Abstract
Whereas acute proximal tibiofibular joint (PTFJ) dislocation may require urgent reduction, chronic or recurrent instability may initially be approached with conservative treatment. Indications for PTFJ reconstruction include persistent lateral knee pain and/or tibiofibular instability for which conservative treatment has failed. Owing to the low incidence of diagnosed isolated PTFJ instability, there is still no consensus regarding the optimal surgical treatment, with an array of options having been previously described. We describe the treatment of isolated PTFJ instability using an anatomic reconstruction with semitendinosus allograft for chronic instability.
Technique Video
Preoperative planning and surgical technique for proximal tibiofibular joint reconstruction for chronic instability with semitendinosus allograft in left knee.
Instability of the proximal tibiofibular joint (PTFJ) is rarely diagnosed and often confused with other pathology of the knee.1 The PTFJ is stabilized by a stronger anterior capsular component and a weaker posterior capsular component. Anavian et al.2 performed a cadaveric study to describe the anatomy of the PTFJ ligamentous complex qualitatively and quantitatively in relation to relevant bony landmarks. They found that up to 4 bundles were identified anteriorly whereas up to 3 bundles were isolated posteriorly. Additionally, the inferior bundle was identified anteriorly and posteriorly in 60% and 20% of cases, respectively. See et al.3 reported that the anterior tibiofibular ligament attaches 15.6 mm posterolateral to the Gerdy tubercle and 17.3 mm anteroinferior to the fibular styloid. Comparatively, the posterior tibiofibular ligament attaches 15.7 mm inferior to the lateral tibial plateau articular surface and 14.2 mm medial to the fibular styloid.3
Ogden4 first described the main function of the PTFJ to dissipate torsional stresses applied at the ankle, lateral tibial bending moments, and tensile forces for weight bearing.5 During dorsiflexion of the ankle, the proximal fibula is known to externally rotate at the PTFJ. During flexion of the knee, a gliding movement is observed in the anterior-posterior axis at the PTFJ and more knee flexion results in the proximal fibula moving anteriorly with relative relaxation of the fibular collateral ligament and the biceps femoris. Comparatively, extension of the knee results in these structures becoming taut, pulling the fibula posteriorly.4, 5, 6, 7 Anterolateral dislocation has classically been reported as the most common PTFJ instability pattern, corresponding to 67% of cases in the landmark study by Ogden4 and 77% to 90% of cases in a recent meta-analysis by Kruckeberg et al.8
Chronic instability cases typically respond poorly to conservative treatment, and closed reduction is no longer an option.4,9 Owing to the low incidence of diagnosed isolated PTFJ instability, there is still no consensus regarding the optimal surgical treatment, with an array of options having been previously described.4,9, 10, 11 Reconstruction procedures with anatomic-based techniques are supported by the recent literature as promising options with satisfactory outcomes and low complication rates.8,11,12 Nevertheless, the use of autografts can disrupt secondary stabilizers (e.g., biceps tendon or iliotibial band [ITB]) or potentially result in donor-site morbidity and decreased function of the harvested structure.13,14 In this article, we describe the treatment of isolated PTFJ instability using an anatomic reconstruction with semitendinosus allograft for chronic instability (Video 1).
Surgical Technique
Preoperative Evaluation and Surgical Decision Making
As opposed to acute PTFJ dislocation, which requires urgent reduction—whether closed or, occasionally, open—chronic or recurrent instability may initially be approached with conservative treatment.9 Indications for reconstruction include persistent knee pain and/or rotational instability for which conservative treatment has failed.
Preoperative planning should aim to identify possible concomitant lesions that would require additional procedures (meniscal repair, cartilage restoration, and so on), particularly in the setting of traumatic injuries, or degenerative changes that may hinder the outcomes of a reconstruction. Routine radiographs (anteroposterior, lateral, and axial views) should be obtained to assess for fracture, dislocation, or arthritic changes. Additionally, in cases in which pathology extending to the distal tibiofibular ligaments is suspected, bilateral comparative stress radiographs of the ankle should be obtained.10 Magnetic resonance imaging is typically obtained to assess for any additional soft-tissue injuries, and a computed tomography scan can be used to obtain the rotational profile as well as rule out occult fracture if there is a high suspicion. Older patients in whom degenerative changes have already developed and who complain of isolated pain without instability may be suited for PTFJ arthrodesis.
Patient Positioning and Anesthesia
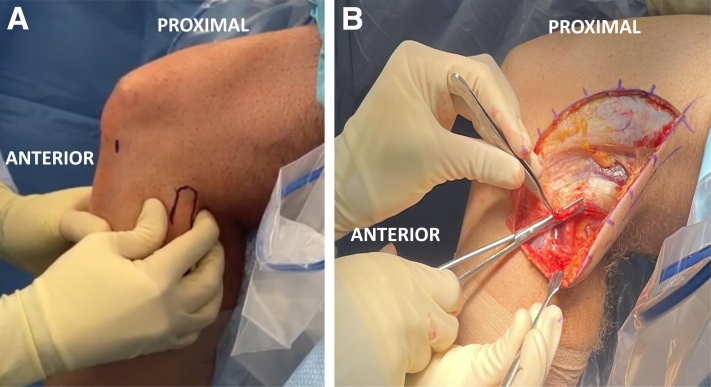
The patient is placed in a supine position under general anesthesia. A bilateral comparative examination under anesthesia confirms the diagnosis of PTFJ instability (Fig 1A). A padded pneumatic tourniquet is placed on the upper thigh of the operative leg, with the contralateral leg secured in extension with a pneumatic compression device. A regional nerve block and periarticular infiltrations are used to maximize postoperative pain management and optimize same-day patient discharge.
Fig 1.
Intraoperative lateral view of left knee. (A) Examination of proximal tibiofibular joint stability is performed with the patient under anesthesia. The proximal fibula is outlined with a marking pen, and a comparative bilateral examination is performed. (B) Initial exposure via a 15-cm hockey-stick incision is performed in line with the iliotibial band fibers.
Surgical Approach and Peroneal Nerve Neurolysis
A hockey-stick incision of about 15 cm is made along the posterior limit of the ITB extending slightly distally past the Gerdy tubercle (Fig 1B). Superficial dissection is then commenced until the ITB fibers are identified, and a subfascial posteriorly based flap is developed. Peroneal nerve neurolysis is performed to minimize the risk of intraoperative nerve injury and postoperative compression due to swelling. Open neurolysis of the common peroneal nerve and tunnel preparation precede any arthroscopic steps with the aim of avoiding distorted anatomy after tissue infiltration due to fluid extravasation.
The common peroneal nerve is located posteromedially to the long head of the biceps femoris, along the fibular neck. Neurolysis should begin at the fibular neck and should be carried out proximally about 6 cm and distally 5 to 7 mm into the peroneus longus fascia. In the setting of a subluxated fibular head, the anatomy may be distorted, increasing the risk of iatrogenic damage to the peroneal nerve during exposure.
Graft Preparation
A semitendinosus allograft (JRF Ortho, Englewood, CO) is prepared on the back table. The extremities of the graft are prepared with No. 2 nonabsorbable high-strength suture loops (FiberLoop; Arthrex, Naples, FL). The graft is tested to fit smoothly into 6-mm tunnels and is then soaked in a solution of vancomycin until the 2 tunnels in the tibia and fibula have been prepared.
Tunnel Formation
Exposure of the PTFJ is achieved via the interval between the soleus muscle and the lateral head of the gastrocnemius tendon. Elevating the soleus from the posterior surface of the fibula and tibia directly exposes the posterior aspect of the PTFJ (Fig 2A). A Chandler retractor is carefully positioned anterior to the lateral gastrocnemius tendon to protect the common peroneal nerve and vascular structures during tunnel formation (Fig 2B).
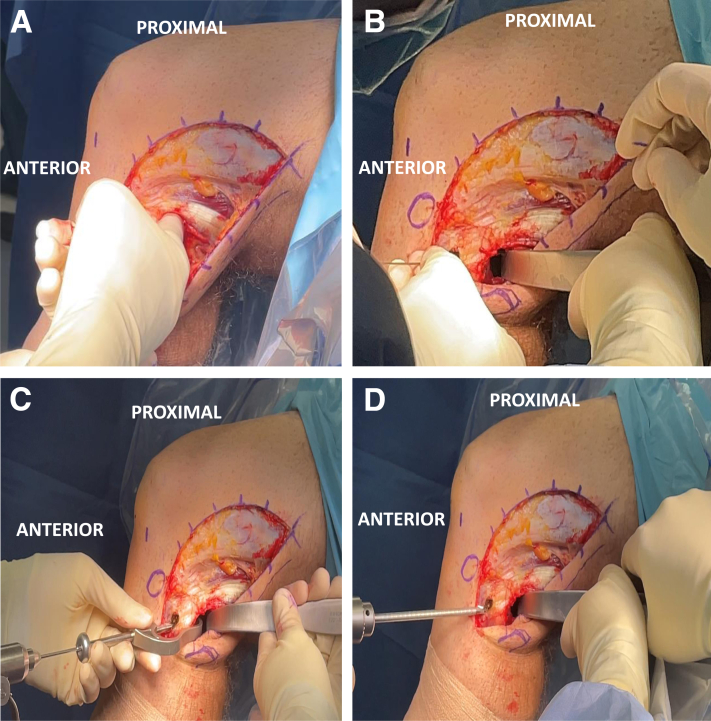
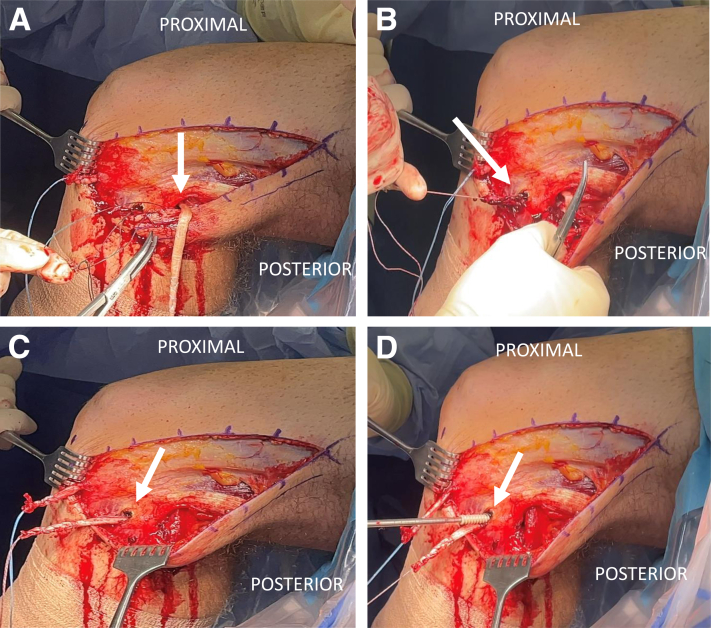
Fig 2.
Fibular tunnel formation in left knee (lateral view). (A) Blunt elevation of soleus muscle and fingertip palpation of posterior aspect of proximal tibiofibular joint. (B) Chandler retractor placement protects the common peroneal nerve and vascular bundle during tunnel formation. (C) Fibular aiming guide and 2.4-mm guide pin in place on fibular head with entry point on anterolateral aspect and aimed posteromedially, exiting just distal to fibular insertion of popliteofibular ligament. (D) Final fibular tunnel formation with 6-mm cannulated reamer over guide pin while Chandler retractor is kept in place to protect neurovascular bundle.
For the fibular tunnel, an aiming guide (Acufex Extra-articular Reconstruction Guide System; Smith & Nephew, Andover, MA) is positioned in the fibular head, with the entry point on the anterolateral aspect and aimed posteromedially, exiting just distal to the fibular insertion of the popliteofibular ligament. With the retractor already in place, a 2.4-mm guide pin is driven and subsequently over-reamed using a 6-mm cannulated reamer (Fig 2 C and D). A passing stitch is then threaded through the fibular tunnel with a suture passer (Hewson Suture Passer; Smith & Nephew) to guide later graft passage.
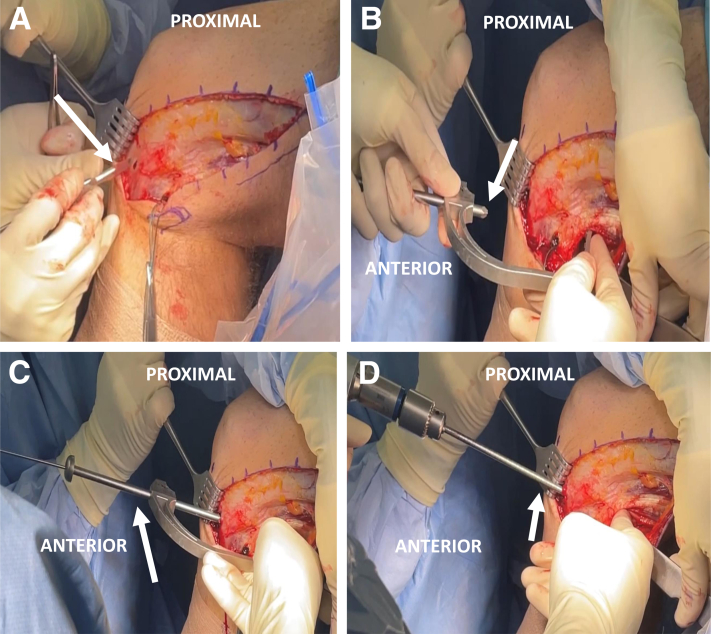
For the tibial tunnel, an anterior tibial dissection is performed, exposing the flat spot between the Gerdy tubercle and the tibial tubercle (Fig 3A). Again, a ligament aiming guide (Acufex Extra-articular Reconstruction Guide System) is used. The entry point is positioned on the flat spot and is aimed posteriorly approximately 1 cm medial and 1 cm proximal to the exit point of the fibular tunnel, adjacent to the medial aspect of the PTFJ (Fig 3B). While an assistant promotes manual reduction of the PTFJ and with the posterior retractor in place, a 2.4-mm guide pin is drilled and then over-reamed with a 6-mm cannulated reamer (Fig 3 C and D). A passing stitch is threaded through the tibial tunnel and recovered posteriorly to guide later semitendinosus graft passage (Fig 4).
Fig 3.
Tibial tunnel formation in left knee (lateral view). (A) Exposure of anterolateral tibial flat spot (arrow) between Gerdy tubercle and tibial tubercle. (B) Positioning of tibial aiming guide (arrow). The posterior tunnel emergence should be 1 cm medial and 1 cm proximal to the posterior fibular tunnel opening. (C) With manual reduction of the proximal tibiofibular joint, by use of a posterior retractor and tibial aiming guide, a 2.4-mm guide pin (arrow) is placed through the posterior aspect of the tibia. (D) Final tibial tunnel formation with 6-mm cannulated reamer (arrow) over guide pin. It should be noted that the Chandler retractor remains in place throughout tunnel formation and proximal tibiofibular joint reduction is maintained.
Fig 4.
Passing stitch placement for future passage of semitendinosus allograft in left knee (lateral view). (A) Placement of tibial passing stitch (arrow) from anterior to posterior. (B) Tibial and fibular passing stitches in place (arrow). These stitches will allow for graft shuttling in both tunnels.
Graft Passage and Fixation
A diagnostic arthroscopy, along with any corresponding treatment (e.g., meniscal repair), is performed at this point, through standard anteromedial and anterolateral portals. After completion of the arthroscopic procedure, all excess fluid is evacuated from the joint.
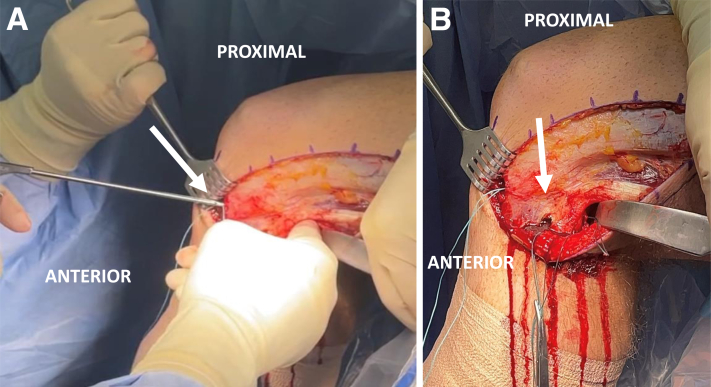
With the aid of the previously positioned passing stitches, the prepared semitendinosus allograft is passed from posterior to anterior through the tibial tunnel and then from posteromedial to anterolateral through the fibular tunnel (Fig 5 A-C). The graft is fixed into the fibular tunnel using a 7 × 25–mm soft-tissue interference screw (Biosure PEEK [polyether ether ketone] Interference Screw; Smith & Nephew) (Fig 5D). Subsequently, the knee is positioned at 70° of flexion and the free tibial limb is tensioned until an anatomically stable PTFJ reduction is achieved. A 7 × 25–mm soft-tissue interference screw (Biosure PEEK Interference Screw) is then inserted into the tibial tunnel. On completion of fixation, PTFJ stability is tested along the knee’s range of motion and any excess graft is excised.
Fig 5.
Graft passage and fixation of semitendinosus allograft in left knee (lateral view). (A) The graft is initially shuttled in the tibial tunnel from posterior (arrow) to anterior. (B) The proximal limb of the graft is then shuttled through the fibular tunnel from posterior to anterior (arrow). (C) Graft in place through tibial and fibular tunnels (arrow). (D) Initial fixation of graft in fibular tunnel (arrow) with 7 × 25 -mm interference screw. The semitendinosus allograft will subsequently be tensioned and fixed into the tibial tunnel at 70° of knee flexion with an additional 7 × 25 -mm interference screw.
Subcutaneous tissue and skin are closed in a layered fashion. The knee is placed in a hinged knee immobilizer locked in extension.
Postoperative Rehabilitation
Postoperatively, the patient is non–weight bearing for 6 weeks. During the same period, the knee immobilizer remains locked in extension while ambulating or sleeping. Physical therapy with an emphasis on passive range of motion and quadriceps activation starts the day after surgery. The goals for range of motion include complete extension and 90° of flexion by 2 weeks, which is further increased as tolerated in the following weeks. At 6 weeks postoperatively, the patient starts partial weight bearing with weekly increments until pain-free gait can be attained and the use of crutches is ultimately discontinued. Activities that elicit increased stress on the reconstruction, such as deep squats beyond 70° of knee flexion, or a varus moment of the knee, such as sitting cross-legged, should be avoided for the initial 4 months. Return to sport typically occurs at about 6 months postoperatively.
Discussion
The proposed surgical technique leverages an anatomic approach yielding appropriate stabilization of the PTFJ for patients with chronic tibiofibular joint instability. Owing to the rarity and under-reporting of PTFJ instability, the current literature does not define a standard of care.4,6,11,12,15 For patients in whom nonoperative treatment including immobilization, physical therapy, and activity modification fails, the current literature reports symptom relief, restored function, and improved subjective knee scores after surgical treatment.8,11,12,16,17
Current surgical techniques include trans-articular fixation of the PTFJ, tibiofibular soft-tissue ligamentous reconstruction, fibular head resection, and PTFJ arthrodesis with mid-fibular ostectomy.8,11,16,18 In a recent systematic review comparing surgical techniques, PTFJ fixation and fibular head resection were associated with increased complication rates and altered ankle loading and biomechanics, leading to pain and reduced function.4,6,8,16 Fixation of the PTFJ is often associated with overconstraint and restricted movement of the joint, as well as implant-related complications requiring additional surgery, such as screw or pin loosening and/or breakage.8,12 Fibular head resection, associated with posterolateral rotatory instability, and PTFJ arthrodesis, associated with ankle pain and instability, should be considered salvage procedures and are not suitable for younger or active patients.
The recent literature has shown that, although more technically demanding, reconstruction of the proximal tibiofibular ligaments effectively improves patient-reported outcomes and function.8,11,16 Different techniques for soft-tissue reconstruction of the PTFJ have recently been described, including the use of nonanatomic rerouting procedures (including the biceps femoris or ITB) and free autografts for anatomic reconstruction.8,18, 19, 20 Considering that nonanatomic procedures are associated with abnormal biomechanics, resulting in overconstraint or constructs prone to stretching out over time, anatomic-based reconstruction is preferred. In the aforementioned systematic review by Kruckeberg et al.,8 graft reconstruction led to improved pain and International Knee Documentation Committee (IKDC) scores, with low complication rates. Another downside to rerouting the ITB or the biceps tendon is disruption to the structures that provide accessory stability to the PTFJ. Regarding graft choice, the benefit of allograft use is multifold: (1) decreased surgical time as graft harvest is obviated13; (2) decreased donor-site morbidity including wound complications, anterior pain, disruption of the infrapatellar branch of the saphenous nerve, and posterior thigh discomfort13,21; and (3) avoidance of the persistent knee flexion strength deficit associated with hamstring autograft.14
Table 1 describes the pearls and pitfalls associated with the described surgical technique, and Table 2 presents advantages and limitations. This technique, which provides an anatomic approach using a free allograft reconstruction, is effective for patients with chronic instability in whom conservative treatment has failed and provides a reliable solution for patients presenting with pathology of the PTFJ.
Table 1.
Pearls and Pitfalls
| Pearls |
| A bilateral stability examination should be performed with the patient under anesthesia before incision and after initial exposure to assess stability of the PTFJ. |
| PTFJ reduction should be maintained throughout tibial tunnel formation to ensure anatomic orientation of the tunnels for future graft placement. |
| The surgeon should maintain a high level of suspicion for associated intra- and extra-articular lesions and be prepared to treat them if encountered (by meniscal repair, cartilage restoration, and so on). |
| Ipsilateral ankle instability should be tested and addressed if needed. |
| Pitfalls |
| A subluxated fibular head may distort the anatomy of the lateral knee; thus, careful dissection during peroneal nerve neurolysis should be performed to avoid injury to this structure. |
| Inadequate neurolysis may lead to postoperative motor and/or sensory deficits in the common peroneal nerve distribution. |
| Failure to identify and treat concomitant lesions may yield unsatisfactory patient-reported functional and pain improvements. |
PTFJ, proximal tibiofibular joint.
Table 2.
Advantages and Limitations
| Advantages |
| In patients with generalized ligamentous laxity, allografts provide better-quality collagen and a more robust and reliable graft for reconstruction. |
| Allograft use avoids donor-site morbidity associated with autograft harvesting from the hamstring insertion, including knee flexion strength deficit, and decreases overall surgical time. |
| Interference screws are widely available and less expensive than other device options for fixation of the graft in the tibia and fibula. |
| Adequate graft length and diameter can be verified preoperatively with the use of an allograft for reconstruction. |
| Limitations |
| Allograft use may theoretically increase the risk of infectious disease transmission if adequate screening is not performed prior to surgery. |
| Cost is increased with the use of a semitendinosus allograft for reconstruction in comparison to an autograft. |
| Allografts are not universally available, which hinders the application of this technique in certain resource-limited areas. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C. is a paid consultant for Arthrex, ConMed Linvatec, Ossur, and Smith & Nephew and is a board or committee member of American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, and International Society of Arthroscopy, Knee Surgery & Orthopaedic Sports Medicine. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Preoperative planning and surgical technique for proximal tibiofibular joint reconstruction for chronic instability with semitendinosus allograft in left knee.
References
- 1.Warner B.T., Moulton S.G., Cram T.R., LaPrade R.F. Anatomic reconstruction of the proximal tibiofibular joint. Arthrosc Tech. 2016;5:e207–e210. doi: 10.1016/j.eats.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anavian J., Marchetti D.C., Moatshe G., et al. The forgotten joint: Quantifying the anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2018;26:1096–1103. doi: 10.1007/s00167-017-4508-8. [DOI] [PubMed] [Google Scholar]
- 3.See A., Bear R.R., Owens B.D. Anatomic mapping for surgical reconstruction of the proximal tibiofibular ligaments. Orthopedics. 2013;36:e58–e63. doi: 10.3928/01477447-20121217-19. [DOI] [PubMed] [Google Scholar]
- 4.Ogden J.A. Subluxation and dislocation of the proximal tibiofibular joint. J Bone Joint Surg Am. 1974;56:145–154. [PubMed] [Google Scholar]
- 5.Sarma A., Borgohain B., Saikia B. Proximal tibiofibular joint: Rendezvous with a forgotten articulation. Indian J Orthop. 2015;49:489–495. doi: 10.4103/0019-5413.164041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogden J.A. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974:186–191. [PubMed] [Google Scholar]
- 7.Andersen K. Dislocation of the superior tibiofibular joint. Injury. 1985;16:494–498. doi: 10.1016/0020-1383(85)90180-9. [DOI] [PubMed] [Google Scholar]
- 8.Kruckeberg B.M., Cinque M.E., Moatshe G., et al. Proximal tibiofibular joint instability and treatment approaches: A systematic review of the literature. Arthroscopy. 2017;33:1743–1751. doi: 10.1016/j.arthro.2017.03.027. [DOI] [PubMed] [Google Scholar]
- 9.LaPrade R.F., Chahla J. Elsevier; St. Louis, MO: 2021. Evidence-based management of complex knee injuries: Restoring the anatomy to achieve best outcomes. [Google Scholar]
- 10.Levy B.A., Vogt K.J., Herrera D.A., Cole P.A. Maisonneuve fracture equivalent with proximal tibiofibular dislocation. A case report and literature review. J Bone Joint Surg Am. 2006;88:1111–1116. doi: 10.2106/JBJS.E.00954. [DOI] [PubMed] [Google Scholar]
- 11.Horst P.K., LaPrade R.F. Anatomic reconstruction of chronic symptomatic anterolateral proximal tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc. 2010;18:1452–1455. doi: 10.1007/s00167-010-1049-9. [DOI] [PubMed] [Google Scholar]
- 12.McNamara W.J., Matson A.P., Mickelson D.T., Moorman C.T. Surgical management of proximal tibiofibular joint instability using an adjustable loop, cortical fixation device. Arthrosc Tech. 2018;7:e271–e277. doi: 10.1016/j.eats.2017.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giedraitis A., Arnoczky S.P., Bedi A. Allografts in soft tissue reconstructive procedures: Important considerations. Sports Health. 2014;6:256–264. doi: 10.1177/1941738113503442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cristiani R., Mikkelsen C., Wange P., Olsson D., Stålman A., Engström B. Autograft type affects muscle strength and hop performance after ACL reconstruction. A randomised controlled trial comparing patellar tendon and hamstring tendon autografts with standard or accelerated rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2021;29:3025–3036. doi: 10.1007/s00167-020-06334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomason P.A., Linson M.A. Isolated dislocation of the proximal tibiofibular joint. J Trauma. 1986;26:192–195. doi: 10.1097/00005373-198602000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Ahmad C.S., ElAttrache N.S. Arthroscopic biceps tenodesis. Orthop Clin North Am. 2003;34:499–506. doi: 10.1016/s0030-5898(03)00093-2. [DOI] [PubMed] [Google Scholar]
- 17.Van Seymortier P., Ryckaert A., Verdonk P., Almqvist K.F., Verdonk R. Traumatic proximal tibiofibular dislocation. Am J Sports Med. 2008;36:793–798. doi: 10.1177/0363546507312162. [DOI] [PubMed] [Google Scholar]
- 18.Mena H., Brautigan B., Johnson D.L. Split biceps femoris tendon reconstruction for proximal tibiofibular joint instability. Arthroscopy. 2001;17:668–671. doi: 10.1053/jars.2001.22359. [DOI] [PubMed] [Google Scholar]
- 19.Morrison T.D., Shaer J.A., Little J.E. Bilateral, atraumatic, proximal tibiofibular joint instability. Orthopedics. 2011;34:133. doi: 10.3928/01477447-20101221-28. [DOI] [PubMed] [Google Scholar]
- 20.O'Reilly O.C., Carruthers K.H., Siparsky P.N. Bilateral, atraumatic proximal tibiofibular joint instability treated with suspensory button fixation. Orthopedics. 2017;40:e1107–e1111. doi: 10.3928/01477447-20170719-05. [DOI] [PubMed] [Google Scholar]
- 21.Laakso M., Kosola J., Niemi P., et al. Operative treatment for the painful posterior thigh after hamstring autograft harvesting. Muscles Ligaments Tendons J. 2017;7:570–575. doi: 10.11138/mltj/2017.7.3.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Preoperative planning and surgical technique for proximal tibiofibular joint reconstruction for chronic instability with semitendinosus allograft in left knee.
Preoperative planning and surgical technique for proximal tibiofibular joint reconstruction for chronic instability with semitendinosus allograft in left knee.