Abstract
Objectives:
Elucidating the active ingredients of psychological treatments is an important step in the scientific validation of these interventions. Component studies are one way to test which aspects of psychological treatments impact outcomes, or in other words, are the active ingredients of treatment. As research and popular interest in mindfulness-based programs grows, it is important to evaluate the active ingredients of these programs and to continually refine theorized models of the mechanisms of mindfulness. Studying active ingredients may help clarify which elements of mindfulness-based programs are most important for dissemination.
Methods:
We conducted a systematic review of component studies of mindfulness-based programs for adults with psychological conditions. PRISMA guidelines for systematic reviews were followed.
Results:
Eight component studies were identified. These studies dismantled mindfulness-based stress reduction, mindfulness-based cognitive therapy, unified mindfulness, and core mindfulness processes. The eight studies differed with respect to types of programs and populations studied, yet similarities emerged. Notably, acceptance coupled with awareness and mindfulness meditation training may be two promising active ingredients of these different programs.
Conclusions:
Future studies examining mindfulness-based programs should continue to attempt to dismantle active ingredients of treatment and use the findings to update theoretical models of mindfulness.
Keywords: systematic review, mindfulness-based programs, mindfulness-based interventions, dismantling, component study, active ingredients
One of the main tenets of psychological clinical science is that psychological services must be delivered only when their benefits are stated clearly and, crucially, scientifically validated (McFall, 2000). Much of the debate in the field of psychotherapy research since the rise in prominence of clinical science has focused on explaining how psychological treatments produce their effects: to what extent treatments are active due to their specific factors (e.g., specific procedures of a treatment protocol) or common factors (e.g., working alliance) (Mulder et al., 2017). That is, scientifically validating psychological treatments involves examining both which treatments work and how they work.
To answer the question of how psychological treatments work, one must first define several terms that are a part of the causal chain explaining how elements of evidence-based treatments produce their effects. Psychological treatments typically include at least one putative active ingredient, or specific factor of the treatment that is hypothesized to be related to the therapeutic change. An active ingredient could be a specific therapeutic skill, procedure, process, or otherwise specified component of a treatment protocol (Magill et al., 2015). Additionally, an active ingredient could also be comprised of common factors, or universal therapeutic processes shared by most or all treatments (Cuijpers, Reijnders, et al., 2019). Given that evidence-based treatments are on average moderately effective (Cohen’s d= .48; Lambert & Bergin, 1994), clarifying which components of treatment are active ingredients and which are more inert may help to improve the overall effectiveness of treatment, stronger engagement of client mechanisms of change, and may ultimately streamline dissemination and implementation of treatments.
Specific study designs have been employed to disentangle the effects of various aspects of treatment on outcomes. The term “component study” is an umbrella term to describe clinical trials that compare hypothesized active components of a particular evidence-based treatment (Bell et al., 2013). Component studies can be additive, in which a component is added to a treatment protocol because it is hypothesized to improve outcomes. Alternatively, in dismantling studies, a full treatment package is compared to a dismantled treatment condition with the hypothesized active component removed. The null hypothesis is that there is no difference in outcome between the full and dismantled treatment. If the full treatment condition is found to be more effective than the dismantled treatment, the component that was removed can be described as an active ingredient of treatment. Well-designed component studies, both additive and dismantled, should address the question of treatment dose. Some studies may choose to control for equal treatment dose between conditions, for example, by matching the number of sessions between conditions. Finally, in multicomponent treatments that are hypothesized to have several active ingredients, individual dismantled components may be compared to one another to test whether they differentially impact outcomes. However, failing to reject the null hypothesis in component studies leads to ambiguous conclusions. All conditions in component studies typically include both specific and common factors of treatments, and therefore null findings do not directly answer questions regarding the relative effects or contributions of specific versus common factors (Bell et al., 2013).
There are important distinctions between component studies and other types of clinical trials. Clinical trials that compare a treatment, or even a component of a treatment, to a non- treatment control group (e.g., waitlist) or to another distinct treatment (e.g., comparing cognitive behavior therapy to psychodynamic therapy) can only make conclusions about the effectiveness of a treatment. They cannot draw conclusions about which elements of treatment are driving the observed treatment effects.
Several meta-analyses have been conducted to study the overall effects of adding or dismantling treatment components, and whether the manipulation of specific factors in treatment has a substantive impact. Ahn and Wampold (2001) examined 27 dismantling studies spanning a broad range of types of treatments and psychological conditions and found no significant differences on outcome between full treatments and treatments with components removed. A similar and more recent meta-analysis revisited the same question (Bell et al., 2013) in 66 component studies. Findings indicated that among additive studies only, there was a small but statistically significant advantage for treatments with additional components on post-treatment targeted outcomes (d= .15) and a slightly larger significant effect on targeted (d= .28) outcomes at longer term follow-up. These effects were not simply due to receiving a greater number of treatment sessions, as the majority of additive studies in this meta-analysis held the number of sessions equal between conditions. Most recently, Cuijpers et al. (2019) synthesized results from 16 component studies of psychotherapies for treating adult depression (Cuijpers, Cristea, et al., 2019). The pooled effect size for full treatments compared to partial dismantled treatments was small but significant (Hedges’ g= .21) with low to moderate heterogeneity. The magnitude of this effect was comparable between additive (g= .22) and dismantling studies (g= .26).
One hurdle facing meta-analyses on methodological features is the difficulty of comprehensively identifying studies. Study design terms are not consistently used as indexing terms and therefore a simple database search of a term such as “dismantling” is likely to miss relevant studies. To address this problem, authors have taken various strategies such as including multiple design search terms, hand searching through prespecified journals and reference lists of publications likely to include component studies, and searching in specific databases of treatment studies (Ahn & Wampold, 2001; Bell et al., 2013; Cuijpers, Cristea, et al., 2019). Furthermore, these meta-analyses include such a broad selection of studies that are frequently underpowered, have uneven quality, and may have high risk of bias. The quality of reviews and meta-analyses is only as strong as the quality of the studies they include (Harris et al., 2014).
Taken together, the literature on component studies suggests that component studies have the potential for providing important knowledge about active ingredients of treatment and, in concert with mechanistic studies, may contribute to a clearer picture of how specific factors interact with client mechanisms of behavior change to impact outcomes. At the same time, component studies may perpetuate ambiguity in answering questions of specific vs. common factors and under which circumstances specific factors have an impact if they are underpowered or biased. Component studies may be more likely to contribute relevant knowledge when they target a specific clinical condition, are well controlled in terms of comparison group, and in the case of null results, make only logically grounded conclusions.
Popular interest and research into mindfulness-based programs (MBPs) for psychological conditions has rapidly expanded in the past two decades, and recent work has focused on elucidating the active components and mechanisms of MBPs. The development of psychotherapeutic protocols grounded in mindfulness theory and practice can be traced back to the development of mindfulness-based stress reduction (MBSR; Kabat-Zinn, 1990) beginning in 1979, with momentum increasing after the validation of mindfulness-based cognitive therapy (MBCT; Teasdale et al., 2000), which integrated mindfulness practice with tenets of cognitive behavioral therapy for depression. More recently, several MBPs have been developed to address addictive behaviors, including mindfulness-based relapse prevention (MBRP; Bowen et al., 2014) and mindfulness oriented recovery enhancement (MORE; Garland, Schwarz, Kelly, Whitt, & Howard, 2012). The effectiveness of MBPs has been well documented in many populations and conditions, such adolescents and young adults (Chi et al., 2018), chronic pain (Khoo et al., 2019), craving and negative consequences in substance use disorder (Grant et al., 2017), post- traumatic stress (Hilton, Maher, et al., 2017), women (Roos et al., 2019), racial and ethnic minorities (Greenfield et al., 2018), incarcerated populations (Bowen et al., 2006), and as a brief intervention for negative affect (Schumer, Lindsay, & Creswell, 2018). Furthermore, there is evidence across several types of MBPs that they may be particularly effective for individuals with greater symptom severity (e.g., those with a greater number of prior depressive episodes or comorbid substance use and mood symptoms Piet & Hougaard, 2011; Roos, Bowen, & Witkiewitz, 2017).
Despite recent evidence for the effectiveness of MBPs, there has yet to be a systematic review of the active ingredients of these types of programs. However, there are numerous theories attempting to explain how mindfulness and its underlying processes work. The Monitor and Acceptance Theory (MAT; Lindsay & Creswell, 2017) asserts that mindful attention skills increase awareness of one’s present moment experience which may directly improve cognitive skills, but also has the potential to increase the experience of affect and reactivity. MAT also describes mindful acceptance skills as changing how one relates to one’s own experiences, which improves emotion regulation, reduces craving and aversion, and improves health outcomes. Others have put forth a phenomenological and neurocognitive framework to understand mindfulness meditation that includes interacting dimensions of mind (object orientation, decentering, and meta-awareness) as well as mental qualities (aperture, clarity, stability, and effort) (Lutz et al., 2015).
Moving towards empirical validation of hypothesized active ingredients of mindfulness is critical at this point in time because as evidence for MBPs has proliferated, so too have its growing pains. Quality of research and implementation of MBPs has been inconsistent. Evaluating the evidence base of MBPs from the perspective of the National Institutes of Health Stage Model, Dimidjian and Segal (2015) reported the preponderance of evidence thus far has been focused on Stage I research, intervention development, and to a lesser extent on basic science and efficacy trials (Dimidjian & Segal, 2015). Further, there is a lack of research on efficacy in community clinics, effectiveness, and implementation and dissemination of MBPs. Researchers have also voiced reasonable criticisms about the lack of a consistent operational definition of mindfulness, problems with its measurement, and the wide array of content and format with which MBPs are delivered (Van Dam et al., 2018). Although not a panacea for all of these criticisms, clarifying the active ingredients of MBPs is an essential step that would guide operationalization of constructs, measurement refinement, and dissemination of the most effective elements of MBPs.
The current study is a systematic review to examine component studies of MBPs in order to identify the most effective elements of this type of treatment. A variety of MBPs have been developed to address a range of psychological conditions in diverse populations, and yet these programs tend to be grounded in the same (or similar) core elements. The core elements of MBPs have been conceptualized variously as shared practices (e.g., body scan meditation) or shared underlying processes (e.g., attentional control). This systematic review aims to study which of these elements is associated with the largest post-program effects on psychological outcome variables.
Given that prior meta-analyses of component studies demonstrate modest effects of active ingredients, but relatively more substantial effects when examining specific treatment outcomes or treatments for specific clinical conditions (Bell et al., 2013; Cuijpers, Cristea, et al., 2019), there are important considerations for this current study. First, we expect that examining components of MBPs specifically, as opposed to psychosocial treatments generally, may hold more promise as a strategy for identifying active ingredients for this type of program. Furthermore, although not a meta-analysis, this systematic review will discuss the impact of treatment components on primary study outcomes. Clarifying how MBP components impact outcomes is an important step towards validating theoretical models and mechanisms of MBPs.
Methods
Search Strategy
The methodology of this systematic review was submitted for pre-registration with PROSPERO, International prospective register of systematic reviews, in May 2019, and currently remains under review (ID 137165). The following electronic databases were used to identify peer-reviewed studies published in English from the earliest year available to July 2019: PubMed, PsycINFO. To identify mindfulness component studies, we included a range of search terms encompassing various types of study designs that allow for the evaluation of differential effects of specific treatment components. These search terms included: (“component study” OR “dismantling” OR “dismantle” OR “active component” OR “active ingredient” OR “additive designs” OR “multicomponent” OR “ABAB” OR “multiple baseline” OR “within-subjects design” OR “crossover design” OR “mechanism of action”) AND “mindfulness”. Additionally, the reference lists of included studies were examined to identify studies that electronic search may have missed.
Eligibility Criteria
All studies included in this systematic review met the following inclusion criteria. First, participants were adults over the age of 18 with an identified psychological condition. We focused on studies of adults with psychological conditions because we wanted the findings to be maximally relevant for development of MBPs for clinical disorders. Second, the studies tested components of an MBP including, but not limited to: mindfulness-based stress reduction or mindfulness-based cognitive therapy. At least one component of the program studied must be a type of formal mindfulness meditation practice. Studies testing interventions that consisted of similar practices such as yoga, tai chi, or other contemplative practices without explicit mention of mindfulness meditation were excluded. Third, study design must use a comparison group that allowed for testing of specific treatments components. For example, studies may use an additive comparator (e.g., standard treatment versus standard treatment plus additional component) or a dismantled comparator (e.g., standard treatment versus standard treatment with one component removed). Studies that compared two distinct treatments (e.g., MBCT versus CBT), or that compared a standard program versus control (e.g., MBSR versus waitlist control) were excluded.
Data Extraction and Synthesis
Titles and abstracts of retrieved citations were screened for initial eligibility. For the citations identified as potentially eligible, full text publications were obtained and screened against inclusion criteria. Data was extracted using the PICOS framework, which organizes characteristics of studies based on Population, Intervention, Comparator, Outcomes and Study design. Data synthesis was done as a formal narrative synthesis. It was expected that studies would be too few and heterogenous to conduct a quantitative synthesis or meta-analysis at this time. Given that we expected this body of literature to be relatively small and recent, we included all studies that met inclusion criteria regardless of their level of evidence or risk of bias, although studies with lower levels of evidence or high risk of bias were interpreted with caution. For all studies, we synthesized the primary psychological outcome variable that was tested for differences in pre- to post-program change between groups (e.g., change in negative affect after full MBP versus dismantled MBP). When available, we reported the standardized effect sizes, Cohen’s d, to compare relative efficacy of different mindfulness components. The studies reviewed were synthesized in a qualitative manner. Specifically, we expected several themes to emerge from the literature. For example, we planned a narrative synthesis of all studies that examined component processes that comprise mindfulness meditation (e.g., present moment awareness versus present moment acceptance of experience). Additionally, we synthesized studies that evaluate specific meditation practices common to several MBPs (e.g., body scan meditation versus loving-kindness meditation).
Quality Assessment
Risk of bias in publications was assessed using the National Institute of Health Quality Assessment of Controlled Intervention Studies (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). All studies meeting inclusion criteria were included in the narrative synthesis of findings even if they demonstrated risk of bias, but they were interpreted in the context of possible bias.
Results
Study Selection and Characteristics
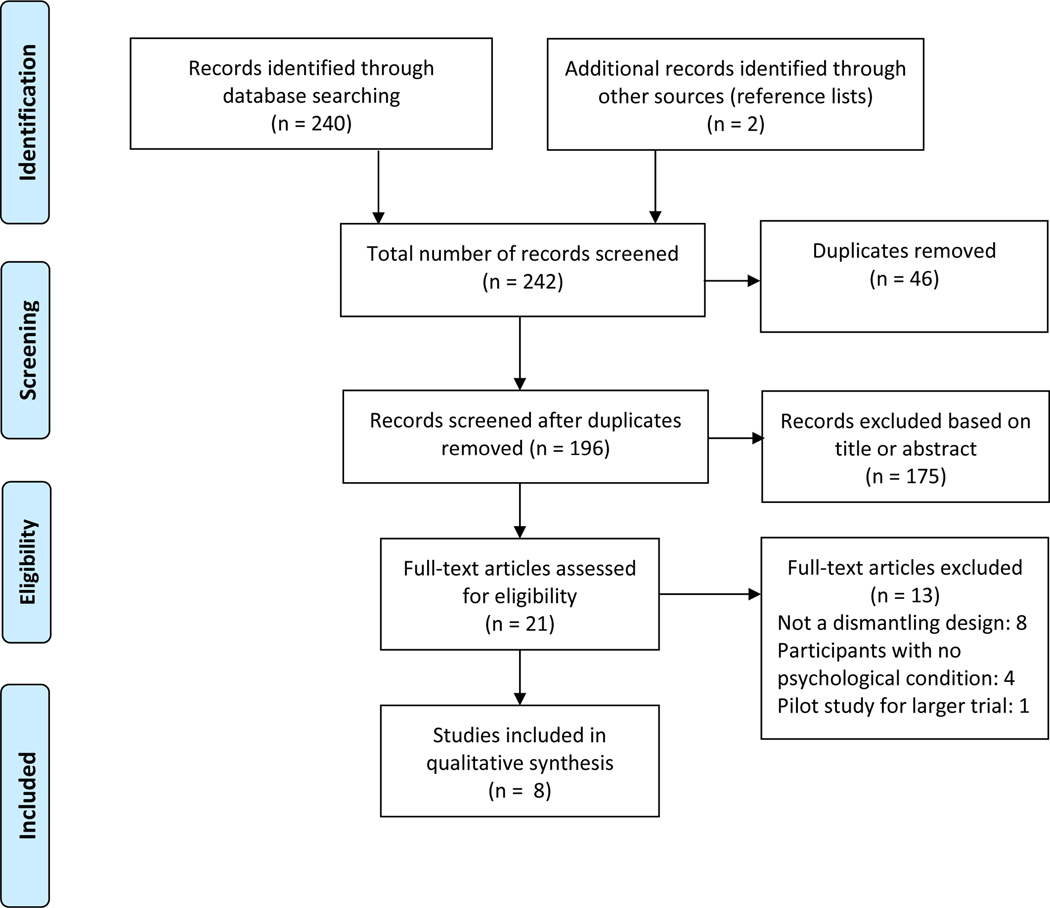
Initial database searches returned a total of 240 references from PubMed (87) and PsycInfo (153). Additionally, two references were identified from the reference list of publications, so the total number of records screened was 242. These references were screened for duplicates and 46 were removed, resulting in a total of 196 references from both databases. Of these 196 references, 175 were deemed ineligible based on initial screening of titles and abstracts by two independent raters. Full text articles were retrieved for the remaining 21 references and evaluated against the eligibility criteria by two independent raters. Twelve studies were excluded because they did not utilize a dismantling study design or recruit participants based on an identified psychological condition. One study (Chiesa et al., 2012) was excluded because it was a pilot study and data from the pilot study were included in the larger trial (Chiesa et al., 2015) that was included in the current review. Thus, eight studies met full eligibility criteria and were included in the qualitative synthesis. See Figure 1 for the PRISMA Flow Diagram (Moher et al., 2009) depicting these findings. Table 1 presents characteristics of these eight studies. Studies were evaluated for risk of bias using the National Institutes of Health’s Study Quality Assessment Tools for controlled intervention studies; these results are presented in Table 2. We attempted to contact the authors of studies that had missing details, but did not receive replies.
Figure 1.
PRISMA Flow Diagram
Table 1.
Study characteristics using PICOS framework (Population, Intervention, Comparator, Outcomes, Study design)
| Study | Population (N enrolled) | Psychological condition | Intervention (MBP) | Comparator | Outcome targeted | Outcome of program | Study design | Findings in relation to active components |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Britton et al., 2018 | 104 | Depression, clinical and subclinical | MBCT (8 week group) | MBCT, Focused Attention (FA), Open Monitoring (OM) | Mindfulness facets and skills, attention control | • FA>OM increased attentional control (ds= .36–75) | Dismantling | Both FA and OM components contribute to different aspects of cognitive control and mindfulness skill use, but more research is needed on health outcomes. |
| • OM>FA increased naming emotions, labeling thoughts, non-reactivity (ds=.33–.60) | ||||||||
| Chiesa et al., 2015 | 50 | Depression and unresponsive to antidepressant medication | MBCT (8 week group) | MBCT, Psychoeducation (MBCT – meditation) | Depression and anxiety symptoms, mindfulness facets, quality of life | MBCT> psychoeducation decreased depression (ds= .26–.79), increased mindfulness facets (ds= .25–.64), increased quality of life (ds= .36–.51), MA>MO decreased stress (ds= .27–.38) and NT (ds= .40–.62) | Dismantling | Meditation component is active for depression and quality of life |
| Chin et al., 2019 | 137 | Stress | MBSR (8 week group) | Monitor + Accept (MA), Monitor Only (MO), No treatment control (NT) | Self- reported stress | Dismantling | Evidence that acceptance skills training is active for stress reduction | |
| Lindsay, Chin et al., 2018 (study 1) | 137 | Stress | MBSR (8 week group) | Monitor + Accept (MA), Monitor Only (MO), No treatment control (NT) | Momentary and daily affect | • MA>MO, NT increased positive affect (gs= .22–.40, .73–.95) | Dismantling | Acceptance is active for positive affective outcomes, and to a lesser extent, negative affect outcomes |
| • MA>NT decreased negative affect (gs= .66) | ||||||||
| Lindsay, Chin et al., 2018 (study 2) | 153 | Stress | Core MBP processes (2 week smartphone program) | Monitor + Accept (MA), Monitor Only (MO), Active coping control | Momentary and daily affect | • MA>MO (gs= .41 – .46), control (gs= .66 – .71) increased positive affect | Dismantling | Acceptance is active for positive affect outcomes |
| Lindsay et al.,2019 | 153 | Stress | Core MBP processes (2 week smartphone program) | Monitor + Accept (MA), Monitor Only (MO), Active coping control | Daily loneliness and social contact | • MA>MO (d= .46), control (d= .45) decreased loneliness | Dismantling | Acceptance is active for social outcomes |
| • MA>MO (ds= .34 –.43), control (ds= .29 – .54) increased social interaction | ||||||||
| Lindsay, Young et al., 2018 | 153 | Stress | Core MBP processes (2 week smartphone program) | Monitor + Accept (MA), Monitor Only (MO), Active coping control | Stress reactivity: subjective and cardiovascular | • MA>MO (ds= .40 – .51), control (ds= .47 – .62) lower stress cortisol response | Dismantling | Acceptance is active for stress reactivity |
| MA>MO (d= .41), control (ds= .72) lower blood pressure | ||||||||
| Valdez et al., 2016 | 40 | Women who experienced assaultive trauma | Core MBP processes (Present moment contact (PMC) laboratory induction) | Non- judgement, control | State affect, trauma intrusions | • Control condition association between PMC and more negative affect, less positive affect | Component comparison | Present moment awareness component may be iatrogenic without concurrent non- judgement |
| • Nonjudgment condition association between PMC and fewer trauma intrusions | ||||||||
| Williams et al., 2014 | 274 | Remitted depression, at least three prior episodes | MBCT (8 week group) | MBCT, Cognitive psychoeducati on (MBCT – meditation), TAU | Time to relapse to depressive episode | • No main effect of condition on risk of relapse. | Dismantling | Meditation may be active for more clinically vulnerable groups |
| • Among those with high childhood trauma, lower risk of relapse to depression for MBCT compared to TAU (hazard ratio= .43) | ||||||||
Table 2.
Risk of bias considerations based on the NIH Quality Assessment of Controlled Intervention Studies tool
| Study | Randomization method | Treatment allocation concealed | Blinding of patients and providers | Blind assessors | No baseline group difference | Drop-out rate >20% | Drop-out rates between groups, >15% | Treatment protocol adherence | Other treatment avoided or similar | Valid and reliable outcomes measures | Sample size with at least 80% power | Pre-specified outcome analyses | ITT analysis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| Britton et al., 2018 | Good | Good | Fair | Good | Good | Good | Good | Good | Good | Fair | Good | Good | Fair |
|
| |||||||||||||
| Chiesa et al., 2015 | Good | Good | CD | Good | Good | Good | Good | Poor | Good | Good | Good | Good | Good |
|
| |||||||||||||
| Lindsay, Chin et al., 2018, Chin et al., 2019 | Good | Good | Fair | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good |
|
| |||||||||||||
| Lindsay, Chin et al., 2018, Lindsay et al., 2019, Lindsay, Young et al., 2018 | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good |
|
| |||||||||||||
| Valdez et al., 2016 | Good | NR | Good | Good | Good | NA | NA | Good | NA | Good | Poor | Good | Good |
|
| |||||||||||||
| Williams et al., 2014 | Good | Good | Poor | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good |
Note. NR=not reported; CD=could not determine; NA=not applicable
Of the eight included studies, three dismantled components of MBCT (Britton et al., 2018; Chiesa et al., 2015; Williams et al., 2014), two dismantled components of MBSR (Chin, Lindsay, Greco, Brown, Smyth, Aidan, et al., 2019; Lindsay, Chin, et al., 2018), three dismantled the Unified Mindfulness system for meditation training (Lindsay et al., 2019; Lindsay, Chin, et al., 2018; Lindsay, Young, et al., 2018), and one evaluated core mindfulness processes that are shared by most MBPs (Valdez et al., 2016).
The studies that met inclusion criteria delivered MBPs in a variety of formats. Four studies delivered the programs in a weekly group format that consisted of instruction in mindfulness practice (or control program), discussion of challenges in practice, and assignment of independent home meditation practice (Britton et al., 2018; Chiesa et al., 2015; Lindsay, Chin, et al., 2018; Williams et al., 2014). Four studies were based on a parent study delivering an MBP via smartphone application (Chin, Lindsay, Greco, Brown, Smyth, Wright, et al., 2019; Lindsay, Chin, et al., 2018; Lindsay et al., 2019; Lindsay, Young, et al., 2018). Finally, one study examined the effects of laboratory induced MBP components (Valdez et al., 2016).
Participant Characteristics
Across these eight studies, a total of 758 participants were enrolled. This number reflects participants initially enrolled and randomized in studies, even if they did not complete program or post-program assessment. Individual studies had sample sizes ranging from 40 to 274. Of note, several of the included publications reported on the same sample of participants (Chin, Lindsay, Greco, Brown, Smyth, Wright, et al., 2019; Lindsay, Chin, et al., 2018; Lindsay et al., 2019; Lindsay, Young, et al., 2018), so this sample was only counted once toward the total number of participants.
The effects of MBP components were tested in a variety of populations. Four studies recruited stressed adults from the community, as assessed by a cut-off score of five on the Perceived Stress Scale (Chin, Lindsay, Greco, Brown, Smyth, Wright, et al., 2019; Lindsay, Chin, et al., 2018; Lindsay et al., 2019; Lindsay, Young, et al., 2018). Three studies delivered MBCT to adults with clinical or subclinical affective symptoms including depression, anxiety, and stress (Britton et al., 2018; Chiesa et al., 2015; Williams et al., 2014). One study enrolled women who experienced physical or sexual assault trauma (Valdez et al., 2016).
Dismantling Mindfulness-Based Cognitive Therapy
Three studies utilized a dismantling design to test components of mindfulness-based cognitive therapy (MBCT; Teasdale et al., 2000). These studies reported the effects of MBCT components on post-program time to depressive episode, affective symptoms, trait mindfulness, mindfulness skill, attentional control, and general well-being. Two of these studies dismantled MBCT by comparing the full MBCT package to a version with mindfulness meditation training removed, thus testing the hypothesis that formal meditation training is the active ingredient of this program (Chiesa et al., 2015; Williams et al., 2014). In these studies, the comparison group was described as a psycho-education group that retained the same structure as MBCT, the same psycho-educational content about depression, and the same non-specific factors attributable to group psychotherapy. A third and more recent study by Britton et al. (2018) was a three-arm dismantling study comparing the full MBCT package to two structurally equivalent groups that isolated distinct hypothesized mechanisms of mindfulness meditation: a focused attention condition and an open monitoring condition. These three studies clarify the role of meditation training generally, and distinct meditation processes specifically, in MBCT.
The first MBCT dismantling trial by Williams et al. (Williams et al., 2014) enrolled adults with at least three prior depressive episodes, but no current episode, consistent with prior findings that MBCT is particularly effective for preventing recurrence of depression among individuals who have had at least three prior episodes (Piet & Hougaard, 2011). This sample had no prior regular meditation practice and were not concurrently receiving other therapy. In this well controlled dismantling study, researchers compared MBCT to a psycho-education comparator group and treatment as usual (TAU; which did not include any specific treatment given that participants were in remission, but instead, encouragement of participants to continue seeking treatment as usual from their health care providers). The researchers took care that the cognitive psycho-education comparator group retained all aspects of MBCT except for the experiential training in mindfulness through meditation practice, thus allowing for a precise examination of the effect of the meditation practice component. Although not strictly an intent- to-treat analysis (Moher et al., 2010) because 7% of the sample were missing all follow-up data, the results may be interpreted as having low risk of bias because of other methodological strengths (see Table 2). Outcomes assessed up to12 months post-treatment unexpectedly indicated that there was no main effect of treatment condition on risk of depression relapse. In other words, there was no statistically significant benefit of the specific factor of meditation training for the full sample of adults vulnerable to depression relapse, contrary to the findings of a prior meta-analysis on the effectiveness of MBCT (Piet & Hougaard, 2011). However, subgroup analyses revealed that those with more childhood trauma had lower risk of depression relapse if they received MBCT (41% relapsing) compared to TAU (65%; statistically significant) or MBCT compared to cognitive psycho-education (54%; not statistically significant, but perhaps clinically meaningful). This dismantling study provides evidence that mindfulness meditation training may be an effective active ingredient of treatment for those who are the most clinically vulnerable.
Similar in study design, Chiesa et al. (2015) also recruited a sample of adults with Major Depressive Disorder whose symptoms had not remitted after at least eight weeks on antidepressant medication. These authors compared MBCT to what they described as a structurally equivalent psycho-educational control group “excluding the main putative ‘active ingredient’ of MBCT (i.e., mindfulness meditation practice)” (Chiesa et al., 2015, p. 474). However, unlike a strict dismantling design where the comparison group is equivalent but for one removed component, the psycho-education control group in this study was described as including additional components not present in MBCT, such as the suggestion for participants to practice stretching or aerobic activity for 30–45 minutes, six days per week, as well as general information about factors to reduce or prevent depressive symptoms such as light exposure, balanced diet, and positive interpersonal relationships, information about behavior activation, and cognitive reappraisal strategies. Furthermore, other non-meditation components of MBCT were excluded from the psycho-education group (i.e., pleasant event recording or writing relapse plans). Although this study found greater improvements from full MBCT compared to the psycho-education group, particularly for depression symptoms and quality of life at long term follow-up, it remains unclear whether these advantages are due specifically to the addition of mindfulness meditation, or if these differences are instead capturing mindfulness meditation’s relative efficacy as compared to behavior activation and physical activity elements in the comparison group. Overall this study presents somewhat low risk of bias (see Table 2), but missing data was imputed using the last observation carried forward method, which may introduce bias (Hallgren & Witkiewitz, 2013). We are limited in drawing concrete conclusions from this study about the specific impact of the meditation component, but there is clear evidence that MBCT confers benefit in reducing depressive symptoms compared to an active control group.
A third MBCT dismantling trial took a different approach, instead disentangling the effects of two distinct meditation processes: focused attention (FA), training sustained attention on a specific target or object (e.g., the breath), and open monitoring (OM), training a nonreactive and nonjudgmental awareness to all present emotional, cognitive, or perceptual experiences, without a specific attentional target (Britton et al., 2018). FA and OM can be thought of as opposing mechanistic targets of MBPs; FA encourages shifting attention away from thoughts and emotions, and instead toward a specific attentional target, while OM directs attention towards whatever thoughts and emotions are happening in the moment. This study recruited a sample that included non-clinical and mild to moderate clinical expressions of affective disturbances, including depression, anxiety, and stress. Britton et al. developed eight-week groups for FA and OM that were structurally equivalent to MBCT. Participants were randomized to receive either MBCT, FA, or OM and pre-post change in mindfulness was assessed by the Five Facet Mindfulness Questionnaire and the Attention Control Questionnaire. Findings indicated that the dismantled components resulted in some differential skill acquisition that corresponded with the hypothesized mechanistic target of each: the OM group more frequently labeled passing thoughts and emotions in response to negative affect than the FA group. The FA group, on the other hand, was more likely to bring focused attention to the breath in response to negative affect than the OM group. However, both FA and OM groups showed increases in non-reactivity and attentional control following the program and the full MBCT group also showed significant increases across all mindfulness skill and attention control measures. Although this component study contributes important evidence that dismantled components of MBCT successfully engage different aspects of mindfulness, it remains unclear from this particular study if or how clinical outcomes are impacted by different mindfulness skill engagement.
Dismantling Mindfulness-Based Stress Reduction
Two articles examined components of mindfulness-based stress reduction (MBSR) and tested their effects on affect, stress, and judgement. These were derived from the same parent study in which MBSR was dismantled by removing the acceptance training skills from the full program in order to compare the effect of present moment monitoring plus an attitude of acceptance versus present moment monitoring alone (Chin, Lindsay, Greco, Brown, Smyth, Wright, et al., 2019; Lindsay, Chin, et al., 2018). These studies shed light on the effects of different psychological processes found within MBSR.
Chin, Lindsay, and colleagues (2019; 2018) used a three-arm dismantling randomized controlled trial to test hypotheses derived from the Monitor and Acceptance Theoretical framework (Lindsay & Creswell, 2018). Participants were 137 adults with scores greater than five on the Perceived Stress Scale, who were recruited from the community. These authors theorized that mindfulness training broadly, and MBSR specifically, can be broken down into monitoring skills (attending to ongoing present moment sensory and perceptual experiences) and acceptance skills (attitude of openness, equanimity, nonjudgement, and nonreactivity toward experiences). The standard eight-week MBSR group program was characterized as Monitor + Accept (MA), while the comparator group was Monitor Only (MO), which retained the structure of MBSR while removing all language and training alluding to acceptance, nonjudgement, or noninterference. Instead, the MO group was trained in concentration and focused attention, redirecting attention back to the target (e.g., breath, body) when the mind wandered. Other standard MBSR practices that indirectly promoted acceptance, such as loving-kindness, were removed from MO. Additionally, there was a no treatment (NT) control group. All three groups completed ecological momentary assessment and end-of-day diary assessments of positive affect, negative affect, stress, and judgement for three days pre- and post-program (MA and MO) or at the equivalent timepoints (NT). Results of this study indicated that both MA and MO significantly increased positive affect from pre- to post-program, but the magnitude of this change was larger for MA (ds= .61-.70) compared to MO (ds= .32-.43). Both MA and MO increased positive affect to a greater extent than the NT control group. The impact of acceptance skills on negative affect was slightly less pronounced: MA and MO showed equivalent decreases in daily diary reports of negative affect, although MA’s decrease was significantly greater than NT, while MO’s decrease was not significantly different from NT. Furthermore, there was only an effect of time, not time by condition, on momentary negative affect ratings. Thus, this study provided evidence that acceptance skills training is an active ingredient of MBSR impacting primarily positive affect, with a weaker effect on negative affect.
In analyses based on the data from the same parent study, Chin et al. (2019) focused on the effect of MBSR components on change in stress resiliency pre- to post-program as measured by both momentary stress ratings and number of daily stress occasions. All groups showed decreases in reports of momentary stress over time (MA: d= .85; MO: d= .59; NT: d=.44). However, consistent with the hypothesis that acceptance skills are a critical component in targeting stress resilience, the MA group showed a significantly greater decrease in momentary stress ratings compared to MO (d= .27) and to NT (d= .40) and there was no significant difference in stress reduction between MO and NT (d= .13). A comparable effect was observed on number of daily stress occasions, where all groups reported a decrease from pre- to post-program (MA: d = .73; MO: d = .36; NT: d = .16), and this change was significantly greater for MA compared to both MO (d= .38) and NT (d= .62). No significant difference in magnitude of change was found between MO and NT (d= .22). Finally, these authors tested the impact of the program on change in perceptions of momentary nonjudgement (i.e., to what extent participants had been judging as good or bad: themselves, their thoughts and feelings, situations, and other people). The hypothesis was that acceptance skills training would be an active ingredient in targeting nonjudgement as a mechanism of change for stress outcomes. Findings indicated a main effect of time such that all participants increased in their reports of nonjudgement (MA: d= .88; MO: d= .73; NT: d= .31), and MA increased nonjudgement significantly more than MO (d= .16) and NT (d= .56). Additionally, MO increased in nonjudgment compared to NT (d= .39). However, it is important to note that ratings of momentary stress and nonjudgment were taken concurrently, which precluded testing of the actual mediation model proposed by these authors. The articles based on this parent study demonstrate that several psychological outcomes (positive affect, stress) were substantially improved with the inclusion of an acceptance skills component and that cultivating an attitude of nonjudgement remains a promising, if yet unconfirmed, mechanism of this effect.
Component Studies of Core Mindfulness Meditation Processes
Several studies that test components of MBPs in order explore the active ingredients do so not by dismantling complete, empirically-validated treatment packages (e.g., MBCT, MBSR), but rather by comparison of components consisting of distinct mindfulness psychological processes (e.g., focused attention) that are central to practically all versions of MBPs. In this way, many of these component studies are not traditional dismantling or additive designs testing specific procedures from full treatment packages. Instead, they test the relative efficacy of core components that may represent distilled processes across MBP type.
Valdez et al. (2016) conducted the only MBP component study based entirely in laboratory manipulation of a two component operational model of mindfulness processes. These authors describe these components as present moment contact (PMC) and nonjudgment. The sample consisted of women who experienced physical or sexual assault, 31% of whom exhibited symptoms consistent with PTSD. Participants completed the following procedures in the laboratory: state affect assessment, Thought Listing Procedure (TLP: writing down “whatever information is present in your awareness from moment to moment [...] includ[ing], but not limited to, descriptions of images, memories, feelings, fantasies, plans, sensations, observations, daydreams, objects that catch your attention, or efforts to solve a problem,” p. 576), then random assignment to either the nonjudgment experimental condition or control condition. The nonjudgment induction asked participants to imagine example written scenarios as vividly, concretely, and objectively as they could, with no explicit instruction to pay attention to the present moment. The control condition asked participants to count the number of verbs in each scenario to match cognitive load. Following the experimental or control manipulation, participants underwent an interview about their traumatic experiences. After the interview, all participants completed the TLP and state affect assessment again. Outcome variables included trauma intrusions in the post-interview TLP (i.e., “intrusive thoughts, images, and/or memories of the traumatic event when tasked with writing about current conscious internal experiences”, p. 575) and post-interview affect. The extent to which participants were attending to the present moment was based on an index of present tense words found in their TLP written responses. This study design, therefore, involves and measures core mindfulness processes (i.e., present moment focus, nonjudgement), but not in the form of actual meditation practice. Valdez et al. found that for those in the control condition, post-interview PMC was negatively associated with positive affect, positively associated with negative affect, and unrelated to trauma intrusions. For those in the nonjudgment induction condition, post-interview PMC was unrelated to either positive or negative affect, but was negatively correlated to trauma intrusions. These findings suggest that the mindfulness component of present-focused awareness may, in fact, be harmful without the concurrent practice of nonjudgment.
In a series of studies based on the same parent study, Lindsay and colleagues tested the effect of dismantled present moment monitoring only (MO), combined present moment monitoring and acceptance (MA), and an active control group (coping control) on a range of outcome variables: subjective stress reactivity, cardiovascular stress reactivity (Lindsay, Young, et al., 2018), positive affect via ecological momentary assessment (EMA) and daily diary reports (Lindsay, Chin, et al., 2018), loneliness, and social contact in daily life (Lindsay et al., 2019). The parent study was a randomized controlled trial that recruited stressed adults from the community to complete one of three 14-day smartphone program conditions, plus three days of EMA and daily diary assessment immediately preceding and following the program. Unlike a prior study by the same researchers that dismantled group-based MBSR into monitor only (MO) and monitor plus acceptance (MA) components (Chin, Lindsay, Greco, Brown, Smyth, Wright, et al., 2019; Lindsay, Chin, et al., 2018), the smartphone iteration allowed for a more precise isolation and distillation of mindfulness component processes by carefully controlling content in each experimental condition and eliminating common factors of a psychotherapy group. In this study, training in core mindfulness components was based on the Unified Mindfulness program (Young, 2016). The MA program taught present moment monitoring as ‘sensory clarity,’ emphasizing detecting subtle experiences and discriminating between types of experiences. Concurrently, acceptance skills were taught as ‘equanimity,’ welcoming and accepting each and every present moment experience. The MO program taught concentration on present moment monitoring as sensory clarity alone, excluding all reference to acceptance and equanimity. Finally, the coping control program instructed participants to let their mind drift (as opposed to concentration) and use past or future-focused cognitive coping skills such as analyzing, reappraising, and problem solving. All three conditions were structurally equivalent, involving a daily 20-minute audio lesson and assigned homework (3–10 minutes). Each of the 14 daily lessons included didactic instruction, guided practice, and self-guided practice.
The primary prediction in this study was that the acceptance skills component would be necessary for lowering stress reactivity. Both subjective ratings of stress and objective biological measures of stress were measured. In the week following MA, MO, or control program, participants completed a stress reactivity protocol that included a social-evaluative stress reactivity laboratory task (a modified Trier Social Stress Test; mTSST). In the mTSST, participants were told they would be giving a speech performance and had three minutes to prepare. Before giving the speech, all participants underwent a 20-minute booster session consistent with whichever program they had been randomized to. Next, study assessors with a cold demeanor filmed the participants giving a speech performance and performing mental arithmetic, then gave them critical feedback afterward. Participants were debriefed at the end. Blood pressure was read during preparation, training, and performance phases of the task, as well as during recovery after the task. Salivary cortisol was measured before and after the task to assess resting and peak cortisol reactivity. Subjective stress ratings were taken immediately after both the speech performance and the arithmetic performance. Results indicated that participants in the MA group exhibited improved cardiovascular stress reactivity compared to both the MO and control groups. Specifically, those in the MA group had significantly lower peak cortisol levels after the mTSST task than the MO group (ds= .50 - .51) and control group (ds= .55 - .62), and there was no significant difference in peak cortisol level between the MO group and control group. A similar pattern was observed with respect to blood pressure such that the MA had lower systolic blood pressure during the mTSST than the MO group (d= .41) and control group (d= .72). This effect was not observed for diastolic blood pressure during the task. Although there were clear improvements in cardiovascular stress reactivity with the inclusion of the acceptance component, this advantage did not extend to subjective stress ratings taken during the mTSST. There were no significant differences in self-reported stress between any of the three conditions. This study provides important evidence that a 14-day smartphone program impacts cardiovascular stress reactivity during a social-evaluative stress induction, and that training acceptance of experiences is a critical component driving these outcomes.
Examining the effect of dismantled monitoring and acceptance on post-program affect, results indicated that participants in both the MA and MO conditions significantly increased daily diary positive affect ratings (overall positive affect, happiness, calm, vigor; MA: ds= .52 - .70; MO: ds= .25 - .35) and momentary positive affect ratings (MA: d= .39; MO: d= .15) from pre- to post-program. The control group did not report an increase in either daily diary or momentary positive affect. Compared to the MO group, the MA group increased to a greater extent on daily diary positive affect ratings (overall positive affect, happiness; gs= .46 - .54) and momentary positive affect ratings (g= .41). The control group and MO group were not statistically different from one another in their positive affect rating changes. Together, these results suggest that without acceptance skills training, present moment monitoring has a mild effect, but acceptance skills training is the active ingredient for improving positive affect. Notably, there was a main effect of time on daily and momentary negative affect ratings such that participants on average reported less negative affect from pre- to post-program, but there was no effect of group. This may indicate that all three types of programs were active for reducing negative affect.
In a third set of analyses, Lindsay et al. (2019) investigated the impact of monitoring and acceptance on loneliness and social interaction, two well documented risk factors for overall mental health and well-being. They hypothesized that training in mindfulness components (specifically the inclusion of acceptance skills), which emphasize intrapersonal processes, might also have an effect on interpersonal outcomes, although they do not test a specific mechanistic model by which these effects might occur. Several social processes were measured using EMA and daily diary assessments in the three days immediately before and after the program, including subjective perceptions of loneliness as well as objective numbers of social interactions and social interaction partners. Consistent with these authors’ previous findings that acceptance was an active ingredient, the MA group significantly decreased daily diary ratings of subjective loneliness from pre- to post-program (d= .44), while the MO and control groups showed no change in loneliness over time. The MA group showed more substantial reductions in loneliness when compared to the MO group (d= .46) and the control group (d= .45), and the MO and control groups were not significantly different from one another. In terms of objective social contact measured using both EMA and daily diary reports, those in the MA group reported a significant increase in the number of daily social interactions from pre- to post-program (d= .31 - .47), while the MO and control groups did not change. The increase in number of daily social contacts was significantly greater for the MA group as compared to the MO group (d= .34 - .35) and control (d= .29 - .52) group. Finally, this same effect was also evident in the daily diary reported total number of social interaction partners, in which the MA group reported a significant increase in social interaction partners from pre- to post-program (d= .39) and the MO and control groups did not change. Direct group comparisons revealed that the MA group had a significantly greater increase in social interaction partners compared to the MO group (d= .43) and the control group (d= .54). These results suggest a consistent pattern that the acceptance component, coupled with present moment monitoring, is an active ingredient in a smartphone program that may impact intrapersonal outcomes and also social processes.
Discussion
This systematic review examined the nascent literature of component studies of mindfulness-based programs (MBP) in order to evaluate the current evidence on active ingredients of this type of treatment for psychological conditions. The eight studies included were diverse in terms of particular MBPs, delivery format, and populations. Three dismantled MBCT with depressed adult samples and two dismantled MBSR with stressed adults recruited from the community. Three studies evaluated components using a smartphone-based program that isolated core MBP process component based on the Unified Mindfulness approach. Lastly, one study tested core MBP processes that are thought to be shared across nearly all MBPs. These studies also took several different theoretical approaches to describing and testing components. The majority of studies utilized a dismantling study design, while one study consisted only of a laboratory induction of core mindfulness components.
Despite the heterogeneity of these component studies, some coherent themes emerged.First, several studies indicate the critical importance of a component consisting of either acceptance skills or related concepts such as openness and nonreactivity to experience. In a series of high quality studies comparing present moment monitoring alone to present moment monitoring plus acceptance, researchers show that those randomized to the condition including acceptance had significantly improved outcomes in terms of positive affect, negative affect, daily stress, social interactions, and physiological stress reactivity compared to the monitoring only and control conditions (Chin, Lindsay, Greco, Brown, Smyth, Aidan, et al., 2019; Lindsay, Chin, et al., 2018; Lindsay, Young, et al., 2018). Notably, these findings were consistent with a proposed mechanistic model explaining how mindfulness impacts health outcomes, that it is the combination of monitoring and acceptance that encourages nonreactivity and improved emotion regulation (Monitor and Acceptance Theory; Lindsay & Creswell, 2017). In a laboratory dismantling experiment, Valdez et al. (2016) show that present moment awareness in the absence of cultivating an attitude of acceptance or nonjudgement may even have the potential to be harmful. However, given that theirs was a laboratory experiment, their findings would be strengthened if replicated in a clinical trial that was designed to test whether acceptance/nonjudgment mediates the effect of present moment awareness on outcomes. Another study by Britton and coauthors (2018) showed an effect of open monitoring, a closely related construct to acceptance. These researchers make the point that there may be different forms of acceptance, one that more closely resembles reappraisal (e.g., deliberately changing one’s response to a difficult experience towards a more accepting stance), and another that involves such intensive and objective open monitoring of experience that there is no room left for reactivity and thus equanimity arises naturally. The latter is what Britton et al. isolated as their open monitoring component, which did not include specific instruction on acceptance in the reappraisal sense. They found that the open monitoring component increased the mindfulness facets of naming emotions, labeling thoughts, and non-reactivity. Taken together, these studies show that acceptance coupled with awareness holds promise as an important active ingredient of MBPs. These findings are consistent with prior literature on the mechanisms of MBPs. Specifically, prior research has demonstrated that acceptance or nonreactivity to experience is a mediator of treatment outcome (Gu et al., 2015). The current study lends further support for an acceptance or nonreactivity active component of MBPs, which is key to many theoretical models of mindfulness and is supported by several lines of research.
An important future step will be to clearly define and operationalize acceptance in order to understand how, mechanistically, it exerts its effect on outcome. It may be the case that acceptance skills training can be thought of as a specific factor of treatment, insofar as it involves specific didactic content and meditation instruction on how to approach all experiences with acceptance. On the other hand, another likely possibility is that aspects of acceptance that operate more like a common factor, especially since most group-based MBPs strongly emphasize that the group facilitator should model nonjudgment and equanimity in order to create an overall atmosphere of acceptance. Indeed, psychotherapy literature originating with Carl Rogers has pointed to the importance of empirically testing constructs similar to acceptance as a key therapeutic component (Miller & Moyers, 2017). As Rogers defines it in his seminal paper on the necessary and sufficient conditions of psychotherapy, unconditional positive regard includes “experiencing a warm acceptance of each aspect of the client’s experience... mean[ing] that there are no conditions of acceptance” (Rogers, 1957). There may be substantial overlap in previously studied common factor constructs including unconditional positive regard, acceptance, and nonjudgement, making it likely that these constructs share higher order meaning.
Another theme supported by studies in this review was that meditation training was an active component. Two studies employed a similar design dismantling MBCT by comparing the full treatment to a condition with meditation features removed. The dismantled component was thus described as a cognitive psychoeducation component (Chiesa et al., 2015; Williams et al., 2014). These studies found advantages for the full MBCT condition in terms of reductions in depression symptoms, increased quality of life, and lower risk of relapse to depressive episodes for the subgroup that also had greater childhood trauma, all indicating that meditation is an active component. From a practical perspective, it may be clinically useful to know that meditation itself, as an experiential component of treatment, has a significant effect on outcomes, at least among subgroups of vulnerable clients. This may be relevant especially as MBPs are adapted and streamlined for other clinical settings and mobile delivery. However, from a specific factors and treatment mechanisms perspective, meditation likely contains several distinct therapeutic elements, and likewise there are different types of meditations involved in MBP that differentially draw upon these elements. For example, some meditations emphasize attentional focus and awareness (e.g., breath meditation), while others cultivate attitudinal qualities (e.g., loving-kindness meditation, mountain meditation). Therefore, knowing that meditation is an active component of treatment is pragmatically useful information, but unanswered questions remain about how meditation training functions as an active ingredient.
Limitations of the Current Literature
Among existing component studies of MBPs, several have methodological limitations that suggest risk of bias including small sample sizes that statistically underpowered and a lack of blinding or protocol adherence measures. Furthermore, an issue that is applicable to these studies, as well as to the broader field of mindfulness research, is the lack of consensus about the definition of mindfulness, its bounds, and most relevant for this systematic review, how it is assessed (Van Dam et al., 2018). In order to evaluate the precise effect from the active components of an MBP, it is critical to have valid and reliable measures. Serious concerns have been raised about the validity of self-report measures of mindfulness in particular because their factor structures and item functioning have been shown to be different between populations, e.g., high trait mindfulness individuals versus low trait mindfulness individuals with the Five Factor Mindfulness Questionnaire (FFMQ) (Pelham et al., 2019), between time points with the FFMQ (Gu et al., 2016), or between studies with a higher order mindfulness latent factor (Hsiao et al., 2019), suggesting overall lack of construct validity. Furthermore, there are critical concerns about lack of discriminant validity (Baer et al., 2019; Goldberg et al., 2016), the potential effect of demand characteristics on responding (e.g., social desirability of responding to items in a certain way after receiving meditation training), and even the effects of increased mindful introspection on responding (e.g., participants who were relatively unaware of their own mind- wandering before MBP develop greater awareness of mind-wandering after MBP, thereby potentially reporting lower mindfulness after intensive mindfulness training) (Van Dam et al., 2018). Given the well document ambiguity around measuring mindfulness as a construct (Baer, 2011), studies that primarily rely on self-report measures of mindfulness as their outcome remain difficult to interpret.
However, there are some more accurate (or less bias-prone) strategies for measuring the impact of MBPs on mindfulness outcomes as well as other relevant psychological outcome variables that suffer from the same concerns with measurement validity and reliability. Studies that take a multimodal approach and incorporate cognitive, behavioral, biological, social, or emotional assessments are likely better able to characterize the functional changes that are related to mindfulness training. For example, Lindsay et al. compared the impact of their MBP on stress reactivity using both cardiovascular and self-report measures of stress (Lindsay, Young, et al., 2018). By including multimodal outcome measures, they found that the acceptance component of their MBP reduced cardiovascular but not self-reported stress. These findings prompt questions how MBPs may impact the measurement of psychological constructs. While it is possible that the acceptance component was inert when it came to self-reported stress, it may also be the case that MBPs impact the validity and reliability of self-report measures of psychological constructs. For example, A question that asks, “On a scale of 1–10, how much stress do you feel?” does not capture acceptance or reactivity to the feeling of stress. There may be measurement error due to confounding of the intensity of experience with reactivity to experience.
Since many theories of mindfulness suggest that nonreactivity to experience is a primary mechanism of action and this systematic review shows evidence for acceptance/nonreactivity as an active component of MBPs, more scientifically rigorous measurements of these psychological constructs and processes are needed.
Recommendations and Future Directions
Existing component studies of MBPs shed light on potential active ingredients of this type of treatment, and yet several gaps in the literature remain. MBP research is at a critical point in its development where there is a growing evidence base supporting its efficacy for improving a broad range of health and mental health outcomes, and several elegant theoretical models have been proposed. However, greater integration between theoretical models, mechanistic models, testing of active ingredients, and measuring client mechanisms of behavior change is needed to fully understand how MBPs work. Currently, few component studies demonstrate that a hypothesized active component of treatment actually engages purported mechanisms of behavior change to affect outcomes. Future studies should use study designs that account for the temporal relationships between treatment components, mechanisms of change, and functional outcomes. As MBPs are increasingly being adapted as digital programs (Mikolasek et al., 2018) and brief programs (Schumer et al., 2018), it will be important to include streamlined and validated active components.
Finally, this body of literature would benefit from more research on MBP treatment components among a wider array of diverse populations and clinical psychological conditions. Although psychological conditions were targeted in all of the studies in this review, only a minority of them included clinical samples. Among those studies that recruited clinical samples, a large proportion of participants were women and, when race/ethnicity was reported, predominantly white with either depression or trauma. Given that there is compelling evidence for the efficacy of MBPs for other clinical groups (Creswell, 2017), including those with substance use disorders (Bowen et al., 2014), anxiety disorders (Hofmann & Gomez, 2017), and chronic pain (Hilton, Hempel, et al., 2017), further research is warranted to determine if treatment is effective through similar or unique components in these populations. In addition, specific attention must be paid to validating the active components of MBPs among individuals from diverse populations and considering different aspects of diversity (e.g., race, ethnicity, gender, socioeconomic status, age, ability/disability, etc.). There is some evidence for MBPs being particularly effective for certain groups such as racial/ethnic minority women (Witkiewitz et al., 2013) and gender diverse groups (Roos et al., 2019). Additionally, mindfulness may buffer the effects of discrimination stress on depression (Shallcross & Spruill, 2018). However, additional work must be done to examine active mechanisms of treatment with diverse samples who have been underrepresented in MBP research to date. It is critical to validate active components and mechanisms of treatment for groups who have historically have faced significant disparities in mental health care access, as well as high levels of stress (e.g., neighborhood disadvantage, discrimination).
Component studies of MBPs, including dismantling, additive, and direct component comparisons, have the ability to provide evidence for which elements of treatment drive outcomes. Elucidating the active ingredients of treatment is consistent with the tenet of clinical science that only scientifically validated treatments should be delivered. In this systematic review of component studies testing the active ingredients of mindfulness-based programs for psychological conditions, we identified eight studies that tested components of MBSR, MBCT, Unified Mindfulness, and core MBP processes. Going forward, more precisely operationalized MBP components should be tested and identified active components should be more thoroughly integrated in mechanistic models to explain how MBPs drive positive psychological outcomes.
Acknowledgments:
We would like to thank Drs. Theresa Moyers and Kevin Vowels for their feedback on this manuscript.
Funding:
Elena Stein was supported by a training grant through the National Institute on Alcohol Abuse and Alcoholism, T32 AA018108-10. Dr. Witkiewitz was supported by R01 AA025539.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Ahn HN, & Wampold BE (2001). Where oh where are the specific ingredients? A meta- analysis of component studies in counseling and psychotherapy. Journal of Counseling Psychology, 48(3), 251–257. 10.1037/0022-0167.48.3.251 [DOI] [Google Scholar]
- Baer RA. (2011). Measuring mindfulness. Contemporary Buddhism, 12(1), 241–261. 10.1080/14639947.2011.564842 [DOI] [Google Scholar]
- Baer R, Gu J, Cavanagh K, & Strauss C (2019). Differential sensitivity of mindfulness questionnaires to change with treatment: A systematic review and meta-analysis. Psychological Assessment, 31(10), 1247–1263. 10.1037/pas0000744.supp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell EC, Marcus DK, & Goodlad JK (2013). Are the parts as good as the whole? A meta- analysis of component treatment studies. Journal of Consulting and Clinical Psychology, 81(4), 722–736. 10.1037/a0033004 [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, & Carroll HA (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry, 71(5), 547–556. 10.1001/jamapsychiatry.2013.4546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Chawla N, Simpson TL, Ostafin BD, Larimer ME, Blume AW, Parks GA, & Marlatt GA (2006). Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors, 20, 343–347. 10.1037/0893-164X.20.3.343 [DOI] [PubMed] [Google Scholar]
- Britton WB, Davis JH, Loucks EB, Peterson B, Cullen BH, Reuter L, Rando A,Rahrig H, Lipsky J, & Lindahl JR (2018). Dismantling mindfulness-based cognitive therapy: Creation and validation of 8-week focused attention and open monitoring interventions within a 3-armed randomized controlled trial. Behaviour Research and Therapy, 101, 92–107. 10.1016/j.brat.2017.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi X., Bo A., Liu T., Zhan P., & Chi I. (2018). Effects of mindfulness-based stress reduction on depression in adolescents and young adults: A systematic review and meta-analysis. In Frontiers in Psychology (Vol. 9, pp. 1–11). 10.3389/fpsyg.2018.01034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiesa A, Castagner V, Andrisano C, Serretti A, Mandelli L, Porcelli S, & Giommi F (2015). Mindfulness-based cognitive therapy vs Psycho-education for patients with major depression who did not achieve remission following antidepressant treatment. Psychiatry Research, 226(2–3), 474–483. 10.1016/j.psychres.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Chin B, Lindsay EK, Greco CM, Brown KW, Smyth JM, Aidan GC, & Creswell JD (2019). Psychological mechanisms driving stress resilience in mindfulness training: A randomized controlled trial. Health Psychology, 38(8), 759–768. 10.1037/hea0000763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin B, Lindsay EK, Greco CM, Brown KW, Smyth JM, Wright AGC, & Creswell JD (2019). Psychological mechanisms driving stress resilience in mindfulness training: A randomized controlled trial. Health Psychology, 38(8), 759–768. 10.1037/hea0000763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JD (2017). Mindfulness Interventions. Annual Review of Psychology, 68(1), 491–516. 10.1146/annurev-psych-042716-051139 [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Cristea IA, Karyotaki E, Reijnders M, & Steven D (2019). Component studies of psychological treatments of adult depression: A systematic review and meta-analysis. Psychotherapy Research, 29(1), 15–29. 10.1080/10503307.2017.1395922 [DOI] [PubMed] [Google Scholar]
- Cuijpers P., Reijnders M., & Huibers MJH. (2019). The role of common factors in psychotherapy outcomes. Annu Rev Clin Psychol, 15, 207–231. 10.1146/annurev-clinpsy-050718-095424 [DOI] [PubMed] [Google Scholar]
- Dimidjian S, & Segal ZV (2015). Prospects for a clinical science of mindfulness-based intervention. American Psychologist, 70(7), 593–620. 10.1037/a0039589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Schwarz NR, Kelly A, Whitt A, & Howard MO (2012). Mindfulness- oriented recovery enhancement for alcohol dependence: Therapeutic mechanisms and intervention acceptability. Journal of Social Work Practice in the Addictions, 12(3), 242–263. 10.1080/1533256X.2012.702638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Wielgosz J, Dahl C, Schuyler B, Maccoon DS, Rosenkranz M, Lutz A, Sebranek CA, & Davidson RJ (2016). Does the five facet mindfulness questionnaire measure what we think it does? Construct validity evidence from an active controlled randomized clinical trial. Psychological Assessment, 28(8), 1009–1014. 10.1037/pas0000233.supp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant S, Colaiaco B, Motala A, Shanman R, Booth M, Sorbero M, & Hempel S (2017). Mindfulness-based relapse prevention for substance use disorders: A systematic review and meta-analysis. J Affict Med, 11(5), 386–396. 10.1097/ADM.0000000000000338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield BL., Roos CR., Hagler KJ., Stein ER., Bowen S., & Witkiewitz KA. (2018). Race/ethnicity and racial group composition moderate the effectiveness of mindfulness-based relapse prevention for substance use disorder. Addictive Behaviors, 81(February 2018), 96–103. 10.1016/j.addbeh.2018.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J, Strauss C, Bond R, & Cavanagh K (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. 10.1016/j.cpr.2015.01.006 [DOI] [PubMed] [Google Scholar]
- Gu J, Strauss C, Crane C, Barnhofer T, Karl A, Cavanagh K, & Kuyken W (2016). Examining the factor structure of the 39-item and 15-item versions of the five facet mndfulness questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychological Assessment, 28(7), 791–802. 10.1037/pas0000263.supp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren KA, & Witkiewitz K (2013). Missing data in alcohol clinical trials: A comparison of methods. Alcoholism: Clinical and Experimental Research, 37(12), 2152–2160. 10.1111/acer.12205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JD, Quatman CE, Manring MM, Siston RA, & Flanigan DC (2014). How to write a systematic review. In American Journal of Sports Medicine (Vol. 42, Issue 11, pp. 2761–2768). 10.1177/0363546513497567 [DOI] [PubMed] [Google Scholar]
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, & Maglione MA (2017). Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine, 51(2), 199–213. 10.1007/s12160-016-9844-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilton L., Maher AR., Colaiaco B., Apaydin E., Sorbero ME., Booth M., Shanman RM., & Hempel S. (2017). Meditation for posttraumatic stress: systematic review and meta- analysis. Psychological Trauma: Theory, Research, Practice, and Policy, 9(4), 453–460. 10.1037/tra0000180 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, & Gomez AF (2017). Mindfulness-based interventions for anxiety and depression. Psychiatric Clinics of North America, 40(4), 739–749. 10.1016/j.psc.2017.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao YY, Tofighi D, Kruger ES, Lee Van Horn M, MacKinnon DP, & Witkiewitz K (2019). The (lack of) replication of self-reported mindfulness as a mechanism of change in mindfulness-based relapse prevention for substance use disorders. Mindfulness, 10(4), 724–736. 10.1007/s12671-018-1023-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. Delacorte Press. [Google Scholar]
- Khoo EL, Small R, Cheng W, Hatchard T, Glynn B, Rice DB, Skidmore B, Kenny S, Hutton B, & Poulin PA (2019). Comparative evaluation of group-based mindfulness- based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: A systematic review and network meta-analysis. Evidence-Based Mental Health, 22(1), 26–35. 10.1136/ebmental-2018-300062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert MJ, & Bergin AE (1994). The effectiveness of psychotherapy. In Bergin AE & Garfield SL (Eds.), Handbook of psychotherapy and behavior change (pp. 143–189). John Wiley & Sons. [Google Scholar]
- Lindsay EK., Chin B., Greco CM., Young S., Brown KW., Wright AGC., Smyth JM., Burkett D., & Creswell JD. (2018). How mindfulness training promotes positive emotions: Dismantling acceptance skills training in two randomized controlled trials. Journal of Personality and Social Psychology, 115(6), 944–973. 10.1037/pspa0000134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2017). Mechanisms of mindfulness training: Monitor and Acceptance Theory (MAT). Clinical Psychology Review, 51, 48–59. 10.1016/j.cpr.2016.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, & Creswell JD (2018). Mindfulness, acceptance, and emotion regulation: perspectives from Monitor and Acceptance Theory (MAT). Current Opinion in Psychology, 28(January), 120–125. 10.1016/j.copsyc.2018.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, Young S, Brown KW, Smyth JM, & Creswell JD (2019). Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. PNAS Proceedings of the National Academy of Sciences of the United States of America, 116(9), 3488–3493. 10.1073/pnas.1813588116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay EK, Young S, Smyth JM, Warren K, Creswell JD, Brown KW, & Creswell JD (2018). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology, 87(May 2017), 63–73. 10.1016/j.psyneuen.2017.09.015 [DOI] [PubMed] [Google Scholar]
- Lutz A, Jha AP, Dunne JD, & Saron CD (2015). Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. American Psychologist, 70(7), 632–658. 10.1037/a0039585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M., Kiluk BD., McCrady BS., Tonigan JS., & Longabaugh R. (2015). Active ingredients of treatment and client mechanisms of change in behavioral treatments for alcohol use disorders: Progress 10 years later. Alcoholism: Clinical & Experimental Research, 39(10), 1852–1862. 10.1111/acer.12848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFall RM (2000). Elaborate reflections on a simple manifesto. Applied & Preventive Psychology, 9, 5–21. 10.1016/S0962-1849(05)80035-6 [DOI] [Google Scholar]
- Mikolasek M, Berg J, Witt CM, & Barth J (2018). Effectiveness of mindfulness- and relaxation-based eHealth interventions for patients with medical conditions: a systematic review and synthesis. International Journal of Behavioral Medicine, 25(1), 1–16. 10.1007/s12529-017-9679-7 [DOI] [PubMed] [Google Scholar]
- Miller WR, & Moyers TB (2017). Motivational interviewing and the clinical science of Carl Rogers. Journal of Consulting and Clinical Psychology, 85(8), 757–766. 10.1037/ccp0000179 [DOI] [PubMed] [Google Scholar]
- Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, & Altman DG (2010). CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ 10.1136/bmj.c869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman DG., Altman D., Antes G., Atkins D., Barbour V., Barrowman N., Berlin JA., Clark J., Clarke M., Cook D., D’Amico R., Deeks JJ., Devereaux PJ., Dickersin K., Egger M., Ernst E., … Tugwell P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. In BMJ (Vol. 6, Issue 7). 10.1371/journal.pmed.1000097 [DOI] [Google Scholar]
- Mulder R, Murray G, & Rucklidge J (2017). Common versus specific factors in psychotherapy: opening the black box. In The Lancet Psychiatry (Vol. 4, Issue 12, pp. 953–962). Elsevier Ltd. 10.1016/S2215-0366(17)30100-1 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gonzalez O, Metcalf SA, Whicker CL, Scherer EA, Witkiewitz K, Marsch LA, & Mackinnon DP (2019). Item response theory analysis of the five facet mindfulness questionnaire and its short forms. Mindfulness, 10(8), 1615–1628. 10.1007/s12671-019-01105-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piet J, & Hougaard E (2011). The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: A systematic review and meta- analysis. In Clinical Psychology Review (Vol. 31, Issue 6, pp. 1032–1040). Elsevier Ltd. 10.1016/j.cpr.2011.05.002 [DOI] [PubMed] [Google Scholar]
- Rogers CR (1957). The necessary and sufficient conditions of therapeutic personality change. Journal of Consulting Psychology, 21(2). 10.1037/h0045357 [DOI] [PubMed] [Google Scholar]
- Roos CR, Bowen S, & Witkiewitz K (2017). Baseline patterns of substance use disorder severity and negative affect moderate the efficacy ofmindfulness-based relapse prevention. Alcoholism: Clinical and Experimental Research, 85(11), 1041–1051. 10.1111/acer.13392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos CR., Stein ER., Bowen S., & Witkiewitz K. (2019). Individual gender and group gender composition as predictors of differential benefit from mindfulness-based relapse prevention for substance use disorders. Mindfulness. 10.1007/s12671-019-01112-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumer MC, Lindsay EK, & David Creswell J (2018). Brief mindfulness training for negative affectivity: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 86(7), 569–583. 10.1037/ccp0000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shallcross AJ, & Spruill TM (2018). The protective role of mindfulness in the relationship between perceived discrimination and depression. Mindfulness, 9(4), 1100–1109. 10.1007/s12671-017-0845-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, & Lau MA (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68(4), 615–623. 10.1037//0022-006X.68.4.615 [DOI] [PubMed] [Google Scholar]
- Valdez CE, Sherrill AM, & Lilly M (2016). Present moment contact and nonjudgment: Pilot data on dismantling mindful awareness in trauma-related symptomatology. Journal of Psychopathology and Behavioral Assessment, 38(4), 572–581. 10.1007/s10862-016-9548-8 [DOI] [Google Scholar]
- Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, Meissner T, Lazar SW, Kerr CE, Gorchov J, Fox KCR, Field BA, Britton WB, Brefczynski-Lewis JA, & Meyer DE (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG., Crane C., Barnhofer T., Brennan K., Duggan DS., Fennell MJV, Hackman A., Krusche A., Muse K., Von Rohr IR., Shah D., Crane RS., Eames C., Jones M., Radford S., Silverton S., Sun Y., Weatherley-Jones E., Whitaker CJ., … Russell IT. (2014). Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology, 82(2), 275–286. 10.1037/a0035036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Greenfield BL, & Bowen S (2013). Mindfulness-based relapse prevention with racial and ethnic minority women. Addictive Behaviors, 38(12), 2821–2824. 10.1016/j.addbeh.2013.08.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young S (2016). What is mindfulness? A contemplative perspective. In Schonert-Reichl KA& Roeser RW (Eds.), Handbook of Mindfulness in Education (pp. 29–45). Springer. [Google Scholar]