Abstract
Smart product-service systems (PSSs) have emerged as a solution for the ongoing digitalization of products and services, especially during the COVID-19 pandemic and under social distancing. However, the conditions for smart PSS adoption remain unclear, requiring the identification of driving attributes and the interrelationships of the attributes for smart PSS implementation in the healthcare industry. This study contributes by determining the cause-effect interrelationship among smart PSS attributes and by identifying and prioritizing the criteria that drive smart PSS adoption in chronic disease management. The study constructed a five-aspect theoretical model to deepen the understanding of digital health service adoption drivers. Data were collected from 233 healthcare industry practitioners to validate the smart PSS adoption attributes. Exploratory factor analysis (EFA) determined the structure of the attributes, the reliability of the criteria, and the validity of the aspects. The EFA result suggested 24 valid and reliable criteria drivers of smart PSS adoption in the healthcare industry, and they were grouped into five aspects. Following the smart PSS literature and stakeholder theory, the aspects are named digital health service adoption, intelligent connected products, stakeholder communication, environmental benefits, and use schemes. In addition, 17 practitioners treating patients with chronic conditions were interviewed to understand the interrelationships among the aspects and criteria. The fuzzy decision-making trial and evaluation laboratory (FDEMATEL) determined the cause-effect interrelationships based on their dependence and driving power. The FDEMATEL results indicated that intelligent connected products and stakeholder communication are the causal and focal attributes of improving digital health service adoption and providing alternative use schemes. For patients and physicians, the driving criteria include managing data, multifunctionality, data reliability, interoperability, patient communication, and resource efficiency. The theoretical and managerial implications are discussed.
Keywords: Smart product-service system, Digital health service adoption, Intelligent connected products, Stakeholder communication, Factor analysis, Fuzzy decision-making trial and evaluation laboratory
Highlights
-
•
Exploratory factor analysis (EFA) and the fuzzy decision-making trial and evaluation laboratory (FDEMATEL) are used.
-
•
Twenty-four criteria are identified as valid drivers of smart product-service system adoption in the healthcare industry.
-
•
Intelligent connected products and stakeholder communication are the driving attributes.
-
•
The driving criteria are managing data, multifunctionality, data reliability, interoperability, and resource efficiency.
1. Introduction
Digital health services allow instant access to physicians despite distance and time, providing prompt service in emergencies and reducing the travel costs for patients with chronic medical problems [1,2]. Digital health technologies showed a peak in adoption during the COVID-19 pandemic, requiring the digital transformation of facilities and technologies and highlighting the gaps within countries [[3], [4], [5]]. Meskó et al. [6] noted that although digital health has empowered patients, other stakeholders were unprepared and lacked the appropriate business model, leading to physician burnout and patient frustration. The lack of preparation for digital health service provision was evident due to the lack of continuous quality services and effective patient engagement, diminishing the potential benefits [4,7]. Smart product-service systems (PSSs) provide digital health services and desirable products in terms of sustainability, profitability, and customer-friendly strategies [[8], [9], [10]]. Smart PSSs refer to the integration of intelligent connected products and digital services into single-solution bundles that are delivered to the market to satisfy individual consumers’ needs [11,12]. Smart PSSs offer a user-centric business model and provide collaboration through interactions between technology suppliers, physicians, and patients [2,13,14]. Thus, a smart PSS business model has the potential to address the challenges in the digital transformation of the healthcare industry. Prior studies have pointed out the drivers of digital health adoption, including high stakeholder engagement, good infrastructure, and the provision of alternative use schemes [[15], [16], [17]]. However, Jia et al. [10] argued that healthcare institutions lack an understanding of smart PSS attributes and have focused on the required technology without considering how connectivity and digital skills affect stakeholder communication and the adoption of digital services. This situation requires determining and prioritizing smart PSS attributes to guide PSS adoption in the healthcare industry.
Smart PSSs integrate intelligent connected products and digital health services as a bundle to create value propositions and alternative use schemes [11,17,18]. They are a solution that meets customers’ needs based on existing products and the offering of new services using information technology [10,19]. Prior studies have highlighted the strengths of the smart PSS business model in regard to product innovation, competitive advantage, revenue potential, flexibility, and digital service adaptation [[20], [21], [22]]. Smart PSS development and adoption provide sustainable relationships that are crucial to business owners and consumers in the healthcare industry [10]. Calvillo-Arbizu et al. [16] observed that digital health services provided through technology overcome the barriers of location and time as well as social barriers. However, Kropp and Totzek [23] reported that firms are reluctant to adopt smart PSSs and that the majority are merely exploring use cases, leaving the conditions for smart PSS adoption unclear. Chang et al. [17] also found that the variability and constant change in user requirements increase the need for additional services and alternative use scheme offerings. However, in smart PSSs, an emphasis on use scheme development to address the ever-changing needs of users is still lacking. In summary, the adoption of smart PSSs requires further understanding, and gaps remain with regard to industry requirements. Such requirements are unique in terms of infrastructure, internal and external stakeholders, and digital knowledge, leaving the interactions of smart PSS attributes unclear.
Smart PSSs should understand and adapt to the needs of the healthcare industry, developing offerings based on the local context and user capabilities to increase added value. Frank et al. [9] highlighted that an improved business model is required to change the interaction between healthcare providers and customers in digital health service development and delivery. Patients and healthcare staff prefer traditional service delivery over smart PSS alternatives due to the lack of user-friendly systems and organizational issues, reducing use acceptance and performance [10,16]. The identification of multiple stakeholders and their integration is necessary to fulfill smart PSS requirements and to combine intelligent connected products and digital health services into a single solution. Stakeholder theory highlights the interconnections between businesses, their internal and external suppliers, customers and other actors who have relations with a health organization [6,10]. However, a theoretical gap is created when stakeholder interaction is poorly understood, and external forces such as technology create constant change in these interactions, reducing performance and stakeholder acceptance. Fénélon-Dimanche et al. [13] noted that in digital health service adoption, it is necessary to consider stakeholder engagement in collaborative innovation and to codesign processes across patients, physicians, technology suppliers and other healthcare-related professionals. However, focusing on technology rather than users may reduce the potential benefits. Furthermore, Song et al. [18] underlined the importance of including environmental benefits in smart PSS evaluation. Therefore, a holistic framework integrating intelligent connected products, digital health services, stakeholder communication, environmental benefits, and use schemes is required to formulate smart PSS adoption strategies.
The COVID-19 lockdown restricted patient and health workers' mobilization and increased healthcare delivery through digital solutions. Hence, digital health services offer alternatives to in-clinic consultations and positively affect chronic disease patients' quality of life. However, Pierce et al. [24] argued that there is a risk that when the COVID-19 pandemic subsides, digital health may regress and the frequency of use may decrease. Data collected during the COVID-19 pandemic are key to determining the opinions of physicians and practitioners. However, smart PSSs are a concept with numerous attributes; hence, the validity and reliability of the attributes need to be determined for healthcare industry measures. Furthermore, understanding causal aspects and identifying the criteria driving digital health service adoption are essential to guide smart PSS service adoption strategies in the healthcare industry. Thus, this study was conducted in two phases and involved physicians as well as practitioners managing chronic disease patients. In phase one, data were collected from physicians. Exploratory factor analysis (EFA) determined the attributes' structure and explained the amount of variance based on the attributes to determine reliability, the quality of the criteria, and the underlying validity of the aspects [25,26]. In phase two, data were collected from practitioners treating patients with chronic medical problems via a linguistic scale. Hence, this study used fuzzy set theory to deal with the linguistic preferences and uncertainties related to the attributes' qualitative nature and the experts’ judgment, such as judging importance and influence levels. Fuzzy set theory converts linguistic preferences into quantitative data. The fuzzy decision-making trial and evaluation laboratory (FDEMATEL) determined the cause-effect relationship of aspects and criteria through a matrix and diagrams based on their dependence and driving power [[27], [28], [29]]. The objectives of this study are as follows:
-
•
To identify valid and reliable smart PSS criteria and the underlying aspects in the healthcare industry
-
•
To determine the cause-effect relationship among smart PSS attributes based on qualitative information
-
•
To identify crucial attributes for smart PSS adoption in chronic disease management
This study deepens the understanding of smart PSSs, proposes a theoretical model, and identifies influencing criteria to improve smart PSS success in chronic disease management. Additionally, it contributes by providing a hierarchical framework to guide digital health service adoption strategies in the healthcare industry. The proposed framework defines causal aspects and extracts the top criteria. Practitioners can refer to the criteria in developing strategies and approaches to chronic disease management using smart PSSs. This study is structured as follows. Section 2 reviews the literature relevant to smart PSS development, perspectives and aspects. Section 3 explains the case background and the methodology used, EFA and the FDEMATEL. Section 4 shows the results obtained. Section 5 discusses the theoretical and managerial implications of smart PSSs in the healthcare sector. Finally, Section 6 explains the conclusions and limitations of this study as well as further research required to extend smart PSS knowledge.
2. Literature review
2.1. Smart product-service systems
Smart PSSs integrate information technology into conventional PSSs, allowing the development of new services. Advances in the Internet of Things enable new capabilities and connectivity, achieving smart PSSs through the integration of new technologies such as deep learning, artificial intelligence, and cloud computing [12,30]. Advanced information technologies allow heterogeneous data extracted from user devices to create a decision support system and digitalized services [8,22,30]. The smart solution allows data collection through sensors and user input to monitor device conditions, external conditions and user conditions and behavior in real time, improving the offering in a customizable option based on the customer context [31,32]. The development allows a new service provision without the uncertainties attached to customer desire through data collection and predictive analysis. The benefits of smart PSSs include information exchange and access, better technical decision-making, enhanced security and control, and improved communication and coordination with stakeholders [22,25,33]. In addition, stated that smart solutions decrease the time to market and related costs, increase customization and ensure trouble-free operations through prognostics instead of diagnostics. The advantages of smart PSSs result in benefits that extend the product lifespan, improve communication and collaboration between stakeholders, and promote the cocreation of value, and the data obtained support decision-making under uncertainties.
However, Kroop and Tozek [23] noted that smart PSS settings create complexity and higher uncertainties due to user novelty, technological comprehension, and interorganizational networking. Smart PSSs require data collection and information exchange through different administrative systems and software, leading to misinterpretation and errors. Prior studies suggest that there has been a focus on technology instead of customers in the design of smart PSSs, leading to poor engagement and adoption and creating concerns over intrusiveness and privacy [17,25]. In addition, the impact of climate change and pollution is a rising environmental concern. Technological development has grown exponentially, and smart PSSs should be designed to extend product lifespan and enhance reuse, proper recycling, and efficient resource management [19,31]. However, studies integrating environmental benefits are still under development, even though the core benefits of smart PSSs are related to environmental benefits [18,34,35]. Hence, assessing the development of smart PSSs can foster adoption and reduce user gaps. In addition, a theoretical model and core drivers can enhance activities with complementing policies and infrastructure.
2.2. Smart product-service systems in the healthcare industry
Smart PSSs in the healthcare industry have integrated technologies to develop digital health services and intelligent products to diagnose, monitor, and treat chronic diseases. Diagnostic services are becoming available and accessible through healthcare-based platforms, such as patient records, next-generation sequencing, biomarker data, and big data research [36,37]. In addition, diagnostic services are translated to the consumer through mobile apps and miniaturized digital electronics that are implantable or wearable, allowing real-time monitoring of daily life signals and aiding in prompt diagnosis and treatment [[38], [39], [40]]. Telemonitoring services can be applied to clinical trials, patient records, patient devices, and virtual consultations to track a patient's health to remotely interpret data and make decisions regarding follow-up and treatment [1,41]. Smartphone apps and devices deliver emergency healthcare, monitor glucose levels, blood pressure, and heart rates, and aid in medication adherence [12,13,42]. For treatment, digital health allows the acquisition of open health information, biomedical research, and patient records, aiding medication decision support systems in treatment [3,37]. Some cases may require surgery as a solution to the health condition; therefore, the use of robotic systems and remote devices provides a prompt response to emergencies [36,41]. For instance, smart PSSs enable remote health provision through collaborative diagnosis, monitoring and treatment for the patient.
However, intelligent connected products and digital services face significant challenges and drawbacks, especially in the digital transformation of consumers [6,16,17]. Intelligent connected products are redefining digital health services and their entire ecosystem, paving the way for smart PSSs in the health domain. Nevertheless, potential barriers to adoption related to stakeholder communication, use schemes, interoperability and the reduction in medical interaction remain [9,24]. The future of health is related to the benefits of digital integration for conventional services. For example, during the COVID-19 pandemic, there was a surge in digital health due to distance restrictions and infection risks [3,5]. For the future, more innovative strategies to innovate services, improve quality and process efficiency, and reduce healthcare management costs are being sought. Digital health services remain key to value delivery based on patient information. The data collected by sensors, user input and electronic medical records can also improve professional collaboration [16,31,43]. Thus, there has been smart PSS development in the healthcare sector. Table 1 highlights articles published between 2016 and 2022 related to smart PSSs in the healthcare industry. However, the effect of intelligent connected products, stakeholder communication, environmental benefits, and use schemes on smart PSS adoption should be further explored.
Table 1.
Smart PSSs in the healthcare industry.
| Literature | Application | Theoretical basis | Factors |
|---|---|---|---|
| Flores-Vaquero et al. [52] | PSSs to develop telehealth | General PSS and telehealth literature |
|
| Chang et al. [17] | Smart PSS development from the user perspective | Stakeholder theory Expectation–confirmation theory |
|
| Abdel-Basst et al. [57] | Smart PSS innovation value evaluation | General smart PSS and decision-making literature |
|
| Bu et al. [11] | Smart PSS framework design using user-centric virtual reality (VR) | General smart PSS and VR literature |
|
| Haber and Fargnoli [49] | Sustainable PSS customization method | General PSS literature |
|
| Zhang et al. [51] | PSS requirement interaction evaluation method | Nonadditive aggregation |
|
| Wang et al. [32] | Smart PSS-based rehabilitation assistive device design | General PSS literature/traditional PSS frameworks |
|
Digital health services refer to the integration of information and communication technologies in health service delivery to improve quality of life and prevent diseases. The growing use of digital health services is forcing the traditional healthcare system to evolve into a new phase dubbed smart PSSs. Disruptive technologies such as genomics, telemedicine, and artificial intelligence are the drivers of digital transformation in the healthcare sector, improving patient care, increasing accessibility, and providing cost-effective treatments and precise diagnoses [10,44]. Meskó et al. [6] argued that despite the benefits of digital health services, they carry the risk of dehumanizing care, highlighting the need to understand cultural challenges and stakeholder requirements. Carlo et al. [7] argued that digital service adoption in healthcare is increasing; however, it is limited by the context, infrastructure, and society. Phillips et al. [43] noted that with the rise of digital health services and intelligent connected products, there is an increase in accessible patient data, posing new challenges related to stakeholder communication, data reliability, and privacy concerns. Due to intelligent connected products, stakeholders and patients are expected to use digital health services and support their adoption, collecting data at real-time speed. Digital health service adoption can be created based on intelligent connected products, stakeholder communication, and sustainability [24,25,31]. Smart-driven technology business success correlates with a value proposition based on digital services complementing intelligent connected products, bringing economic benefits and advantages over competitors.
Stakeholder communication reflects the exchange of information through convenient methods and familiar language, using standards to retain the meaning of the data collected. A smart PSS is a digital-based ecosystem where several stakeholders pursue their interests in a value generation network. In the health industry, stakeholder theory advocates separating or distancing the monetary goal from patient well-being, providing value for all stakeholders and incorporating core values that drive organizations [6,10,17]. Stakeholder communication increases loyalty, allowing value sharing to strengthen relationships and improve collaboration between technology suppliers, physicians, and patients [20,22,34]. Collaboration could lead to increased quality and efficiency through cooperation, coordination, and shared decision-making between providers and patients [1,6,35]. Smart PSSs rely on data sharing and management to increase well-being and equity among stakeholders. Allowing information access and use across stakeholders could increase digital health service adoption and use schemes. Information flow depends on collaboration between users and service providers, requiring the integration of different perspectives and heterogeneous systems. Tseng et al. [35] found that digital knowledge management across stakeholders impacts individual inclusion and socioeconomic development. The literature provides an overview of the benefits of communication; however, the diversity of stakeholders renders it impossible to accurately assess the effect on each one, requiring careful consideration of the user's context.
Intelligent connected products contribute to new forms of data collection, processing, and information exchange, increasing traceability, optimization, resource efficiency, and maintenance [16,31,34]. Smart PSSs adopt technology faster than conventional models, demanding real-time data collection, interoperability across different platforms and continuous availability and changing use schemes and stakeholder communication [40,45]. Cruz-Cárdenas et al. [8] argued that consumer attitudes toward intelligent connect products take into account the potential benefits and result in a willingness to be early adopters; in contrast, new technology adoption may contribute to overwhelming consumers as well as a lack of control, insecurity, and distrust in its consequences. Aceto et al. [36] stated that stakeholders look for the benefits of intelligent connected products in smart PSSs and that adoption is influenced by advanced quality capabilities, access, efficiency, and new value offerings. Intelligent connected products play a crucial role in smart PSSs and enable economic, social, and environmental benefits based on data input and analytics. However, regarding the barriers to the adoption of technological advances, it has been reported that service costs, connectivity issues, low literacy, and digital skills can hinder the potential of smartness in PSSs [16,17,40].
The use scheme is result oriented and user oriented; hence, customers rely on platforms and mobile applications to interact and communicate with service providers [33]. Smart PSS customers and stakeholders try to find faster and more comfortable ways to fulfill their requirements and perform daily activities in a connected and reliable way, guaranteeing customer and service provider interactions through a variety of internet and service platforms [14,46]. Gogia [1] stated that patients and medical staff try to find the advantages of use schemes in digital and service platforms, for example, by sharing health monitoring devices and reducing costs and maintenance burdens. Use scheme alternatives such as sharing stimulate environmental benefits, increase the intelligent connected product lifespan, maximize use, and influence technology employment and social identity [12,32,47]. However, Tseng et al. [28] noted a common concern in the nonownership context over the carelessness of consumers when using products, reducing their lifetime, and increasing their repair and maintenance costs as rebound effects. Prior studies have addressed the urgent need to identify the perception of nonownership consumption, public acceptance, and possible rebound effects [28,33,48]. Recognizing the use scheme and its role in smart PSS adoption allows us to understand the possible drawbacks, especially in independent product offerings, including access-based consumption and result-oriented value propositions.
Environmental benefits such as the reduction in greenhouse gas emissions, improved product lifecycle management, and good practices for waste disposal can mitigate hazardous conditions and impact the ecosystem and human health [20,49,50]. Smart PSSs change the conventional ownership paradigm, proposing a dematerialization approach and improving resource efficiency [12,33]. The characteristics of smart PSSs provide lifespan extension, emission reduction and resource efficiency to alleviate their negative impacts. With service innovation and product reconfiguration, smart PSSs contribute to product lifespan expansion, increase traceability, and provide support for decision-making [30,33,34]. Customers’ lack of awareness of environmental impacts and the ever-changing requirements of users can lessen the potential of smart PSS offerings [32,34]. Smart PSSs, through cleaner production, dematerialization and monitoring systems, can aid in reducing environmental impacts. However, the potential can be diminished due to a lack of user environmental knowledge and inadaptability to external conditions.
3. Method
3.1. Proposed method
Previous studies have used a variety of quantitative and qualitative methodologies to examine and understand smart PSSs from different perspectives and in different contexts. For instance, Chen et al. [31] integrated fuzzy set theory with the best worst method to prioritize the requirements for smart PSSs. Kropp and Totzek [23] used exploratory and confirmatory factor analysis to identify the institutional pressures and system characteristic effects on customers’ acceptance of smart PSSs. Cruz-Cárdenas et al. [8] applied factor analysis to conglomerate criteria based on a factor loading greater than 0.5, creating a factor structure to propose a conceptual model of the drivers of technology readiness and consumption in technology-based services. Henkens et al. [25] applied an experimental approach to calculate customer engagement in the provision of a level of smartness, followed by statistical analysis, and they evaluated a proposed model using a structural equation model. Wu et al. [21] used fuzzy set theory to evaluate functional values, allowing ranking and trimming to optimize smart PSS design. Song et al. [18] proposed integrating rough set theory into multicriteria decision-making problems to handle imprecise and vague decision-making information. However, prior studies have not validated smart PSS measures for the healthcare industry. They have also failed to address the interrelationships among criteria to achieve more precise solutions for smart PSSs. In addition, the literature has not included user feedback in the preliminary design of smart PSSs, and research on the variability in the attributes proposed during data collection is needed [18,51]. Hence, this study employed two phases to validate the healthcare industry measures and to address the interrelationships among smart PSS attributes.
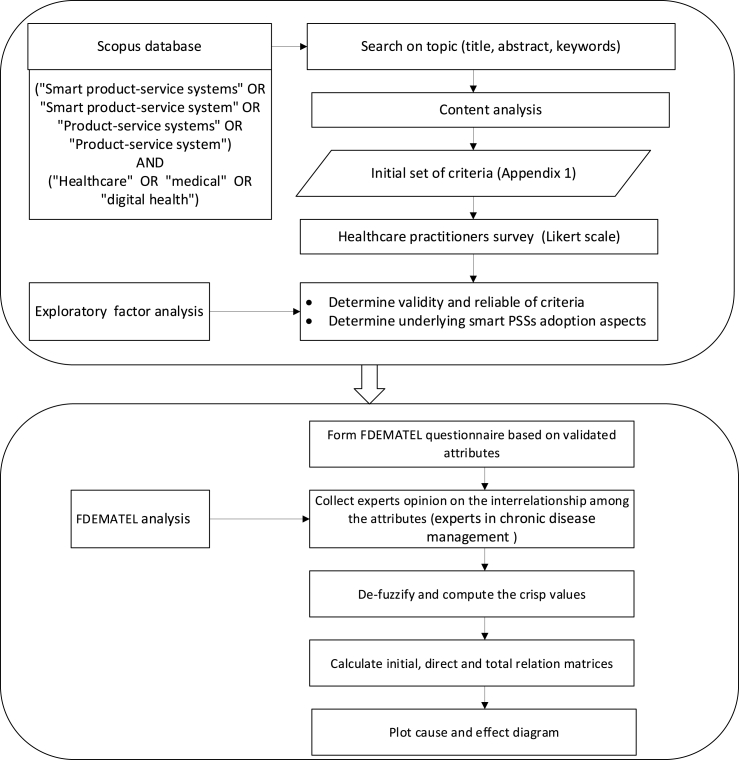
First, an entire set of interdependent relationships was examined based on EFA to determine the validity, reliability and underlying aspects. The relationships among sets of many interrelated variables are represented in terms of a few underlying aspects. Second, the FDEMATEL was employed to explore the interrelationships among digital health services, intelligent connected products, stakeholder communication, environmental benefits, and use schemes in the healthcare industry. The FDEMATEL combines fuzzy set theory with multicriteria decision-making problems to obtain the interrelationships among attributes and to create a smart PSS hierarchical model. The FDEMATEL defines the interdependencies of conceptual factors and highlights reducing the variability and uncertainty among attributes using linguistic scales of triangular fuzzy numbers [20,29,35]. The proposed methodology can provide a hierarchical model for smart PSS adoption in the healthcare industry context and integrate the interpretation of fuzzy advantages and the direction of interdependence among attributes.
3.2. Case background and data collection
Ecuador is adopting the implementation of electronic health records and digital health entrepreneurship in chronic disease management driven by patient care improvement, cost-effectiveness, and accessibility [44]. The prevalence of chronic diseases has proliferated, causing high economic and human costs to the national healthcare system [52]. Furthermore, the COVID-19 pandemic has affected national health systems, as unpreparedness, scarce medical supply, high demand for medical services and slow operational capacity have increased infections and deaths [53,54]. Additionally, patients’ hesitancy to seek care due to fear of contamination and lack of access to hospitals and other healthcare institutions diminished contact with patients, reduced the accessibility of treatment, and increased misinformation [54]. Digital health through teleconsultation, telemonitoring, and videoconferences was an alternative for overcoming the existing challenges. Medical information exchange through information and communication technologies proved helpful in chronic disease management [41]. However, digital health constituted a sudden shift in practice that did not take into account digital and cultural readiness and transformation, diminishing its adoption and benefits [6,16].
This study's target population is practitioners with at least five years of experience who treat patients with chronic conditions. The digital transition in smart PSSs has profound implications for this population, which is why we select it. Data were collected in two rounds in March and April 2021. First, we used a five-point Likert scale for physicians. A convenience sampling strategy was used to conduct an online survey with a self-administered questionnaire. Second, data were obtained from 17 experts in chronic disease management using linguistic preferences. The profile of the experts is shown in Table 2. The experts evaluated the pairwise influence of aspects, and from each participant, 5 × 5 data points were collected. In addition, the pairwise influence among the criteria was collected to identify the most important criteria for developing smart PSSs in the healthcare industry, and 24 × 24 data points were collected from each participant. The responses are presented on fuzzy linguistic scales in Table 3.
Table 2.
Profile of the experts.
| Expert | Description | Experience in healthcare (years) |
|---|---|---|
| 1 | General Practitioner | 20 |
| 2 | Heath institution manager | 5 |
| 3 | Heath institution manager | 6 |
| 4 | General Practitioner | 5 |
| 5 | Nutritionist | 5 |
| 6 | Endocrinologist | 8 |
| 7 | Heath institution manager | 9 |
| 8 | Oncologist | 8 |
| 9 | General Practitioner | 25 |
| 10 | Endocrinologist | 11 |
| 11 | Nutritionist | 10 |
| 12 | Heath institution manager | 5 |
| 13 | Cardiologist | 8 |
| 14 | Oncologist | 12 |
| 15 | Chief Nursing Officer | 30 |
| 16 | Chief Nursing Officer | 35 |
| 17 | Nutritionist | 6 |
Table 3.
Linguistic scale.
| Influence Level | Triangular Fuzzy Number |
|---|---|
| Extreme | (0.75, 1.00, 1.00) |
| Demonstrated | (0.50, 0.75, 1.00) |
| Strong | (0.25, 0.50, 0.75) |
| Moderate | (0.00, 0.25,0.50) |
| Equal | (0.00, 0.00, 0.25) |
3.3. Data analysis and analytical steps
The steps this study followed to identify the underlying aspects of smart PSS development and understand the interrelationships among the aspects are provided in Fig. 1 and explained below.
-
1.
This study proposed a set of 29 criteria influencing smart PSS development in the healthcare industry (Appendix 1). To determine the relationships among sets of 29 interrelated variables collected from the literature analysis and represent them in terms of a few underlying aspects, EFA was performed using varimax rotation in IBM SPSS Statistics. Once the underlying aspects that explain the correlations among a set of smart PSS attributes were identified, the FDEMATEL examined how the underlying aspects are linked together, taking into account experts' assessment of the influence levels and following steps 1 to 8.
-
2.
Normalization: Assume that the decision-making committee consists of n professionals who completed the evaluation using linguistic preferences. Thus, the chosen influence level linguistic preference, , which reflects the ith attribute, had an effect on the jth attribute as determined by the fth expert.
| (1) |
where .
-
3.
Calculate the normalized values for the left and right sides using Eq. (2), as well as the overall normalized crisp value using Eq. (3).
| (2) |
| (3) |
-
4.
Calculate the synthetic values by aggregating the subjective judgments of n assessors.
| (4) |
-
5.
Create an initial direct relation matrix, where and specify the extent to which criterion i has an effect on criterion j. Standardize the initial direct relation matrix.
| (5) |
where
Fig. 1.
Proposed analysis steps.
Generate the total relation matrix.
| (6) |
-
6.
Create a causal diagram; the values of (α + β, α − β) form an important relationship map. The x-axis (α + β) denotes “prominence” and shows importance. The y-axis (α − β) represents “relationship”, and the y-axis (α − β) denotes “connection” and categorizes criteria based on cause and effect. If (α − β) is negative, then it belongs to the effect group; if it is positive, then it belongs to the cause group.
| (7) |
| (8) |
4. Results
4.1. Data screening
After eliminating unusable replies owing to a failure to pass the screening question and poor engagement, 269 responses out of 308 attempts to complete the survey were retained. Mahalanobis D2 measures were used to analyze multivariate outliers, and 36 responses with a significance level of less than 0.005 were excluded. The remaining sample size was 233, corresponding to 75.65% of the total participants. Normality was established satisfactorily by evaluating the normal probability plot. Scatterplots were used to determine homoscedasticity and linearity and demonstrate a fairly uniform dispersion and linear pattern. Thus, it is considered that all of the assumptions for conducting EFA were met.
4.2. Validated smart PSS measures
EFA used principal component analysis with varimax rotation to obtain a five-factor model, as shown in Table 4, with a factor loading greater than 0.5 and an eigenvalue greater than one. Five criteria with a factor loading less than 0.5 were removed. The value of the Kaiser‒Meyer‒Olkin test was 0.919, and the value of Bartlett's test of sphericity approximate chi-square was 3273.542 (p value < 0.01). Cronbach's alpha reliability test was performed for test consistency, with an overall value of 0.938. The five attributes explain 66.594% of the total variance. Factor analysis grouped 24 valid criteria into five aspects, which, following the literature, were named digital health services, intelligent connected products, stakeholder communication, environmental benefits and use schemes. The 24 criteria accepted after EFA are discussed below.
Table 4.
Pattern, reliability and validity of the aspects.
| Aspect | Criteria | Component |
|||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | α | ||
| A1: Digital health service | C1: Digital user identity | 0.708 | 0.907 | ||||
| C2: Data collection | 0.707 | ||||||
| C3: Data processing | 0.702 | ||||||
| C4: Personalized care | 0.698 | ||||||
| C5: data management | 0.680 | ||||||
| C6: Individual empowerment | 0.635 | ||||||
| C7: Health knowledge notification | 0.623 | ||||||
| A2: Intelligent connected products | C8: Reactivity | 0.731 | 0.883 | ||||
| C9: Security configuration | 0.683 | ||||||
| C10: Multifunctionality | 0.626 | ||||||
| C11: Device cooperation | 0.624 | ||||||
| C12: Adaptability | 0.611 | ||||||
| C13: Data reliability | 0.566 | ||||||
| A3: Stakeholder communications | C14: Interoperability | 0.766 | 0.816 | ||||
| C15: Human-like interaction | 0.712 | ||||||
| C16: Social media communication | 0.706 | ||||||
| C17: Autonomy | 0.578 | ||||||
| C18: Patient communication | 0.520 | ||||||
| A4: Environmental benefits | C19: Resource efficiency | 0.726 | 0.812 | ||||
| C20: Additional support | 0.710 | ||||||
| C21: Reducing gas emissions | 0.698 | ||||||
| C22: End-of-life recycling | 0.610 | ||||||
| A5: Use scheme | C23: Shared use | 0.799 | 0.745 | ||||
| C24: Service platform | 0.724 | ||||||
Note, α: Cronbach's alpha.
Digital health services refer to the integration of information technology into service provision, innovating service, increasing customer satisfaction and providing personalized care. The benefits of digital health services are related to the value propositions of smart PSSs, as digital services join with intelligent products, creating a personalized experience for the user. Therefore, digital user identity (C1) creates a digital profile to identify the user, track user activity and provide personalized feedback [17,31]. Data collection (C2) by sensors or user input also includes data searches by the user for data processing (C3) or further analysis [12,45]. Personalized care (C4) is added value, providing customized and individualistic service to the patient, and it is supported by adequate data management (C5), which organizes the information obtained and accesses the information to evaluate the specific situation to support the decision-making process [12,18,55]. Individual empowerment (C6) complements the added value and encourages patients to change their lifestyles [6]. Finally, health knowledge notification (C7) provides feedback on devices and user activities based on reliable health knowledge [36].
Intelligent connected products consider digital capabilities to be a responsiveness mechanism or reactivity (C8), identifying, evaluating and reacting to customer needs, changes and the environment [12,22]. Increasing awareness and privacy concerns require protecting patient information. Therefore, the security configuration (C9) protects private information such as health monitoring, real-time location, video records and clinical reports [16,56]. Today's user requirements exponentially increase the ability to do more with less, as multifunctionality (C10) becomes necessary to provide multiple functions with only one product, such as a smartphone, that can send photos, messages and heart rate monitoring [12]. Connectivity entails the network connection of different users and devices. Consequently, device cooperation (C11) is key to digital capabilities through the communication and cooperation of health monitoring products with smartphones, laptops and personal computers [36,56]. Adaptability (C12) improves adjustment to the variation in context, expanding functionalities and providing new services requiring a close relationship with the customer and knowledge exchange [9,22,57]. In the medical industry, data reliability (C13) refers to the accuracy and completeness of medical data, which is important for proper diagnosis and treatment, creating transparency and building trust [36,43,46].
Stakeholder communication refers to social capabilities and user integration through information exchange, creating a collaborative environment. Interoperability (C14) is a facilitator for data shared between healthcare providers, requiring the use of standards due to the variety of platforms, databases and data formats. Patients need interoperability, as they own different brand devices and components [36,55]. Human-like interaction (C15) in devices creates comfort and promotes data input and exchange, especially in users with low digital literacy. Complementing human-like interactions, smartness makes it possible to integrate these users into the system, facilitating and supporting the use of devices and services [12,16]. Social media (C16) interaction requires sharing and visualizing other user content, is a tool for reaching out to a patient, and creates social inclusion while strengthening customer-provider relationships [25,42]. Autonomy (C17) allows people, platforms and machines to be connected independently of user activity, creating autonomous communication of patient conditions as sensors, networks and processing technologies function based on the data obtained and the requirements previously programmed to assist the patient [19,41]. As the core of digital health, the patient engages in communication with providers to treat their diseases, and patient communication (C18) is key to healthcare delivery and consists of gathering information to aid in diagnosis and to provide counseling and treatment guidelines [13,44].
The environmental benefits highlight the potential environmental capacity of smart PSSs. Because smart PSSs are a smart technology, resource efficiency (C19) allows effective resource use through the continuous monitoring of conditions and proper maintenance based on data management to make the best decision [19,30,33]. Additional support (C20) refers to additional aftersales services, which may require some products such as monitoring sensors to increase their lifespan and added value services to the user [10,33]. In addition, digital health reduces travel to visit doctors, as it can be accessible to rural patients, reducing greenhouse gas emissions (C21) [1,50]. Finally, end-of-life recycling (C22) makes use of the technology to identify the right time for recycling and acknowledges the material composition for a correct recycling process [19]. In addition, dematerialization capability has been linked to PSSs due to the change in ownership perspective. Changing the use scheme to shared use (C23) refers to access-based products, such as renting or leasing for a period of time, but ownership still remains with the provider in charge of maintenance and repair, for example, ambulatory cardiac biosignals such as MoMe Kardia by InfoBionic [39,45,46]. Finally, the service platform (C24) refers to the smart services offered digitally and independently of the product [38].
4.3. Interrelationships among smart PSS attributes
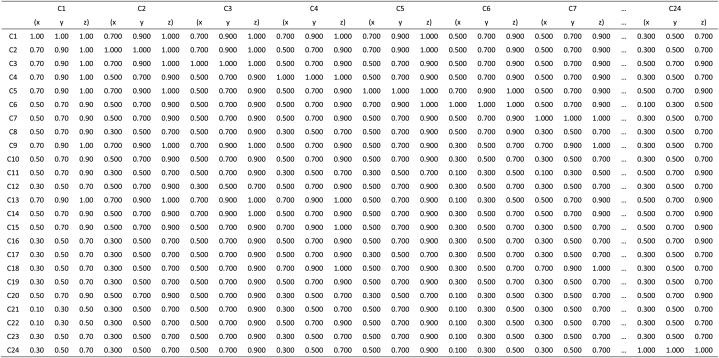
The direct relation matrix of aspects is shown in Table 5, which was derived using Eqs. (1), (2), (3), (4), (5). Then, as illustrated in Table 6, Eqs. (6), (7), (8) are used to generate the total relation matrix of aspects.
Table 5.
Direct relation matrix of aspects.
| Aspect | A1 | A2 | A3 | A4 | A5 |
|---|---|---|---|---|---|
| A1 | 0.72 | 0.52 | 0.53 | 0.37 | 0.41 |
| A2 | 0.54 | 0.73 | 0.46 | 0.34 | 0.36 |
| A3 | 0.49 | 0.50 | 0.47 | 0.35 | 0.33 |
| A4 | 0.41 | 0.37 | 0.39 | 0.75 | 0.40 |
| A5 | 0.33 | 0.39 | 0.46 | 0.37 | 0.74 |
Table 6.
Total interrelationship matrix of aspects.
| Aspect | A1 | A2 | A3 | A4 | A5 | α | β | (α + β) | (α − β) |
|---|---|---|---|---|---|---|---|---|---|
| A1 | 2.90 | 2.85 | 2.62 | 2.37 | 2.44 | 12.94 | 13.18 | 26.12 | −0.24 |
| A2 | 2.72 | 2.84 | 2.49 | 2.26 | 2.33 | 13.10 | 12.64 | 25.74 | 0.46 |
| A3 | 2.37 | 2.41 | 2.20 | 1.99 | 2.03 | 11.94 | 11.00 | 22.94 | 0.94 |
| A4 | 2.51 | 2.53 | 2.33 | 2.33 | 2.23 | 11.06 | 11.92 | 22.98 | −0.86 |
| A5 | 2.41 | 2.48 | 2.30 | 2.11 | 2.33 | 11.35 | 11.63 | 22.98 | −0.28 |
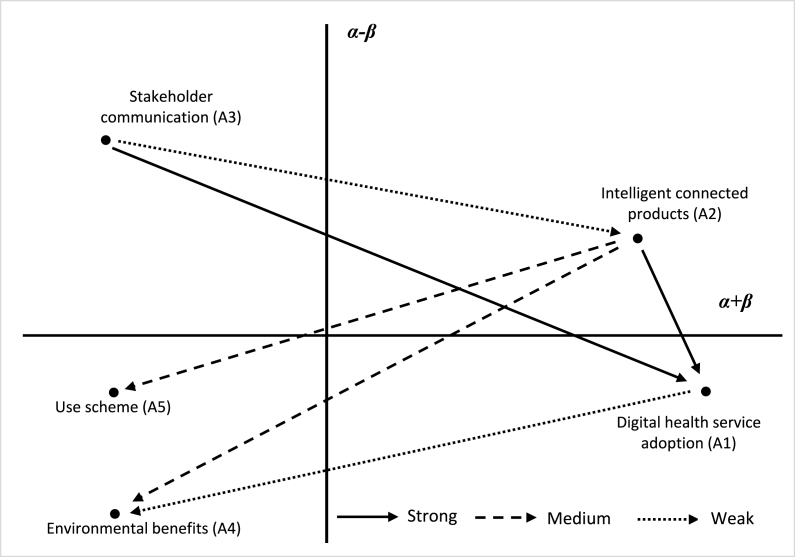
Fig. 2 depicts the relationships between aspects and their causes and effects, in which intelligent connected products (A2) and stakeholder communication (A3) are classified as the cause group. In contrast, digital health service adoption (A1), environmental benefits (A4), and use schemes (A5) are classified as the effect group. The results show that intelligent connected products and stakeholder communication strongly affect digital health service adoption. Intelligent connected products also exert a medium influence on environmental benefits and use schemes. Hence, intelligent connected products are the drivers of digital transformation and new services, providing environmental benefits and changing use schemes. In addition, stakeholder communication increases information exchange, providing valuable data to promote intelligent product development and fostering the adoption of customized digital health services.
Fig. 2.
Smart PSS aspects interrelationship the healthcare industry.
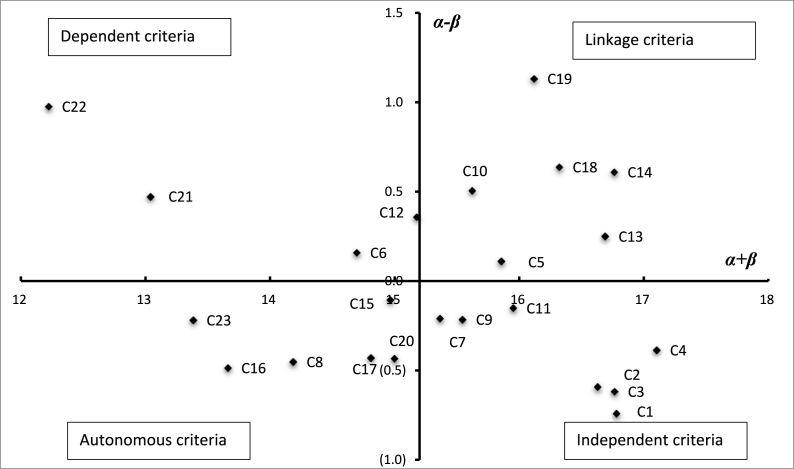
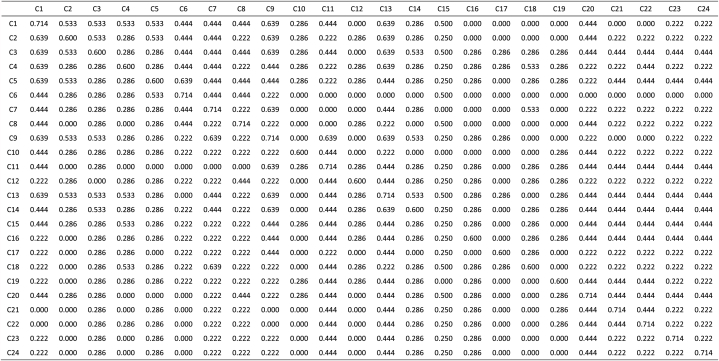
The direct and total relation matrixes of the criteria is shown in Table 7, Table 8, respectively. Fig. 3 illustrates a cause-and-effect diagram of the criteria, showing that the criteria are divided into four quadrants. Quadrant 1, or the linkage/causal criteria, has great power and is crucial for the shift to SMPs. The causal smart PSS criteria are managing data (C5), multifunctionality (C10), data reliability (C13), interoperability (C14), patient communication (C18) and resource efficiency (C19). As managerial implications, smart PSSs in the healthcare industry should focus on these criteria. Four criteria fall under Quadrant 2, often known as the dependent criteria, which have much power but are not as crucial to the system. Quadrant 3, also known as the autonomous criteria, has a low level of dependency and is somewhat detached from the rest of the system. Six criteria are found to be autonomous. The seven criteria in Quadrant 4, often known as the independent criteria, could be enhanced only indirectly by improving Quadrant 1.
Table 7.
Direct relation matrix of criteria.
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | C10 | C11 | C12 | C13 | C14 | C15 | C16 | C17 | C18 | C19 | C20 | C21 | C22 | C23 | C24 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C1 | 0.77 | 0.63 | 0.58 | 0.52 | 0.46 | 0.40 | 0.46 | 0.39 | 0.52 | 0.33 | 0.43 | 0.32 | 0.51 | 0.49 | 0.44 | 0.32 | 0.39 | 0.54 | 0.43 | 0.47 | 0.29 | 0.22 | 0.32 | 0.32 |
| C2 | 0.63 | 0.77 | 0.52 | 0.49 | 0.48 | 0.37 | 0.38 | 0.35 | 0.52 | 0.34 | 0.43 | 0.39 | 0.55 | 0.43 | 0.48 | 0.40 | 0.37 | 0.53 | 0.44 | 0.43 | 0.33 | 0.28 | 0.35 | 0.34 |
| C3 | 0.54 | 0.61 | 0.78 | 0.51 | 0.52 | 0.40 | 0.39 | 0.38 | 0.45 | 0.32 | 0.43 | 0.40 | 0.55 | 0.51 | 0.41 | 0.39 | 0.34 | 0.47 | 0.48 | 0.42 | 0.29 | 0.30 | 0.43 | 0.33 |
| C4 | 0.62 | 0.55 | 0.51 | 0.77 | 0.46 | 0.51 | 0.62 | 0.48 | 0.47 | 0.38 | 0.46 | 0.45 | 0.48 | 0.48 | 0.46 | 0.32 | 0.46 | 0.50 | 0.41 | 0.46 | 0.29 | 0.28 | 0.29 | 0.35 |
| C5 | 0.52 | 0.50 | 0.50 | 0.51 | 0.76 | 0.45 | 0.53 | 0.48 | 0.44 | 0.46 | 0.32 | 0.47 | 0.46 | 0.46 | 0.38 | 0.39 | 0.40 | 0.49 | 0.41 | 0.39 | 0.30 | 0.24 | 0.35 | 0.34 |
| C6 | 0.43 | 0.43 | 0.46 | 0.47 | 0.45 | 0.77 | 0.50 | 0.45 | 0.30 | 0.46 | 0.33 | 0.33 | 0.34 | 0.42 | 0.51 | 0.37 | 0.39 | 0.49 | 0.38 | 0.41 | 0.25 | 0.23 | 0.34 | 0.32 |
| C7 | 0.49 | 0.46 | 0.46 | 0.62 | 0.49 | 0.42 | 0.78 | 0.33 | 0.44 | 0.38 | 0.43 | 0.35 | 0.46 | 0.42 | 0.35 | 0.37 | 0.50 | 0.48 | 0.31 | 0.39 | 0.26 | 0.27 | 0.27 | 0.26 |
| C8 | 0.39 | 0.36 | 0.34 | 0.38 | 0.47 | 0.41 | 0.35 | 0.77 | 0.35 | 0.45 | 0.39 | 0.39 | 0.40 | 0.39 | 0.35 | 0.31 | 0.44 | 0.37 | 0.39 | 0.38 | 0.30 | 0.21 | 0.29 | 0.26 |
| C9 | 0.53 | 0.51 | 0.48 | 0.53 | 0.38 | 0.26 | 0.34 | 0.37 | 0.78 | 0.43 | 0.53 | 0.34 | 0.52 | 0.51 | 0.37 | 0.41 | 0.47 | 0.41 | 0.35 | 0.34 | 0.28 | 0.31 | 0.38 | 0.31 |
| C10 | 0.49 | 0.46 | 0.53 | 0.47 | 0.39 | 0.42 | 0.29 | 0.41 | 0.36 | 0.78 | 0.52 | 0.49 | 0.38 | 0.40 | 0.47 | 0.45 | 0.44 | 0.44 | 0.51 | 0.46 | 0.43 | 0.41 | 0.34 | 0.32 |
| C11 | 0.45 | 0.44 | 0.43 | 0.43 | 0.37 | 0.31 | 0.36 | 0.37 | 0.51 | 0.49 | 0.77 | 0.48 | 0.48 | 0.48 | 0.36 | 0.44 | 0.44 | 0.39 | 0.45 | 0.51 | 0.43 | 0.32 | 0.45 | 0.33 |
| C12 | 0.46 | 0.43 | 0.39 | 0.48 | 0.44 | 0.40 | 0.39 | 0.45 | 0.39 | 0.44 | 0.47 | 0.77 | 0.42 | 0.40 | 0.42 | 0.34 | 0.46 | 0.45 | 0.44 | 0.49 | 0.39 | 0.28 | 0.40 | 0.30 |
| C13 | 0.57 | 0.58 | 0.57 | 0.54 | 0.45 | 0.36 | 0.44 | 0.39 | 0.54 | 0.44 | 0.52 | 0.45 | 0.79 | 0.52 | 0.41 | 0.42 | 0.48 | 0.50 | 0.42 | 0.39 | 0.36 | 0.29 | 0.39 | 0.35 |
| C14 | 0.56 | 0.59 | 0.56 | 0.50 | 0.41 | 0.40 | 0.54 | 0.46 | 0.56 | 0.48 | 0.58 | 0.44 | 0.51 | 0.78 | 0.48 | 0.44 | 0.42 | 0.43 | 0.43 | 0.43 | 0.35 | 0.31 | 0.41 | 0.41 |
| C15 | 0.42 | 0.43 | 0.47 | 0.56 | 0.42 | 0.50 | 0.46 | 0.40 | 0.41 | 0.39 | 0.35 | 0.42 | 0.40 | 0.40 | 0.76 | 0.34 | 0.39 | 0.50 | 0.31 | 0.36 | 0.26 | 0.30 | 0.31 | 0.30 |
| C16 | 0.30 | 0.30 | 0.37 | 0.37 | 0.39 | 0.33 | 0.36 | 0.31 | 0.38 | 0.33 | 0.42 | 0.34 | 0.35 | 0.39 | 0.37 | 0.79 | 0.33 | 0.33 | 0.35 | 0.38 | 0.29 | 0.29 | 0.41 | 0.34 |
| C17 | 0.44 | 0.40 | 0.45 | 0.46 | 0.35 | 0.37 | 0.37 | 0.43 | 0.40 | 0.43 | 0.41 | 0.38 | 0.40 | 0.37 | 0.43 | 0.32 | 0.78 | 0.30 | 0.40 | 0.37 | 0.34 | 0.30 | 0.34 | 0.35 |
| C18 | 0.58 | 0.55 | 0.56 | 0.61 | 0.49 | 0.50 | 0.53 | 0.44 | 0.39 | 0.44 | 0.43 | 0.43 | 0.48 | 0.51 | 0.50 | 0.39 | 0.46 | 0.76 | 0.37 | 0.43 | 0.30 | 0.28 | 0.41 | 0.36 |
| C19 | 0.40 | 0.51 | 0.53 | 0.47 | 0.54 | 0.47 | 0.43 | 0.40 | 0.48 | 0.46 | 0.43 | 0.46 | 0.55 | 0.48 | 0.45 | 0.46 | 0.48 | 0.34 | 0.77 | 0.51 | 0.48 | 0.48 | 0.46 | 0.44 |
| C20 | 0.40 | 0.42 | 0.41 | 0.46 | 0.36 | 0.34 | 0.39 | 0.40 | 0.36 | 0.43 | 0.46 | 0.40 | 0.45 | 0.39 | 0.41 | 0.37 | 0.34 | 0.38 | 0.38 | 0.78 | 0.32 | 0.33 | 0.35 | 0.35 |
| C21 | 0.40 | 0.33 | 0.39 | 0.33 | 0.36 | 0.33 | 0.35 | 0.37 | 0.31 | 0.36 | 0.41 | 0.34 | 0.35 | 0.36 | 0.31 | 0.33 | 0.37 | 0.32 | 0.49 | 0.39 | 0.79 | 0.39 | 0.30 | 0.35 |
| C22 | 0.33 | 0.36 | 0.39 | 0.34 | 0.33 | 0.32 | 0.32 | 0.34 | 0.32 | 0.35 | 0.38 | 0.34 | 0.35 | 0.37 | 0.31 | 0.33 | 0.34 | 0.31 | 0.41 | 0.39 | 0.46 | 0.81 | 0.33 | 0.34 |
| C23 | 0.40 | 0.33 | 0.42 | 0.36 | 0.29 | 0.32 | 0.36 | 0.27 | 0.37 | 0.37 | 0.42 | 0.33 | 0.35 | 0.38 | 0.28 | 0.42 | 0.32 | 0.33 | 0.33 | 0.34 | 0.39 | 0.28 | 0.80 | 0.33 |
| C24 | 0.38 | 0.35 | 0.37 | 0.31 | 0.34 | 0.29 | 0.37 | 0.30 | 0.34 | 0.32 | 0.36 | 0.31 | 0.28 | 0.34 | 0.26 | 0.31 | 0.33 | 0.29 | 0.31 | 0.32 | 0.31 | 0.25 | 0.37 | 0.78 |
Table 8.
Total interrelationship matrix of criteria.
| C1 | C2 | C3 | C4 | C5 | C6 | C7 | C8 | C9 | C10 | C11 | C12 | C13 | C14 | C15 | C16 | C17 | C18 | C19 | C20 | C21 | C22 | C23 | C24 | D | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C1 | 0.41 | 0.39 | 0.39 | 0.39 | 0.35 | 0.32 | 0.34 | 0.32 | 0.35 | 0.32 | 0.35 | 0.32 | 0.37 | 0.36 | 0.33 | 0.30 | 0.33 | 0.35 | 0.33 | 0.34 | 0.27 | 0.24 | 0.29 | 0.27 | 8.02 |
| C2 | 0.40 | 0.40 | 0.38 | 0.38 | 0.35 | 0.31 | 0.34 | 0.31 | 0.35 | 0.32 | 0.35 | 0.32 | 0.37 | 0.35 | 0.33 | 0.31 | 0.33 | 0.35 | 0.33 | 0.34 | 0.27 | 0.24 | 0.29 | 0.27 | 8.02 |
| C3 | 0.39 | 0.39 | 0.41 | 0.39 | 0.35 | 0.32 | 0.34 | 0.32 | 0.35 | 0.32 | 0.35 | 0.32 | 0.37 | 0.36 | 0.33 | 0.31 | 0.33 | 0.35 | 0.34 | 0.34 | 0.27 | 0.24 | 0.30 | 0.27 | 8.07 |
| C4 | 0.41 | 0.40 | 0.40 | 0.42 | 0.36 | 0.34 | 0.37 | 0.34 | 0.36 | 0.34 | 0.37 | 0.34 | 0.38 | 0.37 | 0.35 | 0.31 | 0.35 | 0.36 | 0.34 | 0.35 | 0.28 | 0.25 | 0.30 | 0.28 | 8.36 |
| C5 | 0.39 | 0.38 | 0.38 | 0.38 | 0.37 | 0.32 | 0.35 | 0.33 | 0.34 | 0.33 | 0.34 | 0.33 | 0.36 | 0.35 | 0.32 | 0.31 | 0.33 | 0.35 | 0.33 | 0.33 | 0.27 | 0.24 | 0.29 | 0.27 | 7.98 |
| C6 | 0.35 | 0.35 | 0.35 | 0.36 | 0.32 | 0.33 | 0.32 | 0.30 | 0.31 | 0.31 | 0.32 | 0.30 | 0.33 | 0.33 | 0.32 | 0.29 | 0.31 | 0.33 | 0.30 | 0.31 | 0.25 | 0.22 | 0.27 | 0.25 | 7.43 |
| C7 | 0.37 | 0.36 | 0.36 | 0.38 | 0.33 | 0.30 | 0.36 | 0.30 | 0.33 | 0.31 | 0.33 | 0.30 | 0.34 | 0.33 | 0.31 | 0.29 | 0.32 | 0.33 | 0.30 | 0.32 | 0.25 | 0.23 | 0.27 | 0.25 | 7.58 |
| C8 | 0.33 | 0.32 | 0.32 | 0.32 | 0.30 | 0.28 | 0.29 | 0.31 | 0.29 | 0.29 | 0.30 | 0.28 | 0.31 | 0.30 | 0.28 | 0.26 | 0.29 | 0.29 | 0.28 | 0.29 | 0.23 | 0.20 | 0.25 | 0.23 | 6.87 |
| C9 | 0.37 | 0.37 | 0.36 | 0.37 | 0.33 | 0.29 | 0.32 | 0.30 | 0.36 | 0.32 | 0.35 | 0.30 | 0.35 | 0.35 | 0.31 | 0.30 | 0.32 | 0.33 | 0.31 | 0.32 | 0.26 | 0.24 | 0.29 | 0.26 | 7.66 |
| C10 | 0.39 | 0.38 | 0.39 | 0.38 | 0.34 | 0.32 | 0.33 | 0.32 | 0.34 | 0.36 | 0.36 | 0.33 | 0.35 | 0.35 | 0.34 | 0.32 | 0.34 | 0.35 | 0.34 | 0.34 | 0.28 | 0.26 | 0.30 | 0.27 | 8.06 |
| C11 | 0.37 | 0.37 | 0.37 | 0.37 | 0.33 | 0.30 | 0.33 | 0.31 | 0.35 | 0.33 | 0.38 | 0.33 | 0.36 | 0.35 | 0.32 | 0.31 | 0.33 | 0.33 | 0.33 | 0.34 | 0.28 | 0.24 | 0.30 | 0.27 | 7.90 |
| C12 | 0.37 | 0.36 | 0.36 | 0.37 | 0.33 | 0.31 | 0.33 | 0.32 | 0.33 | 0.32 | 0.34 | 0.35 | 0.35 | 0.34 | 0.32 | 0.30 | 0.33 | 0.33 | 0.32 | 0.33 | 0.27 | 0.23 | 0.29 | 0.26 | 7.77 |
| C13 | 0.41 | 0.41 | 0.41 | 0.41 | 0.36 | 0.33 | 0.36 | 0.33 | 0.37 | 0.35 | 0.38 | 0.34 | 0.41 | 0.38 | 0.35 | 0.33 | 0.35 | 0.37 | 0.34 | 0.35 | 0.29 | 0.25 | 0.31 | 0.29 | 8.47 |
| C14 | 0.42 | 0.41 | 0.42 | 0.41 | 0.37 | 0.34 | 0.38 | 0.35 | 0.38 | 0.36 | 0.39 | 0.35 | 0.39 | 0.41 | 0.36 | 0.34 | 0.36 | 0.37 | 0.35 | 0.36 | 0.29 | 0.26 | 0.32 | 0.30 | 8.69 |
| C15 | 0.35 | 0.35 | 0.35 | 0.36 | 0.32 | 0.31 | 0.32 | 0.30 | 0.32 | 0.31 | 0.32 | 0.30 | 0.33 | 0.33 | 0.34 | 0.28 | 0.31 | 0.33 | 0.30 | 0.31 | 0.25 | 0.23 | 0.27 | 0.25 | 7.43 |
| C16 | 0.30 | 0.30 | 0.31 | 0.31 | 0.29 | 0.26 | 0.28 | 0.26 | 0.28 | 0.27 | 0.29 | 0.27 | 0.29 | 0.29 | 0.27 | 0.30 | 0.27 | 0.28 | 0.27 | 0.28 | 0.23 | 0.20 | 0.25 | 0.23 | 6.59 |
| C17 | 0.34 | 0.33 | 0.34 | 0.34 | 0.30 | 0.28 | 0.30 | 0.29 | 0.31 | 0.30 | 0.32 | 0.29 | 0.32 | 0.31 | 0.30 | 0.27 | 0.33 | 0.30 | 0.30 | 0.30 | 0.25 | 0.22 | 0.27 | 0.25 | 7.19 |
| C18 | 0.41 | 0.40 | 0.41 | 0.41 | 0.37 | 0.34 | 0.37 | 0.34 | 0.36 | 0.35 | 0.37 | 0.34 | 0.38 | 0.38 | 0.35 | 0.32 | 0.35 | 0.39 | 0.34 | 0.35 | 0.28 | 0.25 | 0.32 | 0.29 | 8.48 |
| C19 | 0.40 | 0.40 | 0.41 | 0.41 | 0.38 | 0.34 | 0.36 | 0.34 | 0.37 | 0.36 | 0.37 | 0.35 | 0.39 | 0.38 | 0.35 | 0.34 | 0.36 | 0.36 | 0.38 | 0.37 | 0.30 | 0.28 | 0.32 | 0.30 | 8.63 |
| C20 | 0.34 | 0.34 | 0.34 | 0.35 | 0.31 | 0.29 | 0.31 | 0.29 | 0.31 | 0.30 | 0.32 | 0.30 | 0.33 | 0.32 | 0.30 | 0.28 | 0.30 | 0.31 | 0.30 | 0.34 | 0.25 | 0.23 | 0.27 | 0.25 | 7.28 |
| C21 | 0.32 | 0.31 | 0.32 | 0.31 | 0.29 | 0.27 | 0.28 | 0.27 | 0.28 | 0.28 | 0.30 | 0.27 | 0.30 | 0.30 | 0.27 | 0.26 | 0.28 | 0.28 | 0.29 | 0.29 | 0.28 | 0.22 | 0.25 | 0.24 | 6.75 |
| C22 | 0.31 | 0.31 | 0.31 | 0.31 | 0.28 | 0.26 | 0.28 | 0.26 | 0.28 | 0.27 | 0.29 | 0.27 | 0.29 | 0.29 | 0.27 | 0.25 | 0.27 | 0.28 | 0.28 | 0.28 | 0.24 | 0.25 | 0.25 | 0.23 | 6.60 |
| C23 | 0.31 | 0.30 | 0.31 | 0.31 | 0.28 | 0.26 | 0.28 | 0.26 | 0.28 | 0.27 | 0.29 | 0.26 | 0.29 | 0.29 | 0.26 | 0.26 | 0.27 | 0.28 | 0.27 | 0.28 | 0.23 | 0.20 | 0.29 | 0.23 | 6.58 |
| C24 | 0.29 | 0.28 | 0.29 | 0.28 | 0.26 | 0.24 | 0.26 | 0.24 | 0.26 | 0.25 | 0.27 | 0.25 | 0.27 | 0.27 | 0.24 | 0.24 | 0.25 | 0.26 | 0.25 | 0.25 | 0.21 | 0.19 | 0.23 | 0.25 | 6.08 |
| R | 8.76 | 8.61 | 8.69 | 8.74 | 7.87 | 7.27 | 7.78 | 7.32 | 7.88 | 7.56 | 8.05 | 7.41 | 8.22 | 8.07 | 7.53 | 7.07 | 7.62 | 7.84 | 7.49 | 7.71 | 6.28 | 5.62 | 6.80 | 6.28 | 0.32 |
Fig. 3.
Smart PSS criteria in the healthcare industry.
5. Implications
This section discusses the theoretical implications of smart PSSs and the managerial implications for the healthcare industry, and it proposes guidelines for smart PSS implementation and success.
5.1. Theoretical implications
Smart PSSs build in the integration of digital services and products to offer a unique solution in the market. This study identified five underlying aspects of smart PSS development: digital health services, intelligent connected products, stakeholder communication, environmental benefits and use schemes. Intelligent connected products and stakeholder communication are the drivers for implementing other aspects in smart PSSs. The data collected by intelligent devices are vital for value creation and evaluating the design of analytic tools [40]. Stakeholder communication can play a driving role in supporting digitalized and personalized health services. It allows a real-time reflection of the physical world in a virtual world, the historical data flow, and the self-assessment and evolution of the system [21].
Intelligent connected products provide the infrastructure to build new services and enhance stakeholder communication. The results suggest that intelligent connected products are drivers of the whole smart system, and previous studies highlight their role through digital transformation that could drive the system with proper skills or create barriers due to the lack of technology infrastructure, digital skills, and software management [6,17]. Digital health services correlate with new technologies to collect and process information, using the Internet of Things, big data, and artificial intelligence to gain knowledge about the user and the environment. Similarly, they provide feedback and are the medium of communication across different stakeholders and devices [22,30,45]. These products allow data acquisition, storage, processing, transfer, and integration and use analytics tools to provide knowledge. The degree of smartness is directly correlated with intelligent connected products and their operation, increasing responsiveness and collaboration [31,43]. The adoption of intelligent connected products drives digital health services. Investing in technological infrastructure and embracing advanced technologies foster personalized health service innovation. However, gaps remain, especially among elderly individuals, low-income families and the rural population, and they need to be addressed by the government in collaboration with private enterprises and related stakeholders [4,7,36]. Smart PSS providers must foster the integration and adoption of new technology; national policies and communication infrastructure are needed to increase the accessibility and use of smart products.
This study pointed out that stakeholder communication is a driver of intelligent connected products and personalized health services. Similarly, previous studies have mentioned that collaboration drives information flow and knowledge management, guiding the required data collection and processing from intelligent collected products [35]. Stakeholder communication highlights the information exchange role in smart PSS development, increasing interconnectivity among diverse stakeholders through new technologies. Therefore, communication is key to strengthening customer relations, generating new revenue streams and increasing competitiveness [33]. Stakeholder communication focuses on individual inclusion, increasing participation and collaboration through information exchange and high communication capabilities [22,34]. Interorganizational networks between customers and suppliers create uncertainties and different organizational settings for data exchange [23]. Communication requirements have been drivers of the development of new technologies since the beginning of humankind; however, in the modern era, complex and new requirements supersede the previous implementation. Hence, real-time communication and customers’ needs for predictive analysis drive the development of intelligent connected products. In addition, adequate and precise communication may produce new requirements for value creation, highlighting personalized health services and digital platforms.
Environmental benefits are a consequence of bundling intelligent connected products and digital services. Intelligent connected products collect and analyze information to predict effective and resource-efficient mechanisms to reduce the amount of waste created. Digital services provide new alternatives to reusing and sharing products by digital platforms. In addition, they aid in the dematerialization process by integrating digital services that also reduce fuel consumption and reduce greenhouse gas emissions because stakeholders do not need to physically travel to the supplier. Environmental benefits focus on sustainable production and consumption and include new use schemes and services to promote dematerialization. Environmental benefits have been previously mentioned as an effect of PSS development [35,49,50]. Smart PSSs have a context-awareness feature driven by smart technology that is able to collect and analyze environmental data and material-device data, producing a proactive system using the information to automatically take action and inform and organize other network systems [23]. Environmental benefits are one of the advantages of smart PSS implementation. They are vital for creating a more sustainable business model in circular economies to mitigate the greenhouse effect and global warming.
This study pointed out that the use scheme is a consequence of intelligent connected products in smart PSSs, providing alternative and supporting services to traditional offerings, such as services for managing data and notifying customers about the status of a shared product. Consumers have increased their consumption and acquisition of goods to fulfill their desires; however, this practice is not sustainable and leads to a large amount of garbage. Therefore, the alternative to this consumption pattern is a change in consumer behavior to a more sustainable manner, such as renting or the sharing economy. In recent decades, many examples have been observed in the clothing and car sectors, where ownership remains with the provider and the consumer uses the goods temporarily, achieving needs satisfaction and achieving the desired results [19,33]. Smart PSSs change the ownership paradigm in relation to new use schemes. Service platforms deliver accessibility to customers without the burdens of ownership, such as increased funding, infrastructure, maintenance, and repair, and they provide flexibility to meet user needs as they change over time.
5.2. Managerial implications
This study finds that managing data (C5), multifunctionality (C10), data reliability (C13), interoperability (C14), patient communication (C18) and resource efficiency (C19) are the driving criteria for smart PSS success.
Managing data (C5) refers to the storage, organization and retrieval of information to use it to interpret and make a decision. The acquired data can be converted into valuable knowledge and meaningful suggestions by employing advanced computer technologies and data analytics. In the healthcare industry, storing data in historical medical records has been a basic procedure, as it allows the access, storage, and organization of patient information. Electronic healthcare records (EHRs) have been widely implemented in developed countries, allowing physicians or patients across the territory and medical institutions to check EHRs. This data management system has been scarcely successful in developing countries due to their healthcare and network infrastructure, lack of training, poverty, lack of funds, lack of basic education, and organizational and political issues. Consequently, to increase data management systems, it is necessary to overcome the previously mentioned barriers in a national context. Private and public sector integration is necessary to store and retrieve the most complete and accurate patient information. In addition, managing data systems may take a long time to be fully implemented; thus, adequate strategies are needed to mitigate implementation errors and delays. Finally, workforce development with an interdisciplinary team requires leadership and informatics training for physicians and healthcare-related workers who promote data management and assist in problems and questions.
Interoperability (C14) uses standards that allow data transferability across multiple organizations and system settings to maintain the entire content of data and correctly interpret the information. Smart PSSs necessitate the integration of smart data capabilities with important user actions. The high data velocity yields concrete results for healthcare firms that use data-driven decision-making. Interoperability allows the exchange of information across multiple devices, organizations, physicians, and patients, reducing costs and aiding in upgrades and data transferability. Interoperability is essential for smart PSSs, helping to guarantee data exchange, increase stakeholder communication, facilitate data access, and improve the workflow speed of processes such as diagnosis and treatment. Interoperability must be considered from the beginning of service digitalization and when viewing current partners and possible futures partners. Reduced data friction enables physicians to identify and address patient issues more effectively. The data friction solution should be easily integrated with third-party analytics tools to enhance insight delivery. Hence, guidelines for user data collection must be provided; for example, when taking a picture of a wound, the lighting, background, and written information content must comply with the guidelines provided, creating a photo standard that facilitates interpretation. Consequently, in low-resource settings, smartphones can provide a bridge between the public and private sectors and support access to information by healthcare professionals and patients.
Multifunctionality (C10) refers to the ability to perform various activities in one device supporting a smart PSS value proposition. Various functions in one device fulfill the changing needs of users by applying new technologies that can recognize or predict behaviors and provide complementary services and new product integrated functions. Cost reduction is one of the main advantages of multifunctionality. Previously, the use of different devices dedicated to performing a unique activity was necessary, increasing acquisition costs and production costs. Multifunctionality is driven by the development of technologies that have reduced the size and weight of electronic components such as microchips and the development of nanotechnology to nano circuits, further reducing the size of electronic components. The size reduction allows the bundling of different devices performing different operations, such as smartphones, where the user can take pictures and send videos. In addition, complementary devices can be multifunctional, such as intelligent electronic devices that detect, analyze, and communicate data about, for example, body signals such as vital signs and/or environmental data, and that provide instantaneous biofeedback to the wearer in some situations. To achieve multifunctionality in the healthcare industry, it is necessary to adopt new technologies and provide training to achieve high digital literacy levels to use all the available functions on the devices. Artificial intelligence and digital training by smart PSS providers can aid and educate patients and physicians in the use of multiple functions and benefits to enhance customer satisfaction.
Data reliability (C13) is the accuracy and completeness of the data collected and provided by the patient and healthcare professional. Data processing technologies are highly dependent on the accuracy and precision of the data, as the results will directly correlate to the input. The reliability of measures can be achieved by calibrating devices and regularly controlling and comparing the data collected with standards; for example, monitoring devices that are leased for a period of time can be verified every three to six months by the provider. Instrumental verification is easy when the provider is the owner of the product. However, instrumental verification seems almost impossible in smartphones and other related devices due to cost and the lack of awareness; hence, smartphone data can be handled as slightly informative and complementary, remembering the probability of inaccuracy due to the lack of proper control and verification. Healthcare requires ensuring data reliability, as patients' lives depend on the accuracy of the data obtained. In the case of self-reported data, as usually happens in patient reports about a past event, such data can be biased due to patients’ detailed memory of facts as well as their unwillingness to share private information. The use of digital devices and trackers can increase the reliability of the data reported by patients. To increase data reliability, the accessibility of users drives the engagement in tracking. Trust can play a vital role, as concerns about privacy and security have emerged over the past few years; therefore, trust can help improve data reporting. In addition, patient engagement provides more accurate information due to the increased motivation to report data and control other physiological measures.
Patient communication (C18) is the communication between the patient and the physician or healthcare professional. Stakeholder communication can create inclusion and empower patients in a collaborative approach with the physician for disease treatment. Patient communication can be achieved through the feasibility of sharing information with the physician, connectivity, physician availability, and empathy. The feasibility of sharing information relates to the platform or app that uses the patient to contact the healthcare professional, which allows easy connection between the patient and practitioner. Technologies with a high data velocity influence connectivity and data transmission. In addition, in video conferences, it is necessary to maintain proper virtual etiquette, such as turning off the microphone when another person is speaking to reduce echo. Physician availability can be addressed by a group of professionals with different shifts or the inclusion of physicians in other countries in different time zones, increasing the available time from 8 h to 24 h a day of physician availability. In addition to smart PSSs offering digital services, the direct communication between human beings will remain longer. The practitioner needs to be empathic toward the patient to increase confidence and share the information needed for the diagnosis to improve patient communication.
Resource efficiency (C19) refers to reducing consumption in product manufacturing and the provision of services, providing a workflow with minimal consumption and reducing the production of waste. Resource efficiency can be driven by sustainable production policies, consumption patterns, and technology to measure and analyze lifecycle and product system substitutions. Sustainable production policies focus on the consequences of manufacturing products and integrate a holistic view of inputs and outputs across the operational process and consequences for the environment. Sustainable production policies aim to seek material substitution, changes and the efficiency of operational processes, as well as end-of-pipe solutions. However, sustainable production practices will become useless in the face of increased consumption behavior; for example, more intensive purchasing and use of products will produce more waste over time. Smart PSSs are able to collect information about their customers' product consumption using digital technologies and then use these data to better understand their preferences for products and services. This approach contributes to the development of more appealing goods and services, such as those that incorporate customer-driven product design, individualized maintenance, and product lifecycle management. Additionally, smart products can analyze the status of the device and complementary devices to make preventive maintenance increase the product lifespan and reduce waste.
6. Conclusion
New technical paradigms are causing a fundamental change in the healthcare sector, which has begun a gradual shift to digital service provision. Smart PSSs combine intelligent products, such as wearable devices or even implantable technologies, and digital services, such as video consulting, EHRs, and clinical decision support systems. However, healthcare institutions have focused on the required technology without considering how stakeholder communication and intelligent connected products affect the adoption of digital and personalized services. The COVID-19 pandemic has made patients and physicians temporarily adopt digital health to maintain a distance between individuals, modifying the existing interaction between patients and practitioners. The period during which the study took place was at the height of the pandemic, allowing us to identify which criteria are critical for the success of smart PSSs.
The proposed attributes were obtained by EFA and the FDEMATEL in the Ecuadorian healthcare industry. EFAs grouped the 25 validated criteria into five aspects: intelligent connected products, stakeholder communication, environmental benefits and use schemes. Fuzzy theory converted linguistic preferences into quantifiable values, and the FDEMATEL showed the interrelationships among aspects and criteria based on driving power and dependence.
The smart PSS hierarchical model is provided, which adds to the current body of knowledge by identifying the driving attributes for achieving digital health service adoption. The results indicate that the valid hierarchical model consists of five dimensions and 22 criteria. The causal aspects are intelligent connected products and stakeholder communication. The effect group is found to be use schemes and environmental benefits, especially for technology integration through intelligent connected products. Stakeholder communication influences intelligent connected products and digital health services, taking into account the unique transmission and exchange data requirements of different stakeholders and promoting inclusion through transparent, open, and responsive dialog. Intelligent connected products drive digital health services, use schemes and environmental benefits. The potentiality of data acquisition, processing and predictive analysis allows the prediction and fulfillment of future needs, providing personalized health services that increase customer satisfaction and loyalty. Environmental benefits are a consequence of the implementation of smart technologies in capturing and analyzing material data and consumption behavior to provide alternatives to consumption and increasing environmental practices through efficiency in operational production and service provision. The use scheme is a consequence of the integration of smart intelligent connected products that allow the proposition of new use schemes such as sharing to reduce costs and promote dematerialization.
The causal criteria evaluated from the proposed model were managing data, multifunctionality, data reliability, interoperability, patient communication and resource efficiency. Managing data was related to the system to manage data acquisition and the transmission and retrieval of information, for example, the integration of EHRs into the development of smart PSSs where patients and physicians can have comprehensive access to medical data through different devices and networks. Multifunctionality is an added value function of smart PSSs through the implementation of different functions in one product. Data reliability depends on the accuracy of the data provided by the patient and collected by monitoring devices to reduce the bias in self-reported information, and it is important for building trust, accessibility, engagement with products and easy-to-enter formats. The monitoring devices that are being shared among patients need to comply with instrumental verification to ensure the quality of measures. Interoperability allows information transmission and access among different platforms in interorganizational networks, and the use of standards and guidelines provides a uniform data entry that allows proper interpretation. Patient communication is critical for the development of collaboration across the patient and practitioner, taking into account connectivity and building trust in healthcare service provision through the use of empathy on the part of the professional. Finally, resource efficiency is linked to the use of technology to collect and analyze resource workflows, and it increases the lifespan due to proper preventive maintenance and efficient end-of life recycling for remanufacturing.
The results contribute to the smart PSS literature and the healthcare industry; however, the study presents some limitations. One of the limitations is that the samples need more heterogeneity and that there should be a higher number of samples to be correlated with a national territorial model. The majority of respondents lived in urban areas and had access to the internet. In addition, further validation and a deep sociodemographic analysis are needed, as income, age and other variables can become barriers to the adoption of smart PSSs in healthcare. Finally, a cross-sectional approach was used in this study; the use of longitudinal studies may inform the evolution of smart PSSs in developing countries and provide guidelines for other countries’ adoption of smart PSSs.
Author contribution statement
Yeneneh Tamirat Negash: Conceived and designed the analysis; Analyzed and interpreted the data; Contributed analysis tools or data; Wrote the paper.
Liria Salome Calahorrano Sarmiento: Analyzed and interpreted the data; Contributed analysis tools or data; Wrote the paper.
Funding statement
Dr. Yeneneh Tamirat Negash was supported by National Science and Technology Council in Taiwan [111-2221-E-468 -009 -MY3].
Data availability statement
Data will be made available on request.
Declaration of interest's statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.heliyon.2023.e13137.
Contributor Information
Yeneneh Tamirat Negash, Email: yeneneh@asia.edu.tw, yenuta@gmail.com.
Liria Salome Calahorrano Sarmiento, Email: liria.calahorrano@gmail.com.
Appendix 1. List of the proposed criteria and supporting literature for smart PSS evaluation
| Criteria | Supporting literature |
|---|---|
| Adaptability | [12,17,22,45,48] |
| Additional support | [9,12,31,45] |
| Data collection | [12,37,45] |
| Data management | [12,18,45,55] |
| Data processing | [12,17,31,43,45] |
| Data reliability | [12,17,22,45,48] |
| Device autonomy | [17,48] |
| Device cooperation | [36,56] |
| Personalized care | [9,12,22,31,45] |
| Digital interface | [9,12,22,31,45] |
| Digital user identity | [10,12,16,17,31] |
| End-of-life recycling | [28,33] |
| Reactivity | [12,17,22,45,48] |
| Health knowledge notification | [9,12,22,31,40,45] |
| Human-like interaction | [12,17,22,40,45,48] |
| Individual empowerment | [12,17,31,43,45] |
| Information access | [12,20] |
| Security configuration | [17,21,30,36,38,45,48] |
| Interoperability | [12,20,36,55] |
| Interprofessional collaboration | [13] |
| Multifunctionality | [12,17,22,40,45,48] |
| Patient communication | [13,48] |
| Patient tracking | [12,17,31,43,45] |
| Reduce gas emission | [1,28,50] |
| Resource efficiency | [19,28,30,31,33] |
| Service platforms | [9,12,31,45] |
| Shared use | [12,31,39,46,47] |
| Social media | [12,20,25,42] |
| Task reduction | [12,17,31,43,45] |
Appendix 2. Fuzzy set matrix of respondent 1
Appendix 3. Defuzzified matrix of respondent 1
Appendix D. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Gogia S.B. Academic Press; 2019. Fundamentals of Telemedicine and Telehealth. [Google Scholar]
- 2.Zhou T., et al. An integrated framework of user experience-oriented smart service requirement analysis for smart product service system development. Adv. Eng. Inf. 2022;51 [Google Scholar]
- 3.Barney A., et al. The COVID-19 pandemic and rapid implementation of adolescent and young adult telemedicine: challenges and opportunities for innovation. J. Adolesc. Health. 2020;67(2):164–171. doi: 10.1016/j.jadohealth.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cepal N. 2020. Las oportunidades de la digitalización en América Latina frente al Covid-19. [Google Scholar]
- 5.North S. Telemedicine in the time of COVID and beyond. J. Adolesc. Health. 2020;67(2):145–146. doi: 10.1016/j.jadohealth.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meskó B., et al. Digital Health Is a Cultural transformation of traditional Healthcare. Mhealth. 2017;3 doi: 10.21037/mhealth.2017.08.07. 38–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlo L., et al. Proceedings of the 2020 International Conference on Information and Communication Technologies and Development. ACM; New York, NY, USA: 2020. Healthcare infrastructures in Ecuador: challenges, reflections and opportunities for digital health. [Google Scholar]
- 8.Cruz-Cárdenas J., et al. Drivers of technology readiness and motivations for consumption in explaining the tendency of consumers to use technology-based services. J. Bus. Res. 2021;122:217–225. [Google Scholar]
- 9.Frank A.G., et al. Servitization and Industry 4.0 convergence in the digital transformation of product firms: a business model innovation perspective. Technol. Forecast. Soc. Change. 2019;141:341–351. [Google Scholar]
- 10.Jia G., et al. A synthetical development approach for rehabilitation assistive smart product–service systems: a case study. Adv. Eng. Inf. 2021;48 [Google Scholar]
- 11.Bu L., et al. A user-centric design approach for smart product-service systems using virtual reality: a case study. J. Clean. Prod. 2021;280 [Google Scholar]
- 12.Valencia A., et al. The design of smart product-service systems (PSSs): an exploration of design characteristics. Int. J. Des. 2015;9(1):13–28. [Google Scholar]
- 13.Fénélon-Dimanche R., et al. Development of an electronic tool (e-AdPharm) to address unmet needs and barriers of community pharmacists to provide medication adherence support to patients. Res. Soc. Adm. Pharm. 2021;17(3):506–513. doi: 10.1016/j.sapharm.2020.04.022. [DOI] [PubMed] [Google Scholar]
- 14.Hindi A.M., Schafheutle E.I., Jacobs S. Community pharmacy integration within the primary care pathway for people with long-term conditions: a focus group study of patients', pharmacists' and GPs' experiences and expectations. BMC Fam. Pract. 2019;20(1):1–15. doi: 10.1186/s12875-019-0912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Association g. GSMA HEAD OFFICE; 2020. The Mobile Economy 2020. [Google Scholar]
- 16.Calvillo-Arbizu J., et al. User-centred design for developing e-Health system for renal patients at home (AppNephro) Int. J. Med. Inf. 2019;125:47–54. doi: 10.1016/j.ijmedinf.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 17.Chang D., et al. A user-centric smart product-service system development approach: a case study on medication management for the elderly. Adv. Eng. Inf. 2019;42 [Google Scholar]
- 18.Song W., Niu Z., Zheng P. Design concept evaluation of smart product-service systems considering sustainability: an integrated method. Comput. Ind. Eng. 2021;159 [Google Scholar]
- 19.Alcayaga A., Wiener M., Hansen E.G. Towards a framework of smart-circular systems: an integrative literature review. J. Clean. Prod. 2019;221:622–634. [Google Scholar]
- 20.Liu L., Song W., Han W. How sustainable is smart PSS? An integrated evaluation approach based on rough BWM and TODIM. Adv. Eng. Inf. 2020;43 [Google Scholar]
- 21.Wu C., et al. A function-oriented optimising approach for smart product service systems at the conceptual design stage: a perspective from the digital twin framework. J. Clean. Prod. 2021;297 [Google Scholar]
- 22.Zheng P., et al. A survey of smart product-service systems: key aspects, challenges and future perspectives. Adv. Eng. Inf. 2019;42 [Google Scholar]
- 23.Kropp E., Totzek D. How institutional pressures and systems characteristics shape customer acceptance of smart product-service systems. Ind. Market. Manag. 2020;91:468–482. [Google Scholar]
- 24.Pierce W., Schroeder D., Suchecki R. Telehealth in Latin America: progress, challenges, and opportunities in the face of COVID-19. Telehealth Med. Today. 2021;6(1):1–8. [Google Scholar]
- 25.Henkens B., Verleye K., Lariviére B. The smarter, the better?! Customer well-being, engagement, and perceptions in smart service systems. Int. J. Res. Market. 2021;38(2):425–447. [Google Scholar]
- 26.Higuchi A., Maehara R. A factor-cluster analysis profile of consumers. J. Bus. Res. 2021;123:70–78. [Google Scholar]
- 27.Negash Y.T., Filketu S.A. A hierarchical framework for the transition to sustainable manufacturing practices: technical and social developments drive eco-friendly tanning in Ethiopia. J. Clean. Prod. 2022;368 [Google Scholar]
- 28.Tseng M.-L., et al. A causal sustainable product-service system using hierarchical structure with linguistic preferences in the Ecuadorian construction industry. J. Clean. Prod. 2019;230:477–487. [Google Scholar]
- 29.Du Y.-W., Li X.-X. Hierarchical DEMATEL method for complex systems. Expert Syst. Appl. 2021;167 [Google Scholar]
- 30.Ardolino M., et al. The role of digital technologies for the service transformation of industrial companies. Int. J. Prod. Res. 2018;56(6):2116–2132. [Google Scholar]
- 31.Chen Z., et al. Explore and evaluate innovative value propositions for smart product service system: a novel graphics-based rough-fuzzy DEMATEL method. J. Clean. Prod. 2020;243 [Google Scholar]
- 32.Wang Z., et al. A design method for an intelligent manufacturing and service system for rehabilitation assistive devices and special groups. Adv. Eng. Inf. 2022;51 [Google Scholar]
- 33.Bressanelli G., et al. Exploring how usage-focused business models enable circular economy through digital technologies. Sustainability. 2018;10(3):639. [Google Scholar]
- 34.Li X., et al. A data-driven reversible framework for achieving Sustainable Smart product-service systems. J. Clean. Prod. 2021;279 [Google Scholar]
- 35.Tseng M.-L., et al. Smart product service system hierarchical model in banking industry under uncertainties. Int. J. Prod. Econ. 2021;240 [Google Scholar]
- 36.Aceto G., Persico V., Pescapé A. Industry 4.0 and health: internet of things, big data, and cloud computing for healthcare 4.0. Journal of Industrial Information Integration. 2020;18 [Google Scholar]
- 37.Senbekov M., et al. The recent progress and applications of digital technologies in healthcare: a review. Int. J. Telemed. Appl. 2020 doi: 10.1155/2020/8830200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hiekata K. Transdisciplinary Engineering for Complex Socio-Technical Systems: Proceedings of the 26th ISTE International Conference on Transdisciplinary Engineering. IOS Press; 2019. Smart product-service systems: a novel transdisciplinary sociotechnical paradigm. [Google Scholar]
- 39.Periyaswamy T., Balasubramanian M. Ambulatory cardiac bio-signals: from mirage to clinical reality through a decade of progress. Int. J. Med. Inf. 2019;130 doi: 10.1016/j.ijmedinf.2019.07.007. [DOI] [PubMed] [Google Scholar]
- 40.Zheng P., et al. A systematic design approach for service innovation of smart product-service systems. J. Clean. Prod. 2018;201:657–667. [Google Scholar]
- 41.Parimbelli E., et al. Trusting telemedicine: a discussion on risks, safety, legal implications and liability of involved stakeholders. Int. J. Med. Inf. 2018;112:90–98. doi: 10.1016/j.ijmedinf.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 42.Odeh R., et al. Caring for a child with type 1 diabetes during COVID-19 lockdown in a developing country: challenges and parents' perspectives on the use of telemedicine. Diabetes Res. Clin. Pract. 2020;168 doi: 10.1016/j.diabres.2020.108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Phillips S.A., et al. Advances in health technology use and implementation in the era of healthy living: implications for precision medicine. Prog. Cardiovasc. Dis. 2019;62(1):44–49. doi: 10.1016/j.pcad.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 44.Matricardi P.M., et al. The role of mobile health technologies in allergy care: an EAACI position paper. Allergy. 2020;75(2):259–272. doi: 10.1111/all.13953. [DOI] [PubMed] [Google Scholar]
- 45.Tunn V., et al. Digitalised product-service systems: effects on consumers' attitudes and experiences. Resour. Conserv. Recycl. 2020;162 [Google Scholar]
- 46.Akhmedova A., Marimon F., Mas-Machuca M. Winning strategies for customer loyalty in the sharing economy: a mixed-methods study. J. Bus. Res. 2020;112:33–44. [Google Scholar]
- 47.Jang K.K., Bae J., Kim K.H. Servitization experience measurement and the effect of servitization experience on brand resonance and customer retention. J. Bus. Res. 2021;130:384–397. [Google Scholar]
- 48.Cherry C.E., Pidgeon N.F. Why is ownership an issue? Exploring factors that determine public acceptance of product-service systems. Sustainability. 2018;10(7):2289. [Google Scholar]
- 49.Haber N., Fargnoli M. Sustainable product-service systems customization: a case study research in the medical equipment sector. Sustainability. 2021;13(12):6624. [Google Scholar]
- 50.Negash Y.T., et al. Sustainable product-service system hierarchical framework under uncertainties: the pharmaceutical industry in Ecuador. J. Clean. Prod. 2021;294 [Google Scholar]
- 51.Zhang X., et al. Prioritizing and aggregating interacting requirements for product-service system development. Expert Syst. Appl. 2021;185 [Google Scholar]
- 52.Flores-Vaquero P., et al. A product-service system approach to telehealth application design. Health Inf. J. 2016;22(2):321–332. doi: 10.1177/1460458214558313. [DOI] [PubMed] [Google Scholar]
- 53.Alava J.J., Guevara A. A critical narrative of Ecuador's preparedness and response to the COVID-19 pandemic. Public Health Pract. 2021;2 doi: 10.1016/j.puhip.2021.100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Molina G.A., et al. COVID-19 in Ecuador, how the pandemic strained the surgical healthcare systems over the edge. Int. J. Surg. Open. 2020;26:106. doi: 10.1016/j.ijso.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kruse C.S., et al. The use of electronic health records to support population health: a systematic review of the literature. J. Med. Syst. 2018;42(11):1–16. doi: 10.1007/s10916-018-1075-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meneghello F., et al. IoT: internet of threats? A survey of practical security vulnerabilities in real IoT devices. IEEE Internet Things J. 2019;6(5):8182–8201. [Google Scholar]
- 57.Abdel-Basst M., Mohamed R., Elhoseny M. A novel framework to evaluate innovation value proposition for smart product–service systems. Environ. Technol. Innovat. 2020;20 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.