Abstract
Background and aim
The American College of Radiology (ACR) defines “actionable findings” the ones requiring a special communication between radiologists and referring clinicians, suggesting to organize their categorization in a three-degree scale on the basis of the risk for the patient to develop complications. These cases may fall in a grey-zone communication between different care figures with the risk of being underestimated or even not being considered at all. In this paper, our aim is to adapt the ACR categorization to the most frequent actionable findings encountered when reporting PET/CT images in a Nuclear Medicine Department, describing the most frequent and relevant imaging features and presenting the modalities of communication and the related clinical interventions that can be modulated by the prognostic severity of the clinical cases.
Materials and methods
We performed a descriptive, observational and critical analysis of the most relevant literature on the topic of “actionable findings”, in particular, starting from the reports of the ACR Actionable Reporting Work Group, we categorised and described, in a narrative review, the most relevant “actionable findings” encountered in the Nuclear Medicine PET/CT daily practice.
Results
To the best of our knowledge, to date there are no clear indications on this selective PET/CT topic, considering that the current recommendations target mainly radiologists and assume a certain level of radiological expertise. We resumed and classified the main imaging conditions under the term of “actionable findings” according to the corresponding anatomical districts, and we described their most relevant imaging features (independently of PET avidity or not). Furthermore, a different communication timing and strategy was suggested on the basis of the findings’ urgency.
Conclusion
A systematic categorization of the actionable imaging findings according to their prognostic severity may help the reporting physician to choose how and when to communicate with the referring clinician or to identify cases requiring a prompt clinical evaluation. Effective communication is a critical component of diagnostic imaging: timely receipt of the information is more important than the method of delivery.
Keywords: Actionable findings, PET/CT, Nuclear Medicine, Emergency
Introduction
“Actionable findings” in the radiological scenario
It is well known the importance of a correct and complete report of diagnostic imaging examinations. At the same time, it has relevance and impact on clinical management, also a timely notification of the results [1]. Those aspects become even more relevant if the physician reports an “actionable finding”. There have been different definitions and classifications of “actionable findings” in radiological settings: in particular, the definition by the American College of Radiology (ACR) Actionable Reporting Work Group (first applied in 2014 and recently revised in 2020) was “all findings that require special communication with the referring clinician”, [2]. As declared by the authors of Actionable Reporting Work Group, their paper should not be considered as a guideline or as a strict categorization but as the result of a collective experience and viewpoint of members of the ACR Group. The aim of their work was to support the radiologists and to improve the patient’s management, taking into account both the patient’s clinical condition and the practice environment. The ACR classification focus was the correct timing and communication modality, so that each institute/department should construct their internal finding’s categorization depending on different factors: the referring patients’ characteristics, the radiologist’s expertise, the collaboration and communication between radiologists and clinicians and the different diagnostic/therapeutic options depending on local availability.
On the other hand, the Joint Commission’s (TJC) National Patient Safety Goal defines a critical result as “any finding that may be considered life threatening or that could result in severe morbidity and require urgent or emergent clinical attention” [3].
Different studies tried to assess the prevalence of “actionable findings” in radiology reports [4–6] which varied widely: 1.5%, 13.1%, 32.1% [7]. These differences could be related to several causes: first of all, the challenge to define an “actionable finding” and to categorise it according to different clinical urgency. Some studies adhered to the lists previously suggested by the ACR Work Group report, whereas other ones used a three-degree scale (red, orange and yellow alert) based on the level of urgency but with a fair agreement with the ACR classification. On the other hand, in a few further papers, the exact classification was not specified or could not be retrieved. Another cause is the different prevalence of actionable findings that could be partially explained by the characteristic of the care centre and consequently by the referred patients. In the same study, Visser and colleagues studied also the agreement between two radiologists in classifying the actionable findings according to the three ACR groups. On average, the two readers judged differently the findings amongst the three categories in almost one out of five radiology reports. As stated by the authors, part of this discordance may be explained by the employment of qualitative modifiers within the categorization guideline (i.e. expressions such as “clinically significant”, “highly suggestive”, “probable”, “suspected”, “mild” or “moderate”), because these terms’ interpretation can vary between readers leading to inferior agreement scores. However, most of the discrepancies were relatively small, with annotations that differed by only one category level.
When a physician reports diagnostic images, at first the attention is focussed on the clinical query, but, of course, all body districts included in the field of view should be explored. A finding is usually defined “unexpected” when it is not related to the clinical question and is unknown in the previous examinations. In the ACR document, the authors did not focus on the difference between “expected” or “unexpected” findings, but only on their clinical relevance and urgency. Also, the reporting style could impact on the clinical management: for example, when reporting an actionable finding, it is important to avoid the categorization into “accessory”, potentially leading to underestimation. Considering that, in the near future, the information technology (IT) could help to recognise actionable finding using natural language processing, the technical imaging language will assume an important role [8]: the usage of standardised terms and structured report would improve the relevance of actionable findings and probably reduce the inter-observer variability. Finally, the commercial developers of reporting system may provide solutions to the problems related with a time-consuming communication between imaging specialists and referring clinicians [9].
Both ACR and TJC specify that the list of actionable findings for each category should be considered just as a suggestion and not as a standard of care; the ACR Group underline that their purpose was not specifically to define each clinical situation or category but to put emphasis on findings that need for a timely intervention.
“Actionable findings” in the daily PET/CT practice
“Incidental findings” (incidentally discovered abnormalities apparently unrelated to the patient’s primary condition under evaluation [10]) are increasingly common in positron emission tomography/computed tomography (PET/CT) scans. This is mainly due to its hybrid diagnostic nature (including both a functional-PET and a morphological-CT component) and the non-invasive simultaneous assessment of multiple tissues and parenchyma throughout the whole body. Several publications explored the prevalence and outcomes of incidentalomas [11] and it is well known that incidental findings, showing radiotracer avidity, should be further investigated with additional time consumption and costs. In 15 studies analysed by a recent Danish paper, 642 of [18F]-flourodeoxyglucose ([18F]-FDG) avid foci were judged clinically relevant (PPV = 59%, range: 6–77%); the authors reported that, in some cases, there is sufficient evidence to guide management on the basis of standardized uptake value (SUV), morphological features on CT images, functional features on PET images or clinical information and risk factors [12]. In other cases, this information is insufficient to correctly characterise them and require further investigation or strict follow-up.
However, a finding called “incidental” might not be urgent nor require an action by the interpreting physician. On the other side, what is called “actionable” might be not necessarily related to the clinical condition for which the scan was required.
To the best of our knowledge, currently there are no clear indications on the more selective topic of “actionable findings” for Nuclear Medicine physicians reporting PET/CT; indeed, current recommendations target mainly radiologists and assume a certain level of expertise in radiology [1, 3]. We should also consider that the CT component associated with PET is generally non-diagnostic, without contrast media, with low/intermediate dose for attenuation correction and anatomical mapping. Furthermore, historically Nuclear Medicine training does not cover the comprehensive knowledge of critical care, which is traditionally a radiologists’ prerogative [13].
For all these reasons, in this work, our aim is to adapt the ACR categorization [2] to the most frequent actionable findings encountered when reporting PET/CT images in a Nuclear Medicine Department and to suggest a different communication on the basis of their urgency. The main imaging conditions are presented in Table 1 and as well as a few examples of the most relevant ones, for each category, described in the corresponding anatomical district paragraph.
Table 1.
Suggested categorization of the most frequent actionable findings in a Nuclear Medicine Department: revised on the basis of the ACR Work Group Appendix [2]
| Category 1: communicate within minutes/hour* | Category 2: communicate within day* | Category 3: communicate within weeks* | |
|---|---|---|---|
| General |
Suspected non-accidental trauma Any finding that deserve urgent clinical evaluation for the reporting physician |
Clinically significant mass, tumour or infection Unexpected finding highly suggestive of malignancy Displaced or migrated surgical or other medical device (eg. PICC) Unknown abscess in any body district |
Incidental findings require follow-up or other radiological studies Unexpected finding with low risk of malignancy |
| Neurologic/H&N |
Intracranial mass with significant mass effect (midline shift/herniation) Unstable spine fracture |
Intracranial mass without significant mass effect (no midline shift/herniation) Stable spinal fracture Finding highly suggestive for encephalitis |
Small intracranial mass, likely benign, without mass effect Suspected brain metastasis in patient with cancer diagnosis |
| GI |
Significant pneumoperitoneum High-grade intra-abdominal organ injury |
Unknown abscess Large volume ascites Small bowel obstruction |
Gallstone close to the neck of gallbladder Low volume ascites |
| MSK | Cervical bone lesion at risk of pathologic fracture |
Bone lesion at risk of pathologic fracture (femur, hip, other) Stable spinal fracture Infection (septic arthritis and osteomyelitis) |
Non displaced minor fracture with low risk for worsening Worsening of know lithic lesion |
| Chest |
Pneumotorax Large pericardial effusion |
Lobar or lung collapse Pneumomediastinum, Extensive subcutaneous emphysema Large pleural effusion High-risk contagious pneumonia with suggestive patter (eg. Covid-19) Lung lesion correlated with high risk of active tuberculosis |
Lung nodule or suspected lung nodule, not clearly benign Moderate pleural effusion Mild pericardial effusion |
| Cardiac/vascular |
Arterial aneurysm with high risk of ruptured/leaking Unexpected mass in heart cameras Large pericardial effusion Unknown arterial dissection |
Deep venous thrombosis Thoracic aortic aneurysm > 6 cm or abdominal aortic aneurysm ≥ 6 cm in male and ≥ 5 cm in female Pneumomediastinum, extensive subcutaneous emphysema Worsening of know arterial dissection |
Thoracic aortic aneurysm < 6 cm or abdominal aortic aneurysm < 6 cm in male and < 5 cm in female Peripheral aneurism likely require follow-up Extended coronary calcification Right ventricle muscle FDG hyperfixation |
| GU | High-grade kidney injury | Indirect signs of complete ureter obstruction |
Bladder distension probably related with urethral lumen restriction Severe bilateral Chronic Kidney Insufficiency |
H&N head and neck, GI gastrointestinal, MSK musculoskeletal, GU genito-urinary, PICC peripherally inserted catheter central, FDG fluorodeoxyglucose
*Each finding should be defined: a) new finding or no previous images available; b) worsening of an already know finding
According to the ACR Group, the descriptive terms such as “critical”, “urgent”, “clinically significant”, may cause confusion and may increase subjective interpretation leading to a different inter-observer finding categorization. We also agree with ACR Group that the most important message behind each category is to put emphasis on the need of non-routine communication and to suggest the best timing and action. These clues reflect mainly the daily diagnostic experience in our institution and depend on the local diagnostic and therapeutic work-flow, the expertise of the reporting physician and, last but not least, the network with the referring clinicians. Therefore they are not intended to be inflexible rules or requirements of practice; each institution/department should modify and create its own categorization list according to all these variables.
Categories of PET/CT actionable findings
(Adapted on the original ACR Actionable Reporting Work Group structure) [2]
Category 1: communication: direct verbal communication within minutes/hours. Action: to request an urgent evaluation by the referring clinician or by the emergency department
This category includes those findings that could lead to significant morbidity and need an urgent evaluation by the referring clinician or by the emergency department. These findings usually require a direct verbal communication within minutes/hours to avoid complications: the final report and key images should be elaborated as soon as possible and a short but complete clinical history should be promptly available.
Sending the patient to the emergency department is only one of the possibilities. In most institutions, the Nuclear Medicine specialist or radiologist would contact the referring physician who will decide (conjointly) on the next steps to be taken. Ideally, those steps should not be left to the decision of the individual imaging specialist but they should follow a shared standardised operative procedure (SOP).
Keypoints
Findings related with high risk of acute complications need urgent non-routine communication within minutes/hours with specialist evaluation.
To explore all the body districts, even if not related with the clinical question is mandatory and to check previous available images (e.g. PET/CT, diagnostic CT, MRI) is recommended.
The most frequent actionable findings in this category are bone lytic lesions at risk of instability (i.e. cervical vertebral or femoral lesions).
Category 2: communication: direct communication within a day/few days. Action: to inform the referring clinician
The actionable findings in this category are characterised by clinically significant findings, often associated with the main disease under assessment, that require a specific clinical or surgical evaluation but without the urgency and severity of the category 1. The interpretation of this category is controversial, because it represents a grey zone of severity and the inter-observer variability could be more relevant. A multidisciplinary approach should be warranted to correctly define the timing and to take the best choice.
Another goal to achieve is to ensure that the patient remains in a dedicated clinical-diagnostic work-flow: this may reduce the risk of a subsequent adverse event related to the overlapping of multiple figures potentially leading to an underestimation of the risk and delayed treatments. The adherence to a dedicated pathway may play a significant role particularly when a correct diagnosis has consequences not only for the patient’s but also for the community (i.e. unexpected potentially contagious infectious process) [14].
Keypoints
Findings related with moderate risk of morbidity need non-routine communication within a day/few days.
The adherence to a dedicated institutional diagnostic–therapeutic pathway may improve the patient’s outcome and avoid diagnostic delay.
A multidisciplinary approach, both clinical or surgical and radiologic, could help the reporting physician to be more confident in his final interpretation.
Category 3: communication: standard report delivery. Action: recommendation of dedicated investigation/monitoring of the finding in the report
This category includes all the actionable findings that do not require immediate treatment or counselling because likely not related to important risk or clinical consequences for the patient. It may include the findings that remain unclear for the reporting physician or may need a follow-up or a different imaging examination to be correctly assessed. Although these findings are less important in terms of timing, they might be relevant from the clinical point of view. For this reason, it is recommended to avoid the use of word such as “accessory” when reporting them and to recall the attention of the referring clinician, recommending investigation/monitoring (the best timing for follow-up and the most appropriate diagnostic technique to better characterise the finding should be discussed multidisciplinary, if not indicated in the report).
As a larger proportion of elderly patients and/or of patients with comorbidities is expected as population demographics change, it will be increasingly important to consider unexpected clinically significant findings on PET/CT imaging with more standardised and cost-effective approaches [15].
Keypoints
Findings related with mild risk of morbidity do not require a non-routine communication but should be correctly underlined in the report.
The reporting physician should suggest the most appropriate imaging investigation and/or follow-up timing to better characterise the finding.
The information technology (IT) service may play a role in the future to automatically recognize actionable findings and avoid underestimation.
Clinical applications
Hybrid imaging combines functional and anatomical information; all PET/CT systems permit multi-bed, whole-body imaging within a single examination, using the non-diagnostic CT for attenuation correction and anatomical mapping of the PET data [16]. Although the low/intermediate-dose CT performance remains sub-optimal for a diagnostic intent, it can definitely provide important information. The Nuclear Medicine physician might not have the comprehensive knowledge to accurately define all CT findings; however, he/she should be confident with the most relevant ones potentially representing a risk for the patient and include them in the final report.
In the following paragraphs, our aim is to describe some critical findings that could be detected on PET/CT images, divided by anatomical district, and to report a suggestion of a corresponding category (1–3) in brackets.
Overall, particular attention should be paid to the following findings, if unknown (see also Table1):
Vertebral and femoral bone lytic lesions;
Collections compatible with haemorrhage;
Aortic aneurysm;
Pneumothorax;
Lung consolidations in keeping with active pneumonia at risk of contagiousness (i.e. COVID-19 or open bronchus tuberculosis-tbc), requiring isolation;
Bowel occlusion/sub-occlusion;
Hydronephrosis.
Skeletal system
Most of the examinations in a PET Centre are performed in oncological patients; however, some actionable findings, even if related to the primary oncological disease, may need a different specialist evaluation. From our experience, the most frequent causes of urgency are unknown spinal bone lesions (especially cervical) at risk of instability. Independently from their impact on the oncological stage, the spinal bone lesions, when significant, could lead to severe acute complications and require urgent evaluation.
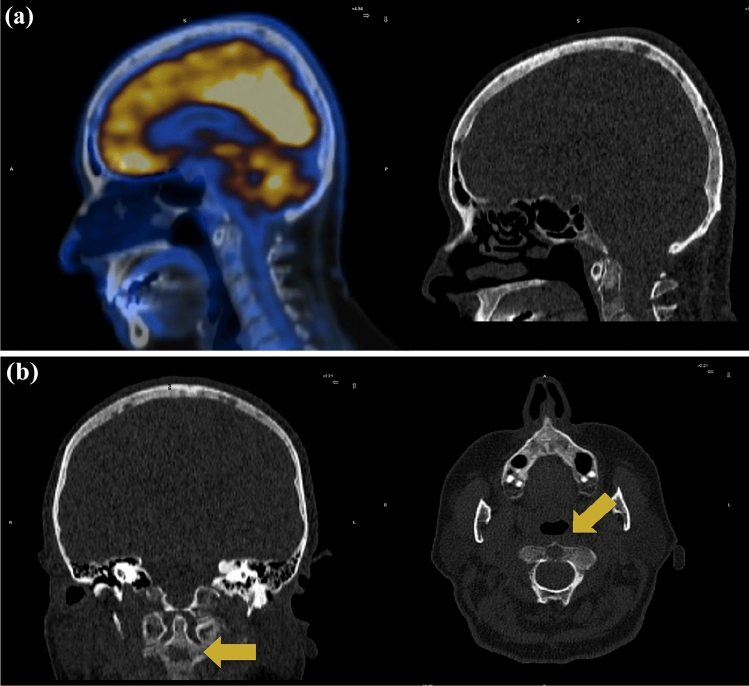
For example, a patient was addressed to our Nuclear Medicine Unit to perform a [18F]-FDG PET/CT scan for staging multiple myeloma; a previously unknown large lithic lesion of C2 vertebral body, with posterior wall cortical interruption, was detected on low-dose CT (LDCT) images (category 1), although non [18F]-FDG avid and without significant symptoms (Fig. 1). A high risk of instability and severe complication was estimated. The PET/CT report was finalised immediately and the patient was sent to the emergency department where the orthopaedic counselling prescribed the use of a Philadelphia collar. In approximately 1 h, the patient was safely discharged with the specific orthopaedic collar, and the referring haematologist was informed about the clinical evolution.
Fig. 1.
Category 1. Unknown lytic lesion of C2 body at risk of fracture (arrows) and lytic lesions of the skull detected on CT images of a whole-body [18F]-FDG PET/CT performed for staging multiple myeloma. a No FDG uptake was shown on PET images; b irregular margins and posterior wall cortical interruption was detected on the low-dose CT images. In this case the patient was sent to the emergency department where the orthopaedic counselling prescribed the use of a Philadelphia collar
There are different referring scales designed for traumatic fractures that can be used to stratify the risk of fracture also in non-traumatic lytic lesions. Specifically, for cervical spine, we can refer to the “Anderson and D’alonzo” [17] classification with three different types of fractures that can derive from the bone lesion. For oncologic lytic lesions, we can refer to a useful score system: the Spinal Instability Neoplastic Score (SINS) [18]. The SINS score helps to assess tumour-related instability of the vertebral column and to guide the management of patients with neoplastic spinal disease; the final score can stratify and select patients for whom an orthopaedic evaluation should be scheduled in the short time or those requiring a direct transfer to the emergency department.
Not only the cervical bones are at risk of adverse events due to lytic lesions, but also the long bones. The “Mirels” [19] classification is a system used to predict the risk of pathological fracture amongst metastatic long bones, and is based on site, location, matrix and other clinical features such us the presence of pain. The final score suggests the correct management and the risk of fracture if that area will be radio-treated. Some studies showed how both SINS and Mirels classifications could lead to unnecessary treatment, but we should keep in mind that the intent of the Nuclear Medicine physician is to preliminarily identify and secure the patient at risk and not to choose the subsequent correct treatment for the patient.
In oncological patients, we are used to pay particular attention to the bone compartment, which can often be involved by metastatic localizations. However, it is a good practice to explore it routinely and carefully in any patient, because lytic lesions (variable category from 1 to 3, depending on location and characteristics) can be found also in non-malignant diseases and without significant symptoms. For example, Nanda S. and colleagues described a case of extensive asymptomatic osteolytic vertebral involvement by sarcoidosis [20]. Histopathological characterisation should be warranted to rule out other aetiologies of non-caseating epithelioid granuloma such as tumour-related granulomas that mimic sarcoid or other infectious granulomas (i.e. tbc).
Independently from their nature and according to the anatomical structure involved, spinal lesions can be differentiated in extradural, extramedullary-intradural and intramedullary [21]. Galbusera and colleagues highlighted the fundamental role of the tumour size on the fracture risk in metastatic spine, but also of the vertebral bulge on the transverse plane and of the canal narrowing [22].
In an unexpected lesion, all these parameters can be preliminarily evaluated on PET/CT images, and further investigated with specific CT reconstruction for a better bone/soft tissue resolution, and/or with dedicated MRI sequences to support management decisions.
Cardiovascular system
Diffuse or even focal [18F]-FDG uptake without pathological significance can be observed in heart tissue in fasted patients [23]; for example, focal uptake can be observed in papillary muscles, the atria, the base and the distal antero-apical region of the left ventricle reflecting the physiologic heart activity. Other FDG distribution patterns can be considered abnormal but not related to malignancy and can be observed in increased atrial activity associated with atrial fibrillation or prominent crista terminalis, lipomatous hypertrophy of the interatrial septum, epicardial and pericardial fat, endocarditis, myocarditis, pericarditis and cardiac sarcoidosis. The detection of unknown intracardiac mass is also a challenging diagnostic issue: the presence of hypodense mass on CT images can be related to a different diagnostic hypothesis and, amongst them, the most frequent are intracardiac thrombus, cardiac tumours or vegetations. FDG images could help to better characterise the mass providing metabolic information: two recent trials [24, 25] reported a good accuracy of FDG PET/CT in distinguishing benign from malignant mass. However, in case of malignancy, the FDG avidity varies depending on the histopathology [26], and sensitivity and specificity could be increased, thanks to morphological-CT features: indeed, the presence of irregular margins, necrosis, pericardial or pleural effusion, involvement of epicardium or adjacent tissue, are more likely correlated with malignant disease [27]. Intracardiac thrombus can occur after myocardial infarction, atrial fibrillation or mitral stenosis and it is correlated with severe morbidity due to embolic events. The FDG uptake in thrombus varies from intense to absent [28] depending on the amount of macrophages infiltration and metabolic active tissue; in fact, a focal intense uptake has been reported also in organised atrial thrombus, mimicking malignancy [29]. It is important to be able to correctly distinguish physiologic, abnormal or malignant patterns to recognize the possible presence of diseases involving heart cameras, paracardiac spaces, myocardium, and pericardium.
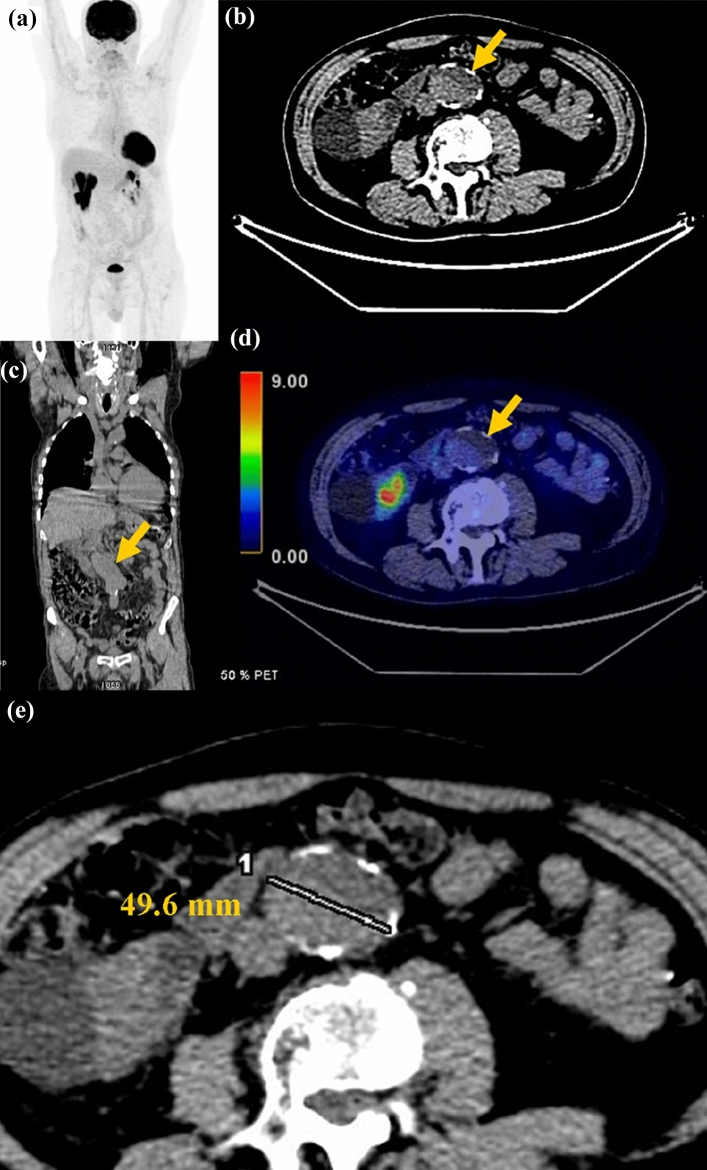
Aortic aneurysm is a dilatation of the aortic lumen that affects most frequently the abdominal tract than the thorax one. The normal aortic diameter varies based on age, sex and body surface area but the term “aneurysm” can be used when the axial diameter is > 5 cm for the ascending aorta (the most commonly affected tract amongst thoracic aneurysm) and > 4 cm for the descending aorta [30]. For the abdominal tract, the term “aneurysm” can be used when the axial diameter is > 3 cm or 50% greater than the proximal normal tract [31]. The risk of rupture and the corresponding category of urgency both depend mostly on the aortic diameter [32] but it can be influenced by other factors: for example, the risk of rupture in male patients with abdominal aortic aneurysm from 5.0 to 5.9 cm is low (category 3) (Fig. 2), whilst in female patients, the risk is four-times higher suggesting that a lower threshold for surgery should be considered in fit women (category 2/3). For instance, the risk of rupture of abdominal aortic aneurysm greatly increases with diameter of 6.0 cm both in male and in female (category 2/3) requiring a prompt surgical counselling. Other features should be useful in the report [33]: (1) size and shape: dimension, luminal diameter (if luminal thrombus is present), longitudinal length, fusiform or saccular; (2) relationship with other vessels (although PET/CT accuracy is limited by the absence of contrast media administration): upper distance from renal arteries and from common iliac artery, if these vessels are interested, location and relationship with other branches involved; (3) complications: proximity to bowel, presence of mural calcifications or mural thrombus, rupture (FDG accumulation amongst the wall similar to blood pool). Furthermore, secondary findings correlated with elevated risk of complications are: the interval growth (when multiple imaging studies are available), the presence of intramural hematoma (can be considered a dissection variant and require urgent surgical repair) and the suspect of rupture or leak (aortic fat stranding, high-density periaortic fluid collection, pleural/pericardial effusion).
Fig. 2.
Category 3. a Abdominal aortic aneurism (arrows). a Maximum Intensity Projection (MIP) negative for focal tracer uptake. b aneurismatic tract on transaxial CT images; c aneurismatic tract on coronal CT images; d aneurismatic tract on PET/CT images showed physiologic blood pool uptake and aneurismatic lumen with mural calcifications; e aneurismatic tract measurement on transaxial CT images. In this case a urgent surgical counselling was requested to evaluate a possible surgical treatment
Brain and skull
Differentiation between tumour and tumour-like lesions of the central nervous system is crucial for planning the correct management, prognosis and follow-up. The physiological FDG uptake of the brain tissue may decrease PET/CT sensitivity when performed without the specific intent to characterise a brain lesion, particularly in lesions with low glucose metabolism. Since several non-neoplastic pathologies may present as mass lesion, the reporting physician should be aware of the extensive differential diagnoses and identify which findings deserve additional studies or follow-up [34].
The presence of acute blood intracranial haemorrhage usually appears as an area with mild FDG uptake corresponding to a hyperdense area on CT images (category 1/2), but in some cases, organised hematoma may present intense focal uptake mimicking malignant mass [35].
Also, skull lesions can be incidentally found on the CT component and it is important to be familiar with their imaging characteristics and to recognise those with malignant features that require an urgent management (category 2/3). Clinical information such as the age of the patient, as well as the patient’s history, are fundamental for a correct interpretation. More frequently benign lesions present sharp margins, narrow zone of transition, uninterrupted periosteal rim and do not involve the surrounding soft tissue, whereas malignant lesions may present wide zone of transition, poorly defined margins and periosteal interruption with soft tissue component (category 3). If the imaging reporter does not feel confident enough to interpret the nature of the lesions as benign or malignant, it remains important to specify if an additional diagnostic study is required.
Thorax
As reported in several studies, when [18F]-FDG PET/CT is performed for standard clinical application, it is not rare to find incidental findings suggestive for infectious diseases (e.g. the detection of unexpected pulmonary infiltrates, lung consolidation or cavitation) that might require a prompt isolation of the patient, even if asymptomatic (category 2) [36–38].In the last 2 years, the most frequent clinical condition related to this risk in PET/CT departments was asymptomatic COVID-19 lung infection in patients undergoing PET/CT scan for other clinical requests. In patients with COVID-19, FDG uptake in lung segmental ground-glass opacities and consolidations is the most common feature but it remains unspecific, being observed also in pneumonia caused by other aetiologies. Other findings suggestive for COVID-19 could be considered enlarged pulmonary vessels (64%), septal (60%) and pleural thickening (42%), the crazy paving pattern (ground glass opacities in combination with underlying interlobular septal thickening) and the reversed halo sign. The reported distribution of the pulmonary CT findings is bilateral (79%), multifocal (70%) or sometimes patchy, with a predominance of the lung periphery and the bases of the lung. Recently, a three grade scale (low, moderate and high) for the suspicion for COVID-19 pneumonia has been proposed based on chest CT patterns [39].
Unexpected findings suggestive for tuberculosis infection (category 2/3) may have a similar impact on patient’s management (Fig. 3). In literature, two distinct patterns of pulmonary tuberculosis have been described: (1) the lymphatic pattern, with more enlarged and FDG avid hilar and mediastinal lymph nodes and (2) the lung pattern, with FDG avid lung consolidation and cavitation surrounded by micronodules and mild uptake within mediastinal lymph nodes [40]. FDG PET–CT can help in differentiating active pulmonary tuberculosis from previous or inactive disease, because active tuberculoma show more avid FDG uptake [41]. To note that the most important step is to identify patients with high risk of open infectious/active pulmonary tuberculosis who should be isolated (category 1/2): a cavity lesion, consolidation involving the superior segment of the right or left lower lobe, consolidation involving the apex or the posterior segment of the right upper lobe or the apicoposterior segment of the left upper lobe, the absence of centrilobular nodules and clusters of nodules are all findings related with higher contagiousness [42].
Fig. 3.
Category 2. a FDG-PET/CT showed pulmonary consolidation on the right lung close to the broncus with mild FDG uptake. b High Resolution CT showed more clearly that the bronchus was going through the consolidation. In this case the patient required isolation due to the risk of contagious active infection
A clinical and radiological consultation may help in better assess the relevance of the finding, because the same one can differently impact on the patient’s management depending on comorbidities and risk factors.
Cardiac effusion ranges from mild asymptomatic (category 2/3) to cardiac tamponade (category 1) with unspecific symptoms such as chest pain with tightness, dyspnoea and fatigue. The accepted thickness of a normal pericardium on CT images is 2 mm and became to be considered pathological when > 3–4 mm [43]. Pericardial sac normally contains between 15 and 30 ml but is considered physiologic up to 50 ml. The presence of a large fluid effusion can be related to different disease (infection, myocardial disease, trauma, malignancies, kidney insufficiency) and warrants reporting.
Other possible mediastinal findings are pericardial recesses [44] (aortic, pulmonic, post-caval, posterior pericardial, pulmonary venous), and pericardial cysts, rare and usually considered as benign findings [45]. When pericardial fluid pool in the recess, it should not be confused with a pathologic lymph node, especially in oncologic patients.
Pneumothorax describes a condition in which there is air within the pleural space; it can be spontaneous, related to a lung disease (e.g. emphysema, asthma, honeycombing, cystic fibrosis, parenchymal necrosis), iatrogenic (percutaneous or transbronchial biopsy perforation of the oesophagus, radiofrequency ablation of a lung mass, central venous catheterization) or traumatic. Clinical presentation depends on the extension and can range from asymptomatic to severe dyspnoea. In a PET Centre, pneumothorax can be observed in patients performing PET/CT after biopsy procedures [46, 47] on a lung or pleural lesion: in these patients, a careful exploration of the chest is recommended even if no pneumothorax is described after the invasive diagnostic procedure. On CT images, even a small pneumothorax can be detected thanks to the presence of air (black signal) around the edge of the lung; on the other hand, a massive pneumothorax usually also shows diffuse mild FDG uptake of the collapsed lung parenchyma and, in case of tension pneumothorax, a typical mediastinal shift (category 1).
Gastrointestinal
Small bowel obstruction presenting with cramping abdominal pain and abdominal distension with nausea and vomiting but radiographic signs can be evident 6–12 h before the onset of clinical symptoms [48]. Suggestive signs on CT images may be: dilated small bowel loops ≥ 2.5 cm up and normal calibre or collapsed loops distally or small bowel faecal sign (faecal like material in dilated small bowel loops). Closed-loop obstructions are diagnosed when a bowel loop is occluded at two adjacent points, showing radial distribution of several dilated, fluid-filled bowel loops, U-shaped or C-shaped configuration, beak sign at the site of fusiform tapering, whirl sign (rotation of bowel loops around a fixed point) [49]. Due to the possible lack of clinical information in the routine PET/CT practice, it is important to focus on the abnormal bowel aspect and then to communicate directly with patient and/or referring clinician for a better interpretation of the urgent condition (sub-occlusion versus occlusion) (category 2 vs. 1).
Gallstone disease is highly prevalent in general population and is a frequent cause of hospitalisation; it is more frequently observed in elderly population and in females [50]. The clinical presentation ranges from asymptomatic, non-complicated symptomatic to complicated symptomatic disease. In asymptomatic carrier patients, it is important to report the presence of gallstone close to the neck of the gallbladder (category 3) because it can become lodged in common cystic duct and provoke acute cholecystitis, gangrene and perforation; gallstone may direct fistulate into the duodenum after a period of silent inflammation and lead to duodenal obstruction (Bouveret’s syndrome), or compress the common hepatic duct leading to jaundice (Mirizzi syndrome) [51].
Pneumoperitoneum describes the presence of air within the peritoneal cavity and can be an indirect sign of perforation of intestine (category 1/2).
Hemoperitoneum is the presence of blood in the peritoneal cavity (category 1/2); the composition of the fluid could be defined by its CT density: recent haemorrhage (acute bleed) measures 30–45 HU, clotted blood measures 45–70 HU, old blood products/seroma or blood in patients with anaemia may measure < 30 HU [52].
Genitourinary
Severe hydronephrosis should be reported and promptly communicated to the referring clinician (category 1/2) because complete urinary blockage can damage the kidney and lead to kidney failure whilst, if promptly treated, most of the patients can completely recover. Hydronephrosis can be due to an obstructive process at any level of the ureter (stone, ab-extrinseco compression, abdominal fibrosis) or congenital (Hirschsprung’s disease, infection, toxic/hormonal/neuromuscular factors). Images can reveal abnormal accumulation of the FDG tracer (characterised by physiologic renal excretion) up to obstructed tract, with different grade of pelvic dilatation that can be estimated on the corresponding CT images.
Conclusion
In the daily PET/CT practice, it is not rare to report findings that might not represent an immediate risk for the patient but still require a timely specialist evaluation to avoid complications. These cases fall in a grey zone of communication between different care figures with the risk of being underestimated.
A systematic categorization of the actionable imaging findings, according to their urgency, may help the reporting physician to choose how and when to communicate with the referring clinician and to be more confident with cases requiring a prompt clinical evaluation. We revised and adapted the ACR Work Group categorization of radiological actionable findings specifically focussing on PET/CT daily practice. Each institute should construct its internal actionable finding’s categorization based on their patients’ settings and health care environment. Effective communication is a critical component of diagnostic imaging: timely receipt of the information is more important than the method of delivery.
Author contributions
FM: conceptualization, literature searching, drafting, reviewing and editing. LZ: conceptualization, reviewing and editing. All the authors: reviewing and editing.
Funding
Not applicable.
Data availability
Data were obtained using a literature review that can be viewed based on given references.
Code availability
Not applicable.
Declarations
Conflict of interest
All the authors declare no conflict of interest regarding this topic.
Ethical approval
This article does not contain any clinical studies with human participants or animals performed by any of the authors. The anonymized images included in this review have been used only to provide an example of the covered topics. All the patients who accessed to our institute subscribe an informed consent for the use of their anonymized data (including diagnostic images) for research purposes.
Footnotes
The original online version of this article was revised: Correction to article title.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
4/3/2023
A Correction to this paper has been published: 10.1007/s40336-023-00556-6
References
- 1.American College of Radiology, ACR Practice Parameter for Communication of Diagnostic Imaging Findings, (Revised 2020). https://www.acr.org/-/media/ACR/Files/Practice-Parameters/CommunicationDiag.pdf. Accessed dec 2021
- 2.Larson PA, Berland LL, Griffith B, Kahn CE, Jr, Liebscher LA. Actionable findings and the role of IT support: report of the ACR actionable reporting work group. J Am Coll Radiol. 2014;11(6):552–558. doi: 10.1016/j.jacr.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 3.Joint Commission’s National Patient Safety Goal. https://www.jointcommission.org/-/media/tjc/documents/standards/national-patient-safety-goals/2021/npsg_chapter_cah_jan2021.pdf. Accessed Dec 2021
- 4.Anthony SG, Prevedello LM, Damiano MM, et al. Impact of a 4-year quality improvement initiative to improve communication of critical imaging test results. Radiology. 2011;259(3):802–807. doi: 10.1148/radiol.11101396. [DOI] [PubMed] [Google Scholar]
- 5.Lacson R, Prevedello LM, Andriole KP, et al. Four-year impact of an alert notification system on closed-loop communication of critical test results. AJR Am J Roentgenol. 2014;203(5):933–938. doi: 10.2214/AJR.14.13064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baccei SJ, DiRoberto C, Greene J, Rosen MP. Improving communication of actionable findings in radiology imaging studies and procedures using an EMR-independent system. J Med Syst. 2019;43(2):30. doi: 10.1007/s10916-018-1150-z. [DOI] [PubMed] [Google Scholar]
- 7.Visser JJ, de Vries M, Kors JA. Assessment of actionable findings in radiology reports. Eur J Radiol. 2020;129:109109. doi: 10.1016/j.ejrad.2020.109109. [DOI] [PubMed] [Google Scholar]
- 8.Heilbrun ME, Chapman BE, Narasimhan E, Patel N, Mowery D. Feasibility of natural language processing-assisted auditing of critical findings in chest radiology. J Am Coll Radiol. 2019;16(9 Pt B):1299–1304. doi: 10.1016/j.jacr.2019.05.038. [DOI] [PubMed] [Google Scholar]
- 9.Meng X, Ganoe CH, Sieberg RT, Cheung YY, Hassanpour S. Assisting radiologists with reporting urgent findings to referring physicians: a machine learning approach to identify cases for prompt communication. J Biomed Inform. 2019;93:103169. doi: 10.1016/j.jbi.2019.103169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.https://www.acr.org/Clinical-Resources/Incidental-Findings. Accessed 10 Jan 22
- 11.O'Sullivan JW, Muntinga T, Grigg S, Ioannidis JPA. Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ. 2018;361:k2387. doi: 10.1136/bmj.k2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pencharz D, Nathan M, Wagner TL. Evidence-based management of incidental focal uptake of fluorodeoxyglucose on PET-CT. Br J Radiol. 2018;91(1084):20170774. doi: 10.1259/bjr.20170774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Port S. Incidental findings on hybrid SPECT-CT and PET-CT scanners: is it time for new training and reporting guidelines? J Nucl Cardiol. 2019;26(5):1694–1696. doi: 10.1007/s12350-018-1257-0. [DOI] [PubMed] [Google Scholar]
- 14.Li Y, Behr S. Acute findings on FDG PET/CT: key imaging features and how to differentiate them from malignancy. Curr Radiol Rep. 2020;8(11):22. doi: 10.1007/s40134-020-00367-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adams SJ, Rakheja R, Bryce R, Babyn PS. Incidence and economic impact of incidental findings on 18F-FDG PET/CT imaging. Can Assoc Radiol J. 2018;69(1):63–70. doi: 10.1016/j.carj.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Townsend DW. Multimodality imaging of structure and function. Phys Med Biol. 2008;53(4):R1–R39. doi: 10.1088/0031-9155/53/4/R01. [DOI] [PubMed] [Google Scholar]
- 17.Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56(8):1663–1674. doi: 10.2106/00004623-197456080-00017. [DOI] [PubMed] [Google Scholar]
- 18.Fox S, Spiess M, Hnenny L, Fourney DR. Spinal instability neoplastic score (SINS): reliability among spine fellows and resident physicians in orthopedic surgery and neurosurgery. Global Spine J. 2017;7(8):744–748. doi: 10.1177/2192568217697691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jawad MU, Scully SP. In brief: classifications in brief: Mirels’ classification: metastatic disease in long bones and impending pathologic fracture. Clin Orthop Relat Res. 2010;468(10):2825–2827. doi: 10.1007/s11999-010-1326-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nanda S, Bhatt SP, Steinberg D, Volk SA. Unusual cause of generalized osteolytic vertebral lesions: a case report. J Med Case Rep. 2007 doi: 10.1186/1752-1947-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen TT, Thelen JC, Bhatt AA. Bone up on spinal osseous lesions: a case review series. Insights Imaging. 2020;11(1):80. doi: 10.1186/s13244-020-00883-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galbusera F, Qian Z, Casaroli G, et al. The role of the size and location of the tumors and of the vertebral anatomy in determining the structural stability of the metastatically involved spine: a finite element study. Transl Oncol. 2018;11(3):639–646. doi: 10.1016/j.tranon.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maurer AH, Burshteyn M, Adler LP, Steiner RM. How to differentiate benign versus malignant cardiac and paracardiac 18F FDG uptake at oncologic PET/CT. Radiographics. 2011;31(5):1287–1305. doi: 10.1148/rg.315115003. [DOI] [PubMed] [Google Scholar]
- 24.Qin C, Shao F, Hu F, et al. 18F-FDG PET/CT in diagnostic and prognostic evaluation of patients with cardiac masses: a retrospective study. Eur J Nucl Med Mol Imaging. 2020;47(5):1083–1093. doi: 10.1007/s00259-019-04632-w. [DOI] [PubMed] [Google Scholar]
- 25.D'Angelo EC, Paolisso P, Vitale G, et al. Diagnostic accuracy of cardiac computed tomography and 18-F fluorodeoxyglucose positron emission tomography in cardiac masses. JACC Cardiovasc Imaging. 2020;13(11):2400–2411. doi: 10.1016/j.jcmg.2020.03.021. [DOI] [PubMed] [Google Scholar]
- 26.Meng J, Zhao H, Liu Y, et al. Assessment of cardiac tumors by 18F-FDG PET/CT imaging: histological correlation and clinical outcomes. J Nucl Cardiol. 2021;28(5):2233–2243. doi: 10.1007/s12350-019-02022-1. [DOI] [PubMed] [Google Scholar]
- 27.Bernhard B, Gräni C. 18F-FDG PET/CT imaging in the workup of cardiac and pericardial masses. J Nucl Cardiol. 2021 doi: 10.1007/s12350-021-02539-4. [DOI] [PubMed] [Google Scholar]
- 28.Rinuncini M, Zuin M, Scaranello F, et al. Differentiation of cardiac thrombus from cardiac tumor combining cardiac MRI and 18F-FDG-PET/CT Imaging. Int J Cardiol. 2016;212:94–96. doi: 10.1016/j.ijcard.2016.03.059. [DOI] [PubMed] [Google Scholar]
- 29.Chaudhuri KG, Revels JW, Yadwadkar KS, Johnson LS. Intense 18F-FDG uptake in an organizing right atrial thrombus mimicking malignancy. Radiol Case Rep. 2017;12(3):449–454. doi: 10.1016/j.radcr.2017.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gaillard F, Knipe H. Thoracic aortic aneurysm. Reference article, Radiopaedia.org. (Accessed on 17 Apr 2022) 10.53347/rID-8884
- 31.D’Souza D, Gaillard F. Abdominal aortic aneurysm. Reference article, Radiopaedia.org. (Accessed on 17 Apr 2022) 10.53347/rID-826
- 32.Davies RR, Goldstein LJ, Coady MA, et al. Yearly rupture or dissection rates for thoracic aortic aneurysms: simple prediction based on size. Ann Thorac Surg. 2002;73(1):17–28. doi: 10.1016/s0003-4975(01)03236-2. [DOI] [PubMed] [Google Scholar]
- 33.Gaillard F, Bell D. Reporting tips for aortic aneurysms. Reference article, Radiopaedia.org. (Accessed on 17 Apr 2022) 10.53347/rID-8885
- 34.Huisman TA. Tumor-like lesions of the brain. Cancer Imaging. 2009;9(Special issue A):S10–S13. doi: 10.1102/1470-7330.2009.9003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nakajima S, Okada T, Arakawa Y, Mikami Y, Togashi K. Organizing intracerebral hematoma mimicking a recurrent brain tumor on FDG-PET. Clin Nucl Med. 2013;38(11):e411–e413. doi: 10.1097/RLU.0b013e31827085ce. [DOI] [PubMed] [Google Scholar]
- 36.Halsey R, Priftakis D, Mackenzie S, et al. COVID-19 in the act: incidental 18F-FDG PET/CT findings in asymptomatic patients and those with symptoms not primarily correlated with COVID-19 during the United Kingdom coronavirus lockdown. Eur J Nucl Med Mol Imaging. 2021;48(1):269–281. doi: 10.1007/s00259-020-04972-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Albano D, Bertagna F, Bertoli M, et al. Incidental findings suggestive of COVID-19 in asymptomatic patients undergoing nuclear medicine procedures in a high-prevalence region. J Nucl Med. 2020;61(5):632–636. doi: 10.2967/jnumed.120.246256. [DOI] [PubMed] [Google Scholar]
- 38.Martí A, Morón S, González E, Rojas J. Incidental findings of COVID-19 in F18-FDG PET/CT from asymptomatic patients with cancer in two healthcare institutions in Bogotá, Colombia. Hallazgos incidentales de COVID-19 en tomografías PET/CT 18F-FDG de pacientes asintomáticos con cáncer en dos instituciones de salud de Bogotá, Colombia. Biomedica. 2020;40(Suppl. 2):27–33. doi: 10.7705/biomedica.5833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19) imaging reporting and data system (COVID-RADS) and common lexicon: a proposal based on the imaging data of 37 studies. Eur Radiol. 2020;30(9):4930–4942. doi: 10.1007/s00330-020-06863-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soussan M, Brillet PY, Mekinian A, et al. Patterns of pulmonary tuberculosis on FDG-PET/CT. Eur J Radiol. 2012;81(10):2872–2876. doi: 10.1016/j.ejrad.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 41.Bomanji JB, Gupta N, Gulati P, Das CJ. Imaging in tuberculosis. Cold Spring Harb Perspect Med. 2015;5(6):a017814. doi: 10.1101/cshperspect.a017814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yeh JJ, Chen SC, Teng WB, et al. Identifying the most infectious lesions in pulmonary tuberculosis by high-resolution multi-detector computed tomography. Eur Radiol. 2010;20(9):2135–2145. doi: 10.1007/s00330-010-1796-5. [DOI] [PubMed] [Google Scholar]
- 43.Munden RF, Carter BW, Chiles C, et al. Managing incidental findings on thoracic CT: mediastinal and cardiovascular findings. A white paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2018;15(8):1087–1096. doi: 10.1016/j.jacr.2018.04.029. [DOI] [PubMed] [Google Scholar]
- 44.Shroff GS, Boonsirikamchai P, Viswanathan C, Godoy MC, Marom EM, Truong MT. Differentiating pericardial recesses from mediastinal adenopathy: potential pitfalls in oncological imaging. Clin Radiol. 2014;69(3):307–314. doi: 10.1016/j.crad.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 45.Peebles CR, Shambrook JS, Harden SP. Pericardial disease: anatomy and function. Br J Radiol. 2011;84(Spec Iss 3):S324–S337. doi: 10.1259/bjr/16168253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ghofrani M, Kim B. Diagnosis of pneumothorax on F-18 FDG PET after transbronchial biopsy. Clin Nucl Med. 2005;30(10):692–694. doi: 10.1097/01.rlu.0000178243.63932.84. [DOI] [PubMed] [Google Scholar]
- 47.Sommerfeldt J, Miao TL, Zuckier LS, Gupta A. High prevalence of pneumothorax on PET-CT studies performed in lung cancer patients following post-transthoracic needle biopsy mandates careful scrutiny. Clin Nucl Med. 2017;42(8):637–638. doi: 10.1097/RLU.0000000000001716. [DOI] [PubMed] [Google Scholar]
- 48.Jones J, Shah V. Small bowel obstruction. Reference article, Radiopaedia.org. (Accessed on 18 Apr 2022) 10.53347/rID-6158
- 49.Chick JF, Mandell JC, Mullen KM, Khurana B. Classic signs of closed loop bowel obstruction. Intern Emerg Med. 2013;8(3):263–264. doi: 10.1007/s11739-012-0897-3. [DOI] [PubMed] [Google Scholar]
- 50.Shabanzadeh DM. Incidence of gallstone disease and complications. Curr Opin Gastroenterol. 2018;34(2):81–89. doi: 10.1097/MOG.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 51.Njeze GE. Gallstones. Niger J Surg. 2013;19(2):49–55. doi: 10.4103/1117-6806.119236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.St-Amant M, Hacking C. Hemoperitoneum. Reference article, Radiopaedia.org. (Accessed on 18 Apr 2022) 10.53347/rID-20113.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data were obtained using a literature review that can be viewed based on given references.
Not applicable.