Composite autograft construction completed on a beating heart.
Central Message.
The composite pulmonary autograft construction can be safely completed on a beating heart to shorten crossclamp time and help increase the adoptability of the Ross procedure.
Case Report
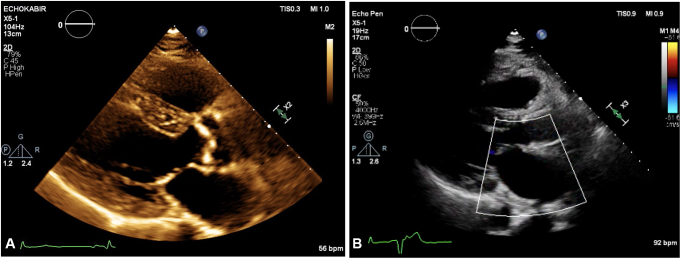
A 63-year-old man with bicuspid aortic valve and history of myocardial infarction after percutaneous coronary intervention with a residual 60% to 70% left anterior descending lesion and left ventricular ejection fraction of 65% was referred to our institution for his severe, symptomatic aortic stenosis and moderate aortic regurgitation. Preoperative echocardiography demonstrated a heavily calcified aortic valve with peak transaortic gradient of 82 mm Hg (Figure 1, A, and Video 1). The patient specifically requested a Ross procedure. Institutional review board approval was not required per the institution; the patient provided informed written consent.
Figure 1.
Preoperative (A) and postoperative (B) transthoracic echocardiography captured in systole and diastole, respectively. Note the severely calcified aortic valve with limited mobility prior to the operation. After the Ross procedure, the autograft valve demonstrated excellent hemodynamics without regurgitation.
Given the history of myocardial infarction and the need for coronary artery bypass grafting, there was an interest in shortening the crossclamp time. Via a median sternotomy after left internal thoracic artery harvesting and while on beating heart on cardiopulmonary bypass, an incision was made in the infundibular area below the pulmonary valve (PV). The PV was then carefully separated from the right ventricular outflow tract by continuing the incision in a curvilinear fashion while maintaining 3 mm of distance from the PV throughout. Care was taken to ensure that the incisional plane was just above the first septal perforator. Hemostasis of the right ventricular incisional plane was obtained (Video 2).
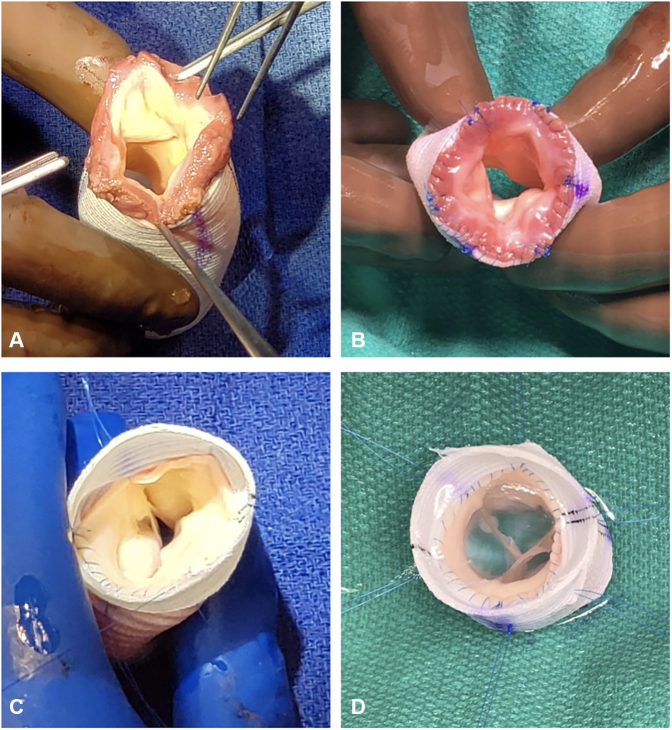
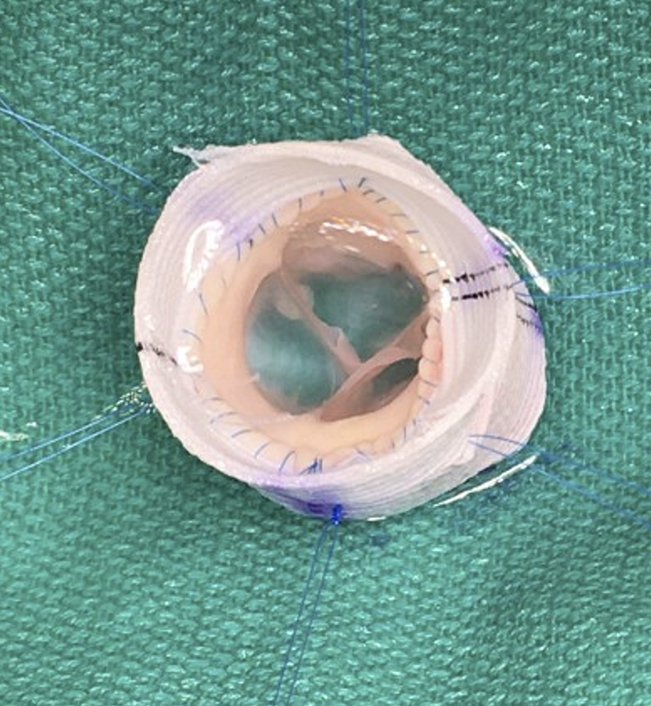
To prepare the pulmonary autograft, extramuscular and fatty tissue were removed from the pulmonary root. After sizing the autograft, it was placed inside of a 26-mm straight polyethylene terephthalate graft (Figure 2, A). The subannular suture line was completed with a running 5–0 polypropylene suture (Figure 2, B). The PV commissures were suspended and attached onto the straight graft. Anticommissural plication (ACP) was performed at the level of the commissures to reduce the diameter of the sinotubular junction. Next, the pulmonary artery suture line was completed at approximately 1 cm above the level of the commissures into the inside of the straight graft using a running 5–0 polypropylene suture (Figure 2, C). PV geometry and competency was confirmed (Figure 2, D, and Video 3), and the composite autograft was placed in cool saline until further use.
Figure 2.
Pulmonary autograft preparation during beating heart using the modified inclusion technique. A, Pulmonary autograft was placed inside of a straight polyethylene terephthalate graft. B, The subannular suture line was completed to attach the pulmonary autograft to the straight polyethylene terephthalate graft. C, The distal suture line was performed to attach the pulmonary artery onto the straight polyethylene terephthalate graft. D, Completed composite pulmonary autograft using the inclusion technique.
Aortic crossclamp was then applied, and cardiac arrest was achieved via single-dose antegrade del Nido cardioplegia. After the left internal thoracic artery to left anterior descending artery anastomosis, the ascending aorta was incised and resected. After coronary buttons mobilization, the heavily diseased bicuspid aortic valve was resected, and the annulus debrided of dense calcification. Next, nonpledgeted horizontal mattress 3–0 polypropylene sutures were circumferentially placed around the annulus and then through the proximal end of the composite pulmonary autograft. After securing the composite pulmonary autograft proximally, the coronary buttons were reimplanted in orthotopic positions using running 5–0 polypropylene sutures. The aortic anastomosis was completed. Lastly, the pulmonary homograft was implanted in the standard fashion. Aortic crossclamp time was 128 minutes, and total cardiopulmonary bypass time was 258 minutes. Patient was extubated on postoperative day 0 and was transferred to the floor on postoperative day 3. No complications were observed. Echocardiography prior to discharge demonstrated excellent autograft function and normal biventricular function (Figure 1, B, and Video 4). He was discharged on postoperative day 7 and is currently alive and doing well 6 months postoperation.
Comment
The Ross procedure is technically demanding, typically requiring aortic crossclamp time of more than 150 minutes.1,2 When concomitant procedures are indicated, the crossclamp time could be further prolonged, potentially having a negative influence on cardiac function and the postoperative course. In this case report, we describe strategies to shorten crossclamp time. We emphasize the utility of harvesting the pulmonary autograft, inspecting the autograft, trimming the excess tissue, and preparing the composite pulmonary autograft via graft inclusion technique all before aortic crossclamping. This could represent an aggregate 30 to 60 minutes of crossclamp time saved, depending upon techniques employed and surgeon experience.
The inclusion technique using straight polyethylene terephthalate graft was developed to reinforce the pulmonary autograft to prevent late dilation.3,4 This technique drastically decreased autograft reintervention rate at 10 years from 27% without reinforcement to 4% with the inclusion technique.3 The modified inclusion technique was described to use the ACP technique that are used in aortic valve reimplantation procedures to recreate neosinuses.4 The use of the ACP was supported by the ex vivo study demonstrating excellent hemodynamics and improved leaflet kinematics compared with straight polyethylene terephthalate graft only.4,5 The improved biomechanics may translate to improved long-term pulmonary autograft durability in the Ross procedure.
Conclusions
This case demonstrates a successful Ross procedure with the autograft harvest and the composite autograft construction with the modified inclusion technique completed on the beating heart. Using this strategy, the crossclamp time was significantly shortened. We believe that this technique can be safely employed to help increase the adoptability of the Ross procedure while producing excellent outcomes.
Footnotes
Disclosures: The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Supplementary Data
Preoperative echocardiography demonstrated a severely calcificed aortic valve with limited mobility. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.
Pulmonary autograft harvest on beating heart. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.
The composite pulmonary autograft constructed using the modified inclusion technique. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.
Postoperative echocardiography demonstrated excellent autograft valve function and hemodynamics. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.
References
- 1.Bansal N., Kumar S.R., Baker C.J., Lemus R., Wells W.J., Starnes V.A. Age-related outcomes of the Ross procedure over 20 years. Ann Thorac Surg. 2015;99:2077–2085. doi: 10.1016/j.athoracsur.2015.02.066. [DOI] [PubMed] [Google Scholar]
- 2.Tan Tanny S.P., Yong M.S., d'Udekem Y., Kowalski R., Wheaton G., D'Orsogna L., et al. Ross procedure in children: 17-year experience at a single institution. J Am Heart Assoc. 2013;2:e000153. doi: 10.1161/JAHA.113.000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Starnes V.A., Elsayed R.S., Cohen R.G., Olds A.P., Bojko M.M., Mack W.J., et al. Long-term outcomes with the pulmonary autograft inclusion technique in adults with bicuspid aortic valves undergoing the Ross procedure. J Thorac Cardiovasc Surg. February 3, 2021 doi: 10.1016/J.JTCVS.2021.01.101. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4.Zhu Y., Marin-Cuartas M., Park M.H., Imbrie-Moore A.M., Wilkerson R.J., Madira S., et al. Ex vivo biomechanical analysis of the Ross procedure using the modified inclusion technique in a 3-dimensionally printed left heart simulator. J Thorac Cardiovasc Surg. September 26, 2021 doi: 10.1016/J.JTCVS.2021.06.070. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu Y., Wilkerson R., Pandya P., Mullis D., Wu C., Madira S., et al. Biomechanical engineering analysis of pulmonary valve leaflet hemodynamics and kinematics in the Ross procedure. J Biomech Eng. 2022;145:011005. doi: 10.1115/1.4055033. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preoperative echocardiography demonstrated a severely calcificed aortic valve with limited mobility. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.
Pulmonary autograft harvest on beating heart. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.
The composite pulmonary autograft constructed using the modified inclusion technique. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.
Postoperative echocardiography demonstrated excellent autograft valve function and hemodynamics. Video available at: https://www.jtcvs.org/article/S2666-2507(22)00535-1/fulltext.