowledge the helpful peer review contributions from Professor Walid El Ansari and Dr Lucie Rychetnik. An additional referee reviewed the first version of this review, but not this updated 2012 version. Finally, the team is particularly grateful to Dr Belinda Burford for her invaluable advice.
Appendices
Appendix 1. APPENDIX 1. Validated tools
Barthel Index(BI) is a widely used measure of functional disability. The index was developed for use in rehabilitation patients with stroke and other neuromuscular or musculoskeletal disorders. Mahoney F, Barthel DW. Functional evaluation: the Barthel index. Maryland State Med J 1965; 14:615. Young 2005
Comprehensive Assessment and Referral Evaluation (CARE) covers a wide range of psychiatric, medical, and social problems. It has been, for certain purposes, reduced to a relatively brief instrument, the SHORT‐CARE, that measures three major content areas: depression, dementia, and disability. Gurland B, Golden R, Tereesi J, Challop J. The Short‐Care: An Efficient Instrument for the Assessment of Depression, Dementia and Disability. Journal of Gerontology 1984; 39:158‐65. Challis 2002
Clifton Assessment Procedures for the Elderly (CAPE) is intended to assess level of disability and estimate need for care. It consists of a short cognitive scale and a behavioural rating scale. The latter has four sub‐scales: physical disability, apathy, communication difficulties and social disturbance. Pattie A, Gilleard C (1979) Manual of the Clifton Assessment Procedures for the Elderly. Hodder & Stoughton: Sevenoaks. Challis 2002
Edinburgh Postnatal Depression Scale (EPDS) screening tool with 10‐question to identify patients at risk for 'perinatal' depression. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10‐item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987; 150:782‐6. Lumley 2006
EuroQol 5 dimensions instrument (EQ‐5D) is a standardised instrument for use as a measure of health outcome. Dolan P (1997). Modeling valuations for EuroQol health states. Med Care, 35(11):1095‐108. Hultberg 2005
Global Assessment of Functioning and Symptoms (GAF) a scale used to assess psychiatric status, ranging from 1 (lowest level of functioning) to 100 (highest level), can be split into GAFs( measuring symptoms) and GAFf (measuring function). American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition. Washington, DC: American Psychiatric Association;1987. Bertelsen 2008, Melle 2008
GHQ‐30 30‐item General Health Questionnaire which provides a measure of the number of psychiatric symptoms reported. Goldberg DP, Williams P. A user’s guide to the General Health Questionnaire. Windsor: NFER‐NELSON, 1988. Cooper 1975
Hospital Anxiety and Depression score, (HAD) is a self screening questionnaire for depression and anxiety. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 1983; 67: 36171. Young 2005
Metabolic Equivalent of Task (MET) or the standard metabolic equivalent is a unit used to estimate the amount of oxygen used by the body during physical activity. Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Montoye HJ, Sallis JF, Paffenbarger RS. Compendium of physical activities: classification of energy costs of human physical activities. Medicine and Science in Sports and Exercise 1993;25:7180. Kloek 2006
Nottingham Extended Activities of Daily Living, (NEADL) in the assessment of disability in chronic airflow limitation in old age. Nouri FM, Lincoln NB. An extended activities of daily living scale for stroke patients. Clin Rehabil 1987; 1:3015. Young 2005
Pediatric Asthma Caregiver's Quality of Life Questionnaire (PACQLQ) measures the problems that are most troublesome to the parents (primary caregivers) of children with asthma. Juniper EF, Guyatt GH, Feeny D, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma. Quality of Life Research 1996b; 5:2734. Bruzzese 2006
Pediatric Quality of Life Inventory generic core scales (PedsQL) measures quality of life in children. The generic module assesses physical health on one subscale (8 items); psychosocial health on 3 subscales; emotional (5 items); social (5 items) and school (5 items). The asthma module has four subscales: symptons (11 items); treatment (11 items); worry (3 items) and communication (3 items). Varni JW, Burwinkle TM, Rapoff MA et al. The PedsQL in pediatric asthma; reliability and validity of the Pediatric Quality of Life Inventory generic core scales and asthma module. J Behav Med 2004; 27(3):297‐318. Woodfine 2011
Positive and Negative Syndrome Scale (PANSS) is a medical scale used for measuring symptom severity of patients with schizophrenia. Kay SR, Fiszbein A et al (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin 1987; 13:261‐7. Melle 2008
Premorbid Adjustment Scale (PAS) is a widely used rating scale to assess premorbid functioning retrospectively. Cannon‐Spoor H, Potkin SG, Wyatt RJ (1982) Measurement of premorbid adjustment in chronic schizophrenia. Schizophrenia Bulletin, 8:470‐84. Melle 2008
Scale for the Assessment of Negative Symptoms (SANS) is a 35 item scale with a six point classification of answers. Mean symptom responses were calculated so the score ranges from 0 to 6. Andreasen NC: Negative symptoms in schizophrenia: definition and reliability. Arch Gen Psychiatry 1982; 39:784–8. Bertelsen 2008
Scale for the Assessment of Positive Symptoms (SAPS) is a 35 item scale with a six point classification of answers. Mean symptom responses were calculated so the score ranges from 0 to 6. Andreasen NC. The Scale for the Assessment of Positive Symptoms (SAPS). Iowa City, IA: The University of Iowa,1984. Bertelsen 2008
Short Form 36 (SF‐36) is a multi‐purpose, short‐form health survey with 36 questions of health‐related quality of life Jenkinson C, Coulter A, Wright L. Short form 36 (SF‐36) health survey questionnaire: normative data for adults of working age. BMJ 1993; 306:1437‐40. Lumley 2006
Visual Analogue Scale (VAS) is the standard tool for rating of pain either patients’ own rating or rated by the health care worker. Gaston‐Johansson F, Asklund‐Gustafsson M (1985). A baseline study for the development of an instrument for the assessment of pain. Journal of Advanced Nursing, 10(6):539‐46. Hultberg 2005
Appendix 2. APPENDIX 2. Search strategies
Database: Ageline
Subject Term: interagency cooperation; interdisciplinary team care; service coordination (exact match) AND Subject Term: service delivery;health services; health promotion; psychiatric services; public health services; day care services; emergency health services; nursing; health needs; alcoholism; drug abuse; hospice; palliative care; terminal care ; psychotherapy; case management; crisis intervention (exact match) AND Subject Term: government agencies; government services; service planning ; public housing; boarding and care homes; sheltered housing; nursing home care; homeless; home modification; (exact match) AND Year: 1966‐2008 AND Audience: Research/Academic AND Document Type: Journal Article
Database: AMED (Allied and Complementary Medicine)
1. Public relations/
2. inter?institutional relation:.mp.
3. exp Interprofessional relations/
4. interprofessional: relation:.mp. or inter‐professional: relation:.tw.
5. community institutional relations.mp.
6. exp Cooperative behavior/
7. (cooperative: behavior: or co‐ooperative: behavior: or cooperative: behaviour: or co‐operative: behaviour: or cooperative: plan:).mp. or co‐operative: plan:.tw.
8. collaborat:.mp.
9. (cross‐system: or cross system: or cross disciplin:).mp. or cross‐disciplin:.tw.
10. interagenc:.mp. or inter‐agenc:.tw.
11. interdisciplin:.mp. or inter‐disciplin:.tw.
12. intersector:.mp. or inter‐sector:.tw.
13. (joint: commission: or joint‐commission: or joint: plan: or joint‐plan: or joint: work: or joint‐work: or joined up: or joined‐up).mp. or jointness:.tw.
14. (multiagenc: or multi‐agenc: or multidisciplin: or multi‐disciplin: or multiprofessional: or multi‐professional: or multi‐sector:).mp. or multisector:.tw.
15. (partnership: or teamwork: or team work:).mp. or team‐work:.tw.
16. (transdisciplin: or trans‐disciplin:).mp.
17. (integrat: adj5 (work: or profession: or partnership: or team: or teamwork: or disciplin: or agenc:)).tw.
18. Public health/
19. Health administration/
20. health planning organizations.mp.
21. community health planning.mp.
22. Health services accessibility/
23. exp Home care services/
24. (health services needs and demand).mp. [mp=abstract, heading words, title]
25. Health planning/
26. exp Health promotion/
27. Health services/
28. "Delivery of health care"/
29. Community health services/
30. community health cent:.tw.
31. community care.mp. or continuing care.tw. or long term care.tw. or longterm care.tw. or long‐term care.tw.
32. exp Health education/
33. exp Primary health care/
34. Comprehensive health care/
35. family physicians.mp.
36. Emergency medical services/
37. exp preventive health services/
38. nursing services.mp.
39. nursing/
40. public health nursing.mp.
41. Rehabilitation nursing/
42. Community health nursing/
43. health services for the aged.mp.
44. Rural health services/
45. indigenous health services.mp.
46. (indigenous and health service:).mp.
47. exp Mental health services/
48. Community mental health services/
49. exp Community mental health centers/
50. case management.mp.
51. community mental health team.mp.
52. crisis intervention.mp.
53. Psychotherapy/
54. adolescent health services.mp.
55. ((adolescent: or youth:) and health services).mp. [mp=abstract, heading words, title]
56. exp Child care/
57. child welfare.mp.
58. exp Child health services/
59. oral health.mp.
60. (teenage: or middle age: or middle‐age: or old age: or elderly).mp. [mp=abstract, heading words, title]
61. exp Geriatrics/
62. exp palliative care/
63. exp Terminal care/
64. exp Long term care/
65. primary prevention.mp.
66. exp Rehabilitation/
67. Occupational therapy/
68. communicable diseases.mp.
69. ((outbreak: or infection:) adj control:).tw.
70. immunization program:.mp.
71. Mass screening/
72. exp Rehabilitation centers/ or rehabilitation centres.mp.
73. exp Nursing homes/
74. nursing hom:.tw.
75. Hospice care/
76. Day care/
77. Respite care/
78. exp Substance related disorders/ and rehabilitation.mp. [mp=abstract, heading words, title]
79. (mass media adj5 (health: or campaign: or scheme: or program: or project: or intervention: or strateg:)).tw.
80. health promot: school:.tw.
81. (health adj5 (promot: or scheme: or program: or project: or strateg: or scheme: or intervention:)).tw.
82. school nurs:.mp.
83. (speech and language therapist:).mp.
84. (family physician: or doctor: or nurse: or general practitioner: or GP or geriatrician: or health visitor: or dietician: or dietitian: or nutritionist: or physiotherapist: or occupational therapist: or therapist: or midwife).mp. or midwives.tw.
85. (dietitian: or dietician:).tw.
86. (community adj2 (program: or scheme: or project: or intervention: or strateg:)).tw.
87. Prenatal care/ or antenatal care.tw. or prenatal care.tw.
88. (postnatal care or post natal care).mp. [mp=abstract, heading words, title]
89. ((geriatric evaluation or geriatric assessment) and management).mp.
90. government agencies.mp.
91. local government.mp.
92. ((municipal: or city or town: or local: or education: or school:) adj5 (council: or authorit: or govern: or board:)).tw.
93. (government: adj5 (agenc: or plan: or polic: or strateg:)).tw.
94. Housing/
95. public housing.mp. or council housing.tw. or local authority housing.tw. or social housing.tw.
96. Residence characteristics/
97. housing for the elderly.mp.
98. Home care services/ or home care agencies.mp.
99. homes for the aged.mp.
100. exp Residential facilities/
101. sheltered housing.mp.
102. ((shelter: or half‐way or half way) adj5 (hous: or home: or accommodat:)).tw.
103. Group homes/ or group home:.tw.
104. ((residential or nurs:) adj5 (home care or facilit:)).tw.
105. exp Nursing homes/
106. nurs: home:.mp.
107. ((foster or care) adj4 home:).tw.
108. (supported living or assisted living).tw.
109. exp homeless persons/
110. homeless:.tw.
111. exp social work/
112. exp social security/
113. exp social welfare/
114. (social: adj4 (work: or support: or security or care: or welfare: or service: or network:)).tw.
115. consumer advocacy.mp.
116. Counseling/
117. Civil rights/
118. Home care services/
119. Day care/ or day services.mp.
120. exp Substance related disorders/ and rehabilitation.mp.
121. Alcoholism/ and rehabilitation.mp. [mp=abstract, heading words, title]
122. Alcohol drinking/ and (prevention or control).mp.
123. exp Social behavior disorders/
124. Juvenile delinquency/
125. ((young or juvenile) adj2 offender:).tw.
126. (youth adj4 service:).tw.
127. ((leisure or community or youth or recreation:) adj2 (center: or centre:)).tw.
128. (play ground: or playground: or school yard: or schoolyard:).tw.
129. parks.mp. and recreation:.tw.
130. (housing and regeneration).mp.
131. ((neighbourhood or neighborhood) and (renew: or improv: or revitali?ation)).tw.
132. built environment.mp. or urban environment.tw.
133. ((child: or domestic: or partner: or spousal) adj3 (abuse: or violen: or protect:)).mp.
134. (foster home care or foster care).mp.
135. ((disabled persons or disabled people) and rehabilitation).mp. [mp=abstract, heading words, title]
136. home adaptation:.tw.
137. (local adj2 (council: or hous:)).tw.
138. play: field:.tw.
139. (school: adj2 (infant: or junior: or kindergarten or senior: or primary or comprehensive or grammar or high or elementary or secondary)).tw.
140. educational psychologist.mp. or Psychology educational/
141. ((environmental health or occupational health or housing or welfare rights or youth) adj5 (worker: or officer:)).tw.
142. public librar:.mp. or school teacher:.tw.
143. or/1‐17 [collaboration]
144. or/18‐89 [health]
145. or/90‐142 [government]
146. and/143‐145
147. Randomized controlled trials/
148. controlled clinical trial.mp.
149. intervention studies.mp.
150. experiment:.tw.
151. (time adj series).tw.
152. (pre test or pretest or (posttest or post test)).tw.
153. Random allocation/
154. impact.tw.
155. intervention?.tw.
156. chang:.tw.
157. evaluation studies.mp.
158. evaluat:.tw.
159. effect?.tw.
160. Comparative study/
161. or/147‐160
162. 146 and 161
163. 146 and 161
164. limit 163 to yr="1966 ‐ 2008"
Database: ASSIA (Applied Social Sciences Index and Abstracts)
Query: ((((DE="collaboration") or(DE="partnerships") or(DE="team work")
or(DE=("cooperation" or "cooperative behaviour")) or(DE=("integration" or
"integrative approach" or "cooperation" or "cooperative behaviour")))
or(AB=(collaborat* or interagenc* or multiagenc*) or
(inter‐institutional* or inter‐professional or inter‐departmental*) or
(interinstitutional* or interprofessional or interdepartmental*)))
or((interprofessional relation*) or(inter‐departmental)
or(multidisciplin*) or("cross disciplin*") or(interagency)))
and(((DE=("public health" or "public health care" or "public health
clinics" or "cooperation" or "cooperative behaviour")) or(DE=("community
health" or "community health care" or "community health centres" or
"community health services" or "community health workers" or
"cooperation" or "cooperative behaviour")) or(DE=("home care" or
"cooperation" or "cooperative behaviour" or "home based services"))
or(DE=("health policy" or "home based services" or "home care"))
or(DE=("behavioural health education" or "cooperation" or "cooperative
behaviour" or "health policy" or "home based services" or "home care"))
or(DE=("nurse practitioners" or "cooperation" or "cooperative behaviour"
or "health policy" or "home based services" or "home care"))
or(DE=("general practice" or "medicine" or "primary health care" or
"practice nurses")) or(DE="preventive health care") or(DE=("mental health
services" or "health services")) or(DE="paediatrics") or(DE="elderly
people") or(DE=("maternal health care" or "antenatal care"))
or(DE=("midwives" or "allied health professionals" or "community
midwifery" or "dietitians" or "health visiting" or "occupational
therapists" or "physiotherapists")) or(DE="health")) or(AB=(("family
physician*") or doctor* or (general practitioner*)) or AB=(nurs* or
("School nurs*") or geriatrician*) or AB=((occupational therapist*) or
physiotherapist* or nutritionist*) or AB=(dietitian* or dietician* or
("health visitor*")) or AB=(therapist* or midwives or midwife) or
AB=(("occupational therapist*") or physiotherapist* or ("respite care")))
or(DE=("antenatal" or "hospices" or "nursing" or "postnatal care" or
"rehabilitation" or "respite care"))) and(((DE=("local government" or
"government" or "district councils" or "local education authorities" or
"metropolitan councils" or "minority local government" or "municipal
government" or "social services departments")) or(KW=("municipal council*
or municipal authorit* government agencies" or "public administration"))
or((DE=("social security" or "social work" or "welfare"))
or(DE=("residential homes" or "social housing"))) or(DE=("child care" or
"disadvantaged people" or "foster care" or "homeless people"))
or(AB=(leisure or community or youth or recreation) NEAR (center* or
centre*)) or(AB=(play ground* or playground* or school yard* or
schoolyard)) or(AB=("built environment*" or "urban environment*"))
or(AB=("educational psychologist*" or "occupational psychologist*"))
or(AB=("environmental health" or "occupational health" or housing or
"welfare rights" or youth) NEAR (worker* or officer*)) or(DE=("child
care" or "disadvantaged people" or "foster care" or "homeless people"))
or(DE=("community care" or "community centres" or "community colleges" or
"community cooperatives" or "community development" or "community
education" or "local communities"))) or(DE=("day care" or "day care
centres" or "day centres" or "day foster care" or "community colleges" or
"community cooperatives" or "health centres")))
Database: CINAHL
(MH "Interprofessional Relations+")
TX interdepartmental* relation* or inter‐departmental* relation*
TX interprofessional* relation* or inter‐professional* relation*
(MH “Community‐Institutional Relations”)
(MH “Cooperative Behavior”)
TX cooperative* behavior* or TX cooperative* behaviour* or TX cooperative* plan* TX collaborat*
TX cross‐system* or TX cross system* or TX cross disciplin* or cross‐disciplin*
TX interagenc* or inter‐agenc*
TX interdisciplin* or inter‐disciplin*
TX intersector* or inter‐sector*
TX joint* commission* or TX joint‐commission* or TX joint* plan* or TX joint‐plan* or TX joint* work* or TX joint‐work* or TX joined up* or TX joined‐up or jointness*
TX multiagenc* or TX multi‐agenc* or TX multidisciplin* or TX multi‐disciplin* or TX multiprofessional* or TX multi‐professional* or TX multi‐sector* or multisector*
TX partnership* or TX teamwork* or TX team work* or team‐work*
TX transdisciplin* or TX trans‐disciplin*
integrat* N5 work*
integrat* N5 profession*
integrat* N5 partnership*
integrat* N5 team*
integrat* N5 teamwork*
integrat* N5 disciplin*
integrat* N5 agenc*
(MH “Public Health”)
(MH “Public Health Administration”)
(MH "Health and Welfare Planning+/AM/MT/TD")
(MH "Community Health Services+/AM/MT/TD")
(MH "Health Services Accessibility/AM")
(MH "Home Health Care+/AM/MA")
(MH "Health Services Needs and Demand+/AM")
(MH "Health Promotion+/AM/MA/MT")
(MH "Health Services")
(MH "Health Care Delivery/AM/MA/MT")
(MH "Community Health Centers/AM/MA")
TX community care or continuing care or long term care or longterm care or long‐term care
(MH "Community Health Services") or (MH "Health Education+/AM/MA/MT")
(MH "Primary Health Care")
(MH "Health Care Delivery+")
(MH "Physicians, Family")
(MH "Emergency Medical Services")
(MH "Nursing Administration+")
(MH "Community Health Nursing")
(MH "Rehabilitation Nursing")
TX community health nurs*
(MH “Health Services for the Aged”)
(MH "Rural Health Services/AM/MA")
(MH “Health Services, Indigenous”)
(MH "Mental Health Services+/AM/MA")
(MH "Community Mental Health Services")
TX community mental health cent*
(MH “Case Management”)
community mental health team*
(MH “Crisis Intervention”)
(MH "Psychotherapy/MT")
(MH “Adolescent Health Services”)
(MH "Child Care+")
(MH “Child Welfare+”)
(MH “Child Health Services+”)
(MH “Oral Health”)
(MH "Aged")
(MH "Geriatrics/MA/MT")
(MH "Palliative Care/MT/NU")
(MH "Terminal Care+/MT/NU")
(MH "Long Term Care/MT/NU")
(MH "Health Care Delivery/AM")
(MH "Health Manpower+/MA")
(MH "Rehabilitation+/AM/MA/MT/NU")
(MH “Rehabilitation”)
(MH “Occupational Therapy”)
(MH “Communicable Diseases”)
control and (outbreak* or infection*)
(MH "Immunization Programs/AM/MA/MT")
(MH "Health Screening+/AM/MT")
(MH "Rehabilitation Centers+")
(MH "Nursing Homes+/AM/MA")
nursing home*
(MH "Hospice Care")
(MH “Day Care”)
(MH “Respite Care”)
(MH "Substance Use Disorders+/RH")
mass media N5 health*
mass media N5 campaign*
mass media N5 program*
mass media N5 project*
mass media N5 intervention*
mass media N5 strateg*
health promot* school*
health N5 promot*
health N5 scheme*
health N5 program*
health N5 project*
health N5 strateg*
health N5 scheme*
health N5 intervention*
TX “speech and language therapist*” or TX speech therapist*
TX family physician* or TX doctor* or TX nurse* or TX general practitioner* or TX GP or TX geriatrician* or TX health visitor* or TX dietician* or TX dietician* or TX nutritionist* or TX physiotherapist* or TX occupational therapist* or TX therapist* or TX midwife or midwives
community N2 program*
community N2 scheme*
community N2 project*
community N2 intervention*
community N2 strateg*
(MH "Prenatal Care/AM/MA/MT")
(MH "Postnatal Care/AM/MA/MT")
TX geriatric evaluation and management
welfare right* N7 health*
(MH “Government Agencies”)
municipal* N5 council*
municipal* N5 authorit*
municipal* N5 govern*
municipal* N5 board*
city* N5 council*
city* N5 authorit*
city* N5 govern*
city* N5 board*
town* N5 council*
town* N5 authorit*
town* N5 govern*
town* N5 board*
local* N5 council*
local* N5 authorit*
local* N5 govern*
local* N5 board*
education* N5 council*
education* N5 authorit*
education * N5 govern*
education * N5 board*
school* N5 council*
school* N5 authorit*
school* N5 govern*
school* N5 board*
government* N5 agenc*
government* N5 plan*
government* N5 polic*
government* N5 strateg*
TX housing
(MH ”Public Housing”)
(MH “Residence Characteristics”)
(MH “Housing for the Elderly”)
(MH ”Home Health Agencies”)
(MH "Residential Facilities+/AM/MA/MT")
(MH “Residential Facilities”)
shelter* N5 hous*
shelter* N5 home*
shelter* N5 accommodat*
half‐way N5 hous*
half‐way N5 home*
halfway N5 hous*
halfway N5 home*
group home*
residential N5 facilit*
nurs* N5 facilit*
residential N5 home care
nurs* N5 home care
(MH “Nursing Homes+”)
TX nurs* home*
foster N4 home*
care N4 home*
supported living
(MH “Homeless Persons”)
homeless*
(MH “Social Work+”)
(MH “Economic and Social Security”)
(MH “Social Welfare+”)
social* N4 work*
social* N4 support*
social* N4 security
social* N4 care*
social* N4 welfare*
social* N4 service*
social* N4 network*
(MH “Consumer Advocacy”)
(MH “Counseling”)
(MH “Civil Rights”)
welfare rights
domestic care
day service
(MH "Alcoholism/RH")
(MH "Alcohol Drinking/PC”)
(MH "Social Behavior Disorders/NU/PC/RH")
(MH "Juvenile Delinquency/PC/RH")
youth offending team*
young N2 offender*
juvenile N2 offender*
youth N4 service*
leisure N2 centre
community N2 centre
youth N2 centre
recreation* N2 centre
leisure N2 center
community N2 center
youth N2 center
recreation* N2 center
play ground* or playground* or school yard* or schoolyard*
TX parks and recreation*
housing N2 regeneration
neighbourhood N2 regeneration
neighbourhood N3 renew*
neighbourhood N3 improv*
neighborhood N3 improv*
neighborhood N3 revitali?ation
TX social planning
TX built environment* or urban environment*
TX child* N3 violen*
TX domestic* N3 violen*
TX partner* N3 violen*
TX spousal N3 violen*
TX child* N3 abuse*
TX domestic* N3 abuse*
TX partner* N3 abuse*
TX spousal N3 abuse*
TX child* N3 protect*
TX domestic* N3 protect*
TX partner* N3 protect*
TX spousal N3 protect*
(MH “Foster Home Care”)
home adaptation*
local N2 hous*
play* field*
school* N2 infant*
school* N2 junior*
kindergarten
school* N2 senior*
school* N2 primary
school* N2 comprehensive
school* N2 grammar
school* N2 high
school* N2 elementary
school* N2 secondary
sixth form college*
educational psychologist*
occupational psychologist*
environmental health N5 worker*
occupational health N5 worker*
housing N5 worker*
youth N5 worker*
occupational health N5 officer*
housing N5 officer*
welfare rights N5 officer*
youth N5 officer*
environmental health N5 officer*
TX public librar*
school teacher*
or/1‐23 [collaboration]
or/24‐105 [health]
or/106‐248 [government]
and/249‐251
PT clinical trial
(MH “Experimental studies+”)
experiment*
time series
pre test or pretest or posttest or post test
(MH “Random Assignment”)
impact
intervention?
Chang*
(MH “Evaluation Research”)
Evaluat*
Effect?
TX comparative study
or/156‐169
170 and 155
limit 171 to yr="1966 ‐ 2008"
Database: Cochrane Central Register of Controlled Trials (CENTRAL)
#1 MeSH descriptor Interprofessional Relations explode all trees
#2 MeSH descriptor Cooperative Behavior, this term only
#3 MeSH descriptor Community‐Institutional Relations, this term only
#4 (partnership* or teamwork* or collaborat* or team work* or team‐work*.):ti,ab,kw
#5 (#1 OR #2 OR #3 OR #4), from 1960 to 2008
#6 MeSH descriptor Health, this term only
#7 MeSH descriptor Public Health explode all trees
#8 (family physician* or doctor* or nurse* or general practitioner* or GP or geriatrician):ti,ab,kw
#9 Geriatrics or aged or "Child health" "adolescent health" or "child welfare":ti,ab,kw
#10 (#6 OR #7 OR #8 OR #9), from 1960 to 2008
#11 (#5 AND #10), from 1960 to 2008
#12 MeSH descriptor Federal Government, this term only
#13 MeSH descriptor City Planning explode all trees
#14 MeSH descriptor Public Housing explode all trees
#15 MeSH descriptor Social Welfare, this term only
#16 MeSH descriptor Social Work, this term only
#17 MeSH descriptor Residence Characteristics explode all trees
#18 MeSH descriptor Geriatrics explode all trees
#19 MeSH descriptor Child Care explode all trees
#20 MeSH descriptor Occupational Health explode all trees
#21 MeSH descriptor Respite Care explode all trees
#22 MeSH descriptor Nursing Homes explode all trees
#23 (city authorities):ti,ab,kw
#24 (#12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #20 OR #21 OR #22 OR #23), from 1960 to 2008
#25 (#11 AND #24)
#26 (#5 AND #10 AND #24)
Database: Cochrane Database of Systematic Reviews (CDSR)
#1 collaboration or team work or mutidiciplinary in Cochrane Reviews
#2 partnership* or teamwork* or team‐work* OR multi‐professional in Cochrane Reviews
#3 Interprofessional Relations in Cochrane Reviews
#4 Cooperative Behavior in Cochrane Reviews
#5 Community‐Institutional Relations in Cochrane Reviews
#6 (#1 OR #2 OR #3 OR #4 OR #5), from 1966 to 2008
#7 Health in Cochrane Reviews
#8 Federal Government OR local government
#9 Government agenc*
#10 Public Housing or city planning
#11 Residence Characteristics
#12 (#8 OR #9 OR #10 OR #11)
#13 (#6 AND #7 AND #12)
Database: Dissertation and Theses and Index to Theses database
Collaboration or partnership or teamwork AND Health AND local government or local council or local authority or municipal counci or municipal authority or government agency
Database: DoPHER (Database of Promoting Health Effectiveness Reviews)
| 385 | Freetext (item record) collaboration |
| 386 | Freetext (item record) "cooperative behavior" |
| 387 | Freetext (item record) "cooperative behaviour" |
| 388 | Freetext (item record) cooperative |
| 389 | Freetext (item record) co‐operative |
| 390 | Freetext (item record) relations |
| 391 | Freetext (item record) "community‐institutional " |
| 392 | Freetext (item record) community |
| 393 | Freetext (item record) community |
| 394 | Freetext (item record) institutional |
| 395 | 393 AND 394 |
| 396 | Freetext (item record) interdepartmental |
| 397 | Freetext (item record) "Interprofessional " |
| 398 | Freetext (item record) Interdisciplinary |
| 399 | 385 OR 388 OR 389 OR 390 OR 395 OR 396 OR 397 OR 398 |
Database: EMBASE
1. Public Relations/
2. inter?institutional relation:.mp.
3. Interprofessional relations.mp.
4. interdepartmental: relation:.mp. or inter‐departmental: relation:.tw.
5. interprofessional: relation:.mp. or inter‐professional: relation:.tw.
6. Cooperation/
7. (cooperative: behavior: or co‐ooperative: behavior: or cooperative: behaviour: or co‐operative: behaviour: or cooperative: plan:).mp. or co‐operative: plan:.tw.
8. collaborat:.mp.
9. (cross‐system: or cross system: or cross disciplin: or cross‐disciplin:).tw.
10. interagenc:.mp. or inter‐agenc:.tw.
11. interdisciplin:.mp. or inter‐disciplin:.tw.
12. intersector:.mp. or inter‐sector:.tw.
13. (transdisciplin: or trans‐disciplin:).mp.
14. (integrat: adj5 (work: or profession: or partnership: or team: or teamwork: or disciplin: or agenc:)).tw.
15. (welfare right: adj7 health:).tw.
16. (partner agenc$ or partner department$).tw.
17. ((behave or behaving or behaves or behaved) adj cooperative$).tw.
18. (cooperativ$ adj2 (work$ or behavio?r or agenc$)).tw.
19. (partnership adj3 (work$ or cooperat$ or plan$ or relations or behavio?r or agenc$)).tw.
20. (interdepartmental adj2 (work$ or cooperat$ or behavio?r)).tw.
21. (interprofessional adj2 (work$ or cooperat$ or behavio?r or agenc$)).tw.
22. (cross sector$ or cross?sector$ or across sector$).tw.
23. (multi department$ or multidepartment$).tw.
24. ((working or work or works or worked) adj together).tw.
25. Interdisciplinary communication/
26. jointness:.tw.
27. (work: adj5 (joint: commission: or joint‐commission: or joint: plan: or joint‐plan: or joint: work: or joint‐work: or joined up: or joined‐up)).mp.
28. (work: adj5 (multiagenc: or multi‐agenc: or multidisciplin: or multi‐disciplin: or multiprofessional: or multi‐professional: or multi‐sector: or multisector:)).tw.
29. (work: adj5 (partnership: or teamwork: or team work: or team‐work:)).tw.
30. or/1‐29
31. Public Health/
32. public health administration.mp. or Public Health Service/
33. Health Care Planning/
34. Health Care Delivery/
35. Home Care/
36. Health Promotion/
37. Health Service/
38. Community Care/
39. Health Center/
40. community care.mp. or continuing care.tw. or long term care.tw. or longterm care.tw. or long‐term care.tw.
41. Health Education/
42. exp Primary Health Care/
43. comprehensive health care/
44. General Practitioner/
45. Emergency Health Service/
46. Preventive Health Service/
47. Nursing/
48. nursing services.mp.
49. Community Health Nursing/
50. rehabilitation nursing.mp. or Rehabilitation Nursing/
51. community health nurs:.mp.
52. Elderly Care/
53. Rural Health Care/
54. health services, indigenous.mp. or Health Service/
55. Mental Health Service/
56. Community Mental Health Center/
57. community mental health team.mp.
58. Crisis Intervention/
59. Psychotherapy/
60. exp Child Health Care/
61. exp Child Care/
62. exp Child Welfare/
63. Child Health/
64. Oral Health.mp. or Health/
65. Aged/
66. Geriatrics/
67. palliative care.mp. or Palliative Therapy/
68. Terminal Care/
69. Long Term Care/
70. Primary Prevention/
71. Rehabilitation/
72. Occupational Therapy/
73. Communicable Disease/
74. ((outbreak: or infection:) adj control:).tw.
75. Preventive Health Service/
76. Mass Screening/
77. Rehabilitation Center/
78. Nursing Home/
79. hospice care/
80. day care/
81. Respite Care/
82. *Addiction/rh [Rehabilitation]
83. (mass media adj5 (health: or campaign: or scheme: or program: or project: or intervention: or strateg:)).tw.
84. health promot: school:.tw.
85. (health adj5 (promot: or scheme: or program: or project: or strateg: or scheme: or intervention:)).tw.
86. (speech and language therapist:).mp.
87. (family physician: or doctor: or nurse: or general practitioner: or GP or geriatrician: or health visitor: or dietician: or dietitian: or nutritionist: or physiotherapist: or occupational therapist: or therapist: or midwife).mp. or midwives.tw.
88. dietitian:.tw.
89. (community adj2 (program: or scheme: or project: or intervention: or strateg:)).tw.
90. *Postnatal Care/
91. *Prenatal Care/
92. geriatric evaluation.mp. and management.tw.
93. or/31‐92
94. government agencies.mp. or Government/
95. local government.mp. or Government/
96. ((municipal: or city or town: or local: or education: or school:) adj5 (council: or authorit: or govern: or board:)).tw.
97. (government: adj5 (agenc: or plan: or polic: or strateg:)).tw.
98. housing.mp.
99. Housing/
100. public housing.mp.
101. Demography/
102. Home for the Aged/
103. Home Care/
104. Residential Home/
105. ((shelter: or half‐way or half way) adj5 (hous: or home: or accommodat:)).tw.
106. group home:.tw.
107. ((residential or nurs:) adj5 (home care or facilit:)).tw.
108. nurs: home:.mp.
109. ((foster or care) adj4 home:).tw.
110. supported living.tw.
111. Homelessness/
112. exp Social Work/
113. exp Social Security/
114. exp Social Welfare/
115. (social: adj4 (work: or support: or security or care: or welfare: or service: or network:)).tw.
116. Consumer Advocacy/
117. Consumer Advocacy/
118. Counseling/
119. Civil Rights/
120. welfare rights.tw.
121. domestic care.tw.
122. day service:.tw.
123. Substance‐Related Disorders.mp.
124. *Alcoholism/rh [Rehabilitation]
125. *Drinking Behavior/pc [Prevention]
126. Alcohol Drinking.mp.
127. Social Behavior Disorders.mp. or Sociopathy/
128. Juvenile Delinquency/pc, rh [Prevention, Rehabilitation]
129. youth offending team:.tw.
130. ((young or juvenile) adj2 offender:).tw.
131. (youth adj4 service:).tw.
132. ((leisure or community or youth or recreation:) adj2 (center: or centre:)).tw.
133. (play ground: or playground: or school yard: or schoolyard:).tw.
134. parks.mp. and recreation:.tw.
135. ((housing or neighbourhood or neighborhood) adj2 regeneration).tw.
136. ((neighbourhood or neighborhood) adj3 (renew: or improv: or revitali?ation)).tw.
137. social planning.mp.
138. built environment:.mp. or urban environment:.tw.
139. ((child: or domestic: or partner: or spousal) adj3 (abuse: or violen: or protect:)).mp.
140. Foster Care/
141. Disabled Person/
142. home adaptation:.tw.
143. (local adj2 (council: or hous:)).tw.
144. play: field:.tw.
145. (school: adj2 (infant: or junior: or kindergarten or senior: or primary or comprehensive or grammar or high or elementary or secondary)).tw.
146. sixth form college:.tw.
147. educational psychologist:.tw.
148. occupational psychologist:.tw.
149. ((environmental health or occupational health or housing or welfare rights or youth) adj5 (worker: or officer:)).tw.
150. public librar:.mp. or school teacher:.tw.
151. (environment agenc: or transport agencies or transport departments or transport sector or housing agency).mp. or education department.tw.
152. or/94‐151
153. 30 and 93 and 152
154. Randomized Controlled Trial/
155. Controlled Clinical Trial/
156. Intervention Study/
157. experiment$.tw.
158. (time adj series).tw.
159. (pre test or pretest or (posttest or post test)).tw.
160. Randomization/
161. impact.tw.
162. intervention?.tw.
163. chang$.tw.
164. Evaluation/
165. evaluat$.tw.
166. effect?.tw.
167. comparative study.pt.
168. Comparative Study/
169. or/154‐168
170. 153 and 169
Database: ERIC (Education Resources Information Center)
Query: ((KW=(random* or ("controlled trial") or ("intervention stud*")) or
KW=(experiment* or ("comparative stud*") or impact)) or(time NEAR series)
or(pretest or posttest) or(randomised control trial) or(randomized
control trial) or(DE=("comparative analysis" or "evaluation methods" or
"intervention" or "longitudinal studies")) or(clinical trial)
or(DE=("control groups" or "experimental groups" or "quasiexperimental
design" or "comparative analysis" or "evaluation methods" or
"intervention" or "longitudinal studies"))) and(((DE=("cooperation" or
"interaction" or "interdisciplinary approach" or "interprofessional
relationship" or "participation" or "teamwork")) or(AB=(collaborat* or
interagenc* or multiagenc*) or (inter‐institutional* or
inter‐professional or inter‐departmental*) or (interinstitutional* or
interprofessional or interdepartmental*))) and((DE=("immunization
programs" or "child health" or "communicable diseases" or "community
health services" or "disease control" or "epidemiology" or "internal
medicine" or "preventive medicine" or "access to health care" or "aging
individuals" or "child care" or "community services" or "dental health"
or "dentistry" or "educational gerontology" or "geriatrics" or
"gerontology" or "health" or "health activities" or "health personnel" or
"health related fitness" or "health services" or "hygiene" or "medicine"
or "mental disorders" or "mental health" or "mental health workers" or
"nursing" or "older adults" or "physical health" or "psychotherapy" or
"public health" or "rehabilitation" or "rehabilitation counseling" or
"well being" or "wellness")) or(AB=(("family physician*") or doctor* or
(general practitioner*)) or AB=(nurs* or ("School nurs*") or
geriatrician*) or AB=((occupational therapist*) or physiotherapist* or
nutritionist*) or AB=(dietitian* or dietician* or ("health visitor*")) or
AB=(therapist* or midwives or midwife) or AB=(("occupational therapist*")
or physiotherapist* or ("respite care")))) and((DE=("leisure education"
or "recreational activities" or "recreational facilities" or
"recreational programs" or "addictive behavior" or "alcoholism" or
"ancillary school services" or "boarding schools" or "child care" or
"child welfare" or "city government" or "community" or "community
services" or "delinquency" or "disabilities" or "educational counseling"
or "educational psychology" or "emergency shelters" or "facilities" or
"foster care" or "government administrative body" or "government
employees" or "group homes" or "housing" or "human services" or
"institutions" or "municipalities" or "nursing homes" or "planning
commissions" or "public agencies" or "regional planning" or
"rehabilitation centers" or "residential institutions" or "residential
programs" or "school districts" or "school psychology" or "social
planning" or "social psychology" or "social services" or "social welfare"
or "social work" or "urban planning" or "welfare services")) or(AB=(("play
ground*") or playground* or schoolyard*) or AB=(("school yard*") or parks
or ("built environment*")))))
Database: HMIC (Health Management Information Consortium)
1. PUBLIC RELATIONS/
2. INTERPROFESSIONAL RELATIONS/
3. interdepartmental relations/
4. interdepartmental: relation:.mp. or inter‐departmental: relation:.tw.
5. interprofessional: relation:.mp. or inter‐professional: relation:.tw.
6. INTERAGENCY RELATIONS/
7. (cooperative: behavior: or co‐ooperative: behavior: or cooperative: behaviour: or co‐operative: behaviour: or cooperative: plan:).mp. or co‐operative: plan:.tw.
8. collaborat:.mp.
9. INTERAGENCY COLLABORATION/
10. (cross‐system: or cross system: or cross disciplin:).mp. or cross‐disciplin:.tw.
11. interagenc:.mp. or inter‐agenc:.tw.
12. interdisciplin:.mp. or inter‐disciplin:.tw.
13. intersector:.mp. or inter‐sector:.tw.
14. (joint: commission: or joint‐commission: or joint: plan: or joint‐plan: or joint: work: or joint‐work: or joined up: or joined‐up).mp. or jointness:.tw.
15. MULTIDISCIPLINARY TEAMS/
16. MULTIDISCIPLINARY SERVICES/
17. (multiagenc: or multi‐agenc: or multidisciplin: or multi‐disciplin: or multiprofessional: or multi‐professional: or multi‐sector:).mp. or multisector:.tw.
18. TEAMWORK/
19. (partnership: or teamwork: or team work:).mp. or team‐work:.tw.
20. (transdisciplin: or trans‐disciplin:).mp.
21. (integrat: adj5 (work: or profession: or partnership: or team: or teamwork: or disciplin: or agenc:)).tw.
22. (welfare right: adj7 health:).tw.
23. WELFARE RIGHTS/ and health.tw.
24. PUBLIC HEALTH/
25. public health administration.mp.
26. exp HEALTH PLANNING/
27. community health planning.mp.
28. ACCESS TO HEALTH SERVICES/
29. (health services accessibility or access to health care).mp. [mp=title, other title, abstract, heading words]
30. home care services.mp. or exp HOME CARE/
31. (health services needs and demand).mp. [mp=title, other title, abstract, heading words]
32. HEALTH PLANNING/
33. exp HEALTH PROMOTION/
34. HEALTH SERVICES/
35. delivery of health care.mp.
36. COMMUNITY HEALTH SERVICES/
37. (community health centers or community health centres).mp. [mp=title, other title, abstract, heading words]
38. community care.mp. or continuing care.tw. or long term care.tw. or longterm care.tw. or long‐term care.tw.
39. COMMUNITY CARE/
40. exp HEALTH EDUCATION/
41. exp PRIMARY CARE/
42. comprehensive health care.mp.
43. family physicians.mp.
44. emergency medical services.mp. or EMERGENCY HEALTH SERVICES/
45. PREVENTIVE MEDICINE/ or preventive health services.mp.
46. exp PREVENTIVE MEDICINE/
47. nursing services.mp.
48. exp NURSING/
49. (public health and nursing).mp. [mp=title, other title, abstract, heading words]
50. (rehabilitation and nursing).mp. [mp=title, other title, abstract, heading words]
51. COMMUNITY NURSING/
52. COMMUNITY PSYCHIATRIC NURSING/
53. (health services for the aged or health services for the elderly).mp.
54. RURAL HEALTH SERVICES/
55. (indigenous and health services).mp. [mp=title, other title, abstract, heading words]
56. exp MENTAL HEALTH SERVICES/
57. COMMUNITY MENTAL HEALTH SERVICES/
58. exp COMMUNITY MENTAL HEALTH CENTRES/
59. exp CASE MANAGEMENT/
60. COMMUNITY MENTAL HEALTH TEAMS/
61. CRISIS INTERVENTION/
62. PSYCHOTHERAPY/
63. exp YOUNG PEOPLES HEALTH SERVICES/ or adolescent health services.mp.
64. exp CHILD CARE/
65. exp CHILD WELFARE/
66. exp CHILDRENS HEALTH SERVICES/
67. ORAL HEALTH/
68. exp ELDERLY PEOPLE/ or exp MIDDLE AGED PEOPLE/ or aged.mp.
69. exp GERIATRICS/
70. exp PSYCHO GERIATRICS/
71. exp PALLIATIVE CARE/
72. exp TERMINAL CARE/
73. exp LONG TERM CARE/
74. primary prevention.mp.
75. exp SERVICE DELIVERY/
76. exp REHABILITATION/
77. REHABILITATION/
78. OCCUPATIONAL THERAPY/
79. exp COMMUNICABLE DISEASES/
80. ((outbreak: or infection:) adj control:).tw.
81. immunization programs.mp. or exp IMMUNISATION/
82. MASS SCREENING/
83. exp REHABILITATION CENTRES/
84. exp NURSING HOMES/
85. nursing hom:.tw.
86. HOSPICE CARE/
87. DAY CARE/
88. RESPITE CARE/
89. (exp DRUG ABUSE/ or substance related disorders.mp.) and rehabilitation.mp. [mp=title, other title, abstract, heading words]
90. (mass media adj5 (health: or campaign: or scheme: or program: or project: or intervention: or strateg:)).tw.
91. health promot: school:.tw.
92. (health adj5 (promot: or scheme: or program: or project: or strateg: or scheme: or intervention:)).tw.
93. school nurs:.mp.
94. (speech and language therapist:).mp.
95. (family physician: or doctor: or nurse: or general practitioner: or GP or geriatrician: or health visitor: or dietician: or dietitian: or nutritionist: or physiotherapist: or occupational therapist: or therapist: or midwife).mp. or midwives.tw.
96. (dietitian: or dietician).tw.
97. (community adj2 (program: or scheme: or project: or intervention: or strateg:)).tw.
98. ANTENATAL CARE/ or prenatal care.mp.
99. exp POST NATAL CARE/ or postnatal care.mp.
100. (geriatric evaluation or geriatric assessment).mp. [mp=title, other title, abstract, heading words]
101. government agencies.mp.
102. LOCAL GOVERNMENT/
103. ((municipal: or city or town: or local: or education: or school:) adj5 (council: or authorit: or govern: or board:)).tw.
104. (government: adj5 (agenc: or plan: or polic: or strateg:)).tw.
105. HOUSING/ or housing.mp.
106. PUBLIC HOUSING/ or SOCIAL HOUSING/ or COMMUNITY HOUSING/ or HOUSING/ or LOCAL AUTHORITY HOUSING/
107. neighbourhood characteristics.mp.
108. housing for the elderly.mp.
109. home care agencies.mp.
110. homes for the aged.mp.
111. residential facilities.mp. or RESIDENTIAL CARE/
112. SHELTERED HOUSING/ or EXTRA CARE HOUSING/ or VERY SHELTERED HOUSING/ or WARDEN SERVICED HOUSING/
113. ((shelter: or half‐way or half way) adj5 (hous: or home: or accommodat:)).tw.
114. group home:.tw.
115. ((residential or nurs:) adj5 (home care or facilit:)).tw.
116. exp NURSING HOMES/
117. nurs: hom:.mp.
118. ((foster or care) adj4 home:).tw.
119. supported living.tw.
120. homeless:.tw.
121. exp HOMELESSNESS/
122. exp SOCIAL WORK/
123. exp SOCIAL SECURITY/
124. exp SOCIAL WELFARE/
125. (social: adj4 (work: or support: or security or care: or welfare: or service: or network:)).tw.
126. exp "PATIENT ADVOCACY AND LIAISON SERVICE"/
127. consumer advocacy.mp.
128. exp COUNSELLING/ or counseling.mp.
129. "CIVIL AND POLITICAL RIGHTS"/
130. WELFARE RIGHTS/
131. domestic care.tw.
132. day service.tw.
133. (exp DRUG ABUSE/ or substance related disorders.mp.) and rehabilitation.mp. [mp=title, other title, abstract, heading words]
134. (ALCOHOLISM/ or ALCOHOLISM TREATMENT/) and rehabilitation.mp. [mp=title, other title, abstract, heading words]
135. (ALCOHOL CONSUMPTION/ or alcohol drinking.mp.) and (prevention and control).mp. [mp=title, other title, abstract, heading words]
136. (BEHAVIOUR DISORDERS/ or social behaviour disorders.mp.) and (nursing or rehabilitation).mp. [mp=title, other title, abstract, heading words]
137. exp JUVENILE DELINQUENCY/
138. youth offending team:.tw.
139. ((young or juvenile) adj2 offender:).tw.
140. (youth adj4 service:).tw.
141. YOUTH SERVICES/
142. ((leisure or community or youth or recreation:) adj2 (center: or centre:)).tw.
143. (play ground: or playground: or school yard: or schoolyard:).tw.
144. (PARKS/ or parks.mp.) and (LEISURE/ or recreation.mp.)
145. ((housing or neighbourhood or neighborhood) adj2 regeneration).tw.
146. ((neighbourhood or neighborhood) adj3 (renew: or improv: or revitali?ation)).tw.
147. URBAN RENEWAL/ or exp URBAN REGENERATION/
148. exp SOCIAL PLANNING/
149. BUILT ENVIRONMENT/ or URBAN ENVIRONMENT/
150. built environment:.mp. or urban environment:.tw.
151. ((child: or domestic: or partner: or spousal) adj3 (abuse: or violen: or protect:)).mp.
152. exp FOSTER CARE/ or foster home.mp.
153. (disabled and rehabilitation).mp. [mp=title, other title, abstract, heading words]
154. exp BUILDING CONVERSION/ or home adaptation.mp.
155. (local adj2 (council: or hous:)).tw.
156. exp SPORTS GROUNDS/ or play: field:.tw.
157. (school: adj2 (infant: or junior: or kindergarten or senior: or primary or comprehensive or grammar or high or elementary or secondary)).tw.
158. sixth form college:.tw.
159. EDUCATIONAL PSYCHOLOGISTS/ or educational psychologist:.tw.
160. occupational psychologist:.tw.
161. ((environmental health or occupational health or housing or welfare rights or youth) adj5 (worker: or officer:)).tw.
162. public librar:.mp. or school teacher:.tw.
163. or/1‐21
164. or/22‐100
165. or/101‐162
166. and/163‐165
167. exp RANDOMISED CONTROLLED TRIALS/
168. controlled clinical trial.mp.
169. intervention studies.mp.
170. experiment:.tw.
171. (time adj series).tw.
172. (pre test or pretest or (posttest or post test)).tw.
173. random allocation.tw.
174. impact.tw.
175. intervention:.tw.
176. chang:.tw.
177. evaluation studies.mp.
178. evaluat:.tw.
179. effect:.tw.
180. exp COMPARATIVE STUDIES/
181. or/167‐180
182. 166 and 181
183. limit 182 to yr="1966 ‐ 2008"
Database: International Bibliography of the Social Sciences (IBSS)
| S161 | S63 and S139 and S160 |
| S160 | S140 or S141 or S142 or S143 or S144 or S145 or S146 or S147 or S148 or S149 or S150 or S151 or S152 or S153 or S154 or S155 or S156 or S157 or S158 or S159 |
| S159 | TX collaborati* |
| S158 | Cooperative Behaviour |
| S157 | Interprofessional Relations |
| S156 | integrat* N5 agenc* |
| S155 | integrat* N5 disciplin* |
| S154 | integrat* N5 team* |
| S153 | integrat* N5 teamwork* |
| S152 | integrat* N5 partnership* |
| S151 | integrat* N5 profession* |
| S150 | integrat* N5 work* |
| S149 | TX partnership* or TX teamwork* or TX team work* or team‐work* |
| S148 | TX multiagenc* or TX multi‐agenc* or TX multidisciplin* or TX multi‐disciplin* or TX multiprofessional* or TX multi‐professional* or TX multi‐sector* or multisector* |
| S147 | TX joint* commission* or TX joint‐commission* or TX joint* plan* or TX joint‐plan* or TX joint* work* or TX joint‐work* or TX joined up* or TX joined‐up or jointness* |
| S146 | TX intersector* or inter‐sector* |
| S145 | TX interdisciplin* or inter‐disciplin* |
| S144 | TX interagenc* or inter‐agenc* |
| S143 | TX cross‐system* or TX cross system* or TX cross disciplin* or cross‐disciplin* |
| S142 | TX cooperative* behavior* or TX cooperative* behaviour* or TX cooperative* plan* |
| S141 | TX interprofessional* relation* or inter‐professional* relation* |
| S140 | TX interdepartmental* relation* or inter‐departmental* relation* |
| S139 | S64 or S65 or S66 or S67 or S68 or S69 or S70 or S71 or S72 or S73 or S74 or S75 or S76 or S77 or S78 or S79 or S80 or S81 or S82 or S83 or S84 or S85 or S86 or S87 or S88 or S89 or S90 or S91 or S92 or S93 or S94 or S95 or S96 or S97 or S98 or S99 or S100 or S101 or S102 or S103 or S104 or S105 or S106 or S107 or S108 or S109 or S110 or S111 or S112 or S113 or S114 or S115 or S116 or S117 or S118 or S119 or S120 or S121 or S122 or S123 or S124 or S125 or S126 or S127 or S128 or S129 or S130 or S131 or S132 or S133 or S134 or S135 or S136 or S137 or S138S64 or S65 or S66 or S67 or S68 or S69 or S70 or S71 or S72 or S73 or S74 or S75 or S76 or S77 or S78 or S79 or S80 or S81 or S82 or S83 or S84 or S85 or S86 or S87 or S88 or S89 or S90 or S91 or S92 or S93 or S94 or S95 or S96 or S97 or S98 or S99 or S100 or S101 or S102 or S103 or S104 or S105 or S106 or S107 or S108 or S109 or S110 or S111 or S112 or S113 or S114 or S115 or S116 or S117 or S118 or S119 or S120 or S121 or S122 or S123 or S124 or S125 or S126 or S127 or S128 or S129 or S130 or ...Show Less |
| S138 | housing association* |
| S137 | (Public or council) and housing |
| S136 | sheltered and (housing or living or accommodation) |
| S135 | Residential Facilit* |
| S134 | Social Security |
| S133 | Consumer Advocacy |
| S132 | Counseling or counselling |
| S131 | civil rights |
| S130 | alcoholism |
| S129 | Alcohol Drinking |
| S128 | (Juvenile or youth) and (delinquency or offending) |
| S127 | (sixth form or tertiary) and college |
| S126 | welfare N5 officer* |
| S125 | school teacher* |
| S124 | TX public librar* |
| S123 | environmental health N5 officer* |
| S122 | youth N5 officer* |
| S121 | housing N5 officer* |
| S120 | youth N5 worker* |
| S119 | housing N5 worker* |
| S118 | occupational health N5 worker* |
| S117 | educational psychologist* |
| S116 | school* N2 secondary |
| S115 | school* N2 high |
| S114 | school* N2 comprehensive |
| S113 | school* N2 senior* |
| S112 | school* N2 junior* |
| S111 | play* field* |
| S110 | home adaptation* |
| S109 | TX spousal N3 protect* |
| S108 | TX domestic* N3 protect* |
| S107 | TX spousal N3 abuse* |
| S106 | TX domestic* N3 abuse* |
| S105 | TX spousal N3 violen* |
| S104 | TX domestic* N3 violen* |
| S103 | TX built environment* or urban environment* |
| S102 | neighborhood N3 revitali?ation |
| S101 | neighbourhood N3 improv* |
| S100 | neighbourhood N2 regeneration |
| S99 | TX parks and recreation* |
| S98 | recreation* N2 center |
| S97 | community N2 center |
| S96 | recreation* N2 centre |
| S95 | community N2 centre |
| S94 | youth N4 service* |
| S93 | young N2 offender* |
| S92 | day service |
| S91 | welfare rights |
| S90 | social* N4 network* |
| S89 | social* N4 welfare* |
| S88 | social* N4 security |
| S87 | social* N4 work* |
| S86 | homeless* |
| S85 | supported living |
| S84 | foster N4 home* |
| S83 | residential N5 home care |
| S82 | residential N5 facilit* |
| S81 | halfway N5 hous* |
| S80 | half‐way N5 home* |
| S79 | shelter* N5 accommodat* |
| S78 | shelter* N5 hous* |
| S77 | government* N5 strateg* |
| S76 | government* N5 plan* |
| S75 | school* N5 board* |
| S74 | school* N5 authorit* |
| S73 | education* N5 board* |
| S72 | education* N5 authorit* |
| S71 | local* N5 board* |
| S70 | local* N5 authorit* |
| S69 | town* N5 board* |
| S68 | town* N5 authorit* |
| S67 | city* N5 board* |
| S66 | city* N5 authorit* |
| S65 | municipal* N5 board* |
| S64 | municipal* N5 authorit* |
| S63 | S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38 or S39 or S40 or S41 or S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 or S53 or S54 or S55 or S56 or S57 or S58 or S59 or S60 or S61 or S62 |
| S62 | service* accessib* |
| S61 | home care |
| S60 | health promotion |
| S59 | health service* |
| S58 | Primary healthcare |
| S57 | Primary health care |
| S56 | "health and welfare" |
| S55 | community and (centre* or center*) |
| S54 | Community health service* |
| S53 | mental health service* |
| S52 | mental health service* |
| S51 | emergency medical service* |
| S50 | nursing administration |
| S49 | health service* and (elderly or aged) |
| S48 | case management |
| S47 | crisis intervention* |
| S46 | psychotherapy |
| S45 | (Adolescent or youth) and health service* |
| S44 | child and (health service* or welfare or care) |
| S43 | oral health |
| S42 | geriatrics or gerontology |
| S41 | (health care or healthcare) and delivery |
| S40 | health manpower |
| S39 | occupational therapy |
| S38 | (communicable or infectious) and disease |
| S37 | Immuni?ation program* |
| S36 | health screening |
| S35 | rehabilitation |
| S34 | (hospice or palliative or terminal) and care |
| S33 | day care |
| S32 | respite care |
| S31 | alcohol and (use or abuse or misuse) |
| S30 | drug and (use or abuse or misuse) |
| S29 | substance and (use or abuse or misuse) |
| S28 | (postnatal or prenatal or antenatal) and care |
| S27 | welfare right* N7 health |
| S26 | community N2 strateg* |
| S25 | community N2 intervention* |
| S24 | community N2 project* |
| S23 | community N2 scheme* |
| S22 | community N2 program* |
| S21 | TX family physician* or TX doctor* or TX nurse* or TX general practitioner* or TX GP or TX geriatrician* or TX health visitor* or TX dietician* or TX dietitian* or TX nutritionist* or TX physiotherapist* or TX occupational therapist* or TX therapist* or TX midwife or midwives |
| S20 | TX "speech and language therapist*" or TX speech therapist* |
| S19 | health N5 intervention* |
| S18 | health N5 scheme* |
| S17 | health N5 strateg* |
| S16 | health N5 project* |
| S15 | health N5 program* |
| S14 | health N5 promot* |
| S13 | health promot* school* |
| S12 | mass media N5 strateg* |
| S11 | mass media N5 intervention* |
| S10 | mass media N5 project* |
| S9 | mass media N5 program* |
| S8 | mass media N5 campaign* |
| S7 | mass media N5 health* |
| S6 | nursing home* |
| S5 | control and (outbreak* or infection*) |
| S4 | community mental health team* |
| S3 | TX community mental health cent* |
| S2 | TX community health nurs* |
| S1 | TX community care or continuing care or long term care or longterm care or long‐term care |
Database: ISI Science Citation Index
| #21 | #20 AND #14 |
| #20 | #19 OR #18 OR #17 OR #16 OR #15 |
| #19 | Topic=("pre test" or pretest or posttest or "post test") |
| #18 | TS=randomised controlled trial OR TS=randomized controlled trial OR TS=controlled clinical trial |
| #17 | TS=intervention stud* OR TS= Evaluation OR TS=time series |
| #16 | TS=randomized controlled study OR TS= "random allocation" OR TS=cross‐sectional |
| #15 | TS= clinical trial* OR TS=research design OR TS=comparative stud* OR TS=evaluation stud* OR TS=controlled trial* OR TS=follow‐up stud* OR TS= cohort OR TS=prospective stud* OR TS=random* OR TS=placebo* OR TS=(single blind*) OR TS=(double blind*) |
| #14 | #13 AND #9 AND #4 |
| #13 | #12 OR #11 OR #10 |
| #12 | TS="rental housing" OR TS="residential institutions" OR TS=metropolitan councils OR TS=district councils OR TS=public housing OR TS=home care agencies |
| #11 | TS=federal government OR TS=municipal government OR TS=goverment agencies OR TS=local authorit* |
| #10 | TS=central government OR TS=city planning OR TS=community services OR TS=councils |
| #9 | #8 OR #7 OR #6 OR #5 |
| #8 | TS=public health OR TS=Mental Health OR TS= health OR TS=occupational therapy OR TS=health promotion OR TS=injury prevention |
| #7 | TS="nursing service*" OR TS="public health nursing" OR TS= rehabilitation OR TS="community health nurs*" OR TS="adolescent health" OR TS=" child health" OR TS="child care" OR TS= "child welfare" OR TS=geriatric |
| #6 | TS=health promotion OR TS="health planning" OR TS="Delivery of Health Care" OR TS=health service OR TS= Community Health OR TS=rural health OR TS=mental health" OR TS=oral health" OR TS=preventive health |
| #5 | TS=family physician* OR TS=doctor* OR TS=nurse* OR TS=general practitioner* OR TS=GP OR TS=geriatrician* OR TS= health visitor* OR TS=dietician* OR TS=dietitian* OR TS=nutritionist* OR TS=physiotherapist* OR TS=occupational therapist* OR TS=therapist* OR TS=midwife OR TS=midwives |
| #4 | #3 OR #2 OR #1 |
| #3 | TS=integrat* OR TS= partnership* OR TS= team* OR TS=teamwork* OR TS=participat* OR TS= collaboration |
| #2 | TS=collaborat* OR TS=multiagenc* OR TS=multi‐agenc* OR TS= multidisciplin* OR TS=multi‐disciplin* OR TS=multiprofessional* OR TS=multi‐professional* OR TS=multi‐sector* |
| #1 | TS=interinstitutional relation* OR TS= cooperative behavior OR TS= interprofessional relation* OR TS= community‐institutional relations |
Database: ISI Social Sciences Citation Index
| #21 | #20 AND #14 |
| #20 | #19 OR #18 OR #17 OR #16 OR #15 |
| #19 | Topic=("pre test" or pretest or posttest or "post test") |
| #18 | TS=randomised controlled trial OR TS=randomized controlled trial OR TS=controlled clinical trial |
| #17 | TS=intervention stud* OR TS= Evaluation OR TS=time series |
| #16 | TS=randomized controlled study OR TS= "random allocation" OR TS=cross‐sectional |
| #15 | TS= clinical trial* OR TS=research design OR TS=comparative stud* OR TS=evaluation stud* OR TS=controlled trial* OR TS=follow‐up stud* OR TS= cohort OR TS=prospective stud* OR TS=random* OR TS=placebo* OR TS=(single blind*) OR TS=(double blind*) |
| #14 | #13 AND #9 AND #4 |
| #13 | #12 OR #11 OR #10 |
| #12 | TS="rental housing" OR TS="residential institutions" OR TS=metropolitan councils OR TS=district councils OR TS=public housing OR TS=home care agencies |
| #11 | TS=federal government OR TS=municipal government OR TS=goverment agencies OR TS=local authorit* |
| #10 | TS=central government OR TS=city planning OR TS=community services OR TS=councils |
| #9 | #8 OR #7 OR #6 OR #5 |
| #8 | TS=public health OR TS=Mental Health OR TS= health OR TS=occupational therapy OR TS=health promotion OR TS=injury prevention |
| #7 | TS="nursing service*" OR TS="public health nursing" OR TS= rehabilitation OR TS="community health nurs*" OR TS="adolescent health" OR TS=" child health" OR TS="child care" OR TS= "child welfare" OR TS=geriatric |
| #6 | TS=health promotion OR TS="health planning" OR TS="Delivery of Health Care" OR TS=health service OR TS= Community Health OR TS=rural health OR TS=mental health" OR TS=oral health" OR TS=preventive health |
| #5 | TS=family physician* OR TS=doctor* OR TS=nurse* OR TS=general practitioner* OR TS=GP OR TS=geriatrician* OR TS= health visitor* OR TS=dietician* OR TS=dietitian* OR TS=nutritionist* OR TS=physiotherapist* OR TS=occupational therapist* OR TS=therapist* OR TS=midwife OR TS=midwives |
| #4 | #3 OR #2 OR #1 |
| #3 | TS=integrat* OR TS= partnership* OR TS= team* OR TS=teamwork* OR TS=participat* OR TS= collaboration |
| #2 | TS=collaborat* OR TS=multiagenc* OR TS=multi‐agenc* OR TS= multidisciplin* OR TS=multi‐disciplin* OR TS=multiprofessional* OR TS=multi‐professional* OR TS=multi‐sector* |
| #1 | TS=interinstitutional relation* OR TS= cooperative behavior OR TS= interprofessional relation* OR TS= community‐institutional relations |
Database: Ovid MEDLINE®
1. inter?institutional relation:.mp.
2. exp Interprofessional relations/
3. interdepartmental relations/
4. interdepartmental: relation:.mp. or inter‐departmental: relation:.tw.
5. interprofessional: relation:.mp. or inter‐professional: relation:.tw.
6. community‐institutional relations/
7. exp cooperative behavior/
8. (cooperative: behavior: or co‐ooperative: behavior: or cooperative: behaviour: or co‐operative: behaviour: or cooperative: plan:).mp. or co‐operative: plan:.tw.
9. collaborat:.mp.
10. (cross‐system: or cross system: or cross disciplin:).mp. or cross‐disciplin:.tw.
11. interagenc:.mp. or inter‐agenc:.tw.
12. interdisciplin:.mp. or inter‐disciplin:.tw.
13. intersector:.mp. or inter‐sector:.tw.
14. (transdisciplin: or trans‐disciplin:).mp.
15. (integrat: adj5 (work: or profession: or partnership: or team: or teamwork: or disciplin: or agenc:)).tw.
16. (welfare right: adj7 health:).tw.
17. jointness.mp.
18. (work: adj5 (joint: commission: or joint‐commission: or joint: plan: or joint‐plan: or joint: work: or joint‐work: or joined up: or joined‐up)).mp.
19. (work: adj5 (partnership: or teamwork: or team work: or team‐work:)).tw.
20. (partner agenc$ or partner department$).tw.
21. ((behave or behaving or behaves or behaved) adj cooperative$).tw.
22. (cooperativ$ adj2 (work$ or behavio?r or agenc$)).tw.
23. (partnership adj3 (work$ or cooperat$ or plan$ or relations or behavio?r or agenc$)).tw.
24. (interdepartmental adj2 (work$ or cooperat$ or behavio?r)).tw.
25. (interprofessional adj2 (work$ or cooperat$ or behavio?r or agenc$)).tw.
26. (cross sector$ or cross?sector$ or across sector$).tw.
27. (multi department$ or multidepartment$).tw.
28. ((working or work or works or worked) adj together).tw.
29. Interdisciplinary communication/
30. (multiagenc: or multi‐agenc: or multidisciplin: or multi‐disciplin: or multiprofessional: or multi‐professional: or multi‐sector:).mp. or multisector:.tw.
31. public health/
32. public health administration/
33. exp health planning/og, mt, td [Organization & Administration, Methods, Trends]
34. exp health planning organizations/
35. community health planning/og, mt, td [Organization & Administration,Methods, Trends]
36. health services accessibility/og [Organization & Administration]
37. exp home care services/og, ma [Organization & Administration, Manpower]
38. exp "Health Services Needs and Demand"/og [Organization & Administration]
39. health planning/
40. exp health promotion/og, ma, mt [Organization & Administration, Manpower, Methods]
41. health services/
42. Community Health Services/og, ma, mt [Organization & Administration, Manpower, Methods]
43. exp Community Health Centers/ma, og [Manpower, Organization & Administration]
44. community care.mp. or continuing care.tw. or long term care.tw. or longterm care.tw. or long‐term care.tw.
45. exp Health Education/mt, og, ma [Methods, Organization & Administration,Manpower]
46. exp primary health care/
47. comprehensive health care/
48. physicians, family/
49. emergency medical services/
50. preventive health services/
51. exp preventive health services/og, ma, mt [Organization & Administration,Manpower]
52. exp nursing services/og, ma [Organization & Administration,Manpower]
53. nursing/og, ma, mt [Organization & Administration, Manpower, Methods]
54. public health nursing/
55. rehabilitation nursing/
56. community health nurs:.mp.
57. health services for the aged/
58. rural health services/og, ma [Organization & Administration, Manpower]
59. health services, indigenous/
60. exp mental health services/og, ma [Organization & Administration, Manpower]
61. community mental health services/
62. exp community mental health centers/
63. exp case management/
64. community mental health team:.tw.
65. crisis intervention/
66. Psychotherapy/ma, mt, og [Manpower, Methods, Organization & Administration]
67. exp adolescent health services/
68. exp child care/
69. exp child welfare/
70. exp child health services/
71. Oral Health/
72. *aged/
73. exp Geriatrics/ma, mt, og [Manpower, Methods, Organization & Administration]
74. exp palliative care/og, ma, mt [Organization & Administration,Manpower,Methods]
75. exp Terminal Care/og, ma, mt [Organization & Administration, Manpower, Methods]
76. exp Long‐Term Care/og, ma, mt [Organization & Administration, Manpower, Methods]
77. exp primary prevention/ma, mt, og [Manpower, Methods, Organization & Administration]
78. "delivery of health care"/mt, og, ma [Methods,Organization & Administration, Manpower]
79. exp rehabilitation/mt, nu, og, ma [Methods, Nursing, Organization & Administration, Manpower]
80. rehabilitation/
81. occupational therapy/
82. exp communicable diseases/
83. ((outbreak: or infection:) adj control:).tw.
84. (welfare right: adj7 health:).tw.
85. exp immunization programs/og, ma, mt [Organization & Administration, Manpower,Methods]
86. mass screening/og, mt [Organization & Administration,Methods]
87. exp rehabilitation centers/
88. exp nursing homes/og, ma [Organization & Administration,Manpower]
89. nursing hom:.tw.
90. hospice care/og, ma, mt [Organization & Administration,Manpower]
91. day care/
92. respite care/
93. exp substance related disorders/rh [rehabilitation]
94. (mass media adj5 (health: or campaign: or scheme: or program: or project: or intervention: or strateg:)).tw.
95. health promot: school:.tw.
96. (health adj5 (promot: or scheme: or program: or project: or strateg: or scheme: or intervention:)).tw.
97. school nurs:.mp.
98. (speech and language therapist:).mp.
99. (family physician: or doctor: or nurse: or general practitioner: or GP or geriatrician: or health visitor: or dietician: or dietitian: or nutritionist: or physiotherapist: or occupational therapist: or therapist: or midwife).mp. or midwives.tw.
100. dietitian:.tw.
101. (community adj2 (program: or scheme: or project: or intervention: or strateg:)).tw.
102. Prenatal Care/mt, og, ma [Methods, Organization & Administration, Manpower]
103. Postnatal Care/og, ma, mt [Organization & Administration, Manpower, Methods]
104. geriatric evaluation.mp. and management.tw.
105. government agencies/
106. local government/
107. ((municipal: or city or town: or local: or education: or school:) adj5 (council: or authorit: or govern: or board:)).tw.
108. (government: adj5 (agenc: or plan: or polic: or strateg:)).tw.
109. housing.mp.
110. public housing/
111. residence characteristics/
112. housing for the elderly/
113. home care agencies/
114. homes for the aged/
115. exp Residential Facilities/og, ma, mt [Organization & Administration, Manpower, Methods]
116. residential facilities/
117. ((shelter: or half‐way or half way) adj5 (hous: or home: or accommodat:)).tw.
118. group home:.tw.
119. ((residential or nurs:) adj5 (home care or facilit:)).tw.
120. exp nursing homes/
121. nurs: home:.mp.
122. ((foster or care) adj4 home:).tw.
123. supported living.tw.
124. exp homeless persons/
125. homeless:.tw.
126. exp social work/
127. exp social security/
128. exp social welfare/
129. (social: adj4 (work: or support: or security or care: or welfare: or service: or network:)).tw.
130. consumer advocacy/
131. *counseling/
132. civil rights/
133. welfare rights.tw.
134. domestic care.tw.
135. day service:.tw.
136. exp Substance‐Related Disorders/rh [Rehabilitation]
137. Alcoholism/rh [Rehabilitation]
138. Alcohol Drinking/pc [Prevention & Control]
139. exp Social Behavior Disorders/nu, rh [Nursing, Rehabilitation]
140. Juvenile Delinquency/pc, rh [Prevention & Control, Rehabilitation]
141. youth offending team:.tw.
142. ((young or juvenile) adj2 offender:).tw.
143. (youth adj4 service:).tw.
144. ((leisure or community or youth or recreation:) adj2 (center: or centre:)).tw.
145. (play ground: or playground: or school yard: or schoolyard:).tw.
146. parks.mp. and recreation:.tw.
147. ((housing or neighbourhood or neighborhood) adj2 regeneration).tw.
148. ((neighbourhood or neighborhood) adj3 (renew: or improv: or revitali?ation)).tw.
149. exp social planning/
150. built environment:.mp. or urban environment:.tw.
151. ((child: or domestic: or partner: or spousal) adj3 (abuse: or violen: or protect:)).mp.
152. foster home care/
153. exp Disabled Persons/rh [Rehabilitation]
154. home adaptation:.tw.
155. (local adj2 (council: or hous:)).tw.
156. play: field:.tw.
157. (school: adj2 (infant: or junior: or kindergarten or senior: or primary or comprehensive or grammar or high or elementary or secondary)).tw.
158. sixth form college:.tw.
159. educational psychologist:.tw.
160. occupational psychologist:.tw.
161. ((environmental health or occupational health or housing or welfare rights or youth) adj5 (worker: or officer:)).tw.
162. public librar:.mp. or school teacher:.tw.
163. or/1‐30 [collaboration]
164. or/31‐104 [Health]
165. or/105‐162 [government]
166. randomized controlled trial.pt.
167. controlled clinical trial.pt.
168. intervention studies/
169. experiment$.tw.
170. (time adj series).tw.
171. (pre test or pretest or (posttest or post test)).tw.
172. random allocation/
173. impact.tw.
174. intervention?.tw.
175. chang$.tw.
176. evaluation studies/
177. evaluat$.tw.
178. effect?.tw.
179. comparative study.pt.
180. or/166‐179
181. or/163‐165
182. 180 and 181
183. limit 182 to yr="1966 ‐ 2008"
Database: PsycINFO
1. exp Public Relations/
2. inter?institutional relation:.mp.
3. interdepartmental: relation:.mp. or inter‐departmental relation:.tw.
4. interprofessional: relation:.mp. or inter‐professional: relat:.tw.
5. exp Cooperation/ or cooperative behavio?r.mp.
6. (cooperative: behavior: or co‐operative: behavior: or cooperative: behaviour: or co‐operative behaviour: or co‐operative: plan:).mp. or co‐operative plan.tw.
7. collaborat:.mp.
8. (cross‐system: or cross system: or cross disciplin:).mp. or cross‐disciplin:.tw.
9. Integrated Services/
10. (inter agency or inter‐agency).mp.
11. Interdisciplinary Treatment Approach/
12. interdisciplin:.mp. or inter‐disciplin:.tw.
13. intersector:.mp. or inter‐sector.tw.
14. (work: adj5 (joint: commission: or joint‐commission: or joint: plan: or joint‐plan: or joint: work: or joint‐work or joined up or joined‐up)).mp.
15. (work: adj5 (multiagenc: or multi‐agenc: or multidisciplin: or multi‐disciplin: or multiprofessional: or multi‐professional: or multi‐sector: or multisector:)).tw.
16. (work: adj5 (partnership: or teamwork: or team work: or team‐work:)).tw.
17. (transdisciplin: or trans‐disciplin:).mp.
18. (integrat: adj5 (work: or profession: or partnership: or team: or teamwork: or disciplin: or agenc:)).mp. [mp=title, abstract, heading word, table of contents, key concepts]
19. ("Welfare Services (Government"/ or welfare right.mp.) adj7 health:.mp. [mp=title, abstract, heading word, table of contents, key concepts]
20. Public Health/
21. Public Health Services/ or public health administration.mp.
22. health planning.mp.
23. health planning organizations.mp.
24. community health planning.mp.
25. health services accessibility.mp.
26. access to health care.mp.
27. exp Home Care/ or home care services.mp.
28. (health services needs and demand).mp. [mp=title, abstract, heading word, table of contents, key concepts]
29. exp Health Promotion/
30. Health Care Services/
31. Health Care Delivery/
32. Community Services/ or community health services.mp.
33. (community health centres or community health centers).mp.
34. community care.mp. or continuing care.tw. or long term care.tw. or longterm care.tw. or long‐term care.tw.
35. exp Health Education/
36. exp Primary Health Care/
37. comprehensive health care.mp.
38. Family Physicians/
39. Emergency Services/ or emergency medical services.mp.
40. preventive health services.mp.
41. nursing services.mp.
42. exp Nursing/
43. exp Psychiatric Nurses/ or mental health nursing.mp.
44. exp Public Health Service Nurses/ or public health nursing.mp.
45. rehabilitation nursing.mp.
46. community health nursing.mp.
47. health services for the aged.mp.
48. rural health services.mp.
49. (indigenous populations and health services).mp.
50. exp Mental Health Services/
51. exp Community Mental Health Services/
52. exp Community Mental Health Centers/ or community mental health centres.mp.
53. exp Case Management/
54. community mental health team.mp.
55. Crisis Intervention/
56. Psychotherapy/
57. exp Adolescent Psychiatry/ or adolescent health services.mp.
58. exp Child Care/
59. exp Child Welfare/
60. child health services.mp.
61. Oral Health/
62. *aged/
63. exp Geriatrics/
64. exp Palliative Care/
65. exp Terminally Ill Patients/ or terminal care.mp.
66. exp Long Term Care/
67. exp Primary Mental Health Prevention/
68. primary prevention.mp.
69. Health Care Delivery/ or delivery of health care.mp.
70. exp Rehabilitation/
71. Occupational Therapy/
72. communicable diseases.mp. or exp Infectious Disorders/
73. ((outbreak: or infection:) adj control:).tw.
74. exp Immunization/ or immunization program:.mp.
75. Screening/ or mass screening.mp.
76. exp Rehabilitation Centers/ or rehabilitation centres.mp.
77. exp Nursing Homes/
78. nursing hom:.tw.
79. nursing hom:.tw.
80. Hospice/ or hospice care.mp.
81. Day Care Centers/ or day care.mp.
82. Respite Care/
83. (exp Drug Abuse/ or substance related disorders.mp.) and rehabilitation.mp.
84. (mass media adj5 (health: or campaign: or scheme: or program: or project: or strateg: or scheme: or intervention: or strateg:)).tw.
85. health promot: school:.tw.
86. (health adj5 (promotion: or scheme: or program: or project: or strateg: or scheme: or intervention:)).tw.
87. school nurs:.mp.
88. (speech and language therapist).mp. [mp=title, abstract, heading word, table of contents, key concepts]
89. (family physician: or doctor: or nurse: or general practitioner: or GP or geriatrician: or health visitor: or dietician: or dietitian: or nutritionist: or physiotherapist: or occupational therapist: or therapist: or midwife:).mp. or midwives.tw.
90. dietitian:.tw.
91. (communit: adj2 (program: or scheme: or project: or intervention: or strateg:)).tw.
92. Prenatal Care/
93. postnatal care.mp.
94. (Geriatric Assessment/ or geriatric evaluation.mp.) and management.tw.
95. Government Agencies/
96. local government.mp.
97. ((municipal: or city or town: or local: or education: or school:) adj5 (council: or authorit: or govern: or board:)).tw.
98. (government: adj5 (agenc: or plan: or polic: or strateg:)).tw.
99. housing.mp. or exp Housing/
100. public housing.mp. or social housing.tw. or council housing.tw.
101. residence characteristics.mp.
102. housing for the elderly.mp.
103. home care agencies.mp.
104. Elder Care/ or homes for the aged.mp.
105. exp Residential Care Institutions/ or residential facilities.mp.
106. ((shelter: or half‐way or half way) adj5 (hous: or home: or accommodat:)).tw.
107. Group Homes/
108. ((residential or nurs:) adj5 (home care or facilit:)).tw.
109. exp Nursing Homes/
110. nurs: home:.mp.
111. ((foster or care) adj4 home:).tw.
112. exp Independent Living Programs/ or supported living.mp.
113. Homeless Mentally Ill/ or Homeless/ or homeless.mp.
114. social work.mp. or exp Social Casework/
115. exp Social Security/
116. exp "Welfare Services (Government)"/ or social welfare.mp.
117. (social: adj4 (work: or support: or security or care: or welfare: or service: or network:)).tw.
118. Advocacy/ or consumer advocacy.mp.
119. *counseling/
120. Civil Rights/
121. welfare rights.tw.
122. Home Care/ or domestic care.mp.
123. Day Care Centers/ or Adult Day Care/ or day service:.mp.
124. (exp Drug Dependency/ or exp Drug Abuse/ or substance related disorders.mp.) and rehabilitation.mp.
125. Alcoholism/ and rehabilitation.mp. [mp=title, abstract, heading word, table of contents, key concepts]
126. (Alcoholism/ or Alcohol Abuse/ or alcohol drinking.mp.) and (prevention and control).mp.
127. Behavior Disorders/ or social behaviour disorders.mp.
128. Juvenile Delinquency/ and (prevention and control).mp. [mp=title, abstract, heading word, table of contents, key concepts]
129. youth offending team.mp.
130. ((young or juvenile) adj2 offender:).tw.
131. (youth adj4 service:).tw.
132. ((leisure or community or youth or recreation:) adj2 (center: or centre:)).tw.
133. (play ground: or playground: or school yard: or schoolyard:).tw.
134. parks.mp. and recreation:.tw.
135. ((housing or neighbourhood or neighborhood) adj2 regeneration).tw.
136. ((neighbourhood or neighborhood) adj3 (renew: or improv: or revitali?ation)).tw.
137. social planning.mp.
138. built environment:.mp. or urban environment:.tw.
139. ((child: or domestic: or partner: or spousal) adj3 (abuse: or violen: or protect:)).mp.
140. Foster Care/ or foster home care.mp.
141. (disabled and rehabilitation).mp.
142. home adaptation.mp.
143. (local adj2 (council: or hous:)).tw.
144. play: field:.tw.
145. (school: adj2 (infant: or junior: or kindergarten or senior: or primary or comprehensive or grammar or high or elementary or secondary)).tw.
146. sixth form college:.tw.
147. Educational Psychologists/
148. occupational psychologist.mp.
149. ((environmental health or occupational health or housing or welfare rights or youth) adj5 (worker: or officer:)).tw.
150. public librar:.mp. or school teacher:.tw.
151. or/1‐19 [collaboration]
152. or/20‐94 [health]
153. or/95‐150 [government]
154. and/151‐153
155. randomized controlled trial.mp.
156. controlled clinical trial.mp.
157. intervention stud:.mp.
158. experiment:.tw.
159. (time adj series).tw.
160. (pre test or pretest or (post test or posttest)).tw.
161. random allocation.tw.
162. intervention?.tw.
163. chang:.tw.
164. evaluation stud:.mp.
165. evaluat:.tw.
166. effect?.tw.
167. comparative stud:.mp.
168. or/155‐167
169. 168 and 154
170. limit 169 to yr="1966 ‐ 2008"
Cochrane Public Health Specialized Register
{collab} OR {local government} OR {multi‐discip} OR {multi‐sector} OR {intersector} OR {interdepart} OR {interdiscip} OR {interagenc} OR {multi‐agenc}
Database: Rehabdata
Government and health and (collaboration or cooperation or interagency)
Database: OpenGrey
#70 (government or "local authority" or council or housing or neighbourhood or nursing home or homeless or alcohol abuse or drug abuse or clinic or rehabilitation) and ("health services" or "primary health care" or "community health services" or "mental health services") and (collaboration or interagency or interprofessional or partnership or teamwork)(34 records)
#69 teamwork(141 records)
#68 partnership(1673 records)
#67 interprofessional(48 records)
#66 interagency(20 records)
#65 collaboration(3304 records)
#64 "services"(44250 records)
#63 "health"(45657 records)
#62 "mental"(2434 records)
#61 "services"(44250 records)
#60 "health"(45657 records)
#59 "community"(35492 records)
#58 "care"(17415 records)
#57 "health"(45657 records)
#56 "primary"(831527 records)
#55 "services"(44250 records)
#54 "health"(45657 records)
#53 rehabilitation(1058 records)
#52 clinic(363 records)
#51 abuse(1118 records)
#50 drug(2696 records)
#49 abuse(1118 records)
#48 alcohol(1133 records)
#47 homeless(435 records)
#46 home(7072 records)
#45 nursing(2265 records)
#44 neighbourhood(508 records)
#43 housing(10491 records)
#42 council(37664 records)
#41 "authority"(7865 records)
#40 "local"(16836 records)
#39 government(9511 records)
#38 government or "local authority" or council or housing or neighbourhood or nursing home or homeless or alcohol abuse or drug abuse or clinic or rehabilitation(58805 records)
#37 rehabilitation(1058 records)
#36 clinic(363 records)
#35 abuse(1118 records)
#34 drug(2696 records)
#33 abuse(1118 records)
#32 alcohol(1133 records)
#31 homeless(435 records)
#30 home(7072 records)
#29 nursing(2265 records)
#28 neighbourhood(508 records)
#27 housing(10491 records)
#26 council(37664 records)
#25 "authority"(7865 records)
#24 "local"(16836 records)
#23 government(9511 records)
#22 "health services" or "primary health care" or "community health services" or "mental health services"(10613 records)
#21 "services"(44250 records)
#20 "health"(45657 records)
#19 "mental"(2434 records)
#18 "services"(44250 records)
#17 "health"(45657 records)
#16 "community"(35492 records)
#15 "care"(17415 records)
#14 "health"(45657 records)
#13 "primary"(831527 records)
#12 "services"(44250 records)
#11 "health"(45657 records)
#10 collaboration or interagency or interprofessional or partnership or teamwork(5140 records)
#9 teamwork(141 records)
#8 partnership(1673 records)
#7 interprofessional(48 records)
#6 interagency(20 records)
#5 collaboration(3304 records)
#4 (government or "local authority" or council or housing or neighbourhood or "nursing home" or homeless or "alcohol abuse" or "drug abuse" or clinic or rehabilitation) and ("health services" or "primary health care" or "community health services" or "mental health services") and (collaboration or interagency or interprofessional or partnership or teamwork)(34 records)
#3 government or "local authority" or council or housing or neighbourhood or "nursing home" or homeless or "alcohol abuse" or "drug abuse" or clinic or rehabilitation(58805 records)
#2 "health services" or "primary health care" or "community health services" or "mental health services"(10613 records)
#1 collaboration or interagency or interprofessional or partnership or teamwork(5140 records)
Database: Social Care Online
(topic="collaboration" or topic="interprofessional relations" or topic="interagency cooperation" or topic="integrated services" or topic="multi‐disciplinary services") and (topic="public health " or topic="planning" or topic="access to services" or topic="health services" or keyword="community health services " or keyword="community health centres" or topic="primary care" or topic="emergency health services" or freetext="nursing" or topic="mental health services" or topic="community mental health services" or topic="case management" or topic="crisis intervention" or topic="psychotherapy" or topic="oral health" or topic="substance misuse" or topic="drug misuse" or topic="alcohol misuse" or freetext="school nurse" or freetext="family physician" or freetext="family doctor" or freetext="doctor" or freetext="community project" or freetext="community intervention") and (topic="local government " or topic="central government " or topic="government policy" or topic="housing " or topic="sheltered housing " or topic="community homes " or freetext="care homes " topic="group homes " or topic="foster care " or topic="homeless people " or freetext="social work " or freetext="social security " or freetext= "social welfare" or freetext="advocacy " or topic="counselling " or topic="juvenile delinquency " or topic="young offenders " or freetext="youth offending team " or freetext="youth service " or freetext="leisure centre" or freetext="playground" or freetext ="neighbourhood regeneration" or freetext= "neighbourhood renewal" or freetext="housing regeneration" or freetext ="housing renewal" or freetext="home adaptation"or freetext="school or college")
Database: Social Services Abstracts
Query: ((DE=("cooperation" or "partner/partners/partnership" or
"teamwork")) or(AB=(collaborat* or interagenc* or multiagenc*) or
(inter‐institutional* or inter‐professional or inter‐departmental*) or
(interinstitutional* or interprofessional or interdepartmental*)))
and((DE=("day care" or "child care services" or "community mental health"
or "elderly" or "emergency medical services" or "foster care" or
"geriatrics" or "health" or "health care services" or "health care
utilization" or "health education" or "health planning" or "health
policy" or "health professions" or "home care" or "home health care" or
"interprofessional approach" or "long term care" or "medicine" or "mental
health" or "mental health services" or "midwifery" or "occupational safety
and health" or "palliative care" or "paramedical personnel" or
"physicians" or "primary health care" or "public health" or "residential
institutions" or "respite care" or "social services" or "social services
utilization" or "vaccination")) or(AB=(("family physician*") or doctor*
or (general practitioner*)) or AB=(nurs* or ("School nurs*") or
geriatrician*) or AB=((occupational therapist*) or physiotherapist* or
nutritionist*) or AB=(dietitian* or dietician* or ("health visitor*")) or
AB=(therapist* or midwives or midwife) or AB=(("occupational therapist*")
or physiotherapist* or ("respite care")))) and(DE=("alcoholism" or
"central government" or "city planning" or "communities" or "community
services" or "councils" or "facilities" or "federal government" or
"homelessness" or "housing" or "juvenile delinquency" or "libraries" or
"local government" or "local planning" or "local politics" or
"neighborhoods" or "nursing homes" or "public housing" or "recreation" or
"residence" or "residential institutions" or "retirement" or "social
policy" or "social security" or "social services" or "social support" or
"social welfare" or "social work" or "welfare services"))
Database: Sociological Abstracts
Query: (((DE=("cooperation" or "intergroup relations" or "interpersonal
relations" or "interaction" or "interdisciplinary approach" or "teams"))
or(AB=(collaborat* or interagenc* or multiagenc*) or
(inter‐institutional* or inter‐professional or inter‐departmental*) or
(interinstitutional* or interprofessional or interdepartmental*))
or((inter‐departmental) or(multidisciplin*) or("cross disciplin*") or
(partnership) or (interagency))) and((DE=("day care" or "activities of
daily living" or "adult care services" or "after care" or "caregiver
burden" or "caregivers" or "crisis intervention" or "elderly" or
"geriatrics" or "gerontology" or "health" or "health care services" or
"health care utilization" or "health education" or "health planning" or
"health policy" or "home care" or "home health care" or "human services"
or "independent living" or "long term care" or "medical decision making"
or "mental health" or "mental health services" or "mental illness" or
"physical education" or "primary health care" or "public health" or
"rehabilitation" or "respite care" or "treatment programs"))
or(AB=(("family physician*") or doctor* or (general practitioner*)) or
AB=(nurs* or ("School nurs*") or geriatrician*) or AB=((occupational
therapist*) or physiotherapist* or nutritionist*) or AB=(dietitian* or
dietician* or ("health visitor*")) or AB=(therapist* or midwives or
midwife) or AB=(("occupational therapist*") or physiotherapist* or
("respite care")))) and((DE=("central government" or "cities" or "city
planning" or "communities" or "community services" or "councils" or
"facilities" or "foster care" or "government" or "government agencies" or
"homelessness" or "housing" or "institutions" or "juvenile correctional
institutions" or "libraries" or "local government" or "local planning" or
"neighborhoods" or "nursing homes" or "public administration" or "public
housing" or "rental housing" or "residential institutions" or "social
security" or "social welfare" or "social work" or "welfare services"))
or(AB=(("play ground*") or playground* or schoolyard*) or AB=(("school
yard*") or parks or ("built environment*"))))) and((KW=("comparative
analysis" or "methodology data analysis" or "cohort analysis" or
"longitudinal studies" or "random samples" or "research design" or
"research subjects" or "sampling")) or(AB=(random* or ("controlled
trial") or ("intervention stud*")) or AB=(experiment* or ("randomized
control trial"))))
Database: TRoPHI (the Trials Register of Promoting Health Interventions)
Collaboration
Cooperation
Partnership
1 or 2 or 3
"health services"
"health care"
"health promotion"
"community care"
"primary care"
"mental health services"
"mental health care"
clinic
"emergency medical services"
nurse
doctor
5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
government
"local government"
"local authority"
council
housing
"nursing home"
homeless
alcoholism
alcohol abuse
"drug abuse"
rehabilitation
17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27
16 and 28
4 AND 36
Database: ZETOC service http://zetoc.mimas.ac.uk/
Collaboration or partnership or teamwork AND Health AND local government or local council or local authority or municipal council or municipal authority or government agency
Data and analyses
Comparison 1. Mortality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 3 | 1994 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.17] |
Comparison 2. Morbidity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mental Health continuous | 5 | 12060 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.52, ‐0.04] |
| 2 Physical Health continuous | 5 | 11388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.10, 0.07] |
| 3 Quality of Life | 3 | 797 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.44, 0.27] |
| 4 Global Assessment of Function symptoms score scale | 2 | 600 | Mean Difference (IV, Random, 95% CI) | ‐2.63 [‐5.16, ‐0.10] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bertelsen 2008.
| Methods | A randomised controlled trial recruiting patients between January 1998 and December 2000 with two year and five year follow‐up. Role of collaborating partners Lead agency: Mental health Strategic involvement (policy making and service planning): Secondary health care Commissioning (implementing strategy taking account of resources available): Primary and secondary health care, social services Operational (providing services directly): Primary and secondary health care, social services Set in Denmark. |
|
| Participants | 547 patients (275 intervention group, 272 control group) aged between 18 and 45 with a first time diagnosis within the schizophrenia spectrum (F2 category codes of ICD 10) and no history of receiving antipsychotic medication for more than 12 continuous weeks. Patients were recruited from inpatient and outpatient mental health services in Copenhagen and Aarhus. Of eligible patients only 5% refused to participate. Male 58% (intervention group) 60% (controls) Mean age 26.6 years in both groups |
|
| Interventions | Intensive early‐intervention programme was defined by protocols and consisted of three core elements, Assertive Community Treatment (ACT), family treatment where possible and social skills training where needed. ACT teams were based at the Copenhagen Hospital Corporation and Psychiatric Hospital, Aarhus and consisted of psychiatrist, psychologist, nurse, vocational therapist and social worker. Psycho‐educational family treatment was provided by a family therapist. Caseload ratio was 1 researcher for every 10 patients. Each intervention patient was allocated a team member responsible for maintaining contact and securing coordination of the treatment across different treatment facilities and across the social and health sectors. Over a two year period patients were offered an individual plan of treatment, regular visits as required, at least weekly, and psycho‐educational treatment lasting 1.5 hours every second week over 18 months. Social skills training was provided if required via modular course. After two years patients returned to standard treatment. Standard treatment for controls and intervention patients after the first 2 years was generally provided at a community mental health centre but in a few cases was a provided by a general practitioner. They may have had contact with social workers. A staff member's caseload in the community mental health centre varied between 20 and 30 patients. |
|
| Outcomes | Outcomes were measured at two year (n=369,) and five year (n=301) follow‐up. Primary outcome measures were symptoms according to the Scale for Assessment of Psychotic Symptoms (SAPS), Scale for Assessment of Negative symptoms (SANS) and the social functioning element of the Global Assessment of Functioning (GAF) scores for symptoms and for function. Secondary outcomes included secondary diagnosis of substance abuse, medication, use of services, depressive symptoms, suicidal behaviour, housing situation and vocational situation. Course of illness measure with Life Chart Schedule. Main diagnosis and substance abuse measured by Schedule for Clinical Assessment in Neuropsychiatry (SCAN Version 2.0 in 1998 and 2.1 since 1999). Duration of untreated psychosis at entry to the trial. Suicidal behaviour measured by self‐reported suicide attempts and ideation. Days in hospital, emergency department contacts, outpatient contacts from the Danish Psychiatric Central Register. Information on independent living and supported housing from the Civil Status Register. Employment, family situation, sick leave, early‐age pension from the Integrated Database for Labour Market Research. Mortality and cause of death from the Cause of Death Register. |
|
| Notes | Follow‐up at 2 years was unequal, 75% in intervention group and 60% in control group. Follow‐up at 5 years was below 60% in both groups (but above threshold set from power calculation of 142 in each arm). Significant additional resource required to deliver intervention. One of the initial hypotheses was that "Increased co‐operation between the primary health and social sectors leads to reduced duration of untreated psychosis, as knowledge of psychosis and easy access to treatment is essential for co‐workers' referral policy." We were unable to obtain further details from the authors on this point. The fidelity of the treatment programme, measured with the index of fidelity of assertive community treatment, was 70% in Copenhagen and Aarhus. Overall risk of bias was high. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Computer generated allocation. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Assessment at 2 year follow‐up was not blinded. Single blind assessment by independent investigator at 5 years but follow‐up rate was below 60% so not reported here. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Estimated mean differences are based on a repeated measurement model, assuming that the distribution of missing data could be estimated from the information from previous interviews. |
| Selective reporting (reporting bias) | Low risk | Protocol provided in linked paper Jørgensen 2000. |
| Other bias | High risk | Problems related to potential selection bias. |
| Randomisation adequately described/protected? | Low risk | Centralised telephone randomisation. |
| Protection against contamination? | Low risk | Control patients may have had access to social worker but this was part of standard treatment. |
| Follow‐up rate adequate? | High risk | Follow‐up rates unequal at 2 years (75% in intervention group and 60% in control group). At the end point of the trial at 5 years, follow‐up assessment rates only 56% (intervention group) and 57% (control group) , 57% and 58.8% respectively when adjusted for deaths, so these results were not included in this review. |
| Reliable primary outcome measure? | Low risk | Scale for Assessment of Positive (SAPS) and Negative (SANS) Symptoms, plus functional GAF (Global Assessment of Functioning) well established and inter‐rater reliability checked. |
| Groups measured at baseline? | Low risk | Groups approximately balanced |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Bruzzese 2006.
| Methods | Cluster randomized controlled trial with 12 and 24 month follow‐up. Schools and families enrolled in May 1998 (wave 1) and September 1999 (wave 2). Collaborating partners Lead agency: Local Education Authority Strategic involvement (policy making and service planning): Primary health care, health promotion, Local Education Authority Commissioning (implementing strategy taking account of resources available): Local Education Authority Operational (providing services directly): Primary health care, health promotion, Local Education Authority Set in United States of America. |
|
| Participants | 591 students in kindergarten to grade 5 (307 in intervention schools, 284 in control schools), mean age at baseline 7.8 years, and their caregivers, from 44 schools (out of 650 schools meeting eligibility criteria of >50% of students receiving free lunch and >67% being ethnic minorities) from all 5 boroughs of New York City. Males 57.8% (intervention), 59.4% (controls). Eligible families (those with a child diagnosed with asthma and symptoms of persistent asthma) were enrolled through telephone call. Identified from case‐detection forms, returned to school by approximately 27% of all caregivers. Schools were paired by size and borough and randomly assigned in each pair to either intervention or control school. Families were enrolled in 2 waves and data collection lasted 2 years for each wave. Wave 1 data collection started for 24 schools in May 1998 and wave 2 in 20 schools began September 1999. |
|
| Interventions | Preventive care networks for each intervention school were established between school staff, health professionals and families of students with asthma. Each school health team included a full time school nurse, school physician 2 days per month, public health assistant 2‐3 days per week, schoolteacher or administrator, and a parent. Columbia University staff led a three day training workshop for the school health teams and an additional single training session was run for teachers on asthma and their role in helping children manage asthma in school. Workshops on preventative therapy, communication, patient education strategies and medication plans were run for children?s primary care providers (PCPs) using PACE (Physician Asthma Care Education) programme. School nurses and physicians worked with families to assess children's asthma severity and healthcare needs. They sent sample treatment plans to the students' PCPs based on each student's asthma severity and encouraged caregivers and PCPs to develop asthma management plans in line with National Heart, Lung and Blood Institute criteria. School health team nurses conveyed instructions from the management plans to teachers and also arranged referral for medical care if needed. They delivered this intervention in full for 2 years and continued to give ad hoc support for a further year. |
|
| Outcomes | Outcomes were measured at 12 month (n= 472) and 24 month (n=368) follow‐up. Primary outcomes Asthma symptoms (number of days with symptoms in past 2 weeks and past 6 months, number of nights woken in past 2 weeks and past 6 months). Limitations due to asthma (number of days restricted activity in past 2 weeks and past 6 months), number of days absent from school as reported by parents in past 2 weeks. School absences for all reasons measured using school records Paediatric Asthma Caregiver's Quality of Life (PACQLQ). Secondary outcomes Health care utilization (number of urgent visits to clinician in past 12 months, number of Emergency Department visits in past 12 months, number of hospitalisations in past 12 months). |
|
| Notes | No power calculation was reported. Only 25% of PCPs completed PACE training and only 10% returned treatment plans to school and these were often inconsistent with NHBLI treatment guidelines. Substantial support will be needed to replicate intervention. Overall risk of bias was high. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation method. |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding but outcome was judged to not be influenced. Pg 309 |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data only provided for 368/591 participants (62%) at 24 months. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available to compare intended with reported outcome measures. |
| Other bias | Unclear risk | Unclear how participants were selected. |
| Randomisation adequately described/protected? | Unclear risk | No description of randomisation method. Pages 307 and 308 |
| Protection against contamination? | High risk | Unrelated to this study, New York City Department Of Health and Mental Hygiene provided Open Airways for Schools (OAS) programme for 3rd‐5th grade students with asthma, including those in control group. Approximately half the sample met the age criteria to receive OAS and intervention and control group participation levels were comparable. |
| Follow‐up rate adequate? | Low risk | Rate >60% and balanced across both arms. |
| Reliable primary outcome measure? | Low risk | After 6 months, intervention group had significantly fewer asthma symptoms but after 2 years, only difference was fewer hospitalisations in past 12 months. |
| Groups measured at baseline? | Low risk | Groups approximately balanced |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Challis 2002.
| Methods | A controlled clinical trial with follow‐up at 6 months and 12 months. Collaborating partners Lead agency: Community mental health Strategic involvement (policy making and service planning): No evidence of collaborating at the strategic level. Commissioning (implementing strategy taking account of resources available): Secondary health care, social services. Operational (providing services directly): Primary health care, secondary health care, social services. Set in United Kingdom. |
|
| Participants | The study looked at elderly adults with dementia in Lewisham, South London. Forty‐five cases in the intervention group and 50 controls were assessed over a two year period. From these, 43 matched pairs were identified to compare destinational outcome and costs. 30.2% male, mean age 80.8 (intervention)/79.8 yrs (control). Subjects were identified by two community mental health teams for the elderly (CMHTE) as new referrals or cases with a major change in circumstances, or with significant needs unmet by existing services, or perceived as at risk of institutionalisation. Over 70% had severe cognitive impairment and high/maximum disability. 80% had a carer and half of the carers were suffering marked stress. |
|
| Interventions | Individuals in the intervention arm received care from Lewisham Case Management Scheme, an intensive case management scheme with case managers in a CMHTE caring for a target population of older people with dementia. Case managers were social services employees with protected case loads of 20‐25 cases and control over a devolved budget. They were integrated into the mental health team and had access to all relevant health and social care resources for the care of older people with dementia. They maintained structured care plans which were completed at regular intervals during the 2 years of the study. Individuals in the control arm received care from a CMHTE without a case management service. |
|
| Outcomes | No primary outcome stated. Assessment of need and quality of life was conducted at 6 and 12 months. Destinational outcomes (still being at home, being placed in a care home or dying) were measured every 6 months for 2 years. Quality of life was measured through the CARE schedule to measure depression, disability through CAPE Behaviour Rating Scale for physical disability, social disturbance, communication disorder and apathy. Quality of care was measured through CAPE, assessing dependency. Overall need ratings and level of risk judged by research assessors. Carers' health was assessed through the Malaise scale as a global indicator of stress. |
|
| Notes | No power calculation was reported. Main changes 44% extra for home care, 24% for extra professional care including case management, 27% acute hospital care. Mean costs per annum: £23,402 for intervention group, £19,053 for control group. Additional resources required could account for any benefits achieved. Majority of additional costs were incurred by Social Services (£8815 per patient per year intervention group/ £4676 per patient per year in control) Overall risk of bias was high. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Groups were not randomised. One community health team received the intervention and another acted as control. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not possible due to nature of allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Full outcome data provided for 43 matched pairs (86 of the 95 cases included). |
| Selective reporting (reporting bias) | High risk | Different outcomes reported at different follow‐up periods. |
| Other bias | High risk | Patients were identified for inclusion in the study by their clinicians |
| Randomisation adequately described/protected? | High risk | No randomisation |
| Protection against contamination? | Low risk | Separate settings so contamination unlikely. |
| Follow‐up rate adequate? | Low risk | >80% and balanced across both arms but rate varied between individual outcomes. |
| Reliable primary outcome measure? | Low risk | No primary outcome stated but reliable measures used to assess health outcomes. |
| Groups measured at baseline? | Low risk | Groups approximately balanced |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Cooper 1975.
| Methods | Controlled clinical trial with follow‐up at 12 months. Collaborating partners Lead agency: Primary care Strategic involvement (policy making and service planning): Primary health care. Commissioning (implementing strategy taking account of resources available): Primary health care, social services. Operational (providing services directly): Primary health care, secondary health care, social services. Set in United Kingdom. |
|
| Participants | 189 primary care patients living in a metropolitan area with chronic neurotic illness were followed up at 12 months. Intervention group 92 patients (86.8% of patients enrolled), males 26.1%, mean age 42.1 years. Control group 97 patients (84.3% of patients enrolled), males 22.7%, mean age 45.5 years. |
|
| Interventions | Attachment of a social worker to a primary care practice, and involvement of research psychiatrists. The GPs, health visitors, social worker and research psychiatrists attended fortnightly meetings to discuss new referrals and progress of cases. Once experiment was established this evaluation was set up to assess the therapeutic value of the service. Patients in intervention group had usual care plus one or all of the following: 1. Recommendations to GP 2. Referral to local psychiatric or social services 3. Social support within practice 4. Consultation with research team psychiatrist |
|
| Outcomes | Change in psychiatric rating (scale now known as GHQ 30) Change in social adjustment score (author scale) |
|
| Notes | No power calculation was reported. Additional resources used included a social worker allocated to GP practice. Involvement of two research team psychiatrists. Overall risk of bias was high. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | No randomisation. Control patients selected from other practices. |
| Blinding (performance bias and detection bias) All outcomes | High risk | It does not appear that there was any blinding. Although assessors who treated patients did not assess those patients at follow‐up there was no indication that psychiatrist was blind to study group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Full outcome data. |
| Selective reporting (reporting bias) | Unclear risk | This study was conducted in the early 1970s and the protocol is not available |
| Other bias | High risk | Possible selection bias. Experimental cases were put forward in the hope that expert help might be given while the control patients were selected purely for research purposes. |
| Randomisation adequately described/protected? | High risk | Non‐randomised controlled study, not possible to randomise. |
| Protection against contamination? | Low risk | Contamination unlikely. Patients for the control group were drawn from separate practices without access to the experimental facility. |
| Follow‐up rate adequate? | Low risk | Follow‐up rate >80% and balanced across both arms. Whilst the authors state that 86.8% of intervention and 84.3% of controls were successfully followed up, it is impossible to confirm this from the way the data are presented. It is equally impossible to say whether the authors conducted an ITT analysis. |
| Reliable primary outcome measure? | Low risk | Standardised psychiatric interview which had been tested for inter‐rater reliability. The psychiatric outcomes are measured using what has become a validated self‐administered checklist: the General Health Questionnaire (GHQ‐30). Social outcomes appear to be measured by a scale developed by one of the authors. |
| Groups measured at baseline? | Low risk | Only sociodemographic baseline data were assessed for statistical differences between groups. Differences noted though none reached significance (but relatively small sample sizes). Relative excess of 60‐65 year olds and social classes I and II in controls and small excess of retired persons and social classes IV and V in experimental group. Groups appeared well matched for psychiatric ratings. |
| Appropriate choice of controls (CBA studies only)? | High risk | Control patients identified up to 18 months ahead of the intervention group. Cannot be certain that treatment/prognosis did not change during period though authors say no reason to believe that this was the case. |
| Contemporaneous data collection (CBA studies only)? | Low risk | Data collected at one year in both groups. |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Coppins 2011.
| Methods | A randomised controlled trial conducted over 2 years. Dates trial conducted not reported. Outcomes were measured at 6 (n=58), 12 (n=55), 18 (n=48) and 24 (n=46) months follow‐up. However this was a cross‐over trial with the intervention being delivered to one group in the first 12 months and the other group in the second twelve months. Collaborating partners Lead agency: Health Strategic involvement (policy making and service planning): health, education, sport Commissioning (implementing strategy taking account of resources available): health, education, sport Operational (providing services directly): Community health, health promotion, education, sport Set in UK |
|
| Participants | 65 participants (Intervention = 35; Control = 30) aged 6 to 14 years with a BMI above the 91st centile and who were able to participate in the intervention activities. Participants were recruited from referrals from healthcare professionals (n=33) or by self‐referral (n=32) as a result of media advertising via the local newspaper and television channel. Sixty‐five people were screened and all gave consent to participate. None were excluded on medical grounds that would affect their ability to participate in the activities. Male 31.7% (intervention group), 30.0% (controls) Mean age 133.4 months (intervention group), 116.9 (controls) |
|
| Interventions | Intervention consisted of two Saturday morning workshops (8 hours in total) in a school, 1 to 2 weeks apart, focused on healthy eating, physical activity, reducing sedentary behaviour, behaviour change and psychological well‐being. In addition, two one‐hour physical activity sessions per week during term‐time through the year‐long intervention period, consisting of junior gym sessions, bikes, circuits, trampolining, rock climbing, table tennis, basketball, tennis, badminton, football and the bleep test. Siblings aged 6 to 14 years and parents/guardians were also encouraged to participate. The workshops were designed and delivered by a dietician, physical activity health promotion officer, an educational or clinical psychologist and physical activity instructors. The physical activity sessions were led by physical activity instructors. The control group received no input in the first year but crossed over in the second year to receive the full intervention and the original intervention group received no input in the second year. |
|
| Outcomes | Primary outcome measure was change in BMI SDS (BMI Z score). Secondary clinical outcomes were changes in waist circumference SDS (Z score), percentage body fat, lifestyle outcomes of diet composition and physical activity levels. |
|
| Notes | Intervention and control groups were not comparable at baseline. There was significant difference for age (p=0.007), height (p=0.011) and sum of skinfolds (p=0.018). Cost per child was estimated at £403 compared with £45 for usual care of 1.5 hours of individual dietetic consultations. 4 participants in the intervention group were excluded after 12 months because they continued with the programme in the second year. Attendance at the physical activity sessions was very low in both groups (mean attendance 24.1% 95% CI 15.4 – 32.9 in the group receiving the intervention in the first year and 31.7% in the group receiving the intervention in the second year. Overall risk of bias was high |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | RCT but no detail given on method of randomisation |
| Blinding (performance bias and detection bias) All outcomes | High risk | Lead researcher was not blind to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Primary outcome measures reported fully but not all secondary outcome measures |
| Selective reporting (reporting bias) | Low risk | All outcomes have been reported |
| Other bias | Unclear risk | Sixty percent of the group receiving the intervention in the first year were self referred compared to 36.7% of the control group. The mean difference in age, with the intervention group significantly older than control group by 16 months, poses a risk of confounding as the age range includes the time of onset of puberty for many children, a time when body fat and BMI can change abruptly. |
| Randomisation adequately described/protected? | High risk | Method not described |
| Protection against contamination? | Low risk | Though the participants allocated to wait for a year before receiving the intervention may have started to change their behaviours in the waiting period. |
| Follow‐up rate adequate? | Low risk | 55/65 participants at cross‐over at 12 months |
| Reliable primary outcome measure? | Unclear risk | Good outcome measure but disparate age of participant groups may make it less reliable in this trial. |
| Groups measured at baseline? | High risk | Significant differences at baseline between the two groups |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | N/A |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | N/A |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERAL RISK OF BIAS WAS HIGH |
Florence 2011.
| Methods | An interrupted time series measuring violence recorded by the police and hospital admissions related to violence in a city between 2000 and 2007. Collaborating partners Lead agency: Health Strategic involvement (policy making and service planning):secondary health care, local government, police Commissioning (implementing strategy taking account of resources available): secondary care, local government, police, ambulance, local licensees Operational (providing services directly): secondary care, local government, police, ambulance, local licensees. Set in UK |
|
| Participants | Rates of violence reported to the Cardiff police and hospital admissions in Cardiff due to violence were recorded for the population of Cardiff (324,800 in 2001), surrounding areas and visitors. Data collection was monthly between 2000 and 2007. There were 33 months of observations before the programme was implemented and 51 months after implementation. Changes in violence were also compared with 14 control cities classified as most similar by the Home Office (Birmingham, Bristol, Coventry, Derby, Leeds, Leicester, Lincoln, Newcastle upon Tyne, Northampton, Plymouth, Preston, Reading, Sheffield, Stoke on Trent). |
|
| Interventions | Cardiff Violence Prevention Programme was established to share data between agencies and use the information for violence prevention through targeted policing and other strategies. The multiagency violence prevention group was set up in 1997 and included city government (education, transport, licensing regulators) police, an emergency department consultant and an oral and maxillofacial surgeon, ambulance service and local licensees. The programme became operational in January 2003 with full data sharing between partners. Information from emergency department consultations and police intelligence data was combined to generate constantly updated violence hotspot maps and summaries of weapon use and violence type, classified to fit with national crime survey categorisation. Adjustments were made to police patrol routes, moving resources from the suburbs into the city centre at weekends, targeting problematic licensed premises and deployment of closed circuit television. Traffic flows and public transport were improved. Sections of the city centre where bars and nightclubs were concentrated were pedestrianised (2004). Plastic glassware was mandated in selected licensed premises (2005). The national crime recording standard was introduced police force by police force between 1999 and 2002 to increase and standardise reporting rates. It was introduced in the South Wales police force, incorporating the Cardiff area in April 2002. |
|
| Outcomes | Health service records of hospital admissions related to violence and police recordings of woundings and less serious assaults | |
| Notes | Additional resource was a data analyst to combine health and police data. Changes were introduced sequentially through the life of the programme. Overall risk of bias was unclear. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Intervention and control populations unlikely to have been aware of formal study |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Research team aware of status of intervention and control areas but routinely collected data (police reports and hospital activity) used to assess progress |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence of incomplete data due to outcomes measured by routine data collection |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | High risk | Control cities selected to be similar in a range of sociodemographic and geographic factors which together are linked to levels of crime. Study design not an RCT and has an inherent risk of bias. |
| Randomisation adequately described/protected? | High risk | No randomisation but the intervention city was compared to a range of other cities. |
| Protection against contamination? | Low risk | Contamination unlikely. Intervention required 33 months to develop for the intervention city. No such time or resource was possible in the control cities. |
| Follow‐up rate adequate? | Low risk | Routinely collected population data used |
| Reliable primary outcome measure? | Low risk | Yes, routinely collected data |
| Groups measured at baseline? | Low risk | Good information pre‐intervention |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | N/A |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | N/A |
| IS THE STUDY AT LOW RISK OF BIAS? | Unclear risk | Well conducted study. At low risk of bias for an ITS |
Hultberg 2005.
| Methods | Controlled before and after study with 12 months follow‐up of 3 intervention sites and 4 control sites. Collaborating partners Lead agency: Primary care. Strategic involvement (policy making and service planning): Primary health care, social services. Commissioning (implementing strategy taking account of resources available): Primary health care, social services. Operational (providing services directly): Primary health care, secondary health care, social services. Set in Sweden. |
|
| Participants | 138 participants with musculoskeletal disorder in Goteburg (107 attending DELTA intervention health centres and 31 attending control health centres outside the DELTA trial area) who completed 3 interviews at baseline, 6 months and 12 month follow‐up. Intervention group 36% male and 21% aged 16 ‐ 30, 50% aged 31 ‐ 50, 29% aged 51 ‐ 65 years. Control group 19% male and 25% aged 16 ‐ 30, 65% aged 31 ‐ 50, 10% aged 51 ‐ 65 years. |
|
| Interventions | Collaboration consisted of a co‐financed collaborative care model to intensify rehabilitation through multidisciplinary teams (health centre physicians and nurses with occupational therapists, physiotherapists, social workers and social insurance officers) based in health centres. They had access to a joint budget from a common administrative body. They met weekly to discuss the rehabilitation of individual patients. | |
| Outcomes | Pain level measured by the Visual Analogue Scale (VAS) Long term or repeated sick leave Health‐related quality of life measured through EuroQol 5 dimensions instrument (EQ‐5D) |
|
| Notes | Power calculation was not reported but they aimed for a sample size of 450 patients. Smaller sample size achieved than aimed for despite study recruiting 8 months longer than planned. Potential for selection bias. The total healthcare cost for an average patient in the intervention was 1979 Euro and 1286 Euro for the control group. Overall risk of bias was high. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Unlikely due to selection methods, as patients were recruited to intervention and control arms by their physicians, who would have been aware of their status. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Unlikely that assessments were conducted blind due to study design. Some assessments were conducted in the intervention and control health centres. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Follow‐up rates adequate. |
| Selective reporting (reporting bias) | High risk | Linked paper Hultberg 2002 (p 5), together these papers report on three projects from a wider set of 20 DELTA projects in Goteborg. |
| Other bias | High risk | Low recruitment rate (aimed to recruit 450 but achieved 167). Control group small at 39 patients. P117, even though the planned recruitment period had been extended by 8 months, they only managed to recruit about half the targeted sample size. A large proportion of those invited declined to participate. |
| Randomisation adequately described/protected? | High risk | Not randomised |
| Protection against contamination? | Low risk | Adequate as intervention delivered at health centres |
| Follow‐up rate adequate? | Low risk | Follow‐up rate 83% (84% in intervention and 79% in control group) |
| Reliable primary outcome measure? | Unclear risk | The authors concluded that this co‐financing model was not associated with better patient outcome for patients with musculoskeletal disorders but the authors questioned their own findings. P122 |
| Groups measured at baseline? | Low risk | P118 table2 Control group small compared to intervention group though groups appeared balanced at baseline. Not clear about recruitment process. |
| Appropriate choice of controls (CBA studies only)? | Low risk | Adequate choice of control areas but low recruitment rates for controls |
| Contemporaneous data collection (CBA studies only)? | Low risk | Yes |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Kloek 2006.
| Methods | Controlled before and after study over 2 years, September 2000 to September 2002. Collaborating partners Lead agency: Municipal health. Strategic involvement (policy making and service planning): Local health planners, primary health care, social services. Commissioning (implementing strategy taking account of resources available): No evidence of additional collaboration at this level. Operational (providing services directly): Primary health care, health promotion, social services. Set in Netherlands. |
|
| Participants | Residents in deprived areas (population range 1800 ‐ 6700) in Eindhoven. 4800 residents aged 18‐65 years from three intervention areas and three control areas received a postal questionnaire at baseline. 2781 returned completed questionnaires at baseline (response rate 60%). 1929 returned questionnaires at 2 year follow‐up (69% of respondents at baseline). |
|
| Interventions | The programme "Wijkgezondheidswerk" consisted of two coalitions in the intervention areas (one coalition covered two intervention areas which bordered each other) led by the Municipal Health Services with representatives from social work, social welfare, city development department, a neighbourhood organisation representing residents, a general practitioner and researchers. Each coalition assessed the health needs of the neighbourhood to develop neighbourhood action plans related to determinants of health. Lifestyle intervention goals were focused to improve health related behaviour measured by self‐reported fruit consumption, vegetable consumption, physical activity, smoking cessation and excessive alcohol consumption. Examples of interventions include nutrition projects in primary schools, neighbourhood walking classes, gymnastic classes, quit smoking courses and large annual community events related to health. |
|
| Outcomes | Primary aim was to improve health‐related behaviours as measured by impact on fruit and vegetable consumption, physical activity, smoking and alcohol consumption. Intermediate aims were to assess health‐related knowledge, attitudes and beliefs. | |
| Notes | No power calculation was reported. The intervention was not delivered in full. Fifty‐three activities were planned but only 43 were implemented. Some elements were delivered to children but only outcomes for adults were measured. Expensive programme to implement, so additional service could explain any improvements rather than the collaboration itself. Overall risk of bias was high |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not clear |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Researchers likely to be aware of status of participants but this is unlikely to have influenced the results as measurement was through postal questionnaire. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Adequate |
| Selective reporting (reporting bias) | High risk | All available data appear to be presented |
| Other bias | High risk | Intervention was not delivered in full. Elements were delivered to children but only outcomes for adults were measured. Expensive programme to implement so additional service could explain any improvements rather than the collaboration itself. |
| Randomisation adequately described/protected? | High risk | Not randomised |
| Protection against contamination? | High risk | Assessed by authors "The process outcomes clearly showed some contamination of the comparison neighbourhoods, which is almost unavoidable because the comparison neighbourhoods were situated in the same city." |
| Follow‐up rate adequate? | Low risk | >60% and balanced across both arms |
| Reliable primary outcome measure? | High risk | Self‐reported behaviours and attitudes |
| Groups measured at baseline? | Low risk | Groups approximately balanced |
| Appropriate choice of controls (CBA studies only)? | Low risk | Yes |
| Contemporaneous data collection (CBA studies only)? | Low risk | Yes |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Lumley 2006.
| Methods | Cluster‐randomised trial of 3 years. Collaborating partners Lead agency: Local authority. Strategic involvement (policy making and service planning): Primary and secondary health care, health promotion, social services, environmental public protection services. Commissioning (implementing strategy taking account of resources available): No evidence of additional collaboration at this level. Operational (providing services directly): Primary and secondary health care, health promotion, social services, environmental public protection services, sport and leisure services, voluntary agencies. Set in Australia. |
|
| Participants | 16 out of 33 eligible local government authority areas in Victoria were matched into pairs. Women giving birth in these areas between 7 February 2000 and 5 August 2001 were sent postal questionnaires six months after the birth. Mothers whose infants had died were excluded. Questionnaires were returned by 6248 mothers in intervention states (out of 10,471 mailed, 61.6% response rate) and 5057 mothers in control states (out of 8722 mailed, 60.1% response rate). Age range: Intervention group (%) Control group (%) >20 yrs 1.6 1.1 20 ‐ 24 9.2 7.6 25 ‐ 29 27.8 26.3 30 ‐ 34 37.9 39.4 >34 21.5 23.8 Missing 2.0 1.8 |
|
| Interventions | The trial followed the PRISM (Program of Resources, Information and Support for Mothers) approach. A small steering committee of key stakeholders (local government, GPs, Maternal and Child Health Nurses, community and consumer organisations) was locally appointed to coordinate the implementation of the intervention, supported by a community development officer (CDO) in each intervention community. Ideas were shared between the intervention states through newsletters and other communications. Clinical audits were conducted. The intervention consisted of two components, one directed to primary care, the other to community services (local government and community agencies). Interventions were varied but included: Education and training programmes for maternal and child health nurses and general practitioners Local co‐ordination Mothers' Information Kits and vouchers Booklet developed by fathers for fathers Making environments more mother‐and‐baby friendly Befriending strategies for mothers through breaking down isolation and increasing opportunities to meet and make friends. |
|
| Outcomes | EPDS, a 10‐item scale for use in the postnatal period in which a score > 12 identifies probable depression SF36 physical and mental component scores at 6 months |
|
| Notes | Power calculations suggested 2337 participants were needed in each arm but this was adjusted upwards to account for cluster randomisation design. Aimed to invite 9600 women to participate in each arm and achieved this for the intervention arm but not for the control arm, despite prolonging the recruitment period. Additional resource requirements included employment and training of Community Development Officers and the production and distribution of information packs. Overall risk of bias was low. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Individual consent to participate was not requested so population (intervention group and control group) was not aware of the trial |
| Blinding (performance bias and detection bias) All outcomes | High risk | There was no blinding but outcome was not influenced by this. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participant flow diagram given |
| Selective reporting (reporting bias) | Low risk | Results presented in full |
| Other bias | Low risk | |
| Randomisation adequately described/protected? | Low risk | Local government authorities were stratified into rural and metropolitan areas and all possible pair matches were identified. From these possible pair matches in each stratum one set of eight pairs of areas was randomly selected. |
| Protection against contamination? | Low risk | Some in the comparison group received the information packs given to mothers in the intervention group but the relative impact of this would be small as the intervention included many other components. |
| Follow‐up rate adequate? | Low risk | Follow‐up rate of women > 60% and balanced in both arms. No clusters were lost from the study. |
| Reliable primary outcome measure? | Low risk | Validated measures used. |
| Groups measured at baseline? | Low risk | Sociodemographic profiles of intervention and control communities were presented (Table 1). |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | Low risk | OVERALL RISK OF BIAS WAS LOW |
Melle 2008.
| Methods | Controlled clinical trial started on 1 January 1997 with patient recruitment continuing to 31 December 2000. Patients diagnosed in intervention areas were followed up at 3 months, 1 year and 2 years after diagnosis. Collaborating partners Lead agency: Mental health. Strategic involvement (policy making and service planning): Secondary health care. Commissioning (implementing strategy taking account of resources available): Secondary health care and the Local Education Authority. Operational (providing services directly): Secondary health care, social services and the Local Education Authority. Intervention set in Norway and control areas in Norway and Denmark. |
|
| Participants | Patients aged 18‐65 years from four catchment areas (total population of 665,000) in Norway and Denmark, diagnosed with first‐episode psychosis and meeting a range of inclusion criteria including DSM‐IV diagnosis of psychotic disorder and IQ higher than 70. 380 people met the inclusion criteria (186 from Early Detection (ED) intervention area and 194 from the control areas). 281 agreed to participate (74% of all eligible patients, 141 in ED area, 140 in non‐ED area). Male 69% (intervention), 66% (control) Mean age at study entry 26.4 (intervention) 30.7 (control). |
|
| Interventions | Mental health clinicians, nurses, psychologists, GPs, school staff and social workers delivered the Early Detection Programme, which consisted of two approaches. Two specialist teams integrated into the ordinary outpatient units, providing rapid assessment of first episode patients, and raising awareness through visiting schools, working with GPs and the media. Community information campaigns about mental health directed at schools and the general population and general practitioners. Use was made of postcards, flyers, and car stickers and a booklet was sent to all the households. |
|
| Outcomes | Primary outcome was to reduce the duration of untreated first episode psychosis. Secondary outcomes included assessment of symptom levels through the PANSS scores and level of functioning through the Global Assessment of Functioning scores. |
|
| Notes | Power calculations suggested they required 100 participants in each group, which they achieved. Joa paper in Schizophrenia Bulletin 34, 466 ‐ 472, 2008 looked at position after information campaign had ceased. Authors note possibility of assessment bias as clinical ratings of PANSS interviews were not masked. Additional resources would be required to replicate this service. Overall risk of bias was medium |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not clear if participants were aware at recruitment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Clinical assessments for symptoms and function were not performed blind. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All available data appears to be presented. |
| Selective reporting (reporting bias) | High risk | There is full reporting of the outcomes they claimed to have measured but the study is due to run for up to 10 years. Data is reported for here only for the 2 year follow‐up. Joa paper reported on 2 cohorts1997‐2000 and 2000‐2004. |
| Other bias | High risk | Different reports of the same work have different age groups for the subjects (15 ‐ 65 in Johannessen, 16 ‐ 65 in Melle 2005, 18 ‐ 65 in Melle 2004). Also, there may be differences in disease severity between people identified early and people identified late with psychosis. Those identified early may have less severe underlying disease and be more likely to make good progress on treatment. |
| Randomisation adequately described/protected? | High risk | Not randomised |
| Protection against contamination? | Low risk | Intervention delivered in discrete geographical areas |
| Follow‐up rate adequate? | Low risk | Rate > 60% and balanced across both arms (Melle 2004 pg. 145 Table 2) |
| Reliable primary outcome measure? | Low risk | Stated in the Johannessen paper page 41, to reduce duration of untreated psychosis and therefore improve course and outcome of illness. |
| Groups measured at baseline? | Low risk | Groups approximately balanced |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS MEDIUM |
Rosen 2006.
| Methods | A cluster randomised controlled trial. Initially developed in the spring of 1999, and piloted in the 1999–2000 school year, the main study was run during the 2000–2001 school year, with the intervention delivered January to March 2001 and follow up two to three times to June 2001. In a concurrent subtrial, the families of children in the intervention preschools were individually randomised to home intervention group or home control group to test the impact of a home intervention. Collaborating partners Lead agency: Public health Strategic involvement (policy making and service planning): Local public health department, Ministry of Health, Hadassah Medical Organization, Ministry of Education, Effrata Teachers’ College, Preschool Department of the Municipality of Jerusalem. Commissioning (implementing strategy taking account of resources available): public health, teachers, preschools Operational (providing services directly): public health, teachers, preschools, doctors, educational experts, school nurses Set in Israel. |
|
| Participants | 40 preschools (20 intervention, 20 control), stratified by sector (religious and secular) in the state‐run public system of the Jerusalem region, including 1029 toilet‐trained children, aged 3and 4. 73,779 child days were yielded from observations on 6 baseline and 66 study days. In a concurrent subtrial, the 469 families of children in the intervention preschools were randomised to receive a home component (intervention group 237 families, controls 232 families). Preschool teachers likely to comply with the trial protocol were recommended by Ministry of Education officials (60% of eligible teachers). Nearly 90% of those invited agreed to join. |
|
| Interventions | The preschool educators were given lectures, printed materials and experiential learning. The children were encouraged to wash their hands for at least 10s by singing a handwashing song. They also had puppet theatre, a self‐reward system, games, posters, puzzles, a video and presentations by school nurses. Environmental interventions included providing each classroom with liquid soap dispensers, paper towel dispensers, cup racks, liquid soap, paper towels ( instead of cloth towels) and individual cups (instead of communal cups) over a three month period. Equipment was provided and fitted to ensure all intervention schools had the same facilities at the start of the intervention. Control preschools had no input until the close of the study period, when the full intervention was delivered on site and they were followed up once after the intervention. The home component consisted of a video, card and magnet sent home with the children in individually labelled packages about one month after the launch of the intervention. The home component control families received materials related to toothbrushing. |
|
| Outcomes | The primary outcome measure was illness absence from preschool. Absences were recorded via telephone using a structured questionnaire. They were classified as due to illness, for unknown reason or for reason unrelated to illness. Where the reason for absence was unknown parents were contacted to clarify the reason. Secondary outcomes were the overall percentage of children washing hands with soap before eating lunch and after bathroom use. Handwashing was measured from 3 post‐intervention visits to the 20 intervention preschools between January and June 2001 and 1 post‐intervention visit to the 20 control preschools in June 2001. In total there were 6 days collecting baseline measurements and 66 study days, yielding 73,779 child days of observation. Preschools were grouped into religious and secular subgroups within the intervention and control groups for comparative analysis. 88% of teachers and 95% of parents agreed to participate. No preschools dropped out from the study. Drop‐out of children was 0.9%, and 0.7% were lost to follow‐up. |
|
| Notes | The teachers invited to deliver the programme were identified by Ministry of Education officials. 60% of all eligible teachers were suggested, of which nearly 90% agreed to take part. Additional resources included lectures for the teachers, environmental equipment for the preschools, educational resource packs and puppet theatre visits. For the home intervention there were information packages. Teachers needed to spend time reinforcing hand hygiene messages with the children. Fidelity of the programme was assessed as good but imperfect. Contamination of the control group was minimal. Two intervention preschools were unexpectedly exposed to raw sewage during the study but results were unchanged following sensitivity analysis excluding these preschools. Overall risk of bias was high. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Parents and field research staff were not aware |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Educators, parents and field research staff were not informed of the study design but sometimes became aware that the programme was being run in a certain school. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data appears to be presented |
| Selective reporting (reporting bias) | High risk | The educators consistently under‐reported absenteeism. The research team conducted surveys which showed that 28% of absences reported by parents were not reported by educators. (ref) |
| Other bias | High risk | Potential selection bias as the teachers' were put forward by Ministry of Education officials rather than volunteering or all eligible teachers being directly approached. |
| Randomisation adequately described/protected? | Low risk | Used computer generated random numbers |
| Protection against contamination? | Low risk | Contamination assessed as minimal. Intervention delivered through discrete pre‐schools |
| Follow‐up rate adequate? | Low risk | No schools dropped out. 0.9% children dropped out and 0.7% were lost to follow‐up. |
| Reliable primary outcome measure? | High risk | It was hard to assess which absences were due to illness and educators consistently under‐reported absences when compared to parent's reports. |
| Groups measured at baseline? | Low risk | Groups approximately balanced. |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | N/A |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | N/A |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Smylie 2008.
| Methods | A controlled before after trial run in schools (3 study and 3 control) in February 2005 and evaluated one month following the end of the programme. Collaborating partners Lead agency: Health Strategic involvement (policy making and service planning): public health, education, community organisations Commissioning (implementing strategy taking account of resources available): public health, education, community organisations Operational (providing services directly): secondary care health professionals, local authorities (teachers, social services) community organisations, peers. Set in Canada |
|
| Participants | 427 Grade Nine students from six public schools participated in the programme, of which 240 (intervention = 124; control = 116) who had parental consent took part in the evaluation. Public schools in Windsor‐Essex County, Ontario were invited to participate and six principals responded. Three schools were designated as intervention and three as controls. Male 138 (42% intervention group, 74% control group) |
|
| Interventions | The intervention extended aspects of the basic sex education curriculum to cover areas in more depth. The in‐school classed‐ based learning consisted of a five‐session sexual health education programme covering anatomy and physiology of the reproductive system, STIs, HIV, building safe and healthy relationships and a teen panel discussion with personal stories from a teen mom, a teen dad and an HIV positive individual. The sessions were delivered by a public health nurse, a health promoter from the local AIDS Committee and a social worker from the local Sexual Assault Crisis Centre. A newsletter on teens interacting with parents about sexuality was distributed to parents and students and a workshop was run for parents to help them become more confident and approachable to their children in discussing matters of sexual health with them. Concerns and questions raised by the students through the course were incorporated directly into the programme and questions posted anonymously in a question box were answered daily through the programme. The programme was run in the intervention schools in February 2005 and evaluation completed by April 2005, following which the intervention was implemented in the control schools. Baseline was measured in the intervention and control groups at the same time and immediately before the start of the programme. |
|
| Outcomes | Outcomes were measured one month after the end of the programme. Follow‐up data was obtained on 117 intervention and 116 control group students. However, results for the intervention group are only presented for the 95 students (81%) who reported attending at least one of the five classes. There were no primary outcomes on behaviour change. Secondary outcomes known to be associated with behaviour change were measured including knowledge of STI and HIV prevention, effectiveness and correct use of contraceptives, risks of pregnancy (22 items) ; birth control attitudes (four items); contraceptive agency (four items); communication with others (six items); awareness of sexual response (three items); sex role attitudes (four items); sexual interaction values (five items). |
|
| Notes | The method of allocation of schools is not given. The total number of schools invited to participate is not given. 22 intervention group students responding to the follow‐up questionnaire reported not attending any class‐based sessions and their data are omitted from the results. However, the intervention included newsletter and workshop for the parents, which may have had an impact on those students who had not attended any class‐based sessions. The routine sex education curriculum is usually delivered by physical education teachers and varied in time spent and style of delivery, whereas the intervention programme was highly structured. Overall risk of bias high |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | No concealment |
| Blinding (performance bias and detection bias) All outcomes | Low risk | No blinding at assessment but questionnaires were completed by students themselves so lack of blinding is unlikely to have affected the results. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Results for all items appear to be presented. As 95 of the 117 intervention students responding at follow‐up (81%) indicated that they had attended at least one class (78 attended all five classes), follow‐up results are only presented for these 95, not the full 117, though their results were available. |
| Selective reporting (reporting bias) | High risk | Follow‐up data on 22 students in the intervention group were not reported as they had not attended any class‐based sessions. |
| Other bias | Low risk | Good overall follow‐up rate and high rate of attendance at classes. |
| Randomisation adequately described/protected? | High risk | Not randomised |
| Protection against contamination? | Low risk | Intervention delivered in selected schools. |
| Follow‐up rate adequate? | Low risk | Adequate |
| Reliable primary outcome measure? | High risk | No primary outcome measure was possible as it was seen to be inappropriate to include questions on actual student sexual behaviour so measures associated with behaviour change were used. |
| Groups measured at baseline? | Low risk | Yes |
| Appropriate choice of controls (CBA studies only)? | Low risk | Yes |
| Contemporaneous data collection (CBA studies only)? | Low risk | Yes |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Tucker 2006.
| Methods | Controlled before and after study. Data were collected at baseline (2001) and two years later (2003). Collaborating partners Lead agency: Local health board. Strategic involvement (policy making and service planning): Health Board. Commissioning (implementing strategy taking account of resources available): Health Board and the Local Education Authority. Operational (providing services directly): Health promotion, Local Education Authority and voluntary agencies. Set in UK. |
|
| Participants | Secondary school Year 3 and 4 students (average age 14 years and 6 months) from all 10 Healthy Respect SHARE schools in Lothian region (intervention schools) and 5 comparison schools in Grampian region, with standard sexual health education programmes. In 2001 of 5237 eligible children 2760 (80%) responded in Lothian and 1564 (87%) responded in Grampian. In 2003, of 5193 eligible children 2796 (83%) responded in Lothian and 1583 (86%) responded in Grampian. |
|
| Interventions | Ten schools implemented the Sexual Health And Relationships Education (SHARE) project developed as part of the Healthy Respect programme through a partnership between health, education and voluntary sector agencies in the Lothian Health Board region. The programme involved multidisciplinary staff training, planned multidisciplinary classroom delivery by teachers and nurses, alongside access to sexual health services at drop‐in centres for pupils located in or close to schools. | |
| Outcomes | Primary outcomes were self‐reported sexual intercourse at <16 years, and knowledge, attitudes and intentions about sexually transmitted diseases and condom use:
|
|
| Notes | Power calculations suggested they needed 2700 participants in the intervention schools and 1350 in the control schools, which they achieved. Service provision was noted as patchy. Drop‐in centres were available in Grampian, but were not linked to schools. Evaluation report notes that a relatively small proportion of young people in the intervention (Lothian) catchment (about 20%) were actually exposed to it. Although the paper's title refers to Healthy Respect, it only looks at one aspect of this demonstration project: SHARE (Sexual Health and Relationships Education). The authors concluded that these findings raise questions about the likely and achievable sexual health gains for teenagers from school‐based interventions. It appears that phase 2 of this project is currently being evaluated. See interim report: http://www.healthscotland.com/uploads/documents/8835‐Evaluation%20of%20HRPhase2Interim.pdf Exact costs unclear though additional costs for training and new drop‐in centres. Overall risk of bias was high |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | No concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | not applicable |
| Selective reporting (reporting bias) | Low risk | No published protocol but the paper is specific that changes were made following previous study and that pre‐defined questions were used in the evaluation. Only 5/17 potential comparison schools agreed to participate and these may have been more confident in their sexual education services. |
| Other bias | High risk | Authors note some limitations lack of classroom observation to explore the actual implementation of the new programme and possible selection bias arising from both volunteer schools in Lothian and low recruitment of schools in Grampian. |
| Randomisation adequately described/protected? | High risk | not applicable |
| Protection against contamination? | Low risk | Some practices may have leaked to control schools. |
| Follow‐up rate adequate? | Low risk | Follow‐up at population level. Different students surveyed at each round (high school years 3 and 4 in 2001 and again in 2003). Response rate in first survey (2001) was 83% (80% in intervention schools and 87% in control schools). Response rate to the second survey (2003) was 84% (83% in intervention schools and 86% in control schools). |
| Reliable primary outcome measure? | Low risk | As good as could be arranged for this topic. |
| Groups measured at baseline? | Low risk | Groups not balanced. |
| Appropriate choice of controls (CBA studies only)? | High risk | Through no fault of the study team. Potential for selection bias. Only 5/17 potential comparison schools agreed to participate and these may have been more confident in their sexual education services. Some difference in baseline socio‐demographic variables. Where differences were significant (e.g. accommodation, religion, parental education and employment) they were adjusted for in the multivariate models. |
| Contemporaneous data collection (CBA studies only)? | Low risk | No contemporaneous data collection is identified in the paper. |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Vickrey 2006.
| Methods | A cluster randomised controlled trial with enrolment from August 2001 to November 2002. Participants surveyed at baseline, 12 months and 18 month follow‐up. Collaborating partners Lead agency: Primary care. Strategic involvement (policy making and service planning): Primary health care, social services and voluntary agencies. Commissioning (implementing strategy taking account of resources available): Primary health care, social services and voluntary agencies. Operational (providing services directly): Primary health care, social services and voluntary agencies. Set in United States of America. |
|
| Participants | 18 primary care clinics in Southern California were randomly assigned to intervention (9) and usual care (9) clinics. From the 18 primary care clinics 1043 patients were contacted. 91 were ineligible and 544 declined to participate or failed to respond. 408 patients with dementia aged 65 or older and receiving Medicare were enrolled with their caregivers (aged 18 or over) (Intervention 238 dyads; Control 170 dyads). Caregivers' overall survey response rates 88% at 12 months and 82% at 18 months, excluding caregivers of 54 patients who died before the 12 month survey. Male 55.8% (intervention group) 54.1% (control group) Mean participants' age 80.1 years in intervention and control groups. Mean caregiver age 65.8 years in intervention group and 65.2 years in the control group. |
|
| Interventions | A steering committee with physicians, leaders from community agencies, a community caregiver and the investigators identified 23 existing dementia guideline recommendations as care goals. They also designed a structured assessment, algorithms linking care management actions to assessment results and they established inter‐organisation care coordination and referral protocols. Community agency care managers and healthcare care managers received the same formal training and used internet‐based care management software system for monitoring care planning. Monthly meetings were held to refine care coordination. Introduction of a disease management programme with active collaboration between health organisation and community agency staff providing support to patients with dementia and their carers. Care managers assessed patients at home and sent assessment summaries, problem list and selected recommendations to patients' primary care physicians and other designated providers. |
|
| Outcomes | PRIMARY OUTCOME WAS NOT RELEVANT: The mean percentage of per patient guideline recommendations to which care was adherent. Secondary health‐related outcomes reported were in‐study mortality, patient health‐related quality of life (HRQoL) and use of cholinesterase inhibitors. Caregiver health‐related quality of life was also measured. |
|
| Notes | Power calculations suggested they needed 438 dyads, which they did not achieve. It looks like significant additional resources were used in the intervention group, although it is unclear what costs were associated with this. Overall risk of bias was medium |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not concealed |
| Blinding (performance bias and detection bias) All outcomes | Low risk | As good as could be. Participants were blinded at baseline and not reminded of status at follow‐up. Data abstractors were blinded. Outcome assessment of medical record extraction also blind (unaware of participant clinic status or outcome measures). Carers were blinded for baseline survey. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Unclear |
| Selective reporting (reporting bias) | Low risk | No reason to assume selective reporting but protocol added retrospectively. See http://www.controlled‐trials.com/isrctn/pf/72577751 |
| Other bias | Low risk | The authors report that the study sample well‐educated, were predominantly white, had a usual source of care, and were not institutionalized. Therefore, the intervention may need to be modified for institutionalized patients and for those without a usual source of care and stable insurance. |
| Randomisation adequately described/protected? | Low risk | Computerised clinical level cluster randomisation ‐ "Within each health care organization, we paired clinics by patient volume; within each pair, we randomly assigned 1 clinic to the intervention and the other clinic to usual care using a computerized random‐number generator operated by a study statistician." |
| Protection against contamination? | Low risk | No reason to think contamination has occurred. |
| Follow‐up rate adequate? | Low risk | Rate > 80% and balanced across both arms. If deaths are excluded, follow‐up (i.e. survey response rates excluding patients who died) at 12 months = 88% and at 18 months = 82%. Medical record follow‐up was 97.5% . |
| Reliable primary outcome measure? | Low risk | Adequate measures of adherence to guideline with as many measures as possible (14/23) checked via patient record. Note: primary outcome is irrelevant as it is not a health outcome. Secondary outcomes relating to health are reliable. |
| Groups measured at baseline? | Low risk | Looks reasonably well balanced from Table 2. At baseline, intervention and usual care groups did not differ regarding patient and caregiver sociodemographic and clinical characteristics. |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS MEDIUM |
Woodfine 2011.
| Methods | A randomised controlled trial. Recruitment period not stated. Follow‐up 4 months and 12 months from randomisation (approx 3 and 11 months from intervention). Collaborating partners Lead agency: Public health Commissioning and strategic involvement: CHARISMA Study Group(Children’s Health in Asthma Research to Improve Status by Modifying Accommodation) ‐ Wrexham County Borough Council, Wrexham public health team (National Public Health Service Wales), Betsi Cadwalydr University Health Board and academia Operational: GPs identified families, Wrexham County Borough Council paid for and provided housing modifications. Family surveys and installation undertaken by Housing Officers. Set in UK |
|
| Participants | 192 children aged 5‐14 years living in Wrexham, UK, registered with one of 20 participating GP practices, who had received ≥3 prescriptions of corticosteroid inhalers in the preceding year and with written consent from parent/guardian to take part, complete questionnaires, and allow access to child’s medical records. Children with Cystic Fibrosis, or who were likely to move away within 12 months or whose home had a ventilation system already installed and adequate central heating at pre‐randomisation base line were all excluded. Elibigle: 445; recruited 195 (includes 3 siblings); 192 randomised: I = 96; C = 96. |
|
| Interventions | Installation of Vent‐Axia HR200XL ventilation system in the roof space and improvement/replacement of central heating system if required; all delivered by local government. Note: trial protocol indicates single room ventilation system if a single child but study report indicates that installation was in the roof space. Control: Nothing. Wait list (12 months) |
|
| Outcomes | Month 4 (3 months post intervention): 173 [90%] I = 87; C = 86 Month 12 (11 months post intervention): 169 [88%] I = 88; C = 89. Parent‐completed asthma‐specific, physical and psychosocial subscores of PedsQL (a validated quality of life measure for children), Childrens' mean days off School over the study period for all causes and for asthma. Cost effectiveness of intervention measured. Shift from ‘severe’ to ‘moderate’ asthma: I = 17% ; C =3% Mean cost of modifications: £1718 per child treated or £12,300 per child shifted from ‘severe’ to ‘moderate’. No significant difference in healthcare costs over 12 months between groups. ‘Bootstrapping’ gave an incremental cost‐effectiveness ratio (ICER) of £234 per point improvement on the 100‐point PedsQL™ asthma‐specific scale (95% CI: £140 to £590). ICER fell to £165 (95%CI: £84 to £424) for children with ‘severe’ asthma. |
|
| Notes | Study underpowered: power calculation required 200 children to detect a change in asthma‐specific QoL of ≥0.4 of asthma‐specific PedsQL. Study is a ventilation enhancement intervention and was not designed to explore the effect of local government and local health collaboration versus separate services. Thus it’s unclear how much the study can contribute to answering the review question. Significant additional resource required (see cost‐effectiveness data above). Treatment fidelity: Yes, other than installing ventilation in roof space rather than for single room as stated in protocol. Overall risk of bias: Low |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Remote allocation concealment using contemporaneous dynamic randomisation. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinded outcome assessment, although not possible to blind participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ≥88% at each time point |
| Selective reporting (reporting bias) | Low risk | Unselective reporting – as per registered protocol: ISRCTN13912429 |
| Other bias | Low risk | Randomisation and control children paired to avoid seasonal bias |
| Randomisation adequately described/protected? | Low risk | Stratified randomisation well described. |
| Protection against contamination? | Low risk | Unlikely control families would have installed ventilation. |
| Follow‐up rate adequate? | Low risk | Outcome data available for 88% at 12 months and balanced in both arms. |
| Reliable primary outcome measure? | Unclear risk | Subjective data but validated tool (PedsQL) |
| Groups measured at baseline? | Low risk | Groups stratified. Significant difference between groups for social functioning. |
| Appropriate choice of controls (CBA studies only)? | Unclear risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Unclear risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | Low risk | OVERALL RISK OF BIAS WAS LOW |
Young 2005.
| Methods | Controlled clinical trial with historical controls recruited in two blocks (November 1998 ‐July 1999 and May ‐ November 1999) and intervention patients recruited in later blocks (January ‐ July 2001 and May ‐ October 2001). Collaborating partners Lead agency: Health authority. Strategic involvement (policy making and service planning): Health planners, primary health care and social services. Commissioning (implementing strategy taking account of resources available): Health planners, primary health care and social services. Operational (providing services directly): Primary health care and social services. Set in UK. |
|
| Participants | Patients living in three of five local Primary Care Trust areas around Leeds who had presented as emergency admissions to elderly care departments with falls, confusion, incontinence or immobility and who were still in hospital after 7 days were recruited by research nurses, aiming to recruit 50 per elderly care department per month. 848 intervention patients and 800 controls were recruited, of which 483 and 490 patients respectively were assessed for the primary outcome at 12 months. 333 patients in the intervention group (39%) and 301 in the control group (38%) had died by 12 months. Male 33% (intervention group) and 30% (control group). Median age at baseline 85 (intervention group) and 83 (control group). |
|
| Interventions | Leeds Health Authority and Leeds City Council developed jointly a commissioning framework to provide support and rehabilitation to older patients following a health crisis at home or hospital admission, with care being given either at home or through short‐term care home placements. A joint care management team (multi‐agency, multidisciplinary) assessed need and purchased services from a Primary Care Trust based Intermediate Care team comprising nurses, therapists and social services staff. Control patients received usual care. |
|
| Outcomes | Primary outcome was independence at 6 months post recruitment measured by the Nottingham Extended Activities of Daily Living (NEADL) score six months after recruitment. Deaths and clinical outcomes, hospital and long‐term care use were also measured. |
|
| Notes | Power calculations suggested they required 600 analysable participants in each arm and they recruited 848 (intervention) and 800 (control) participants. Overall seems to be a reasonable evaluation study of a very poorly implemented service so little can be concluded about effectiveness. Only 29% intervention patients received the service and there was an apparent delay in service engagement as 44% of IC patients did not receive the service until more than 10 days after discharge. The authors suggest that close integration with other older peoples services, a factor considered important to successful intermediate care, has not been adequately achieved. Appears to be reorganisation of existing resource rather than utilising additional resources. Overall risk of bias was high |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | No concealment |
| Blinding (performance bias and detection bias) All outcomes | High risk | Historical control group. Statistician was independent of study group. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No incomplete outcome data |
| Selective reporting (reporting bias) | Low risk | Range of outcomes reported and no reason to suspect selectivity. |
| Other bias | Unclear risk | Contemporaneous controls would have been better but groups appear to be well matched. |
| Randomisation adequately described/protected? | High risk | Not applicable |
| Protection against contamination? | Low risk | Potential threat is introduction of Primary Care Trusts (PCTs) during the study but no reason to assume major differences. |
| Follow‐up rate adequate? | Low risk | Excellent follow‐up of 97% in intervention and 96% in control group. Note: Uses historical controls pre‐dating the introduction of intermediate care. |
| Reliable primary outcome measure? | Low risk | Well used Nottingham Extended Activities of Daily Living score. |
| Groups measured at baseline? | Low risk | Groups approximately balanced. Historical controls and establishment of PCTs took place during recruitment process. Groups look well matched (Table 1) and no reason to assume major differences. The potential impact of seasonality was controlled for by recruitment at similar times of year. |
| Appropriate choice of controls (CBA studies only)? | High risk | Not applicable |
| Contemporaneous data collection (CBA studies only)? | Low risk | Not applicable |
| IS THE STUDY AT LOW RISK OF BIAS? | High risk | OVERALL RISK OF BIAS WAS HIGH |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aagaard 2011 | Health outcome not measured in control group |
| Ahlner‐Elmqvist 2004 | Collaboration evident in both intervention and control groups |
| Anaya 2010 | No local government involvement |
| Andersson 2009 | No local government involvement |
| Applegate 1990 | No collaboration with local government; Correspondence with the authors clarified that the social worker was a member of the health care team |
| Arbeit 1992 | Heart Smart intervention versus no intervention. Does not explore the differential effects of local collaboration versus separate agency approach. Local health involvement unclear |
| Arean 2008 | No collaboration with local government; social worker is a member of the health care team |
| Arifeen 2009 | No local health involvement |
| Azad 2010 | No local government involvement |
| Batty 2010a | No local government involvement |
| Batty 2010b | No local government involvement |
| Beatty 2010 | No local government involvement |
| Beharie 2011 | No local health involvement |
| Bell 2008 | No local government involvement |
| Bellantonio 2008 | No local government involvement |
| Benger 2008 | No health outcomes |
| Blumenthal 2010 | No local government involvement |
| Boisson 2009 | No local government involvement |
| Bonner 2011 | International collaboration delivered locally |
| Boult 2001 | No collaboration with local government; social worker is a member of the health care team (Geriatric Evaluation and Management,GEM, model) |
| Bradford 2007 | No local government involvement. Collaboration was between health agencies |
| Breysse 2011 | Excluded study design – observational study |
| Brown 2009 | Excluded study design – observational study |
| Buhrer‐Skinner 2009 | Excluded study design – prospective study |
| Burns 2000 | No collaboration with local government; social worker a member of the health care team (Geriatric Evaluation and Management, GEM, model) |
| Buttner 2011 | Uncontrolled study |
| Byford 1999 | Intervention was enhanced single agency (social work) involvement. Level of partnership between health and local government cannot be determined |
| Campbell 2008 | No local government involvement |
| Carrasquilla 2001 | Excluded study design: before and after programme evaluation. |
| Carruth 2010 | No health outcomes data |
| Chan 2011 | no local government involvement; collaboration between local health and national goverment. |
| Chapman 2007 | Collaboration evident in both intervention and control groups |
| Chaytor 2011 | No local government involvement |
| Chen 2010 | No local government involvement |
| Chomitz 2010 | ITS without the minimum 3 points before and after intervention |
| Choudhry 2010 | No local health involvement: collaboration between University of Chicago and schools |
| Cross 2009 | No health outcome data |
| Dawes 2010 | No local government involvement |
| Deschodt 2011 | No local government involvement |
| Doyle 2010 | No local government involvement |
| Droes 2000 | Excluded study design: incomplete baseline data; unable to estimate drop‐out rates |
| Eagle 1991 | No collaboration with local government; social worker a member of the health care team |
| Edwards 2011 | Exclude study design – an observational study |
| Eggert 1991 | Collaboration evident in both intervention and control groups |
| Eisenmann 2011 | Study protocol only. [Not added to the Studies in progress list as study is CBA without a minimum of 2 study and 2 control sites] |
| Ell 2010 | No local government involvement |
| Eloniemi‐Sulkava 2009 | No health outcomes data |
| Evans 1995 | No collaboration with local government; social worker a member of the health care team |
| Farber 2009 | Excluded study design – observational study |
| Franzen‐Dahlin 2008 | No local government involvement |
| Freeman 2001 | Study design: no baseline data since intervention already ongoing |
| Gagnon 2011 | No local government involvement |
| Gatewood 2010 | No local government involvement |
| Gayton 1987 | No collaboration with local government; social worker a member of the health care team |
| Gilmer 2010 | Excluded study design ‐ retrospective cohort study |
| Guidotti 2009 | CBA without a minimum of 2 study and 2 control sites |
| Hadid 2010 | Excluded study design ‐ retrospective case‐control chart review |
| Harrington 2010 | No local government involvement |
| Harris 1998 | No collaboration with local government; social worker a member of the health care team |
| Helderman 1997 | No collaboration with local health |
| Hendriks 2005 | No collaboration with local government: multidisciplinary health team only |
| Hendriksen 1984 | Nurse may involve local services if required following assessment, but no evidence of joint working arrangements and shared objectives |
| Hiscock 2008 | No local government involvement |
| Hollar 2010 | No local health involvement |
| House of Commons 2010a | No local government involvement |
| House of Commons 2010b | No local government involvement |
| Howden‐Chapman 2011 | No local government involvement |
| Johnson 1991 | Collaboration evident in both intervention and control groups |
| Karppi 1995 | Collaboration is within health agencies |
| Kelaher 2009 | CBA without a minimum of 2 study and 2 control sites |
| Killaspy 2006 | Collaboration evident in both intervention and control groups |
| Kintner 2009 | Collaboration unclear |
| Kumpusalo 1996 | Excluded study design: no effective control group |
| Lambert 2010 | Unclear if local government involvement |
| Landi 2001 | Excluded study design: uncontrolled before and after study |
| Layne 2008 | Collaboration evident in both study arms |
| Lee 2004 | Follow‐up rate < 60% |
| Liddle 2011 | Collaboration between health and justice ‐ no local goverment involvement, |
| Lowell 2011 | No local government involvement |
| Luepker 1996 | No collaboration with health agency |
| Mackintosh 2006 | Level of partnership between health and local government cannot be determined |
| Magana‐Valladares 2011 | Excluded study design – not an intervention |
| Marcus 1998 | No collaboration with local government. Intervention is delivered by a national service |
| Markle‐Reid 2010 | No local government involvement |
| Matsubayashi 2011 | Excluded study design – cross sectional study |
| McConachie 2000 | Excluded study design: no effective control group |
| McDonald 2009 | Excluded study design – programme evaluation with no control group. |
| McHugo 2004 | No collaboration with local government; social worker is a member of the health care team |
| Meade 2010 | No local government involvement |
| Miller K 2011 | No local government involvement |
| Miller P 2011 | No health outcome data |
| Murphy 2010a | Collaboration between local health and national Government |
| Murphy 2010b | Excluded study design – uncontrolled study |
| Murray 1997 | Collaboration is evident in both intervention and control groups |
| Naglie 2002 | No collaboration with local government; social worker a member of the health care team |
| Norberg 2010 | Excluded study design – post‐hoc evaluation based on observational data |
| Norman 2007 | No health outcomes data |
| O'Brien 2010 | Excluded study design – cross sectional analysis |
| O'Farrell 2010 | Excluded study design – observational study |
| Oakes 2010 | Excluded study design – post‐hoc evaluation based on observational data |
| Pattanayak 2009 | No health outcomes data |
| Piarroux 2009 | No local government involvement |
| Post 2010 | Excluded study design – observational study |
| Puska 2009 | Excluded study design – observational study |
| Raja 2009 | Excluded study design – uncontrolled study |
| Rees 2006 | Excluded study design: CBA with only one control site |
| Reza‐Paul 2008 | No local government involvement |
| Richardson 2008 | No local government involvement |
| Richardson 2010 | No local government involvement |
| Rivera 2007 | Collaboration in intervention and control groups |
| Robbers 2008 | Excluded study design – uncontrolled study |
| Rog 2004 | Study outcomes were not health‐related |
| Rosenblum 2005 | No local government involvement |
| Rosenheck 1999 | Study outcomes not health‐related |
| Rutter 2004 | Collaboration evident in both intervention and control groups |
| Salihu 2011 | Excluded study design – CBA without minimum of 2 study and 2 control arms |
| Scholten 1999 | Level of partnership between health and local government cannot be determined |
| Selassie 2011 | Excluded study design – cross sectional survey |
| Sexton 2011 | No local health involvement |
| Shriqui 2008 | No local government involvement |
| Singh 2009 | No local government involvement |
| Smith 2010 | No local government involvement |
| Sommers 2000 | No collaboration with local government; social worker a member of the health care team |
| Stallard 2008 | No local health involvement |
| Sytema 2007 | No collaboration with local government; social worker a member of the health care team |
| Teufel‐Shone 2005 | Excluded study design: uncontrolled before and after study. |
| Thibault 2010 | No local government involvement |
| Thornicroft 1998 | Collaboration evident in both intervention and control groups |
| Tinetti 1994 | No collaboration with local government in intervention group |
| Tourigny 2004 | Follow‐up rate < 60% |
| Tucker 2008 | Exclude study design ‐ no intervention |
| Tucker 2011 | Excluded study design, CBA without a minimum of 2 intervention and 2 control sites |
| Van Assema 1994 | Excluded study design ‐ CBA without a minimum of 2 intervention and 2 control sites |
| Weingarten 1985 | No collaboration with local government; social worker a member of the health care team |
| Wierdsma 2007 | No health outcomes: service use only |
| Williams 2006 | Excluded study design ‐ uncontrolled study |
| Williams 2011 | Excluded study design ‐ uncontrolled study |
| Zayas 2004 | Follow‐up response rate <60% |
Characteristics of ongoing studies [ordered by study ID]
Wall 2009.
| Trial name or title | Well London |
| Methods | Cluster RCT |
| Participants | 20 matched pairs of intervention and control communities |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes | ISRCTN68175121. Scheduled to complete in December 2012 Protocol: Wall M, Hayes R, Moore D, Petticrew M, Clow A, Schmidt E, Draper A, Lock K, Lynch R, Renton A. Evaluation of community level interventions to address social and structural determinants of health: a cluster randomised controlled trial. BMC Public Health. 2009 Jun 28;9:207 |
Differences between protocol and review
In the original review 24 databases were searched. For the update three databases (Ageline, ChildData and CommunityWISE) were not searched as institutional access had been terminated and the databases were not available to the review team.
The team had planned to search the Internet using Google Scholar, however it was decided searching relevant websites was more appropriate.
The protocol indicated that when no primary endpoint was identified by the study authors, the effect sizes would be ranked and the median selected. However, In order to investigate long‐lasting effects it was decided to use the longest follow‐up reported (where attrition did not exceed 40%).
The data analysis section of the protocol indicated that dichotomous outcomes would be presented as odds ratios and risk differences. To aid clarity it was decided that relative risks were a more intuitive measure so they were used throughout.
Where multiple outcomes from the same outcome category were reported from a single study, the stated primary outcome was used. If a primary outcome was not stated, the outcome used for the sample size calculation was selected. If the outcome used for the sample size calculation was not stated, the first outcome reported in the abstract or, failing that, the results section was selected for reporting.
A Summary of findings table was completed. It was decided that the inclusion of evidence quality for each group of outcomes (based on the GRADE approach) was not feasible given the heterogeneity and range of study designs. It was clear, however, that if it had been feasible to do this the quality of evidence would have been ranked low or very low for each outcome group.
Contributions of authors
The searches were performed by MKM and FMM. Papers were screened and data extracted by SLH, MKM, FMM, ALW and MJK. MJK provided statistical expertise and conducted the data analysis. The review was written by SLH, MKM, ALW, MJK and FMM.
Sources of support
Internal sources
-
Welsh Government & Abertawe Bro Morgannwg University Health Board, UK, UK.
Funding provided to SLH time to support and update the review.
External sources
-
National Institute for Health Research, Cochrane Review Incentive Scheme, UK., UK.
Funding provided to assist in completion of review update
-
The Victorian Health Promotion Foundation (VicHealth), Australia.
VicHealth provides funding to support the editorial process for all Cochrane Public Health Group reviews
Declarations of interest
None known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Bertelsen 2008 {published data only}
- Bertelsen M, Jeppesen P, Petersen L, Thorup A, Ohlenschlaeger J, Quach P, et al. Five‐year follow‐up of a randomized multicenter trial of intensive early intervention vs. standard treatment for patients with a first episode of psychotic illness. Archives of General Psychiatry 2008;65(7):71. [DOI] [PubMed] [Google Scholar]
- Jørgensen P, Nordentoft M, Abel MB, Gouliaev G, Jeppesen P, Kassow P. Early detection and assertive community treatment of young psychotics: the Opus study. Rationale and design of the trial. Social Psychiatry and Psychiatric Epidemiology 2000;35(7):283‐7. [Protocol published] [DOI] [PubMed] [Google Scholar]
- Nordentoft M, Jeppesen P, Abel M, Kassow P, Petersen L, Thorup A, et al. OPUS study: suicidal behaviour, suicidal ideation and hopelessness among patients with first‐episode psychosis. One‐year follow‐up of a randomised controlled trial. British Journal of Psychiatry Supplement 2002;43(s):98‐106. [DOI] [PubMed] [Google Scholar]
- Petersen L, Jeppesen P, Thorup A, Abel MB, Øhlenschlaeger J, Christensen TØ, et al. A randomised multicentre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. BMJ 2005;331(7524):1065.771. [10.1136/bmj.38565.415000.E01 (published 6 September 2005)] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruzzese 2006 {published data only}
- Bruzzese J, Evans D, Wiesemann S, Pinkett‐Heller M, Levison M, Du Y, et al. Using school staff to establish a preventive network of care to improve elementary school students' control of asthma. Journal of School Health 2006;76(6):307‐12. [DOI] [PubMed] [Google Scholar]
Challis 2002 {published data only}
- Brown P, Challis D, Abendorff R. The work of a community mental health team for the elderly: referrals, caseloads, contact history and outcomes. International Journal of Geriatric Psychiatry 1996;11:29‐39. [Google Scholar]
- Challis D, Abendorff R, Brown P, Chesterman J, Hughes J. Care management, dementia care and specialist mental health services: an evaluation. International Journal of Geriatric Psychiatry 2002;17(4):315‐25. [DOI] [PubMed] [Google Scholar]
Cooper 1975 {published data only}
- Cooper B, Depla C, Harwin BG, Shepherd M, Cooper B, Depla C, et al. An experiment in community mental health care. Lancet 1974;2(7893):1356‐8. [DOI] [PubMed] [Google Scholar]
- Cooper B, Harwin BG, Depla C, Shepherd M. Mental health care in the community: an evaluative study. Mental health care in the community: an evaluative study. 1975;5(4):372‐80. [DOI] [PubMed] [Google Scholar]
Coppins 2011 {published data only}
- Coppins DF, Margetts BM, Fa JL, Brown M, Garrett F, Huelin S. Effectiveness of a multi‐disciplinary family‐based programme for treating childhood obesity (The Family Project). European Journal of Clinical Nutrition 2011;65(8):903‐9. [DOI] [PubMed] [Google Scholar]
Florence 2011 {published data only}
- Florence C, Shepherd J, Brennan I, Simon T. Effectiveness of anonymised information sharing and use inhealth service, police, and local government partnership forpreventing violence related injury: experimental study andtime series analysis. BMJ 2011;342:d3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hultberg 2005 {published data only}
- Hultberg E, Lönnroth K, Allebeck P. Interdisciplinary collaboration between primary care, social insurance and social services in the rehabilitation of people with musculoskeletal disorder: Effects on self‐rated health and physical performance. Journal of Interprofessional Care 2005;19(2):115‐24. [DOI] [PubMed] [Google Scholar]
- Hultberg EL, Lönnroth K, Allebeck P. Effects of a co‐financed interdisciplinary collaboration model in primary health care on service utilisation among patients with musculoskeletal disorders. Work 2007;28(3):239‐47. [PubMed] [Google Scholar]
Kloek 2006 {published data only}
- Kloek GC, Lenthe FJ, Meertens YMG, Koelen MA, Mackenbach JP. Process evaluation of a Dutch intervention to improve health related behaviour in deprived neighbourhoods. Sozial‐ und Praventivmedizin 2006;51:259‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloek GC, Lenthe FJ, Nierop PW, Koelen MA, Mackenbach JP. Impact evaluation of a Dutch community intervention to improve health‐related behaviour in deprived neighbourhoods. Health & Place 2006;12(4):665‐77. [DOI] [PubMed] [Google Scholar]
Lumley 2006 {published data only}
- Lumley J, Small R, Brown S, Watson L, Gunn J, Mitchell C, Dawson W. PRISM (Program of Resources, Information and Support for Mothers) Protocol for a community‐randomised trial [ISRCTN03464021]. BMC Public Health 2003;20(3):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley J, Watson L, Small R, Brown S, Mitchell C, Gunn J. PRISM (Program of Resources, Information and Support for Mothers): a community‐randomised trial to reduce depression and improve women's physical health six months after birth [ISRCTN03464021]. BMC Public Health 2006;6(37):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley J, Watson L, Small R, Brown S, Mitchell C, Gunn J. PRISM (Program of Resources, Information and Support for Mothers): a community‐randomised trial to reduce depression and improve women's physical health six months after birth. BMC Public Health 2003;20(3):1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Melle 2008 {published data only}
- Joa I, Johannessen JO, Auestad B, Friis S, McGlashan T, Melle I, et al. The key to reducing duration of untreated first psychosis: information campaigns. Schizophrenia Bulletin 2008;34(3):466‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johannessen JO, McGlashan TH, Larsen TK, Horneland M, Joa I, Mardal S, et al. Early detection strategies for untreated first‐episode psychosis. Schizophrenia Research 2001;51(1):39‐46. [DOI] [PubMed] [Google Scholar]
- Larsen TK, McGlashan TH, Johannessen JO, Friis S, Guldberg C, Haahr U, et al. Shortened duration of untreated first episode of psychosis: changes in patient characteristics at treatment. American Journal of Psychiatry 2001;158(11):1917‐9. [DOI] [PubMed] [Google Scholar]
- Melle I, Larsen TK, Haahr U, Friis S, Johannesen JO, Opjordsmoen S, et al. Prevention of negative symptom psychopathologies in first‐episode schizophrenia: two‐year effects of reducing the duration of untreated psychosis. Archives of General Psychiatry 2008;65(6):634‐40. [DOI] [PubMed] [Google Scholar]
- Melle I, Larsen TK, Haahr U, Friis S, Johannessen JO, Opjordsmoen S, et al. Reducing the duration of untreated first‐episode psychosis: effects on clinical presentation. Archives of General Psychiatry 2004;61(2):143‐50. [DOI] [PubMed] [Google Scholar]
Rosen 2006 {published data only}
- Rosen L. A controlled trial to assess the effect of a health promotionintervention on hygiene behavior and absenteeism in Jerusalem preschools. Dissertation: Hebrew University 2004.
- Rosen L. Can a handwashing intervention make a difference? Results from a randomized controlled trial in Jerusalem preschools. Prevention Medicine 2006;42(1):27‐32. [DOI] [PubMed] [Google Scholar]
- Rosen L, Manor O, Engelhard D, Zucker D. Design of the Jerusalem Handwashing Study: meeting the challenges of a preschool‐based public health intervention trial. Clinical Trials 2006;3(4):376‐84 Erratum in: Clin Trials. 2007;4(4):475. [DOI] [PubMed] [Google Scholar]
- Rosen L, Zucker D, Brody D, Engelhard D, Manor O. The effect of a handwashing intervention on preschool educator beliefs, attitudes, knowledge and self‐efficacy. Health Education Research 2009;24(4):686‐98. [DOI] [PubMed] [Google Scholar]
- Rosen L, Zucker D, Brody D, Engelhard D, Meir M, Manor O. Enabling hygienic behavior among preschoolers: improving environmental conditions through a multifaceted intervention. American Journal of Health Promotion 2011;25(4):248‐56. [DOI] [PubMed] [Google Scholar]
Smylie 2008 {published data only}
- Smylie L, Maticka‐Tyndale E, Boyd DE‐MA, Smylie LSC. Evaluation of a school‐based sex education programme delivered to Grade Nine students in Canada. Sex Education 2008;8(1):25‐46. [Google Scholar]
Tucker 2006 {published data only}
- Scottish Executive. External Evaluation of Healthy Respect: Full Report. Edinburgh: Scottish Executive, 2005. [Google Scholar]
- Tucker JS, Fitzmaurice AE, Imamura M, Penfold S, Penney GC, Teijlingen E, et al. The effect of the national demonstration project Healthy Respect on teenage sexual health behaviour. European Journal of Public Health 2007;17(1):33‐41. [DOI] [PubMed] [Google Scholar]
Vickrey 2006 {published data only}
- Chodosh J, Pearson ML, Connor KI, Vassar SD, Kaisey M, Lee ML, Vickrey BG. A dementia care management intervention: which components improve quality?. The American Journal of Managed Care 2012;18:85‐94. [PubMed] [Google Scholar]
- Kaisey M, Mittman B, Pearson M, Connor KI, Chodosh J, Vassar SD, et al. Predictors of acceptance of offered care management intervention services in a quality improvement trial for dementia. International Journal of Geriatric Psychiatry 2011;20:2830. [DOI] [PubMed] [Google Scholar]
- Vickrey BG, Mittman BS, Connor KI, Pearson ML, Penna RD, Ganiats TG, et al. The effect of a disease management intervention on quality and outcomes of dementia care: a randomized, controlled trial. Annals of Internal Medicine 2006;145(10):713‐26. [DOI] [PubMed] [Google Scholar]
Woodfine 2011 {published data only}
- Woodfine L, Neal RD, Bruce N, Edwards RT, Link P, Mullock L, et al. Enhancing ventilation in homes of children with asthma: Pragmatic randomised controlled trial. British Journal of General Practice 2011;61(592):e724‐32. [Edwards RT, Neal RD, Linck P, Bruce N, Mullock L, Nethans N, et al. 2011. Enhancing ventilation in homes of children with asthma: Cost‐effectiveness study alongside randomised controlled trial. British Journal of General Practice, 61, (592) e733‐41] [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 2005 {published data only}
- Young JB, Robinson M, Chell S, Sanderson D, Chaplin S, Burns E, et al. A whole system study of intermediate care services for older people. Age & Ageing 2005;34(6):577‐83. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aagaard 2011 {published data only}
- Aagaard J, Muller‐Nielsen K. Clinical outcome of assertive community treatment (ACT) in a rural area in Denmark: A case‐control study with a 2‐year follow‐up. Nordic Journal of Psychiatry 2011;65(5):299‐305. [DOI] [PubMed] [Google Scholar]
Ahlner‐Elmqvist 2004 {published data only}
- Ahlner‐Elmqvist M, Jordhoy MS, Jannert M, Fayers P, Kaasa S. Place of Death: hospital‐based advanced home care versus conventional care. A prospective study in palliative cancer care. Palliative Medicine 2004 Oct;18(7):585‐93. [DOI] [PubMed] [Google Scholar]
Anaya 2010 {published data only}
- Anaya HF, Feld J, Hoang T, Knapp H, Asch S. Implementing an HIV rapid testing intervention for homeless veterans in shelter settings within Los Angeles county. Journal of the International Association of Physicians in AIDS Care 2010;9(1):47. [Google Scholar]
Andersson 2009 {published data only}
- Andersson N, Cockcroft A, Ansari NM, Omer K, Baloch M, Foster AH, et al. Evidence‐based discussion increases childhood vaccination uptake: a randomised cluster controlled trial of knowledge translation in Pakistan. BMC International Health and Human Rights 2009;1(9):S1‐S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Applegate 1990 {published data only}
- Applegate WB. A randomized, controlled trial of a geriatric assessment unit in a community rehabilitation hospital. New England Journal of Medicine 1990;322(22):1572‐8. [DOI] [PubMed] [Google Scholar]
Arbeit 1992 {published data only}
- Arbeit ML, Johnson CC, Mott DS, Harsha DW, Nicklas TA, Webber LS, et al. The Heart Smart cardiovascular school health promotion: behaviour correlates of risk factor change. Preventine Medicine 1992;21(1):18‐32. [DOI] [PubMed] [Google Scholar]
Arean 2008 {published data only}
- Arean PA, Ayalon L, Jin CS, McCulloch CE, Linkins K, Chen HT, et al. Integrated speciality mental health care among older minorities improves access but not outcomes: results of the PRISMe study. International Journey of Geriatric Psychiatry 2008;23(10):1086‐92. [DOI] [PubMed] [Google Scholar]
Arifeen 2009 {published data only}
- Arifeen SE, Hoque DM, Akter T, Rahman M, Hoque ME, Begum K, et al. Effect of the Integrated Management of Childhood Illness strategy on childhood mortality and nutrition in a rural area in Bangladesh a cluster randomised trial. Lancet 2009;374(9687):393‐403. [DOI] [PubMed] [Google Scholar]
Azad 2010 {published data only}
- Azad K, Barnett S, Banerjee B, Shaha S, Khan K, Rego AR, et al. Effect of scaling up women's groups on birth outcomes in three rural districts in Bangladesh: a cluster‐randomised controlled trial. Lancet 2010;375(9721):1193‐202. [DOI] [PubMed] [Google Scholar]
Batty 2010a {published data only}
- Batty E, Beatty C, Foden M, Lawless P, Pearson S, Wilson I. Improving outcomes for people in deprived neighbourhoods: evidence from the New Deal for Communities programme: the New Deal for Communities national evaluation: final report: volume 4. Great Britain. Department for Communities and Local Government 2010;4:1‐97. [Google Scholar]
Batty 2010b {published data only}
- Batty E, Beatty C, Foden M, Lawless P, Pearson S, Wilson I. The New Deal for Communities experience: a final assessment: the New Deal for Communities evaluation: final report: volume 7. Great Britain. Department for Communities and Local Government 2010; Vol. 7.
Beatty 2010 {published data only}
- Beatty T, Foden M, Lawless P, Wilson I. Area‐based regeneration partnerships and the role of central government: the New Deal for Communities programme in England. Policy and Politics 2010;38(2):235‐251. [Google Scholar]
Beharie 2011 {published data only}
- Beharie N, Kalogerogiannis K, McKay M, Paulino A, Miranda A, Rivera‐Rodriguez A, et al. The HOPE Family Project: A family‐based group intervention to reduce the impact of homelessness on HIV/STI and drug risk behaviors. Social Work With Groups 2011;34(1):61‐78. [Google Scholar]
Bell 2008 {published data only}
- Bell CC. Building protective factors to offset sexually risky behaviors among black youths: A randomized control trial. Journal of the National Medical Association 2008;100(8):936‐944. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bellantonio 2008 {published data only}
- Bellantonio S, Kenny AM, Fortinsky RH, Kleppinger A, Robison J, Gruman C, et al. Efficacy of a geriatrics team intervention for residents in dementia‐specific assisted living facilities: effect on unanticipated transitions. Journal of the American Geriatrics Society 2008;56(3):523‐8. [DOI] [PubMed] [Google Scholar]
Benger 2008 {published data only}
- Benger JC. Could inter‐agency working reduce emergency department attendances due to alcohol consumption?. Emergency Medicine Journal 2008;25(6):331‐4. [DOI] [PubMed] [Google Scholar]
Blumenthal 2010 {published data only}
- Blumenthal DS, Smith SA, Majett CD, Alema‐Mensah E. A trial of 3 interventions to promote colorectal cancer screening in African Americans. Cancer 2010;116(4):922‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boisson 2009 {published data only}
- Boisson S, Schmidt WP, Berhanu T, Gezahegn H, Clasen T. Randomized controlled trial in rural Ethiopia to assess a portable water treatment device. Environmental Science & Technology 2009;43(15):5934‐9.. [DOI] [PubMed] [Google Scholar]
Bonner 2011 {published data only}
- Bonner K, Mwita A, McElroy PD, Omari S, Mzava A, Lengeler C, et al. Design, implementation and evaluation of a national campaign to distribute nine million free LLINs to children under five years of age in Tanzania. Malaria Journal 2011;31(10):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boult 2001 {published data only}
- Boult C, Boult LB, Morishita L, Dowd B, Kane RL, Urdangarin CF. A randomized clinical trial of outpatient geriatric evaluation and management. Journal of the American Geriatric Society 2001;49(4):351‐9. [DOI] [PubMed] [Google Scholar]
Bradford 2007 {published data only}
- Bradford JB. The promise of outreach for engaging and retaining out‐of‐care persons in HIV medical care. AIDS Patient Care and STDs 2007;21 Suppl 1:85‐91. [DOI] [PubMed] [Google Scholar]
Breysse 2011 {published data only}
- Breysse J, Jacobs DE, Weber W, Dixon S, Kawecki C, Aceti S, Lopez J. Health Outcomes and Green Renovation of Affordable Housing. Public Health Reports 2011;2(126):64‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2009 {published data only}
- Brown DM, Tammineni SK, Brown DM, Tammineni SK. Managing sales of beverages in schools to preserve profits and improve children's nutrition intake in 15 Mississippi schools. Journal of the American Dietetic Association 2009;109(12):2036‐42. [DOI] [PubMed] [Google Scholar]
Buhrer‐Skinner 2009 {published data only}
- Buhrer‐Skinner M, Muller R, Menon A, Gordon R. Novel approach to an effective community‐based chlamydia screening program within the routine operation of a primary healthcare service. Sexual Health 2009;6(1):51‐6. [DOI] [PubMed] [Google Scholar]
Burns 2000 {published data only}
- Burns BJ, Farmer EMZ, Angold A, Costello EJ, Behar L. A randomized trial of case management for youths with serious emotional disturbance. Journal of Clinical Child Psychology 1996;25(4):476‐86. [Google Scholar]
Buttner 2011 {published data only}
- Büttner P, Rücker S, Petermann U, Petermann F. Youth welfare and therapy: effects of youth welfare alone and youth welfare combined with additional therapy. Praxis der Kinderpsychologie und Kinderpsychiatrie 2011;60(3):224‐38. [DOI] [PubMed] [Google Scholar]
Byford 1999 {published data only}
- Byford S, Harrington R, Torgerson D, Kerfoot M, Dyer E, Harrington V. Cost effectiveness analysis of a home‐based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. The British Journal of Psychiatry 1999;174:56‐62. [DOI] [PubMed] [Google Scholar]
Campbell 2008 {published data only}
- Campbell K, Hesketh K, Crawford D, Salmon J, Ball K, McCallum Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: cluster‐randomised controlled trial. BMC Public Health 2008;8(31):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carrasquilla 2001 {published data only}
- Carrasquilla G. An ecosystem approach to malaria control in an urban setting. Cadernos de Saude Publica 2001;17 Suppl:171‐9. [DOI] [PubMed] [Google Scholar]
Carruth 2010 {published data only}
- Carruth AK, Pryor S, Cormier C, Bateman A, Matzke B, Gilmore K. Evaluation of a school‐based train‐the‐trainer intervention program to teach first aid and risk reduction among high school students. Journal of School Health 2010;80(9):453‐60. [DOI] [PubMed] [Google Scholar]
Chan 2011 {published data only}
- Chan WS, Whitford DL, Conroy R, Gibney D, Hollywood B. A multidisciplinary primary care team consultation in a socio‐economically deprived community: An exploratory randomised controlled trial. BMC health services research 2011;11:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chapman 2007 {published data only}
- Chapman DG, Toseland RW. Effectiveness of advanced illness care teams for nursing home residents with dementia. Social Work 2007;52(4):321‐9. [DOI] [PubMed] [Google Scholar]
Chaytor 2011 {published data only}
- Chaytor N, Ciechanowski P, Miller JW, Fraser R, Russo J, Unutzer J, Gilliam F. Long‐term outcomes from the PEARLS randomized trial for the treatment of depression in patients with epilepsy. Epilepsy and Behavior 2011;20(3):545‐9. [DOI] [PubMed] [Google Scholar]
Chen 2010 {published data only}
- Chen LK, Chen YM, Hwang SJ, Peng LN, Lin MH, Lee WJ, Lee CH, Longitudinal Older Veterans Study Group. Effectiveness of community hospital‐based post‐acute care on functional recovery and 12‐month mortality in older patients: A prospective cohort study. Annals of Medicine 2010;42(8):630‐6. [DOI] [PubMed] [Google Scholar]
Chomitz 2010 {published data only}
- Chomitz VR, McGowan RJ, Wendel JM, Williams SA, Cabral HJ, King SE, et al. Healthy Living Cambridge Kids: A community‐based participatory effort to promote healthy weight and fitness. Obesity 2010;18(1):S45‐S53. [DOI] [PubMed] [Google Scholar]
Choudhry 2010 {published data only}
- Choudhry SS. Power‐up: A collaborative after school and family pilot study to prevent obesity. Progress in Community Health Partnerships. Research, Education, and Action 2011;5(4):363‐73. [PMC free article] [PubMed] [Google Scholar]
Cross 2009 {published data only}
- Cross JE, Dickmann E, Newman‐Gonchar R, Fagan JM. Using mixed‐method design and network analysis to measure development of interagency collaboration. American Journal of Evaluation 2009;30(3):310‐29. [Google Scholar]
Dawes 2010 {published data only}
- Dawes H. Long‐term Individual Fitness Enablement (LIFE) study. Oxford: Oxford Brookes University, 2010.
Deschodt 2011 {published data only}
- Deschodt M, Braes T, Broos P, Sermon A, Boonen S, Flamaing J, Milisen K. Effect of an inpatient geriatric consultation team on functional outcome, mortality, institutionalization, and readmission rate in older adults with hip fracture: a controlled trial. Journal of the American Geriatrics Society 2011;59(7):1299‐308. [DOI] [PubMed] [Google Scholar]
Doyle 2010 {published data only}
- Doyle AM, Ross DA, Maganja K, Baisley K, Masesa C, Andreasen A, et al. Long‐Term Biological and Behavioural Impact of an Adolescent Sexual Health Intervention in Tanzania: Follow‐up Survey of the Community‐Based MEMA kwa Vijana Trial. PLoS Medicine 2010;7(6):e1000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
Droes 2000 {published data only}
- Droies RM, Breebaart E, Ettema TP, Tilburg W, Mellenbergh GJ. Effect of integrated family support versus day care only on behaviour and mood of patients with dementia. International Psychogeriatrics 2000 Mar;12(1):99‐115. [DOI] [PubMed] [Google Scholar]
Eagle 1991 {published data only}
- Eagle DJ, Guyatt GH, Patterson C, Turpie I, Sackett B, Singer J. Effectiveness of a geriatric day hospital. Canadian Medical Association Journal 1991;144(6):699‐704. [PMC free article] [PubMed] [Google Scholar]
Edwards 2011 {published data only}
- Edwards B, Gray M, Wise S, Hayes A, Katz I, Muir K, Patulny R. Early impacts of Communities for Children on children and families: findings from a quasi‐experimental cohort study. Journal of Epidemiology and Community Health 2011;65(10):909‐14. [DOI] [PubMed] [Google Scholar]
Eggert 1991 {published data only}
- Eggert GM, Zimmer JG, Hall WJ, Friedman B. Case management: a randomized controlled study comparing a neighbourhood team and a centralized individual model. Health Services Research 1991;26:471‐507. [PMC free article] [PubMed] [Google Scholar]
Eisenmann 2011 {published data only}
- Eisenmann JC, Alaimo K, Pfeiffer K, Paek HJ, Carlson JJ, Hayes H, et al. Project FIT: rationale, design and baseline characteristics of a school‐ and community‐based intervention to address physical activity and healthy eating among low‐income elementary school children. BMC public health 2011;29(11):607. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ell 2010 {published data only}
- Ell KK. Collaborative care management of major depression among low‐income, predominantly hispanic subjects with diabetes: A randomized controlled trial. Diabetes Care 2010;33(4):706‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eloniemi‐Sulkava 2009 {published data only}
- Eloniemi‐Sulkava U, Saarenheimo M, Laakkonen ML, Pietilä M, Savikko N, Kautiainen H, et al. Family care as collaboration: Effectiveness of a multicomponent support program for elderly couples with dementia. Randomized controlled intervention study. Journal of the American Geriatrics Society 2009;57(12):2200‐8. [DOI] [PubMed] [Google Scholar]
Evans 1995 {published data only}
- Evans LK, Yurkow J, Siegler EL. The CARE programnme: a nurse‐managed collaborative outpatient programme to improve function of frail older people. Collaborative Assessment and Rehabilitation for Elders. Journal of the American Geriatrics Society 1995;43(10):1155‐60. [PubMed] [Google Scholar]
Farber 2009 {published data only}
- Farber MLZ. Parent Mentoring and Child Anticipatory Guidance with Latino and African American Families. Health & Social Work 2009;34(3):179‐89. [DOI] [PubMed] [Google Scholar]
Franzen‐Dahlin 2008 {published data only}
- Franzén‐Dahlin A, Larson J, Murray V, Wredling R, Billing E. A randomized controlled trial evaluating the effect of a support and education programme for spouses of people affected by stroke. Clinical Rehabilitation 2008;22(8):722‐30. [DOI] [PubMed] [Google Scholar]
Freeman 2001 {published data only}
- Freeman R, Oliver M, Bunting G, Kirk J, Saunderson W. Addressing children's oral health inequalities in Northern Ireland: a research‐practice‐community partnership initiative. Public Health Reports 2001;116(6):617‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gagnon 2011 {published data only}
- Gagnon C, Brown C, Couture C, Kamga‐Ngande CN, Hivert MF, Baillargeon JP, et al. A cost‐effective moderate‐intensity interdisciplinary weight‐management programme for individuals with prediabetes. Diabetes & Metabolism 2011;37(5):410‐8. [DOI] [PubMed] [Google Scholar]
Gatewood 2010 {published data only}
- Gatewood SA. Expansion of clinical pharmacy services in an underserved population through an academic‐community partnership. Journal of the American Pharmacists Association Conference 2010;50(2):268‐9. [Google Scholar]
Gayton 1987 {published data only}
- Gayton D, Wood DS, Lorimer M, Tousignat P, Hanley J. Trial of a geriatric consultation team in an acute care hospital. Journal of the American Geriatrics Society 1987;35:726‐36. [DOI] [PubMed] [Google Scholar]
Gilmer 2010 {published data only}
- Gilmer TP, Stefancic A, Ettner SL, Manning WG, Tsemberis S. Effect of full‐service partnerships on homelessness, use and costs of mental health services, and quality of life among adults with serious mental illness. Archives of General Psychiatry 2010;67(6):645‐52. [DOI] [PubMed] [Google Scholar]
Guidotti 2009 {published data only}
- Guidotti TL, Deb P, Bertera R, Ford L. The Fort McMurray Demonstration Project in Social Marketing: No Demonstrable Effect on Already Falling Injury Rates Following Intensive Community and Workplace Intervention. Journal of Community Health 2009;34(5):392‐9. [DOI] [PubMed] [Google Scholar]
Hadid 2010 {published data only}
- Hadid T, Sanchez‐Reilly S. Implications of interdisciplinary palliative care when caring for older adults with advanced cancer. Journal of Pain and Symptom Management 2010;39(2):394. [Google Scholar]
Harrington 2010 {published data only}
- Harrington R, Taylor G, Hollinghurst S, Reed M, Kay H, Wood A. A community‐based exercise and education scheme for stroke survivors: a randomized controlled trial and economic evaluation. Clinical Rehabilitation 2010;24(1):3‐15. [DOI] [PubMed] [Google Scholar]
Harris 1998 {published data only}
- Harries LE, Luft FC, Rudy DW, Kesterson JG, Tierney WM. Effects of multidisciplinary case management in patients with chronic renal insufficiency. American Journal of Medicine 1998;105(6):464‐71. [DOI] [PubMed] [Google Scholar]
Helderman 1997 {published data only}
- Helderman WHV, Munck L, Mushendwa S, vantHof MA, Mrema FG. Effect evaluation of an oral health education programme in primary schools in Tanzania. Community Dentistry and Oral Epidemiology 1997;25(4):296‐300. [DOI] [PubMed] [Google Scholar]
Hendriks 2005 {published data only}
- Hendriks MR, Haastregt JC, Diederiks JP, Evers SM, Crebolder HF, Ejik JT, et al. Effectiveness and cost‐effectiveness of a multidisciplinary intervention programme to prevent new falls and functional decline among elderly persons at risk: design of a replicated randomised controlled trial. BMC Public Health 2005;5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hendriksen 1984 {published data only}
- Hendriksen C, Lund E, StrØmgard E. Consequences of assessment and intervention among elderly people: a three year randomised controlled trial. BMJ (Clinical Research Edition) 1984;1(289):1522‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hiscock 2008 {published data only}
- Hiscock H, Bayer JK, Hampton A, Ukoumunne OC, Wake M. Long‐term mother and child mental health effects of a population‐based infant sleep intervention: cluster‐randomized, controlled trial. Pediatrics 2008;122(3):e621‐7. [DOI] [PubMed] [Google Scholar]
Hollar 2010 {published data only}
- Hollar D, Lombardo M, Lopez‐Mitnik G, Hollar TL, Almon M, Agatston AS, Messiah SE. Effective multi‐level, multi‐sector, school‐based obesity prevention programming improves weight, blood pressure, and academic performance, especially among low‐income, minority children. Journal of Health Care for the Poor & Underserved 2010;21(2 Suppl):93‐108. [DOI] [PubMed] [Google Scholar]
House of Commons 2010a {published data only}
- House of Commons Children, Schools and Families Committee. Sure Start children's centres: fifth report of session 2009‐10: volume 1: report, together with formal minutes. Report 2010;1. [Google Scholar]
House of Commons 2010b {published data only}
- House of Commons Children, Schools and Families Committee. Sure Start children's centres: fifth report of session 2009‐10: volume 2: oral and written evidence. Report. Sure Start children's centre, 2010; Vol. 2.
Howden‐Chapman 2011 {published data only}
- Howden‐Chapman P, Crane J, Chapman R, Fougere G. Improving health and energy efficiency through community‐based housing interventions. International Journal of Public Health 2011;56(6):583‐8. [DOI] [PubMed] [Google Scholar]
Johnson 1991 {published data only}
- Johnson CC, Nicklas TA, Arbeit ML, Harsha DW, Mott DS, Hunter SM, et al. Cardiovascular intervention for high‐risk families: the Heart Smart Program. Southern Medical Journal 1991;84(11):1305‐12. [DOI] [PubMed] [Google Scholar]
Karppi 1995 {published data only}
- Karppi P, Karppi P. Effects of a geriatric inpatient unit on elderly home care patients: a controlled trial. Aging Clinical and Experimental Research 1995;7(3):207‐11. [DOI] [PubMed] [Google Scholar]
Kelaher 2009 {published data only}
- Kelaher M, Dunt D, Feldman P, Nolan A, Raban B. The effect of an area‐based intervention on breastfeeding rates in Victoria, Australia. Health Policy 2009;90(1):89‐93. [DOI] [PubMed] [Google Scholar]
Killaspy 2006 {published data only}
- Killaspy H, Bebbington P, Blizard R, Johnson S, Nolan F, Pilling S, et al. The REACT study: randomised evaluation of assertive community treatment in north London. BMJ 2006;332(7545):815‐8A. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kintner 2009 {published data only}
- Kintner EK, Sikorskii A. Randomized clinical trial of a school‐based academic and counseling program for older school‐age students. Nursing research 2009;58(5):321‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumpusalo 1996 {published data only}
- Kumpusalo EN. Finnish healthy village study: Impact and outcome of a low‐cost local health promotion programme. Health Promotion International 1996;11(2):105‐15. [Google Scholar]
Lambert 2010 {published data only}
- Lambert M, Bock T, Schöttle D, Golks D, Meister K, Rietschel L, et al. Assertive Community Treatment as part of integrated care versus standard care: A 12‐month trial in patients with first‐ and multiple‐episode schizophrenia spectrum disorders treated with quetiapine Immediate Release (ACCESS Trial). Journal of Clinical Psychiatry 2010;71(10):1313‐23. [DOI] [PubMed] [Google Scholar]
Landi 2001 {published data only}
- Landi F, Onder G, Tua E, Carrara B, Zuccala G, Gambassi G, et al. Impact of a new assessment system, the MDS‐HC, on function and hospitalisation of homebound older people: A controlled clinical trial. Journal of the American Geriatrics Society 2001;49(10):1288‐93. [DOI] [PubMed] [Google Scholar]
Layne 2008 {published data only}
- Layne CM, Saltzman WR, Poppleton L, Burlingame GM, Pasalić A, Duraković E, et al. Effectiveness of a school‐based group psychotherapy program for war‐exposed adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry 2008;47(9):1048‐62. [DOI] [PubMed] [Google Scholar]
Lee 2004 {published data only}
- Lee BC, Westaby JD, Berg RL. Impact of a national rural youth health and safety initiative: results from a randomized controlled trial. American Journal of Public Health 2004;94(10):1743‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liddle 2011 {published data only}
- Liddle HA, Dakof GA, Henderson C, Rowe C. Implementation outcomes of Multidimensional Family Therapy‐Detention to Community: a reintegration program for drug‐using juvenile detainees. International Journal of Offender Therapy & Comparative Criminology 2011;55(4):587‐604. [DOI] [PubMed] [Google Scholar]
Lowell 2011 {published data only}
- Lowell DI, Carter AS, Godoy L, Paulicin B, Briggs‐Gowan MJ. A randomized controlled trial of Child FIRST: a comprehensive home‐based intervention translating research into early childhood practice. Child Development 2011;82(1):193‐208. [DOI] [PubMed] [Google Scholar]
Luepker 1996 {published data only}
- Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, et al. Outcomes of a field trial to improve children's dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative group. JAMA 1996;275(10):768‐76. [DOI] [PubMed] [Google Scholar]
Mackintosh 2006 {published data only}
- Mackintosh JW, White M. Randomised controlled trial of welfare rights advice accessed via primary health care. Pilot study. BMC Public Health 2006;21(6):162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Magana‐Valladares 2011 {published data only}
- Magana‐Valladares LC. Cooper K. The National Institute of Public Health: Shaping public policy to advance population health in Mexico. Public Health Reviews 2011;33(1):332‐8. [Google Scholar]
Marcus 1998 {published data only}
- Marcus AC, Garrett KM, Cella D, Wenzel LB, Brady MJ, Crane LA, et al. Telephone counselling of breast cancer patients after treatment: a description of a randomised clinical trial. Psycho‐Oncology 1998;7(6):470‐82. [DOI] [PubMed] [Google Scholar]
Markle‐Reid 2010 {published data only}
- Markle‐Reid M, Browne G, Gafni A, Roberts J, Weir R, Thabane L, et al. The effects and costs of a multifactorial and interdisciplinary team approach to falls prevention for older home care clients 'at risk' for falling: a randomized controlled trial. Canadian Journal on Aging 2010;29(1):139‐61. [DOI] [PubMed] [Google Scholar]
Matsubayashi 2011 {published data only}
- Matsubayashi T, Manabe YC, Etonu A, Kyegombe N, Muganzi A, Coutinho A, Peters DH. The effects of an HIV project on HIV and non‐HIV services at local government clinics in urban Kampala. BMC International Health and Human Rights 2011;9(11 Suppl 1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
McConachie 2000 {published data only}
- McConachie H, Huq S, Munir S, Ferdous S, Zaman S, Khan NZ, et al. A randomized controlled trial of alternative modes of service provision to young children with cerebral palsy in Bangladesh. Journal of Pediatrics 2000;137(6):769‐76. [DOI] [PubMed] [Google Scholar]
McDonald 2009 {published data only}
- McDonald L, Conrad T, Fairtlough A, Fletcher J, Green L, Moore L, Lepps B. An evaluation of a groupwork intervention for teenage mothers and their families.. Child & Family Social Work 2009;14(1):45‐57. [Google Scholar]
McHugo 2004 {published data only}
- McHugo GJ, Bebout RR, Harris M, Cleghorn S, Herring G, Xie HY, et al. A randomized controlled trial of integrated versus parallel housing services for homeless adults with severe mental illness. Schizophrenia Bulletin 2004;30(4):969‐82. [DOI] [PubMed] [Google Scholar]
Meade 2010 {published data only}
- Meade CS, Drabkin AS, Hansen NB, Wilson PA, Kochman A, Sikkema KJ. Reductions in alcohol and cocaine use following a group coping intervention for HIV‐positive adults with childhood sexual abuse histories. Addiction 2010;105(11):1942‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miller K 2011 {published data only}
- Miller KA. Exploring placement instability among young children in the multidimensional treatment foster care preschool study. Dissertation Abstracts International: Section B: The Sciences and Engineering 2011;6(68):10‐B. [Google Scholar]
Miller P 2011 {published data only}
- Miller P, Sonderlund A, Coomber K, Palmer D, Gillham K, Tindall J, Wiggers J. Do community interventions targeting licensed venues reduce alcohol‐related emergency department presentations?. Drug and Alcohol Review 2011;30(5):546‐53. [DOI] [PubMed] [Google Scholar]
Murphy 2010a {published data only}
- Murphy S, Raisanen L, Moore G, Edwards RT, Linck P, Williams N, et al. A pragmatic randomised controlled trial of the Welsh National Exercise Referral Scheme: protocol for trial and integrated economic and process evaluation. BMC Public Health 2010;18(10):352. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2010b {published data only}
- Murphy KR, Hopp RJ, Kittelson EB, Hansen G, Windle ML, Walburn JN. The attack on Asthma Nebraska program: A school‐based treatment model for life‐threatening asthma and anaphylaxis: An update since 2004. Annals of Allergy, Asthma and Immunology 2010;34:398‐405. [DOI] [PubMed] [Google Scholar]
Murray 1997 {published data only}
- Murray J, Manela M, Shuttleworth A, Livingston G. An intervention study with husband and wife carers of older people with a psychiatric illness. Journal of Affective Disorders 1997;46(3):279‐84. [DOI] [PubMed] [Google Scholar]
Naglie 2002 {published data only}
- Naglie G, Tansey C, Kirkland JL, Ogilvie‐Harris DJ, Detsky AS, Etchells E, et al. Interdisciplinary inpatient care for elderly people with hip fracture: a randomized controlled trial. Canadian Medical Association Journal 2002;167(1):25‐32. [PMC free article] [PubMed] [Google Scholar]
Norberg 2010 {published data only}
- Norberg M, Wall S, Boman K, Weinehall L. The Vasterbotten Intervention Programme: background, design and implications. Global Health Action 2010;3:1654‐9880. [DOI] [PMC free article] [PubMed] [Google Scholar]
Norman 2007 {published data only}
- Norman C, Axelsson R. Co‐operation as a strategy for provision of welfare services: a study of a rehabilitation project in Sweden. European Journal of Public Health 2007;17(5):532‐6. [DOI] [PubMed] [Google Scholar]
O'Brien 2010 {published data only}
- O'Brien LM, Polacsek M, MacDonald PB, Ellis J, Berry S, Martin M. Impact of a school health coordinator intervention on health‐related school policies and student behavior. Journal of School Health 2010;80(4):176‐85. [DOI] [PubMed] [Google Scholar]
O'Farrell 2010 {published data only}
- O'Farrell D, Aubrey DL. Rural Responses to H1N1: A Flexible Model for Community Collaboration. Rural Society 2010;20(1):76‐84. [Google Scholar]
Oakes 2010 {published data only}
- Oakes SLE. Successful implementation of an interdisciplinary team approach to reduce psychoactive medications in a community based nursing home: Tackling F‐Tag. Journal of the American Medical Directors Association 2010;11(3):B23‐4. [Google Scholar]
Pattanayak 2009 {published data only}
- Pattanayak SK, Yang JC, Dickinson KL, Poulos C. Shame or subsidy revisited: social mobilization for sanitation in Orissa, India. Bulletin of the World Health Organanization 2009;87(8):580‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Piarroux 2009 {published data only}
- Piarroux R, Bompangue D. Dynamics and control strategies of cholera epidemics in the African region of the Great Lakes. Tropical Medicine and International Health 2009;14:28‐9. [Google Scholar]
Post 2010 {published data only}
- Post LA, Klevens J, Maxwell CD, Shelley GA, Ingram E. An examination of whether coordinated community responses affect intimate partner violence. Journal of Interpersonal Violence 2010;25(1):75‐93. [DOI] [PubMed] [Google Scholar]
Puska 2009 {published data only}
- Puska P. Fat and heart disease: yes we can make a change‐‐the case of North Karelia (Finland). Annals of Nutrition & Metabolism 2009;54(1):33‐8. [DOI] [PubMed] [Google Scholar]
Raja 2009 {published data only}
- Raja S, Ball M, Booth J, Haberstro P, Veith K. Leveraging neighborhood‐scale change for policy and program reform in Buffalo, New York. American Journal of Preventive Medicine 2009;37(6 Suppl 2):S352‐60. [DOI] [PubMed] [Google Scholar]
Rees 2006 {published data only}
- Rees L, Clark‐Stone S. Can collaboration between education and health professionals improve the identification and referral of young people with eating disorders in schools? A pilot study. Journal of Adolescence 2006;29(1):137‐51. [DOI] [PubMed] [Google Scholar]
Reza‐Paul 2008 {published data only}
- Reza‐Paul S, Beattie T, Syed HU, Venukumar KT, Venugopal MS, Fathima MP, et al. Declines in risk behaviour and sexually transmitted infection prevalence following a community‐led HIV preventive intervention among female sex workers in Mysore, India. AIDS 2008;22(5):S91‐S100. [DOI] [PubMed] [Google Scholar]
Richardson 2008 {published data only}
- Richardson B. Comparative analysis of two community‐based efforts designed to impact disproportionality. Child Welfare 2008;87(2):297‐317. [PubMed] [Google Scholar]
Richardson 2010 {published data only}
- Richardson J, Letts L, Chan D, Stratford P, Hand C, Price D, et al. Rehabilitation in a primary care setting for persons with chronic illness: A randomized controlled trial. Primary Health Care Research and Development 2010;11(4):382‐95. [Google Scholar]
Rivera 2007 {published data only}
- Rivera JJ, Sullivan AM, Valenti SS. Adding consumer‐providers to intensive case management: does it improve outcome?. Psychiatric Services 2007;58(6):802‐9. [DOI] [PubMed] [Google Scholar]
Robbers 2008 {published data only}
- Robbers MLP. The Caring Equation: An Intervention Program for Teenage Mothers and Their Male Partners. Children & Schools 2008;30(1):37‐47. [Google Scholar]
Rog 2004 {published data only}
- Rog D, Boback N, Barton‐Villagrana H, Marrone‐Bennett P, Cardwell J, Hawdon J, et al. Sustaining collaborative: a cross‐site analysis of the national funding collaborative on violence prevention. Evaluation and Programme Planning 2004;3:249‐61. [Google Scholar]
Rosenblum 2005 {published data only}
- Rosenblum A, Magura S, Kayman DJ, Fong C. Motivationally enhanced group counselling for substance users in a soup kitchen: a randomized clinical trial. Drug and Alcohol Dependence 2005;80(1):91‐103. [DOI] [PubMed] [Google Scholar]
Rosenheck 1999 {published data only}
- Rosenheck R, Frisman L, Kasprow W. Improving access to disability benefits among homeless persons with a mental illness: an agency‐specific approach to services integration. American Journal of Public Health 1999;89(4):524‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rutter 2004 {published data only}
- Rutter D, Tyrer P, Emmanuel J, Weaver T, Byford S, Hallam A, et al. Internal versus external care management in severe mental illness: randomized controlled trial and qualitative study. Journal of Mental Health 2004;13(5):453‐66. [Google Scholar]
Salihu 2011 {published data only}
- Salihu H.M, August E.M, Jeffers D.F, Mbah A.K, Alio A.P, Berry E. Effectiveness of a Federal Healthy Start Program in Reducing Primary and Repeat Teen Pregnancies: Our Experience over the Decade. Journal of Pediatric and Adolescent Gynecology 2011;24(3):153‐60. [DOI] [PubMed] [Google Scholar]
Scholten 1999 {published data only}
- Scholten C, Brodowicz T, Graninger W, Garavsky I, Pils K, Pesau B, et al. Persistant functional and social benefit 5 years after a multidisciplinary arthritis training program. Archives of Physical Medicine and Rehabilitation 1999;80(10):1282‐7. [DOI] [PubMed] [Google Scholar]
Selassie 2011 {published data only}
- Selassie TG, Fantahun M. In what ways can Community Integrated Management of Neonatal and Childhood Illnesses (C‐IMNCI) improve child health?. Ethiopian Journal of Health Development 2011;25(2):143‐9. [Google Scholar]
Sexton 2011 {published data only}
- Sexton E, Ryst E, Gardner J, Bennett K. Effective practice in an ever‐shifting landscape: A multidisciplinary approach to behavioral and mental health support in schools. Advances in School Mental Health Promotion 2011;4(4):13. [Google Scholar]
Shriqui 2008 {published data only}
- Shriqui C, Lachance I. Improving metabolic health outcomes in mentally ill populations with the Mieux‐tre Wellness program. European Neuropsychopharmacology 2008;18:S275‐6.. [Google Scholar]
Singh 2009 {published data only}
- Singh AS, Chin A Paw MJ, Brug J, Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school‐based program on body composition and behavior. Archives of Pediatrics & Adolescent Medicine 2009;163(4):309‐17. [DOI] [PubMed] [Google Scholar]
Smith 2010 {published data only}
- Smith RJ, Jennings JL, Cimino A. Forensic continuum of care with Assertive Community Treatment (ACT) for persons recovering from co‐occurring disabilities: Long‐term outcomes. Psychiatric Rehabilitation Journal 2010;33(3):207‐18. [DOI] [PubMed] [Google Scholar]
Sommers 2000 {published data only}
- Sommers LS, Marton KI, Barbaccia JC, Randolph J. Physician, nurse and social worker collaboration in primary care for chronically ill seniors. Archives of Internal Medicine 2000;160(2):1825‐33. [DOI] [PubMed] [Google Scholar]
Stallard 2008 {published data only}
- Stallard P. No long‐lasting effects of classroom‐based cognitive behavioural and interpersonal prevention programmes on depressive symptoms in adolescents. Evidence‐Based Mental Health 2008;11(3):75. [DOI] [PubMed] [Google Scholar]
Sytema 2007 {published data only}
- Sytema S, Wunderink L, Bloemers W, Roorda L, Wiersma D. Assertive community treatment in the Netherlands: a randomized controlled trial. Acta Psychiatrica Scandinavica 2007;116(2):105‐12. [DOI] [PubMed] [Google Scholar]
Teufel‐Shone 2005 {published data only}
- Teufel‐Shone NI, Drummond R, Rawiel U. Developing and adapting a family‐based diabetes program at the U.S. ‐ Mexico border. Preventing Chronic Disease 2005;2(1):A20. [PMC free article] [PubMed] [Google Scholar]
Thibault 2010 {published data only}
- Thibault H, Boulard S, Carriere C, Ruello M, Atchoarena S, Delmas C, et al. Prevention and treatment of childhood obesity in the Aquitaine region (France). International Journal of Pediatric Obesity 2010;5 Suppl 1:39‐40. [Google Scholar]
Thornicroft 1998 {published data only}
- Thornicroft G, Strathdee G, Phelan M, Holloway F, Wykes T, Dunn G, et al. Rationale and design ‐ PRiSM Psychosis Study I. The British Journal of Psychiatry 1998;173:363‐70. [DOI] [PubMed] [Google Scholar]
Tinetti 1994 {published data only}
- Tinetti ME, Baker DI, McAvay G, Claus EB, Garrett P, Gottschalk M, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. New England Journal of Medicine 1994;331(13):821‐7. [DOI] [PubMed] [Google Scholar]
Tourigny 2004 {published data only}
- Tourigny A, Durand PJ, Bonin L, Hebert R, Rochette L. Quasi‐experimental study of the effectiveness of an integrated service delivery network for the frail elderly. Canadian Journal of Aging‐Revue Canadienne du Vieillissement 2004;23(3):231‐46. [PubMed] [Google Scholar]
Tucker 2008 {published data only}
- Tucker S, Hughes J, Sutcliffe C, Challis D. Care management for older people with mental health problems: from evidence to practice. Australian Health Review 2008;32(2):210‐22. [DOI] [PubMed] [Google Scholar]
Tucker 2011 {published data only}
- Tucker S, Lanningham‐Foster L, Murphy J, Olsen G, Orth K, Voss J, et al. A school based community partnership for promoting healthy habits for life. Journal of Community Health 2011;36(3):414‐22. [DOI] [PubMed] [Google Scholar]
Van Assema 1994 {published data only}
- Tucker S, Hughes J, Sutcliffe C, Challis D. [Care management for older people with mental health problems: from evidence to practice]. Australian Health Review 2008;32(2):210‐22. [DOI] [PubMed] [Google Scholar]
- Assema P. Results of the Dutch community project 'Healthy Bergeyk'. Preventive Medicine 1994;23(3):394‐401. [DOI] [PubMed] [Google Scholar]
Weingarten 1985 {published data only}
- Wall M, Hayes R, Moore D, Petticrew M, Clow A, Schmidt E, et al. Evaluation of community level interventions to address social and structural determinants of health: a cluster randomised controlled trial. BMC public health 2009;9:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weingarten MA, Goldberg J, Teperberg Y, Harrison N, Oded A. A pilot study of the multidisciplinary management of childhood asthma in a family practice. Journal of Asthma 1985;22(5):261‐5. [DOI] [PubMed] [Google Scholar]
Wierdsma 2007 {published data only}
- Wierdsma AI, Poodt HD, Mulder CL. Effects of community‐care networks on psychiatric emergency contacts, hospitalisations and involuntary admissions. Journal of Epidemiology and Community Health 2007;61(7):613‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2006 {published data only}
- Williams N, Nasir R, Smither G, Troon S. Providing opiod substitution treatment to indigenous heroin users within a community health service setting in Adelaide. Drug and Alcohol Review 2006;25(3):227‐32. [DOI] [PubMed] [Google Scholar]
Williams 2011 {published data only}
- Williams A, Matthews M, Washington K, Krishnamurti L. A community based educational support program for children with sickle cell disease improves school attendance and educational performance. American Journal of Hematology 2011;86(10):E25. [Google Scholar]
Zayas 2004 {published data only}
- Zayas LHM. Adapting psychosocial intervention research to urban primary care environments: A case example. Annals of Family Medicine 2004;2(5):504‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Wall 2009 {published data only}
- Well London. Ongoing study Starting date of trial not provided. Contact author for more information.
Additional references
Benzeval 1995
- Benzeval M, Judge K, Whitehead M (editors). Tackling inequalities in health; an agenda for action. London: King's Fund 1995.
Burger 2005
- Burger VW. Selection Bias and covariate imbalances in Randomised Clinical Trials. John Wiley and Sons Ltd, 2005. [Google Scholar]
CDC 2007
- US Department of Health and Human Services, Centers for Disease Control and Prevention, Coordination Center for Health Promotion. Wisewoman. A crosscutting program to improve the health of uninsured women. Atlanta: Centers for Disease Control and Prevention 2007.
Dickinson 2006
- Dickinson H. The evaluation of health and social care partnerships: an analysis of approaches and synthesis for the future. Health and Social Care in the Community 2006;14(5):375‐83. [DOI] [PubMed] [Google Scholar]
EPOC 2007a
- Cochrane Effective Practice and Organisation of Care Review Group. Data Collection Checklist. Ottawa: Cochrane Effective Practice and Organisation of Care Review Group 2007.
EPOC 2007b
- Cochrane Effective Practice and Organisation of Care Review Group. Data Abstraction Form. Ottawa: Cochrane Effective Practice and Organisation of Care Review Group 2007.
Gillies 1998
- Gillies P. Effectiveness of alliances and partnerships for health promotion. Health Promotion International 1998;13(2):99‐120. [Google Scholar]
Great Britain 1970
- Great Britain. Local Authority Social Services Act 1970. London: HMSO 1970.
Great Britain 1972
- Great Britain. Local Government Act 1972 (c70). London: HMSO 1972.
Great Britain 1973
- Great Britain. National Health Service Reorganisation Act 1973 (c32). London: HMSO 1973.
Great Britain 1977
- Great Britain. The National Health Services Act 1977 (c22). London: HMSO 1977.
Great Britain 1999
- Great Britain. Health Act 1999 (c31). London: Office of Public Sector Information 1999.
Hardy 2003
- Hardy B, Husdon B, Waddington E. Assessing strategic partnership The Partnership Assessment Tool. London: Office of the Deputy Prime Minister 2003.
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.0 [updated February 2008]. Oxford: The Cochrane Collaboration 2008.
HM Government 1995
- HM Government. Tackling drugs together: A strategy for England 1995‐1998 (Cmd 2846). London: HMSO 1995.
HM Government 1998
- HM Government. Tackling drugs to build a better Britain: The government’s ten year strategy for tackling drug misuse (Cmd 3945). London: HMSO 1998.
Jakarta 1997
- World Health Organization. Jakarta Declaration. Jakarta: Fourth International Conference on Health Promotion. 1997.
Laws Statutes 1973a
- Laws, Statutes. London:HMSO. 1973. Reorganisation of the National Health Service and Local Government in England and Wales: A report of the working party on Collaboration between the NHS and Local Government on its activities to the end of 1972. London: HMS0 1973.
Laws Statutes 1973b
- Laws, Statutes. Reorganisation of the National Health Service and Local Government in England and Wales: A report of the working party on Collaboration between the NHS and Local Government on its activities from January to July 1973 [London: HMSO]. 1973.
Laws Statutes 1974
- Laws, Statutes. Reorganisation of the National Health Service and Local Government in England and Wales: A report of the working party on Collaboration between the NHS and Local Government on its activities from July 1973 to April 1974. London: HMSO 1974.
Marmot 2005
- Marmot M. Social determinants of health inequalities. Lancet 2005;365:1099‐103. [DOI] [PubMed] [Google Scholar]
Marmot 2010
- Marmot M. Fair Society, Healthy Lives. The Marmot Review. The Marmot Review 2010:1‐242. [Google Scholar]
Morris 2007
- Morris EB for the Cochrane Health Equity Field. Equity Checklist for Reviewers. Version 2007=10=10. Personal communication. November 21, 2007.
Padgett 2004
- Padgett SM, Bekemeir B, Berkowitz B. Collaborative partnerships at state and national levels: promoting systems changes in public health infrastructure. Journal of Public Health Management and Practice 2004;10(3):251‐7. [DOI] [PubMed] [Google Scholar]
Primary 2004
- Primary and Community Health Branch, Victorian Government Department of Human Services. Primary Care Partnerships Strategic Directions 2004‐2006. Melbourne: Department of Human Services, State of Victoria 2004:http://www.health.vic.gov.au/pcps/downloads/strategy/pcp_strat_2004_06.pdf.
Primary 2005
- Primary and Community Health Branch, Victorian Government Department of Human Services. Primary Care Partnerships: Working together, achieving more. Melbourne: Department of Human Services, State of Victoria, 2005:http://www.health.vic.gov.au/pcps/downloads/publications/pcp_generalrpt_jul05.pdf.
Primary 2009
- Primary Care Partnerships. Good Practice Guide 2009. A resource of the Victorian Service Coordination Practice Manual. Melbourne: Department of Human Services, State Government of Victoria, 2009. [http://www.health.vic.gov.au/pcps/coordination] [Google Scholar]
Smith 2009
- Smith KE, Bambra C, Joyce KE, Perkins N, Hunter DJ, Blenkinsopp EA. Partners in health? A systematic review of the impact of organizational partnerships on public health outcomes in England between 1997 and 2008. Journal of Public Health 2009;31(2):210‐21. [DOI] [PubMed] [Google Scholar]
Sure Start 2004
- HM Treasury. Choice for Parents, the best start for children: a ten year strategy for childcare. London: The Stationery Office 2004:http://www.surestart.gov.uk/aboutsurestart/about/strategy/.
Victorian Health Promotion Foundation 2005
- Victorian Health Promotion Foundation. The Partnerships Analysis Tool For Partners in Health Promotion. Carlton South: Victorian Health Promotion Foundation 2005:http://www.vichealth.vic.gov.au/˜/media/ResourceCentre/PublicationsandResources/VHP%20part%20toollow%20res.ashx.
Wales Office 2001
- Wales Office of Research and Development for Health and Social Care. A systematic review of health outcomes from collaboration between health and local government agencies. Cardiff: Wales Office of Research and Development for Health and Social Care 2001.
WHO 1986
- World Health Organization. Ottawa Charter for Health Promotion. Ottawa: First International Conference on Health Promotion 1986. http://www.who.int/hpr/NPH/docs/ottawa_charter_hp.pdf, 1986.
WHO 2005
- World Health Organization. The Bangkok Charter for Health Promotion in a Globalized World. The 6th Global Conference on Health Promotion. Bangkok: WHO, 2005:http://www.who.int/healthpromotion/conferences/6gchp/hpr_050829_%20BCHP.pdf.
WHO 2011
- World Health Organisation. Bugs, Drugs and Smoke. Stories from Public Health. World Health Organisation, 2011. [Google Scholar]


