ABSTRACT
Background
Parent training (PT) is a promising support for improving parents’ mental health, and behavior in children with autism spectrum disorders (ASD). In recent years, there has been an increase in online PT studies. We developed a prototype for the on-demand PT. In this study, we examined changes in the program implementation, accomplishment of homework, parents’ mental health, and behavior of children among parents of children with ASD.
Methods
This study participated two mothers of children with ASD. The first was the mother of a child aged three years and eight months with ASD and intellectual disability; the second was the mother of a child aged four years and 5 months who had a diagnosis of ASD. An on-demand PT consisting of six sessions was provided online. The program was structured so that the participants watched lecture videos for each session, answered a confirmation test, and submitted homework to advance to the next session. Feedback for the submitted homework and questions was provided via email by the researchers.
Results
Both participants watched the program on a schedule for all sessions and submitted all tests and homework assignments. The percentage of correct responses to the tests per session was 100% for both participants. Two of the four target behaviors of the children changed significantly. Pre- and post-questionnaires also showed improvements in the scores of parental depression and parenting stress, as well as overall behavior of the child.
Conclusion
The program in this study was developed as a prototype for on-demand PT, and two case studies showed positive results. Although this program was on-demand, changes in parent and child behaviors were confirmed by the scale and actual behavior records. Further demonstration is needed to increase the number of cases and to compare the results between the groups.
Keywords: applied behavior analysis, autism spectrum disorder, internet, parent
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication and the presence of restricted interests and repetitive behaviors.1 In individuals with ASDs, “challenging behaviors” that make their daily activities and social participation difficult, such as self-injurious, aggressive/disruptive, and/or stereotypical behavior, have been noted to be common, with prevalence rates estimated at 56–94%.2 These challenging behaviors are seen from early childhood, often become severe, and persist into adulthood, pointing to the need for early intervention.3
Parents of children with ASD face many potential challenges and daily stress related to parenting, including challenging behaviors. Parents of children with ASD have been noted to have a higher risk of stress compared to parents of children with typical development, and parents of children with non-ASD psychiatric disorders.4 Parents of children with ASD have also been shown to be at a higher risk of developing psychological symptoms such as depression and anxiety.5
Parent training (PT) is a promising form of support for improving parents’ mental health and behavior of children with ASD and those who are developmentally disabled.6 In this regard, many systematic reviews have provided evidence for improved parental mental health7 and child behavior.8 Recently, internet-based PT has been gaining popularity as face-to-face PT has become more difficult due to the COVID-19 pandemic. A review of PT by telehealth points to its effectiveness and the need for further research.9, 10
Several types of internet-based PT exist, the major categories of which are on-demand and real-time.11 The on-demand type uses materials posted on the web and allows participants to progress at their own pace.12 In contrast, in case of the real-time PT, lectures and exercises are delivered in real-time using internet video communication technology, and participants attend them at a particular time.13 Along with program effectiveness, these previous studies have also discussed the ease of participation and operational efficiency of program delivery methods.
The knowledge of how to interact with children based on applied behavior analysis (ABA) is useful for parents,14 and consequently, many PTs incorporate techniques and knowledge based on ABA.15 Inoue, Tatsumi, and Fukuzaki11 examined the effects of an Internet-based parent education program for parents of children with ASD on child behavior change in ABA-based behavioral principles on parents’ mental health. The short-term on-demand program consisted of nine 15-minute sessions and lasted one month. The results showed that 21 participants showed improvement in their knowledge of ABA, mental health (anxiety), and mood modulation. This short-term, on-demand type program had a very low withdrawal rate of 12%, And the participants had a high level of satisfaction with the program.
However, the study was a parent education program and did not provide sufficient data to record or improve children’s targeted behavior at home. As the need for early intervention for challenging behaviors has been highlighted, ABA-based PT is considered a promising method. ABA-based functional training identifies the functions of challenging behaviors and teaches equivalent appropriate communication. A large body of evidence supports its efficacy in ASD. The effectiveness of a parent-mediated ABA-based treatment system using functional communication training to challenging behaviors through telehealth has been reported,16 but there are many barriers in implementing this system with the current Japanese resources, including the number of specialized ABA institutions, collaboration with medical care, and the telemedicine system.
In this study, we developed a prototype of an effective on-demand PT program by expanding on the program of Inoue et al.11 and incorporating the treatment of relatively mild challenging behaviors into it. We then analyzed how the program changes the participants’ mental health and the targeted and non-targeted behavior of the children through case studies. The implementation potential of this program was also discussed based on an analysis of questionnaires regarding the number of interactions with staff and social acceptance of the program.
MATERIALS AND METHODS
Participants
A flyer was distributed to Kindergarten A’s parents to recruit participants. The flyer included a brief description of PT, its purpose, expected effects, and the content of each session. The conditions for participation were as follows: (i) parents of preschool children with a diagnosis or suspicion of ASD, (ii) difficulties due to mild behavioral problems such as hyperactivity or impulsivity, and (iii) access to the internet at home.
Prospective participants signed up using the entry form at the URL provided on the flyer. Explanation and consent for participation in the study were provided in writing via e-mail. Both participants who met the criteria applied were mothers. P1 was 36 years old and had a family of four: a husband and two children (C1 and his older brother). Her educational background was a junior college degree, and she viewed this program on her smartphone. C1 was a boy aged three years and eight months who was diagnosed with ASD at three years and four months of age. He had no speech and was intellectually delayed. He was in an included kindergarten class, and his parents’ chief complaints before the start of PT were lack of speech, aggression, obsession, inattention, and irritability.
P2 was a 36-year-old mother with a family of five: a husband and three children (two girls and C2). Her educational background was a college graduate degree; P2 took the course on her computer. C2 was a boy aged four years and five months who was diagnosed with ASD at the age of four years and two months after his preschool indicated group maladjustment, leading to a medical visit. He was in an inclusive kindergarten class; chief parental complaints before PT initiation were self-injurious behavior, inattention, obsession, and anxiety. Both P1 and P2 had Wi-Fi access in their homes, and the viewing process went smoothly. The two children were not on medication.
Content of parent training program
This study developed the program shown in Table 1 with reference to Inoue et al.11 The PT consisted of six web-based sessions. Each session consisted of (i) a review test of the previous session, (ii) a lecture video, (iii) a confirmation test (review test of the lecture content), and (iv) a homework assignment related to the theme of that session. The entire duration of this PT program was nine weeks. Each session was designed to take 15 minutes to complete and was offered at a gap of two weeks, except between Session 1 and 2, which were presented during the first week, and the participants were expected to attend the lectures during this time. The next week was the homework period for Session 2. Next, Session 3 was offered for one week, and the next week was used for homework for this session.
Table 1. Program contents and homework.
| Session | Topic | Contents | Homework |
| 1 | Orientation | What is parent training? | Make a list of your child’s favorite things and activities (submit by e-mail). |
| 2 | Behavior | Definition of behavior | Determine which behaviors to increase and which to decrease (enter on website). Use the application to record behaviors for the “behaviors to increase” and “behaviors to decrease”(data submission). |
| Appropriate behaviors and behaviors you want to reduce |
|||
| 3 | Reinforcement | Effective praise | Reinforce the “behaviors to increase” and the appropriate behaviors that are incompatible with the “behaviors to decrease” recorded in #2, and record them (data submission). |
| Technology for reinforcement | |||
| Shaping | |||
| 4 | Function of Behavior | A-B-C analysis | Perform an ABC analysis of some behaviors in everyday situations (submit by e-mail). |
| Functions of problem behavior | |||
| 5 | Antecedent Control | Arranging the environment | Perform and record antecedent controls for “behaviors to decrease (data submission). |
| 6 | Instruction and Prompt | Effective instructions and prompts Fade-in and fade-out techniques |
Improve the way they give instructions for some behaviors in everyday life (Submit by e-mail). |
Session 1 consisted of an orientation to the PT program. In Session 2, participants learned to define behaviors specifically. The participants categorized their children’s behaviors as “behaviors to increase” and “behaviors to decrease”. The homework was to use the application to record behaviors for the “behaviors to increase” and “behaviors to decrease” as set by them. In Session 3, participants learned the principles of reinforcement and how to select and effectively use reinforcers for their children. The homework was to reinforce and record “behaviors to increase” and to reinforce and record appropriate alternative behaviors for “behaviors to decrease”. In Session 4, participants learned how to perform an ABC analysis and the function of the behaviors. The homework was to perform an ABC analysis of some behaviors in everyday situations. In Session 5, the participants learned about antecedent control to prevent inappropriate behaviors from occurring. The homework was to perform and record antecedent controls for “behaviors to decrease”. In Session 6, participants learned about effective instruction and prompts. For effective instruction, participants learned to get the child’s attention before instruction, to keep instruction short and specific, and to lower the level of demands. For prompts, participants learned about types of prompts and how to fade in and out. The homework was to improve the way they gave instructions for some behaviors in everyday situations and report back.
Recording of behavior in the home setting
The targeted-behavior records submitted in the homework were maintained by the participants themselves using an application called Observations.17 Observations is an application that can easily record the occurrence of target behaviors, automatically generate graphs as they are entered, and provide immediate feedback on the results. Data can be sent using the ‘Send’ function in Observations. The staff provided individual feedback to participants via email based on Observation records.
Communication with participants
The staff (second author) provided feedback via email on effective aspects and those needing improvement each time a participant reported a homework assignment or record. The number of e-mail communications between each participant and staff was measured.
Questionnaire evaluation
Questionnaires were administered pre- and post-intervention periods. The Parent Stress Index (PSI) and Beck Depression Scale II (BDI-II) were administered on the participants themselves. The children’s behavior was assessed using the Strengths and Difficulties Questionnaire (SDQ).
Parenting Stress Index: The Japanese version of the PSI (Parenting Stress Index) was used. This is based on the Parenting Stress Index developed in the U.S.18 and standardized by Kanematsu et al.19 for Japanese parents. The questionnaire consists of 78 items, 38 related to the children and 40 related to the parents. The questionnaire format collected responses on a five-point Likert scale from not at all to exactly as it is.
Beck Depression Index II: The Beck Depression Index II (BDI-II) is the second version of the BDI, which was designed by Beck et al.20 in 1996. This questionnaire consists of 21 items, each of which assesses a symptom related to depression over the two weeks prior to the administration of the questionnaire. Each item is scored on a 4-point scale from 0 to 3, with higher scores indicating more severe symptoms. The severity of depression is categorized based on the following BDI-II scores in the Japanese samples: a score of 13 or less as minimal (or remission), 14 to19 as mild, 20 to 28 as moderate, and 29 or greater as severe. The reliability and validity of the Japanese version of the BDI-II were established by Kojima et al.21
Strengths and Difficulties Questionnaire: The Strengths and Difficulties Questionnaire (SDQ) was developed by Goodman22 for behavioral screening of three to-16-year-olds. The SDQ consists of 25 items divided into five scales of five items each: emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems, and prosocial behavior. Each of the 25 items is rated as not true (0 points), somewhat true (1 point), or certainly true (2 points). Support needs in each area can be divided into three categories: High Need, Some Need, and Low Need. According to Mitsubishi et al.,23 High Need is indicated by five points or more for emotional problems, five points or more for behavioral problems, seven points or more for hyperactivity, five points or more for peer problems, and four points or fewer for prosocial behavior.
Acceptability Questionnaire
From Session 2 onward, a questionnaire regarding the previous session was administered during each session using Google FormsⓇ. The questionnaire consisted of five questions. Question 1, related to the comfort of video viewing, was answered on a 3-point Likert scale. Question 2 (about the adequacy of the period during which the video is available for viewing), Question 3(about the difficulty level of lecture content), and Question 4 (about the difficulty level of homework) were answered on a 4-point Likert scale. Question 5, which asked for any other questions from the participants, was the free response. Homework was submitted via Google Forms for Sessions 1, 4, and 6, and via email for all others, with data recorded using the application.
Statistical analysis
Tau-U is an effect size developed by Parker et al.24 There are two types of Tau-U: Tau which does not take into account the trend in the baseline period and Tau-U which does take into account the trend in the baseline period. In this study, Tau-U was used to analyze whether a difference existed in the number of occurrences of the target behavior between the baseline and intervention periods. Tau-U uses all data points, calculates standard values for the baseline and intervention periods, and performs a significance test between each condition. An effect size of 0.80 or above indicated a very large effect; 0.60–0.80, a large effect; 0.20–0.60, a moderate effect; and less than 0.20, a small effect.25 The web app of Vannest et al.26 was used for the statistical analysis, with a significance level of less than 5%.
Ethical considerations
This study was approved by the Ethics Committee of the Organization for Educational Support and International Affairs, Tottori University (Approval Number 2020-02). The study was conducted in accordance with the ethical standards established by the 1964 Declaration of Helsinki.
RESULTS
Participation in programs
P1 used only a smartphone, whereas P2 used both a PC and smartphone. Both participants were able to complete the program during the pre-scheduled delivery period. The percentage of correct answers on the confirmation test for each session was 100% for both participants.
Homework accomplished
Both participants submitted all homework tasks. In the homework for Session 2, each participant was first asked to fill out and send in a list of behaviors they wanted to increase and decrease. P1 identified “gestures and utterances of requests” as behaviors she would like to increase and “hanging around during meals” and “taking toys used by friends at the school” as behaviors she would like to decrease. The behaviors that P2 would like to increase were “apologizing immediately when I tell them I don’t like what he does to me”, and the behaviors P2 would like to decrease were “hanging around during meals”, “not being able to return greetings”, and “not being able to read the room”.
After receiving these responses, we explained the behavioral theory again by e-mail and organized the target behaviors. As a result, the target behaviors to increase for P1 were set as “signing requests” and the ones to decrease as “hanging around during meals”. The target behaviors to increase for P2 were set as “greeting (good morning, good night, thank you, and thank you for the food)” and those to decrease as “hanging around during meals”. The participants were then asked to use the application to record the extent to which these behaviors occurred in their daily lives. The homework for Session 3 was to reinforce the behavior that should be increased with a reinforcer determined by the participant, and for the behavior that should be decreased, to reinforce the appropriate alternative behavior to the unwanted behavior.
Both participants reinforced each behavior that should be increased and recorded. Both participants also reinforced “sitting and eating,” an alternative to the behavior “hanging around during meals”. In Session 4, we asked the participants to conduct an ABC analysis of some behaviors in their children’s lives and report back to us by e-mail with a description of the situation. Although P1 said that ABC analysis was difficult, both participants were able to properly categorize the behaviors into ABCs. Participants also shared with the staff the functions of those behaviors.
In Session 5, the participants were asked to consider and report environmental adjustments (antecedent control) for the behaviors recorded in Session 3. P1 used magnets with instructions on the order of actions she wanted the child to perform, and used self-help tools such as corrective chopsticks when eating. P2 showed some ingenuity in the way she gave instructions, such as showing an actual object, calling out a name or tapping on the shoulder to get attention, and confirming eye contact before giving instructions. Both P1 and P2 were also able to prepare in advance the reinforcers they would use when they completed the task. In the homework for Session 6, both participants reported that they set new appropriate target behaviors in their lives and devised new ways to instruct and praise them. P1 worked on seven behaviors, including wearing a hoodie alone, saying “bread” when you want bread, and cleaning up, using instruction, prompting, and reinforcement techniques, and reported positive outcomes. P2 set six target behaviors for his daily life, including brushing his teeth alone and wearing pajamas alone, and received positive reports.
Recording of behavior in the home setting
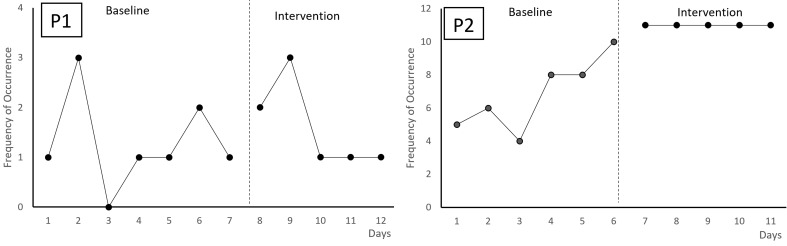
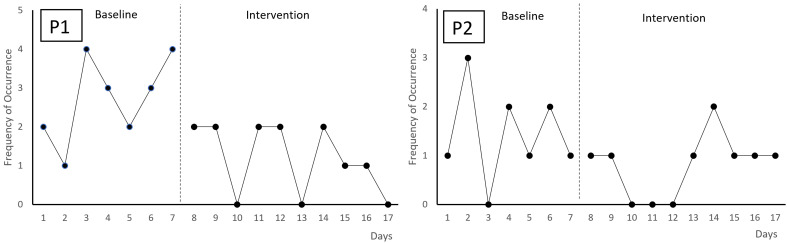
Both participants were able to use the application to record the target behaviors to increase and decrease. Figures 1 and 2 shows the frequency of occurrences of the targeted behaviors. The target behaviors to be increased for P1 was sign-requiring behavior and for P2 was spontaneous greeting (Fig. 1). P1 and P2 had different baseline measurement counts due to varying baseline recording start dates. During the intervention phase, these behaviors were reinforced with verbal praise. The target behavior to be reduced was “hanging around during meals” (Fig. 2). During the intervention phase, both participants reinforced “siting and eating” as an alternative to the behavior “hanging around during meals”.
Fig. 1.
The frequency of the occurrences of targeted behaviors to increase.
Fig. 2.
The frequency of the occurrences of targeted behaviors to decrease.
In the behaviors to be increased (Fig. 1), the targeted behavior of P1 saw no significant increase from the baseline period to the intervention period (Tau = 0.2, n.s. 90% CI = –0.38 – 0.78). On the other side, the targeted behavior of P2 was significantly increased (Tau = 1, P < 0.01, 90% CI = 0.40 – 1). In the behaviors to be decreased (Fig. 2), the targeted behavior of P1 was significantly reduced from the baseline period to the intervention period (Tau = – 0.69, P < 0.05, 90% CI = –1 – –0.26).There was moderately effective, although not significantly less, decrease in target behavior for P2 (Tau = –0.39, n.s. 90% CI = –0.87 – –0.10).
Communication with participants
Email communication between staff and participants regarding questions and assignment submissions was 18 times for P1 and 19 times for P2. The number of email communications per session was zero for Session 1, 12 for Session 2 (P1 = 6, P2 = 6), ten for Session 3 (P1 = 4, P2 = 6), five for Session 4 (P1 = 2, P2 = 3), six for Session 5 (P1 = 4, P2 = 2), and four for Session 6 (P1 = 2, P2 = 2).
Questionnaire evaluation
Table 2 shows the pre-post scale scores. Excluding “prosocial behavior” on the SDQ, the decrease in scores indicates improvement.
Table 2. Scale scores Pre and Post the program.
| P1 | P2 | ||||
| Pre | Post | Pre | Post | ||
| PSI | Child | 110 | 60 | 66 | 64 |
| Parents | 123 | 62 | 63 | 60 | |
| Total | 233 | 122 | 129 | 124 | |
| BDI | 19 | 9 | 16 | 13 | |
| SDQ | Total difficulties score | 29 | 26 | 30 | 27 |
| Conduct Problems | 8 | 7 | 7 | 6 | |
| Hyperactivity/Inattention | 7 | 7 | 7 | 7 | |
| Emotional Symptoms | 5 | 4 | 8 | 6 | |
| Peer Problems | 9 | 8 | 8 | 8 | |
| Prosocial Behavior | 4 | 3 | 10 | 10 | |
PSI, Parenting Stress Index; BDI, Beck Depression Index II; SDQ, Strengths and Difficulties Questionnaire.
Parenting Stress Index: The overall PSI scores decreased for both P1 and P2; from 233 to 122 for P1, and from 129 to 124 for P2. P1 decreased from 123 to 62 points for the parental aspect, and from 110 to 60 points for the child aspect. P2 showed a slight decrease from 63 to 60 points for the parental aspect, and from 66 to 64 points for the child aspect.
Beck Depression Index II: The BDI scores before and after the intervention showed a significant decrease in P1 from 19 (mild level) to 9 (minimal level), and a slight decrease in P2 from 16 (mild level) to 13 (minimal level), indicating an improvement in depression level.
Strengths and Difficulties Questionnaire: Total difficulty score on the SDQ decreased from 29 to 26 for P1, and from 30 to 27 for P2. On the subscale scores, P1 decreased in “conduct problems,” “emotional symptoms,” and “peer problems;” while “hyperactivity/inattention” remained unchanged. P2 decreased in “conduct problems” and “emotional symptoms,” and did not change in “hyperactivity/inattention” and “peer problems.” There was little change in “prosocial behavior,” from 4 to 3 points for P1, and 10 to 10 points for P2.
Acceptability Questionnaire
Both Q1 “Comfort of video viewing” and Q2 “Adequacy of the period during which the video is available for viewing” were shown to be appropriate throughout the entire session. Q3, “difficulty level of lecture content,” was rated as easy by both participants for Sessions 1, 2, and 6. Both participants rated Session 4 as difficult. For Q4’s “Difficulty level of homework”, Sessions 2 and 6 were rated as easy, but for Session 4, both rated it difficult. In the free response section for Q5, regarding ease of attending the course, P1 reported, “It was good that I was able to watch the program at a time convenient for me so that I could participate in the program even while working. I was glad to be able to listen to the next session after submitting my assignments.” On the other hand, regarding communication with the staff, P1 reported, “I wondered if it was safe to ask questions, so it was difficult to ask questions.” P2 said “I felt distance from the staff because I did not have many opportunities to talk directly with them.” Both participants watched the video on the same day it was released, and it was noted that the two-week interval between each session was too long.
DISCUSSION
In this study, we developed a prototype of an effective on-demand PT program by expanding on the program of Inoue et al.11 We then analyzed how the program changes the participants’ mental health and the targeted and non-targeted behavior of the children through case studies. The implementation potential of this program has also been discussed based on an analysis of questionnaires regarding the number of interactions with staff and social acceptance of the program.
Both participants were able to complete the program during the pre-scheduled delivery period. The percentage of correct answers on the confirmation test and homework for each session was 100% for both participants. Although this study did not measure a general knowledge scale for behavior analysis such as Knowledge of Behavioral Principle as Applied to Children (KBPAC),27 we believe that participants achieved an appropriate level of knowledge based on their performance on the confirmation test in each session, the results of their homework, and the survey results.
Despite the importance of the number of interactions in telehealth interventions in terms of the implementation potential, few studies have described them.28 Email correspondence with participants for each session revealed that the number of such sessions varied from session to session, and that the need for follow-up on homework assignments varied from assignment to assignment. For example, when determining a child’s target behavior (Session 2), participants had difficulty determining the appropriate behavior based on the program alone and had to coordinate through email correspondence with staff. Also, in the homework for Session 3, a lot of back and forth was necessary regarding determinate alternative behavior for behaviors that should be decreased. On the Acceptability Questionnaire, Session 4 indicated higher difficulty with both lecture content and homework. These results suggest that in Sessions 2-4, there was a need to revise lecture content, split up homework assignments, and provide efficient feedback methods.
In PT, parental implementation of the program at home and behavioral change in the child are important elements. In terms of SDQ scores, both participants indicated improvement in their children’s behavior, but the changes were slight in terms of scores. Diaz-Stransky et al29 reported statistically significant improvements in Disruptive Behavior measures before and after online parent training with eight 10-minute online modules and three 45-minute videoconferences. For this study to achieve greater results, it may be necessary to implement videoconferencing as shown in previous studies.
This study evaluated changes not only in the pre-and post-questionnaire measures but also the results of parent implementation and recording of both baseline and intervention in two target behaviors, “behaviors to increase” and “behaviors to decrease” in everyday situations. The results showed that of the four tasks in total, those that significantly benefited from the intervention were an increase in greetings for P2 and a decrease in hanging around during meals for P1.
Of the two target behaviors, behaviors to increase and behaviors to decrease, the former promoted using the child’s preferred stimulus selected by the participant in Session 3 as the reinforcer. For the latter, participants were instructed to reinforce appropriate behaviors incompatible with the target. For reinforcement to work correctly, reinforcer selection and timing are essential. These strategies may not work well for tasks that did not show clear effects. Normally, when ABA is not effective in behavior modification, we should formulate a hypothesis of the factors that may be contributing to the behavioral change, introduce new intervention variables, and record the results again. However, this program was constructed as a linear process and did not provide an optional program in case the homework assignment did not produce sufficient results. In the future, it may be necessary to add a procedure whereby if sufficient results are not achieved, the staff is asked to send videos of instructional situations that they analyze and subsequently suggest areas for improvement.
Regarding parental mental health at the pre- and post-stages, there was an improvement in both parenting stress (PSI) and depression (BDI) for both parents. No worsening was observed in all any sub-scales. There are many examples of synergistic effects between children’s behavior change and parents’ mental health,30 and the results of this study supported this.
Online PTs may be easier to participate in than regular face-to-face PTs, no matter where the parents live. The free-response statements on the acceptability questionnaire also suggested that the advantage of on-demand PT such as in this study, is that students can take the course in their free time and watch the videos as often as they want. Previous studies have also pointed out that the on-demand type provides fewer opportunities for interaction with other participants,31 and that it would be considered necessary to include some sessions in which participants can interact with each other using videoconferencing systems or other means.
The program in this study was developed as a prototype for on-demand PT and it was the result of two case studies. Further demonstration is needed to increase the number of cases and to compare the results between groups. Another issue to be addressed in the future is the comparison of the effectiveness of different types of PT programs, such as on-demand and real-time programs. This study was able to record and confirm the behavioral changes of children in actual homes. However, these are behavioral observation records made by parents and need to be revalidated to increase their reliability, such as through objective analysis of video data. In addition, some of the behaviors targeted in this study were not fully effective in their intervention. In order to guarantee sufficient behavior change through remote support, it is important to be able to select various intervention methods depending on the needs of the participant parents and the main complaints and conditions of the children.32 Creating variations to meet the needs of participants and the progress of the program is also a possible challenge for the future.
Acknowledgments
Acknowledgments: This work was supported by Grant-in-Aid for Scientific Research (C) Grant Number (JP18k02756). We are grateful to the participants in this study.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Publishing; 2013. DOI: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- 2.Rattaz C,Michelon C,Munir K,Baghdadli A. Challenging behaviours at early adulthood in autism spectrum disorders: topography, risk factors and evolution. J Intellect Disabil Res. 2018;62:637-49. 10.1111/jir.12503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inoue M,Gomi Y,Matsuda S. Developmental trajectories of challenging behaviors reported retrospectively by Japanese parents of adult children with intellectual disabilities. Int J Dev Disabil. 2022;1-9. 10.1080/20473869.2022.2087450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayes SA,Watson SL. The impact of parenting stress: a meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J Autism Dev Disord. 2013;43:629-42. 10.1007/s10803-012-1604-y [DOI] [PubMed] [Google Scholar]
- 5.Schnabel A,Youssef GJ,Hallford DJ,Hartley EJ,McGillivray JA,Stewart M,et al. Psychopathology in parents of children with autism spectrum disorder: A systematic review and meta-analysis of prevalence. Autism. 2020;24:26-40. 10.1177/1362361319844636 [DOI] [PubMed] [Google Scholar]
- 6.Haraguchi H,Inoue M. Evaluating outcomes of a community-based parent training program for Japanese children with developmental disabilities: a retrospective pilot study. Int J Dev Disabil. 2022;1-10. 10.1080/20473869.2022.2070420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lichtlé J,Downes N,Engelberg A,Cappe E. The effects of parent training programs on the quality of life and stress levels of parents raising a child with autism spectrum disorder: A systematic review of the literature. Rev J Autism Dev Disord. 2020;7:242-62. 10.1007/s40489-019-00190-x [DOI] [Google Scholar]
- 8.Postorino V,Sharp WG,McCracken CE,Bearss K,Burrell TL,Evans AN,et al. A systematic review and meta-analysis of parent training for disruptive behavior in children with an autism spectrum disorder. Clin Child Fam Psychol Rev. 2017;20:391-402. 10.1007/s10567-017-0237-2 [DOI] [PubMed] [Google Scholar]
- 9.Sullivan ADW,Forehand R,Acosta J,Parent J,Comer JS,Loiselle R,et al. COVID-19 and the acceleration of behavioral parent training telehealth: current status and future directions. Cognit Behav Pract. 2021;28:618-29. 10.1016/j.cbpra.2021.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ros-DeMarize R,Chung P,Stewart R. Pediatric behavioral telehealth in the age of COVID-19: brief evidence review and practice considerations. Curr Probl Pediatr Adolesc Health Care. 2021;51:100949. 10.1016/j.cppeds.2021.100949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Inoue M,Tatsumi A,Fukuzaki T. Effectiveness of the internet based parent education program on applied behavior analysis for parents of children with autism spectrum disorder. Brain Dev. 2022;44:655-63. 10.1016/j.braindev.2022.07.008 [DOI] [PubMed] [Google Scholar]
- 12.Dodds RL. Helping optimize language acquisition (HOLA) online parent training modules for latinx parents of toddlers at risk for ASD: protocol for a pilot funded by the Organization for Autism Research. JMIR Res Protoc. 2020;9:e18004. 10.2196/18004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wainer AL,Ingersoll BR. Increasing access to an ASD imitation intervention via a telehealth parent training program. J Autism Dev Disord. 2015;45:3877-90. 10.1007/s10803-014-2186-7 [DOI] [PubMed] [Google Scholar]
- 14.Pennefather J,Hieneman M,Raulston TJ,Caraway N. Evaluation of an online training program to improve family routines, parental well-being, and the behavior of children with autism. Res Autism Spectr Disord. 2018;54:21-6. 10.1016/j.rasd.2018.06.006 [DOI] [Google Scholar]
- 15.Steiner AM,Koegel LK,Koegel RL,Ence WA. Issues and theoretical constructs regarding parent education for autism spectrum disorders. J Autism Dev Disord. 2012;42:1218-27. 10.1007/s10803-011-1194-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16..Lindgren S,Wacker D,Suess A,Schieltz K,Pelzel K,et al. Telehealth and autism: treating challenging behavior at lower cost. Pediatrics. 2016;137 Suppl 2(Suppl 2):S167-75. DOI: 10.1542/peds.2015-2851O [DOI] [PMC free article] [PubMed]
- 17.Inoue M,Nakatani K,Higashino M. Development of behavior record application “Observations” for behavior problems. Jpn J Behav Anal. 2019;34:78-86. Japanese with English abstract. 10.24456/jjba.34.1_78 [DOI] [Google Scholar]
- 18.Abidin RR. Parenting Stress Index: Manual. Administration booklet,[and] Research Update; 1983. [Google Scholar]
- 19.Kanematsu Y,Araki A,Narama M,Shirahata N,Maru M,Arayashiki R. PSI–parental stress index manual. Tokyo: Koyo Mondai Kenkyukai; 2006. Japanese [Google Scholar]
- 20.Beck AT,Steer RA,Brown G. Beck Depression Inventory–II. Psychol Assess. 1996. 10.1007/978-1-4419-1005-9_441 [DOI] [Google Scholar]
- 21.Kojima M,Furukawa TA,Takahashi H,Kawai M,Nagaya T,Tokudome S. Cross-cultural validation of the Beck Depression Inventory-II in Japan. Psychiatry Res. 2002;110:291-9. 10.1016/S0165-1781(02)00106-3 [DOI] [PubMed] [Google Scholar]
- 22.Goodman R. The Strengths and Difficulties Questionnaire: A Research Note. J Child Psychol Psychiatry. 1997;38:581-6. 10.1111/j.1469-7610.1997.tb01545.x [DOI] [PubMed] [Google Scholar]
- 23.Matsuishi T,Nagano M,Araki Y,Tanaka Y,Iwasaki M,Yamashita Y,et al. Scale properties of the Japanese version of the Strengths and Difficulties Questionnaire (SDQ): A study of infant and school children in community samples. Brain Dev. 2008;30:410-5. 10.1016/j.braindev.2007.12.003 [DOI] [PubMed] [Google Scholar]
- 24.Parker RI,Vannest KJ,Davis JL,Sauber SB. Combining nonoverlap and trend for single-case research: Tau-U. Behav Ther. 2011;42:284-99. 10.1016/j.beth.2010.08.006 [DOI] [PubMed] [Google Scholar]
- 25.Vannest KJ,Ninci J. Evaluating intervention effects in single-case research designs. J Couns Dev. 2015;93:403-11. 10.1002/jcad.12038 [DOI] [Google Scholar]
- 26.Vannest KJ,Parker RI,Gonen O,Adiguzel T. Single Case Research: web-based calculators for SCR analysis. version 2.0. [Internet]. TX: Texas A&M University; 2016. [cited 2022 Oct 29]. Available from: http://www.singlecaseresearch.org/calculators/tau-u
- 27.O’Dell SL,Tarler-Benlolo L,Flynn JM. An instrument to measure knowledge of behavioral principles as applied to children. J Behav Ther Exp Psychiatry. 1979;10:29-34. 10.1016/0005-7916(79)90033-8 [DOI] [Google Scholar]
- 28.Ito H,Inoue M. Parent-mediated toilet training for a child with autism spectrum disorder through teleconsultation: A case report. Yonago Acta Med. 2022;65:90-5. 10.33160/yam.2022.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diaz-Stransky A,Rowley S,Zecher E,Grodberg D,Sukhodolsky DG. Tantrum tool: development and open pilot study of online parent training for irritability and disruptive behavior. J Child Adolesc Psychopharmacol. 2020;30:558-66. 10.1089/cap.2020.0089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker BL,McIntyre LL,Blacher J,Crnic K,Edelbrock C,Low C. Pre-school children with and without developmental delay: behaviour problems and parenting stress over time. J Intellect Disabil Res. 2003;47:217-30. 10.1046/j.1365-2788.2003.00484.x [DOI] [PubMed] [Google Scholar]
- 31.Ingersoll B,Berger NI. Parent engagement with a telehealth-based parent-mediated intervention program for children with autism spectrum disorders: predictors of program use and parent outcomes. J Med Internet Res. 2015;17:e227. 10.2196/jmir.4913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rodriguez KA. Maintaining treatment integrity in the face of crisis: A treatment selection model for transitioning direct ABA services to telehealth. Behav Anal Pract. 2020;13:291-8. 10.1007/s40617-020-00429-8 [DOI] [PMC free article] [PubMed] [Google Scholar]