This cohort study assesses the cumulative incidence of glaucoma-related adverse events and factors associated with these adverse events in children during the first 5 years after lensectomy.
Key Points
Question
What were the cumulative incidence and factors associated with risk of glaucoma-related adverse events (glaucoma or glaucoma suspect) during the first 5 years following lensectomy performed in children aged 12 years or younger?
Findings
In this cohort study of 810 children (1049 eyes), glaucoma-related adverse events developed in 29% of aphakic eyes and were associated with age less than 3 months at time of surgery and with other anterior segment abnormalities. Glaucoma-related adverse events developed in 7% of pseudophakic eyes.
Meaning
The high incidence of glaucoma-related adverse events in aphakic and pseudophakic eyes found in this study suggests the need for close monitoring for glaucoma after lensectomy.
Abstract
Importance
Glaucoma can develop following cataract removal in children.
Objective
To assess the cumulative incidence of glaucoma-related adverse events (defined as glaucoma or glaucoma suspect) and factors associated with risk of these adverse events in the first 5 years after lensectomy prior to 13 years of age.
Design, Setting, and Participants
This cohort study used longitudinal registry data collected at enrollment and annually for 5 years from 45 institutional and 16 community sites. Participants were children aged 12 years or younger with at least 1 office visit after lensectomy from June 2012 to July 2015. Data were analyzed from February through December 2022.
Exposures
Usual clinical care after lensectomy.
Main Outcomes and Measures
The main outcomes were cumulative incidence of glaucoma-related adverse events and baseline factors associated with risk of these adverse events.
Results
The study included 810 children (1049 eyes); 443 eyes of 321 children (55% female; mean [SD] age, 0.89 [1.97] years) were aphakic after lensectomy, and 606 eyes of 489 children (53% male; mean [SD] age, 5.65 [3.32] years) were pseudophakic. The 5-year cumulative incidence of glaucoma-related adverse events was 29% (95% CI, 25%-34%) in 443 eyes with aphakia and 7% (95% CI, 5%-9%) in 606 eyes with pseudophakia; 7% (95% CI, 5%-10%) of aphakic eyes and 3% (95% CI, 2%-5%) of pseudophakic eyes were diagnosed as glaucoma suspect. Among aphakic eyes, a higher risk for glaucoma-related adverse events was associated with 4 of 8 factors, including age less than 3 months (vs ≥3 months: adjusted hazard ratio [aHR], 2.88; 99% CI, 1.57-5.23), abnormal anterior segment (vs normal: aHR, 2.88; 99% CI, 1.56-5.30), intraoperative complications at time of lensectomy (vs none; aHR, 2.25; 99% CI, 1.04-4.87), and bilaterality (vs unilaterality: aHR, 1.88; 99% CI, 1.02-3.48). Neither of the 2 factors evaluated for pseudophakic eyes, laterality and anterior vitrectomy, were associated with risk of glaucoma-related adverse events.
Conclusions and Relevance
In this cohort study, glaucoma-related adverse events were common after cataract surgery in children; age less than 3 months at surgery was associated with elevated risk of the adverse events in aphakic eyes. Children with pseudophakia, who were older at surgery, less frequently developed a glaucoma-related adverse event within 5 years of lensectomy. The findings suggest that ongoing monitoring for the development of glaucoma is needed after lensectomy at any age.
Introduction
Childhood glaucoma is commonly associated with cataract surgery early in life. Prior reports have evaluated the incidence and factors associated with risk of glaucoma after lensectomy, with varied estimates depending on study design and participant characteristics.1,2,3,4,5,6,7,8,9,10,11,12 To our knowledge, factors associated with risk of glaucoma following cataract removal have not been prospectively studied in a large cohort of children undergoing lensectomy prior to 13 years of age.
The Pediatric Eye Disease Investigator Group (PEDIG) developed a registry to collect data over 5 years on children undergoing lensectomy prior to 13 years of age.13,14 We evaluated the 5-year cumulative incidence for glaucoma-related adverse events and factors associated with risk of glaucoma-related adverse events within 5 years of cataract surgery.
Methods
The protocol for this cohort study and Health Insurance Portability and Accountability Act–compliant informed consent forms were approved by each participating site’s institutional review board. A list of participating sites is published elsewhere.12 The parent or guardian of each child provided written informed consent for the data collection, and assent was obtained from older children in accordance with institutional review board requirements. Participants and parents or guardians did not receive any incentives or compensation. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Population
The study was designed as a clinical research registry, reported in detail elsewhere.12 Medical and ophthalmic data were collected from medical record review at enrollment and at annual record reviews thereafter through 5 years of initial surgery. If a lensectomy had been performed on the second eligible eye, data from both eyes were included. Overall, 994 children (1382 eyes) aged 12 years or younger who had undergone unilateral or bilateral lensectomy during the preceding 45 days (between June 2012 and July 2015) were enrolled in the registry across 61 sites.12 Outcomes through 5 years of follow-up for the entire cohort are reported elsewhere.12,13,14,15 For this analysis of glaucoma-related adverse events, eyes with a preoperative diagnosis of glaucoma, glaucoma suspect, traumatic cataract, Lowe syndrome, or aniridia were excluded. Of the remaining eyes, 1050 (in 811 children) had at least one follow-up examination within 5.5 years (≤2008 days) of lensectomy in the first eye and were eligible for inclusion.
Ethnicity, race, and sex were reported by the parent or guardian. Race and ethnicity categories were American Indian/Alaska Native, Asian, Black/African American, Hispanic or Latino, White, more than 1 race, and unknown or not reported.
Study-Specific Definitions
Participants were classified as having unilateral or bilateral lensectomy. Bilateral surgery was defined as surgery in both eyes by the last completed annual data collection or by history of a lensectomy in the fellow eye prior to study enrollment. Glaucoma was defined as intraocular pressure (IOP) greater than 21 mm Hg and 1 of the following: abnormal corneal enlargement (≥11 mm), increased optic nerve cupping (≥0.2 increase in the horizontal cup-disc ratio from preoperative ratio), use of medication to reduce IOP, or glaucoma surgery.15 Glaucoma suspect was defined as an IOP greater than 21 mm Hg in the absence of a criterion for glaucoma. The sum of glaucoma and glaucoma suspect diagnoses are referred to as glaucoma-related adverse events.
Statistical Analysis
Data were analyzed from February through December 2022. Analyses were stratified by whether an intraocular lens (IOL) was implanted in the eye at the time of initial lensectomy (pseudophakia) or not (aphakia). The lack of overlap in age at surgery precluded comparisons between aphakic and pseudophakic eyes. Within each cohort, a Cox proportional hazards regression model was used to estimate the 5-year cumulative incidence and the corresponding 95% CI for developing a glaucoma-related adverse event. The model further evaluated whether the following factors reported at time of lensectomy were associated with developing a glaucoma-related adverse event: (1) age at lensectomy, with categories based on clinical input (<6 weeks, 6 weeks to <3 months, 3 months to <6 months, 6 months to <2 years, and 2 to <13 years among aphakic eyes; <3 years, 3 to <5 years, 5 to <8 years, and 8 to <13 years among pseudophakic eyes); (2) laterality (unilateral or bilateral); (3) performance of anterior vitrectomy (yes or no); (4) performance of other concomitant ocular surgeries (yes or no); (5) whether surgical complications were reported (yes or no); (6) presence of anterior segment abnormalities (yes or no); (7) sex (male vs female), and (8) parent- or guardian-identified race and ethnicity (White vs racial and ethnic minority groups). Racial and ethnic minority groups were combined in the analysis given the small number of participants in some groups and included those who were American Indian/Alaskan Native, Asian, Black/African American, Hispanic or Latino, and more than 1 race; unknown or not reported were not included in the analyses. Among aphakic eyes, given the number of events, all factors were included in the model when evaluating each factor (except for anterior vitrectomy, which was done for 97% of eyes). For pseudophakic eyes, which had few events, the model was limited to 2 factors (laterality and anterior vitrectomy). Collinearity or high correlation between factors in the model was evaluated; there were no covariates with a correlation greater than 0.80 or collinearity greater than 3.0. The robust sandwich variance estimator was used to adjust for the correlation between eyes of participants who underwent bilateral lensectomy. Factors were considered significant if the P value was <.01 to adjust for multiple testing, and 99% CIs were calculated. All analyses were repeated for the outcome of glaucoma alone and glaucoma suspect alone.
Visual acuity scores at 5 years were tabulated for eyes with glaucoma, glaucoma suspect, and eyes without a glaucoma-related adverse event or ocular complication(s) prior to 5 years. To compare the visual acuity at 5 years between bilateral aphakic eyes subsequently diagnosed with glaucoma and those with no glaucoma and no complications, the logMAR scores were transformed to Van der Waerden normal scores and compared using a linear mixed model adjusting for correlation between the eyes from the same participant. Analyses were performed using SAS, version 9.4 (SAS Institute Inc).
Results
There were 810 children (1049 eyes) included in these analyses; 443 eyes of 321 children (55% female; 45% male; mean [SD] age, 0.89 [1.97] years) were aphakic after lensectomy, and 606 eyes of 489 children (47% female; 53% male; mean [SD] age, 5.65 [3.32] years) were pseudophakic. Patient-level characteristics are detailed in eTable 1 in Supplement 1, and eye-level characteristics are detailed in Table 1. A total of 5 children (<1%) were American Indian/Alaska Native, 27 (3%) were Asian, 104 (13%) were Black/African American, 39 (5%) were Hispanic or Latino, 584 (72%) were White, 32 (4%) were more than 1 race, and 19 (2%) had unknown or unreported race and ethnicity. Median age at first lens surgery was 0.21 years (range, 0.04-12.40 years) in aphakic eyes and 5.32 years (range, 0.13-12.98 years) in pseudophakic eyes. We were unable to compare the development of glaucoma or glaucoma suspect between aphakic and pseudophakic eyes because most aphakic eyes in the cohort were from children younger than 6 months of age at time of lensectomy (237 [74%]) and most primary IOLs were placed in children older than 6 months (482 [99%]). Additional anterior segment abnormalities were reported twice as often with aphakia vs pseudophakia (63 eyes [14%] vs 42 eyes [7%]). Anterior vitrectomy at the initial lens surgery was performed in nearly every aphakic eye (428 [97%]) and in 357 pseudophakic eyes (59%). Most aphakic eyes in the cohort were from children younger than 6 months at time of lensectomy (237 [74%]), and most primary IOLs were placed in children older than 6 months (482 [99%]).
Table 1. Eye Characteristics According to Primary Intraocular Lens Implantation.
| Characteristic | Eyes, No. (%) | |
|---|---|---|
| Aphakia (n = 443) | Pseudophakia (n = 606) | |
| Age at lensectomy | ||
| <6 wk | 117 (26) | 0 |
| 6 wk to <3 mo | 134 (30) | 6 (<1) |
| 3 mo to <6 mo | 82 (19) | 4 (<1) |
| 6 mo to <2 y | 65 (15) | 84 (14) |
| 2 to <3 y | 6 (1) | 69 (11) |
| 3 to <5 y | 14 (3) | 133 (22) |
| 5 to <8 y | 12 (3) | 171 (28) |
| 8 to <13 y | 13 (3) | 139 (23) |
| Mean (SD), y | 0.89 (1.99) | 5.56 (3.27) |
| Median (range), y | 0.20 (0.04-12.44) | 5.23 (0.13-12.98) |
| Presence of anterior segment abnormalities at lensectomy | ||
| Yes | 63 (14) | 42 (7) |
| No | 372 (84) | 561 (93) |
| Unknown | 8 (2) | 3 (<1) |
| Operative complications at lensectomy | ||
| None | 419 (95) | 575 (95) |
| Ruptured posterior capsule | 3 (<1) | 11 (2) |
| Iris | ||
| Damage | 7 (2) | 2 (<1) |
| Prolapse | 1 (<1) | 5 (<1) |
| Anterior capsule tear | 0 | 4 (<1) |
| Retained lens material | 0 | 3 (<1) |
| IOL exchanged after insertion due to damage or malposition | 0 | 2 (<1) |
| Hyphema | 1 (<1) | 1 (<1) |
| Lens fragment in vitreous | 2 (<1) | 0 |
| Wound-related tear in Descemet membrane | 2 (<1) | 0 |
| Cloudy cornea | 0 | 1 (<1) |
| IOL dislocation | 0 | 1 (<1) |
| Iris bleeding | 1 (<1) | 0 |
| Anterior vitrectomy at lensectomy | ||
| Yes | 428 (97) | 357 (59) |
| No | 14 (3) | 237 (39) |
| Unknown | 1 (<1) | 12 (2) |
| Other eye surgeries performed at lensectomy | ||
| Yes | 44 (10) | 42 (7) |
| No | 396 (89) | 557 (92) |
| Unknown | 3 (<1) | 7 (1) |
Abbreviation: IOL, intraocular lens.
The 5-year cumulative incidence of glaucoma-related adverse events was 29% (95% CI, 25%-34%) in 443 eyes with aphakia (116 events) and 7% (95% CI, 5%-9%) in 606 eyes with pseudophakia (32 events); 7% (95% CI, 5%-10%) of aphakic eyes (28 events) and 3% (95% CI, 2%-5%) of pseudophakic eyes (14 events) were diagnosed as glaucoma suspect. Of the 47 participants who underwent bilateral lensectomy and had glaucoma-related adverse events, 11 (23%) had the event reported in only 1 eye and 36 (77%) had the event reported in both eyes. Figure 1 provides the cumulative incidences within each group.
Figure 1. Cumulative Incidence of Glaucoma-Related Adverse Events in Aphakic vs Pseudophakic Eyes.
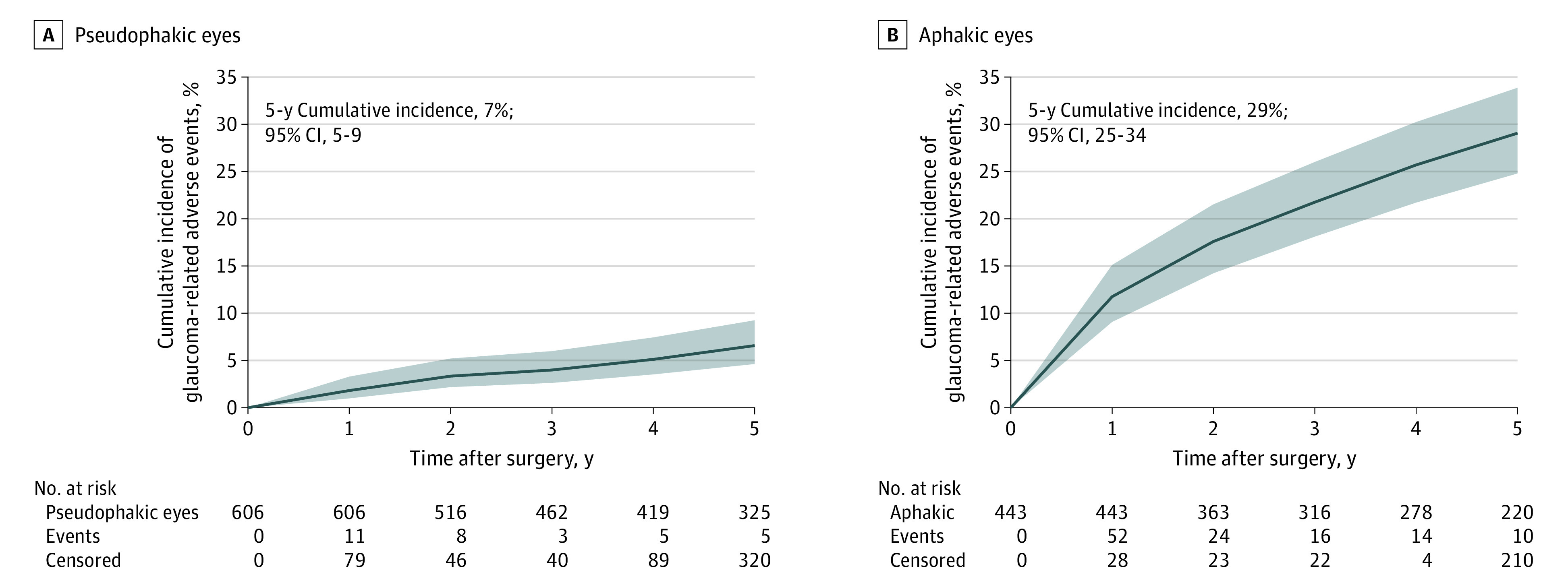
Shaded areas indicate 95% CIs.
Among aphakic eyes, a higher risk for a glaucoma-related adverse event within 5 years was associated with age less than 3 months (vs ≥3 months: adjusted hazard ratio [aHR], 2.88; 99% CI, 1.57-5.23), abnormal anterior segment (vs normal: aHR, 2.88; 99% CI, 1.56-5.30), intraoperative complications at time of lensectomy (none: aHR, 2.25; 99% CI, 1.04-4.87), and bilaterality (vs unilaterality: aHR, 1.88; 99% CI, 1.02-3.48) (Figure 2). The highest rates of glaucoma-related events were seen for infants younger than 6 weeks at lensectomy (44%; 95% CI, 35%-53%) and for infants 6 weeks to less than 3 months of age (35%; 95% CI, 28%-44%) (Figure 2). Among pseudophakic eyes, fewer children developed a glaucoma-related adverse event within 5 years (32 [5%]), and none of the factors evaluated was associated with an increased or decreased risk (Figure 3).
Figure 2. Development of Glaucoma-Related Adverse Events (AEs) According to Characteristics at Time of Lensectomy Among Children With Aphakic Eyes.
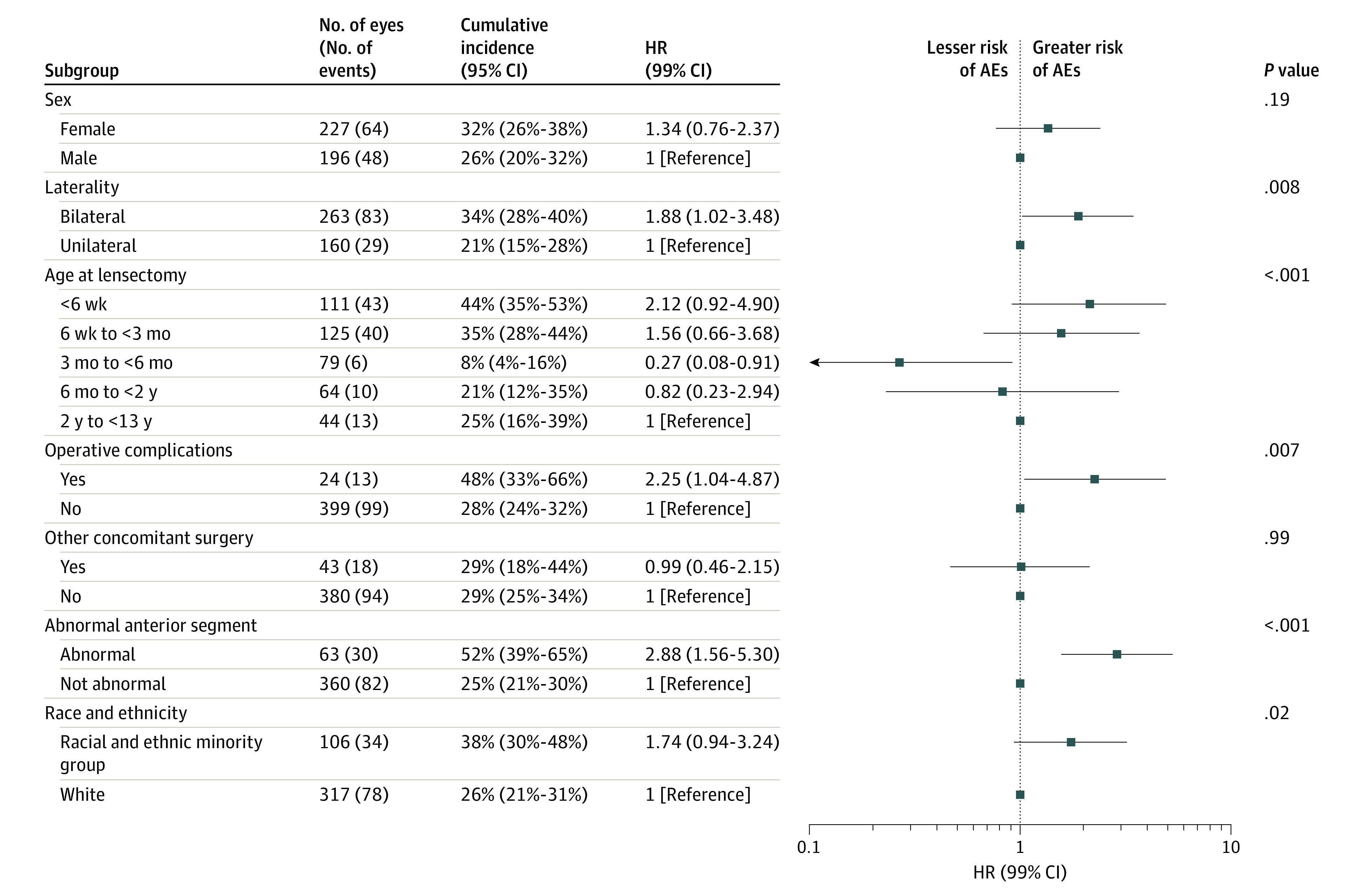
A Cox proportional hazards regression model was used to estimate the 5-year cumulative incidence of glaucoma-related AEs. The robust sandwich variance estimator was used to adjust for the correlation between eyes of participants who contributed data from both eyes to the analysis. The date of the glaucoma-related AE was not collected, so the date of the most recent office visit at which the complication was reported was used to estimate the cumulative incidence. Office visits were included in the analysis if reported up to 5.5 years following lensectomy to estimate the cumulative incidence (referred to as 5-year incidence). Hazard ratios (HRs) are adjusted estimates from a Cox proportional hazards regression model including all factors listed as categorical covariates. P ≤ .01 was considered significant. Observations with missing or unknown values in any of the subgroup factors were not included in the model.
Figure 3. Development of Glaucoma-Related Adverse Events (AEs) According to Characteristics at Time of Lensectomy Among Children With Pseudophakic Eyes.
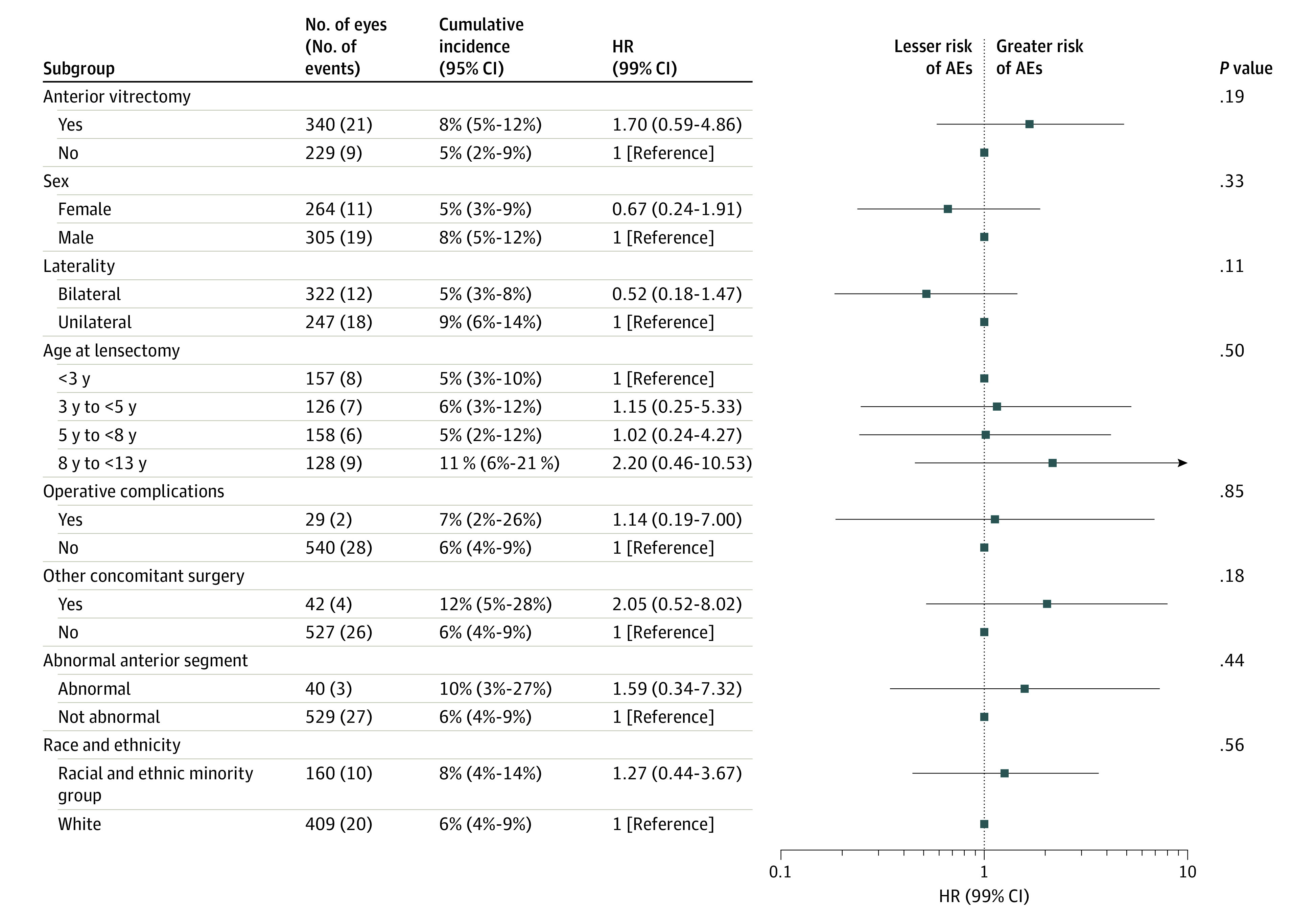
A Cox proportional hazards regression model was used to estimate the 5-year cumulative incidence of glaucoma-related AEs. The robust sandwich variance estimator was used to adjust for the correlation between eyes of participants who contributed data from both eyes to the analysis. The date of the glaucoma-related AE was not collected, so the date of the most recent office visit at which the complication was reported was used to estimate the cumulative incidence. Office visits were included in the analysis if reported up to 5.5 years following lensectomy to estimate the cumulative incidence (referred to as 5-year incidence). Hazard ratios (HRs) are adjusted estimates from a Cox proportional hazards regression model. The model was limited to 3 factors as categorical (laterality, anterior vitrectomy, and both). If the factor of interest was laterality or anterior vitrectomy, only 2 factors were included in the model. P ≤ .01 was considered significant. Observations with missing or unknown values in any of the subgroup factors were not included in the model.
Glaucoma surgery was performed in 33 of 443 aphakic eyes (7%) and 3 of 606 pseudophakic eyes (0.5%) during the first 5 years after lensectomy. The types of surgery among aphakic eyes included trabeculectomy (n = 5), trabeculotomy (n = 5), trabeculotomy and trabeculectomy combined (n = 3), goniotomy (n = 4), glaucoma drainage device (n = 8), endocyclophotocoagulation (n = 1), glaucoma drainage device with endocyclophotocoagulation (n = 1), peripheral iridectomy with anterior vitrectomy (n = 1), selective laser trabeculoplasty (n = 1), and unknown surgical type (n = 4) (eTable 2 in Supplement 1). Among aphakic eyes requiring glaucoma surgery, 29 of 33 (88%) were in children younger than 3 months at the time of their lensectomy, and in 15 (45%) of these 33 eyes, glaucoma surgery was performed within 6 months of cataract surgery (median, 7.1 months [range, 0.9-57.9 months).
Visual acuity 5 years after lens surgery for eyes with a glaucoma-related adverse event varied based on laterality of the cataract surgery and use of an IOL (Table 2). The median visual acuity among 41 eyes with bilateral aphakia subsequently diagnosed with glaucoma (20/80 [IQR, 20/40-20/160]) was worse than the median visual acuity observed for 109 eyes with bilateral aphakia without glaucoma or other complications (20/63 [IQR, 20/40-20/100]) (P = .03).
Table 2. Visual Acuity at 5 Years by Subgroup in Children Developing Glaucoma or Glaucoma Suspect and Children Without Ocular Complications.
| Subgroup | Eyes, No. | Visual acuity, Snellen fraction | ||
|---|---|---|---|---|
| Median (IQR) | Best | Worst | ||
| Glaucoma | ||||
| Bilateral | ||||
| Aphakia | 41 | 20/80 (20/40-20/160) | 20/20 | <20/800 |
| Pseudophakia | 2 | 20/32 (20/25-20/32) | 20/25 | 20/32 |
| Unilateral | ||||
| Aphakia | 17 | 20/50 (20/50-20/250) | 20/32 | <20/800 |
| Pseudophakia | 6 | 20/125 (20/40-20/200) | 20/40 | 20/400 |
| Glaucoma suspect | ||||
| Bilateral | ||||
| Aphakia | 7 | 20/32 (20/32-20/63) | 20/25 | 20/63 |
| Pseudophakia | 2 | 20/50 (20/40-20/63) | 20/40 | 20/63 |
| Unilateral | ||||
| Aphakia | 7 | 20/125 (20/80-20/640) | 20/80 | <20/800 |
| Pseudophakia | 7 | 20/125 (20/63-20/160) | 20/32 | <20/800 |
| No glaucoma and/or ocular complications a | ||||
| Bilateral | ||||
| Aphakia | 109 | 20/63 (20/40-20/100) | 20/12 | <20/800 |
| Pseudophakia | 175 | 20/32 (20/25-20/50) | 20/16 | <20/800 |
| Unilateral | ||||
| Aphakia | 85 | 20/200 (20/50-20/640) | 20/20 | <20/800 |
| Pseudophakia | 148 | 20/63 (20/32-20/200) | 20/16 | <20/800 |
No glaucoma-related adverse event (glaucoma, glaucoma suspect, or glaucoma surgery) and no ocular complication at any time through 5 years of follow up.
Discussion
In this large, prospective cohort study using a cataract surgery registry, we evaluated the 5-year cumulative incidence of developing a glaucoma-related adverse event in children aged 12 years or younger at the time of their initial lensectomy. Glaucoma-related adverse events were frequent with surgery in infancy (mostly aphakic eyes) and uncommon in children 1 to 12 years of age (mostly pseudophakic eyes). We were unable to compare the development of glaucoma or glaucoma suspect between aphakic and pseudophakic eyes because most aphakic eyes in the cohort were from children younger than 6 months (74%) at time of lensectomy and most primary IOLs were placed in children older than 6 months (99%).
Glaucoma-related adverse events were most common among aphakic eyes when lensectomy was performed within the first 6 weeks of life (44%) and between 6 weeks and 3 months of age (35%). Our finding of increased risk in the first 3 months of life is consistent with the 5-year risk of a glaucoma-related adverse event (15%-31%) identified in other randomized clinical trials or multicenter cohort studies evaluating lensectomy performed in the first 3 months of life.1,2,3,4,5,6,7,8,9,10 These include the Infant Aphakia Treatment Study (IATS) (birth to 6 months of age),1,2,3 IoLunder2 (birth to 2 years of age),4,5 the Swedish National Pediatric Cataract Registry (PECARE) (birth to 8 years of age),9 and the Toddler Aphakia and Pseudophakia Study (TAPS) (6 months to 2 years of age).6,7,8 The PECARE registry9 (288 eyes with follow-up) identified an increased risk of glaucoma associated with early surgery, with the majority of children with glaucoma having lensectomy prior to 3 months of age and 73% having a history of lensectomy in the first month of life. Of note, IATS,1,2,3 IoLunder2,4,5 and TAPS6,7,8 excluded certain high-risk eyes from enrollment or analysis and studied eyes of younger children, whereas the PECARE9 and PEDIG13,14,15 cataract registries included cataract associated with a range of comorbidities, including microcornea, persistent fetal vasculature, and other ocular diseases. The first 3 months of life have also been identified as the highest risk period for development of glaucoma in retrospective case series.11,16 Surgeons should be cautious when considering cataract surgery in the first 6 weeks of life given data suggesting that this is the highest risk period for development of postoperative glaucoma.
It is notable that no child in IoLunder2 developed glaucoma during 5 years of follow-up if the lensectomy was performed after 6 months of life.4,5 This observation was true for surgery performed after 7.5 months of age in a case series of 147 eyes by Ruddle et al11 and after 12 months of age in the PECARE registry,9 with mean 3.31 years follow-up. The TAPS registry,6,8 a retrospective study of children 7 to 24 months of age at lensectomy with 5 years of follow-up, documented that the risk of developing glaucoma-related events was less than 5% for unilateral and bilateral cases. With a clinical population and wide range of ocular phenotypes, the PEDIG cataract registry12,13,14 found that the risk of glaucoma after 6 months of age was low for both eyes with aphakia and eyes with pseudophakia but remained present if cataract surgery was performed at any age up to and including 12 years (the oldest age in the present study).
The large number of aphakic infant eyes in our study provided the opportunity to evaluate additional factors associated with risk of glaucoma, including laterality, intraoperative findings, and demographic variables. We found a higher risk for glaucoma and glaucoma-related adverse events for bilateral aphakic eyes vs unilateral aphakic eyes. The IoLunder24,5,6,8 and PECARE9 studies found a higher rate of glaucoma-related adverse events in bilateral cases, whereas the TAPS studies did not. Because all ocular phenotypes were included in the PEDIG registry,7,17 the higher rate of glaucoma in bilateral cases may be related to the familial, systemic, or ocular anomalies commonly identified in children with bilateral cataracts. Anterior segment abnormalities at surgery were also associated with elevated risk of glaucoma in our study. A population-based observational study4,5 suggested that significant ocular comorbidity is associated with additional risk for postoperative glaucoma. Although microophthalmia has been implicated as such a risk factor, recent studies suggest that eyes with microcornea may deserve the closest monitoring postoperatively.1,2,3,6,7,8 We found elevated glaucoma risk in aphakic cases in which operative complications occurred at the time of lensectomy. This association was not identified in the IATS1,2,3 or TAPS6,7,8 studies, whether due to their smaller size or their more standardized protocol and selected surgeon group. In addition, in the present study, this association was not found in the mostly older children with pseudophakic eyes in the PEDIG registry. Concomitant surgeries (eg, corneal transplant) during cataract surgery were uncommon and did not appear to be associated with elevated risk for glaucoma and glaucoma-related adverse events. Glaucoma surgery was performed in 33 of 443 aphakic eyes (7%), with 29 eyes (88%) in children younger than 3 months at lensectomy. This rate of surgery was less than that reported in IoLunder2 (14%),4,5 IATS,1,2,3 (9%) and PECARE (23.7%)9 by 5 years.
In the current study, children with pseudophakic eyes had less than a 1 in 10 chance of developing a glaucoma-related adverse event within 5 years of lensectomy. This study was limited with respect to evaluating the effect of age in young children because there were only 10 eyes in children younger than 6 months at the time of lensectomy with primary IOL placement. When cataract surgery was performed after 1 year of age, no patient in the IoLunder2 study4,5 was diagnosed with glaucoma by 5 years follow-up. However, the larger, present study using the PEDIG registry and enrolling children aged 12 years or younger found that the risk of glaucoma-related adverse events was not 0 with primary IOL insertion in older children.
With respect to visual acuity through 5 years of follow up, bilateral aphakic eyes with glaucoma-related events were significantly worse than eyes without glaucoma-related events (median, 20/80 vs 20/63). Eyes with glaucoma in IoLunder24,5 had worse median visual acuity than those without; however, this difference was not statistically significant. Glaucoma after pediatric lensectomy did not impact visual acuity in 2 series from Australia and Sweden.4,5,11 Glaucoma-related events were uncommon in children with pseudophakic eyes in our study; therefore, an assessment of associations with visual acuity outcomes in that group was not possible.
Limitations
Limitations of this registry-based study include a lack of overlap in age between the cohorts with pseudophakic and aphakic eyes. Because children younger than 6 months typically had aphakic eyes and children aged 6 months or older commonly received an IOL, the association of IOL implantation with glaucoma or glaucoma-related adverse events could not be analyzed. Additionally, our study definition of glaucoma differed from that in the Childhood Glaucoma Consensus18 and other multicenter studies.1,2,3 In those studies, a child receiving topical medication but lacking anatomical signs or changes consistent with glaucoma was given a diagnosis of glaucoma suspect, whereas in the current study, such a child was considered to have glaucoma. Although the glaucoma diagnosis incidence may have been slightly elevated owing to this difference in definitions, the incidence of glaucoma-related adverse events would be consistent with other studies. An additional limitation is substantial loss to completion of full 5 years of follow-up. However, the children who did and did not complete the full length of the study did not appear to differ in any important baseline characteristics. The number lost to follow-up reduces the precision of the cumulative incidence estimate resulting in a wider CI.
Conclusions
In this cohort study, glaucoma-related adverse events were common in aphakic eyes within 5 years of lensectomy. Age less than 3 months at surgery was associated with elevated risk of glaucoma-related adverse events in aphakic eyes. Children with pseudophakia, who were older at surgery, were less likely to develop a glaucoma-related adverse event. The incidence of glaucoma in aphakic and pseudophakic eyes increased slowly during follow-up, suggesting the need for continued monitoring for the development of glaucoma.
eTable 1. Participant Characteristics According to Primary Intraocular Lens Implantation
eTable 2. Eyes with Initial Glaucoma Surgery Performed in First Five Years following Lensectomy
Pediatric Eye Disease Investigator Group
Data Sharing Statement
References
- 1.Lambert SR, Lynn MJ, Hartmann EE, et al. ; Infant Aphakia Treatment Study Group . Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: a randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol. 2014;132(6):676-682. doi: 10.1001/jamaophthalmol.2014.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman SF, Lynn MJ, Beck AD, Bothun ED, Örge FH, Lambert SR; Infant Aphakia Treatment Study Group . Glaucoma-related adverse events in the first 5 years after unilateral cataract removal in the Infant Aphakia Treatment Study. JAMA Ophthalmol. 2015;133(8):907-914. doi: 10.1001/jamaophthalmol.2015.1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freedman SF, Beck AD, Nizam A, et al. ; Infant Aphakia Treatment Study Group . Glaucoma-related adverse events at 10 years in the Infant Aphakia Treatment Study: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol. 2021;139(2):165-173. doi: 10.1001/jamaophthalmol.2020.5664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solebo AL, Cumberland P, Rahi JS; British Isles Congenital Cataract Interest Group . 5-Year outcomes after primary intraocular lens implantation in children aged 2 years or younger with congenital or infantile cataract: findings from the IoLunder2 prospective inception cohort study. Lancet Child Adolesc Health. 2018;2(12):863-871. doi: 10.1016/S2352-4642(18)30317-1 [DOI] [PubMed] [Google Scholar]
- 5.Solebo AL, Rahi JS; British Congenital Cataract Interest Group . Glaucoma following cataract surgery in the first 2 years of life: frequency, risk factors and outcomes from IoLunder2. Br J Ophthalmol. 2020;104(7):967-973. doi: 10.1136/bjophthalmol-2019-314804 [DOI] [PubMed] [Google Scholar]
- 6.Bothun ED, Wilson ME, Traboulsi EI, et al. ; Toddler Aphakia and Pseudophakia Study Group (TAPS) . Outcomes of unilateral cataracts in infants and toddlers 7 to 24 months of age: Toddler Aphakia and Pseudophakia Study (TAPS). Ophthalmology. 2019;126(8):1189-1195. doi: 10.1016/j.ophtha.2019.03.011 [DOI] [PubMed] [Google Scholar]
- 7.Bothun ED, Wilson ME, Vanderveen DK, et al. Outcomes of bilateral cataracts removed in infants 1 to 7 months of age using the Toddler Aphakia and Pseudophakia treatment Study registry. Ophthalmology. 2020;127(4):501-510. doi: 10.1016/j.ophtha.2019.10.039 [DOI] [PubMed] [Google Scholar]
- 8.Bothun ED, Wilson ME, Yen KG, et al. ; Toddler Aphakia and Pseudophakia Study . Outcomes of bilateral cataract surgery in infants 7 to 24 months of age using the Toddler Aphakia and Pseudophakia Treatment Study registry. Ophthalmology. 2021;128(2):302-308. doi: 10.1016/j.ophtha.2020.07.020 [DOI] [PubMed] [Google Scholar]
- 9.Nyström A, Haargaard B, Rosensvärd A, Tornqvist K, Magnusson G. The Swedish National Pediatric Cataract Register (PECARE): incidence and onset of postoperative glaucoma. Acta Ophthalmol. 2020;98(7):654-661. doi: 10.1111/aos.14414 [DOI] [PubMed] [Google Scholar]
- 10.Vasavada AR, Vasavada V, Shah SK, et al. Five-year postoperative outcomes of bilateral aphakia and pseudophakia in children up to 2 years of age: A randomized clinical trial. Am J Ophthalmol. 2018;193:33-44. doi: 10.1016/j.ajo.2018.06.005 [DOI] [PubMed] [Google Scholar]
- 11.Ruddle JB, Staffieri SE, Crowston JG, Sherwin JC, Mackey DA. Incidence and predictors of glaucoma following surgery for congenital cataract in the first year of life in Victoria, Australia. Clin Exp Ophthalmol. 2013;41(7):653-661. doi: 10.1111/ceo.12067 [DOI] [PubMed] [Google Scholar]
- 12.Repka MX, Dean TW, Lazar EL, et al. ; Pediatric Eye Disease Investigator Group . Cataract surgery in children from birth to less than 13 years of age: baseline characteristics of the cohort. Ophthalmology. 2016;123(12):2462-2473. doi: 10.1016/j.ophtha.2016.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Repka MX, Dean TW, Kraker RT, et al. ; Writing Committee for the Pediatric Eye Disease Investigator Group (PEDIG) . Visual acuity and ophthalmic outcomes in the year after cataract surgery among children younger than 13 years. JAMA Ophthalmol. 2019;137(7):817-824. doi: 10.1001/jamaophthalmol.2019.1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freedman SF, Kraker RT, Repka MX, et al. ; Pediatric Eye Disease Investigator Group (PEDIG) . Incidence and management of glaucoma or glaucoma suspect in the first year after pediatric lensectomy. JAMA Ophthalmol. 2020;138(1):71-75. doi: 10.1001/jamaophthalmol.2019.4571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Repka MX, Dean TW, Kraker RT, et al. ; Pediatric Eye Disease Investigator Group . Visual acuity and ophthalmic outcomes 5 years after cataract surgery among children younger than 13 years. JAMA Ophthalmol. 2022;140(3):269-276. doi: 10.1001/jamaophthalmol.2021.6176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirwan C, Lanigan B, O’Keefe M. Glaucoma in aphakic and pseudophakic eyes following surgery for congenital cataract in the first year of life. Acta Ophthalmol. 2010;88(1):53-59. doi: 10.1111/j.1755-3768.2009.01633.x [DOI] [PubMed] [Google Scholar]
- 17.Nyström A, Almarzouki N, Magnusson G, Zetterberg M. Phacoemulsification and primary implantation with bag-in-the-lens intraocular lens in children with unilateral and bilateral cataract. Acta Ophthalmol. 2018;96(4):364-370. doi: 10.1111/aos.13626 [DOI] [PubMed] [Google Scholar]
- 18.Beck AD, Chang TC, Freedman SF. Definition, Classification and Differential Diagnosis. In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman SF, eds. Childhood Glaucoma: World Glaucoma Association Consensus Series 9. Kugler Publications; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Participant Characteristics According to Primary Intraocular Lens Implantation
eTable 2. Eyes with Initial Glaucoma Surgery Performed in First Five Years following Lensectomy
Pediatric Eye Disease Investigator Group
Data Sharing Statement


