Abstract
Objective
Diabetes affects 1 in 10 adults in China. Diabetic retinopathy (DR) is a diabetes-related complication that, if untreated, impairs vision and causes blindness. Evidence on DR diagnosis and risk factors is limited. This study aimed to add evidence from socioeconomic factors.
Design
A cross-sectional survey of people with diabetes conducted in 2019 was analysed by using logistic regression to evaluate the association of socioeconomic factors with the glycated haemoglobin (HbA1c) level and DR.
Setting
Five counties/districts of western China (Sichuan) were included.
Participants
Registered participants with diabetes aged from 18 to 75 years were selected, and at last 2179 participants were included in the analysis.
Results
In this cohort, 37.13% (adjusted value 36.52%), 19.78% (adjusted value 19.59%) and 17.37% of participants had HbA1c<7.0%, DR (24.96% of those in the high-HbA1c group) and non-proliferative DR, respectively. Participants with higher social health insurance coverage (urban employee insurance (UEI)), higher income and urban residents tended to have glycaemic control (HbA1c) compared with their counterparts (OR: 1.48, 1.08 and 1.39, respectively). Participants with UEI or higher income had a lower risk of DR (OR: 0.71 and 0.88, respectively); higher education was associated with a 53%–69% decreased risk of DR.
Conclusion
This study shows disparities in the effect of socioeconomic factors on glycaemic (HbA1c) management and DR diagnosis among people with diabetes in Sichuan. Lower socioeconomic (especially non-UEI) status conferred a higher risk of high HbA1c and DR. The insights from this study indicate the need for national programmes to implement community-level measures to facilitate access to better HbA1c management and early detection of DR in patients with lower socioeconomic status and diabetes.
Trial registration number
Chinese Clinical Trial Registry (ChiCTR1800014432).
Keywords: Diabetic retinopathy, Epidemiology, HEALTH ECONOMICS, Quality in health care
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This investigation used a multistage, stratified, random sampling method, adopted the sampling frame of the China Chronic Disease and Risk Factors Surveillance and accorded to the local sex and age structure to improve the representation of data.
A wide range of important confounders were considered in the association exploration, as detailed information was available on sociodemographic factors, management and physiological indicators.
The limitation of this study, which was based on a cross-sectional survey, is that the results reflect the association, but not necessarily causality.
Introduction
The global burden of diabetes has significantly increased over the past few decades, with 537 million people with diabetes in 2021, an increase from 108 million in 1980, that has affected most of low-income and middle-income countries.1 2 Approximately 1 in 10 adults in China has been diagnosed with diabetes, and the annual diabetes incidence rates are high. China, followed by India, has the highest diabetes prevalence rate.3 Diabetic retinopathy (DR) is a diabetes-related complication wherein hyperglycaemia induces retinal damage that, if untreated, can affect sight and lead to blindness. The results of 2018 Chinese chronic disease surveillance (a cross-sectional survey) revealed that residents with diabetes in Sichuan Province (western China) constituted 6%–7% (approximately 8.6 million individuals) of the national population with diabetes,4–6 of which 60.48% were undiagnosed before the survey.6 A retrospective analysis of inpatients with diabetes in more than 30 provinces of China from 1991 to 2000 showed that the disease burden of DR (prevalence rate 34.3%) ranked second among all diabetes-related complications.7 A review of diabetes-related complications revealed that DR ranked in the top three complications.8 A meta-analysis of DR studies reported pooled prevalence rates of DR, non-proliferative DR (NPDR) and proliferative DR (PDR) of 18.45% (beween 5.43% and 44.84% during 1990–2017), 15.06% and 0.99%, respectively.9
A higher blood glucose level, longer diabetes duration and rural residence are significant risk factors for DR,9–11 and timely diagnosis and effective treatment to access normal blood glucose level may help prevent or slow the progression of DR in this patient group. In the USA, insurance status is a strong predictor of effective diabetes management.10 However, there is limited research-based evidence of the association between insurance type and DR in China as previous research has focused on macro-level socioeconomic determinants of general health.12 13
We hypothesised that those who are covered by social health insurance (SHI) are more likely to have controlled blood glucose levels and are less likely to develop DR. This study aimed to investigate the situation of glycaemic control (glycated haemoglobin (HbA1c)) and DR prevalence in Sichuan Province and to examine the effects of socioeconomic factors, including SHI, as risk factors for DR and poor glycaemic control.
Methods
Data collection and study population
A cross-sectional survey among people with diabetes was conducted in 2019 in Sichuan Province, China, using a multistage, stratified, random sampling method. The China and Sichuan Diabetes Society, China and Sichuan CDC and Bethune Public Welfare Foundation organised the survey. As a part of the national investigation, this study adopted the sampling frame of the China Chronic Disease and Risk Factors Surveillance (CCDRFS) in 2013. Based on the urban–rural ratio of Sichuan, two urban districts and three rural counties were sampled from the Sichuan CCDRFS.14–16 Every county/district has a diabetes management registration system for local residents, which forms a part of the Basic Public Health Services System. In each county/district, we chose the four township-level administrative regions that were investigated in the 2013 Sichuan CCDRFS. According to the overall sample design of the national project and the sample size formula,15 16 120 adult participants (age 18–75 years) were to be enrolled in each region. In combination with this study’s aim, the formula with a two-sided significance level of 0.05 (u=1.96) and a DR prevalence of 18.45% (reported previously),9 design efficiency (deff) of 1.5, relative error (σ) of 0.22 and fourfold expansion (N=4) with rural–urban-based and sex-based stratification, a sample of at least 2104 participants was needed.
Therefore, residents with diabetes who had lived in the survey region for more than 6 months and were registered in the Basic Public Health Services System (inclusion criteria) were stratified and sampled according to the sex and age structure in 2013 (16%, 44% and 40% of 18–44, 45–59 and 60–74 years, respectively, with an equal male-to-female ratio were selected; online supplemental figure 1). The diagnostic criteria of diabetes were a fasting plasma glucose level of 7.0 mmol/L or higher, or a 2-hour plasma glucose level of 11.1 mmol/L or higher during a 75 g oral glucose tolerance test. People with diabetes who had a mental disorder or were pregnant were excluded while sampling. Finally, 2241 participants were investigated, and 2179 participants were included in the analysis, without distinguishing those with type 1 and 2 diabetes. Approximately 62 respondents who were missing values of insurance status, diabetes diagnosis and prognosis were excluded.
bmjopen-2022-067475supp001.pdf (419.9KB, pdf)
The provincial and local working groups conducted the on-site surveys and uploaded survey data to the national system platform.15 Trained staff members conducted all interviews and physical examinations. Information regarding participants’ demographic characteristics, such as education level, income, insurance status, family history of diabetes, history of diseases and healthcare usage, was collected via face-to-face interviews. Similarly, information on exercise days in a week (≥30 min, during leisure time), food intake frequency (per day, week, month or year) and average amount per consumption (gram), days per week when dietary advice of doctors was followed, current cigarette consumption (every day, not every day, non-smoker) and participation in diabetes management programmes were obtained via face-to-face questionnaire survey. Anthropometric data of the participants’ height, weight and blood pressure were obtained using a TGZ height gauge, TANITA HD-390 body weight scale and Omron blood pressure monitor (HBP-1300, China). Two 45° colour fundus photographs were taken for each eye using a digital non-mydriatic retinal camera (Canon CR-2; Canon, Tokyo, Japan or TRC-NW400; Topcon Corporation, Tokyo, Japan); one was centred on the optic disc and the other on the macula. Subsequently, every fundus photograph was remotely reviewed and classified by two ophthalmologists from the Shanghai Sixth People’s Hospital according to the International Clinical Diabetic Retinopathy Disease Severity Scale.11 If the result was inconsistent, another senior ophthalmologist reviewed the case again. The biochemical tests were conducted using fasting blood samples (after a 10-hour overnight fast before the examination), as in a previous surveillance study.14 17 HbA1c and lipid values were measured using high-performance liquid chromatography (Bio-Rad D10 Hemoglobin Analyser) and enzymatic methods (Roche Cobas c701/702), respectively. All biomarker samples used in this study were tested in the same laboratory (Guangzhou KingMed Diagnostics Group Co., China).
Key dependent and independent variables
HbA1c values were used to assess glycaemic control, and an HbA1c greater than 7.0% was considered high.18–24 The participants were diagnosed with DR and no apparent DR. DR was classified into four levels: levels 1–3 represented NPDR (mild, moderate or severe) and level 4 indicated PDR (a higher level equated to greater severity of DR). In this study, DR included participants with newly and previously diagnosed DR.
Based on the SHI, participants were divided into two groups. The urban employee insurance (UEI, including the former free medical services) group covers urban residents with formal employment and state workers. Participants with the urban resident insurance (URI) type, or the new rural cooperative medical scheme (NCMS), were combined into a single group, which covered urban residents without formal employment and those who were rural residents.25–27
Income was reflected by the monthly household income per capita. Systolic blood pressure (SBP) <130 mm Hg and diastolic blood pressure <80 mm Hg were considered the target values.21–24 The target value of total cholesterol (TC) was set at <5.2 mmol/L.28 The target triglyceride (TG) value was defined as <1.7 mmol/L.24 28 When the high-density lipoprotein cholesterol (HDLC) level was >1 mmol/L for men or >1.3 mmol/L for women, HDLC was categorised as within the target level.24 Target values of low-density lipoprotein cholesterol (LDLC) were classified into three categories: LDLC<1.8 mmol/L with atherosclerotic cardiovascular disease, LDLC<2.6 mmol/L (in participants aged ≥40 years) and LDLC<3.4 mmol/L (in participants aged <40 years).28
The target range of body mass index (BMI) (weight) was set as a BMI between 18.5 and 24 kg/m2 (including 26 participants with BMI slightly less than 18.5),24 or a BMI between 24 and 28 kg/m2 (overweight, by Chinese standards) if the reported weight decreased by >2.5 kg in the year (after self weight management). The self weight management in this study refers to the participants undertaking proactive, planned steps to lose or gain BMI/weight to achieve the target BMI (weight) range.
We included a diabetes management programme in the analysis. The programme was conducted by the general practitioners at community healthcare facilities and included at least four blood pressure measurements and blood tests of people with diabetes in the past year, as well as medical and lifestyle guidance. The medical guidance included a review and adjustment of prescription medicine based on blood sugar levels. The lifestyle guidance covered diet, physical activity, smoking cessation and quitting drinking.
Statistical analysis
A descriptive analysis of the participants’ characteristics was conducted. The population structure (sex, age and rural/urban) of people with diabetes aged 18–74 years in Sichuan in 2018 was used as the reference to calculate the adjusted values. The participants were stratified based on DR type. HbA1c control status and DR diagnosis were set as dependent variables in the logistic models by using SAS (SAS Institute, V.9.4). Sociodemographic characteristics that were set as independent variables included insurance type, place of residence, income level, HbA1c values and education. Univariate logistic regression analysis was performed initially (online supplemental table 1), and the multivariate logistic regression models were tested step by step (from models 1 to 3). Model 1 only contained socioeconomic and demographic factors. Models 2 and 3 were adjusted for behavioural and physiological indicators (eg, exercise, diet, smoking), respectively, based on model 1. A p value <0.05 was considered statistically significant. Missing income values were imputed through the MICE package (developing by Stef van Buuren, et al) of R software using the predictive mean matching method, which is a widely used statistical semi-parametric imputation approach for calculating missing values.29–31
Patient and public involvement
None. It was not appropriate or possible to involve patients or the public in the design, conduct, reporting, or dissemination plans of our research.
Results
In total, 2179 participants with diabetes (49.75% men, 50.25% women; 40.39% urban, 59.61% rural; table 1) were included in the analysis. Among these participants, only 37.13% (adjusted value 36.52%) achieved glycaemic control (HbA1c<7.0%).
Table 1.
Characteristics of the groups defined by HbA1c level
| Total (n=2179) | HbA1c ≥7.0% (n=1370) | HbA1c <7.0% (n=809) | |
| n (crude, adjusted value, %) | n (crude value %) | n (crude value %) | |
| Socioeconomic and demographic factors | |||
| Urban area | 880 (40.39%, 35.68%) | 465 (33.94%) | 415 (51.3%) |
| Female | 1095 (50.25%, 49.54%) | 664 (48.47%) | 431 (53.28%) |
| Age (years) | 57.13, 55.82 | 57.17 | 57.06 |
| Age at diabetes diagnosis (years) | 49.62, 48.51 | 48.96 | 50.75 |
| Duration of diabetes (years) | 6.52, 6.33 | 7.25 | 5.29 |
| Insurance of UEI | 617 (28.32%, 26.95%) | 302 (22.04%) | 315 (38.94%) |
| Monthly household income per capita (RMB) | 1392.41, 1408.72 | 1220.58 | 1683.4 |
| Receiving HbA1c blood test every 3 months | 596 (27.35%, 26.94%) | 330 (24.09%) | 266 (32.88%) |
| Education level | |||
| High school level or higher | 466 (21.39%, 21.39%) | 237 (17.30%) | 229 (28.31%) |
| Middle school | 633 (29.05%, 29.05%) | 404 (29.49%) | 229 (28.31%) |
| Primary and below | 1080 (49.56%, 49.56%) | 729 (53.21%) | 351 (43.39%) |
| Family history of diabetes (yes) | 875 (40.16%, 39.84%) | 567 (41.39%) | 308 (38.07%) |
| Self-management of diabetes | |||
| Monitor blood sugar at home | 992 (45.53%, 44.7%) | 597 (43.58%) | 395 (48.83%) |
| Exercise 30 min ≥1 day last week | 1085 (49.79%, 47.96%) | 600 (43.80%) | 485 (59.95%) |
| Follow diet advice of doctors ≥1 day last week | 1629 (74.76%, 74.81%) | 974 (71.09%) | 655 (80.96%) |
| Eat vegetable and fruit ≥400 g per day | 1039 (47.68%, 47.52%) | 599 (43.72%) | 440 (54.39%) |
| Non-smoker currently | 1620 (74.35%, 73.78%) | 987 (72.04%) | 633 (78.24%) |
| Participating in diabetes management programme | 410 (18.82%, 18.86%) | 267 (19.49%) | 143 (17.68%) |
| Achievement of target values of physiological indicators | |||
| SBP | 1088 (49.93%, 51.68%) | 654 (47.74%) | 434 (53.65%) |
| DBP | 1466 (67.28%, 66.97%) | 908 (66.28%) | 558 (68.97%) |
| TC | 1419 (65.12%, 65.61%) | 827 (60.36%) | 592 (73.18%) |
| TG | 1173 (53.83%, 53.65%) | 704 (51.39%) | 469 (57.97%) |
| HDLC | 1511 (69.34%, 69.32%) | 944 (68.91%) | 567 (70.09%) |
| LDLC | 875 (40.16%, 41.32%) | 511 (37.30%) | 364 (44.99%) |
| Range of BMI (weight) | 1025 (47.04%, 46.8%) | 648 (47.30%) | 377 (46.60%) |
| Diagnosed with DR | 431 (19.78%, 19.59%) | 342 (24.96%) | 89 (11.00%) |
BMI, body mass index; DBP, diastolic blood pressure; DR, diabetic retinopathy; HbA1c, glycated haemoglobin; HDLC, high-density lipoprotein cholesterol; LDLC, low-density lipoprotein cholesterol; SBP, systolic blood pressure; TC, total cholesterol; TG, triglyceride; UEI, urban employee insurance.
Those who were insured with the UEI accounted for 28.32% (adjusted value 26.95%) of all observations and were more likely to have a normal HbA1c level (38.94%). Participants with normal HbA1c levels tended to reside in urban areas, predominantly included women, had a shorter history of diagnosed diabetes, had a higher monthly household income per capita, underwent HbA1c tests every 3 months and were educated to high school level or above. Furthermore, the participants who had better self-management following the doctor’s advice or controlled the related physiological indicators (to reach the target value) mostly accounted for a higher proportion of the normal HbA1c level group. The total prevalence of DR was 19.78% (adjusted value 19.59%). A lower prevalence of DR was observed in the group in which HbA1c levels were <7.0%.
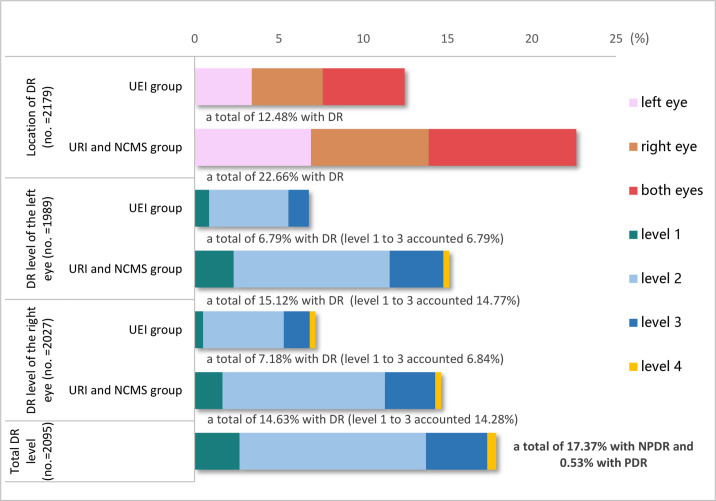
Figure 1 shows that those who were insured with the UEI were more likely to have glycaemic control (HbA1c level <7.0%) compared with those who were insured with the NCMS. The prevalence of DR (22.66%) and self-reported impaired vision (77.98%) were higher for those who were insured with the URI or the NCMS than for those who were insured with the UEI. The distribution of participants with previously diagnosed and newly identified DR in different subgroups revealed that the awareness of DR was higher among those who lived in urban areas, were covered by the UEI, or underwent regular HbA1c testing. Among the participants who were previously diagnosed with DR, the proportion of those who received treatment was higher among those who lived in urban areas, were covered by the UEI, or were able to monitor their blood sugar regularly at home (online supplemental table 2). Figure 2 presents the bilateral DR distribution. The number of right and left eyes with clear photographs was 2027 and 1989, respectively. Among the recorded observations with clear fundus photographs of at least one eye (n=2095), the rates of NPDR and PDR were 17.37% and 0.53%, respectively. Both in the left eye and right eye, regardless of the kind of insurance group, the main DR type was NPDR (levels 1 to 3 ranged from 6.79% to 14.77%). Moreover, level 2 (moderate NPDR) accounted for the largest proportion of NPDR.
Figure 1.
HbA1c level control and diabetic retinopathy (DR) conditions observed in participants covered by the two types of insurance. Values are presented as proportions and 95% CIs per group. HbA1c, glycated haemoglobin; NCMS, new rural cooperative medical scheme; UEI, urban employee insurance; URI, urban resident insurance.
Figure 2.
The distribution of diabetic retinopathy (DR) location and DR level in the eyes of participants covered by different insurance providers. DR location analysis included newly diagnosed and previously diagnosed participants. The DR level was confirmed based on an eye-ground photography test (the total DR level group included the participants who were graded in at least one eye). Fundus photos with poor-quality were excluded. Levels 1–3 represent non-proliferative DR (NPDR) status (mild, moderate or severe). Level 4 was proliferative DR (PDR). NCMS, new rural cooperative medical scheme; UEI, urban employee insurance; URI, urban resident insurance.
In table 2 model 3, urban residents were more likely to have a normal HbA1c level (<7.0%) compared with rural residents, and that in women was 1.41 times that in men. The corresponding probability of achieving the HbA1c target in participants with UEI was 48% higher than that of participants with URI or NCMS. Every 1000 RMB increase in monthly household income per capita potentially increased the probability of achieving the HbA1c target by 8%. Undergoing an HbA1c blood test every 3 months might improve this probability by 28%. After adjusting for hypertension and dyslipidaemia, achieving the target values of SBP, TC and TG was positively associated with achieving the target HbA1c level (table 2).
Table 2.
Multivariate logistic regression models for socioeconomic factors associated with HbA1c level <7%
| Independent variable (reference group) | Model 1 | Model 2 | Model 3 | |||
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| Urban areas (ref: rural areas) | 1.51 (1.22 to 1.87) | <0.001*** | 1.50 (1.20 to 1.89) | <0.001*** | 1.39 (1.11 to 1.74) | 0.005*** |
| Sex (ref: male) | 1.45 (1.19 to 1.75) | <0.001*** | 1.25 (0.99 to 1.58) | 0.056* | 1.41 (1.11 to 1.80) | 0.005*** |
| Age at diabetes diagnosis (year) | 1.01 (1.00 to 1.02) | 0.012** | 1.01 (1.00 to 1.02) | 0.037** | 1.01 (1.00 to 1.02) | 0.039** |
| Duration of diabetes | 0.94 (0.92 to 0.96) | <0.001*** | 0.93 (0.92 to 0.95) | <0.001*** | 0.93 (0.92 to 0.95) | <0.001*** |
| Insurance type, UEI group (ref: URI and NCMS group) | 1.53 (1.18 to 1.99) | 0.001*** | 1.47 (1.12 to 1.93) | 0.005*** | 1.48 (1.13 to 1.94) | 0.004*** |
| Monthly household income per capita (1000 RMB) | 1.09 (1.02 to 1.17) | 0.009*** | 1.09 (1.02 to 1.16) | 0.017** | 1.08 (1.01 to 1.15) | 0.024** |
| Undergoing an HbA1c blood test every 3 months (ref: not received) | 1.43 (1.16 to 1.77) | 0.001*** | 1.35 (1.08 to 1.68) | 0.008*** | 1.28 (1.03 to 1.60) | 0.028** |
| Middle school education (ref: high school level or higher) | 0.84 (0.63 to 1.12) | 0.228 | 0.84 (0.62 to 1.13) | 0.251 | 0.83 (0.62 to 1.12) | 0.231 |
| Primary school education and below (ref: high school level or higher) | 0.78 (0.57 to 1.05) | 0.105 | 0.82 (0.59 to 1.13) | 0.214 | 0.83 (0.60 to 1.14) | 0.248 |
| Family history of diabetes (ref: no history) | 0.82 (0.68 to 1.00) | 0.050** | 0.83 (0.68 to 1.01) | 0.063* | 0.82 (0.67 to 1.01) | 0.057* |
| Monitor blood sugar at home (ref: not at home) | 0.92 (0.74 to 1.14) | 0.444 | ||||
| Exercise 30 min ≥1 day per week (ref: unreached) | 1.50 (1.22 to 1.84) | <0.001*** | 1.53 (1.25 to 1.88) | <0.001*** | ||
| Follow dietary advice of doctors ≥1 day per week (ref: unreached) | 1.63 (1.28 to 2.06) | <0.001*** | 1.64 (1.29 to 2.08) | <0.001*** | ||
| Vegetables and fruit intake <400 g per day (ref: higher intake) | 0.70 (0.58 to 0.85) | <0.001*** | 0.73 (0.60 to 0.88) | 0.001*** | ||
| Smoke currently (ref: not currently) | 0.76 (0.58 to 0.99) | 0.039** | 0.76 (0.59 to 0.99) | 0.045** | ||
| With hypertension or dyslipidaemia (ref: without) | 1.32 (1.02 to 1.71) | 0.035** | ||||
| Achieving the target SBP value (ref: unachieved) | 1.27 (1.00 to 1.60) | 0.047** | ||||
| Achieving the target DBP value (ref: unachieved) | 1.00 (0.79 to 1.28) | 0.973 | ||||
| Achieving the target TC value (ref: unachieved) | 1.61 (1.27 to 2.05) | <0.001*** | ||||
| Achieving the target TG value (ref: unachieved) | 1.26 (1.01 to 1.58) | 0.04** | ||||
| Achieving the target HDLC value (ref: unachieved) | 1.19 (0.94 to 1.51) | 0.157 | ||||
| Achieving the target LDLC value (ref: unachieved) | 1.08 (0.87 to 1.35) | 0.488 | ||||
| Achieving the target BMI (weight) (ref: unachieved) | 0.92 (0.75 to 1.12) | 0.393 | ||||
*p<0.1, **p<0.05, ***p<0.01.
BMI, body mass index; DBP, diastolic blood pressure; HbA1c, glycated haemoglobin; HDLC, high-density lipoprotein cholesterol; LDLC, low-density lipoprotein cholesterol; NCMS, new rural cooperative medical scheme; TC, total cholesterol; TG, triglyceride; UEI, urban employee insurance; URI, urban resident insurance.
The UEI and higher monthly household income per capita constituted protective factors against DR. Participants with UEI had a 29% lower risk for DR than those with URI or NCMS. Furthermore, every 1000 RMB increase in monthly household income per capita decreased the DR risk by 12%. Middle and primary school or lower level education were associated with a 1.69 and 1.53 times higher risk of DR than that associated with high school and higher education. Participation in the diabetes management programme and reaching the target values of SBP were associated with a reduction in the DR risk by 28% and 25%, respectively (figure 3).
Figure 3.
Regression analysis results of socioeconomic factors affecting diabetic retinopathy. *p<0.1, **p<0.05, ***p<0.01. DBP, diastolic blood pressure; NCMS, new rural cooperative medical scheme; UEI, SBP, systolic blood pressure; UEI, urban employee insurance; URI, urban resident insurance.
Discussion
Our study presents novel findings on glycaemic management (HbA1c) and DR diagnosis among participants with diabetes in Sichuan Province, western China. First, the study shows disparities in the effect of socioeconomic factors, including the place of residence and type of medical insurance available, on glycaemic control (HbA1c). The adjusted HbA1c control rate in our study (36.52%) was lower than the national level in China (50.1% in 2018) and the USA (50.5% in 2015–2018).17 20 The decreased HbA1c control rate in rural areas was consistent with that of a previous Chinese nationwide study (treated: 44.1% in rural areas vs 54.1% in urban areas).17 Women seem to have relatively better HbA1c status than men, although this did not affect the DR rates.
In China, although those with SHI usually have public healthcare insurance, there is a significant disparity in the reimbursement rates, covered services and benefit packages across different insurance types. The UEI has wide coverage and relatively higher reimbursement ratios.25–27 This study comprised a higher proportion of participants with HbA1c<7%, a lower proportion of DR and better self-reported vision in the UEI group than in the URI and NCMS group. The findings of participants with diabetes further confirmed the conclusions of some previous studies that the NCMS failed to improve outcomes in China (eg, hospitalised treatment in the NCMS group vs UEI and URI groups, 17.7% vs 24.2% and 24.9%),25 32 or eliminate inequalities in access to healthcare and treatment due to differences in insurance schemes,33 which constitute common issues worldwide. For example, individuals who were insured through the formal sector had a 3.31, 1.47 and 2.23 times higher probability of being diagnosed with diabetes in Colombia, Mexico and the USA, respectively, than uninsured individuals.10 34 The distribution of DR levels in the right and left eyes indicated that many people were in an intermediate stage of disease progression, which implied a risk for marked visual impairment. Moreover, a lower income was associated with a higher risk of high HbA1c levels, and this effect was significant for DR. Furthermore, in terms of medical resource application, people with diabetes who tested their HbA1c regularly (every 3 months) in medical institutions could better manage their HbA1c levels, which may have been associated with more regular communication with doctors and greater access to supportive management. The study suggests that flexible medical insurance (reducing gaps in financing patterns and reimbursement ratios) and extensive socioeconomic assistance may facilitate the access of low-income people with diabetes to health resources and reduce the burdens of diabetes and the associated complications. The relationship between higher education levels and a lower risk of DR in this study suggests the need to close the gap caused by educational background. Health awareness campaigns may help improve patients’ knowledge of diabetes and its complications, including options for treatment and prevention.
Furthermore, achievement of target values of lipid indicators was used to adjust the HbA1c control models; the effects of two blood lipids (TC and TG) were significant. Achieving the target SBP value was beneficial for reducing the HbA1c level and risk of DR. Based on overall evidence, we recommend that in China, doctors should focus on blood glucose (eg, HbA1c) and SBP management. Furthermore, doctors should encourage exercise and diet control in the early stages of diabetes.
This study had the following limitations. First, the cross-sectional study design made it difficult to derive causal relationships. Second, the household income per capita data were incomplete; thus, the presented results of income may be inaccurate, despite imputation. As this study is part of a national project, the sampling process is influenced by the overall design. Although this study obtained the estimated sample size based on a formula that could use the previous DR prevalence to explain the rationality to some extent, the sample size was limited. In addition, information on the management and treatment of people with DR is limited. In the future, expanding the survey sample and collecting more information on public health investment and environmental construction are expected to be collected to further explore the fairness of management.
Overall, our results show disparities in the effect of socioeconomic factors on HbA1c management and DR diagnosis among people with diabetes in Sichuan Province, China, which might be attributable to the difference in the locations of residence, insurance schemes, accessibility to HbA1c testing and household income per capita. Improving the living environment (ie, facilities), insurance benefits (specifically for URI and NCMS) and social security for the low-income population may help improve the health outcomes of patients with diabetes in China. Changes implemented at the community and national levels may help patients with lower socioeconomic status access better HbA1c management, education and early detection of DR, which could reduce the disease burden of diabetes-related complications.
Supplementary Material
Acknowledgments
The authors thank Hejia, Xu Hao and Zhang Chenghui for their helpful comments with regard to this manuscript. The authors thank the national and provincial workgroup members and staff of the local Centers for Disease Control and Prevention for conducting the survey. We thank the respondents for their participation in this study.
Footnotes
Contributors: XX and WY developed this study’s analytical strategy and conceptual framework. XX, XW, YD, JK, XZ, TD and JZ performed surveys and data extraction. WY and XZ conducted the literature review and assisted in the data analyses. XX was mainly responsible for the data analyses and drafted the first version of the manuscript. WY provided valuable suggestions and revised the manuscript accordingly. CL and LL provided valuable suggestions and a county-level environmental data. XW and YD provided administrative, technical and material support. XX and XW are responsible for the overall content as guarantor. All the authors critically reviewed and approved the final manuscript.
Funding: This study was supported by the Tianfu famous doctor fund. The China Scholarship Council (No. 201908510072) supported XX.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The socioeconomic data of city units may be obtained from the public national and provincial statistics website (https://data.stats.gov.cn/easyquery.htm?cn=C01, https://mzt.sc.gov.cn/scmzt/zcfg2/2017/11/14/e29db6312f6440d593f8a62a13f83cd9.shtml). https://mzt.sc.gov.cn/scmzt/zcfg2/2017/11/14/b7aa43cb7cce485ea88c0403c93b8bf8.shtml). The data on diabetes are currently unavailable publicly owing to legal restrictions and the rules of the project; however, these data may be obtained from the corresponding author after approval of an application with a reasonable request that is submitted to the Sichuan Centre for Disease Control and Prevention.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the Shanghai Sixth People’s Hospital Ethics Committee (approval number: 2 018-010), and participants provided written informed consent. Participants gave informed consent to participate in the study before taking part.
References
- 1.World Health Organization . Key facts of diabetes. 2021. Available: https://www.who.int/news-room/fact-sheets/detail/diabetes [Accessed 1 Apr 2022].
- 2.International Diabetes Federation . IDF diabetes atlas. 2021. Available: https://diabetesatlas.org/ [accessed 1 May 2022]. [Google Scholar]
- 3.Diabetes in china. 2022. Available: https://www.diabetes.co.uk/global-diabetes/diabetes-in-china.html [Accessed 18 Jun 2022].
- 4.China Centre for Disease Control and Prevention . Report on chronic disease risk factor surveillance in china 2018. 1st ed. Beijing, China: People’s Medical Publishing House, 2021: 2–20. [Google Scholar]
- 5.National Bureau of Statistics of China . National data. Available: https://data.stats.gov.cn/easyquery.htm?cn=C01 [Accessed 1 May 2022].
- 6.Sichuan Centre for Disease Control and Prevention . Report on chronic disease and nutrition surveillance in sichuan 2018. 1st ed. Chengdu, China: University of Electronic Science and Technology of China Press, 2021: 1–5. [Google Scholar]
- 7.Investigation Group for Chronic Diabetic Complications, Chinese Diabetes Society, Chinese Medical Association . Chronic diabetic complications and related macro-vascular diseases of inpatients with diabetes in mainland of china: a national retrospective analysis in recent 10 years. Chin J Diabetes 2003;11:232–7. Available: http://en.cnki.com.cn/Article_en/CJFDTOTAL-ZGTL200304001.htm [Google Scholar]
- 8.Ma RCW. Epidemiology of diabetes and diabetic complications in china. Diabetologia 2018;61:1249–60. 10.1007/s00125-018-4557-7 [DOI] [PubMed] [Google Scholar]
- 9.Song P, Yu J, Chan KY, et al. Prevalence, risk factors and burden of diabetic retinopathy in china: a systematic review and meta-analysis. J Glob Health 2018;8:010803. 10.7189/jogh.08.010803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gakidou E, Mallinger L, Abbott-Klafter J, et al. Management of diabetes and associated cardiovascular risk factors in seven countries: a comparison of data from national health examination surveys. Bull World Health Organ 2011;89:172–83. 10.2471/BLT.10.080820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic retinopathy preferred practice pattern®. Ophthalmology 2020;127:66–145. 10.1016/j.ophtha.2019.09.025 [DOI] [PubMed] [Google Scholar]
- 12.Chen R, Li N-X, Liu X. Study on the equity of medical services utilization for elderly enrolled in different basic social medical insurance systems in an underdeveloped city of southwest china. Int J Equity Health 2018;17:54. 10.1186/s12939-018-0765-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu J, Zheng J, Xu L, et al. Equity of health services utilisation and expenditure among urban and rural residents under universal health coverage. Int J Environ Res Public Health 2021;18:593. 10.3390/ijerph18020593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu X, Zeng J, Yang W, et al. Prevalence of metabolic syndrome among the adult population in western china and the association with socioeconomic and individual factors: four cross-sectional studies. BMJ Open 2022;12:e052457. 10.1136/bmjopen-2021-052457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hou XH, Wang LM, Chen SY, et al. Data resource profile: a protocol of china national diabetic chronic complications study. Biomed Environ Sci 2022;35:633–40. 10.3967/bes2022.078 [DOI] [PubMed] [Google Scholar]
- 16.Gorstein J, Sullivan KM, Parvanta I, et al. Indicators and methods for cross-sectional surveys of vitamin and mineral status of populations. 2007. Available: http://motherchildnutrition.org/nutrition-protection-promotion/pdf/mcn-micronutrient-surveys.pdf
- 17.Wang L, Peng W, Zhao Z, et al. Prevalence and treatment of diabetes in china, 2013-2018. JAMA 2021;326:2498–506. 10.1001/jama.2021.22208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in china in 2013. JAMA 2017;317:2515–23. 10.1001/jama.2017.7596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alzubaidi H, Sulieman H, Mc Namara K, et al. The relationship between diabetes distress, medication taking, glycaemic control and self-management. Int J Clin Pharm 2022;44:127–37. 10.1007/s11096-021-01322-2 [DOI] [PubMed] [Google Scholar]
- 20.Fang M, Wang D, Coresh J, et al. Trends in diabetes treatment and control in U.S. adults, 1999-2018. N Engl J Med 2021;384:2219–28. 10.1056/NEJMsa2032271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization 2020 (WHO/UCN/NCD/20.1). Licence: CC BY-NC-SA 3.0 IGO . Diagnosis and management of type 2 diabetes (HEARTS-D). Geneva.: Available: https://www.who.int/publications/i/item/who-ucn-ncd-20.1 [Accessed 1 May 2022]. [Google Scholar]
- 22.Diabetes Federation . IDF clinical practice recommendations for managing type 2 diabetes in primary care guidelines. 2017. Available: https://www.idf.org/our-activities/care-prevention/type-2-diabetes.html [Accessed 1 May 2022]. [DOI] [PubMed]
- 23.National Institute for Health and Care Excellence . Type 2 diabetes in adults: management. 2015. Available: https://www.nice.org.uk/guidance/ng28 [Accessed 1 May 2022]. [PubMed]
- 24.Chinese Diabetes Society . Guideline for the prevention and treatment of type 2 diabetes mellitus in china. Chin J Diabetes Mellitus 2021;13:315–409. 10.3760/cma.j.cn115791-20210221-00095 [DOI] [Google Scholar]
- 25.Chen R, Li NX, Liu X. Study on the equity of medical services utilization for elderly enrolled in different basic social medical insurance systems in an underdeveloped city of southwest china. Int J Equity Health 2018;17:54. 10.1186/s12939-018-0765-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhu K, Zhang L, Yuan S, et al. Health financing and integration of urban and rural residents’ basic medical insurance systems in china. Int J Equity Health 2017;16:194. 10.1186/s12939-017-0690-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li H, Jiang L. Catastrophic medical insurance in china. Lancet 2017;390:1724–5. 10.1016/S0140-6736(17)32603-X [DOI] [PubMed] [Google Scholar]
- 28.Guideline for primary care of dyslipidemias. Chinese Journal of General Practitioners 2019;18:406–16. doi:10.3760%2Fcma.j.issn.1671-7368.2019.05.003 [Google Scholar]
- 29.Rubin DB. Statistical matching using file concatenation with adjusted weights and multiple imputations. Journal of Business & Economic Statistics 1986;4:87. 10.2307/1391390 [DOI] [Google Scholar]
- 30.Morris TP, White IR, Royston P. Tuning multiple imputation by predictive mean matching and local residual draws. BMC Med Res Methodol 2014;14:75. 10.1186/1471-2288-14-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allison P. Imputation by predictive mean matching: promise & peril statistical horizons. Available: https://statisticalhorizons.com/predictive-mean-matching/ [Accessed 1 Apr 2022].
- 32.Zhang F, Shi X, Zhou Y. The impact of health insurance on healthcare utilization by migrant workers in china. Int J Environ Res Public Health 2020;17:1852. 10.3390/ijerph17061852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Luo Z, Fabre G, Rodwin VG. Meeting the challenge of diabetes in china. Int J Health Policy Manag 2020;9:47–52. 10.15171/ijhpm.2019.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim TJ, Vonneilich N, Lüdecke D, et al. Income, financial barriers to health care and public health expenditure: a multilevel analysis of 28 countries. Soc Sci Med 2017;176:158–65. 10.1016/j.socscimed.2017.01.044 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-067475supp001.pdf (419.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The socioeconomic data of city units may be obtained from the public national and provincial statistics website (https://data.stats.gov.cn/easyquery.htm?cn=C01, https://mzt.sc.gov.cn/scmzt/zcfg2/2017/11/14/e29db6312f6440d593f8a62a13f83cd9.shtml). https://mzt.sc.gov.cn/scmzt/zcfg2/2017/11/14/b7aa43cb7cce485ea88c0403c93b8bf8.shtml). The data on diabetes are currently unavailable publicly owing to legal restrictions and the rules of the project; however, these data may be obtained from the corresponding author after approval of an application with a reasonable request that is submitted to the Sichuan Centre for Disease Control and Prevention.