Abstract
Background
The mechanisms by which parental early life stress can be transmitted to the next generation, in some cases in a sex-specific manner, are unclear. Maternal preconception stress may increase susceptibility to suboptimal health outcomes via in utero programming of the fetal hypothalamic–pituitary–adrenal (HPA) axis.
Methods
We recruited healthy pregnant women (N = 147), dichotomized into low (0 or 1) and high (2+) adverse childhood experience (ACE) groups based on the ACE Questionnaire, to test the hypothesis that maternal ACE history influences fetal adrenal development in a sex-specific manner. At a mean (standard deviation) of 21.5 (1.4) and 29.5 (1.4) weeks gestation, participants underwent three-dimensional ultrasounds to measure fetal adrenal volume, adjusting for fetal body weight (waFAV).
Results
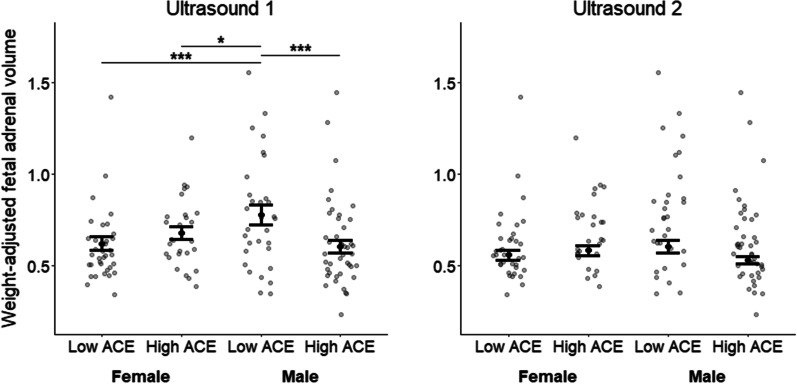
At ultrasound 1, waFAV was smaller in high versus low ACE males (b = − 0.17; z = − 3.75; p < .001), but females did not differ significantly by maternal ACE group (b = 0.09; z = 1.72; p = .086). Compared to low ACE males, waFAV was smaller for low (b = − 0.20; z = − 4.10; p < .001) and high ACE females (b = − 0.11; z = 2.16; p = .031); however, high ACE males did not differ from low (b = 0.03; z = .57; p = .570) or high ACE females (b = − 0.06; z = − 1.29; p = .196). At ultrasound 2, waFAV did not differ significantly between any maternal ACE/offspring sex subgroups (ps ≥ .055). Perceived stress did not differ between maternal ACE groups at baseline, ultrasound 1, or ultrasound 2 (ps ≥ .148).
Conclusions
We observed a significant impact of high maternal ACE history on waFAV, a proxy for fetal adrenal development, but only in males. Our observation that the waFAV in males of mothers with a high ACE history did not differ from the waFAV of females extends preclinical research demonstrating a dysmasculinizing effect of gestational stress on a range of offspring outcomes. Future studies investigating intergenerational transmission of stress should consider the influence of maternal preconception stress on offspring outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13293-023-00492-0.
Keywords: Maternal early life stress, Preconception stress, Fetal hypothalamic–pituitary–adrenal axis, Fetal adrenal gland, Dysmasculinization, Sex differences
Highlights
Three-dimensional ultrasound serves as a non-invasive way to measure fetal adrenal volume as a proxy for development of the fetal hypothalamic–pituitary–adrenal axis.
Weight-adjusted fetal adrenal volume (waFAV) differed between subgroups based on offspring sex and the mother’s history of adverse childhood experiences (ACEs).
In males of mothers with a high ACE history, waFAV was significantly smaller than in males of mothers with a low ACE history but indistinguishable from the waFAV of females from either maternal ACE group; however, males of mothers with a low ACE history had larger waFAV than females from either maternal ACE group.
These findings suggest male vulnerability to dysmasculinization of waFAV in response to maternal preconception stress in line with previous animal studies showing a dysmasculinizing effect of gestational stress on a range of offspring outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13293-023-00492-0.
Introduction
Mothers with a history of adverse childhood experiences (ACEs)—such as abuse, neglect, and family dysfunction—are more likely to have offspring with poorer mental health outcomes across the lifespan [1, 2]. Although rodent models suggest that maternal preconception stress impacts offspring through epigenetic changes to oocytes or in utero exposures [3–6], no studies have tested the effect of maternal ACEs on human fetal development despite its impact being theoretically plausible [7]. Presumably, dysregulated maternal stress physiology associated with maternal ACEs [8–15] could alter communication with the maternal–placental–fetal unit in a manner that leads to intergenerational transmission of a stress phenotype [16–20].
Although no human or animal studies have tested for an effect of maternal preconception stress (occurring before pregnancy) on fetal hypothalamic–pituitary–adrenal (HPA) axis, studies have examined this in the context of prenatal stress (occurring during pregnancy) or hormonal proxies of prenatal stress (glucocorticoid administration). In humans, ACEs impact maternal glucocorticoids in complex ways during pregnancy [17] and increase placental corticotropin releasing hormone (pCRH) [16]. In turn, higher maternal cortisol and placental pCRH levels during gestation have been linked to fetal growth restriction [21], earlier birth [22], lower birthweight [23], and enhanced offspring stress response [24, 25]. Although maternal cortisol is largely inactivated by placental 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD-2), maternal cortisol levels still explain a third of the variation in fetal cortisol levels [26]. In animal models, maternal HPA axis function altered by administration of either ACTH or dexamethasone provide direct evidence of the impact of high glucocorticoid exposure on fetal brain regions involved in stress responsivity [18, 19] and the fetal HPA axis, including the weight of the adrenal glands [18]. In an animal model of prenatal stress focusing exclusively on male offspring, male rats of stress exposed mothers exhibited decreased weight of the fetal adrenal glands relative to control males [20].
To our knowledge, the current study is the first to examine the volume of the human fetal adrenal gland as a proxy for the impact of maternal ACEs on fetal HPA axis development. We chose to focus on the fetal adrenal for three reasons. First, the adrenals are an essential stress-responsive organ of the HPA axis and the earliest and fastest growing organ in the fetal HPA axis [27]. Second, in animal models, its volume varies based on gestational stress exposure, at least in males [20], suggesting that high maternal ACEs and their potential to disrupt maternal HPA axis function during gestation could impact fetal adrenal development. Third, technological advances in three-dimensional (3-D) ultrasound have made it possible to measure fetal adrenal volume (FAV) noninvasively in humans [28, 29], with good intra- and interrater reliability [30].
We designed this study (1) to evaluate the relationship between maternal ACEs and fetal body weight-adjusted FAV (waFAV) and (2) to consider fetal sex as a potential moderator. In animal models, the impact of gestational stress exposure on fetal adrenal gland development has not been studied in females and, in humans, prenatal stress exposure impacts offspring outcomes in a sex-dependent manner (e.g., [23, 31–38, 40, 42]). Our sample included psychiatrically and medically healthy women, with the intention of isolating the effect of maternal ACEs on waFAV without the confounding impact of maternal mental health or medical problems during gestation. Despite the absence of robust data on the relationship between maternal childhood adversity and fetal outcomes, we predicted that the fetuses of pregnant women with higher exposure to childhood adversity versus those low or no exposure would exhibit differences in waFAV—particularly for males, given a review of clinical studies suggesting greater male vulnerability to gestational stress [41].
Methods and materials
Participant recruitment and screening
Women 18+ years old (at 8–17 weeks gestation) were recruited and screened while waiting for a perinatal care visit at three obstetrics and gynecology clinics affiliated with an academic health system. Participants were required to have a singleton pregnancy, be fluent in written and spoken English, and be willing to give written informed consent. Exclusions included reporting a serious medical or neurological illness, an active psychiatric illness, or a history of drug or alcohol abuse within the previous two years; feeling sad most days over the past two weeks; using steroid drugs or antihypertensives during pregnancy; having a history of fetal loss or preterm birth; or having a known abnormality with the current pregnancy or fetus. Eligible women were invited to undergo full screening for a longitudinal study that spanned pregnancy to 6 months postpartum. We recruited equal numbers of women reporting 0–1 and 2 + ACEs based on previous research demonstrating that 2+ ACEs increase risk for preterm birth [42], depression [43], cognitive complaints [44], and gut microbiota associated with inflammation [45] in women during reproductive transitions. All analyses in this paper focus on the sample of 147 participants who had waFAV data from at least one of the two ultrasounds (both ultrasounds: N = 128; only one ultrasound: N = 19; first ultrasound: N = 140; second ultrasound: N = 138), which occurred on average (SD) at 21.5 (1.4) weeks gestation and 29.5 (1.4) weeks gestation. The timepoints were chosen based on precedent for measuring fetal adrenal gland size [29, 46], physiological relevance as indicated by previous studies [47, 48], and feasibility constrained by when women typically present for their first perinatal visit as well as when FAV can be most accurately visualized by 3D ultrasound. The University of Pennsylvania’s institutional review board approved all research activities. Our data are publicly available at Open Science Framework (https://osf.io/bp7as/). For participant characteristics, see Table 1.
Table 1.
Participant characteristics overall and by maternal ACE group
| N with data | Overall (N = 147) | Low ACE (N = 71) | High ACE (N = 76) | P-value | |
|---|---|---|---|---|---|
| Maternal demographics | |||||
| Maternal age | 147 | 28.4 (5.3) | 28.7 (5.0) | 28.1 (5.5) | .480 |
| BMI | 143 | .012 | |||
| Normal/underweight | 72 (49%) | 43 (60.6%) | 29 (38.2%) | ||
| Overweight/obese | 71 (48.3%) | 27 (38%) | 44 (57.9%) | ||
| Missing | 4 (2.7%) | 1 (1.4%) | 3 (3.9%) | ||
| Race | 147 | .032 | |||
| African American/Black | 72 (49.0%) | 28 (39.4%) | 44 (57.9%) | ||
| Caucasian/other | 75 (51.0%) | 43 (60.6%) | 32 (42.1%) | ||
| Ethnicity | 147 | 1 | |||
| Non-Hispanic/unknown | 136 (92.5%) | 66 (93.0%) | 70 (92.1%) | ||
| Hispanic | 11 (7.5%) | 5 (7.0%) | 6 (7.9%) | ||
| Marital status | 147 | .008 | |||
| Married/domestic partner | 76 (51.7%) | 45 (63.4%) | 31 (40.8%) | ||
| Single/divorced | 71 (48.3%) | 26 (36.6%) | 45 (59.2%) | ||
| Education | 147 | .001 | |||
| High school education or less | 37 (25.2%) | 14 (19.7%) | 23 (30.3%) | ||
| Some education after high school | 40 (27.2%) | 12 (16.9%) | 28 (36.8%) | ||
| College degree or more | 70 (47.6%) | 45 (63.4%) | 25 (32.9%) | ||
| Income | 145 | < .001 | |||
| $25K or less | 52 (35.4%) | 20 (28.2%) | 32 (42.1%) | ||
| $25K to $75K | 38 (25.9%) | 11 (15.5%) | 27 (35.5%) | ||
| $75K or more | 55 (37.4%) | 38 (53.5%) | 17 (22.4%) | ||
| Parity | 120 | 0.7 (0.9) | 0.6 (0.7) | 0.8 (1.0) | .175 |
| Maternal psychological measures | |||||
| Baseline PSS score | 145 | 14.0 (6.3) | 13.7 (5.7) | 14.3 (6.8) | .562 |
| Ultrasound 1 PSS score | 144 | 10.8 (6.7) | 10.6 (6.0) | 11.6 (7.1) | .148 |
| Ultrasound 2 PSS score | 143 | 10.0 (6.8) | 9.7 (6.8) | 10.4 (6.9) | .504 |
| Baseline EPDS score | 146 | 4.4 (4.1) | 3.7 (3.3) | 5.2 (4.6) | .023 |
| Baseline STAI state score | 147 | 28.9 (9.4) | 30.2 (10.3) | 27.5 (8.2) | .080 |
| Baseline STAI trait score | 147 | 31.6 (8.4) | 33.2 (9.7) | 29.9 (6.4) | .016 |
| Offspring demographics | |||||
| Offspring sex | 147 | .070 | |||
| Male | 78 (53.1%) | 32 (45.1%) | 46 (60.5%) | ||
| Female | 69 (46.9%) | 39 (54.9%) | 30 (39.5%) | ||
| Gestational age (weeks) | |||||
| Ultrasound 1 | 142 | 21.5 (1.4) | 21.8 (1.4) | 21.3 (1.4) | .039 |
| Ultrasound 2 | 141 | 29.5 (1.4) | 29.8 (1.3) | 29.2 (1.4) | .018 |
| Birthweight (g) | 115 | 3270 (515) | 3220 (557) | 3317 (471) | .317 |
Maternal and offspring characteristics for women who had at least one ultrasound measuring fetal adrenal volume. Continuous variables are summarized with means and standard deviations, and differences between maternal ACE groups are tested using two-sample t-tests. Categorical variables are summarized with frequencies and percentages, and differences between maternal ACE groups are tested using Fisher’s exact tests. Tests with significant p-values are bolded. Values are summarized overall and stratified by maternal adverse childhood experiences (ACE) group: low = 0–1 ACEs; high = 2 + ACEs. PSS = Perceived Stress Scale; EPDS = Edinburgh Postnatal Depression Scale; STAI = State-Trait Anxiety Inventory
Study procedures
Self-report measures at initial and full screening (Table 2)
Table 2.
Descriptions of psychological measures
| Adverse Childhood Experiences Questionnaire (ACE-Q) | Participants completed the 10-item Adverse Childhood Experiences Questionnaire (ACE-Q) [49], which assessed exposures that occurred before age 18: abuse (emotional, physical, and sexual), neglect (emotional and physical), and household dysfunction (parental separation or divorce, household domestic violence, household substance abuse, parental mental illness, and member of household imprisoned). Each exposure counted as one point. ACE scores were computed by summing all exposures (0–10) |
| Perceived Stress Scale (PSS) | Participants completed the Perceived Stress Scale (PSS) [54], which assessed how unpredictable, uncontrollable, overloaded, and stressful they perceived their life to be. On 10 questions related to perceived stress, participants indicated how often they felt or thought a certain way over the last month (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, 4 = very often). PSS scores were calculated by summing all items |
| Edinburgh Postnatal Depression Scale (EPDS) | Participants completed the Edinburgh Postnatal Depression Scale (EPDS) [50], which assessed depressive symptomatology over the past week. Although the scale was originally developed to measure depressive symptoms in postpartum women, it has been validated for use in antepartum women as well [83, 84]. On 10 items measuring depressive symptoms, participants indicated how often they felt or thought a certain way (e.g., “I have been sad or miserable”) on a four-point scale, with higher scores indicating greater frequency of depressive symptoms. EPDS scores were calculated by summing all items |
| Spielberger State-Trait Anxiety Inventory (STAI) | Participants completed the Spielberger State‐Trait Anxiety Inventory (STAI) [53]. The trait anxiety subscale (STAI-T) asked participants to report how they generally felt on 20 items related to their general anxiety, e.g., “some unimportant thought runs through my mind and bothers me” (1 = almost never, 2 = sometimes, 3 = often, 4 = almost always). The state anxiety subscale (STAI-S) asked participants to report how they felt at the moment on 20 items related to their current anxiety, e.g., “I feel nervous” (1 = not at all, 2 = somewhat, 3 = moderately so, 4 = very much so). Trait and state anxiety scores were calculated by summing all items |
At initial screening, participants completed the Adverse Childhood Experiences Questionnaire (ACE-Q) [49], the Edinburgh Postnatal Depression Scale (EPDS) [50], and a questionnaire assessing demographics as well as medical/obstetrics history. At full screening, participants were administered the Structured Clinical Interview for DSM-IV-TR (SCID) [51] to rule out current psychiatric illness and the Hamilton Depression Rating Scale (HAM-D) [52] to assess subclinical depressive symptoms. At this visit, they also completed the EPDS and the Spielberger State‐Trait Anxiety Inventory (STAI) [53]. At the full screening and at each ultrasound visit, participants completed the Perceived Stress Scale (PSS) [54].
Fetal adrenal volume
For each ultrasound, either the right or left adrenal gland was selected to be measured based upon which adrenal had the clearest boundaries. Two raters (GE, EW) then measured the adrenal gland in replicate, repeating the measurement either two or three times. The replicates were averaged within rater and then between raters. The intraclass correlation coefficients were excellent for both ultrasounds within rater (ultrasound 1, rater 1: 0.899, 95% CI: [0.875, 0.920]; ultrasound 1, rater 2: 0.902, 95% CI: [0.878, 0.923]; ultrasound 2, rater 1: 0.859, 95% CI: [0.825, 0.888]; ultrasound 2, rater 2: 0.912 95% CI: [0.891, 0.931]) and between raters (ultrasound 1: 0.973, 95% CI: [0.964, 0.980]; ultrasound 2: 0.979, 95% CI: [0.971, 0.984]). Fetal body weight was estimated using a formula that included abdominal circumference, femur length, and head circumference [55]. We then divided FAV (cm3) by fetal body weight (kg) to yield weight-adjusted FAV (waFAV cm3/kg). See Additional file 1: Tables S1 and S2 for gestational age, adrenal volume, fetal body weight, and body weight-adjusted fetal adrenal volume data stratified by maternal ACE group and offspring sex for ultrasounds 1 and 2. See Additional file 1: Figures S1 and S2 in supplementary materials for histograms of fetal adrenal volumes overall and separately by sex. For details on 3-D ultrasound methods, see supplementary materials and Kim et al. [30]. During a postpartum visit, fetal sex was confirmed.
Statistical plan
Rationale for ACE as a dichotomous variable
Through visualization of the data, we determined that the relationship between maternal ACE and waFAV was not linear. To assess the validity of our a priori hypothesis that 2+ ACEs would indicate the risk group in this sample, we tested whether continuous ACEs versus dichotomized ACEs (at all possible cutoff points) produced the best fitting model. As such, we modeled the three-way interaction of maternal ACEs, offspring sex (male vs. female), and time (ultrasound 1 vs. 2) on waFAV in a linear mixed effects model with a random intercept for each participant. We found that dichotomizing ACE by a low (0–1 ACEs) and high (2+ ACEs) group led to the best fitting model based on having the lowest Akaike Information Criterion (AIC) (Additional file 1: Table S3).
Testing for covariates
We included the maternal and offspring demographic variables (listed in Table 1) as covariates in subsequent models if the covariate was associated with maternal ACE group and at least one of the ultrasound measures of waFAV with a p < 0.10. Although offspring sex is listed under offspring demographics in Table 1, we did not consider it for inclusion as a covariate given that we included it as a moderator.
Modeling the effect of maternal ACE group, offspring sex, and time on fetal adrenal volume
To determine whether a three-way interaction existed between maternal ACE group (low vs. high), offspring sex (male vs. female), and time (ultrasound 1 vs. 2) on waFAV, we modeled the effect of maternal ACE group, offspring sex, time, and all combinations of their interactions using a linear mixed effects model with a random intercept for each participant. This allowed us to model data even if participants were missing one of the two ultrasounds. Within this larger model, we tested for pairwise comparisons of the offspring sex/maternal ACE subgroups at ultrasounds 1 and 2 as these were our primary outcomes of interest.
Results
Sample characteristics
The sample consisted of 147 participants (age: M = 28.4, SD = 5.3), roughly balanced between the low and high maternal ACE groups (low ACE: N = 71; high ACE: N = 76), who differed on several participant characteristics, such as BMI, race, marital status, education, and income (see Table 1). Compared to the low ACE group, the high ACE group had lower trait anxiety (STAI-trait; t = 2.44; df = 130.97; p = 0.016) but higher depressive symptoms (EPDS; t = 2.30; df = 135.76; p = 0.023)—although their average was far below the cutoff of ≥ 14 that indicates possible clinical depression [56]. Perceived stress (PSS) did not differ between maternal ACE groups at baseline (t = − 0.58; df = 142.18; p = 0.562) or ultrasound 1 (t = − 1.46; df = 141.05; p = 0.148) or 2 (t = − 0.67; df = 140.55; p = 0.504).
Testing for covariates
The only two demographic variables that met criteria to be included as covariates were race (maternal ACE group: p = 0.032; waFAV [cm3/kg] at ultrasound 1: t = 2.28, df = 134, p = 0.024; waFAV [cm3/kg] at ultrasound 2: t = 0.14, df = 133, p = 0.89) and gestational age at the first ultrasound (maternal ACE group: df = 2.08, df = 138.97, p = 0.039; waFAV at ultrasound 1: t = − 2.95; df = 133; p = 0.004) but not at the second ultrasound (maternal ACE group: t = 2.39, df = 138.99, p = 0.018; waFAV at ultrasound 2: t = − 1.88; df = 131; p = 0.062). For all analyses involving waFAV as an outcome, race and time-varying gestational age were included as covariates.
Three-way interaction of maternal ACE group, offspring sex, and time on fetal adrenal volume
We first tested for a three-way interaction of maternal ACE group, offspring sex, and time on waFAV (cm3/kg), controlling for race and time-varying gestational age. Although the three-way interaction was not significant (= 2.48; df = 1; p = 0.115), our primary interest was the pairwise comparisons of the maternal ACE/offspring sex subgroups at ultrasounds 1 and 2 (Fig. 1 and Table 3), particularly given previous data suggesting that males would be more vulnerable to maternal early life stress [20, 41] and given that we did not necessarily predict changes over time in these effects. At ultrasound 1, high ACE males had a smaller waFAV (M = 0.625; SD = 0.188) than low ACE males (M = 0.776; SD = 0.299; b = − 0.17; 95% CI [− 0.26, − 0.08]; z = − 3.75; p < 0.001), but females did not differ significantly by maternal ACE group (b = 0.09; 95% CI [− 0.01, 0.19]; z = 1.72; p = 0.086)—although the effect was marginal with high ACE females exhibiting larger waFAV (M = 0.679; SD = 0.188) than low ACE females (M = 0.602; SD = 0.199), the opposite pattern from what was observed in males. Low (b = − 0.20; 95% CI [− 0.10, − 0.29]; z = − 4.10; p < 0.001) and high ACE females (b = − 0.11; 95% CI [− 0.21, − 0.01]; z = − 2.16; p = 0.031) had smaller waFAV than low ACE males. High ACE males did not differ from low (b = 0.03; 95% CI [− 0.06, 0.11]; z = 0.57; p = 0.570) or high ACE females (b = − 0.06; 95% CI [− 0.16, 0.03]; z = − 1.29; p = 0.196) in waFAV. At ultrasound 2, two marginal findings emerged: compared to low ACE males (M = 0.605; SD = 0.190), high ACE males (M = 0.560; SD = 0.174; b = − 0.08; 95% CI [− 0.17, 0.02]; z = − 1.58; p = 0.114) and low ACE females (M = 0.530; SD = 0.130; b = − 0.09; 95% CI [− 0.19, 0.00]; z = − 1.92; p = 0.055) had marginally smaller waFAV. Sex differences in ACE effects do not appear to be due to confounding as males and females with the low and high ACE groups did not differ on any of the maternal and offspring variables tested in supplemental Tables 4S (low ACE group) and 5S (high ACE group).
Fig. 1.
Fetal adrenal volume by maternal adverse childhood experiences (ACE) group and offspring sex. Although the three-way interaction of maternal ACE group (low vs. high), offspring sex (male vs. female), and time (ultrasound 1 vs. 2) on body weight-adjusted fetal adrenal volume (cm3/kg) was not significant (= 2.48; df = 1; p = .115), our primary interest was in the pairwise comparisons of the subgroups (characterized by maternal ACE and offspring sex) at ultrasounds 1 and 2. For ultrasound 1, significant differences emerged in weight − adjusted fetal adrenal volumes between low ACE boys and high ACE boys (b = − 0.17, z = − 3.75, p < .001), low ACE boys and low ACE girls (b = 0.20, z = 4.10, p < .001), and between low ACE boys and high ACE girls (b = − 0.11, z = − 2.16; p = .031). For the second ultrasound, no significant differences emerged for any pairwise comparisons although two findings were marginal: compared to low ACE males, high ACE males (b = − 0.08; 95% CI [− 0.17, 0.02]; z = − 1.58; p = .114) and low ACE females (b = − 0.09; 95% CI [− 0.19, 0.00]; z = − 1.92; p = .055) had marginally smaller weight-adjusted FAV. The overall model adjusts for race and gestational age at ultrasound. Bar plots display the mean and standard error of weight-adjusted fetal adrenal volume stratified by maternal ACE group and offspring sex. Maternal ACE group: low = 0–1 ACEs; high = 2 + ACEs. ***p < .001; **p < .01; *p < .05
Table 3.
Pairwise comparisons at the first and second ultrasounds
| Ultrasound | Group 1 | Group 2 | Estimate for group 1—group 2 (95% CI) | Z value | p value |
|---|---|---|---|---|---|
| Ultrasound 1 | High ACE females | Low ACE females | 0.09 (− 0.01, 0.19) | 1.72 | .086 |
| Ultrasound 1 | Low ACE males | Low ACE females | 0.20 (0.10, 0.29) | 4.10 | < .001 |
| Ultrasound 1 | High ACE males | Low ACE females | 0.03 (− 0.06, 0.11) | 0.57 | .570 |
| Ultrasound 1 | High ACE females | Low ACE males | − 0.11 (− 0.21, − 0.01) | − 2.16 | .031 |
| Ultrasound 1 | High ACE males | Low ACE males | − 0.17 (− 0.26, − 0.08) | − 3.75 | < .001 |
| Ultrasound 1 | High ACE males | High ACE females | − 0.06 (− 0.16, 0.03) | − 1.29 | .196 |
| Ultrasound 2 | High ACE females | Low ACE females | 0.06 (− 0.04, 0.15) | 1.12 | .262 |
| Ultrasound 2 | Low ACE males | Low ACE females | 0.09 (0.00, 0.19) | 1.92 | .055 |
| Ultrasound 2 | High ACE males | Low ACE females | 0.02 (− 0.07, 0.11) | 0.44 | .662 |
| Ultrasound 2 | High ACE females | Low ACE males | − 0.04 (− 0.14, 0.07) | − 0.73 | .467 |
| Ultrasound 2 | High ACE males | Low ACE males | − 0.08 (− 0.17, 0.02) | − 1.58 | .114 |
| Ultrasound 2 | High ACE males | High ACE females | − 0.04 (− 0.13, 0.06) | − 0.78 | .437 |
Maternal adverse childhood experiences (ACE) group and offspring sex pairwise comparisons on fetal body weight-adjusted fetal adrenal volume (waFAV). At the first ultrasound, males of mothers from the low ACE group had a larger waFAV than the other three subgroups. No significant pairwise comparisons emerged at the second ultrasound although males of mothers from the low ACE group had marginally larger waFAV than males of mothers from the high ACE group and females of mothers from the low ACE group. Tests with significant p-values are bolded
Discussion
In a study examining the association between maternal childhood adversity and FAV (as a proxy for fetal HPA axis development), we found that, in mid-gestation, maternal ACEs were associated with significant differences in waFAV in males. On average, males of mothers with a high ACE history had smaller waFAV than males of mothers with a low ACE history. Not surprisingly, males of mothers with a low ACE history had larger waFAV than both groups of females, in line with previous findings that male fetuses have larger fetal adrenal glands than female fetuses [30, 57]. In contrast, males of mothers with a high ACE history had waFAV that was indistinguishable from both female groups. We speculate that high maternal ACEs may have dysmasculinized fetal adrenal development in males. This is in line with preclinical studies in mice and rats showing that prenatal stress or gestational exposure to corticosteroids produce male offspring dysmasculinized across a range of outcomes, such as stress responsivity [58, 59], gene expression in the brain [60], anogenital distance [20], sexual motivation and behavior [61–64], spatial memory [65], as well as play, exploratory, and risk-taking behaviors [65, 66]. The underlying mechanism for these effects may be stress hormone disruption of testosterone production during important early developmental stages of sex differentiation [67].
Although maternal ACE group effects on waFAV were not significant in females, there was a trend towards the opposite pattern from what was observed in males. At both the first and the second ultrasounds, females of high ACE mothers exhibited larger waFAVs than females of low ACE mothers. However, high standard deviations prohibited these mean differences from reaching statistical significance (see Additional file 1: Tables S1, S2 for means and standard deviations).
Because no prior studies have examined the relationship between preconception stress (before pregnancy) and adrenal gland development, we rely on studies assessing prenatal stress (during pregnancy) to speculate on the underlying mechanisms driving these effects, with the caveat that prenatal stress may impact the offspring differently than preconception stress. One possible mechanism is that males may be more susceptible to maternal ACE effects. Mothers carrying male fetuses already exhibit higher cortisol [68], at least during mid-gestation [69]. Furthermore, prenatal stress decreases expression of placental 11β-HSD-2 in preclinical and clinical studies [20, 70, 71], particularly when stress is chronic rather than acute [72], and some preliminary evidence in humans suggests that this effect may differ by sex [73]. Thus, maternal adversity may affect placental barriers, which may in turn impact the extent to which male fetuses may be exposed to glucocorticoids.
A second possible mechanism that could underlie our effects is the placental enzyme O-linked N-acetylglucosamine transferase (OGT), an X-linked gene expressed at lower levels in male placentas in mice and humans whose expression is further reduced by maternal prenatal stress in mice [74]. Lower OGT has been associated with reduced testosterone in male placental tissue [75], postulating a putative mechanism by which prenatal stress could result in a dysmasculinized phenotype. Although no studies have examined the impact of early life stress on OGT or OGT’s potential effects on FAV, it is possible that maternal early life stress affects OGT expression similarly to prenatal stress and could underlie our observation that high maternal ACE scores are associated with a dysmasculinized phenotype in FAV. However, this hypothesis will remain speculative until further research is conducted. Overall, fetal characteristics, such as sex, in addition to maternal factors, such as maternal ACE history, may influence maternal placental function in ways that affect fetal glucocorticoid and androgen exposure that could impact the fetal HPA axis development.
Currently, there is little data to guide the timing of when to study preconception stress effects on human fetal development. However, our study showed that findings at the second ultrasound were less robust than at the first ultrasound—although the pattern of results was the same and trended towards significance. The signal may be stronger and/or easier to detect earlier in development. One possible explanation for our significant effects at the first but not the second ultrasound is that fetal organs may become more difficult to accurately visualize using 3-D ultrasound later in gestation as the fetal bones become more ossified. This is because ossified fetal bones create more acoustic shadowing, potentially limiting the borders of fetal organs. Another possible explanation is that maternal cortisol exposure may differ across gestation depending on offspring sex. One study found that maternal cortisol was higher in mid-gestation with male fetuses and higher in late gestation with female fetuses [69]. This crossover effect, if it occurred in our sample, could have diminished the magnitude of our effects later in gestation.
Limitations
Although our study had unique strengths in terms of measuring a novel biomarker of the fetal stress system, in retrospect, additional measures could have been useful to collect (e.g., hair cortisol in the mother during pregnancy, hair cortisol in the offspring at birth, placenta levels of 11β-HSD-2 and OGT). Although we recently published data from this cohort showing that women’s acoustic startle response did not differ by ACE during pregnancy but did in the postpartum [76], we did not measure any maternal factors that allowed us to understand the physiological impact of ACEs on the mother during pregnancy. Thus, a next important step in this research is to study the mechanisms by which maternal ACEs become biologically embedded to influence offspring development.
Given our focus on pregnant women and their offspring, ACEs could not be measured prospectively, nor did we rely on external records to confirm the occurrence of ACEs (e.g., court records). Although retrospective reporting is more susceptible to misclassification, a previous study assessing the test–retest reliability of an 8-item version of the ACE-Q [77] found its reliability to be “good” as defined by Fleiss [78] and “moderate to substantial” as defined by Landis and Koch [79].
Perspectives and significance
Research has long established that parental life experiences impact the offspring, with studies indicating effects across the lifespan, from the time of conception to adulthood [31, 59, 80–82]. However, all previous human studies investigating outcomes in the fetus have focused on the effects of prenatal stress rather than preconception stress. To our knowledge, this study is the only one that has examined an association between a biological marker of risk in the fetus and maternal childhood adversity rather than adversity during pregnancy. Even in animal models, only one study has tested for a relationship between maternal stress and fetal adrenal gland size, but that study only examined effects of prenatal stress in male fetuses. Our finding of sex-specific effects of maternal ACEs on waFAV emphasize the importance of considering maternal early life stress as well as offspring sex in biomedical research. Our significant findings would have been obscured if we had excluded either as a factor in our statistical analyses.
Conclusions
In a novel study testing for associations between maternal ACEs and waFAV as a marker of fetal HPA axis development, we demonstrate that maternal exposure to ACEs impacts the development of the fetal adrenal gland in a sex-specific manner. The sex differences that we observed are consistent with the limited preclinical data investigating this [20]. In males of mothers with a high ACE history, waFAV was significantly smaller than in males of mothers with a low ACE history but indistinguishable from the waFAV of females regardless of their mother’s ACE history. Importantly, our sample consisted of psychiatrically and medically healthy women, allowing us to isolate the impact of maternal ACEs on waFAV without the confounding impact of maternal mental and physical health problems during gestation. The observed effects were presumably not due to maternal ACE effects on prenatal stress as perceived stress did not differ between maternal ACE groups at baseline or either of the two ultrasounds. Overall, our findings suggest male vulnerability to dysmasculinization of waFAV in response to maternal preconception stress.
Supplementary Information
Additional file 1. Supplementary Figures and Tables.
Acknowledgements
Thanks to Claudia Iannelli, Anna Belyavskaya, Stephanie Criniti, Jessica Snell, Lisa Lamprou, and Dina Appleby for their support in collecting data. We appreciate Aviva Olvslavsky for her feedback on the manuscript.
Author contributions
CNE, MDS, and DRK contributed to the conception and design of the study. DRK, EYW, SLK, LH, RLJ, and GE contributed to the acquisition of the data. RLJ, MDS, EYW, and LH contributed to analysis of the data. CNE, RLJ, MDS, KAD, TLB, and LH interpreted the data. KAD, TLB, RLJ, and MDS drafted the manuscript. CNE substantively revised it. All authors read and approved the final manuscript.
Funding
This research was funded through NIH Grants K23MH102360 and P50MH099910.
Availability of data and materials
Our data are publicly available at Open Science Framework (https://osf.io/bp7as/).
Declarations
Ethics approval and consent to participate
The University of Pennsylvania’s institutional review board approved all research activities. Participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
CNE consults for Sage Therapeutics and Asarina Pharma and is an investigator for a multisite clinical trial conducted by Sage Therapeutics. She is also on the scientific advisory board of Babyscripts and receives research support from HealthRhythms. KAD, MDS, RLJ, DRK, EYW, GE, LH, SLK, and TLB have no disclosures to report.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Korrina A. Duffy, Email: korrina.duffy@cuanschutz.edu
Mary D. Sammel, Email: mary.sammel@cuanschutz.edu
Rachel L. Johnson, Email: rachel.johnson@cuanschutz.edu
Deborah R. Kim, Email: drkim@pennmedicine.upenn.edu
Eileen Y. Wang, Email: Eileen.Wang@pennmedicine.upenn.edu
Grace Ewing, Email: ewing.grace0@gmail.com.
Liisa Hantsoo, Email: liisahantsoo@gmail.com.
Sara L. Kornfield, Email: sarakorn@pennmedicine.upenn.edu
Tracy L. Bale, Email: tracy.bale@cuanschutz.edu
C. Neill Epperson, Email: neill.epperson@cuanschutz.edu.
References
- 1.Schickedanz A, Halfon N, Sastry N, Chung PJ. Parents’ adverse childhood experiences and their children’s behavioral health problems. Pediatrics. 2018;142:e20180023. doi: 10.1542/peds.2018-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doi S, Fujiwara T, Isumi A. Association between maternal adverse childhood experiences and mental health problems in offspring: An intergenerational study. Dev Psychopathol. 2020;89:1–18. doi: 10.1017/S0954579420000334. [DOI] [PubMed] [Google Scholar]
- 3.Zaidan H, Leshem M, Gaisler-Salomon I. Prereproductive stress to female rats alters corticotropin releasing factor type 1 expression in ova and behavior and brain corticotropin releasing factor type 1 expression in offspring. Biol Psychiatry. 2013;74:680–687. doi: 10.1016/j.biopsych.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 4.Huang Y, Shi X, Xu H, Yang H, Chen T, Chen S, Chen X. Chronic unpredictable stress before pregnancy reduce the expression of brain-derived neurotrophic factor and N-methyl-D-aspartate receptor in hippocampus of offspring rats associated with impairment of memory. Neurochem Res. 2010;35:1038–1049. doi: 10.1007/s11064-010-0152-0. [DOI] [PubMed] [Google Scholar]
- 5.Zaidan H, Gaisler-Salomon I. Prereproductive stress in adolescent female rats affects behavior and corticosterone levels in second-generation offspring. Psychoneuroendocrinology. 2015;58:120–129. doi: 10.1016/j.psyneuen.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Dias BG, Ressler KJ. Parental olfactory experience influences behavior and neural structure in subsequent generations. Nat Neurosci. 2014;17:89–96. doi: 10.1038/nn.3594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buss C, Entringer S, Moog NK, Toepfer P, Fair DA, Simhan HN, et al. Intergenerational transmission of maternal childhood maltreatment exposure: Implications for fetal brain development. J Am Acad Child Adolesc Psychiatry. 2017;56:373–382. doi: 10.1016/j.jaac.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartwell KJ, Moran-Santa Maria MM, Twal WO, Shaftman S, DeSantis SM, McRae-Clark AL, Brady KT. Association of elevated cytokines with childhood adversity in a sample of healthy adults. J Psychiatr Res. 2013;47:604–610. doi: 10.1016/j.jpsychires.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heim C, Newport DJ, Wagner D, Wilcox MM, Miller AH, Nemeroff CB. The role of early adverse experience and adulthood stress in the prediction of neuroendocrine stress reactivity in women: a multiple regression analysis. Depress Anxiety. 2002;15:117–125. doi: 10.1002/da.10015. [DOI] [PubMed] [Google Scholar]
- 10.Nemeroff CB. Neurobiological consequences of childhood trauma. J Clin Psychiatry. 2004;65:18–28. [PubMed] [Google Scholar]
- 11.Carpenter LL, Tyrka AR, McDougle CJ, Malison RT, Owens MJ, Nemeroff CB, Price LH. Cerebrospinal fluid corticotropin-releasing factor and perceived early-life stress in depressed patients and healthy control subjects. Neuropsychopharmacology. 2004;29:777–784. doi: 10.1038/sj.npp.1300375. [DOI] [PubMed] [Google Scholar]
- 12.Carpenter LL, Carvalho JP, Tyrka AR, Wier LM, Mello AF, Mello MF, et al. Decreased adrenocorticotropic hormone and cortisol responses to stress in healthy adults reporting significant childhood maltreatment. Biol Psychiatry. 2007;62:1080–1087. doi: 10.1016/j.biopsych.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA. 2000;284:592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- 14.Morrison KE, Epperson CN, Sammel MD, Ewing G, Podcasy JS, Hantsoo L, et al. Preadolescent adversity programs a disrupted maternal stress reactivity in humans and mice. Biol Psychiatry. 2017;81:693–701. doi: 10.1016/j.biopsych.2016.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stein MB, Yehuda R, Koverola C, Hanna C. Enhanced dexamethasone suppression of plasma cortisol in adult women traumatized by childhood sexual abuse. Biol Psychiatry. 1997;42:680–686. doi: 10.1016/S0006-3223(96)00489-1. [DOI] [PubMed] [Google Scholar]
- 16.Moog NK, Buss C, Entringer S, Shahbaba B, Gillen DL, Hobel CJ, Wadhwa PD. Maternal exposure to childhood trauma is associated during pregnancy with placental-fetal stress physiology. Biol Psychiatry. 2016;79:831–839. doi: 10.1016/j.biopsych.2015.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Epstein CM, Houfek JF, Rice MJ, Weiss SJ. Integrative review of early life adversity and cortisol regulation in pregnancy. JOGNN - J Obstet Gynecol Neonatal Nurs. 2021;50:242–255. doi: 10.1016/j.jogn.2020.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fameli M, Kitraki E, Stylianopoulou F. Effects of hyperactivity of the maternal hypothalamic-pituitary-adrenal (HPA) axis during pregnancy on the development of the HPA axis and brain monoamines of the offspring. Int J Dev Neurosci. 1994;12:651–659. doi: 10.1016/0736-5748(94)90017-5. [DOI] [PubMed] [Google Scholar]
- 19.Liu L, Li A, Matthews SG. Maternal glucocorticoid treatment programs HPA regulation in adult offspring: Sex-specific effects. Am J Physiol - Endocrinol Metab. 2001;280:729–739. doi: 10.1152/ajpendo.2001.280.5.E729. [DOI] [PubMed] [Google Scholar]
- 20.Mairesse J, Lesage J, Breton C, Bréant B, Hahn T, Darnaudéry M, et al. Maternal stress alters endocrine function of the feto-placental unit in rats. Am J Physiol - Endocrinol Metab. 2007;292:1526–1533. doi: 10.1152/ajpendo.00574.2006. [DOI] [PubMed] [Google Scholar]
- 21.Farzad Mohajeri Z, Aalipour S, Sheikh M, Shafaat M, Hantoushzadeh S, Borna S, Khazardoost S. Ultrasound measurement of fetal adrenal gland in fetuses with intrauterine growth restriction, an early predictive method for adverse outcomes. J Matern Neonatal Med. 2019;32:1485–1491. doi: 10.1080/14767058.2017.1410125. [DOI] [PubMed] [Google Scholar]
- 22.Giurgescu C. Are maternal cortisol levels related to preterm birth? J Obstet Gynecol Neonatal Nurs. 2009;38:377–390. doi: 10.1111/j.1552-6909.2009.01034.x. [DOI] [PubMed] [Google Scholar]
- 23.Cherak SJ, Giesbrecht GF, Metcalfe A, Ronksley PE, Malebranche ME. The effect of gestational period on the association between maternal prenatal salivary cortisol and birth weight: a systematic review and meta-analysis. Psychoneuroendocrinology. 2018;94:49–62. doi: 10.1016/j.psyneuen.2018.04.023. [DOI] [PubMed] [Google Scholar]
- 24.Davis EP, Glynn LM, Waffarn F, Sandman CA. Prenatal maternal stress programs infant stress regulation. J Child Psychol Psychiatry. 2010;52:119–129. doi: 10.1111/j.1469-7610.2010.02314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gutteling BM, de Weerth C, Buitelaar JK. Prenatal stress and children’s cortisol reaction to the first day of school. Psychoneuroendocrinology. 2005;30:541–549. doi: 10.1016/j.psyneuen.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Mastorakos G, Ilias I. Maternal and fetal hypothalamic-pituitary-adrenal axes during pregnancy and postpartum. Ann N Y Acad Sci. 2003;997:136–149. doi: 10.1196/annals.1290.016. [DOI] [PubMed] [Google Scholar]
- 27.Chen Y, He Z, Chen G, Liu M, Wang H. Prenatal glucocorticoids exposure and fetal adrenal developmental programming. Toxicology. 2019;428:152308. doi: 10.1016/j.tox.2019.152308. [DOI] [PubMed] [Google Scholar]
- 28.Chang C-H, Yu C-H, Chang F-M, Ko H-C, Chen H-Y. Assessment of fetal adrenal gland volume using three-dimensional ultrasound. Ultrasound Med Biol. 2002;28:1383–1387. doi: 10.1016/S0301-5629(02)00650-6. [DOI] [PubMed] [Google Scholar]
- 29.Hoffman MK, Turan OM, Parker CB, Wapner RJ, Wing DA, Haas DM, et al. Ultrasound measurement of the fetal adrenal gland as a predictor of spontaneous preterm birth. Obstet Gynecol. 2016;127:726–734. doi: 10.1097/AOG.0000000000001342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim D, Epperson CN, Ewing G, Appleby D, Sammel MD, Wang E. Methodology for using 3-dimensional sonography to measure fetal adrenal gland volumes in pregnant women with and without early life stress. J Ultrasound Med. 2016;35:2029–2037. doi: 10.7863/ultra.15.10046. [DOI] [PubMed] [Google Scholar]
- 31.Neuenschwander R, Hookenson K, Brain U, Grunau RE, Devlin AM, Weinberg J, et al. Children’s stress regulation mediates the association between prenatal maternal mood and child executive functions for boys, but not girls. Dev Psychopathol. 2018;30:953–969. doi: 10.1017/S095457941800041X. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein JM, Cohen JE, Mareckova K, Holsen L, Whitfield-Gabrieli S, Gilman SE, et al. Impact of prenatal maternal cytokine exposure on sex differences in brain circuitry regulating stress in offspring 45 years later. Proc Natl Acad Sci U S A. 2021;118:1–8. doi: 10.1073/pnas.2014464118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campbell RK, Devick KL, Coull BA, Cowell W, Askowitz T, Goldson B, et al. Prenatal cortisol modifies the association between maternal trauma history and child cognitive development in a sex-specific manner in an urban pregnancy cohort. Stress. 2019;22:228–235. doi: 10.1080/10253890.2018.1553950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Doyle C, Werner E, Feng T, Lee S, Altemus M, Isler JR, Monk C. Pregnancy distress gets under fetal skin: Maternal ambulatory assessment & sex differences in prenatal development. Dev Psychobiol. 2015;57:607–625. doi: 10.1002/dev.21317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Molenaar NM, Tiemeier H, van Rossum EFC, Hillegers MHJ, Bockting CLH, Hoogendijk WJG, et al. Prenatal maternal psychopathology and stress and offspring HPA axis function at 6 years. Psychoneuroendocrinology. 2019;99:120–127. doi: 10.1016/j.psyneuen.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Ping EY, Laplante DP, Elgbeili G, Hillerer KM, Brunet A, O’Hara MW, King S. Prenatal maternal stress predicts stress reactivity at 2.5 years of age: The Iowa Flood Study. Psychoneuroendocrinology. 2015;56:62–78. doi: 10.1016/j.psyneuen.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 37.Brown AS, Susser ES, Lin SP, Neugebauer R, Gorman JM. Increased risk of affective disorders in males after second trimester prenatal exposure to the Dutch hunger winter of 1944–45. Br J Psychiatry. 1995;166:601–606. doi: 10.1192/bjp.166.5.601. [DOI] [PubMed] [Google Scholar]
- 38.Franzek EJ, Sprangers N, Janssens ACJW, Van Duijn CM, Van De Wetering BJM. Prenatal exposure to the 1944–45 Dutch “hunger winter” and addiction later in life. Addiction. 2008;103:433–438. doi: 10.1111/j.1360-0443.2007.02084.x. [DOI] [PubMed] [Google Scholar]
- 39.Robinson M, Carter KW, Pennell CE, Jacoby P, Moore HC, Zubrick SR, Burgner D. Maternal prenatal stress exposure and sex-specific risk of severe infection in offspring. PLoS ONE. 2021;16:1–13. doi: 10.1371/journal.pone.0245747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maxwell SD, Fineberg AM, Drabick DA, Muphy SK, Ellman LM. Maternal prenatal stress and other developmental risk factors for adolescent depression: Spotlight on sex differences. J Abnorm Child Psychol. 2018;46:381–397. doi: 10.1007/s10802-017-0299-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.DiPietro J, Voegtline K. The gestational foundation of sex differences in development and vulnerability. Neuroscience. 2017;342:4–20. doi: 10.1016/j.neuroscience.2015.07.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Christiaens I, Hegadoren K, Olson DM. Adverse childhood experiences are associated with spontaneous preterm birth: a case-control study. BMC Med. 2015;13:1–9. doi: 10.1186/s12916-015-0353-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Epperson CN, Sammel M, Bale T, Kim D, Conlin S, Scalice S, et al. Adverse childhood experiences and risk for first-episode major depression during the menopause transition. J Clin Psychiatry. 2017;78:e298–e307. doi: 10.4088/JCP.16m10662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shanmugan S, Sammel MD, Loughead J, Ruparel K, Gur RC, Brown TE, et al. Executive function after risk-reducing salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers: Does current mood and early life adversity matter? Menopause J North Am Menopause Soc. 2020;27:746–755. doi: 10.1097/GME.0000000000001535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hantsoo L, Jašarević E, Criniti S, McGeehan B, Tanes C, Sammel MD, et al. Childhood adversity impact on gut microbiota and inflammatory response to stress during pregnancy. Brain Behav Immun. 2019;75:240–250. doi: 10.1016/j.bbi.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Blue NR, Hoffman M, Allshouse AA, Grobman WA, Simhan HN, Turan OM, et al. Antenatal fetal adrenal measurements at 22 to 30 weeks’ gestation, fetal growth restriction, and perinatal morbidity. Am J Perinatol. 2021;38:676–682. doi: 10.1055/s-0039-3400308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wadhwa PD, Porto M, Garite TJ, Chicz-DeMet A, Sandman CA. Maternal CRH levels in early third trimester predicts length of gestation in human pregnancy. Am J Obstet Gynecol. 1998;179:1079–1985. doi: 10.1016/S0002-9378(98)70219-4. [DOI] [PubMed] [Google Scholar]
- 48.Hobel CJ, Dunkel-Schetter C, Roesch SC, Castro LC, Arora CP. Maternal plasma corticotropin-releasing hormone associated with stress at 20 weeks’ gestation in pregnancies ending in preterm delivery. Am J Obstet Gynecol. 1999;180:S257–S263. doi: 10.1016/S0002-9378(99)70712-X. [DOI] [PubMed] [Google Scholar]
- 49.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. Am J Prev Med. 1998;14:245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 50.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 51.First MB, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR axis I Disorders, Research Version, Non-patien. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 52.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–296. doi: 10.1111/j.2044-8260.1967.tb00530.x. [DOI] [PubMed] [Google Scholar]
- 53.Spielberger C. Manual for the State-Trait Anxiety Inventory (STAI) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 54.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 55.Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK. Estimation of fetal weight with the use of head, body, and femur measurements – A prospective study. Am J Obstet Gynecol. 1985;151:333–337. doi: 10.1016/0002-9378(85)90298-4. [DOI] [PubMed] [Google Scholar]
- 56.Lyubenova A, Neupane D, Levis B, Wu Y, Sun Y, He C, et al. Depression prevalence based on the Edinburgh Postnatal Depression Scale compared to Structured Clinical Interview for DSM Disorders classification: Systematic review and individual participant data meta-analysis. Int J Methods Psychiatr Res. 2021;30:1–13. doi: 10.1002/mpr.1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Karsli T, Strickland D, Livingston J, Wu Q, Mhanna MJ, Shekhawat PS. Assessment of neonatal adrenal size using high resolution 2D ultrasound and its correlation with birth demographics and clinical outcomes. J Matern Neonatal Med. 2019;32:377–383. doi: 10.1080/14767058.2017.1378340. [DOI] [PubMed] [Google Scholar]
- 58.Mueller BR, Bale TL. Early prenatal stress impact on coping strategies and learning performance is sex dependent. Physiol Behav. 2007;91:55–65. doi: 10.1016/j.physbeh.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 59.Mueller BR, Bale TL. Sex-specific programming of offspring emotionality after stress early in pregnancy. J Neurosci. 2008;28:9055–9065. doi: 10.1523/JNEUROSCI.1424-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Morgan CP, Bale TL. Early prenatal stress epigenetically programs dysmasculinization in second-generation offspring via the paternal lineage. J Neurosci. 2011;31:11748–11755. doi: 10.1523/JNEUROSCI.1887-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gerardin DCC, Pereira OCM, Kempinas WG, Florio JC, Moreira EG, Bernardi MM. Sexual behavior, neuroendocrine, and neurochemical aspects in male rats exposed prenatally to stress. Physiol Behav. 2005;84:97–104. doi: 10.1016/j.physbeh.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 62.Stylianopoulou F. Effect of maternal adrenocorticotropin injections on the differentiation of sexual behavior of the offspring. Horm Behav. 1983;17:324–331. doi: 10.1016/0018-506X(83)90032-6. [DOI] [PubMed] [Google Scholar]
- 63.Wang C-T, Shui H-A, Huang R-L, Tai M-Y, Peng M-T, Tsai Y-F. Sexual motivation is demasculinized, but not feminized, in prenatally stressed male rats. Neuroscience. 2006;138:357–364. doi: 10.1016/j.neuroscience.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 64.Ward IL. Prenatal stress feminizes and demasculinizes the behavior of males. Science. 1972;175:82–84. doi: 10.1126/science.175.4017.82. [DOI] [PubMed] [Google Scholar]
- 65.Verhaeghe R, Gao V, Morley-Fletcher S, Bouwalerh H, Van Camp G, Cisani F, et al. Maternal stress programs a demasculinization of glutamatergic transmission in stress-related brain regions of aged rats. GeroScience. 2021;6:1–23. doi: 10.1007/s11357-021-00375-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ward IL, Stehm KE. Prenatal stress feminizes juvenile play patterns in male rats. Physiol Behav. 1991;50:601–605. doi: 10.1016/0031-9384(91)90552-Y. [DOI] [PubMed] [Google Scholar]
- 67.Bale TL. The placenta and neurodevelopment: sex differences in prenatal vulnerability. Dialogues Clin Neurosci. 2016;17:459–464. doi: 10.31887/DCNS.2016.18.4/tbale. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Enlow MB, Sideridis G, Bollati V, Hoxha M, Hacker MR, Wright RJ. Maternal cortisol output in pregnancy and newborn telomere length: Evidence for sex-specific effects. Psychoneuroendocrinology. 2019;102:225–235. doi: 10.1016/j.psyneuen.2018.12.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.DiPietro JA, Costigan KA, Kivlighan KT, Chen P, Laudenslager ML. Maternal salivary cortisol differs by fetal sex during the second half of pregnancy. Psychoneuroendocrinology. 2011;36:588–591. doi: 10.1016/j.psyneuen.2010.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.O’Donnell KJ, Bugge Jensen A, Freeman L, Khalife N, O’Connor TG, Glover V. Maternal prenatal anxiety and downregulation of placental 11β-HSD2. Psychoneuroendocrinology. 2012;37:818–826. doi: 10.1016/j.psyneuen.2011.09.014. [DOI] [PubMed] [Google Scholar]
- 71.Peña CJ, Monk C, Champagne FA. Epigenetic effects of prenatal stress on 11β-hydroxysteroid dehydrogenase-2 in the placenta and fetal brain. PLoS ONE. 2012;7:1–9. doi: 10.1371/journal.pone.0039791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Welberg LAM, Thrivikraman KV, Plotsky PM. Chronic maternal stress inhibits the capacity to up-regulate placental 11β-hydroxysteroid dehydrogenase type 2 activity. J Endocrinol. 2005;186:7–12. doi: 10.1677/joe.1.06374. [DOI] [PubMed] [Google Scholar]
- 73.Jahnke JR, Terán E, Murgueitio F, Cabrera H, Thompson AL. Maternal stress, placental 11β-hydroxysteroid dehydrogenase type 2, and infant HPA axis development in humans: Psychosocial and physiological pathways. Placenta. 2021;104:179–187. doi: 10.1016/j.placenta.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Howerton CL, Morgan CP, Fischer DB, Bale TL. O-GlcNAc transferase (OGT) as a placental biomarker of maternal stress and reprogramming of CNS gene transcription in development. Proc Natl Acad Sci U S A. 2013;110:5169–5174. doi: 10.1073/pnas.1300065110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Howerton CL, Bale TL. Targeted placental deletion of OGT recapitulates the prenatal stress phenotype including hypothalamic mitochondrial dysfunction. Proc Natl Acad Sci U S A. 2014;111:9639–9644. doi: 10.1073/pnas.1401203111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hantsoo L, Duffy KA, Sammel M, Johnson RL, Kim D, Grillon C, Epperson CN. Enduring impact of childhood adversity: Affective modulation of acoustic startle response during pregnancy and postpartum. Physiol Behav. 2023;258:114031. doi: 10.1016/j.physbeh.2022.114031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dube SR, Williamson DF, Thompson T, Felitti VJ, Anda RF. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abus Negl. 2004;28:729–737. doi: 10.1016/j.chiabu.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 78.Fleiss JL (1981) Chapter 13: The analysis of data from matched samples. Statistical Methods for Rates and Proportions, 2nd ed. New York: Wiley, pp 213–219.
- 79.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 80.Morgan CP, Chan JC, Bale TL. Driving the next generation: Paternal lifetime experiences transmitted via extracellular vesicles and their small RNA cargo. Biol Psychiatry. 2019;85:164–171. doi: 10.1016/j.biopsych.2018.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yehuda R, Daskalakis NP, Bierer LM, Bader HN, Klengel T, Holsboer F, Binder EB. Holocaust exposure induced intergenerational effects on FKBP5 ethylation. Biol Psychiatry. 2016;80:372–380. doi: 10.1016/j.biopsych.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 82.Yehuda R, Schmeidler J, Wainberg M, Binder-Brynes K, Duvdevani T. Vulnerability to posttraumatic stress disorder in adult offspring of Holocaust survivors. Am J Psychiatry. 1998;155:1163–1171. doi: 10.1176/ajp.155.9.1163. [DOI] [PubMed] [Google Scholar]
- 83.Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Depression Scale. J Reprod Infant Psychol. 1990;8:99–107. doi: 10.1080/02646839008403615. [DOI] [Google Scholar]
- 84.Murray L, Carothers A. The validation of the Edinburgh Postnatal Depression Scale on a community sample. Br J Psychiatry. 1990;157:288–290. doi: 10.1192/bjp.157.2.288. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary Figures and Tables.
Data Availability Statement
Our data are publicly available at Open Science Framework (https://osf.io/bp7as/).