Abstract
Objective
The objective of this scoping review was to identify the modifiable factors that impact the health and quality of life (QOL) of community-dwelling people with spinal cord injury (SCI).
Methods
Empirical journal articles were identified using three academic databases: CINAHL Complete, MEDLINE with Full Text, and PsycINFO. Full-text journal articlesincluded studies of participants who were community-dwelling with traumatic or nontraumatic SCI and were over the age of 18 years without cognitive impairment; published between 2000 and 2021; focused on modifiable factors impacting health and QOL; and conducted inAustralia, Europe, orNorth America. A data table was used to extract article information including authors, year of publication, country, sample, design and methods, purpose/objectives, and main findings. Qualitative data analysis software was used to categorize major findings inductively through content analysis.
Results
Thirty-one peer-reviewed articles consisting of qualitive, quantitative, and mixed-methods study design were included. This scoping review revealed modifiable factors that impact the health and QOL of community-dwelling people with SCI: sociostructural factors (social attitudes, health care access, information access, and funding and policies) and environmental factors (built environment, housing, transportation, assistive technology, and natural environment).
Conclusion
Future research should examine the influence of the modifiable factors on health and QOL using qualitative inquiry, adopting a community-based participatory research approach, and considering the implications of individual characteristics and resources.
Keywords: environmental, health, quality of life, sociostructural, spinal cord injury
Introduction
According to the World Health Organization (WHO), each year approximately 250,000 to 500,000 people sustain a spinal cord injury (SCI) globally.1 Around 85,556 people with SCI reside in Canada compared to 1,462,220 people in the United States.2,3 In Canada, it is estimated that 43,974 people sustained their SCI through traumatic and 41,582 through nontraumatic mechanisms.2 Causes of traumatic SCI include violence, accidents, natural disasters, and motor vehicle accidents, whereas causes of nontraumatic SCI include infections; neoplastic tumors; and degenerative, autoimmune, or congenital conditions.2,4 Longitudinal studies in high-income countries found that life expectancy for people with SCI has increased over the past seven decades, resulting from improved medical and rehabilitative care.4 Secondary health conditions (SHCs) are no longer the primary cause of mortality for people with SCI in developed nations4; however, they remain prevalent and negatively affect health and quality of life (QOL).5–8 With improved life expectancy, there has been an increased focus on the advancement of community rehabilitation goals, including health and QOL.4,5,9
The WHO defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”10 Health for people with SCI involves the daily management of the functional and physical effects of the condition, including SHCs such as pain, fatigue, autonomic dysreflexia, urinary and fecal incontinence, urinary tract infections, spasticity, pressure sores, hypotension, osteoporosis, cardiac disease, and mental health conditions.4,5,8,11,12 These effects negatively influence health and QOL.11,13
QOL is defined as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns.”14 Given the health and functional challenges of SCI, health is often used as a primary indicator of QOL.15 Health and QOL for people with SCI are closely intertwined; however, unmet community needs also contribute to and detract from QOL.4,8,15 Some of the unmet needs of people with SCI who are living in the community are related to transportation, accessibility of the built environment, and funding.8,16
A collaborative report by the WHO and the International Spinal Cord Society (ISCoS)4 highlighted the disruptive, yet modifiable (e.g., “amenable to intervention”17(p424)) nature of most unmet community needs. Previous reviews have identified some modifiable factors associated with QOL and community participation for people with SCI. For example, Hammell’s review,18 which focused exclusively on QOL for people with quadriplegia, found that disrupted QOL primarily results from limited social circumstances (e.g., inadequate transportation and income). Further, Barclay and colleagues19 provided insights into the barriers (e.g., transportation, built environment, health care providers, and associated services) and facilitators (e.g., personal assistance, equipment, social supports) related to community participation for people with SCI. Despite the evidence in the existing reviews and the call to action in the WHO and ISCoS report to redress these barriers and strive toward enabling environments, unmet community needs persist and disrupt health and QOL for people with SCI.4,8,20 This review aims to expand upon these earlier findings and call to action by focusing on modifiable factors that influence the health and QOL of community-dwelling people with SCI.
Objective
The primary objective of this scoping review is to identify the modifiable factors that impact the health and QOL of community-dwelling people with SCI. This review offers a preliminary discussion on how the identified modifiable factors are interconnected and interact with one another and provides an understanding into the complexity of achieving health and QOL for community-dwelling people with SCI.
Methods
This scoping review focuses on mapping extant literature examining the modifiable factors that impact health and QoL of community-dwelling people with SCI. This review follows the scoping studies framework by Levac and colleagues,21 which enables the investigation of broad research questions related to complex topics. The framework consists of five required stages: “(i) identifying the research question/s; (ii) identifying relevant studies; (iii) study selection; (iv) charting the data; (v) collating, summarizing, and reporting results.”21(p4) This review complies with the PRISMA-ScR extension.22
Stage one: Identifying the research question
This scoping review was guided by the following research question: What are the modifiable factors impacting the health and QOL of community-dwelling people with SCI? The target population for this review was community-dwelling people with SCI. The specific outcomes of interest were health and QOL; the concept was modifiable factors. Modifiable factors in this review refer to those that are “amenable to intervention.”17(p424)
Stage two: Identifying relevant studies
This scoping review was conducted by a research team consisting of individuals with content (e.g., SCI research) and methodological (e.g., research analysis) expertise. At this stage, two reference librarians (health and social sciences) were consulted by the research team for their content expertise to refine and further develop the search terms (e.g., key words) and strategy (e.g., search strings and pertinent databases) for study selection.
Stage three: Study selection
Relevant articles reporting original research were identified from three databases: CINAHL Complete, MEDLINE with Full Text, and PsycINFO (see search strings in eTable 1). Database searches were conducted in two phases: an initial search in November 2020, which identified articles published from 2000 to 2020, and a supplemental search in December 2021, which identified articles published in 2021. Key words were used for the database searches, organized by population, modifiable factor, and outcomes: population (e.g., spinal cord injur*, paraplegi*, quadriplegi*), modifiable factor (e.g., built environment), and outcomes (e.g., health and quality of life). Key word truncation was utilized to expand the searches. Peer-reviewed journal articles containing original research were selected based on the following inclusion criteria: published between 2000 and 2021; population included community-dwelling people with SCI (traumatic or nontraumatic) over the age of 18 without cognitive disability; published in Australia, Europe, or North America; and focused on modifiable factors that impact health and QOL. The exclusion criteria consisted of studies that included participants under the age of 18; participants who were living with cognitive disabilities (e.g., acquired brain injury) or locked-in syndrome, amyotrophic lateral sclerosis, cerebrovascular accident, or scoliosis; research conducted in acute care, subacute care, long-term care, and inpatient rehabilitation; and not conducted in Australia, Europe, or North America. Studies were excluded if they did not contain original research, including all types of literature reviews; however, their reference lists were searched by the first two authors (S.G., H.-T.J.) for relevant original research studies that met the inclusion and exclusion criteria.
Following the database searches, Covidence, an online tool that streamlines the review process,23 was used to screen article titles and abstracts based on the key words and research question to identify full-text articles for potential inclusion. The first and second authors independently screened all the imported titles and abstracts, resolving conflicts and reaching consensus through ongoing discussion. Subsequently, all the full-text articles were independently reviewed by the first and second authors. At this stage, conflicts resulting from full-text review were resolved by the third and fourth authors (H.C., W.B.M.) through ongoing discussion.
Stage four: Charting the data
The data chart format was determined in consultation with all research team members and was used to organize and synthesize findings. The chart contained the following headings: (a) authors, year of publication, and country, (b) participants, (c) methods, (d) purpose, and (e) salient findings (see eTable 2). Pertinent data from the final list of included articles were extracted and charted by the first and second authors collaboratively. This process was iterative and was subject to several revisions focused on how the extracted data were answering the research question.
Stage five: Collating, summarizing, and reporting the results
Inductive content analysis was utilized to analyze, collate, summarize, and report the results. As a research method, inductive content analysis aids in the process of distilling words into smaller content-specific categories.24 Inductive content analysis involved initial open coding (e.g., generating headings and corresponding notes), formulation of content-related categories (e.g., collapsing of open coding), and abstraction in relation to the research question. The process of inductive content analysis was supported by using NVivo, a qualitative software that enhances data management.25
Results
A total of 1507 articles were identified, of which 468 were excluded after eliminating the duplicates. This yielded 1039 articles that were evaluated for title and abstract screening. Eighty full-text articles were assessed for eligibility, resulting in a total of 30 items that were reviewed to identify the modifiable factors impacting health and QOL of community-dwelling people with SCI as illustrated in Figure 1. During the peer review process, an additional article was suggested to the authors for inclusion, bringing the total articles included in this review to 31. Of the 31 articles, 20 were qualitative, 10 were quantitative, and one was a mixed-methods study design. Moreover, 12 were conducted in Canada, 13 in the United States, four in Europe, and two in Australia. eTable 2 summarizes the characteristics of the studies selected for this scoping review.
Figure 1.
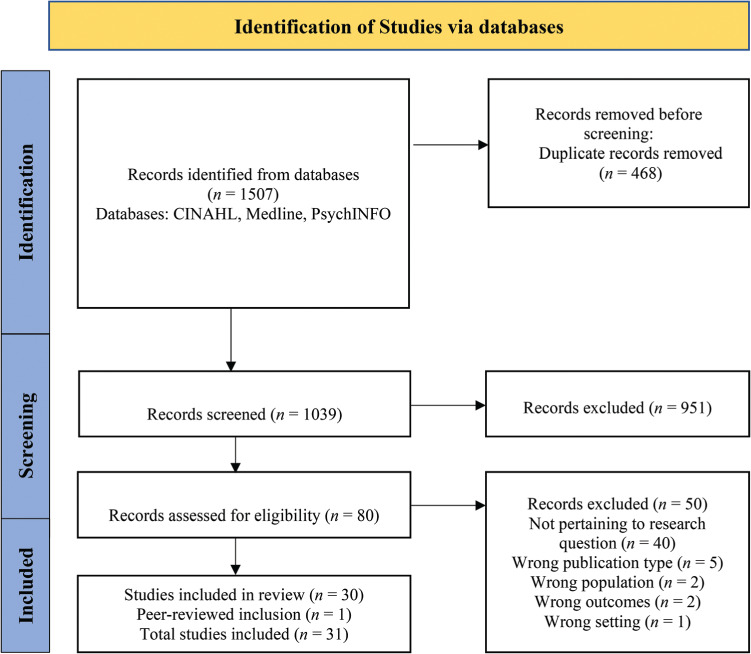
Flowchart showing the process for inclusion of studies.
Findings on modifiable factors that impact health and QOL
The health and QOL of community-dwelling people with SCI was found to be influenced by 10 modifiable sociostructural and environmental factors. Sociostructural factors included social attitudes, health care access, information access, and funding and policies. Environmental factors included the built environment, housing, transportation, assistive technology, and natural environment (eTable 3).
Sociostructural factors
Social attitudes
Included studies found that negative social attitudes in community settings can stigmatize, discriminate, and ostracize people with SCI, potentially leading to exclusion and a sense of invisibility. One study found a significant negative association between stigma and QOL and a positive association between stigma and symptoms of depression.26 Negative attitudes were experienced in various public settings including health care, the workplace, the community, and school.15,27–33 Family members, friends, and coworkers were reported to have negative attitudes toward people with SCI.27,28,32 However, a quantitative study reported that negative social attitudes were not a common experience for people with SCI.34 This finding was supported by a qualitative study that found not being treated differently by family and friends, as well as by the public, was disassociated with negative social attitudes.27 The impact of social attitudes, including stigma, can be connected to the length of time lived with injury, the length of an individual’s stay in rehabilitation, wheelchair use including the type of wheelchair (e.g., power wheelchair), perceptions of disability, and the internalization of previously held beliefs about disability.15,26
Health care access
Access to health care was affected by the expertise and skill sets of health care professionals, including primary care, specialists, interprofessional health care providers, and personal care assistants, and by administrative and system barriers.28,29,30,33 Some physicians and interprofessional health care providers were found to have limited SCI-specific knowledge and related interpersonal skills.29,35–41 Physicians who are not regularly treating people with SCI can be unaware of supportive resources; this resulted in missed opportunities to access other medical and interprofessional providers, as physicians often acted as primary gatekeepers.36–38
Access to health care can be facilitated by health care providers who go beyond meeting the basic care needs of people with SCI. When health care workers bypassed administrative procedures to expedite access to health care, it enhanced the autonomy and control of people with SCI over their care; for example, physicians granted standing orders for urine tests, enabling people with SCI to seek this care as and when they felt it was required.29 Homecare and nursing staff also provided care extending beyond their formally recognized duties.29 Occupational therapists were found to be key in facilitating both seating technology and wheelchairs, easing and supporting the process of procurement.35 Physicians who presented information clearly and concisely also supported the uptake of health knowledge and subsequent access to health care.42 Other dimensions facilitating access to health care that were related to professionals included qualities such as being committed, compassionate, and reliable and having a caring attitude.43
Timely health care access was hampered by administrative and systems barriers, including waitlists, wait times, and scheduling.29,30,43 Rigid scheduling can result in having to decide between accessing physician care and daily homecare services.29 Persons living in rural or remote settings experienced trouble accessing health care when physicians did not account for their additional travel time when scheduling appointments.29 When their health needs were unmet, people with SCI accessed the emergency room to obtain primary care health services; when accessing emergency services, they also faced barriers, such as long wait times.29
Alternative approaches to health care delivery and alternative treatment methods (e.g., music therapy, acupuncture)41 can potentially overcome barriers that impede health care access and cause ineffective treatment. Telehealth, self-management models, interdisciplinary approaches, and web-based services allowed people with SCI to access services with ease by avoiding the aforementioned barriers (e.g., scheduling, travel, and built environment).36,42
Information access
Health literacy played an important role in life satisfaction and was found to affect rates of morbidity and physical health.44 Limited access to required and reliable SCI-specific information was a barrier for many people with SCI.31,36–38,45,46 People with SCI experienced challenges with accessing information from health care professionals. Even though they are the preferred information source, health care professionals often had limited knowledge on SCI-specific needs or they were unavailable to people with SCI.29,38 Nevertheless, people with SCI identified that they accessed health information from the following sources: physicians, complementary and alternative medicine (CAM) specialists, informal networks, and other interprofessional providers.38,45,47 Other sources, such as the internet, were found to be readily accessible but were overwhelming or lacked trustworthiness.38,45,46 The timing of information delivery and the readiness to receive information can influence access to health information and its utilization.33,38
Funding and policies
Sufficient external funding directly affected health and QOL, as it allowed health services and equipment to be obtained as needed.27,48 Funding sources included social funding, private medical insurance, insurance from injury claims, and employment income.27 The cost of equipment (e.g., adapted vehicles and home modifications) and services (e.g., homecare, housekeeping, and formal caregiving) was high for people with SCI.9,15,35,46,49 Without sufficient external funding, people paid out of pocket for services such as optometry, dental, massage, rehabilitation services, CAM, professional counselling services, and equipment.15,29,30,37,43,46 Lack of financial assistance and prohibitive costs led to limited choices in equipment, reducing the options to items that did not always best support their needs.29 Insufficient funding was a common and prohibitive barrier; the impact of not having adequate funding for one aspect of community dwelling can create a cascading effect on health and QOL.
Gaps and overlooked aspects in policies and external funding can result in care fragmentation; a lack of access to suitable equipment, CAM services, interprofessional health services, and housing; and a lack of accountability for health service provision and equipment acquisition and maintenance.9,29,30,32,35,37,43,46,49–51 Policy gaps led to increased health expenditures for people with SCI and the health care system.15
Environmental factors
Built environment
Aspects and features of the built environment created physical barriers and acted as a deterrent to health and QOL. Inadequate curb cuts, steep gutters, potholes, and rough terrain were identified as disruptive sidewalk features15,27,29,40,48,49; this resulted in individuals using the roadways, which posed additional safety concerns, as vehicle operators can be unaware of people using mobility devices.29 Physical barriers were also found in outdoor spaces such as parks, beaches, trails, public swimming pools, and marinas.27,48
Despite accessibility being mandated via building codes, barriers in the built environment were also found in hospitals, health services buildings, hotels, public washrooms, motels, office spaces, stores, gyms, churches, and leisure centers.15,29,31,33,35,37,40,49,51 Buildings deemed accessible were sometimes inaccessible; for instance, despite the presence of a ramp, a participant in Manns and Chad’s study15 noted they were unable to access the post office due to the inaccessibility of the door. Even if a building had an accessible entry, studies noted that features within buildings could also present as obstacles.29,30,35 For example, some hospitals and health service offices lacked adjustable equipment to accommodate treatment.29,30 People with SCI living in rural Canada perceived barriers in the built environment more frequently compared to urban dwellers.12 Improving the accessibility and availability of fitness facilities, gyms, and public spaces was identified as a potential means to facilitate better community access and improve participation.48 Access to open space was found to be associated with better self-reported health.52 Increasing physical activity was anticipated to promote better health and QOL.48
Housing
Accessible housing was difficult to procure due to the lack of availability.29,40 This caused incongruent living environments that increased stress, negatively impacting QOL.29 Physical barriers within the home hampered individuals’ ability to engage in activities of daily living (ADL) and instrumental activities of daily living (IADL).28,40,50 Inaccessible homes resulted in an increased risk of injury and disrupted opportunities to engage with family and friends.28,40 Despite home modifications, challenges around accessibility to and within homes can persist and were similarly found to exist in rural settings, such as on reserve40 (e.g., federally owned land that is allocated for “the use and benefit of an Indian band”53(para. 5)). The inaccessibility of the homes of family members or friends was a commonly experienced environmental barrier impacting QOL.28
Transportation
Adapted vehicles and public transportation were not always readily available or equipped with accessibility features (e.g., lifts).15,27,28,31,32,40,48,49,51 This directly impacted access to community resources, such as health care professionals and equipment vendors, leading to decrements in health and QOL.27,51 This challenge was compounded for individuals living in rural and remote areas as they had to travel longer distances to access community, leisure, and health services.40 All forms of available public transportation needed to be accessible, including flexible features such as frequent bus service.32,48
Private transportation was not accessible to all people with SCI due to the cost and policies related to obtaining and maintaining an adapted vehicle.15,49,51 Individuals who owned vehicles faced barriers to utilizing them if they were unable to drive independently.48,51 Moving mobility devices in and out of vehicles presented additional challenges.32 A mismatch between the mobility device of the person with SCI and their adapted vehicle’s accessibility features also precluded the use of private transportation.49 The use of private transportation was frequently complicated by the features of parking spaces and the process of obtaining gasoline (e.g., assembling the wheelchair, filling the car with gasoline, going into the store to pay).27,29 Parking space location and the compatibility of parking space designs, including parking meters, were hindering aspects of designated parking.27,29 Actions that remediated parking issues included locating disability parking spaces closer to building entrances, providing sheltered parking, and increasing the size of parking spaces.48
Assistive technology
Assistive technology (AT) (e.g., equipment and software) had the potential to foster QOL for people with SCI.27,32,47 People with SCI used a variety of AT to carry out their ADLs and IADLs and to participate in their communities.29,35,40,51,54 AT can become inhibitory if it has shortcomings that complicate its use (e.g., physical aspects that impact the ability to grip the device), and people reported having difficulties gaining information about the diverse technologies available for their use.46 The integral facilitating nature of technology was highlighted by the following quote: “All these things are made easier and facilitated by technology so it’s invaluable that way.”46(p1365) In connection to health, functioning, and QOL, “the technology’s available to keep you mobile and healthy.”9(p615)
Natural environment
Even though weather conditions were not considered modifiable, study findings point to measures that can reduce the barriers created by weather conditions, such as adequate snow removal and sheltered bus stops.40,49 Inclement weather was identified as a barrier to transportation, community access, mobility, and access to resources.15,27,28,31,40,49 Weather conditions included precipitation, snowfall, temperature, and humidity, and they posed additional challenges for persons living in remote areas, such as on reserve.28,40,49 The heavy snowfall and subsequent melting that occur on reserve can cause unpaved roads to become inaccessible for prolonged periods of time.40
Discussion
This scoping review identifies sociostructural (e.g., social attitudes, health care access, information access, and funding and policies) and environmental (e.g., built environment, housing, transportation, AT, and natural environment) modifiable factors that impact the health and QOL of community-dwelling people with SCI; these determinants shape health and QOL through their independent and interdependent influences.
Comparing the link between the performance of the health system and subjective QOL across 22 (lower, middle, and upper income) countries revealed that the two greatest indicators of QOL for people with SCI were access to health care and social attitudes.55 The performance of the health care system is found to contribute to QOL; however, the current system is situated within a biomedical model that does not align with the care and support needs of people with SCI.55,56 Our findings show that access to health care is impeded for people with SCI and that health care providers can limit health care access by overlooking SCI and general health-related needs, inadequately prescribing medical supplies and equipment, and failing to refer to outside resources (e.g., occupational therapists).28–30,35–37,57 Within the biomedical model, primary care physicians are the first point of contact for health care needs, and their role extends beyond gatekeeping as they are central in mediating, coordinating, and providing health care and referrals.37,38,56,58
People with SCI also identified health care workers, including physicians, as lacking the necessary skillsets and knowledge to treat and manage their health needs.37,38 The challenges encountered by physicians in gaining the clinical fluency to treat people with SCI are identified by McMillan and colleagues57 to be the composition of residency training, unavailability of mentors and collaborative opportunities, fewer people with SCI in their practices, and the accessibility of SHC practice guidelines. The inability of community-dwelling persons with SCI to have their needs met causes them to use alternative strategies to access health care (e.g., internet, out-of-pocket services), which often prove unsustainable, resulting in avoidable health complications and the potential use of the emergency room as a means of primary care.29,30
The attitudes of health care providers also have implications for how people with SCI receive, respond to, and engage with health services and providers. Access to health care was facilitated when providers prioritized the needs of people with SCI by engaging in collaborative care, bypassing bureaucratic formalities, providing services beyond standard duties, and anticipating needs (e.g., equipment replacement).29,43 However, access to care can be negatively impacted by a lack of consideration by health care professionals when providing services, which is exhibited as negative social attitudes and practices.30 Health care encounters can be influenced by the inaccessibility of the built environment, which may originate from a failure to adopt universal design principles. For example, when examination beds lacked adjustability, untrained staff had to perform transfers, resulting in an unpleasant experience for people with SCI and demonstrating the interdependency between the social and physical environment. This connection is also illustrated by Chang and colleagues20 where people with SCI indicated that accessible elevators in transport stations become inaccessible due to able-bodied individuals occupying these spaces and their unwillingness to vacate them when necessary.
The biomedical perspective pathologizes disability; it leads to the prominent belief that people living with impairments are responsible for their disability and overlooks the sociostructural and environmental factors.59,60 Disabling situations occur when lifestyle factors (i.e., the social activities and roles that people engage in and adopt over the lifetime) interact with sociostructural and environmental factors that act as barriers to hinder the accomplishment of life habits.59 Notably, most modifiable factors can inhibit and enable the performance of life habits; for example, AT not only supports the immediate needs of people with SCI but can also increase independence in carrying out ADLs, resulting in a decreased demand for personal assistance from both informal and formal caregivers.54 A decreased requirement for caregivers can elicit positive psychosocial responses, restoring a sense of independence and autonomy for people with SCI.54 AT also enables people with SCI to regain privacy and the choice to be alone, which can afford control and autonomy and contribute to enhanced health and QOL.54 AT can also create disabling situations if its features create barriers to its utilization.46 Reframing disability as a social construct foregrounds the salience of the sociostructural and environmental factors and can promote the creation of environments that allow the full accomplishment of life habits.4,59
Identifying and situating the modifiable factors within three concentric layers (e.g., micro, meso, macro) is acknowledged by Fougeyrollas and colleagues59 to provide clarity into the origin of sociostructural and environmental factors and the intervention strategies required to alter them. Disability is not a static state; over their lifetime, people will fluctuate through environmental conditions that are disabling and nondisabling, and thus disabling situations are contextually and temporally dependent.59 Modifying the factors that create disabling situations, in a manner that fosters health and QOL, will counteract biomedical notions of disability, aid in the creation of inclusive environments, and allow for equitable societal participation of people with SCI. In identifying a broad range of modifiable factors, this review offers a starting point for understanding the complexities of factors that impact the health and QOL of community-dwelling people with SCI.
Implications for policy and practice
The identified sociostructural and environmental factors can be modified to support health and QOL for community-dwelling people with SCI. The findings from this scoping review have implications for more effective policy and program development and implementation. For example, access to health care can be improved through measures such as specialized training for health care providers including improved disability literacy (e.g., sensitivity training), advanced clinical handling and transferring skills, and models of care in favor of adopting flexible scheduling, individualization, and alternative delivery methods (e.g., online).56, 60–62 This includes also incorporating and co-locating multidisciplinary health care providers who specialize in SCI throughout the continuum of care and including SCI peer mentors into the provision of care.63 It is also important to address gaps in services that exist for people living rurally or remotely by capacity building for local care providers and supporting the use of telehealth.63 Improving social attitudes and reducing stigma can be achieved through a three-tiered approach that targets the intrapersonal, interpersonal, and structural levels.26 This can include providing counselling services and education to people with SCI to reduce the impact of stigma, building public awareness about disability and associated stigma through social campaigns, positively portraying disability in mass media, and enacting legislative changes that address the structural forces that propagate negative social attitudes.20,26 Further, there are several opportunities to reduce built environment and housing barriers that impede community access. Removal of these barriers can be facilitated by municipal policies that address poor neighborhood infrastructure (e.g., absent curb cuts) and the adoption of design policies and bylaws that are guided by the principles of “universal design” that extend beyond the minimum standards typically adopted in creating accessible facilities and homes.51,64 AT can increase accessibility and QOL; however, access to AT can be impeded by informational barriers (e.g., not knowing what AT is available) and challenges with the AT itself (e.g., design features causing cumbersome use).46,54 Addressing these barriers requires enhanced informational awareness about the variety of AT available, customization of the AT in alignment with the individual’s needs, and the provision of personalized training,46 which can be facilitated by providing access to trained professionals (e.g., OT) across the continuum of care (e.g., acute through community rehabilitation).65 Lastly, it is imperative that participatory research consider the lived experience of people with SCI in order to develop policies and programs in alignment with the needs of this population. In 2001, Manns and Chad15 advocated for this approach, stating that investigating QOL through subjective measures can lead to the creation of valid QOL indicators for this population and subsequently meaningful programs and policies.
Limitations
Studies included in this review were selected based on the criteria that they identified a modifiable factor in relation to health and QOL for community-dwelling people with SCI. Research that did not include health as a mediating variable was excluded; thus, few studies fully describe the importance of other determinants of QOL, such as employment and physical activity. Such factors have mediating effects on health and QOL; for example, income generated from employment may enhance a person’s ability to access out-of-pocket health services and maintain health and QOL, but it may also result in the termination of disability benefits.29 Included studies were conducted in Australia, Europe, and North America; this may limit the applicability of the findings to other geopolitical contexts as some of these countries have shifted toward a social model of disability. This is noteworthy because the current findings and implications for policy and practice have limited relevance in global south countries that may understand disability as an individual problem. Although a comprehensive search strategy was employed, a limitation may exist related to the particular databases utilized; there may be additional pertinent literature that was not captured in the search. Nonetheless, this review identifies and collates findings that contribute to our understanding of how these factors can create disabling situations and detract from health and QOL.
Future Directions
Future research should use qualitative methodologies66,67 to further elucidate an understanding of the complex and dynamic nature of the modifiable factors and their influence on health and QOL while adopting approaches that allow for collaboration and empowerment of people with SCI.68 Capturing the lived experience and co-creating knowledge will lead to a more holistic understanding of the impact of the factors and subsequent ability to create more targeted and actionable interventions. Characteristics of identity mediate between the individual and sociocultural contexts and should also be considered in relation to the modifiable factors and disabling situations.59 Thus, future research should be inclusive of the diverse groups within the SCI population and should explore how the modifiable factors are experienced and differentially influenced in the context of intersecting identities, such as race, ethnicity, gender, and age. Adopting sociostructural and environmental policy and practice changes with consideration of individuals’ intersecting identities can strengthen the capacity to enhance health and QOL of community-dwelling people with SCI.
Supplementary Material
Funding Statement
Financial Support Research was funded by the Praxis Spinal Cord Institute. Dr. Mortenson’s work was supported by a New Investigator Award from the Canadian Institutes of Health Research.
Footnotes
Conflicts of Interest
The authors report no conflict of interest.
REFERENCES
- 1.World Health Organization Spinal cord injury. November 19, 2013. https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury.
- 2.Noonan VK, Fingas M, Farry A et al. Incidence and prevalence of spinal cord injury in Canada: A national perspective. Neuroepidemiology . 2012;38(4):219–226. doi: 10.1159/000336014. [DOI] [PubMed] [Google Scholar]
- 3.Christopher and Dana Reeve Foundation Stats about paralysis. 2013. https://www.christopherreeve.org/living-with-paralysis/stats-about-paralysis .
- 4.World Health Organization, International Spinal Cord Society, eds, editor. International Perspectives on Spinal Cord Injury . World Health Organization; 2013. [Google Scholar]
- 5.Cobb J, Dumont FS, Leblond J, Park SE, Noonan VK, Noreau L. An exploratory analysis of the potential association between SCI secondary health conditions and daily activities. Top Spinal Cord Inj Rehabil . 2014;20(4):277–288. doi: 10.1310/sci2004-277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hetz SP, Latimer AE, Arbour-Nicitopoulos KP, Martin Ginis KA. Secondary complications and subjective well-being in individuals with chronic spinal cord injury: Associations with self-reported adiposity. Spinal Cord . 2011;49(2):266–272. doi: 10.1038/sc.2010.100. [DOI] [PubMed] [Google Scholar]
- 7.Levi R, Hultling C, Nash MS, Seiger Å. The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Spinal Cord . 1995;33(6):308–315. doi: 10.1038/sc.1995.70. [DOI] [PubMed] [Google Scholar]
- 8.Noreau L, Noonan VK, Cobb J, Leblond J, Dumont FS. Spinal cord injury community survey: A national, comprehensive study to portray the lives of Canadians with spinal cord injury. Top Spinal Cord Inj Rehabil . 2014;20(4):249–264. doi: 10.1310/sci2004-249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammell KW. Quality of life among people with high spinal cord injury living in the community. Spinal Cord . 2004;42(11):607–620. doi: 10.1038/sj.sc.3101662. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization Constitution of the World Health Organization, 45th ed., supplement. 2006. https://www.who.int/governance/eb/who_constitution_en.pdf
- 11.DeJong G, Hoffman J, Meade MA et al. Postrehabilitative health care for individuals with SCI: Extending health care into the community. Top Spinal Cord Inj Rehabil . 2011;17(2):46–58. doi: 10.1310/sci1702-46. [DOI] [Google Scholar]
- 12.Glennie RA, Batke J, Fallah N et al. Rural and urban living in persons with spinal cord injury and comparing environmental barriers, their health, and quality-of-life outcomes. J Neurotrauma . 2017;34(20):2877–2882. doi: 10.1089/neu.2016.4931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Garshick E, Kelley A, Cohen SA et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord . 2005;43(7):408–416. doi: 10.1038/sj.sc.3101729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization WHOQOL: Measuring quality of life. https://www.who.int/tools/whoqol
- 15.Manns PJ, Chad KE. Components of quality of life for persons with a quadriplegic and paraplegic spinal cord injury. Qual Health Res . 2001;11(6):795–811. doi: 10.1177/104973201129119541. [DOI] [PubMed] [Google Scholar]
- 16.Cox RJ, Amsters DI, Pershouse KJ. The need for a multidisciplinary outreach service for people with spinal cord injury living in the community. Clin Rehabil . 2001;15(6):600–606. doi: 10.1191/0269215501cr453oa. [DOI] [PubMed] [Google Scholar]
- 17.Trenaman L, Miller WC, Querée M, Escorpizo R. Modifiable and non-modifiable factors associated with employment outcomes following spinal cord injury: A systematic review. J Spinal Cord Med . 2015;38(4):422–431. doi: 10.1179/2045772315Y.0000000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hammell KW. Exploring quality of life following high spinal cord injury: A review and critique. Spinal Cord . 2004;42(9):491–502. doi: 10.1038/sj.sc.3101636. [DOI] [PubMed] [Google Scholar]
- 19.Barclay L, McDonald R, Lentin P. Social and community participation following spinal cord injury: A critical review. Int J Rehabil Res Int Z Rehabil Rev Int Rech Readaptation . 2015;38(1):1–19. doi: 10.1097/MRR.0000000000000085. [DOI] [PubMed] [Google Scholar]
- 20.Chang FH, Liu CH, Hung HP. An in-depth understanding of the impact of the environment on participation among people with spinal cord injury. Disabil Rehabil Int Multidiscip J . 2018;40(18):2192–2199. doi: 10.1080/09638288.2017.1327991. [DOI] [PubMed] [Google Scholar]
- 21.Levac D, Colquhoun H, O’Brien KK. Scoping studies: Advancing the methodology. Implement Sci . 2010;5(1):69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tricco AC, Lillie E, Zarin W et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med . 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 23.Babineau J. Product review: Covidence (systematic review software) J Can Health Libr Assoc . 2014;35:68–71. doi: 10.5596/c14-016. [DOI] [Google Scholar]
- 24.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs . 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 25.Zamawe F. The implication of using NVivo software in qualitative data analysis: evidence-based reflections. Malawi Med J . 2015;27(1):13. doi: 10.4314/mmj.v27i1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Monden KR, Philippus A, MacIntyre B et al. The impact of stigma on psychosocial outcomes following spinal cord injury: A cross-sectional analysis of stigma-mediated relationships. Rehabil Psychol . 2021;66(2):202–212. doi: 10.1037/rep0000371. [DOI] [PubMed] [Google Scholar]
- 27.Barclay L, McDonald R, Lentin P, Bourke-Taylor H. Facilitators and barriers to social and community participation following spinal cord injury. Aust Occup Ther J . 2015;63(1):19–28. doi: 10.1111/1440-1630.12241. [DOI] [PubMed] [Google Scholar]
- 28.Bökel A, Dierks ML, Gutenbrunner C et al. Perceived environmental barriers for people with spinal cord injury in Germany and their influence on quality of life. J Rehabil Med Stiftelsen Rehabiliteringsinformation . 2020;52(8):1–6. doi: 10.2340/16501977-2717. [DOI] [PubMed] [Google Scholar]
- 29.Goodridge D, Rogers M, Klassen L et al. Access to health and support services: Perspectives of people living with a long-term traumatic spinal cord injury in rural and urban areas. Disabil Rehabil Int Multidiscip J . 2015;37(16):1401–1410. doi: 10.3109/09638288.2014.972593. [DOI] [PubMed] [Google Scholar]
- 30.Neri MT, Kroll T. Understanding the consequences of access barriers to health care: Experiences of adults with disabilities. Disabil Rehabil Int Multidiscip J . 2003;25(2):85–96. doi: 10.1080/713813479. [DOI] [PubMed] [Google Scholar]
- 31.Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB. Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil . 2004;85(11):1793–1803. doi: 10.1016/j.apmr.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 32.Barclay L, Lentin Primrose, McDonald R, Bourke-Taylor H. Understanding the factors that influence social and community participation as perceived by people with non-traumatic spinal cord injury. Br J Occup Ther . 2017;80(10):577–586. doi: 10.1177/0308022617713699. [DOI] [Google Scholar]
- 33.Manns PJ, May LA. Perceptions of issues associated with the maintenance and improvement of long-term health in people with SCI. Spinal Cord . 2007;45(6):411–419. doi: 10.1038/sj.sc.3101973. [DOI] [PubMed] [Google Scholar]
- 34.Krause JS. Self-reported problems after SCI. Implications for rehabilitation practice. Top Spinal Cord Inj Rehabil . 2007;12(3):35–44. doi: 10.1310/sci1203-35. [DOI] [Google Scholar]
- 35.Gallagher A, Cleary G, Clifford A, McKee J, O’Farrell K, Gowran RJ. “Unknown world of wheelchairs” A mixed methods study exploring experiences of wheelchair and seating assistive technology provision for people with spinal cord injury in an Irish context. Disabil Rehabil . 2020:1–13. doi: 10.1080/09638288.2020.1814879. [DOI] [PubMed] [Google Scholar]
- 36.Hampton NZ, Zhu Y, Ordway A. Access to health services: Experiences of women with neurological disabilities. J Rehabil . 2011;77(2):3–11. [Google Scholar]
- 37.Kehn M, Kroll T. Staying physically active after spinal cord injury: A qualitative exploration of barriers and facilitators to exercise participation. BMC Public Health . 2009;9:168. doi: 10.1186/1471-2458-9-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Norman C, Bender JL, Macdonald J et al. Questions that individuals with spinal cord injury have regarding their chronic pain: A qualitative study. Disabil Rehabil Int Multidiscip J . 2010;32(2):114–124. doi: 10.3109/09638280903033248. [DOI] [PubMed] [Google Scholar]
- 39.Schladen MM, Libin A, Ljungberg I, Tsai B, Groah S. Toward literacy-neutral spinal cord injury information and training. Top Spinal Cord Inj Rehabil . 2011;16(3):70–83. doi: 10.1310/sci1603-70. [DOI] [Google Scholar]
- 40.Wearmouth H, Wielandt T. “Reserve is no place for a wheelchair”: Challenges to consider during wheelchair provision intended for use in First Nations community. Disabil Rehabil Assist Technol . 2009;4(5):321–328. doi: 10.1080/17483100902807120. [DOI] [PubMed] [Google Scholar]
- 41.Buscemi V, Cassidy E, Kilbride C, Reynolds FA. A qualitative exploration of living with chronic neuropathic pain after spinal cord injury: An Italian perspective. Disabil Rehabil . 2018;40(5):577–586. doi: 10.1080/09638288.2016.1271023. [DOI] [PubMed] [Google Scholar]
- 42.Jalovcic D, Pentland W. Accessing peers’ and health care experts’ wisdom: A telephone peer support program for women with SCI living in rural and remote areas. Top Spinal Cord Inj Rehabil . 2009;15(1):59–74. doi: 10.1310/sci1501-59. [DOI] [Google Scholar]
- 43.Matsuda SJ, Clark MJ, Schopp LH, Hagglund KJ, Mokelke EK. Barriers and satisfaction associated with personal assistance services: Results of consumer and personal assistant focus groups. OTJR Occup Particip Health . 2005;25(2):66–74. doi: 10.1177/153944920502500204. [DOI] [Google Scholar]
- 44.Johnston MV, Diab ME, Kim SS, Kirshblum S. Health literacy, morbidity, and quality of life among individuals with spinal cord injury. J Spinal Cord Med . 2005;28(3):230–240. doi: 10.1080/10790268.2005.11753817. [DOI] [PubMed] [Google Scholar]
- 45.Burkell JA, Wolfe DL, Potter PJ, Jutai JW. Information needs and information sources of individuals living with spinal cord injury. Health Inf Libr J . 2006;23(4):257–265. doi: 10.1111/j.1471-1842.2006.00686.x. [DOI] [PubMed] [Google Scholar]
- 46.Mattar AAG, Hitzig SL, McGillivray CF. A qualitative study on the use of personal information technology by persons with spinal cord injury. Disabil Rehabil Int Multidiscip J . 2015;37(15):1362–1371. doi: 10.3109/09638288.2014.963708. [DOI] [PubMed] [Google Scholar]
- 47.Drainoni ML, Houlihan B, Williams S et al. Patterns of Internet use by persons with spinal cord injuries and relationship to health-related quality of life. Arch Phys Med Rehabil . 2004;85(11):1872–1879. doi: 10.1016/j.apmr.2004.07.350. [DOI] [PubMed] [Google Scholar]
- 48.Carpenter C, Forwell SJ, Jongbloed LE, Backman CL. Community participation after spinal cord injury. Arch Phys Med Rehabil . 2007;88(4):427–433. doi: 10.1016/j.apmr.2006.12.043. [DOI] [PubMed] [Google Scholar]
- 49.Mortenson WB, Hammell KW, Luts A, Soles C, Miller WC. The power of power wheelchairs: Mobility choices of community-dwelling, older adults. Scand J Occup Ther . 2015;22(5):394–401. doi: 10.3109/11038128.2015.1049289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Duggan CH, Dijkers M. Quality of life after spinal cord injury: A qualitative study. Rehabil Psychol . 2001;46(1):3–27. doi: 10.1037/0090-5550.46.1.3. [DOI] [Google Scholar]
- 51.Scheer J, Kroll T, Neri MT, Beatty P. Access barriers for persons with disabilities: The consumer’s perspective. J Disabil Policy Stud . 2003;13(4):221–230. doi: 10.1177/104420730301300404. [DOI] [Google Scholar]
- 52.Botticello AL, Rohrbach T, Cobbold N. Differences in the community built environment influence poor perceived health among persons with spinal cord injury. Arch Phys Med Rehabil . 2015;96(9):1583–1590. doi: 10.1016/j.apmr.2015.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Statistics Canada Area of residence - On reserve - National Household Survey (NHS) Dictionary. 2011. https://www12.statcan.gc.ca/nhs-enm/2011/ref/dict/pop150-eng.cfm .
- 54.Verdonck MC, Chard G, Nolan M. Electronic aids to daily living: Be able to do what you want. Disabil Rehabil Assist Technol . 2011;6(3):268–281. doi: 10.3109/17483107.2010.525291. [DOI] [PubMed] [Google Scholar]
- 55.Barzallo D, Gross-Hemmi M, Bickenbach J et al. Quality of life and the health system: A 22-country comparison of the situation of people with spinal cord injury. Arch Phys Med Rehabil . 2020;101(12):2167–2176. doi: 10.1016/j.apmr.2020.04.030. [DOI] [PubMed] [Google Scholar]
- 56.Ho CH. Primary care for persons with spinal cord injury - not a novel idea but still under-developed. J Spinal Cord Med . 2016;39(5):500–503. doi: 10.1080/10790268.2016.1182696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McMillan C, Milligan J, Hillier L et al. Why do challenges still exist in primary care for patients with spinal cord injury? Exploring the medical model through a social disability lens. Can J Disabil Stud. 2020;9(4):111–137. [Google Scholar]
- 58.World Health Organization Main terminology. 2004. https://www.euro.who.int/en/health-topics/Health-systems/primary-health-care/main-terminology
- 59.Fougeyrollas P, Boucher N, Edwards G, Grenier Y, Noreau L. The Disability Creation Process Model: A comprehensive explanation of disabling situations as a guide to developing policy and service programs. Scand J Disabil Res . 2019;21(1):25–37. doi: 10.16993/sjdr.62. [DOI] [Google Scholar]
- 60.Oliver M. The individual and social models of disability. Paper presented at Joint Workshop of the Living Options Group and the Research Unit of the Royal College of Physicians; July 23, 1990; Published online 1990:7. [Google Scholar]
- 61.Braaf SC, Lennox A, Nunn A, Gabbe BJ. Experiences of hospital readmission and receiving formal carer services following spinal cord injury: A qualitative study to identify needs. Disabil Rehabil Int Multidiscip J . 2018;40(16):1893–1899. doi: 10.1080/09638288.2017.1313910. [DOI] [PubMed] [Google Scholar]
- 62.Fisher KR, Purcal C. Policies to change attitudes to people with disabilities. Scand J Disabil Res . 2017;19(2):161–174. doi: 10.1080/15017419.2016.1222303. [DOI] [Google Scholar]
- 63.Ho C, Atchison K, Noonan VK et al. Models of care delivery from rehabilitation to community for spinal cord injury: A scoping review. J Neurotrauma . 2021;38(6):677–697. doi: 10.1089/neu.2020.7396. [DOI] [PubMed] [Google Scholar]
- 64.Mace RL. Universal design in housing. Assist Technol . 1998;10(1):21–28. doi: 10.1080/10400435.1998.10131957. [DOI] [PubMed] [Google Scholar]
- 65.Mortenson WB, Clarke LH, Best K. Prescribers’ experiences with powered mobility prescription among older adults. Am J Occup Ther . 2013;67(1):100–107. doi: 10.5014/ajot.2013.006122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Meade MA, Reed KS, Krause JS. The impact of health behaviors and health management on employment after SCI: Physical health and functioning. Top Spinal Cord Inj Rehabil . 2016;22(1):39–48. doi: 10.1310/sci2201-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Patton MQ. Qualitative Research & Evaluation Methods Integrating Theory and Practice . 4th ed. SAGE; 2015. [Google Scholar]
- 68.Baum F. Participatory action research. J Epidemiol Community Health . 2006;60(10):854–857. doi: 10.1136/jech.2004.028662. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


