Abstract
Background:
Discrimination is experienced across demographic attributes (e.g., race and gender) and vantage points (e.g., personal and vicarious), yet few studies have classified these different experiences of discrimination within healthcare systems. Moreover, which discriminatory experiences have greater influence on patient-reported quality outcomes remains poorly understood. To address these gaps, we used latent class analysis (LCA) to identify typologies of past experiences with healthcare discrimination among adults with depression—who experience more frequent and stigmatizing healthcare interactions than the general population—and assess the relationship between class membership and current ratings of patient-reported quality outcomes.
Methods:
We surveyed a nationally representative sample of adults with depression (n = 803) to assess past experiences of discrimination by medical providers in terms of both the characteristics targeted for discrimination and whether healthcare discrimination was experienced personally or by friends and family members. We conducted an LCA to identify discrimination–exposure classes and a modified Poisson regression to identify associations between class membership and patient-reported quality outcomes (e.g., overall medical provider quality, respect, clear communication, and careful listening), while adjusting for covariates.
Results:
We identified four latent classes of healthcare discrimination: low discrimination (LD; referent class: 72.2% of total sample), vicarious linguistic discrimination (VL; 13.9%), elevated personal and vicarious racial discrimination (EPVR; 10.5%), and high racial/ethnic discrimination (HRE; 3.4%). Compared to those in the LD class, individuals in the EPVR class had higher rates of reporting their current medical provider’s respect and careful listening skills as sometimes or never, (Respect aIRR: 1.90, 95% CI: 1.05–3.42; Listening aIRR: 2.18, 95% CI: 1.29–3.66). Those in the HRE class reported higher rates of reporting their medical provider’s quality and communication as poor or fair and lower ratings of careful listening (Quality aIRR: 2.06, 95% CI: 1.08–3.93; Communication aIRR: 1.97, 95% CI: 1.00–3.63; Listening aIRR: 2.41, 95% CI: 1.27–4.59), compared to those in the LD class. Those in the VL class had higher rates of reporting that their medical provider never or sometimes respected or carefully listened to them (Respect aIRR: 2.12, 95% CI: 1.20–3.72; Listening aIRR:1.67, 95% CI:1.03–2.71) than those in, the LD class.
Conclusions:
Healthcare organizations committed to providing equitable patient care should establish more robust quality improvement approaches to prevent discrimination at the medical provider level as well as structures of accountability to reconcile previously embedded social inequities within the healthcare system.
Keywords: Healthcare discrimination, Patient-reported outcomes, Medical providers, Latent class analysis, Intersectionality, Depression
1. Background
Experiencing discrimination, defined as unfair treatment on the basis of socially-determined characteristics, is associated with adverse physical and mental health outcomes, including higher levels of allostatic load, hypertension, and psychological distress (Williams et al., 2019). Discrimination in the United States healthcare system is a function of both implicit attitudes (e.g., racialized perceptions of depression) and explicit behaviors (e.g., reduced diagnosis of depression) (Hall et al., 2015; Merino et al., 2018; Sonik et al., 2020; Trivedi and Ayanian, 2006). However, little is known about how this experience occurs among individuals with depression, who experience significantly more frequent and stigmatizing healthcare interactions than the general population (Bock et al., 2014; Robinson et al., 2016). Additionally, how the discrimination–mental health relationship operates in the healthcare system across multiple demographic characteristics such as race, gender, and sexual orientation is not fully understood (Alasmawi et al., 2020; Evans-Lacko et al., 2015; LeBrón et al., 2019; Williams et al., 2007). Thus, a critical next step in advancing discrimination research is understanding the potential relationships between experiences with past healthcare discrimination and patient-reported outcomes for individuals with depression.
In the United States, depression is one of the most commonly experienced and disabling mental health disorders, with 10.4% and 20.6% of adults experiencing depression in a 12-month period and lifetime, respectively (Hasin et al., 2018). Depression co-morbidities are also common, with those with clinical depression also meeting diagnostic criteria for at least one additional mental health or chronic physical disorder, such as anxiety, diabetes, or cancer (Al-Asadi et al., 2015; Krishnan et al., 2002; Read et al., 2017). As a result of the frequent co-morbidities associated with depression, depression is associated with healthcare utilization—those with higher depressive symptoms or a depression diagnosis are more likely to have greater healthcare utilization across emergency, general, and specialty settings (Egede et al., 2016; Koenig et al., 1989; Mausbach and Irwin, 2017; Robinson et al., 2016).(Egede et al., 2016; Koenig et al., 1989; Mausbach and Irwin, 2017; Robinson et al., 2016). As a result, individuals with depression navigate complex healthcare systems more frequently than patients without depression. Because they are frequently exposed to the healthcare system, individuals with depression may also be increasingly exposed to discrimination in the healthcare setting due to stigma surrounding their diagnosis or biases related to other socially determined patient characteristics.
Mental health service disparities research has generally analyzed the extent to which poor mental health status and treatment outcomes among socially marginalized groups are explained by health services indicators such as lack of access, limited insurance, or inability to seek or maintain care (Cook et al., 2017; Creedon and Cook, 2016; McGuire et al., 2006; Safran et al., 2009). However, few studies have explored the role of prior healthcare discrimination in current ratings of healthcare quality and medical provider attributes that are essential to delivery of quality care. Indeed, discrimination in the healthcare system influences subsequent healthcare-seeking behaviors (Progovac et al., 2020; Schwei et al., 2017) and results in avoidance of the healthcare system altogether. For individuals with depressive symptoms, who are also more likely to experience chronic physical diseases (e.g., heart disease and cancer) (Firth et al., 2019), avoiding the healthcare system may be detrimental to both their mental and physical wellbeing and thus have particularly high negative health consequences.
When assessing healthcare discrimination, researchers also must reconcile how structural inequalities at the macro-level (e.g., poverty, racism, and sexism) manifest for those with historically marginalized identities. In particular, the joint influence of micro-level individual characteristics, such as gender, sexual orientation, or a combination of the two, influence the healthcare experience and shape subsequent perceptions of medical provider care (Seaton et al., 2010; Wilson et al., 2019).
Black feminist scholars developed and advanced intersectionality theory as an integral framework to understand health disparities—rather than assuming one aspect of identity singularly impacts outcomes (e.g., social identity or minority stress frameworks), intersectionality suggests that social identities (e.g., race, gender, and class) are mutually constitutive and operate in concert with one another across systems of oppression (Bowleg, 2012; Crenshaw, 1991). In the healthcare context, intersectionality theory can help recognize how historically disparate power dynamics between the patient and medical provider (and the healthcare system itself) may manifest through reports of perceived discrimination. Moreover, intersectionality allows us to conceptualize beyond the presence of social attributes (e.g., gender and race categories) to examine how multiple social inequities (e.g., racism and sexism) may be observed in the healthcare system. For instance, when examined independently and intersectionally, both racism and sexism influence utilization of healthcare services in the United States (Bowleg, 2012; Clark et al., 1999; Dunlop et al., 2002; LaVeist et al., 2009; Williams, 2008). However, it remains unknown how multiple and interlocking systems of oppression, such as racism and sexism, interact within the healthcare system to yield disproportionate patient-reported experiences.
Theories of vicarious stress posit that discrimination influences health outcomes not only through direct exposure, but also indirectly through vicarious discrimination (i.e., unfair treatment) experienced by people within one’s social network, including family, friends, and romantic partners (Harrell, 2000). Vicarious exposure to discriminatory experiences can have broadly felt indirect impacts on mental well-being and interpersonal relationships (Bor et al., 2018; Tynes et al., 2008; Wofford et al., 2019). Studies using this framework affirm that Black Americans’ frequent vicarious exposure to racially salient traumatic or discriminatory experiences (e.g., police killings and online victimization) may adversely affect their mental health (Bor et al., 2018; Tynes et al., 2008). Looking at individuals experiencing discrimination and their partners, Wofford et al. (2019) found that discrimination exposure is associated with poor health status and high relationship strain among both members of these dyads (Wofford et al., 2019).
More research is needed to clarify the consequences of unfair treatment in healthcare settings with both direct and indirect exposure to discrimination. Additionally, although the effects of personal and vicarious discrimination on the mental well-being of Black Americans are well-documented (Arshanapally et al., 2017; Bor et al., 2018; Goodwill et al., 2019; Harrell, 2000; Lewis et al., 2015; Seaton et al., 2010; Williams et al., 1997; Williams and Mohammed, 2009), this relationship has not been fully explored across multiple and overlapping social identities, such as race, ethnicity, gender, sexual orientation, and language.
1.1. Latent class analysis as a quantitative method of exploring intersectional attributes of personally and vicariously experienced healthcare discrimination
Current methodological approaches to quantify discrimination from an intersectional lens are sparse. Madina Agénor (2020) asserts that this may be because limited analytic approaches account for interactions between multiple social identities and systems that perpetuate these inequities. Such techniques would need to incorporate multiple marginalized identities into analyses while acknowledging the realities of systemic oppression that are embedded within systems such as the healthcare sector.
Latent class analysis (LCA) is one approach to simultaneously test the joint influence of socially marginalized identities, discrimination, and health outcomes in the healthcare context. LCA captures heterogeneity within populations and yields distinct subgroups that share attributes across a common set of observed indicators (Lanza and Rhoades, 2013). Community-based studies integrating intersectionality theory with LCA have found that intersectional subgroups experiencing discrimination have more severe mental and physical health consequences than those experiencing discrimination for single-identity attributes (e.g., race only) (Garnett et al., 2014; Tynes et al., 2008). Given the potential effects of both personal and vicarious experiences on health (Bor et al., 2018; Wofford et al., 2019), identifying multiple intersectional attributes of discrimination through LCA may provide important insights to inform multi-level interventions at the individual, interpersonal, and system levels.
1.2. The present study
To address these gaps, the goals of the present study are to (i) identify latent classes related to personally and vicariously experienced healthcare discrimination among those with depression and (ii) assess associations between the resulting latent classes and self-reported quality of care outcomes. Based on previous studies and theoretical frameworks, we hypothesized that our LCA model would yield a multi-class solution to address these goals by expressing heterogeneity among respondents through subgroups of distinct sociodemographic characteristics and healthcare discrimination experiences (Hypothesis 1). Guided by research that suggests that marginalized racial/ethnic patients are more likely to perceive discriminatory treatment than their white counterparts and that discrimination may result in the receipt of poor quality of care (Bleich et al., 2019; Findling et al., 2019; Findling et al., 2019), we hypothesized that latent classes reporting high healthcare discrimination at the personal and vicarious levels would comprise a high proportion of Black and Hispanic respondents (Hypothesis 2) and be associated with poor patient-reported quality outcomes (Hypothesis 3).
2. Methods
2.1. Sample and data collection
Data for this study were from a nationally representative survey conducted in 2017 eliciting respondents’ prior experiences with discrimination in the healthcare system as well as the individual, familial, community, and sociocultural factors that influence patient preferences for healthcare. The survey was developed in coordination with community partners residing in the greater Boston area. The web-based survey was distributed using GfK Knowledge Panel, a validated internet-based survey system that uses probability sampling from residential addresses of U.S. households oversampled to include underrepresented groups and those without internet access. The survey was administered in English and Spanish and consisted of four modules focused on health status, demographics, healthcare preferences, and past experiences of discrimination in the healthcare system. Specific sampling procedures for identification and recruitment of the nationally representative sample are described elsewhere (Sonik et al., 2020).. We identified a sample of 803 adults with moderate to severe depression, determined by PHQ-9 scores ≥10 (Kroenke et al., 2001). This study was approved by the Institutional Review Board at Cambridge Health Alliance.
2.2. Measures
2.2.1. Healthcare discrimination
Healthcare discrimination was measured by adapting previously validated discrimination questions (Trivedi and Ayanian, 2006; Williams et al., 1997) to assess if the survey respondent was treated unfairly by a medical provider. Respondents were asked two questions regarding unfair treatment: (1) if they were ever treated unfairly while receiving medical care by a medical provider, and (2) if someone close to them was treated unfairly while receiving healthcare (described herein as vicarious discrimination). For each question, respondents could select one or more of the following five responses (race/color, ethnicity, language/accent, sexual orientation, and gender) to reflect which attributes were the perceived rationale for the discriminatory experience or indicate there was no discrimination.
2.2.2. Patient-reported medical provider quality outcomes
Respondents were asked how many times in the past 12 months they visited a medical provider to receive care for themselves. Those who reported one or more visits were subsequently asked to rate (poor, fair, good, or excellent) the medical provider and office on the following issues: (1) communication with medical provider, and (2) quality of care received. Respondents were also asked to report the frequency (never, sometimes, usually, or always) that the medical provider listened carefully and showed respect for what they had to say. For our study sample of respondents who reported a PHQ-9 score ≥10, “medical provider” referred to the doctor, nurse, or therapist with whom the respondent discussed feelings or symptoms of depression.
2.2.3. Covariates
Sociodemographic variables included as covariates in the regression analysis were age (continuous), race (non-Hispanic white, non-Hispanic Black, Hispanic), gender (male or female), education (less than high school, high school, some college, and college graduate/graduate degree), marital status, employment status, and frequency of past year healthcare utilization (continuous).
2.3. Statistical analysis
We conducted LCA to identify the joint influence of personal and vicarious discrimination attributes and to assess the associations of LCA membership to patient-reported quality outcomes among a sample of ethnically diverse adults with moderate to severe depression. Decisions about the final number of discrimination class profiles (e.g., latent class enumeration) were based on published model fit criteria (Collins and Lanza, 2009; Lanza and Rhoades, 2013; Nylund-Gibson and Choi, 2018) guiding theoretical frameworks related to vicarious discrimination and intersectionality (Bowleg, 2012; Crenshaw, 1991; Harrell, 2000; Wofford et al., 2019) and class interpretability (Nylund et al., 2007). Absolute model fit was determined by Akaike information criteria (AIC) and Bayesian information criteria (BIC). Additionally, we incorporated the sample-size-adjusted Bayesian information criterion (SABIC). Lower BIC, AIC, and SABIC values indicate adequate model fit (Nylund-Gibson and Choi, 2018). The Lo–Mendell–Rubin likelihood ratio test (LMR-LRT) was also used to assess relative model fit. A non-significant p-value (p > 0.05) on the LMR-LRT implies no difference in model fit between a model with k classes compared to a model with k−1 classes (Lo et al., 2001). Latent class enumeration was conducted in Mplus v.8 (Muthén and Muthén, 2019). Finally, we considered entropy, which is an estimate to distinguish between latent classes. Entropy values > 0.80 indicate acceptable separation of latent profiles.
Once model fit was determined, class membership data were exported to Stata v.15 for additional analysis (StataCorp, 2017). We conducted ANOVA and chi-square tests to determine sociodemographic characteristics of each latent class. We constructed binary outcome variables for patient-reported outcomes for provider quality and communication (e.g. poor-fair, good-excellent) and provider listening and respect (never--sometimes, usually-always) ratings. Finally, to assess associations between LCA membership and patient-reported quality outcomes, we conducted a modified Poisson regression, adjusting for sociodemographic covariates. Models 1 and 2 report how latent class membership is associated with the adjusted incidence rate ratio (aIRR) of rating medical provider quality and communication as “poor” or “fair” (relative to “excellent” or “good”), respectively. Models 3 and 4 repeat this analysis to report how latent class membership is associated with the incidence rates of responding that the medical provider was respectful and listened carefully either “never” or “sometimes” (relative to “always” or “usually”), respectively. All analyses used survey weights to adjust for sampling design and yield nationally representative estimates.
3. Results
3.1. Latent profile enumeration
LCA yielded a four-class solution that provided the most optimal fit for our data (Table 1). We selected the four-class final solution based on lower BIC and SABIC scores compared to k+1 latent classes and a significant LMR-LRT value (0.002), which implies distinction in relative model fit from the three-class model. Additionally, the four-class entropy value of 0.83demonstrated acceptable fit of our predefined criteria of >0.80. Finally, we selected the four-class solution to provide adequate class sizes for subsequent Poisson regression modeling.
Table 1.
Latent class enumeration and measures of absolute and relative fit of latent classes in study sample (n = 741).
| LLa | Entropy | BICb | AICc | LMR-LRTd (p value) | |
|---|---|---|---|---|---|
|
| |||||
| 1 Class | −1784.47 | N/A | 3635.01 | 3588.93 | N/A |
| 2 Class | −1549.42 | 0.81 | 3237.61 | 3140.84 | 0.00 |
| 3 Class | −1508.51 | 0.80 | 3228.48 | 3081.02 | 0.072 |
| 4 Class | −1471.17 | 0.83 | 3226.50 | 3028.36 | 0.00 |
| 5 Class | −1446.92 | 0.86 | 3250.68 | 3001.84 | 0.00 |
| 6 Class | −1429.64 | 0.89 | 3288.79 | 2989.27 | 0.03 |
Bolded values indicate the selected latent class.
Log-likelihood.
Bayesian Information Criteria.
Akaike’s Information Criteria (AIC).
Lo-Mendell-Rubin likelihood ratio test (LMR-LRT).
3.2. Descriptive statistics
Our study presents results from 741 adults ≥18 years old in the full sample (92.2%), among whom completed data for all study variables and were included in our latent class analysis. Weighted summary statistics of the full sample are presented in Table 2. On average, respondents were 43.2 years old (SD: 15.8), predominantly identify as female (65.7%), and employed (58.0%). About half (49.4%) of our respondents were married and had some college (37.9%) or completed a bachelor’s or graduate degree (25.4%). There was fairly even distribution of racial and ethnic background in our study sample, with 34.7% non-Hispanic White, followed by 30.6% non-Hispanic Black, and 34.6% Hispanic. eTables 1 and 2 displays detailed information regarding descriptive statistics, including unweighted summary statistics and reporting on our study variables of interest (e.g. personal and vicarious healthcare discrimination indicators and patient-reported outcomes). More than half of the respondents in this sample reported visiting their medical provider in the past year, with the 15.5% of the sample (n = 122) reporting a single visit, followed by 38.8% (n = 305) reporting 2–5 visits, 12.5% (n = 98) with 6–9 visits, and 13.6% (n = 107) with 10 or more visits to a medical provider. 19.7% (n = 155) of respondents reported not visiting their medical provider in the past year. Racial discrimination was the highest reported personal and vicarious healthcare discrimination indicator (10.2% and 15.5%, respectively). Patient-reported outcomes were generally skewed positive, with the majority of the sample responding to frequency (e.g. provider respect and listening carefully) and rating (e.g. provider quality and communication) outcome questions as “always” or “excellent”, respectively.
Table 2.
Description of latent class membership (n = 741, weighted).
| Full sample | High racial/ethnic discrimination |
Vicarious linguistic discrimination |
Low discrimination |
Elevated personal and vicarious racial discrimination |
|
|---|---|---|---|---|---|
| (HRE n = 25, 3.37%) | (VL n = 103, 13.9%) | (LD n = 535, 72.2%) | (EPVR n = 78, 10.5%) | ||
|
| |||||
| Age, M (SD) # @ | 43.2 (15.8) | 38.3 (13.8) | 35.3 (11.4) | 42.3 (17.0) | 41.9 (13.4) |
| Gender, % Male * ^ % | 34.3 | 13.2 | 44.0 | 40.8 | 45.2 |
| Racial category, % ^#&@ | |||||
| Non-Hispanic White | 34.7 | 24.9 | 25.7 | 73.7 | 42.3 |
| Non-Hispanic Black | 30.6 | 36.5 | 18.1 | 9.15 | 45.5 |
| Hispanic | 34.6 | 38.6 | 56.3 | 17.2 | 12.2 |
| Married, % yes | 49.4 | 45.4 | 51.5 | 44.3 | 53.7 |
| Education, % *%#& | |||||
| Less than high school | 13.8 | 12.3 | 35.3 | 15.1 | 28.8 |
| High school | 22.9 | 23.0 | 24.6 | 34.7 | 14.4 |
| Some college | 37.9 | 26.8 | 29.3 | 31.0 | 49.3 |
| Bachelors or Graduate degree | 25.4 | 38.0 | 10.9 | 19.3 | 7.63 |
| Employed (full or part-times), % yes %@ | 58.0 | 76.4 | 62.3 | 54.9 | 41.3 |
Note: Values are presented as column percentages (e.g. within class).
significant at p < 0.05 between High racial/ethnic discrimination and Moderate Intersectional classes.
significant at p < 0.05 between High racial/ethnic discrimination and Low Discrimination classes.
significant at p < 0.05 between High racial/ethnic discrimination and Elevated personal and vicarious racial discrimination classes.
significant at p < 0.05 between Moderate Intersectional and Low Discrimination classes.
significant at p < 0.05 between Moderate Intersectional and Elevated personal and vicarious racial discrimination classes.
significant at p < 0.05 between Low Discrimination and Elevated personal and vicarious racial discrimination classes.
3.3. Description of latent classes
Figure 1 illustrates the conditional item probability profiles of the final four-class solution. Observed conditional item-class probabilities are listed in eTable 3. The largest class (72.2% of total sample) represented low discrimination (LD) and comprised respondents who had low item-class probabilities of reporting personal or vicarious discrimination across all identity attributes. The second largest class (13.9%) described vicarious linguistic (VL) discrimination and comprised respondents with low item-class probabilities on personally observed and vicarious discrimination across race and ethnicity, and LGBTQ attributes and moderate probabilities of endorsing vicarious language discrimination. The third largest class (10.5%) was characterized as elevated personal and vicarious racial (EPVR) discrimination and comprised respondents with personally observed discrimination and relatively higher item-class probabilities of reporting vicarious discrimination on racial attributes. Finally, the smallest class (3.4%) was characterized as high racial and ethnic discrimination (HRE) and comprised respondents with higher item-class probabilities of personally and vicariously experienced discrimination on race and ethnicity attributes.
Fig. 1.
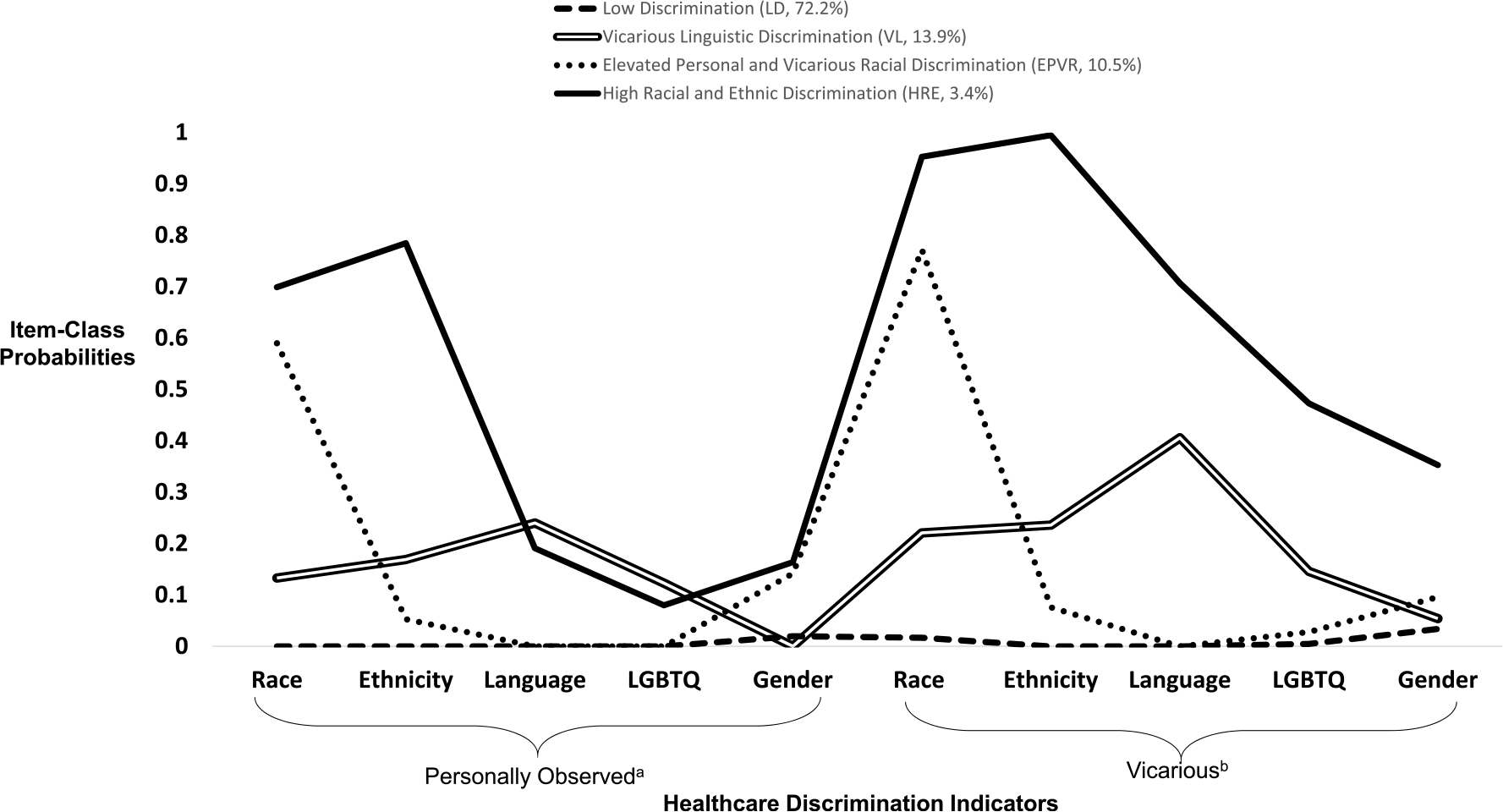
Conditional item probability profile for the four-class model of personal and vicarious discrimination (n = 741)
a Personally observed = Have you ever felt that YOU were treated unfairly by a doctor based on [attribute]
bVicarious = Have you ever felt that SOMEONE CLOSE TO YOU was treated unfairly by a doctor based on [attribute].
3.4. Descriptors of latent class membership
Table 2 illustrates the distribution of sociodemographic characteristics and mental health outcomes across each of the four distinct latent classes and the total sample. Individuals in the VL class reflected the youngest average age (mean: 35.3 years, SD:11.4) and were significantly younger than individuals in the LD and EPVR classes. Individuals in the HRE class reported a significantly lower proportion of male respondents (13.2%) than the remaining three latent class groups. The racial composition within latent classes varied widely, with significantly higher proportion of white respondents in the LD class (73.7%) than other latent classes. Additionally, the highest proportion of non-Hispanic Black respondents (45.5%) was in the EPVR class, which was significantly higher compared to those in the LD and VL classes. Finally, the VL class included the highest proportion of Hispanic respondents (51.5%) among the four classes. Education status among classes also varied, with those in the VL class reporting the highest proportion of respondents with less than a high school education (35.3%), and those in the HRE class reporting the highest proportion of college or graduate degree holders (38.0%). The proportion of married respondents did not differ significantly across classes.
3.5. Associations among latent classes and medical provider characteristics
Finally, using modified Poisson regression, we assessed whether latent class membership was significantly associated with patient-reported quality outcomes, after adjusting for covariates. Table 3 illustrates results of the adjusted Poisson regression models, illustrated as incidence rate ratios, by quality outcome (Model 1: Overall provider quality; Model 2: Provider communication; Model 3: Provider respect; Model 4: Provider listened carefully). In Model 1 (provider quality), those in the HRE class reported higher rates of reporting their medical provider’s quality as poor or fair (aIRR: 2.06, 95% CI: 1.08–3.93). In Model 2 (communication), individuals in the HRE class had higher rates of reporting their current medical provider’s careful listening skills as sometimes or never (aIRR: 1.97, 95% CI: 1.00–3.63). In Model 3 (respect), those in the VL and EPVR class had higher rates of reporting that their medical provider sometimes or never respected them (VL: aIRR: 2.12, 95% CI: 1.20–3.72; EPVR aIRR: 1.90, 95% CI: 1.05–3.42). Finally, in Model 4 (carefully listening), those in the HRE, VL, and EPVR class all reported higher rates of reporting their medical provider sometimes or never listened carefully (HRE aIRR: 2.41, 95% CI: 1.27–4.59; VL aIRR: 1.67, 95% CI: 1.03–2.71; EPVR aIRR: 2.18 95% CI: 1.29–3.66).
Table 3.
Adjusted modified Poisson regression models of latent class correlates of provider characteristic ratings, weighted.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|
|---|---|---|---|---|
| Overall quality |
Communication |
Respect |
Listened carefully |
|
| aIRR (95% CI) | aIRR (95% CI) | aIRR (95% CI) | aIRR (95% CI) | |
|
| ||||
| Class membership | ||||
| Low Discrimination | REF | REF | REF | REF |
| High Racial and Ethnic Discrimination | 2.06 (1.08–3.93) | 1.97 (1.0–3.63) | 2.16 (0.78–5.94) | 2.41 (1.27–4.59) |
| Vicarious Linguistic Discrimination | 0.85 (0.42–1.71) | 1.15 (0.64–2.05) | 2.12 (1.20–3.72) | 1.67 (1.03–2.71) |
| Elevated Personal and Vicarious Racial Discrimination | 1.59 (0.94–2.70) | 1.53 (0.91–2.60) | 1.90 (1.05–3.42) | 2.18 (1.29–3.66) |
| Covariates | ||||
| Race/Ethnicity | ||||
| White, non-Hispanic | REF | REF | REF | REF |
| Black, non-Hispanic | 1.15 (0.69–1.94) | 1.07 (0.66–1.72) | 1.11 (0.64–1.92) | 1.01 (0.63–1.64) |
| Hispanic | 1.13 (0.70–1.83) | 0.96 (0.61–1.49) | 0.77 (0.43–1.38) | 0.87 (0.56–1.35) |
| Age | 0.99 (0.98–1.01) | 0.99 (0.98–1.00) | 0.99 (0.97–1.01) | 0.99 (0.98–1.00) |
| Gender | ||||
| Male | REF | REF | REF | REF |
| Female | 0.82 (0.54–1.25) | 0.79 (0.54–1.16) | 0.70 (0.44–1.10) | 0.88 (0.59–1.28) |
| Marital status | ||||
| Not married | REF | REF | REF | REF |
| Married | 1.22 (0.81–1.84) | 1.22 (0.84–1.78) | 1.34 (0.82–2.18) | 1.26 (0.87–1.81) |
| Education status | ||||
| Less than high school | REF | REF | REF | REF |
| High School | 0.74 (0.42–1.30) | 0.89 (0.52–1.52) | 0.93 (0.48–1.80) | 0.86 (0.52–1.44) |
| Some College | 0.72 (0.42–1.25) | 0.74 (0.44–1.24) | 0.56 (0.29–1.07) | 0.68 (0.43–1.08) |
| Bachelor’s degree or higher | 0.46 (0.21–0.98) | 0.64 (0.33–1.24) | 0.37 (0.15–0.89) | 0.44 (0.22–0.88) |
| Employment status | ||||
| Not working/unemployed | REF | REF | REF | REF |
| Employed | 0.66 (0.44–1.00) | 0.70 (0.48–1.03) | 0.86 (0.53–1.40) | 0.75 (0.52–1.08) |
| Past year service frequency | 0.78 (0.63–0.96) | 0.79 (0.66–0.95) | 0.96 (0.79–1.16) | 0.79 (0.68–0.92) |
aIRR = adjusted Incidence Rate Ratio, CI= Confidence Interval, ref = reference group, Bold parameters are significant at p < 0.05.
Model 1: Provider quality (compared to “excellent-good” rating); Model 2: Provider communication (compared to “excellent-good” rating); Model 3: Provider respect (compared to “always-usually” frequency); Model 4: Provider listened carefully (compared to “always-usually” frequency).
4. Discussion
This study highlights the complex nature of healthcare discrimination experiences and their disproportionate impact on patient-reported quality of care outcomes. Moreover, we contribute to the growing literature that empirically examines intersectionality using an applied quantitative approach (Agénor, 2020; Bauer et al., 2021; Harari and Lee, 2021). One of the core tenets of applied intersectionality research is to understand how individual level social categories jointly manifests in macro-level structural conditions (e.g. racism, sexism, poverty etc.) to perpetuate known inequalities. In contrast to previous studies that have focused on the relationship between intersectional discrimination and health outcomes in the community or school-based settings (English et al., 2020; Garnett et al., 2014; Seaton et al., 2010; Tynes et al., 2008), we focus specifically medical provider attributes uniquely present in the healthcare setting. The healthcare environment is also a context in which macro-level inequities, such as racism and sexism, can co-occur and shape not only healthcare experiences, but health outcomes themselves. Scholars have previously identified potential pathways in which experiencing healthcare discrimination may further produce health inequities, driven by reduced motivations to seek out future healthcare encounters or avoidance of the healthcare system altogether (Progovac and Cortés et al., 2020; Romanelli and Lindsey, 2020). Additional empirical evidence is needed to clarify the potential influence of intersectional experiences of discrimination on an expanded range of health service outcomes, such as healthcare cost and utilization.
The current study focuses specifically on individuals with clinically relevant depressive symptoms who may be likely to present with complex therapeutic needs that may result in frequent healthcare interactions (Gold et al., 2020; Moussavi et al., 2007). Our latent class findings align with extant literature that found similar typologies of intersectional discrimination, including a low discrimination class, followed by classes focused on a single demographic indicator (e.g. racial discrimination only) and a multiple indicator class (e.g. racial and weight discrimination) (Earnshaw et al., 2018; Garnett et al., 2014). Previous studies also found that frequent exposure to healthcare discrimination among vulnerable populations results in poor health outcomes and low healthcare utilization (Frank et al., 2014; Peek et al., 2011; Rogers et al., 2015). These health consequences are further exacerbated among marginalized patients (Husaini et al., 2004; Lauderdale et al., 2006; Lindsey et al., 2019; Sheppard et al., 2014). Our results provide growing support to the notion that experiences of discrimination across both single and intersectional domains present negative repercussions in varied social contexts.
A possible alternative explanation for our findings is that negative patient-reported experiences from our respondents were reflective of the discrimination experiences themselves—that is, there may be overlapping constructs shared between how we measure discrimination (e.g., unfair treatment by a medical provider) and our outcomes (e.g., listening carefully, respectful nature). Previous research focused on measuring interpersonal discrimination generally includes items that capture instances of unfair treatment, such as being treated with “less courtesy” and “less respect”, which may highly correlate with patient-reported outcomes (Krieger et al., 2005; Shariff-Marco et al., 2011; Williams et al., 1997). Due to the cross-sectional nature of our study and the timeframe in which we asked about past discrimination (e.g., “… ever felt that you were treated unfairly”), we are not able to ascertain the temporal order of discrimination experiences and patient-reported outcomes. Additional research is needed to determine the direction of this association, particularly whether lower patient-reported outcomes are aligned conceptually with discrimination experiences or whether they are the resulting consequences of discriminatory behavior.
Although the HRE and EPVR classes both include individuals that endorse experiencing racial discrimination, they hold distinct characteristics and differential associations in relation to patient-reported outcomes. Of note, the HRE class included individuals with higher than average item-class probabilities on both racial and ethnic discrimination indicators. The HRE class also includedmore racial and ethnically diverse individuals that were more likely to have higher education attainment and employment than the EPVR class. Although individuals in the HRE class report poorer provider quality and communication than those in the LD class, these estimates were not significant for provider respect and communication. One potential explanation for this finding is the small sample size of the HRE class itself. Despite not being uniformly significant, however, we believe these associations may highlight the importance given to provider attributes of communication and overall quality among diverse populations of higher socioeconomic status, as measured by education or employment status. In contrast, the EPVR class reflected high item-class probabilities for the racial discrimination indicator only and was comprised of mostly non-Hispanic Black respondents and males. EPVR respondents had higher rates of reporting poor overall medical provider respect and carefully listening, which may be indicative of the salience that racial discrimination plays on these specific patient-reported outcomes.
The VL class consisted of the highest proportion of Hispanic respondents, who reported lower ratings of provider respect and careful listening than the LD class. These findings may reflect the detrimental influence of vicarious healthcare discrimination due to language barriers, particularly among Hispanic individuals. Studies using an acculturative stress framework show that experiencing a high frequency of discriminatory experiences while adapting to a dominant cultural setting influences subsequent healthcare engagement (Alegría et al., 2017; D’Anna et al., 2010; Lai et al., 2017). However, less is known regarding the mechanisms of this association—researchers have yet to identify pathways that influence the discrimination–utilization association among Hispanic populations. Our findings allude to the possibility that perceived discrimination in a healthcare encounter, experienced vicariously, may enhance perceptions of discourteous care. Another notable feature of the VL latent class is that personal and vicarious gender discrimination was rarely encountered among respondents. The ethnic-prominence hypothesis asserts that while gender and race jointly influence one’s expectation of experiencing more unfair treatment, respondents are more likely to attach mistreatment to their marginalized ethnic status rather than gender (Levin et al., 2002). Collectively, these frameworks may help explain why the VL class demonstrated salience of language discrimination compared to other more salient demographic attributes.
Finally, a lifecourse perspective may explain why the LD class, which consisted of significantly older and white respondents, reported fewer instances of healthcare discrimination. Older Black and Hispanic adults report fewer discriminatory experiences than their younger counterparts, and white adults are less likely to report discrimination than other racial/ethnic minority groups (Gee et al., 2012; Otiniano and Gee, 2012; Pérez et al., 2008; Sims et al., 2009). As individuals grow older, they are more likely to identify age, which was not included as an indicator in our study, as the most salient attribute for discrimination (Gee et al., 2007). The LD class comprised most of our respondents, which is consistent with literature showing that discrimination is often underreported due to either minimization or avoidance of the negative experience (Lewis et al., 2015). Future studies should further explore the mediating associations of discrimination, including enhanced vigilance or minimization of the experience with a particular focus on sensitive periods in the lifecourse where healthcare discrimination is particularly detrimental to healthcare utilization (e.g., emerging and late adulthood). Additionally, studies should further examine the influence of age-based discrimination as a key attribute in inequitable healthcare experiences.
Despite its strengths, this study has limitations that may influence the generalizability of our findings. This study is cross-sectional, so we are unable to infer causation in the relationships between healthcare discrimination and quality outcomes. To date, there is limited evidence to clarify the associations between discrimination and patient-reported outcomes in the healthcare system, and future research should focus on investigating these associations longitudinally. Further, framing of the terminology “medical provider” for our study encompassed diverse providers who are not traditionally limited to specialty healthcare settings. Thus, we do not have complete clarity whether the respondents reported behavior about a provider in the specialty mental health setting or in other contexts, such as emergency or primary care. Additionally, based on the stratified nature of our sampling framework, we only selected individuals with moderate to severe depression PHQ-9 scores, rather than a medical diagnosis, which limits our ability to determine whether respondents reflected patients seeking treatment for a depression diagnosis. Further, although our analysis captured socially marginalized identities frequently described in the literature (e.g., race, ethnicity, gender, language, sexual orientation), there may be additional domains that warrant further study using LCA, such as age, skin tone, and non-binary gender identity. Additional covariates related to service utilization or comorbidities, such as health insurance, medical expenditures, and past history of physical and mental disorders, were not available for investigation in the current study but may provide explanatory value in future research.
5. Conclusion
This study affirms the growing need to leverage an applied intersectional framework to derive vulnerable patient groups of interrelated identities that may experience disparate healthcare interactions than the general population. Our study findings provide an opportunity to understand how multiple social attributes interrelate in patient-provider interactions, both personally and vicariously. These past discriminatory experiences may shape persistent negative perceptions of the system as a whole, which can be detrimental to the healthcare experience of individuals with depression. Approaches to mitigate the harmful effects of healthcare discrimination should consider how social inequities manifest in recurring clinical interactions and place historically marginalized patients at a disadvantage when seeking care for depression or other medical needs. To provide more equitable care, healthcare organizations are uniquely positioned to consider the lasting influence of past discriminatory experiences from their patient populations to address organizational culture change in the healthcare system.
Supplementary Material
Funding
This research was supported by a grant from the Patient-Centered Outcomes Research Institute (Grant ME-1507-31469, PI: BL Cook). The first author, LB Adams is supported by the National Institute on Minority Health and Health Disparities (NIMHD L60MD014539).
Footnotes
Declaration of competing interests
The authors declare that they have no competing interests for this study.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmmh.2022.100105.
References
- Agénor M (2020). Future directions for incorporating intersectionality into quantitative population health research. Am. J. Publ. Health, 110(6), 803–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Asadi AM, Klein B, & Meyer D (2015). Multiple comorbidities of 21 psychological disorders and relationships with psychosocial variables: a study of the online assessment and diagnostic system within a web-based population. J. Med. Internet Res, 17(3), Article e4143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alasmawi K, Mann F, Lewis G, White S, Mezey G, & Lloyd-Evans B (2020). To what extent does severity of loneliness vary among different mental health diagnostic groups: a cross-sectional study. Int. J. Ment. Health Nurs. 10.1111/inm.12727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Álvarez K, & DiMarzio K (2017). Immigration and mental health. Curr. Epidemiol. Rep, 4(2), 145–155. 10.1007/s40471-017-0111-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arshanapally S, Werner KB, Sartor CE, & Bucholz KK (2017). The association between racial discrimination and suicidality among African-American adolescents and young adults. Arch. Suicide Res.: Off. J. Int. Acad. Suicide Res, 22(4), 584–595. 10.1080/13811118.2017.1387207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer GR, Mahendran M, Walwyn C, & Shokoohi M (2021). Latent variable and clustering methods in intersectionality research: systematic review of methods applications. Soc. Psychiatr. Psychiatr. Epidemiol, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich SN, Findling MG, Casey LS, Blendon RJ, Benson JM, SteelFisher GK, Sayde JM, & Miller C (2019). Discrimination in the United States: experiences of black Americans. Health Serv. Res, 54, 1399–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bock J-O, Luppa M, Brettschneider C, Riedel-Heller S, Bickel H, Fuchs A, Gensichen J, Maier W, Mergenthal K, Schäfer I, Schön G, Weyerer S, Wiese B, van den Bussche H, Scherer M, & König H-H (2014). Impact of depression on health care utilization and costs among multimorbid patients—From the MultiCare Cohort Study. PLoS One, 9(3), Article e91973. 10.1371/journal.pone.0091973. e91973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bor J, Venkataramani AS, Williams DR, & Tsai AC (2018). Police killings and their spillover effects on the mental health of black Americans: a population-based, quasi-experimental study. Lancet (London, England), 392(10144), 302–310. 10.1016/S0140-6736(18)31130-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L (2012). The problem with the phrase women and minorities: intersectionality—an important theoretical framework for public health. Am. J. Publ. Health, 102(7), 1267–1273. 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, & Williams DR (1999). Racism as a stressor for African Americans: a biopsychosocial model. Am. Psychol, 54(10), 805. [DOI] [PubMed] [Google Scholar]
- Collins LM, & Lanza ST (2009). Latent Class and Latent Transition Analysis: with Applications in the Social, Behavioral, and Health Sciences, 718. John Wiley & Sons. [Google Scholar]
- Cook BL, Trinh N-H, Li Z, Hou SS-Y, & Progovac AM (2017). Trends in racial-ethnic disparities in access to mental health care. Psychiatric Services (Washington, D.C.), 68(1), 9–16. 10.1176/appi.ps.201500453, 2004–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creedon TB, & Cook BL (2016). Access to mental health care increased but not for substance use, while disparities remain. Health Affairs (Project Hope), 35(6), 1017–1021. 10.1377/hlthaff.2016.0098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (1991). Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev, 43(6), 1241–1299. [Google Scholar]
- D’Anna LH, Ponce NA, & Siegel JM (2010). Racial and ethnic health disparities: evidence of discrimination’s effects across the SEP spectrum. Ethn. Health, 15(2), 121–143. 10.1080/13557850903490298 [DOI] [PubMed] [Google Scholar]
- Dunlop DD, Manheim LM, Song J, & Chang RW (2002). Gender and ethnic/racial disparities in health care utilization among older adults. J. Gerontol. B Psychol. Sci. Soc. Sci, 57(4), S221–S233. [DOI] [PubMed] [Google Scholar]
- Earnshaw VA, Rosenthal L, Gilstad-Hayden K, Carroll-Scott A, Kershaw TS, Santilli A, & Ickovics JR (2018). Intersectional experiences of discrimination in a low-resource urban community: an exploratory latent class analysis. J. Community Appl. Soc. Psychol, 28(2), 80–93. [Google Scholar]
- Egede LE, Bishu KG, Walker RJ, & Dismuke CE (2016). Impact of diagnosed depression on healthcare costs in adults with and without diabetes: United States, 2004–2011. J. Affect. Disord, 195, 119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- English D, Carter JA, Forbes N, Bowleg L, Malebranche DJ, Talan AJ, & Rendina HJ (2020). Intersectional discrimination, positive feelings, and health indicators among Black sexual minority men. Health Psychol, 39(3), 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Lacko S, Clement S, Corker E, Brohan E, Dockery L, Farrelly S, Hamilton S, Pinfold V, Rose D, Henderson C, Thornicroft G, & McCrone P (2015). How much does mental health discrimination cost: valuing experienced discrimination in relation to healthcare care costs and community participation. Epidemiol. Psychiatr. Sci, 24(5), 423–434. 10.1017/S2045796014000377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findling MG, Bleich SN, Casey LS, Blendon RJ, Benson JM, Sayde JM, & Miller C (2019a). Discrimination in the United States: experiences of latinos. Health Serv. Res, 54, 1409–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findling MG, Casey LS, Fryberg SA, Hafner S, Blendon RJ, Benson JM, Sayde JM, & Miller C (2019b). Discrimination in the United States: experiences of native Americans. Health Serv. Res, 54, 1431–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth J, Siddiqi N, Koyanagi A, Siskind D, Rosenbaum S, Galletly C, Allan S, Caneo C, Carney R, & Carvalho AF (2019). The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatr, 6(8), 675–712. [DOI] [PubMed] [Google Scholar]
- Frank JW, Wang EA, Nunez-Smith M, Lee H, & Comfort M (2014). Discrimination based on criminal record and healthcare utilization among men recently released from prison: a descriptive study. Health & Justice, 2, 6. 10.1186/2194-7899-2-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett BR, Masyn KE, Austin SB, Miller M, Williams DR, & Viswanath K (2014). The intersectionality of discrimination attributes and bullying among youth: an applied latent class analysis. J. Youth Adolesc, 43(8), 1225–1239. [DOI] [PubMed] [Google Scholar]
- Gee GC, Pavalko EK, & Long JS (2007). Age, cohort and perceived age discrimination: using the life course to assess self-reported age discrimination. Soc. Forces, 86(1), 265–290. [Google Scholar]
- Gee GC, Walsemann KM, & Brondolo E (2012). A life course perspective on how racism may be related to health inequities. Am. J. Publ. Health, 102(5), 967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold SM, Köhler-Forsberg O, Moss-Morris R, Mehnert A, Miranda JJ, Bullinger M, Steptoe A, Whooley MA, & Otte C (2020). Comorbid depression in medical diseases. Nat. Rev. Dis. Prim, 6(1), 1–22. [DOI] [PubMed] [Google Scholar]
- Goodwill JR, Taylor RJ, & Watkins DC (2019). Everyday discrimination, depressive symptoms, and suicide ideation among African American men. Arch. Suicide Res.: Off. J. Int. Acad. Suicide Res, 1–20. 10.1080/13811118.2019.1660287 [DOI] [PubMed] [Google Scholar]
- Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, Eng E, Day SH, & Coyne-Beasley T (2015). Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am. J. Publ. Health, 105(12), e60–76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harari L, & Lee C (2021). Intersectionality in quantitative health disparities research: a systematic review of challenges and limitations in empirical studies. Soc. Sci. Med, 277, Article 113876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell SP (2000). A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am. J. Orthopsychiatry, 70(1), 42–57. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, & Grant BF (2018). Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatr, 75(4), 336–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husaini BA, Hull PC, Sherkat DE, Emerson JS, Overton MT, Craun C, Cain VA, & Levine RS (2004). Diabetes, depression, and healthcare utilization among African Americans in primary care. J. Natl. Med. Assoc, 96(4), 476. [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, Shelp F, Goli V, Cohen HJ, & Blazer DG (1989). Survival and health care utilization in elderly medical inpatients with major depression. J. Am. Geriatr. Soc, 37(7), 599–606. [DOI] [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, & Barbeau EM (2005). Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc. Sci. Med, 61(7), 1576–1596. [DOI] [PubMed] [Google Scholar]
- Krishnan KRR, Delong M, Kraemer H, Carney R, Spiegel D, Gordon C, McDonald W, Dew MA, Alexopoulos G, & Buckwalter K (2002). Comorbidity of depression with other medical diseases in the elderly. Biol. Psychiatr, 52(6), 559–588. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med, 16(9), 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai DW, Li L, & Daoust GD (2017). Factors influencing suicide behaviours in immigrant and ethno-cultural minority groups: a systematic review. J. Immigr. Minority Health, 19(3), 755–768. [DOI] [PubMed] [Google Scholar]
- Lanza ST, & Rhoades BL (2013). Latent class analysis: an alternative perspective on subgroup analysis in prevention and treatment. Prev. Sci, 14(2), 157–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale DS, Wen M, Jacobs EA, & Kandula NR (2006). Immigrant perceptions of discrimination in health care: the California Health Interview Survey 2003. Medical Care, 44(10), 914–920. 10.1097/01.mlr.0000220829.87073.f7 [DOI] [PubMed] [Google Scholar]
- LaVeist TA, Isaac LA, & Williams KP (2009). Mistrust of health care organizations is associated with underutilization of health services. Health Serv. Res, 44(6), 2093–2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeBrón AMW, Spencer M, Kieffer E, Sinco B, & Palmisano G (2019). Racial/ethnic discrimination and diabetes-related outcomes among latinos with type 2 diabetes. J. Immigr. Minority Health, 21(1), 105–114. 10.1007/s10903-018-0710-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin S, Sinclair S, Veniegas RC, & Taylor PL (2002). Perceived discrimination in the context of multiple group memberships. Psychol. Sci, 13(6), 557–560. 10.1111/1467-9280.00498 [DOI] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, & Williams DR (2015). Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu. Rev. Clin. Psychol, 11, 407–440. 10.1146/annurev-clinpsy-032814-112728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsey MA, Sheftall AH, Xiao Y, & Joe S (2019). Trends of suicidal behaviors among high school students in the United States: 1991–2017. Pediatrics, 144(5). 10.1542/peds.2019-1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, & Rubin DB (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. [Google Scholar]
- Mausbach BT, & Irwin SA (2017). Depression and healthcare service utilization in patients with cancer. Psycho Oncol, 26(8), 1133–1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, & Zaslavsky AM (2006). Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Serv. Res, 41(5), 1979–2005. 10.1111/j.1475-6773.2006.00583.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merino Y, Adams L, & Hall WJ (2018). Implicit bias and mental health professionals: priorities and directions for research. Psychiatric Services (Washington, D.C.), 69(6), 723–725. 10.1176/appi.ps.201700294 [DOI] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, & Ustun B (2007). Depression, chronic diseases, and decrements in health: results from the world health surveys. Lancet, 370(9590), 851–858. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén B (2019). Mplus. The Comprehensive Modelling Program for Applied Researchers: User’s Guide, 5. [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct. Equ. Model.: A Multidiscip. J, 14(4), 535–569. [Google Scholar]
- Nylund-Gibson K, & Choi AY (2018). Ten frequently asked questions about latent class analysis. Transl. Issues Psychol. Sci, 4(4), 440. [Google Scholar]
- Otiniano AD, & Gee GC (2012). Self-reported discrimination and health-related quality of life among whites, blacks, Mexicans and central Americans. J. Immigr. Minority Health, 14(2), 189–197. 10.1007/s10903-011-9473-6 [DOI] [PubMed] [Google Scholar]
- Peek ME, Wagner J, Tang H, Baker DC, & Chin MH (2011). Self-reported racial discrimination in health care and diabetes outcomes. Medical Care, 49(7), 618–625. 10.1097/MLR.0b013e318215d925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez DJ, Fortuna L, & Alegria M (2008). Prevalence and correlates of everyday discrimination among US Latinos. J. Community Psychol, 36(4), 421–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Progovac AM, Cortés DE, Chambers V, Delman J, Delman D, McCormick D, Lee E, De Castro S, Sánchez Román MJ, & Kaushal NA (2020). Understanding the Role of Past Health Care Discrimination in Help-Seeking and Shared Decision-Making for Depression Treatment Preferences. Qualitative Health Research. 10.1177/1049732320937663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JR, Sharpe L, Modini M, & Dear BF (2017). Multimorbidity and depression: a systematic review and meta-analysis. J. Affect. Disord, 221, 36–46. [DOI] [PubMed] [Google Scholar]
- Robinson RL, Grabner M, Palli SR, Faries D, & Stephenson JJ (2016). Covariates of depression and high utilizers of healthcare: impact on resource use and costs. J. Psychosom. Res, 85, 35–43. 10.1016/j.jpsychores.2016.04.002 [DOI] [PubMed] [Google Scholar]
- Rogers SE, Thrasher AD, Miao Y, Boscardin WJ, & Smith AK (2015). Discrimination in healthcare settings is associated with disability in older adults: health and retirement study, 2008–2012. J. Gen. Intern. Med, 30(10), 1413–1420. 10.1007/s11606-015-3233-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romanelli M, & Lindsey MA (2020). Patterns of healthcare discrimination among transgender help-seekers. Am. J. Prev. Med, 58(4), e123–e131. 10.1016/j.amepre.2019.11.002 [DOI] [PubMed] [Google Scholar]
- Safran MA, Mays RA Jr., Huang LN, McCuan R, Pham PK, Fisher SK, McDuffie KY, & Trachtenberg A (2009). Mental health disparities. Am. J. Publ. Health, 99(11), 1962–1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwei RJ, Johnson TP, Matthews AK, & Jacobs EA (2017). Perceptions of negative health-care experiences and self-reported health behavior change in three racial and ethnic groups. Ethn. Health, 22(2), 156–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seaton EK, Caldwell CH, Sellers RM, & Jackson JS (2010). An intersectional approach for understanding perceived discrimination and psychological well-being among African American and Caribbean Black youth. Dev. Psychol, 46(5), 1372–1379. 10.1037/a0019869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shariff-Marco S, Breen N, Landrine H, Reeve BB, Krieger N, Gee GC, Williams DR, Mays VM, Ponce NA, Alegría M, Liu B, Willis G, & Johnson TP (2011). Measuring everyday racial/ethnic discrimination in health surveys. Du. Bois Rev. : Social Sci. Res. Race, 8(1), 159–177. 10.1017/S1742058X11000129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppard VB, Williams KP, Wang J, Shavers V, & Mandelblatt JS (2014). An examination of factors associated with healthcare discrimination in latina immigrants: the role of healthcare relationships and language. J. Natl. Med. Assoc, 106(1), 15–22. 10.1016/S0027-9684(15)30066-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims M, Wyatt SB, Gutierrez ML, Taylor HA, & Williams DR (2009). Development and psychometric testing of a multidimensional instrument of perceived discrimination among African Americans in the Jackson Heart Study. Ethn. Dis, 19(1), 56. [PMC free article] [PubMed] [Google Scholar]
- Sonik Rajan A., Creedon Timothy B., Progovac Ana M., Carson Nicholas, Delman Jonathan, Delman Deborah, Lê Cook Benjamin, & Health Equity Consortium. (2020). Depression treatment preferences by race/ethnicity and gender and associations between past healthcare discrimination experiences and present preferences in a nationally representative sample, 253, 112939. 10.1016/j.socscimed.2020.112939 [DOI] [PubMed] [Google Scholar]
- Sonik RA, Creedon TB, Progovac AM, Carson N, Delman J, Delman D, Lê Cook B, & Health Equity Consortium. (2020). Depression treatment preferences by race/ethnicity and gender and associations between past healthcare discrimination experiences and present preferences in a nationally representative sample. Soc. Sci. Med, 253, Article 112939. 10.1016/j.socscimed.2020.112939, 1982. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2017). Stata Statistical Software: Release 15. StataCorp LLC. [Google Scholar]
- Trivedi AN, & Ayanian JZ (2006). Perceived discrimination and use of preventive health services. J. Gen. Intern. Med, 21(6), 553–558. 10.1111/j.1525-1497.2006.00413.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tynes BM, Giang MT, Williams DR, & Thompson GN (2008). Online racial discrimination and psychological adjustment among adolescents. J. Adolesc. Health: Off. Publ. Soc. Adolescent Med, 43(6), 565–569. 10.1016/j.jadohealth.2008.08.021 [DOI] [PubMed] [Google Scholar]
- Williams DR (2008). The health of men: structured inequalities and opportunities. Am. J. Publ. Health, 98(Suppl. ment_1), S150–S157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, & Jackson JS (2007). Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Arch. Gen. Psychiatr, 64(3), 305–315. 10.1001/archpsyc.64.3.305 [DOI] [PubMed] [Google Scholar]
- Williams DR, Lawrence JA, Davis BA, & Vu C (2019). Understanding how discrimination can affect health. Health Serv. Res, 54, 1374–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2009). Discrimination and racial disparities in health: evidence and needed research. J. Behav. Med, 32(1), 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yan Yu, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health: socio-economic status, stress and discrimination. J. Health Psychol, 2(3), 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- Wilson Y, White A, Jefferson A, & Danis M (2019). Intersectionality in clinical medicine: the need for a conceptual framework. Am. J. Bioeth, 19(2), 8–19. [DOI] [PubMed] [Google Scholar]
- Wofford N, Defever AM, & Chopik WJ (2019). The vicarious effects of discrimination: how partner experiences of discrimination affect individual health. Soc. Psychol. Personal. Sci, 10(1), 121–130. 10.1177/1948550617746218 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


