Abstract
A discoid meniscus is a congenital abnormality that usually affects the lateral meniscus, leading to instability and increased risk of tearing. A discoid medial meniscus is an extremely rare pathology that is seldom described in literature. In this report, we present the technique of operative treatment of a symptomatic, torn discoid medial meniscus. The meniscus is saucerized to 6-8 mm of stable rim, and the inside-out technique is used as the modality of meniscal fixation. Although a discoid medial meniscus is an uncommon finding, all treating surgeons should be aware of the possibility during surgical intervention.
Technique Video
This video demonstrates the diagnosis, surgical technique, and postoperative treatment of a patient with a medial discoid meniscus. Diagnosis and the decision to operate are made through clinical findings and are guided by radiographs and MRIs. Intraoperatively, an examination under anesthesia and diagnostic arthroscopy are performed. The meniscus is saucerized to a stable border of 6-8 mm. An inside-out meniscal repair is performed. Immediately postoperation, the patient is locked in extension and weight bearing as tolerated. Range of motion progression is carried out under the supervision of the treating orthopedic surgeon and physical therapist.
Introduction
A discoid medial meniscus is an extremely rare congenital abnormality first described by Cave and Staples in 1941.1 Usually, this pathology involves the lateral meniscus with an overall incidence of 3 to 5%. Currently, fewer than 80 cases of medial discoid meniscus are reported in the literature, according to a review conducted by our team.
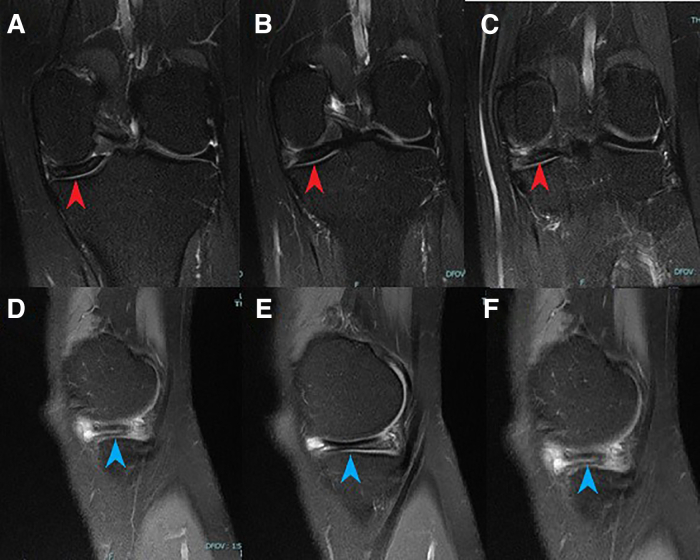
We present the technique of arthroscopic saucerization to a stable peripheral rim and repair using an inside-out technique (Video 1). Clinical findings may include medial joint line tenderness, a knee effusion, a positive McMurray’s test, a snapping sensation, and pain. Diagnosis is guided by a radiograph and MRI (Fig 1).
Fig 1.
Left knee, preoperative T2 MRI coronal cuts (A-C) demonstrate increased meniscal body width (red arrowheads) and sagittal cuts (D-F) show increased central thickness consistent with discoid meniscus (blue arrowheads).
Surgical Technique
Set Up
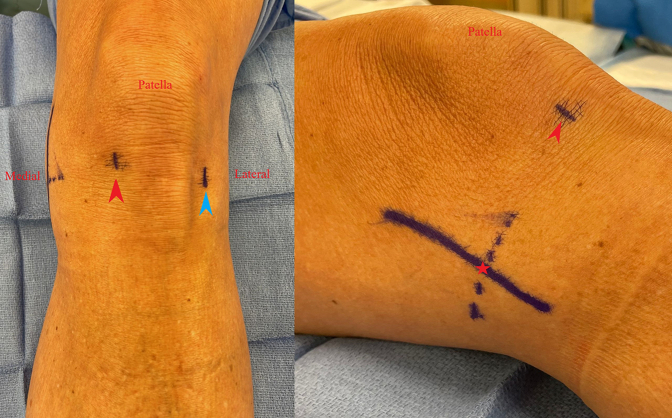
The standard room setup for arthroscopy is used. Preoperative examination under anesthesia is performed to demonstrate intact ligaments, assess knee range of motion, and document additional abnormalities. The surgical procedure is conducted in the standard fashion using supine positioning, a proximal tourniquet, and a lateral post to stress the knee in valgus. The surgical incision sites are marked for the inside-out repair to prevent knee landmark distortion after fluid insufflation (Fig 2). 1% lidocaine with epinephrine is injected into the knee joint, fat pad, and portal sites.
Fig 2.
Left knee, outside view of arthroscopic incision sites marked prior to fluid insufflation to prevent distortion. The red arrowhead marks the inferomedial portal site, the blue arrowhead marks the inferolateral portal site, and the red star marks the medial incision site.
Diagnostic Knee Arthroscopy
The inferolateral viewing portal and inferomedial working portals are established, through which a diagnostic knee arthroscopy is performed. The use of superior lateral outflow portal is optional and depends on surgeon preference. A hook probe (Smith & Nephew, Andover, MA) is used to confirm a medial discoid meniscus tear. Stability is tested by placing the probe through the tear and pulling the posterior horn anteriorly (Fig 3). At this point, any additional pathology can be diagnosed and addressed, including cartilage defects, symptomatic plicae, and lateral meniscus pathology (Fig 4).
Fig 3.
Left knee, arthroscopic view through the inferomedial (A) and inferolateral (B) portals visualizing a left discoid medial meniscus. Stability is tested by placing a hook probe through the tear and pulling the posterior horn anteriorly. Anterior subluxation of the posterior horn is indicative of a meniscocapsular injury.
Fig 4.
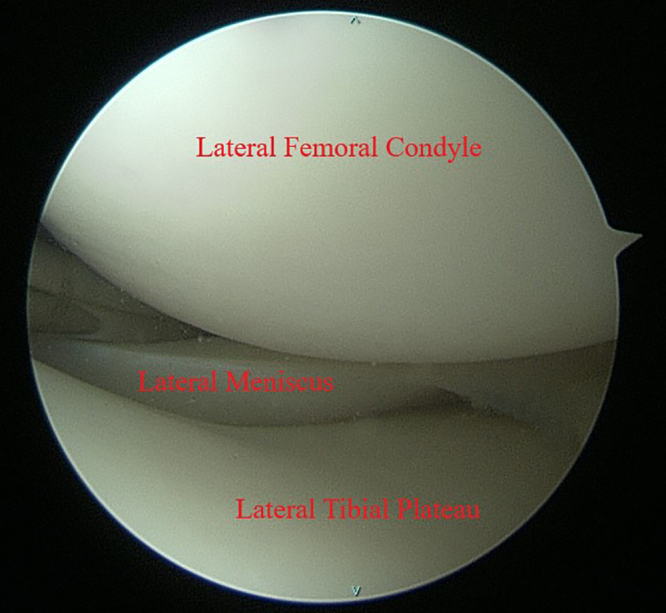
Left knee, arthroscopic view through the inferolateral portal. The lateral meniscus is visualized during the diagnostic arthroscopy to assess for any additional pathologies that need to be addressed.
Saucerization
Saucerization is performed anteriorly to posteriorly using an arthroscopic punch (Smith & Nephew) and shaver (Arthrex, Naples, FL), taking care to leave a 6- to 8-mm stable rim of the meniscus (Fig 5). After saucerization, the tear is re-examined, and meniscus stability is assessed using the probe and by flexing the knee (Fig 6). If visualization of the root is challenging, a 70° scope can be used to perform the Guillquist maneuver to further assess the posterior horn of the medial meniscus posteriorly (Fig 7). A meniscal rasp (ConMed Linvatec, Largo, FL) is used to abrade the meniscus on both sides. If there is still difficulty in visualization of the medial compartment, pie-crusting of the medial collateral ligament is done with an 18-gauge needle percutaneously.
Fig 5.
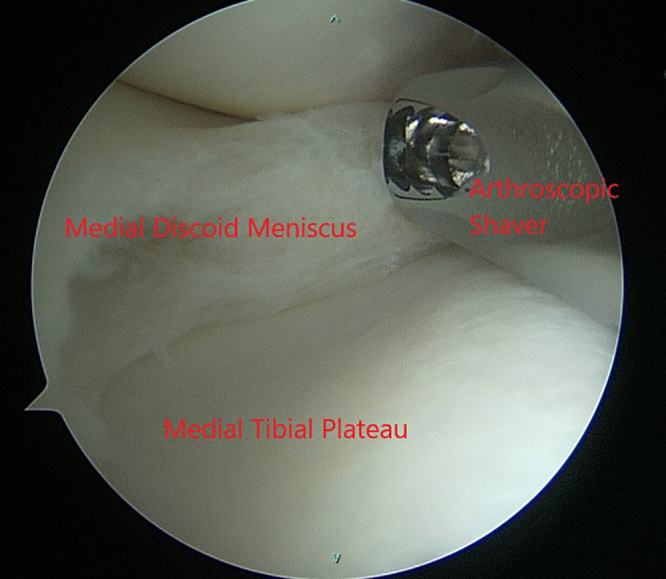
Left knee, arthroscopic view through the inferomedial portal. The discoid medial meniscus is saucerized to 6-8 mm of stable rim using an arthroscopic punch and shaver.
Fig 6.

Left knee, arthroscopic view of the saucerized medial discoid meniscus through the inferolateral portal. A hook probe (blue arrowhead) is used to assess for meniscal stability after saucerization is complete.
Fig 7.
Left knee, arthroscopic view through the inferolateral portal using a 70° scope. The Guillquist maneuver can be used to better visualize the posterior horn of the medial discoid meniscus through the notch to assess meniscocapsular injury.
Meniscus Repair
Anterior subluxation of the posterior horn of the medial meniscus is often due to a meniscocapsular injury. This injury is amenable to repair due to the medial meniscus having a good peripheral blood supply.2 A standard posterior medial approach for inside-out meniscal repair is performed using the previously marked incision. The skin is dissected to the subcutaneous tissue, the sartorial fascia is identified and divided longitudinally. Then the interval between the joint capsule and the medial head of gastrocnemius is developed. The semimembranosus tendon is identified.
The medial gastrocnemius tendon and muscle are separated from any posterior capsular adhesions using a Cobb elevator. A tablespoon or a similar device (e.g., Graves speculum blade, MedGyn, Addison, IL) can be placed in this interval to act as a retractor, protecting the popliteal vessels.
The ZoneNavigator System (Arthrex) is used through the inferolateral portal. Multiple sutures are passed through the meniscal repair needles by the surgical assistant in a vertical mattress fashion. The repair is started posteriorly to secure the meniscus to the posterior capsule and carried on through the meniscal body, as needed (Fig 8). The suture needles are retrieved under direct visualization through the medial incision. After passing all of the sutures through the medial incision, a slight tension is applied and arthroscopic examination of the subluxating meniscus is performed. At this point, the absence of subluxation should be noted. The sutures then can be tied over the capsule. A microfracture awl is used in the notch to release bone marrow and further induce healing. Incision and portals are closed in the standard surgical fashion. Table 1 discusses pearls and pitfalls of this procedure.
Fig 8.

Left knee, arthroscopic view through the inferolateral portal. Vertical mattress sutures are placed posteriorly to secure the meniscus to the posterior capsule and carried on through the meniscal body as needed (blue arrowheads). Absence of subluxation of the meniscus should be noted upon completion of the repair.
Table 1.
Pearls and Pitfalls of Arthroscopic Saucerization and Inside-Out Repair of a Torn Discoid Medial Meniscus
| Pearls | Pitfalls |
|---|---|
|
|
Post-Op
A knee immobilizer locked in extension is applied. Partial weight-bearing protocol in the immediate postoperative period (2 weeks) is used. Subsequent graduated gentle range of motion is carried on under the supervision of the treating orthopedic surgeon and physical therapist.
Discussion
A medial discoid meniscus is a rare pathology, with few cases reported in the literature.
It is recommended that the discoid meniscus be preserved if no severe symptoms are present.3 However, a torn medial discoid meniscus can be associated with medial joint line tenderness, severe discomfort from a snapping meniscus, and interference with activities of daily living. Other symptoms reported include locking of the knee, pain in flexion and extension, effusion, positive McMurray’s test, and reduced range of motion.4,5 Repairing a torn posterior horn is important, given its role as a secondary stabilizer, as well as to protect the cartilage.6 A medial discoid meniscus may have its anterior horn anomalously inserted on the anterior cruciate ligament (Fig 9). The anterior horn insertion at the ACL can be neglected in accordance with previous literature.7
Fig 9.

Left knee, arthroscopic view through the inferolateral portal. An anomalous insertion of the discoid medial meniscus anterior horn on the anterior cruciate ligament.
Historically, most symptomatic discoid menisci have been treated with partial meniscectomies with attempts to preserve as much as possible of the meniscus to reduce the rate of degenerative changes.4 However, a recent article by Ahn et al. described 23 pediatric patients with discoid lateral meniscal tears with peripheral instability that were treated with saucerization and meniscal peripheral repair. The technique demonstrated positive results at a mean 51 months follow-up.8 Although medial and lateral discoid menisci are structurally and biomechanically different, success with saucerization of lateral discoid menisci has been extrapolated to medial menisci with good results. Desai et al. describe treatment of a medial discoid meniscus tear in an 18-year-old male with saucerization and meniscus repair, reporting the patient was asymptomatic at 6 months and 1 year follow-ups and returned to full physical activity.9 Jin et al. describe saucerization of a symptomatic discoid medial meniscus coalesced with the anterior cruciate ligament in a 29-year-old male, resulting in no symptoms and full return to physical activities at 12 months.10 Sevillano-Perez et al. describe treatment of bilateral medial discoid meniscus tears in a 13-year-old football player with saucerization and inside-out repair, resulting in return to preinjury activity level and no symptoms at 2-year follow up.11 Case reports by Farlett and Wood, Lukas et al., and Iorio et al. show good outcomes at 4-7-month follow-up in pediatric patients undergoing saucerization of medial discoid menisci.12, 13, 14 Finally, Feroe et al. describe 11 saucerized discoid medial menisci in 8 pediatric and adolescent patients with a mean follow-up of 19.1 months. Concomitant meniscal repair was performed in 7 cases. Four cases sustained retears and 1 developed arthrofibrosis, while all other patients were asymptomatic at final follow-up.5
Ultimately, recent literature shows some promising outcomes for this technique; however, there is a dearth of literature that analyzes long-term outcomes. Still, advantages of saucerization of a medial discoid meniscus include a meniscus-preserving, reproducible technique that requires standard equipment and operative setup (Table 2).
Table 2.
Advantages and Disadvantages of Arthroscopic Saucerization and Inside-Out Repair of a Torn Discoid Medial Meniscus
| Advantages | Disadvantages |
|---|---|
|
|
We prefer the inside-out technique as the modality of fixation for a concomitant meniscal tear, since it is still considered the gold standard for treating these tears. This technique allows for direct visualization of sutures tied over the capsule, but it requires a relatively large medial incision. It is associated with decreased implant cost compared to the all-inside technique, but also increased operative time and risk for iatrogenic nerve injury.15,16 In addition, recent reports show no difference in complications and functional outcomes between the two methods, so either may be an appropriate choice.15,16
Although discoid medial meniscus is an uncommon pathology, the treating surgeon should be aware of the possibility when intervening surgically, especially with the presence of a palpable snap, which indicates that the tear is highly likely to be unstable. In these circumstances, saucerization and repair of the meniscus are a treatment option that can be considered.
Supplementary Data
This video demonstrates the diagnosis, surgical technique, and postoperative treatment of a patient with a medial discoid meniscus. Diagnosis and the decision to operate are made through clinical findings and are guided by radiographs and MRIs. Intraoperatively, an examination under anesthesia and diagnostic arthroscopy are performed. The meniscus is saucerized to a stable border of 6-8 mm. An inside-out meniscal repair is performed. Immediately postoperation, the patient is locked in extension and weight bearing as tolerated. Range of motion progression is carried out under the supervision of the treating orthopedic surgeon and physical therapist.
References
- 1.Cave E.F., Staples O.S. Congenital discoid meniscus. A cause of internal derangement of the knee. Am J Surg. 1941;54:371–376. [Google Scholar]
- 2.Woodmass J.M., LaPrade R.F., Sgaglione N.A., Nakamura N., Krych A.J. Meniscal repair: Reconsidering indications, techniques, and biologic augmentation. J Bone Joint Surg Am. 2017;99:1222–1231. doi: 10.2106/JBJS.17.00297. [DOI] [PubMed] [Google Scholar]
- 3.Kocher M.S., Logan C.A., Kramer D.E. Discoid lateral meniscus in children: Diagnosis, management, and outcomes. J Am Acad Orthop Surg. 2017;25:736–743. doi: 10.5435/JAAOS-D-15-00491. [DOI] [PubMed] [Google Scholar]
- 4.Tachibana Y., Yamazaki Y., Ninomiya S. Discoid medial meniscus. Arthroscopy. 2003;19:E12–E18. doi: 10.1016/s0749-8063(03)00688-1. [DOI] [PubMed] [Google Scholar]
- 5.Feroe A.G., Hussain Z.B., Stupay K.L., et al. Surgical management of medial discoid meniscus in pediatric and adolescent patients. J Pediatr Orthop. 2021;41:e804–e809. doi: 10.1097/BPO.0000000000001906. [DOI] [PubMed] [Google Scholar]
- 6.Levy I.M., Torzilli P.A., Warren R.F. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Jt Surg - Ser A. 1982;64:883–888. [PubMed] [Google Scholar]
- 7.Atay Ö.A., Doral M.N., Aydingöz Ü., Leblebicioglu G. Bilateral discoid medial menisci: Association with bone changes in the tibia. Knee Surg Sport Traumatol Arthrosc. 2001;9:217–220. doi: 10.1007/s001670100204. [DOI] [PubMed] [Google Scholar]
- 8.Ahn J.H., Lee S.H., Yoo J.C., Lee Y.S., Ha H.C. Arthroscopic partial meniscectomy with repair of the peripheral tear for symptomatic discoid lateral meniscus in children: Results of minimum 2 years of follow-up. Arthroscopy. 2008;24:888–898. doi: 10.1016/j.arthro.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Desai B., Warren M., Lavie L.G., Nammour M., Waldron S. Arthroscopic saucerization of a symptomatic posterior horn tear in a discoid medial meniscus. Ochsner J. 2021;21:115–118. doi: 10.31486/toj.19.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jin G., Xin T., Weng Z., et al. Symptomatic complete discoid medial meniscus completely coalesced with the anterior cruciate ligament: A case report and literature review. Orthop Surg. 2022;14:2391–2395. doi: 10.1111/os.13377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sevillano-Perez E., Espejo-Reina A., Espejo-Reina M.J. Symptomatic bilateral torn discoid medial meniscus treated with saucerization and suture. Case Rep Orthop. 2016;2016 doi: 10.1155/2016/8487194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farlett J., Wood J.R. Ipsilateral medial and lateral discoid menisci: A rare combination of infrequent anatomic variants. J Clin Imaging Sci. 2020;10:11. doi: 10.25259/JCIS_133_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lukas K., Livock H., Kontio K., Carsen S. Bilateral discoid medial menisci: A case report and review of the literature. J Am Acad Orthop Surg Glob Res Rev. 2020;4:e20. doi: 10.5435/JAAOSGlobal-D-20-00069. 00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iorio R., Viglietta E., Mazza D., Redler A., Pagnotta S.M., Ferretti A. Saucerization and suture of symptomatic bilateral medial discoid meniscus in a 13 years old male football player: A case report and literature review. Orthop Rev (Pavia) 2022;14 doi: 10.52965/001c.33699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grant J.A., Wilde J., Miller B.S., Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: A systematic review. Am J Sports Med. 2018;6 doi: 10.1177/0363546511411701. [DOI] [PubMed] [Google Scholar]
- 16.Vint H., Quartley M., Robinson J.R. All-inside versus inside-out meniscal repair: A systematic review and meta-analysis. Knee. 2021;28:326–337. doi: 10.1016/j.knee.2020.12.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video demonstrates the diagnosis, surgical technique, and postoperative treatment of a patient with a medial discoid meniscus. Diagnosis and the decision to operate are made through clinical findings and are guided by radiographs and MRIs. Intraoperatively, an examination under anesthesia and diagnostic arthroscopy are performed. The meniscus is saucerized to a stable border of 6-8 mm. An inside-out meniscal repair is performed. Immediately postoperation, the patient is locked in extension and weight bearing as tolerated. Range of motion progression is carried out under the supervision of the treating orthopedic surgeon and physical therapist.
This video demonstrates the diagnosis, surgical technique, and postoperative treatment of a patient with a medial discoid meniscus. Diagnosis and the decision to operate are made through clinical findings and are guided by radiographs and MRIs. Intraoperatively, an examination under anesthesia and diagnostic arthroscopy are performed. The meniscus is saucerized to a stable border of 6-8 mm. An inside-out meniscal repair is performed. Immediately postoperation, the patient is locked in extension and weight bearing as tolerated. Range of motion progression is carried out under the supervision of the treating orthopedic surgeon and physical therapist.