Abstract
Background
In a suspected case of biliary obstruction with clinical and laboratory data suggesting obstructive jaundice, the major goal is to confirm the presence of obstruction, its nature and cause, location, and extent. Ultrasonography (USG) and magnetic resonance cholangiopancreatography (MRCP) are primarily used to diagnose suspected biliary tract illnesses. The aim of the study is to evaluate and compare the accuracy of MRCP and USG with endoscopic retrograde cholangiopancreatography (ERCP)/surgical/histopathological outcomes for finding the cause and level of obstruction in the case of clinically suspected biliary obstruction.
Methods
This was a prospective observational study conducted at Kalinga Institute of Medical Sciences and Pradyumna Bal Memorial Hospital, Bhubaneswar, India, from September 2020 to September 2022 on 120 patients. It included patients with clinical suspicion of biliary obstruction who underwent both USG and MRCP. Characteristics of the obstruction were evaluated for both benign and malignant lesions through USG and MRCP. The findings were then correlated with ERCP, histopathology, or surgery to calculate the diagnostic performance of the former two modalities.
Results
Out of 120 patients, USG was correctly able to predict the cause of obstruction in 40 patients. The sensitivity, specificity, and accuracy of detecting the nature of obstruction by USG were 33.3%, 84%, and 48.9%, respectively. The overall diagnostic accuracy of USG in predicting the site of obstruction was 64.3%. MRCP was correctly able to predict the cause of obstruction in 113 patients. The sensitivity, specificity, and accuracy of detecting the nature of obstruction by MRCP were 94.1%, 91.9%, and 94.8% respectively. The overall diagnostic accuracy of MRCP in predicting the site of obstruction was 98.33%. Out of 120 patients, no cause of biliary obstruction could be found in 71 patients by USG, out of which the correct diagnosis was made in 67 patients through MRCP.
Conclusion
USG should be used as the initial screening modality of choice for predicting the level and nature of obstruction in patients with a clinical suspicion of obstructive jaundice. MRCP should be the radiological investigation of choice in patients with clinical suspicion of obstructive jaundice. MRCP has the potential to become the new "Gold standard" investigation for diagnosis in patients with biliary obstruction owing to its excellent diagnostic performance, and non-invasiveness.
Keywords: imaging, ultrasonography, endoscopic retrograde cholangiopancreatography, magnetic resonance cholangiopancreatography, mri, ercp, biliary obstruction, mrcp, usg
Introduction
Obstructive jaundice is a prevalent clinical issue. In a suspected case of biliary obstruction with clinical and laboratory data suggesting obstructive jaundice, the major goal is to confirm the presence of obstruction, its nature and cause, location, and extent. Primarily, ultrasonography (USG) and magnetic resonance cholangiopancreatography (MRCP) are used to diagnose biliary tract illnesses.
Due to its many benefits, such as its simplicity of use, low cost, and lack of ionizing radiation, USG is used as the initial screening tool. The visualization of the distal common bile duct (CBD) and pancreas is limited in around 30% of instances due to obscuration caused by bowel gas [1,2]. MRCP, unlike USG, is not affected by bowel gas and gives a clear view of the hepatobiliary system [3]. It has inherent high contrast resolution, the ability to completely map the biliary ductal system, no need for contrast media, multiplanar capability, and virtually artifact-free display of anatomy and pathology in patients with biliary obstruction [4]. The aim of our study is to evaluate and compare the diagnostic performance of USG and MRCP with ERCP/surgical/histopathological outcomes for finding the cause and level of obstruction in the case of clinically suspected biliary obstruction.
Materials and methods
Study criteria
The study was a prospective observational study conducted at Kalinga Institute of Medical Sciences and Pradyumna Bal Memorial Hospital, Bhubaneswar, India, from September 2020 to September 2022. Patients with clinical suspicion of biliary obstruction who underwent both USG and MRCP were included in the study. Those patients who either went for only USG or MRCP were not included in the study.
Machines
Transabdominal USG was performed with Voluson™ S10 (GE HealthCare Technologies Inc., Chicago, Illinois, United States) and Affiniti 30 (Koninklijke Philips N.V., Amsterdam, Netherlands) machines using a curvilinear probe of 2-5 MHz frequency. MRCP was performed with a GE Signa HDxT 1.5 Tesla MRI machine using T1WI, coronal and axial T2 single-shot fast spin echo (SSFSE) pulse sequence, apparent diffusion coefficient (ADC), diffusion-weighted imaging (DWI), coronal and axial fast imaging employing steady-state acquisition (FIESTA), axial and coronal three-dimensional MRCP, and thick slab MRCP sequences.
The nature and level of obstruction were evaluated for both benign and malignant lesions through both modalities. The findings were then correlated with ERCP, histopathology, or surgery to calculate the diagnostic performance of USG and MRCP.
Results
During this two-year period, of the 120 patients who were referred for both USG and MRI, 57 (47.5%) were male and 63 (52.5%) were female, showing a slight female preponderance. The youngest patient was one year old and the oldest was 88 years old. The mean age of patients was 52.2 years (Figure 1).
Figure 1. Age distribution of the population.
Thirty patients (25%) had cholelithiasis without any signs of cholecystitis. Twenty-four patients (20%) had chronic calculus cholecystitis and eight patients (6.67%) had acute calculus cholecystitis. Gallbladder cancer was found in 17 patients (14.17%). Post-cholecystectomy status was noted in 16 patients (13.3%). No pathology was found in 14 patients (11.67%) (Figure 2).
Figure 2. Gallbladder status in the patients.
GB: gallbladder
In our study, benign pathology was found in 91 patients (75.8%), whereas malignant pathology was found in 29 patients (24.2%) (Figure 3). In benign lesions, 67 cases (55.8%) of choledocholithiasis were reported, out of which four were associated with other pathologies (one with carcinoma pancreas, one with a blocked self-expanding metallic stent (SEMS), and two with Mirizzi syndrome). Twelve cases (10%) of benign biliary stricture and five cases (4.1%) of Mirizzi syndrome were reported. Two cases (1.67%) each of intrahepatic hydatid cysts (Figure 4), ampullary stenosis, and periampullary diverticulum causing biliary obstruction were reported. In our study, the most common pathology leading to obstructive jaundice was choledocholithiasis. In malignant lesions, 17 cases (14.17%) of gallbladder carcinoma, followed by eight cases (6.67%) of cholangiocarcinoma and two cases (1.67% each) of pancreatic carcinoma and periampullary carcinoma were reported (Table 1).
Table 1. Total case distribution.
| 1. | Malignant | Periampullary Carcinoma | 2 |
| 2. | Carcinoma Pancreas | 2 | |
| 3. | Gallbladder Carcinoma | 17 | |
| 4. | Cholangiocarcinoma | 8 | |
| 5. | Benign | Ampullary Stenosis | 2 |
| 6. | Autoimmune Hepatitis | 1 | |
| 7. | Benign Biliary Stricture | 12 | |
| 8. | Biliary Sludge | 1 | |
| 9. | Choledocholithiasis | 63 | |
| 10. | Hydatid Cyst | 2 | |
| 11. | Mirizzi Syndrome | 5 | |
| 12. | Main Pancreatic Duct Stricture | 1 | |
| 13. | Periampullary Diverticulum | 2 | |
| 14. | Type IV A Choledochal Cyst | 1 | |
| 15 | Blocked Self-Expanding Metallic Stent with Choledocholithiasis | 1 |
Figure 3. Demographic characteristics of nature of lesions.
Figure 4. Intrahepatic hydatid cyst. (A) Axial three-dimensional reconstructed image shows serpentine-like floating structures, internal floating membranes; (B) Axial three-dimensional reconstructed image shows cysto-biliary communication through left hepatic duct.
Diagnostic performance of USG versus MRCP in benign lesions
Out of 91 patients presenting with a benign pathology, USG was able to correctly diagnose the cause in 19 patients (20.9%). In 66 patients (72.5%), no obstructive cause could be found. In three patients, Mirizzi syndrome was erroneously diagnosed as choledocholithiasis. A benign stricture of the left hepatic duct was missed in one patient post hepaticojejunostomy. In another patient, a benign distal CBD stricture was erroneously diagnosed as a type-1 choledochal cyst. A patient with a blocked self-expandable metallic stent in the CBD with features of biliary obstruction and porcelain gallbladder was erroneously suspected of having gallbladder carcinoma. The sensitivity, specificity, and accuracy in detecting benign lesions by USG were 20.9%, 79.3%, and 35% respectively.
Out of 91 patients presenting with a benign pathology, MRCP was able to correctly diagnose the cause in 87 patients (95.6%). One case of ampullary stricture was erroneously diagnosed as choledocholithiasis, and another case of choledocholithiasis was misdiagnosed as Mirizzi syndrome. Another case of blocked SEMS and choledocholithiasis with porcelain gallbladder was suspected to be carcinoma gallbladder (Figure 5). No cause of obstruction could be detected in one case, which was later found to be a small calculus in the ampullary region. The sensitivity, specificity, and accuracy in detecting benign lesions by MRCP were 95.6%, 89.6%, and 94.2%, respectively (Figure 6).
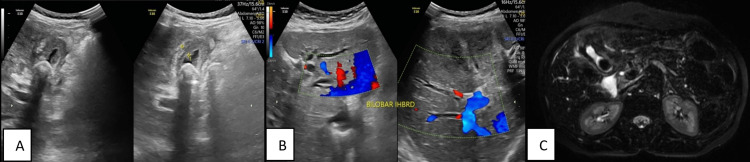
Figure 5. Blocked self-expanding metallic stent with porcelain GB. (A) Transabdominal ultrasonography shows calcified and thickened gallbladder wall; (B) Transabdominal USG shows dilated common bile duct with stent in situ and non-homogenous echogenic material; (C) Coronal T2 SSFSE shows cholelithiasis with porcelain GB and bilobar intrahepatic biliary radicle dilatation with common bile duct stent in situ; (D) Removal of blocked stent.
GB: gallbladder; SSFSE: single-shot fast spin echo
Figure 6. Diagnostic performance of USG and MRCP in estimating cause of obstruction in benign lesions.
MRCP: magnetic resonance cholangiopancreatography
Out of 120 patients, 67 were reported to have been associated with choledocholithiasis. In 53 patients, acalculous pathologies were reported. The sensitivity, specificity, and accuracy of detecting acalculous pathology by USG were 54.72%, 79.10%, and 68.33%, respectively. Out of 67 cases of choledocholithiasis, only 15 (23.4%) were diagnosed on USG whereas 65 cases (97%) were diagnosed on MRCP. The sensitivity, specificity, and diagnostic accuracy of USG and MRCP for choledocholithiasis were 22%, 92.4%, 53.3% and 97%, 98.1%, 97.5%, respectively.
Out of 22 patients with proximal CBD obstruction, USG was correctly able to predict the level of obstruction in 11 patients (sensitivity: 50%) and MRCP was correctly able to predict the level of obstruction in all patients (sensitivity: 100%). Out of 69 patients with distal CBD obstruction, USG was correctly able to predict the level of obstruction in 41 patients (sensitivity: 59.4%) and MRCP was correctly able to predict the level of obstruction in 67 patients (sensitivity: 97.1%). The diagnostic accuracy in predicting the level of obstruction for USG and MRCP came out to be 57.4% and 97.8%, respectively (Figure 7, Table 2).
Table 2. Level of obstruction in benign lesions.
MRCP: magnetic resonance cholangiopancreatography; ERCP: endoscopic retrograde cholangiopancreatography
| Histopathology/ERCP/Surgery | |||
| Proximal common bile duct | Distal common bile duct | ||
| USG | Proximal common bile duct | 11 | 0 |
| Inconclusive | 8 | 28 | |
| Distal common bile duct | 3 | 41 | |
| Proximal common bile duct | Distal common bile duct | ||
| MRCP | Proximal common bile duct | 22 | 1 |
| Inconclusive | 0 | 1 | |
| Distal common bile duct | 0 | 67 | |
Figure 7. Diagnostic performance of USG and MRCP in estimating level of obstruction in benign lesions.
MRCP: magnetic resonance cholangiopancreatography
Diagnostic performance of USG versus MRCP in malignant lesions
Out of 29 patients presenting with a malignant pathology, USG was able to correctly diagnose the cause in 21 patients (72.5%). In five (17.2%) patients, no cause of obstruction could be determined. Two patients were diagnosed with choledocholithiasis, which turned out to be gallbladder carcinoma with distal CBD mass and periampullary infiltrating carcinoma. One patient with gallbladder carcinoma was erroneously diagnosed with cholangiocarcinoma. The sensitivity, specificity, and accuracy in detecting malignant lesions by USG were 72.4%, 98.9%, and 92.5%, respectively.
Out of 29 patients presenting with a malignant pathology, MRCP was able to correctly diagnose the cause in 26 patients (89.6%). One case of periampullary carcinoma and one of pancreatic carcinoma were each diagnosed erroneously as benign distal CBD strictures. One case of cholangiocarcinoma was erroneously suspected to be Mirizzi syndrome with CHD narrowing. The sensitivity, specificity, and accuracy in detecting malignant lesions by MRCP were 89.6%, 98.9%, and 96.7% respectively (Figure 8).
Figure 8. Diagnostic performance of USG and MRCP in estimating cause of obstruction in malignant lesions.
MRCP: magnetic resonance cholangiopancreatography
Out of 23 patients with proximal CBD obstruction, USG was correctly able to predict the level of obstruction in 20 patients (sensitivity: 86.9%). Out of six patients with distal CBD obstruction, USG was correctly able to predict the level of obstruction in five patients (sensitivity: 83.3%). MRCP was correctly able to predict the level of obstruction in both proximal and distal CBD obstruction patients (sensitivity: 100%). The diagnostic accuracy in predicting the level of the malignant lesion for USG and MRCP were 86.20% and 100% respectively (Figure 9, Table 3).
Table 3. Level of obstruction in malignant lesions.
MRCP: magnetic resonance cholangiopancreatography; ERCP: endoscopic retrograde cholangiopancreatography
| Histopathology/ERCP/Surgery | |||
| Proximal common bile duct | Distal common bile duct | ||
| USG | Proximal common bile duct | 20 | 1 |
| Inconclusive | 2 | 0 | |
| Distal common bile duct | 1 | 5 | |
| Proximal common bile duct | Distal common bile duct | ||
| MRCP | Proximal common bile duct | 23 | 0 |
| Distal common bile duct | 0 | 6 | |
Figure 9. Diagnostic performance of USG and MRCP in estimating level of obstruction in malignant lesions.
MRCP: magnetic resonance cholangiopancreatography
Overall diagnostic performance
Out of 120 patients, USG was correctly able to predict the cause of obstruction in 40 patients. The sensitivity, specificity, and accuracy of detecting the nature of obstruction by USG were 33.3%, 84%, and 48.9% respectively. The overall diagnostic accuracy of USG in predicting the level of obstruction was 64.3%.
Out of 120 patients, MRCP was correctly able to predict the cause of obstruction in 113 patients. The sensitivity, specificity, and accuracy of detecting the nature of obstruction by MRCP were 94.1%, 91.9%, and 94.8% respectively. The overall diagnostic accuracy of MRCP in predicting the level of obstruction was 98.33% (Figures 10, 11).
Figure 10. Diagnostic performance of USG versus MRCP in predicting cause of obstruction in all 120 patients.
MRCP: magnetic resonance cholangiopancreatography
Figure 11. Diagnostic accuracy of USG versus MRCP in predicting level of obstruction.
MRCP: magnetic resonance cholangiopancreatography
Out of 120 patients, no cause of biliary obstruction could be found in 71 patients by USG, out of which the correct diagnosis was made in 67 patients through MRCP. The sensitivity, specificity, and diagnostic accuracy of MRCP in detecting the cause of obstruction in inconclusive USG for biliary obstruction were 94.37%, 93.88%, and 94.17%, respectively. The diagnostic performance of USG and MRCP for individual lesions are shown in Table 4.
Table 4. Diagnostic performance of USG and MRCP in biliary obstructive lesions.
MRCP: magnetic resonance cholangiopancreatography
| USG | MRCP | ||||||
| Sensitivity | Specificity | Accuracy | Sensitivity | Specificity | Accuracy | ||
| 1 | Ampullary Stenosis | 50 | - | 99 | 50 | - | 99 |
| 2 | Autoimmune Hepatitis | 0 | - | 99 | 100 | - | 100 |
| 3 | Benign Biliary Stricture | 17 | 100 | 92 | 100 | 99 | 99 |
| 4 | Biliary Sludge | 0 | 99 | 98 | 100 | 100 | 100 |
| 5 | Choledocholithiasis | 22 | 92 | 53 | 97 | 98 | 97 |
| 6 | Carcinoma Pancreas | 50 | 100 | 99 | 100 | 100 | 100 |
| 7 | Gallbladder Carcinoma | 76 | 99 | 95 | 100 | 99 | 99 |
| 8 | Cholangiocarcinoma | 87 | 99 | 98 | 87 | 100 | 99 |
| 9 | Hydatid Cyst | 100 | 100 | 100 | 100 | 100 | 100 |
| 10 | Mirrizi Syndrome | 20 | 100 | 97 | 100 | 98 | 98 |
| 11 | Main Pancreatic Duct Stricture | 100 | 100 | 100 | 100 | 100 | 100 |
| 12 | Periampullary Carcinoma | 0 | 100 | 98 | 50 | 100 | 98 |
| 13 | Periampullary Diverticulum | 0 | 100 | 98 | 100 | 100 | 100 |
| 14 | Choledochal Cyst | 100 | 99 | 99 | 100 | 100 | 100 |
Discussion
A slight female preponderance, with a female-to-male ratio of 1.1:1, was noted in patients with obstructive jaundice. Patients aged 51 to 60 years were the most numerous, followed by those aged 41 to 50 years. Our results show similarity with the study conducted by Upadhyaya et al. [5]. The majority of the patients (51.67%) had gallstones.
Diagnostic performance of USG in benign lesions
In the majority of patients, no cause of obstruction could be determined. The correct cause of obstruction was found in nearly one-fifth of the patients. The most common cause of benign biliary obstruction detected on USG was choledocholithiasis, which was similar to studies conducted by Upadhyaya et al. [5], Singh et al. [6], and Siva et al. [7]. The diagnostic performance of USG in choledocholithiasis is relatively poor (one in five cases), though an estimate about the level of obstruction could be made. Our study showed marked similarity with the study conducted by Alsaigh et al. [8], who found that there was 26.6% sensitivity and 100% specificity in detecting CBD stones.
Mirizzi syndrome was one of the most common cases that were misdiagnosed as choledocholithiasis. The diagnostic performance of the USG in benign biliary stricture, ampullary stenosis, periampullary diverticulum, and Mirizzi syndrome was fairly low. Our study related to benign CBD stricture is in accordance with a study conducted by Kaur et al. [9], who found the sensitivity and specificity of USG in diagnosing benign strictures to be 20% and 100%, respectively. The excellent specificity was due to the ability of USG to find true negatives in benign stenosis, thereby demonstrating the origin of the obstruction as a CBD stone or malignant stricture. The low sensitivity numbers were due to the inherent limitations of the approach, which, while displaying indirect indicators of stenosis, did not provide excellent viewing of the distal CBD and the periampullary region, where benign stenosis was frequently situated [9].
A high specificity of USG in detecting benign lesions was found in studies conducted by Prusty et al. (100%) [10], Verma et al. (88.4%) [11], and Ferrari et al. (94%) [12], which is similar to our study.
Only in about half of the patients with benign obstructive lesions could a diagnostically accurate estimate of the level of obstruction be made using USG in our study. Other studies have reported a variation of 27-95% in detecting level and 18-85% in detecting the cause of obstruction through USG [13-17].
Diagnostic performance of USG in malignant lesions
In the majority (more than two-thirds) of the patients, a correct diagnosis about the cause of obstruction could be made. The most common malignant cause of biliary obstruction detected on USG was gallbladder carcinoma, followed by cholangiocarcinoma (Figure 12). Diagnostic performance of USG in malignant lesions like gallbladder carcinoma and cholangiocarcinoma was fairly high, which is similar to that of Kaur et al. [9] and Singh et al. [6]. The overall sensitivity, specificity, and accuracy were 66.67%, 100%, and 96%, respectively, for cases with cholangiocarcinoma on USG in the study conducted by Singh et al. [6], which is similar to our study. Hann et al. [18] also found a sensitivity of 87% in detecting Hilar cholangiocarcinoma, which is in concordance with our study.
Figure 12. Distal cholangiocarcinoma. Coronal three-dimensional reconstructed image (A) and coronal T2 SSFSE image (B) show shouldering of distal common bile duct mass with dilated proximal biliary system.
SSFSE: single-shot fast spin echo
High sensitivity and specificity of USG in detecting neoplastic lesions were found in studies conducted by Verma et al. (88.4% and 85.3%) [11], Ferrari et al. (61.12% and 98.3%) [12], and Singh et al. (79.17% and 96.15%) [6].
Relatively poor diagnostic performance is noted in periampullary carcinoma and pancreatic carcinoma, likely due to obscuration of the field of view by overlying bowel gas. In patients with malignant obstructive lesions, a fairly high (nine-tenths) diagnostically accurate estimate of the site of obstruction could be made.
Diagnostic performance of MRCP in benign lesions
The majority of patients had a correct diagnosis of the cause of obstruction. The most common benign cause of biliary obstruction detected on MRCP was choledocholithiasis (Figure 13), followed by benign biliary stricture and Mirizzi syndrome. The present study is similar to that of Soto et al., who reported sensitivity and specificity of 94% and 100%, respectively, for detecting biliary calculi in MRCP [19]. Pavone et al. discovered that identifying CBD calculus on MRCP had an 88.9% sensitivity and a 100% specificity [20]. Our study also showed similarity with Guibaud et al., who found 100% accuracy in detecting CBD calculi on MRCP in cases with equivocal sonographic results [21]. Varghese et al. reported a sensitivity of 91%, specificity of 98%, and diagnostic accuracy of 97% on the MRCP [22]. Sugiyama et al. reported a sensitivity of 91%, specificity of 100%, and diagnostic accuracy of 97% on the MRCP [23].
Figure 13. Choledocholithiasis. (A) Coronal T2 SSFSE showing two round calculi in distal common bile duct along with cholelithiasis; (B) ERCP film showing two oval filing defects; (C) Calculi extraction during ERCP.
ERCP: endoscopic retrograde cholangiopancreatography: SSFSE: single-shot fast spin echo
Excellent diagnostic performance was noted in detecting all benign lesions, especially benign CBD strictures. According to a study by Bhatt et al., benign or malignant bile duct strictures and neoplastic lesions in the lower part of the CBD can be examined more effectively by MRCP [24], which is similar to our study. Our study is in concordance with a study conducted by Al-Obaidi et al., in which the sensitivity, specificity, and accuracy of MRCP for cases with benign biliary strictures were 100%, 98.5%, and 98.7%, respectively [25]. Our study is also in concordance with a study conducted by Singh et al., who found 100% accuracy for MRCP in diagnosing benign CBD strictures [6]. Munir et al. found the sensitivity and specificity of MRCP in detecting benign main bile duct strictures to be 83.3% and 97.6%, respectively [26]. Our research is consistent with that of Singh et al., who discovered that MRCP has 100% sensitivity and 98% diagnostic accuracy for benign diseases [6]. MRCP showed excellent diagnostic accuracy in predicting the site of the lesion. The most common level of obstruction was found to be distal CBD.
Diagnostic performance of MRCP in malignant lesions
In the majority of patients, a correct diagnosis of the cause of obstruction was made through MRCP. The most common malignant cause of biliary obstruction detected on MRCP was gallbladder carcinoma (Figure 14), followed by cholangiocarcinoma. Excellent diagnostic performance was noted in detecting all malignant lesions.
Figure 14. GB carcinoma. (A) Transabdominal USG shows irregularly thickened GB wall with cholelithiasis; (B) Transabdominal USG shows bilobar intrahepatic biliary dilatation; (C) Axial three-dimensional reconstructed image shows irregularly thickened GB wall with surrounding T2 hyperintensity and cholelithiasis.
GB: gallbladder
The sensitivity and specificity of MRCP for malignant pathologies found in studies conducted by Munir et al. (92% and 100%) [26], Prusty et al. (93.75% and 100%) [10], Verma et al. (86% and 92%) [11], and Ferrari et al. (90% and 94%) [12] are similar to our study.
The most common site of obstruction on MRCP was the proximal common duct. In our study, MRCP demonstrated excellent diagnostic performance in detecting the site of a lesion, which is consistent with the findings of Singh et al. [6].
Overall diagnostic performance of USG and MRCP
USG was correctly able to predict the cause of obstruction in one-third of all patients. The overall diagnostic accuracy of USG in predicting the site of obstruction was 64.3%. Other studies have reported a variation of 27-95% in detecting levels and 18-85% in detecting the cause of obstruction through USG [21-25]. Our study's overall specificity is comparable to that of Kaur et al. (100%) [9], Shadan et al. (83.3%) [27], and Kurian et al. (97.14%) [28].
MRCP was correctly able to predict the cause of obstruction in the majority (>90%) of patients. The overall diagnostic accuracy of MRCP in predicting the site of obstruction was 98.33%. Our study is in accordance with a study conducted by Farid et al., who found 97% accuracy in detecting the cause and 100% accuracy in detecting the site of obstructive jaundice [29]. Similar studies were conducted by Varghese et al. (sensitivity: 97%) [17], Romagnuolo et al. (sensitivity: 97%) [30], Shadan et al. (sensitivity: 97.7% and specificity: 100%) [27], and Kurian et al. (sensitivity: 97.14%) [28]. Upadhyaya et al. found MRCP was able to detect the level of obstruction in 95.45% of cases and the cause in 87.50% of cases [5]. Other studies have also reported very good results, with the ability to detect levels ranging from 85% to 100% [3,31-33].
On USG, no cause of biliary obstruction was found in nearly half of the patients in whom MRCP showed excellent diagnostic performance.
Conclusions
The diagnostic performance of USG in benign lesions is low as compared to MRCP. The diagnostic accuracy of USG in predicting the site of obstruction in benign cases is somewhat equivocal. As a result, USG cannot be used as the primary investigation in benign obstructive pathologies. The diagnostic performance of USG in acalculous pathologies is relatively higher as compared to choledocholithiasis. When compared to benign lesions, the diagnostic performance of USG in malignant lesions is slightly higher in detecting the cause and level of obstruction, though less than that of MRCP. In cases of clinical suspicion of a malignant cause of obstructive jaundice, MRCP could be considered the first choice of investigation for evaluation of the nature and level of obstruction. It could be used as the modality of choice and next step of investigation when clinical suspicion of obstructive jaundice is present, and no definite cause of biliary obstruction is seen on USG.
Overall, USG could be used as the initial screening modality of choice for predicting the level and nature of obstruction in patients with a clinical suspicion of obstructive jaundice. MRCP should be the radiological investigation of choice in patients with a clinical suspicion of obstructive jaundice and has the potential to become the new "Gold standard" investigation for diagnosis in patients with biliary obstruction owing to its excellent diagnostic performance and non-invasiveness.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Institutional Ethics Committee of Kalinga Institute of Medical Sciences (KIMS), Bhubaneswar, India issued approval ECR/321/Inst/OR/2013/RR-20. Investigating team will keep dignity, rights, safety, and well-being of participants, maintaining high ethics and will keep privacy of the individuals and confidentiality of the data and documents of Ethics Committee.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Body ultrasonography (second of two parts) Ferrucci JT Jr. N Engl J Med. 1979;300:590–602. doi: 10.1056/NEJM197903153001104. [DOI] [PubMed] [Google Scholar]
- 2.Ultrasound and scintigraphy in the differential diagnosis of obstructive jaundice. Taylor KJ, Carpenter DA, McCready VR. J Clin Ultrasound. 1974;2:105–116. doi: 10.1002/jcu.1870020205. [DOI] [PubMed] [Google Scholar]
- 3.Utility of magnetic resonance cholangiography in the evaluation of biliary obstruction. Magnuson TH, Bender JS, Duncan MD, Ahrendt SA, Harmon JW, Regan F. J Am Coll Surg. 1999;189:63–72. doi: 10.1016/s1072-7515(99)00082-4. [DOI] [PubMed] [Google Scholar]
- 4.Pitfalls in the interpretation of MR cholangiopancreatography. David V, Reinhold C, Hochman M, et al. https://www.ajronline.org/doi/pdf/10.2214/ajr.170.4.9530058. AJR Am J Roentgenol. 1998;170:1055–1059. doi: 10.2214/ajr.170.4.9530058. [DOI] [PubMed] [Google Scholar]
- 5.Comparative assessment of imaging modalities in biliary obstruction. Upadhyaya V, Upadhyaya DN, Ansari MA, Shukla VK. https://go.gale.com/ps/i.do?p=AONE&sw=w&issn=09702016&v=2.1&it=r&id=GALE%7CA164904435&sid=googleScholar&linkaccess=fulltext&userGroupName=anon%7E2a1c78e4 Ind J Radiol Imag. 2006;16 [Google Scholar]
- 6.Diagnostic accuracy of MRCP as compared to ultrasound/CT in patients with obstructive jaundice. Singh A, Mann HS, Thukral CL, Singh NR. J Clin Diagn Res. 2014;8:103–107. doi: 10.7860/JCDR/2014/8149.4120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ultrasound and magnetic resonance cholangio-pancreatography correlation in biliary disorders. Siva Prasad A, Sandeep J. MRIMS J Health Sci. 2015;3:142–146. [Google Scholar]
- 8.Diagnostic reliability of ultrasound compared to magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography in the detection of obstructive jaundice: a retrospective medical records review. Alsaigh S, Aldhubayb MA, Alobaid AS, et al. Cureus. 2020;12:0. doi: 10.7759/cureus.10987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Comprehensive evaluation of MRCP versus ultrasonography in biliary obstruction. Kaur A, Malaviya A, Deepika KN. Int J Med Res Rev. 2018;6:143–152. [Google Scholar]
- 10.Ultrasonography vs MRCP in evaluation of obstructive jaundice. Prusty SK, Bhagat S, Panda BB. J Med Sci Clin Res. 2019;7:1120–1128. [Google Scholar]
- 11.Obstructive jaundice- aetiological spectrum, clinical, biochemical and radiological evaluation at a tertiary care teaching hospital. Verma SR, Sahai SB, Gupta PK, Munshi A, Verma SC, Goyal P. https://ispub.com/IJTM/7/2/13053 Int J Trop Med. 2011;7 [Google Scholar]
- 12.US, MRCP, CCT and ERCP: a comparative study in 131 patients with suspected biliary obstruction. Ferrari FS, Fantozzi F, Tasciotti L, Vigni F, Scotto F, Frasci P. https://pubmed.ncbi.nlm.nih.gov/15735576/ Med Sci Monit. 2005;11:0–18. [PubMed] [Google Scholar]
- 13.Ultrasonography in obstructive jaundice. Malini S, Sabel J. Radiology. 1977;123:429–433. doi: 10.1148/123.2.429. [DOI] [PubMed] [Google Scholar]
- 14.A prospective comparison of the evaluation of biliary obstruction using computed tomography and ultrasonography. Baron RL, Stanley RJ, Lee JK, Koehler RE, Melson GL, Balfe DM, Weyman PJ. Radiology. 1982;145:91–98. doi: 10.1148/radiology.145.1.7122903. [DOI] [PubMed] [Google Scholar]
- 15.Role of ultrasonography in obstructive jaundice. Khandelwal KC, Merchant NH, Udani RJ, et al. Ind J Radiol Imag. 1991;1:17–20. [Google Scholar]
- 16.Diagnostic value of abdominal ultasonography and endoscopic retrograde cholangiopamcreatography in obstructive jaundice (Article in Hungarian) Zagoni T, Benko Z, Telegdy L, Antóny A, Keleti G, Péter Z. https://pubmed.ncbi.nlm.nih.gov/7637963/ Orv Hetil. 1995;136:1483–1486. [PubMed] [Google Scholar]
- 17.Relative merits of ultrasonography, computed tomography and cholangiography in patients of surgical obstructive jaundice. Kumar M, Prashad R, Kumar A, Sharma R, Acharya SK, Chattopadhyay TK. https://pubmed.ncbi.nlm.nih.gov/9951858/ Hepatogastroenterology. 1998;45:2027–2032. [PubMed] [Google Scholar]
- 18.Cholangiocarcinoma at the hepatic hilus: sonographic findings. Hann LE, Greatrex KV, Bach AM, Fong Y, Blumgart LH. AJR Am J Roentgenol. 1997;168:985–989. doi: 10.2214/ajr.168.4.9124155. [DOI] [PubMed] [Google Scholar]
- 19.Diagnosing bile duct stones: comparison of unenhanced helical CT, oral contrast-enhanced CT cholangiography, and MR cholangiography. Soto JA, Alvarez O, Múnera F, Velez SM, Valencia J, Ramírez N. AJR Am J Roentgenol. 2000;175:1127–1134. doi: 10.2214/ajr.175.4.1751127. [DOI] [PubMed] [Google Scholar]
- 20.MR cholangiography (MRC) in the evaluation of CBD stones before laparoscopic cholecystectomy. Pavone P, Laghi A, Lomanto D, et al. Surg Endosc. 1997;11:982–985. doi: 10.1007/s004649900507. [DOI] [PubMed] [Google Scholar]
- 21.Diagnosis of choledocholithiasis: value of MR cholangiography. Guibaud L, Bret PM, Reinhold C, Atri M, Barkun AN. AJR Am J Roentgenol. 1994;163:847–850. doi: 10.2214/ajr.163.4.8092021. [DOI] [PubMed] [Google Scholar]
- 22.Role of MR cholangiopancreatography in patients with failed or inadequate ERCP. Varghese JC, Farrell MA, Courtney G, Osborne H, Murray FE, Lee MJ. AJR Am J Roentgenol. 1999;173:1527–1533. doi: 10.2214/ajr.173.6.10584796. [DOI] [PubMed] [Google Scholar]
- 23.Magnetic resonance cholangiography using half-Fourier acquisition for diagnosing choledelocholithiasis. Sugiyama M, Atomi Y, Hachiya J, et al. Am J Gastroenterol. 1998;93:1886–1890. doi: 10.1111/j.1572-0241.1998.00543.x. [DOI] [PubMed] [Google Scholar]
- 24.Comparison of diagnostic accuracy between USG and MRCP in biliary and pancreatic pathology. Bhatt C, Shah PS, Prajapati HJ, Modi J. Indian J Radiol Imaging. 2005;15:177–181. [Google Scholar]
- 25.The role of ultrasound and magnetic resonance imaging in the diagnosis of obstructive jaundice. Al-Obaidi S, Al-Hilli MR, Fadhel AA. https://www.iasj.net/iasj/download/dac84cfdcbe759ea Iraqi Postgraduate Medical Journal. 2007;6:7–17. [Google Scholar]
- 26.The role of magnetic resonance cholangiopancreatography (MRCP) in obstructive jaundice. Munir K, Bari V, Yaqoob J, Khan DB, Usman MU. https://ecommons.aku.edu/pakistan_fhs_mc_radiol/264/ J Pak Med Assoc. 2004;54:128–132. [PubMed] [Google Scholar]
- 27.Role of MRCP in evaluation of suspected biliary and pancreatic diseases. Shadan A, Malik GM, Kamili MM, Umar K, Showkat H, Willayat A, Suhail M. http://jkpractitioner.com/pdfs/JkPract_Vol16_No1_4.pdf JK Pract. 2011;16:19–23. [Google Scholar]
- 28.A comparative evaluation of USG and MRCP findings in biliary and pancreatic pathologies. Kurian JM, Ganesh K, John PK, Hegde P, Murthy C, Kumar A. https://www.ijcmr.com/uploads/7/7/4/6/77464738/ijcmr_1223_feb_18.pdf Int J Contemp Med Res. 2017;4:212–215. [Google Scholar]
- 29.Role of magnetic resonance cholangiopancreatography (MRCP) in the evaluation of patients with obstructive jaundice. Farid S, Perumal RS. https://www.ijcmr.com/uploads/7/7/4/6/77464738/ijcmr_2490_v1.pdf Int J Contemp Med Res. 2019;6:0. [Google Scholar]
- 30.Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Romagnuolo J, Bardou M, Rahme E, Joseph L, Reinhold C, Barkun AN. Ann Intern Med. 2003;139:547–557. doi: 10.7326/0003-4819-139-7-200310070-00006. [DOI] [PubMed] [Google Scholar]
- 31.MR cholangiography in biliary obstruction using half-Fourier acquisition. Regan F, Smith D, Khazan R, Bohlman M, Schultze-Haakh H, Campion J, Magnuson TH. J Comput Assist Tomogr. 1996;20:627–632. doi: 10.1097/00004728-199607000-00024. [DOI] [PubMed] [Google Scholar]
- 32.Comparison of magnetic resonance and endoscopic retrograde cholangiopancreatography in malignant pancreaticobiliary obstruction. Georgopoulos SK, Schwartz LH, Jarnagin WR, et al. Arch Surg. 1999;134:1002–1007. doi: 10.1001/archsurg.134.9.1002. [DOI] [PubMed] [Google Scholar]
- 33.Magnetic resonance imaging in gastroenterology: time to say good-bye to all that endoscopy? Adamek HE, Breer H, Karschkes T, Albert J, Riemann JF. Endoscopy. 2000;32:406–410. doi: 10.1055/s-2000-639. [DOI] [PubMed] [Google Scholar]