Abstract
Purpose
This study aimed to assess the prevalence of self-reported polycystic ovary syndrome (PCOS) among Emiratis and examine bi-directional associations of PCOS with self-reported chronic diseases, namely: diabetes, asthma, high cholesterol, and high blood pressure.
Patients and Methods
A cross-sectional analysis was performed using the UAE Healthy Future Study (UAEHFS) data collected from February 2016 to April 2022 involving 1040 Emirati women aged 25–67 years from recruitment centers in the United Arab Emirates (UAE). The bi-directional associations between self-reported PCOS and self-reported chronic diseases were evaluated by establishing temporality based on reported age-at-diagnoses. Firstly, the associations between PCOS (diagnosed at ≥25 years) and chronic diseases (diagnosed at <25 years) were examined, followed by PCOS (diagnosed at <25 years) and chronic diseases (diagnosed at ≥25 years). Finally, a Poisson regression under unadjusted and age-and-body mass index (BMI) adjusted models was performed to obtain the risk ratio (RR) and its 95% confidence interval (CI).
Results
The prevalence of PCOS in this study was 25.9%. Those with asthma and high cholesterol diagnosed at <25 years had increased risks of PCOS diagnosed at ≥25 years (RR = 1.79, 95% CI: 1.17–2.76 for asthma; and RR = 1.61, 95% CI: 1.01–2.59 for high cholesterol), compared to those respective healthier counterparts, after adjusting for age and BMI. No significant association was observed between PCOS diagnosed at <25 years and respective chronic diseases diagnosed at ≥25 years.
Conclusion
PCOS prevalence among Emirati women was high. Asthma and high cholesterol in earlier life were associated with PCOS in later life. Understanding how chronic disease conditions and PCOS are associated in bi-directional ways may improve the surveillance of chronic disease conditions among women with PCOS and may also contribute to more targeted PCOS prevention strategies.
Keywords: polycystic ovary syndrome, self-reported diagnosis, epidemiology, women’s health, United Arab Emirates, UAE Healthy Future Study
Introduction
Polycystic ovary syndrome (PCOS) is a common hormonal disorder affecting 4% to 20% of women of reproductive age worldwide.1,2 To date, there are no universal criteria for PCOS diagnosis, making the definition of PCOS vary from one setting to another.3,4 The clinical manifestations of PCOS include irregular or prolonged menstruation, excessive androgen level, and, frequently, obesity.1,5,6 The exact etiology of PCOS is not fully known, however, there are several known common triggers, including genetic, hormonal, and environmental factors.3 Females with low birthweight history,7,8 with low levels of vitamin D,3 with parental PCOS history,9,10 as well as with childhood overweight or adult obesity,10,11 were reported to be at increased risk for subsequent PCOS.
PCOS has been recognized as a chronic metabolic condition beyond a merely reproductive disorder,12 and females with PCOS were found to be more susceptible to chronic diseases compared to females without PCOS.13 Previous studies have established a relationship between concomitant health disorders in females with PCOS.13–15 Obesity and insulin resistance or diabetes among females with PCOS are known to exacerbate the symptoms of PCOS.3,16 Females with PCOS are also known to have a higher risk of cardiovascular diseases, compared to their healthier counterparts.17 In addition, females with PCOS are at higher risk for other chronic diseases, namely: asthma, high cholesterol, and high blood pressure.14,18 The previously-mentioned chronic diseases and PCOS are known to have shared risk factors, including systemic inflammation,16 metabolic factors,12 and hormonal factors.3
Despite the fact of shared risk factors for chronic diseases and PCOS, to our knowledge, there is no bi-directional study on chronic disease conditions and PCOS. We, therefore, aimed to assess the prevalence of self-reported PCOS among Emirati women aged 25 years or above and to examine possible bi-directional associations of self-reported PCOS with self-reported chronic diseases, namely: diabetes, asthma, high cholesterol, and high blood pressure, based on age at diagnoses.
Materials and Methods
Study Design, Participants, and Setting
This is a retrospective cross-sectional study using the UAE Healthy Future Study (UAEHFS) data fielded between February 2016 to April 2022 involving 1040 Emirati women aged 25–67 years. The study design, questionnaire, and methodologies of the UAEHFS are described elsewhere.19 In brief, the UAEHFS is a population-based study that aims to explore risk factors for non-communicable diseases (NCDs) among Emirati nationals aged 18 years and older. Emirati adults were asked to fill out the questionnaire and had some physical measurements taken at multiple centers across major cities in the United Arab Emirates (UAE), namely: Abu Dhabi, Al-Ain, Dubai, and Ras Al Khaimah. All participants were informed of the purpose of the UAE Healthy Future Study.
Measurements
Disease Diagnoses
Self-reported physician diagnoses for PCOS were determined based on the questionnaire response to: “Has a doctor ever told you that you have polycystic ovary syndrome/disease?” (yes, no). Self-reported diabetes or asthma was determined based on the respective questionnaire response to: ‘Has a doctor ever told you that you have diabetes?’ (yes, no); ‘Has a doctor ever told you that you have asthma?’ (yes, no). Whereas, self-reported cholesterol or high blood pressure was determined based on the respective questionnaire response to: ‘Has a doctor ever told you that you have or had high cholesterol?’ (yes, no); ‘Has a doctor ever told you that you have or had high blood pressure?’ (yes, no).
Demographic Characteristics
Age was constructed based on the questionnaire response to “What is your date of birth”. Body Mass Index (BMI) was calculated using the Tanita MC 780 (Tanita Inc., Tokyo, Japan) by nurses at the recruitment centers. Due to a high number of missing values of BMI (15%), we used a missing indicator and categorized BMI into: normal or below (<25 kg/m2), overweight or obese (≥25 kg/m2), and missing.20
Statistical Analysis
Sensitivity analysis to compare the demographic characteristics and self-reported chronic disease conditions between those included in the study and those with missing values of PCOS history was performed to evaluate the pattern of missingness. Demographic characteristics and self-reported chronic disease conditions between women with vs without self-reported PCOS in our study were evaluated using frequencies with percentage (n, %) for categorical variables and means with standard deviations (means ± SD) for continuous variables. A Poisson regression with robust variance to estimate the risk ratio (RR) and its 95% confidence interval (95% CI) were modelled to assess its bi-directional associations. The bi-directional associations between PCOS and chronic diseases were evaluated by establishing temporality between PCOS and chronic diseases based on reported age at diagnoses. The associations between PCOS (diagnosed at ≥25 years) and chronic diseases (diagnosed at <25 years) were evaluated first, followed by PCOS (diagnosed at <25 years) and chronic diseases (diagnosed at ≥25 years). For each bi-directional association, the RR and its 95% CI were obtained for two models: unadjusted and age and BMI-adjusted models. Age and BMI are known to be strong confounding factors in epidemiological studies involving disease outcomes.13,14 The inclusion criteria of those aged 25 years or above with certain PCOS diagnoses (yes or no) and the exclusion of those with PCOS status missing values were made to better address immortal-time bias, as those aged <25 years could not possibly have been diagnosed with PCOS or chronic diseases at 25 years of age or above. The age cut-off of 25 years was used in this study since previous epidemiological studies of PCOS have involved adult populations (mean age of 25 years or above).21 Analyses were carried out using STATA 17.0 (StataCorp, TX, USA). p values < 0.05 were considered statistically significant.
Ethical Approval
The study and its procedures have been reviewed and approved by the Institutional Review Board at New York University Abu Dhabi, Dubai Health Authority, Ministry of Health and Prevention in the UAE, and Health Research and Technology Committee, reference number DOH/HQD/2020/516. Written consent was obtained from participants at the centers or by filling out an online consent form before data collection started.
Results
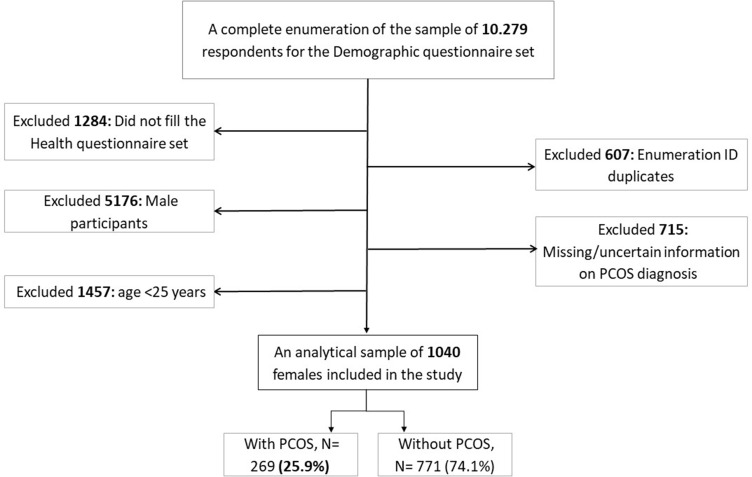
Figure 1 shows the flowchart of the final analytical sample included in this study. For the temporality establishment, we excluded those with uncertain PCOS status and those aged <25 years. After the exclusion criteria, the final analytical sample in our study was 1040 women aged ≥25 years. The prevalence of PCOS in this study was 25.9% (n=269).
Figure 1.
Flowchart of the final analytical sample included in the study.
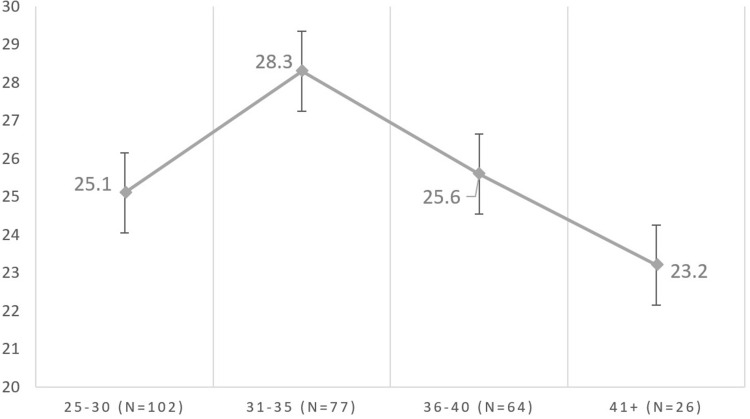
Figure 2 illustrates the prevalence of PCOS in the 5-year age group among participants aged ≥25 years in this study. The PCOS prevalence for each group was described as follows: 25–30 years of age: 25.1%; 31–35 years of age: 28.3%; 36–40 years of age: 25.6%; and 41 years of age or above: 23.2%.
Figure 2.
Prevalence of PCOS by age group among participants in this study (N=1040).
Table 1 shows the demographic characteristics and chronic disease conditions of the participants aged ≥25 years based on PCOS status. Compared to those without PCOS, Emirati women with PCOS had higher BMI levels, a higher proportion reported being overweight or obese, had a higher proportion with poor or fair health status. had a higher proportion with self-reported chronic disease conditions, namely: diabetes, asthma, high cholesterol, and high blood pressure.
Table 1.
Demographic Characteristics and Self-Reported Chronic Disease Conditions Based on PCOS Status (N= 1040)
| Demographic Characteristics and Self-Reported Chronic Disease Conditions | Without PCOS (N=771) | With PCOS (N=269) |
|---|---|---|
| Age, year (mean ± SD) | 33.5 ± 6.8 | 33.0 ± 6.0 |
| BMI, kg/m2 (mean ± SD) | 27.8 ± 6.8 | 28.8 ± 6.6 |
| Overweight/obesity status, n (%) | ||
| Normal or below (<25 kg/m2) | 239 (31.0) | 78 (29.0) |
| Overweight or obese (≥25 kg/m2) | 412 (53.4) | 165 (61.3) |
| Missing | 120 (15.6) | 26 (9.7) |
| Urbanicity, n (%) | ||
| Rural or other non-urban | 80 (10.4) | 27 (10.0) |
| Urban | 691 (89.6) | 242 (90.0) |
| Education levels, n (%) | ||
| <6 years of schooling | 22 (2.9) | 9 (3.4) |
| 6 to 12 years of schooling | 210 (27.2) | 69 (25.7) |
| >12 years of schooling | 539 (69.9) | 191 (71.0) |
| Overall health status, n (%) | ||
| Excellent or good | 593 (76.9) | 196 (72.9) |
| Poor or fair | 178 (23.1) | 73 (27.1) |
| With diabetes, n (%) | ||
| No | 727 (94.3) | 240 (89.2) |
| Yes | 44 (5.7) | 29 (10.8) |
| With asthma, n (%) | ||
| No | 674 (87.4) | 222 (82.5) |
| Yes | 97 (12.6) | 47 (17.5) |
| With high cholesterol, n (%) | ||
| No | 614 (79.6) | 199 (74.0) |
| Yes | 157 (20.4) | 70 (26.0) |
| With high blood pressure, n (%) | ||
| No | 698 (90.5) | 238 (88.5) |
| Yes | 73 (9.5) | 31 (11.5) |
Note: Inclusion age criteria for this analysis: ≥25 years.
Abbreviations: SD, Standard deviation; BMI, Body mass index.
Table 2 presents the risk ratios (RRs) of the associations between self-reported chronic diseases diagnosed at <25 years of age and self-reported PCOS diagnosed at ≥25 years of age. In the age-and-BMI adjusted model, those with asthma and high cholesterol diagnosed at <25 years had significantly increased risk for self-reported older adult PCOS diagnosed at ≥25 years (RR = 1.79, 95% CI: 1.17–2.76 for asthma; RR = 1.61, 95% CI: 1.01–2.59 for high cholesterol), compared to those respective healthier counterparts.
Table 2.
Associations Between Chronic Diseases Diagnosed at <25 Years of Age with PCOS Diagnosed at ≥25 Years of Age
| Risk for Self-Reported PCOS at ≥25 Years | Crude Model | Age and BMI-Adjusted Model | ||
|---|---|---|---|---|
| RR [95% CI] | p-value | RR [95% CI] | p-value | |
| Chronic disease conditions diagnosed at 25 years or below | ||||
| Diabetes | 2.25 [0.86–5.89] | 0.099 | 2.08 [0.81–5.36] | 0.129 |
| Asthma | 1.73 [1.11–2.67] | 0.015 | 1.79 [1.17–2.76] | 0.008 |
| High cholesterol | 2.20 [1.13–4.30] | 0.021 | 1.61 [1.01–2.59] | 0.047 |
| High blood pressure | 1.16 [0.41–3.33] | 0.783 | 1.15 [0.40–3.30] | 0.790 |
Notes: Reference group: those without respective chronic disease conditions. Bold values: Significant at 0.05 (p=value<0.05).
Abbreviations: *CI, Confidence Interval; RR, Risk Ratio; BMI, Body mass index.
Table 3 shows the risk ratios (RRs) of the associations between self-reported PCOS diagnosed at <25 years of age and self-reported chronic diseases diagnosed at ≥25 years of age. We did not find any significant association between self-reported PCOS diagnosed at <25 years and self-reported chronic diseases diagnosed at ≥25 years.
Table 3.
Associations Between PCOS Diagnosed at <25 Years of Age with Chronic Diseases Diagnosed at ≥25 Years of Age
| Risk for Self-Reported Chronic Diseases at ≥25 Years | Crude Model | Age and BMI-Adjusted Model | ||
|---|---|---|---|---|
| RR [95% CI] | p-value | RR [95% CI] | p-value | |
| Diabetes | 0.70 [0.17–2.97] | 0.630 | 0.76 [1.18–3.23] | 0.709 |
| Asthma | N/A | N/A | ||
| Cholesterol | 0.92 [0.52–1.62] | 0.760 | 1.06 [0.60–1.88] | 0.842 |
| High blood pressure | 0.78 [0.34–1.78] | 0.554 | 1.23 [0.53–2.86] | 0.633 |
Notes: Reference group: women without PCOS.
Abbreviations: *CI, Confidence Interval; RR, Risk Ratio; N/A, not available; BMI, Body mass index.
Table 4 presents the comparison of demographic characteristics and self-reported chronic disease conditions of Emirati women aged 18+ years between women with vs without self-reported PCOS status. Those with missing PCOS status information were shown to be older and had a similar BMI. Furthermore, those with missing PCOS status had significant missing values of other chronic disease conditions ranging from 36.8% to 60.8%.
Table 4.
Demographic Characteristics and Self-Reported Chronic Disease Conditions Based on Certain and Uncertain PCOS Status
| Demographic Characteristics and Self-Reported Chronic Disease Conditions | Final Sample (N=2497) | Missing on PCOS Status (N=715) |
|---|---|---|
| Age, year (mean ± SD) | 25.9 ± 7.7 | 27.8 ± 9.3 |
| BMI, kg/m2 (mean ± SD) | 26.0 ± 6.8 | 26.6 ± 6.8 |
| Overweight/obesity status, n (%) | ||
| Normal or below (<25 kg/m2) | 1088 (43.6) | 212 (29.7) |
| Overweight or obese (≥25 kg/m2) | 1004 (40.2) | 240 (33.6) |
| Missing | 405 (16.2) | 263 (36.8) |
| Urbanicity, n (%) | ||
| Rural or other non-urban | 362 (14.5) | 46 (6.4) |
| Urban | 2135 (85.5) | 234 (32.7) |
| Missing | 435 (60.8) | |
| Education attainment, n (%) | ||
| <6 years of schooling or missing | 97 (3.9) | 257 (35.9) |
| 6 to 12 years of schooling | 1122 (44.9) | 204 (28.5) |
| >12 years of schooling | 1278 (51.2) | 254 (35.5) |
| Overall health status, n (%) | ||
| Excellent or good | 1903 (76.2) | 292 (40.9) |
| Poor or fair | 594 (23.8) | 96 (13.5) |
| Missing | 327 (45.7) | |
| With diabetes, n (%) | ||
| No | 2392 (95.8) | 345 (48.3) |
| Yes | 105 (4.2) | 11 (1.5) |
| Missing | 359 (50.2) | |
| With asthma, n (%) | ||
| No | 2215(88.7) | 262 (36.6) |
| Yes | 282 (11.3) | 25 (3.5) |
| Missing | 428 (59.9) | |
| With high cholesterol, n (%) | ||
| No | 2145 (85.9) | 342 (47.8) |
| Yes | 352 (14.1) | 48 (6.7) |
| Missing | 325 (45.5) | |
| With high blood pressure, n (%) | ||
| No | 2329 (93.3) | 367 (51.3) |
| Yes | 168 (6.7) | 23 (3.2) |
| Missing | 325 (45.5) |
Abbreviations: SD: Standard deviation, BMI: Body mass index. Inclusion criteria: women aged 18+ years.
Discussion
In this study, the prevalence of self-reported PCOS among Emirati women aged ≥25 years was 25.9% (Figure 1), and the distribution of those with PCOS among adult Emiratis aged ≥25 years based on the 5-year age group showed that women aged 31–35 years had the highest PCOS prevalence (Figure 2). Our estimates were found to be similar to another United Arab Emirates (UAE) study that found 27.6% PCOS prevalence based on the NIH criteria among university students aged 18–24 years.10 In contrast, the prevalence in our study from multiple recruitment center across UAE was shown to be higher than a recent single site UAE study that found 13% of self-reported PCOS prevalence among Emirati university students aged 18–25 years.22 We believe the difference in diagnosis criteria, sample characteristics, and sampling design used in the studies, contributed to these differences. The Middle Eastern population in general and the Gulf region especially are known to have a considerable prevalence of PCOS, with at least 20%-25% of women in this region affected by PCOS.3 In the UAE, an increasing rate of obesity has been suspected to contribute to an increasing rate of PCOS in this country, as obesity increases PCOS susceptibility.3
The significant association between self-reported asthma in earlier life (diagnosed at age <25 years) with self-reported PCOS later in life (diagnosed at ≥25 years) were observed, after adjusting for age and BMI. Asthma and PCOS were suggested to have similar risk factors and known to be associated in many ways, including in metabolic syndrome and proinflammatory profiles.16 Compared to non-asthmatics, those with asthma tend to be diagnosed with subsequent chronic diseases due to immune system impairment and persistent systemic inflammation.23,24 Similarly, those with PCOS are known to be associated with low-grade systemic inflammation.25 Our finding on the association between asthma and PCOS was different from an Australian study that found no association between asthma and PCOS in their age and BMI-adjusted model.14 However, this study could not establish the temporality and only included self-reported respiratory symptoms for asthma diagnosis, whereas we used self-reported doctor-diagnosed asthma with clear temporality based on age at diagnosis of asthma or PCOS. Due to the very low sample size in our analysis for this direction, we could not explore the association between self-reported PCOS in earlier life (diagnosed at <25 years) and self-reported asthma later in life (diagnosed at ≥25 years). A previous epidemiological study suggested that PCOS was an independent risk factor for subsequent asthma and suggested chronic systemic inflammation as one of the possible mechanisms to explain this linkage.26
In addition, this study also revealed a significant association between high cholesterol diagnosed in earlier life with PCOS later in life, independent of age and BMI status. Metabolic syndrome, including high cholesterol profile in earlier life (childhood and adolescence), is known to be associated with other metabolic syndromes such as PCOS.27 On a different note, we found no significant association in another direction (PCOS diagnosed in earlier life and high cholesterol in later life). Women with a history of PCOS are known to have higher concentrations of total cholesterol, compared to those without PCOS.28 A cross-sectional Australian study found no significant association between cholesterol medication use and PCOS.14 On the contrary, a prospective British study revealed a significant association between PCOS and high cholesterol, in their crude and BMI-adjusted models.28 However, this study included middle-aged women in the baseline, implying a different phenotype of PCOS. The expression of PCOS in adolescence and early adulthood may differ from and does not necessarily resemble that of clinical and endocrinological features observed in later adulthood.21
The influence of BMI in this study was shown to only shift the point estimates, however, the significance persisted even after adjusting for BMI (Table 2), implying that BMI (or obesity) was not fully responsible for the associations between chronic disease conditions and PCOS bi-directionally. A previous study revealed that the relationship between PCOS and chronic disease conditions can be explained only partially by the relationship between PCOS and obesity.28 Obesity is known to be associated with PCOS due to the involvement of low-grade systemic inflammation, hence promoting insulin resistance and metabolic disorders, all of which contribute to the development of PCOS.29 We believe future studies to examine whether obesity mediates the association between PCOS and chronic diseases are worth exploring.
In this study, there was no significant association observed between diabetes and high blood pressure with PCOS. Even though previous studies found a significant association between diabetes and PCOS.13,14 Shared metabolic risk factors such as insulin resistance, may explain the association between diabetes or high blood pressure with PCOS.12 Our findings were in agreement with from previous studies that found significant associations between diabetes,13,14 and hypertension,13 with PCOS. We believe that a low sample size and statistical power for the association of diabetes and high blood pressure with PCOS in our analysis may contribute to these non-significant findings.
Strengths and Limitations
This cross-sectional study comprehensively examined the bi-directional associations between several chronic disease conditions, namely: self-reported diabetes, asthma, high cholesterol, and high blood pressure, with self-reported PCOS. The clear temporality based on age at disease diagnosis for each self-reported disease included in this study were able to improve the validity our findings. To improve the generalizability of this study, multiple recruitment centers in four major cities across the UAE were chosen to be included. Despite the above strengths, our study was subject to several limitations. One major limitation was self-reported PCOS and other chronic disease conditions, raising concerns about disease ascertainment accuracies. However, previous epidemiological studies found self-reported PCOS and other chronic diseases to be reliable.30,31 In addition, the self-reported age of diagnoses, such as asthma and diabetes, have been shown to be accurate.32,33 Furthermore, by adjusting for age in our age and BMI, this study aimed to better address possible age effects of recall error for the self-reported diseases. This study also prone to selection bias due to inclusion criteria based on PCOS status, however, our sensitivity analyses revealed non-systematic mechanisms in the missingness pattern of those with and without PCOS status (Table 4). Lastly, our study may be prone to residual confounding factors, such as physical activity and smoking status.13
Conclusion
PCOS prevalence among Emirati women in this study was high. Asthma and high cholesterol in earlier life were associated with PCOS in later life. Understanding how chronic disease conditions and PCOS are associated in bi-directional ways may improve the surveillance of comorbid conditions among women with PCOS and may also contribute to more targeted PCOS prevention strategies.
Acknowledgments
The authors would like to thank all members of the Public Health Research Center at New York University Abu Dhabi and those who are actively involved in the UAE Healthy Future Study (UAEHFS).
Funding Statement
This publication is based upon works supported by Tamkeen under Research Institute Grant No. G1206.
Disclosure
The authors declare no conflicts of interest in this work.
References
- 1.March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25(2):544–551. doi: 10.1093/humrep/dep399 [DOI] [PubMed] [Google Scholar]
- 2.Deswal R, Narwal V, Dang A, Pundir CS. The prevalence of polycystic ovary syndrome: a brief systematic review. J Hum Reprod Sci. 2020;13(4):261. doi: 10.4103/jhrs.JHRS_95_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dalibalta S, Abukhaled Y, Samara F. Factors influencing the prevalence of polycystic ovary syndrome (PCOS) in the United Arab Emirates. Rev Environ Health. 2022;37(3):311–319. doi: 10.1515/reveh-2021-0036 [DOI] [PubMed] [Google Scholar]
- 4.Wiencek JR, McCartney CR, Chang AY, Straseski JA, Auchus RJ, Woodworth A. Challenges in the assessment and diagnosis of polycystic ovary syndrome. Clin Chem. 2019;65(3):370–377. doi: 10.1373/clinchem.2017.284331 [DOI] [PubMed] [Google Scholar]
- 5.Barbieri RL, Ehrmann DA. Clinical manifestations of polycystic ovary syndrome in adults. UpToDate. 2014;17. [Google Scholar]
- 6.Franks S, McCarthy MI, Hardy K. Development of polycystic ovary syndrome: involvement of genetic and environmental factors. Int J Androl. 2006;29(1):278–285. doi: 10.1111/j.1365-2605.2005.00623.x [DOI] [PubMed] [Google Scholar]
- 7.Sadrzadeh S, Hui E, Schoonmade L, Painter R, Lambalk C. Birth weight and PCOS: systematic review and meta-analysis. Hum Reprod Open. 2017;2017(2):hox010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Melo A, Vieira C, Barbieri M, et al. High prevalence of polycystic ovary syndrome in women born small for gestational age. Hum Reprod. 2010;25(8):2124–2131. doi: 10.1093/humrep/deq162 [DOI] [PubMed] [Google Scholar]
- 9.De Leo V, Musacchio M, Cappelli V, Massaro M, Morgante G, Petraglia F. Genetic, hormonal and metabolic aspects of PCOS: an update. Reprod Biol Endocrinol. 2016;14(1):1–17. doi: 10.1186/s12958-016-0173-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Begum GS, Shariff A, Ayman G, Mohammad B, Housam R, Khaled N. Assessment of risk factors for development of polycystic ovarian syndrome. Diabetes. 2017;1:2. [Google Scholar]
- 11.Aarestrup J, Pedersen DC, Thomas PE, et al. Birth weight, Childhood body mass index, height and growth, and risk of polycystic ovary syndrome. Obes Facts. 2021;14(3):283–290. doi: 10.1159/000515294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El Hayek S, Bitar L, Hamdar LH, Mirza FG, Daoud G. Polycystic ovarian syndrome: an updated overview. Front Physiol. 2016;7:124. doi: 10.3389/fphys.2016.00124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kujanpää L, Arffman RK, Pesonen P, et al. Women with polycystic ovary syndrome are burdened with multimorbidity and medication use independent of body mass index at late fertile age: a population‐based cohort study. Acta Obstet Gynecol Scand. 2022;101(7):728–736. doi: 10.1111/aogs.14382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Avery JC, Moran LJ, Moore V, et al. Prevalence of self-reported polycystic ovary syndrome and profiles of health among women of different generations: a cross sectional study. Fertil Reprod. 2019;1(03):141–147. doi: 10.1142/S2661318219500154 [DOI] [Google Scholar]
- 15.Glintborg D, Hass Rubin K, Nybo M, Abrahamsen B, Andersen M. Morbidity and medicine prescriptions in a nationwide Danish population of patients diagnosed with polycystic ovary syndrome. Eur J Endocrinol. 2015;172(5):627–638. doi: 10.1530/EJE-14-1108 [DOI] [PubMed] [Google Scholar]
- 16.Xu Y, Zhou Z-Y, Pan J-X, Huang H-F. Associations between asthma and polycystic ovary syndrome: current perspectives. Front Endocrinol. 2022;13:936948. doi: 10.3389/fendo.2022.936948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Scicchitano P, Dentamaro I, Carbonara R, et al. Cardiovascular Risk in Women With PCOS. Int J Endocrinol Metab. 2012;10(4):611–618. doi: 10.5812/ijem.4020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grieger JA, Hodge A, Mishra G, Joham AE, Moran LJ. The association between dietary intake, asthma, and PCOS in women from the Australian Longitudinal Study on Women’s Health. J Clin Med. 2020;9(1). doi: 10.3390/jcm9010233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdulle A, Alnaeemi A, Aljunaibi A, et al. The UAE healthy future study: a pilot for a prospective cohort study of 20,000 United Arab Emirates nationals. BMC Public Health. 2018;18(1):1–9. doi: 10.1186/s12889-017-5012-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization Consultation on Obesity. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]
- 21.Michelmore KF. Polycystic ovary syndrome in adolescence and early adulthood. Hum Fertil. 2000;3(2):96–100. doi: 10.1080/1464727002000198771 [DOI] [PubMed] [Google Scholar]
- 22.Pramodh S. Exploration of lifestyle choices, reproductive health knowledge, and polycystic ovary syndrome (Pcos) awareness among female Emirati University students. Int J Womens Health. 2020;12:927. doi: 10.2147/IJWH.S272867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Juhn YJ. Influence of asthma epidemiology on the risk for other diseases. Allergy Asthma Immunol Res. 2012;4(3):122–131. doi: 10.4168/aair.2012.4.3.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sumino K, O’Brian K, Bartle B, Au DH, Castro M, Lee TA. Coexisting chronic conditions associated with mortality and morbidity in adult patients with asthma. J Asthma. 2014;51(3):306–314. doi: 10.3109/02770903.2013.879881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zierau L, Gade EJ, Lindenberg S, Backer V, Thomsen SF. Coexistence of asthma and polycystic ovary syndrome: a concise review. Respir Med. 2016;119:155–159. doi: 10.1016/j.rmed.2016.08.025 [DOI] [PubMed] [Google Scholar]
- 26.Htet TD, Teede HJ, De Courten B, et al. Asthma in reproductive-aged women with polycystic ovary syndrome and association with obesity. Eur Respir J. 2017;49:5. doi: 10.1183/13993003.01334-2016 [DOI] [PubMed] [Google Scholar]
- 27.Al-Hamad D, Raman V. Metabolic syndrome in children and adolescents. Trans Pediatr. 2017;6(4):397. doi: 10.21037/tp.2017.10.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wild S, Pierpoint T, Jacobs H, McKeigue P. Long-term consequences of polycystic ovary syndrome: results of a 31 year follow-up study. Hum Fertil. 2000;3(2):101–105. doi: 10.1080/1464727002000198781 [DOI] [PubMed] [Google Scholar]
- 29.Hardy OT, Czech MP, Corvera S. What causes the insulin resistance underlying obesity? Curr Opin Endocrinol Diabetes Obes. 2012;19(2):81. doi: 10.1097/MED.0b013e3283514e13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teede HJ, Joham AE, Paul E, et al. Longitudinal weight gain in women identified with polycystic ovary syndrome: results of an observational study in young women. Obes. 2013;21(8):1526–1532. doi: 10.1002/oby.20213 [DOI] [PubMed] [Google Scholar]
- 31.Van der Heyden J, De Bacquer D, Tafforeau J, Van Herck K. Reliability and validity of a global question on self-reported chronic morbidity. J Public Health. 2014;22(4):371–380. doi: 10.1007/s10389-014-0624-9 [DOI] [Google Scholar]
- 32.Torén K, Palmqvist M, Löwhagen O, Balder B, Tunsäter A. Self-reported asthma was biased in relation to disease severity while reported year of asthma onset was accurate. J Clin Epidemiol. 2006;59(1):90–93. doi: 10.1016/j.jclinepi.2005.03.019 [DOI] [PubMed] [Google Scholar]
- 33.Pastorino S, Richards M, Hardy R, et al. Validation of self-reported diagnosis of diabetes in the 1946 British birth cohort. Prim Care Diabetes. 2015;9(5):397–400. doi: 10.1016/j.pcd.2014.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]