Abstract
Lateral collateral ligament (LCL) is known as an important ligament to restrain varus force of the knee, especially in 30° knee flexion. From the anatomical study, the insertion of LCL at proximal fibula is intimately close to the insertion of biceps femoris (BF) tendon. Since LCL is infrequently injured in isolation, and with limitation in availability of autograft and allograft, this study proposes the partial anterior BF tendon as an alternative autograft source to reconstruct the LCL. This could be performed either by minimally invasive procedure or standard open technique. The core concept is to preserve the posterior part of the BF tendon to protect the peroneal nerve, by which exploration of this nerve and the proximal fibula prior to LCL reconstruction could be exempted. Minimally invasive LCL reconstruction using this autograft would essentially reduce soft tissue injury, shorten the operative time, and enhance recovery of the reconstructed knee.
Technique Video
This video demonstrates the technique of the minimally invasive knee lateral collateral ligament reconstruction using partial biceps femoris tendon autograft. The patient is lying supine as for standard lateral collateral ligament (LCL) reconstruction. A pneumatic thigh tourniquet is installed and inflated. The entire left lower limb is prepped and draped in a standard fashion. With the knee in flexion, the fibular head is palpated and outlined by the surgical pen. The surgeon makes a 2.5-cm oblique incision parallel to the posterior border of the proximal fibula. Use the demarcation line between the tendon and the muscle as a landmark for graft harvesting. A stab incision is created at 1 cm below the anterior margin of the biceps femoris (BF) tendon. Dissect the BF tendon from its muscle mass, leaving the entire muscle bundle attached to its insertion at the proximal fibula. Insert the clamps beneath the BF tendon strip, then apply an umbilical cord tape under the graft to be used as a traction tool. Sharply dissect the graft in proximal and distal directions to free up the tendon from the underlying muscle. After performing the proximal release of BF tendon, it is important to ensure that the posterior part of the BF tendon remains intact before harvesting the graft to protect the peroneal nerve. Insert an open-loop tendon stripper into the tendon graft and slide it proximally against the counter-traction of the umbilical cord tape to complete the graft harvesting process. The harvested partial upper BF autograft with slight muscle attached is demonstrated. Measure the graft length and remove the remaining muscle from the BF graft. Metzenbaum scissors are used to further extend and separate the distal stump toward its insertion at proximal fibula. The required graft length for LCL reconstruction could be estimated by measuring the distance from the tip of the proximal fibula to the LFE plus 2 cm. Prepare the graft with whip stitch sutures. Double-strand BF autograft is ready for insertion. Make a 1-2-cm skin incision over the LFE and expose the iliotibial band (ITB). Then split the ITB to identify the attachment of the LCL at LFE. Pass a surgical clamp medial to the ITB. Dilate the retrieval passage and then bring the BF graft to the LFE. Pretension the graft, then temporarily insert a guidewire at the desired location to adjust the femoral insertion of the LCL by using the isometric point technique. Measuring the femoral tunnel length and graft size. Predrill the femoral tunnel using an Endobutton reamer to facilitate the passing of the guidewire and to estimate the entire femoral tunnel length. Ream the femoral tunnel slightly deeper than the estimated tunnel length. Pull out the BF graft through the tunnel hole. Insert the guidewire, and then recheck the range-of-motion before graft fixation. Tap the femoral tunnel. With the knee in 30° flexion and neutral rotation. Then insert the screw to securely fix the BF graft. Finally, check the knee for range-of-motion and stability. Close the BF fascia with absorbable suture, and then close the wound in the usual manner.
Introduction
LCL is a crucial structure at the posterolateral corner (PLC) of the knee. Its principal functions include primary restraint for varus force at all knee flexion angles, but greatest at 30° flexion; and also for internal rotation at this angle.1 LCL is about 70 mm long, wider at its fibular attachment; after that, it turns into a 4-5 mm-wide “cord-like” structure and inserts into the lateral femoral epicondyle (LFE) of the knee. The proximal insertion starts in a small bony depression at 1.4 mm proximal and 3.1 mm posterior to the LFE, then traverses under the superficial layer of the iliotibial band. The distal insertion locates at 8.2 mm posterior to the anterior border of the fibula and 28.4 mm distal to the fibular tip, embraced by the anterior and direct head of the BF tendon, which is an essential landmark for distal LCL insertion.2,3
Isolated PLC injury occurs rarely. It is usually occurs in combination with anterior cruciate ligament (ACL) and/or posterior cruciate ligament (PCL) insufficiency.4 If left untreated or inadequately treated, this injury could further alter knee biomechanics and might lead to devastating complications, including varus instability and knee deformation. If the healing capacity of the injured LCL is uncertain, the common treatment for the midsubstance or chronic LCL insufficiency is a reconstruction using either autograft or allograft.5 Because of the higher expense for allograft6 and its biological inferiority when compared with the autograft, the latter is generally the recommended source for ligament reconstructions.7,8 However, with the limited availability of the tendon allograft, establishing an additional donor source is admissible.
We propose using partial BF autograft as an alternative local tendon donor in reconstructing the LCL, as well as other PLC structures of the knee. Inherent anatomical advantages include 1) its distal insertion adjacent to the native LCL insertion; 2) less donor site morbidities by taking partial BF tendon using a tendon stripper, while leaving the muscle unit with the remaining tendon; 3) technical simplicity in graft harvesting that could minimize the risk of peroneal nerve injury, as compared with the standard reconstruction technique (requiring larger exposure to identify this nerve before making the tunnel hole at the fibular head); 4) shorter time through minimizing soft tissue dissection using the minimally invasive measures; and 5) no need for fibular head preparation and fixation.
Surgical Technique
The surgical technique can be observed in Video 1. The patient is lying supine as for standard LCL reconstruction and under general or regional anesthesia. The entire limb is prepped and draped as usual. The pneumatic thigh tourniquet is installed and inflated to enhance the exposure and lessen intraoperative blood loss. A standard arthroscopic examination is usually performed first to address other intra-articular pathologies and injury of the posterolateral complex. In case of other concomitant injuries, the general sequence is to treat the injured meniscus and reconstruct the cruciate ligament(s) prior to operating on the injured collateral ligament and adjacent structures.
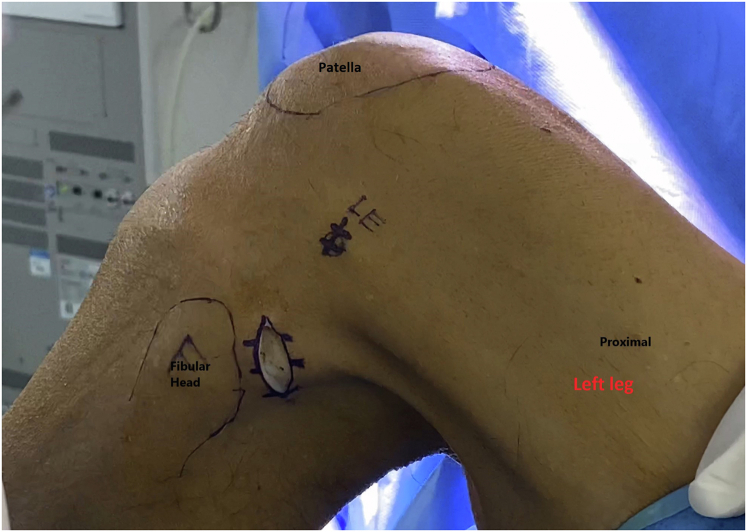
With the knee in flexion, the fibular head is palpated and outlined by the surgical pen (Fig 1). Make a 2.5-cm oblique incision parallel to the posterior border of the proximal fibula (Fig 2). Subcutaneous tissues are divided in line with the skin incision until reaching the BF fascia (Fig 3). By blunt dissection, identify the demarcation line between the BF tendon and muscle to be used as a landmark for graft harvesting (Fig 4). Maintaining the knee in flexion will keep the peroneal nerve away from the posterior border of the BF.
Fig 1.
Demonstrated lateral side of the left leg in the supine position with knee in 90° flexion. The BF tendon is apparently seen and palpated with the knee in flexion (red arrow), the fibular head is then palpated, and the surgical incision is outlined by the surgical pen just parallel to the posterior border of the fibula head.
Fig 2.
Left knee in the supine position with 90° knee flexion. Make a 2.5-cm oblique incision parallel to the posterior border of the proximal fibula.
Fig 3.
Left knee in supine position with 90° knee flexion. Divide the subcutaneous tissue in line with the skin incision until reaching the biceps femoris fascia.
Fig 4.
Left knee in supine position with 90° knee flexion. Blunt dissection to remove the soft tissue coverage above the biceps femoris (BF). The demarcation line (red arrow) separates the upper border of BF tendon and muscle.
A stab incision is initiated at the anterior margin of the BF tendon (Fig 5). This is then continued by blind splitting using Metzenbaum scissors to separate the anterior margin of the BF tendon from its muscle along the demarcation line toward the proximal part. Dissect the BF tendon through the initial stab opening to detach the underneath muscle mass, leaving the entire muscle bundle attaches to its insertion at the proximal fibula. Depending on the determined graft size (generally, 1-cm graft width is sufficient), make another stab incision at 1-1.5 cm parallel and posterior to the previous one to create the initial part of the tendon graft (Fig 6). The important message in this minimally invasive partial BF technique is to keep the remaining posterior tendinous bundle intact as a guardian for the peroneal nerve, while harvesting the graft (Fig 7). Insert right angle clamps beneath the initial part of the detached tendon strip and then apply an umbilical cord tape under the graft to be used as a traction tool. Then sharply dissect the graft in proximal and distal directions to free up the tendon from the underlying muscle (Fig 8). Insert an open-loop tendon stripper (Smith & Nephew) into the tendon graft and slide it proximally to complete the graft harvesting process (Fig 9).
Fig 5.
The knee is kept in a flexed position. Stab incision is made over the upper border of biceps femoris tendon along the demarcation line.
Fig 6.
The knee is kept in a flexed position. Make another stab incision at 1-1.5 cm parallel and posterior to the previous one to create the initial part of the tendon graft.
Fig 7.
The patient is place in a supine position with the knee in 90° flexion. Demonstrated remaining posterior tendinous bundle of biceps femoris tendon acts as a protector for peroneal nerve, while harvesting the graft (red arrow).
Fig 8.
The knee is kept in a flexed position. Sharply dissect the graft in proximal and distal direction, freeing up the tendon from the underlying muscle (red star). At this step, using cord tape as a traction tool could facilitate in this process.
Fig 9.
The knee is kept in a flexed position. The surgeon retrieves the cord tape under the graft using a traction tool, inserts the open loop-end tendon stripper (Smith & Nephew) into the tendon graft, and then slides the tendon stripper in the proximal direction to complete the graft-harvesting process. At this step, avoid premature graft rupture by not overstuffing the graft and preliminarily dissecting the proximal end of the BF graft with Metzenbaum scissors.
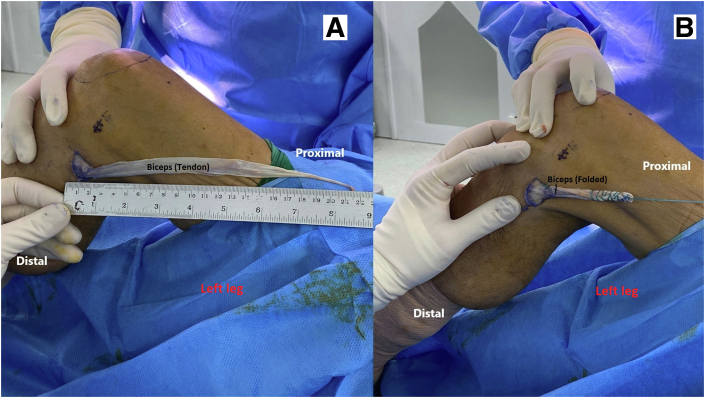
Metzenbaum scissors or a surgical knife is used to partially release the distal stump toward its insertion at proximal fibula (Fig 10). If the remnant of the LCL stump is seen, suture the distal BF graft together with the LCL stump to strengthen the distal insertion. Measure the graft length and prepare the graft with whip stitch sutures (Ethibond 2-0 Ethicon) at the proximal end (Fig 11). The required graft length for LCL reconstruction could be estimated by measuring the distance from the tip of the proximal fibula to the LFE plus 2 cm (Fig 12). Generally, a twofold 7-cm graft is sufficient for LCL reconstruction with interference screw fixation at the LFE. While preparing the proximal insertion at LFE, cover the prepared graft with normal saline-soaked gauze, or leave the graft inside the tissue.
Fig 10.
Lateral side of left knee in flexion. The surgeon uses Metzenbaum scissors or a surgical knife to partially release the distal stump back to its insertion at proximal fibula (red star). This facilitates the graft turning process.
Fig 11.
Measure the graft length (A) and prepare the graft (B) with whip stitch sutures (Ethibond 2-0 Ethicon) at the proximal end. Extremely large graft can cause difficulties during the graft passage.
Fig 12.
(A) The required graft length for LCL reconstruction could be estimated by measuring the distance from the tip of the proximal fibula to the LFE (Red star) plus two centimeters. (B) Demonstrated final preparation of two-strand BF tendon autograft.
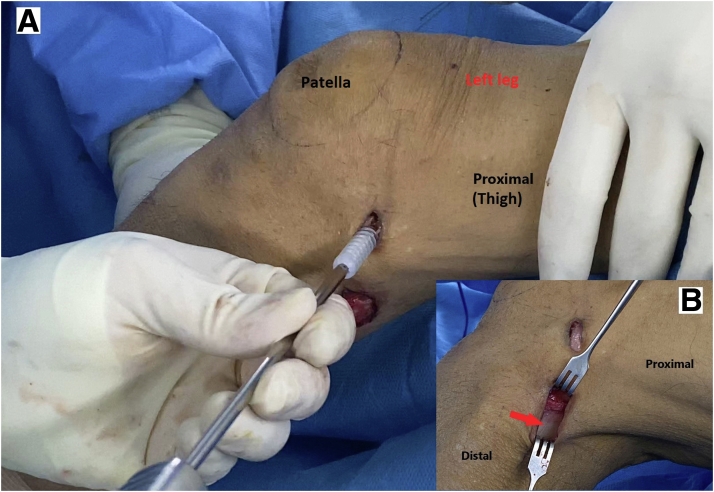
Identify the proximal insertion either by directly palpating the LFE or using fluoroscopic guidance for the landmark. Through a 1-2-cm skin incision over the LFE, expose the iliotibial band (ITB) (Fig 13) and split along the fascial band to identify the attachment of the LCL at LFE. Pass a surgical clamp or suture retriever medial to the ITB to bring the BF graft back to the LFE (Fig 14 and Fig 15). Identify the femoral insertion by isometric point technique. Insert a guidewire at the desired location and ream a tunnel hole for graft fixation with an appropriate screw or other apparatus (Fig 16). With the knee in 30° flexion, slightly valgus, and neutral rotation, pass the graft into the tunnel hole. Tension the graft and check ranges of motion by cycling the knee in flexion-extension several times before graft fixation (Fig 17). Recheck the knee stability and close the wound in a standard fashion (Fig 18). The immobilization and rehabilitation protocols are done in a standard fashion.
Fig 13.
Left knee in flexion. (A) Make 1-2 cm vertical or longitudinal skin incision over the LFE (Red arrowhead), (B) continue the dissection until exposing to the ITB (Red star).
Fig 14.
Left knee in flexion. After splitting the tensor fascia lata (Red arrow) along its bundles to expose to the origin of lateral collateral ligament at lateral femoral epicondyle (red star), pass the surgical clamps or suture retriever beneath the TFL. Dilated the graft retrieval passage before passing the BF graft.
Fig 15.
Left knee in flexion. The biceps femoris (BF) graft is shuttled back to LFE. At this step, pretensioning of the graft is done by cyclic loading of the BF in knee flexion and extension.
Fig 16.
Left knee in flexion. (A) The guidewire is drilled at the desired location by using anatomical landmarks or radiographic guidance. The guidewire is aimed in anterior and proximal direction to avoid neurovascular injury and tunnel jamming. (B) In case of combining with ACL reconstruction. Separated tunnel reaming passage need to be planed, to avoid tunnel jamming and iatrogenic grafts injury.
Fig 17.
(A) Tension the graft at 30° knee flexion, slightly valgus, and neutral rotation. Then checking ranges of motion before graft fixation (bioabsorbable screw, Smith and Nephew). (B) After final graft fixation, the lower part of biceps femoris tendon is demonstrated to be still intact (red arrow).
Fig 18.
(A) Repair the biceps femoris fascia (red star) with absorbable suture. (B) The wound is then closed in a standard fashion.
Discussion
Treatments of LCL injury vary depending on the site and chronicity of the injury. In a chronic case or a midsubstance tear, the treatment trend is reconstruction rather than repair. Techniques to reconstruct the injured LCL can be anatomic or nonanatomic. BF tendon has been used as a nonanatomic reconstruction by means of the tenodesis effect.9,10 Although this biceps tenodesis is equally effective with anatomic LCL reconstruction in restoring varus stability of the knee,11 many surgeons do not prefer the former, as of its nonanatomic nature and lack of reported long-term results.12
The authors advocate the use of a minimally invasive technique using partial BF autograft as an alternative for LCL reconstruction. This technique is simple and requires only basic instruments to harvest the graft. The principal concept is based on the distinctive anatomy of the BF tendon. Its insertion is not merely close to the LCL attachment but also acts as an integral structure to protect the peroneal nerve that always runs posteroinferiorly. The conventional anatomic LCL reconstruction usually requires moderate lateral exposure to identify and retract away the peroneal nerve to reduce the risk of its injury. But in this technique, with the knee in flexion and preserving the posterior part of the BF tendon and the entire muscle, exposure and dissection could be minimized. In the standard fibular-based LCL reconstruction, reaming the proximal fibular tunnel in tiny patients with osteoporotic bone might be troublesome.13 Our technique could simply omit this step, resulting in less time consumption and reduced risk of complication. Since only the anterior tendinous strip of the BF tendon is taken as the graft, this would leave the entire muscle and major tendon mass for the important function as a dynamic stabilizer of the knee. By the way, the donor site morbidity is much less when compared with other autologous tendon reconstruction or the conventional technique mentioned above.
This technique should be avoided in cases with proximal fibula tip fracture, complete injury of the BF tendon, and injury to the proximal tibiofibular joint. For incomplete BF rupture or peeling-off from the insertion, stitching the injured tendon with the LCL stump or augmenting with a suture anchor is recommended. For pre-existing peroneal nerve injury, larger exposure might be required to perform peroneal nerve neurolysis or repair. In case a larger BF graft is preferred, the anterior two-thirds of the BF tendon could be taken by a larger open-loop tendon stripper.
In conclusion, this minimally invasive partial BF autograft technique is reproducible for knee LCL reconstruction with less donor site morbidity and is technically simple. This could be operated as an isolated procedure, an augmentation of LCL repair in acute knee injury, or a combination with other ligamentous reconstructions in multiligamentous injuries of the knee, especially in environments with limited allograft availability. The advantages and limitations, and tips and pearls for this technique are presented in Table 1 and Table 2.
Table 1.
Advantages, Disadvantages, and Limitations
| Advantages | Disadvantages and Limitations |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
Table 2.
Tips and Pearls
|
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video demonstrates the technique of the minimally invasive knee lateral collateral ligament reconstruction using partial biceps femoris tendon autograft. The patient is lying supine as for standard lateral collateral ligament (LCL) reconstruction. A pneumatic thigh tourniquet is installed and inflated. The entire left lower limb is prepped and draped in a standard fashion. With the knee in flexion, the fibular head is palpated and outlined by the surgical pen. The surgeon makes a 2.5-cm oblique incision parallel to the posterior border of the proximal fibula. Use the demarcation line between the tendon and the muscle as a landmark for graft harvesting. A stab incision is created at 1 cm below the anterior margin of the biceps femoris (BF) tendon. Dissect the BF tendon from its muscle mass, leaving the entire muscle bundle attached to its insertion at the proximal fibula. Insert the clamps beneath the BF tendon strip, then apply an umbilical cord tape under the graft to be used as a traction tool. Sharply dissect the graft in proximal and distal directions to free up the tendon from the underlying muscle. After performing the proximal release of BF tendon, it is important to ensure that the posterior part of the BF tendon remains intact before harvesting the graft to protect the peroneal nerve. Insert an open-loop tendon stripper into the tendon graft and slide it proximally against the counter-traction of the umbilical cord tape to complete the graft harvesting process. The harvested partial upper BF autograft with slight muscle attached is demonstrated. Measure the graft length and remove the remaining muscle from the BF graft. Metzenbaum scissors are used to further extend and separate the distal stump toward its insertion at proximal fibula. The required graft length for LCL reconstruction could be estimated by measuring the distance from the tip of the proximal fibula to the LFE plus 2 cm. Prepare the graft with whip stitch sutures. Double-strand BF autograft is ready for insertion. Make a 1-2-cm skin incision over the LFE and expose the iliotibial band (ITB). Then split the ITB to identify the attachment of the LCL at LFE. Pass a surgical clamp medial to the ITB. Dilate the retrieval passage and then bring the BF graft to the LFE. Pretension the graft, then temporarily insert a guidewire at the desired location to adjust the femoral insertion of the LCL by using the isometric point technique. Measuring the femoral tunnel length and graft size. Predrill the femoral tunnel using an Endobutton reamer to facilitate the passing of the guidewire and to estimate the entire femoral tunnel length. Ream the femoral tunnel slightly deeper than the estimated tunnel length. Pull out the BF graft through the tunnel hole. Insert the guidewire, and then recheck the range-of-motion before graft fixation. Tap the femoral tunnel. With the knee in 30° flexion and neutral rotation. Then insert the screw to securely fix the BF graft. Finally, check the knee for range-of-motion and stability. Close the BF fascia with absorbable suture, and then close the wound in the usual manner.
References
- 1.Coobs B.R., LaPrade R.F., Griffith C.J., Nelson B.J. Biomechanical analysis of an isolated fibular (lateral) collateral ligament reconstruction using an autogenous semitendinosus graft. Am J Sports Med. 2007;35:1521–1527. doi: 10.1177/0363546507302217. [DOI] [PubMed] [Google Scholar]
- 2.Moorman C.T., LaPrade R.F. Anatomy and biomechanics of the posterolateral corner of the knee. J Knee Surg. 2005;18:137–145. doi: 10.1055/s-0030-1248172. [DOI] [PubMed] [Google Scholar]
- 3.James E.W., LaPrade C.M., LaPrade R.F. Anatomy and biomechanics of the lateral side of the knee and surgical implications. Sports Med Arthrosc Rev. 2015;23:2–9. doi: 10.1097/JSA.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 4.Geeslin A.G., LaPrade R.F. Location of bone bruises and other osseous injuries associated with acute grade III isolated and combined posterolateral knee injuries. Am J Sports Med. 2010;38:2502–2508. doi: 10.1177/0363546510376232. [DOI] [PubMed] [Google Scholar]
- 5.Stannard J.P., Brown S.L., Farris R.C., McGwin G., Volgas D.A. The posterolateral corner of the knee: Repair versus reconstruction. Am J Sports Med. 2005;33:881–888. doi: 10.1177/0363546504271208. [DOI] [PubMed] [Google Scholar]
- 6.Nagda S.H., Altobelli G.G., Bowdry K.A., Brewster C.E., Lombardo S.J. Cost analysis of outpatient anterior cruciate ligament reconstruction: Autograft versus allograft. Clin Orthop Relat Res. 2010;468:1418–1422. doi: 10.1007/s11999-009-1178-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tian S., Wang B., Liu L., et al. Irradiated hamstring tendon allograft versus autograft for anatomic double-bundle anterior cruciate ligament reconstruction: Midterm clinical outcomes. Am J Sports Med. 2016;44:2579–2588. doi: 10.1177/0363546516655333. [DOI] [PubMed] [Google Scholar]
- 8.Mascarenhas R., Erickson B.J., Sayegh E.T., et al. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: A systematic review of overlapping meta-analyses. Arthrosc J Arthrosc Relat Surg. 2015;31:364–372. doi: 10.1016/j.arthro.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Martin S.D., Clancy W.G. Posterolateral instability of the knee: treatment using the clancy biceps femoris tenodesis. Oper Tech Sports Med. 1996;4:182–191. [Google Scholar]
- 10.Fanelli G.C. Surgical treatment of lateral posterolateral instability of the knee using biceps tendon procedures. Sports Med Arthrosc Rev. 2006;14:37–43. doi: 10.1097/00132585-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Beiro C., Parks B.G., Tsai M., Hinton R.Y. Biceps tenodesis versus allograft reconstruction for varus instability. J Knee Surg. 2014;27:133–137. doi: 10.1055/s-0033-1357495. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade R.F., Johansen S., Wentorf F.A., Engebretsen L., Esterberg J.L., Tso A. An analysis of an anatomical posterolateral knee reconstruction: An in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32:1405–1414. doi: 10.1177/0363546503262687. [DOI] [PubMed] [Google Scholar]
- 13.Meislin R.J., Halbrecht J. Springer Science & Business Media; New York: 2009. Complications in knee and shoulder surgery: Management and treatment options for the sports medicine orthopedist. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the technique of the minimally invasive knee lateral collateral ligament reconstruction using partial biceps femoris tendon autograft. The patient is lying supine as for standard lateral collateral ligament (LCL) reconstruction. A pneumatic thigh tourniquet is installed and inflated. The entire left lower limb is prepped and draped in a standard fashion. With the knee in flexion, the fibular head is palpated and outlined by the surgical pen. The surgeon makes a 2.5-cm oblique incision parallel to the posterior border of the proximal fibula. Use the demarcation line between the tendon and the muscle as a landmark for graft harvesting. A stab incision is created at 1 cm below the anterior margin of the biceps femoris (BF) tendon. Dissect the BF tendon from its muscle mass, leaving the entire muscle bundle attached to its insertion at the proximal fibula. Insert the clamps beneath the BF tendon strip, then apply an umbilical cord tape under the graft to be used as a traction tool. Sharply dissect the graft in proximal and distal directions to free up the tendon from the underlying muscle. After performing the proximal release of BF tendon, it is important to ensure that the posterior part of the BF tendon remains intact before harvesting the graft to protect the peroneal nerve. Insert an open-loop tendon stripper into the tendon graft and slide it proximally against the counter-traction of the umbilical cord tape to complete the graft harvesting process. The harvested partial upper BF autograft with slight muscle attached is demonstrated. Measure the graft length and remove the remaining muscle from the BF graft. Metzenbaum scissors are used to further extend and separate the distal stump toward its insertion at proximal fibula. The required graft length for LCL reconstruction could be estimated by measuring the distance from the tip of the proximal fibula to the LFE plus 2 cm. Prepare the graft with whip stitch sutures. Double-strand BF autograft is ready for insertion. Make a 1-2-cm skin incision over the LFE and expose the iliotibial band (ITB). Then split the ITB to identify the attachment of the LCL at LFE. Pass a surgical clamp medial to the ITB. Dilate the retrieval passage and then bring the BF graft to the LFE. Pretension the graft, then temporarily insert a guidewire at the desired location to adjust the femoral insertion of the LCL by using the isometric point technique. Measuring the femoral tunnel length and graft size. Predrill the femoral tunnel using an Endobutton reamer to facilitate the passing of the guidewire and to estimate the entire femoral tunnel length. Ream the femoral tunnel slightly deeper than the estimated tunnel length. Pull out the BF graft through the tunnel hole. Insert the guidewire, and then recheck the range-of-motion before graft fixation. Tap the femoral tunnel. With the knee in 30° flexion and neutral rotation. Then insert the screw to securely fix the BF graft. Finally, check the knee for range-of-motion and stability. Close the BF fascia with absorbable suture, and then close the wound in the usual manner.
This video demonstrates the technique of the minimally invasive knee lateral collateral ligament reconstruction using partial biceps femoris tendon autograft. The patient is lying supine as for standard lateral collateral ligament (LCL) reconstruction. A pneumatic thigh tourniquet is installed and inflated. The entire left lower limb is prepped and draped in a standard fashion. With the knee in flexion, the fibular head is palpated and outlined by the surgical pen. The surgeon makes a 2.5-cm oblique incision parallel to the posterior border of the proximal fibula. Use the demarcation line between the tendon and the muscle as a landmark for graft harvesting. A stab incision is created at 1 cm below the anterior margin of the biceps femoris (BF) tendon. Dissect the BF tendon from its muscle mass, leaving the entire muscle bundle attached to its insertion at the proximal fibula. Insert the clamps beneath the BF tendon strip, then apply an umbilical cord tape under the graft to be used as a traction tool. Sharply dissect the graft in proximal and distal directions to free up the tendon from the underlying muscle. After performing the proximal release of BF tendon, it is important to ensure that the posterior part of the BF tendon remains intact before harvesting the graft to protect the peroneal nerve. Insert an open-loop tendon stripper into the tendon graft and slide it proximally against the counter-traction of the umbilical cord tape to complete the graft harvesting process. The harvested partial upper BF autograft with slight muscle attached is demonstrated. Measure the graft length and remove the remaining muscle from the BF graft. Metzenbaum scissors are used to further extend and separate the distal stump toward its insertion at proximal fibula. The required graft length for LCL reconstruction could be estimated by measuring the distance from the tip of the proximal fibula to the LFE plus 2 cm. Prepare the graft with whip stitch sutures. Double-strand BF autograft is ready for insertion. Make a 1-2-cm skin incision over the LFE and expose the iliotibial band (ITB). Then split the ITB to identify the attachment of the LCL at LFE. Pass a surgical clamp medial to the ITB. Dilate the retrieval passage and then bring the BF graft to the LFE. Pretension the graft, then temporarily insert a guidewire at the desired location to adjust the femoral insertion of the LCL by using the isometric point technique. Measuring the femoral tunnel length and graft size. Predrill the femoral tunnel using an Endobutton reamer to facilitate the passing of the guidewire and to estimate the entire femoral tunnel length. Ream the femoral tunnel slightly deeper than the estimated tunnel length. Pull out the BF graft through the tunnel hole. Insert the guidewire, and then recheck the range-of-motion before graft fixation. Tap the femoral tunnel. With the knee in 30° flexion and neutral rotation. Then insert the screw to securely fix the BF graft. Finally, check the knee for range-of-motion and stability. Close the BF fascia with absorbable suture, and then close the wound in the usual manner.