Abstract
The number of patients that return for recall appointments has great importance to validate endodontic treatment outcomes. The purpose of this review was to investigate the rate of return on recall and the main factors that influence this rate of return. A literature review was performed in the PubMed database for the years from 1978 to 2017, using the following keywords: recall rate, endodontic treatment, endodontic retreatment, apical surgery. The inclusion criteria were: prospective studies in English, and in vivo research with humans, which included patient return rates. A total of 35 studies that fulfilled the established criteria were selected. The percentage of patients who returned on recall was 56%. More female patients (60%) attended the recall appointments than male (40%). The three main reasons for not returning were: patients did not observe the follow-up appointment (490), not returning due to a lack of interest (99) and changing their address (222). The age of the patients attending the appointments varied from 28.6 to 62 years old, with the highest percentage of patients that returned ranging from 40 to 52.5 years old. According to the literature the optimal rate of return for follow-up treatment should be greater than 80%, for the validity of the research. However, the reality presented in the studies is far from ideal. Many studies do not even mention these rates of return in their methodologies or in their results, which may mask the true treatment success rates.
Key Words: Endodontic Recall, Follow-up, Recall
Introduction
Microorganisms are the main etiological factor of pulp and periradicular diseases, which can be due to caries, dental trauma or iatrogenic procedures. The main goal of endodontic treatment is to treat or prevent the development of periradicular lesions. Therefore, adequate mechanical and chemical preparation of the root canal, along with the use of auxiliary irrigation solutions and intracanal medication with effective antimicrobial action should be carried out. Also, root canal filling must be carried out with great care to prevent any possible reinfection. These precautions reduce the presence of bacteria in the root canal system, creating an appropriate environment to treat periradicular diseases [1].
The success rates described for primary endodontic treatments are considered high, since less than 15% of the cases fail. However, even in adequately treated canals the disinfection procedures often fail to reach the bacteria located in isthmuses, branches, apical deltas, irregularities and dentinal tubules. Such regions, which are difficult to access with endodontic instruments or intracanal medication, may be involved in the failure of endodontic therapy, and therefore require endodontic reintervention [2].
Proper follow-up and recall visits are required to define the success or failure of the endodontic therapy. It is important that patients return for revision visits at least 6 and 12 months after the end of treatment. Clinical examinations and control radiographs at these consultations allow the evaluation of the quality of the obturation, the coronally sealing and the tissue response in the periapical region [3].
However, many patients do not return for these recall visits. Consequently, the low number of returns, frequently described in longitudinal studies, may negatively influence the quality of the scientific evidence obtained. The outcome of endodontic treatment of patients who do not return for these recall appointments is impossible to determine, and this could certainly influence the rates of success and failure described in the studies [4]. Thus, these returns or recall visits are important to evaluate the outcome of endodontic therapies.
The present study characterizes, through a literature review, the frequency of return for different types of endodontic treatment (primary treatment, retreatment and para-endodontic surgery).
Materials and Methods
An electronic search was performed in the PubMed (MEDLINE) database for the years from 1978 to 2017 using the following keywords: recall rate, endodontic treatment, endodontic retreatment and apical surgery. The inclusion criteria for this review were: human studies, published in English, and those that referred to the rate of return of patients. In vitro studies, animal studies and studies that did not include the initial sample number were excluded, as were retrospective studies.
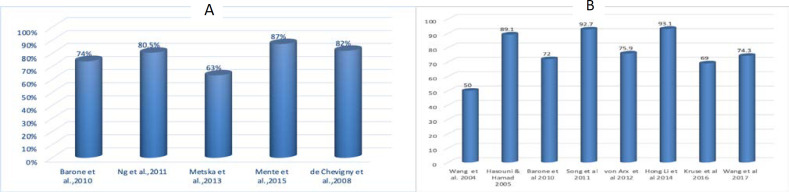
The percentages indicated in Figures 1, 2 and 4, as well as the data represented in Tables 1 and 2, were collected from the articles included in the present study. The percentage calculations in Figure 3 were based on the total sum of the population surveyed and the number of individuals who returned for the recall consultations. These data were from the studies included in this review.
Figure 1.
A) Patient return rates; B) Recall rates based on teeth
Figure 2.
Percentage of return; A) by patients; B) by teeth; C) by gender
Figure 4.
A) Percentage of successful non-surgical retreatment; B) Success rates of surgical retreatment (%)
Table 1.
Studies included in the present review
| Authors | Year | Age | Women | Men | Initial Consultation |
Final
Consultation |
Recall | Treatment success | Retreat. success | Surgical success | Evaluated period |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jurcak et al . [ 5 ] | 1993 | 18-50 | - | 97 | 167 | 97 | 58% | 89% | - | - | 1 y |
| Sjögren et al .[ 15 ] | 1997 | - | - | - | 55 | 53 | 96.30% | 68% | - | - | 5 y |
| Kvist & Reit [ 23 ] | 1999 | 52 | - | - | 92 | 88 | 95% | - | - | - | 48 m |
| Weiger et al .[ 30 ] | 2000 | 11-84 | 37 | 30 | 73 | 67 | 92% | 76% | - | - | 5 years |
| Peters; Wesselink [ 28 ] | 2002 | 19-86 | 19 | 20 | 39 | 39 | 100% | 81% | - | - | 4 and a half y |
| Friedman et al. [ 19 ] | 2003 | - | - | - | 277 | 141 | 51% | 81% | - | - | 4-6 y |
| Farzaneh et al . [ 20 ] | 2004 | 45 | - | - | 316 | 153 | 48% | 87% | - | - | 4-6 y |
| Gorni; Gagliani [ 24 ] | 2004 | 16-74 | 214 | 211 | 451 | 425 | 94.20% | - | - | - | 24 m |
| Hasouni & Hamad [ 13 ] | 2005 | 12-67 | 120 | 136 | 336 | 256 | 76.20% | - | - | 89.10% | 6, 12 and 24 m |
| Chevigny et al. [ 22 ] | 2008 | 45 | - | - | 511 | 137 | 27% | 88% | - | - | 4-6 years |
| Ross et al . [ 3 ] | 2009 | 6-80 | 1716 | 1033 | 5641 | 2749 | 49.00% | - | - | - | 6 m-1 y |
| Barone et al . [ 12 ] | 2010 | - | - | - | 226 | 146 | 85% | - | 74% | 72% | 4 - 10 y |
| Ng et al . [ 17 ] | 2011 | - | - | - | 1093 | 675 | 69.2% T, 55%R | 83.90% | 80.50% | - | 1 - 4 y |
| Song et al . [ 2 ] | 2011 | 30-60 | - | - | 54 | 42 | 77.80% | - | - | 92.70% | 6 m- 2 y |
| Ricucci et al. [ 29 ] | 2011 | - | - | - | 780 | 470 | 60.30% | 92.00% | - | - | 5 y |
| VonArx et al . [ 14 ] | 2012 | - | - | - | 194 | 170 | 87.60% | - | - | 75,9 % | 5 y |
| Saini et al . [ 26 ] | 2012 | 18-72 | - | - | 167 | 130 | 77.8 | 99.20% | - | X | 1 y |
| Ferrari et al . [ 33 ] | 2012 | - | - | - | 345 | 304 | 88.10% | 60% | - | X | 72 m |
| Angerame et al. [ 16 ] | 2013 | - | - | - | 84 | 63 | 75% | 95% | - | X | 6 m |
| Metska et al . [ 10 ] | 2013 | 20-70 | - | - | 37 | 27 | 73% | - | 6% | X | 1 y |
| Dorasani et al . [ 27 ] | 2013 | 18-62 | - | - | 57 | 44 | 71.87% | 61% | - | X | 1 y |
| Mente et al . [ 18 ] | 2014 | - | - | - | 282 | 205 | 73% | - | - | X | 42 m |
| Li et al. [ 6 ] | 2014 | 11-62 | 49 | 33 | 94 | 82 | 87.20% | - | - | 93,10% | 2 y |
| Mente et al . [ 9 ] | 2015 | 23-69 | - | - | 24 | 22 | 92% | - | 87% | X | 8 y |
| Kruse et al . [ 25 ] | 2016 | 40-85 | - | - | 44 | 30 | 68% | - | - | 69% | 1-6 y |
| Walivaara et al . [ 32 ] | 2016 | - | - | - | 186 | 166 | 89.20% | 85% | - | X | 12 m |
| Wang et al . [ 11 ] | 2017 | 14-57 | - | - | 81 | 59 | 72.80% | - | 74.30% | 12-30 mo | |
| Wang et al . [ 34 ] | 2004 | - | - | - | 203 | 194 | 95.50% | - | 50% | 4-8 y | |
| Zhang et al . [ 35 ] | 2015 | - | - | - | 130 | 54 | 67% | - | X | 2 y | |
| Patel et al . [ 36 ] | 2012 | 6-76 | - | - | 132 | 99 | 75% | 73,90% | - | X | 1 y |
| Song et al. [ 7 ] | 2013 | - | - | - | 584 | 431 | 74% | - | - | 85.60% | 10 y |
| Song et al. [ 8 ] | 2013 | - | 85 | 55 | 199 | 140 | 68% | - | - | 85.20% | 7 y |
| Friedman et al . [ 31 ] | 1995 | - | - | - | 486 | 378 | 78% | - | - | X | 8-18 m |
| Jokinen et al . [ 37 ] | 1978 | 16-75 | - | - | 2592 | 1199 | 46% | 53.00% | X | 2-7 y | |
| Chevigny et al. [ 22 ] | 2008 | 45 | - | - | 383 | 157 | 41% | - | 82% | X | 4-6 y |
Table 2.
Reasons for absence from follow-up visits
| Number of patients who did not attend recall visit | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Authors | No reply | Refusal | Lack of interest | Sickness | Death | Change of address | Not found | Teeth lost | *D/S/CA | Others |
| Friedman et al. [19] | - | - | - | - | 9 | 100 | - | - | - | - |
| Farzaneh et al. [20] | 121 | 11 | - | - | 4 | 105 | - | - | - | - |
| Chevigny et al. [21] | 331 | - | 99 | - | - | - | - | - | - | - |
| Barone et al. [12] | - | - | - | - | - | - | - | - | 66 | - |
| VonArx et al. [14] | 6 | - | - | - | - | - | 3 | 12 | - | 3 |
| Mente et al. [18] | 30 | 30 | - | - | - | 17 | - | - | - | - |
| Kruse et al. [25] | 1 | - | - | 2 | 3 | - | - | - | - | 6 |
| Total | 490 | 41 | 99 | 2 | 16 | 222 | 3 | 12 | 66 | 9 |
Figure 3.
A) Mean age versus recall consultations (%); B) Success rate for initial endodontic treatment
Results
Having applied the inclusion criteria, 35 articles were selected for the present study to build the database [2, 3, 5-37] (Table 1).
The return rates reported in this review, when the reference unit was the patient, ranged from 27-100% (Figure 1), while in the studies using the number of teeth, the return rates ranged from 26% -100% (Figure 1).
In the studies included in this review, 8,489 patients out of 15,209 (56% of the sample) returned for the recall appointments (Figure 2).
When using the "teeth" as the reference unit, a total of 12,623 were initially evaluated and 7,038 returned for the follow-up consultation, representing a 56% return percentage (Figure 2).
Women attended more recall visits (60%) than men (40%) (Figure 2). However, this calculation was only based on the articles that cited the number of men and women in the study. Thus, the articles that did not include gender information were not included here; also the article by Metska et al. [10] was left out as it only evaluated male patients in the military.
Not all the studies reported the reason the patients did not attend these recall visits. Only seven studies included such data. A total of 490 patients did not respond to the calls for the recall visit, while 222 could not be contacted due to a change of address and 99 did not return due to a lack of interest. The main reasons for these absences are represented in Table 2.
The present study pointed out that only 13 authors included the mean age of the patients who returned for their recall appointments. The blue columns in Figure 3 represent the mean ages, while the red columns represent the percentage of patients who returned. According to the data collected, the mean age ranged from 28.6 to 62 years old, and the highest return rates were of patients with mean ages of 40 and 52.5 years old.
The follow-up period of the studies in this review ranged from six months to ten years. The success rates for primary treatment, non-surgical retreatment and surgical retreatment ranged from 60% to 99.2%, from 63% to 87%, and from 50% to 93.1%, respectively (Figure 4).
Discussion
The present study collected data from 15,209 patients that underwent endodontic therapy (primary endodontic treatment, endodontic retreatment and periradicular surgery) and of these, only 56% (8,489) returned for the recall visits. This return rate was considered relatively low. In the Toronto studies phases 3 and 4, these values were even lower, because 333 teeth were lost to follow up, 18 were extracted and only 41% were examined for [21, 22].
The ideal in longitudinal studies is that there is no loss of patient follow-ups; however, a minimum of 80% is considered acceptable in the literature for patients who return for reevaluation visits [22].
However, the authors in the majority of the studies did not include the number of patients who returned for the reassessment consultations in their methodology; this lack of data may well generate inconsistent results[38].
There was a notable difference between female and male patients where women showed greater interest in the reassessment consultations than men. This difference was also noted [3] where the female rate of return was 52%, a rate higher than that of men. The most plausible explanation for this is that the female sex is more concerned with health care as a whole, besides being more attentive to aesthetics than men [3].
Only 13 studies in this review evaluated age as a variable. In those studies, the age ranged from 28.6 to 62 years old. Patients included in the 40- to 52-year-olds made a higher percentage of follow-up visits. In general the older patients returned for the recall appointments at a statistically higher rate than expected [3]. This can possible be explained by the fact that retired patients have more time available to return for consultations, in contrast, patients who work most of the day often have difficulties scheduling a recall visit, thus reducing rates of return [4].
However, in the selected studies of this review, the occupational status of the patients who returned to the recall appointments was not reported; consequently, it was not possible to make a link between occupational statuses and return rates.
In order to achieve a minimum return percentage of 80%, some strategies are needed to reduce the absenteeism of these patients [22]. In the studies included in the present review, various strategies were made to get the patients to return, such as phone calls, more than once if necessary, leaving messages when direct contact was not established, sending letters and in the most recent studies, sending e-mails. Similar strategies were used in other study [17] where the authors aimed to obtain the largest possible number of patients to evaluate the results of endodontic treatments. Some papers, in this review, did not even explain in their methodology when or how such strategies were made. Most studies only reported that the patients did not return, without specifying any reasons for the absence.
The patients who were diagnosed with pulp necrosis prior to treatment and those with periradicular lesions had higher rates of return[3]. This is probably due to the fact that the professionals emphasized that there was a bone lesion in that region, which generates a certain concern on the part of the patient and therefore an incentive to return for a more complete follow-up. These authors also pointed out that patients who had some kind of pre-existing symptom such as pain or swelling are more likely to return than asymptomatic patients are.
The studies that reported the return rate of patients to evaluate the success of non-surgical endodontic retreatments, showed that the success rates ranged from 63% to 87% (mean of 75%), These results are very close to those presented [39] in 2009, where the percentage of successful non-surgical retreatment was between 54.17% and 85.9%. These authors [39] demonstrated that the follow-up time of these studies ranged from two to six years, whereas in the present review, the follow-up time was one to eight years.
The follow-up period for the rates of surgical retreatment, ranged from six months to eight years, and they had a 50% to 93% success rate (mean of 71.5%). The study [39] reported success rates ranging from 27.84% to 94.29%, with a follow-up period ranging from 2 to ≥ 6 years.
Previous publications have stated that the longer the follow-up period, the lower the patient's return rates [40]. In other words, over time there is a greater loss of patients, and consequently this could lead to an overestimation or even an underestimation of the success rates. This statement is confirmed in the results of Kurse et al. study [25] that in their six year follow-up program, the return rate was only 20%. In other study [7] the follow-up period was ten years and presented an incredibly low percentage of return in the final period of around 0.5%. As this study had a very long follow-up period (ten years) many patients did not return for numerous reasons, including the loss of the tooth in question [7].
The present study investigated the return rate for recall visits through a review of studies that reported such values. A low number of absenteeism is important for the scientific validity of the studies, since representative samples generate a greater weight in the results of the analyses. However, some limitations were observed in the present study, such as: most longitudinal studies did not report the number of patients that returned for the follow-up evaluations, and this therefore impedes an accurate analysis for these research models and consequently the results may not represent the reality of the study objective.
Other factors also hindered making of this review, for example: many authors did not mention in their methodology whether there was a patient recruitment program or not; the studies had different reference units (teeth, roots, channels, patients, treatment, retreatment) and, finally, the follow-up periods varied widely among the studies.
Conclusion
According to the current literature, the ideal rate of return for recall appointments should be at least 80% of the initial population; so that the results of clinical studies can be considered representative [22].
When this minimum return rate is not reached, the results may be compromised, that is, the results of successes or failures may not represent that particular population. However, the present study clearly showed that female patients return more frequently to their recall visits than male patients.
Finally, there is a need to carry out new studies that previously review the standardization of their methodologies and new technologies should be applied to encourage patients to attend their clinical recall evaluations.
Conflict of Interest:
‘None declared’.
References
- 1.Siqueira JF Jr. Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J. 2001;34(1)::1–10. doi: 10.1046/j.1365-2591.2001.00396.x. [DOI] [PubMed] [Google Scholar]
- 2.Song M, Shin , SJ , Kim E. Outcomes of endodontic micro-resurgery: a prospective clinical study. J Endod. 2011;37(3)::316–20. doi: 10.1016/j.joen.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 3.Ross C, Scheetz J, Crim G, Caicedo R, Morelli J, Clark S. Variables affecting endodontic recall. Int Endod J. 2009;42(3)::214–9. doi: 10.1111/j.1365-2591.2008.01504.x. [DOI] [PubMed] [Google Scholar]
- 4.Rubinstein RA. Reflections on designing and conducting long-term surgical studies. J Endod. 2002;28:384–5. doi: 10.1097/00004770-200205000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Jurcak JJ, Bellizzi R, Loushine , RJ Successful single-visit endodontics during Operation Desert Shield. J Endod. 1993;19(8)::412–3. doi: 10.1016/S0099-2399(06)81507-4. [DOI] [PubMed] [Google Scholar]
- 6.Li H, Zhai F, Zhang R, Hou B. Evaluation of microsurgery with SuperEBA as root-end filling material for treating post-treatment endodontic disease: a 2-year retrospective study. J Endod. 2014;40(3)::345–50. doi: 10.1016/j.joen.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Song M, Kim SG, Lee SJ, Kim B, Kim E. Prognostic factors of clinical outcomes in endodontic microsurgery: a prospective study. J Endod. 2013;39(12)::1491–7. doi: 10.1016/j.joen.2013.08.026. [DOI] [PubMed] [Google Scholar]
- 8.Song M, Kim SG, Shin SJ, Kim HC, Kim E. The influence of bone tissue deficiency on the outcome of endodontic microsurgery: a prospective study. J Endod. 2013;39(11)::1341–5. doi: 10.1016/j.joen.2013.06.036. [DOI] [PubMed] [Google Scholar]
- 9.Mente J, Leo M, Michel A, Gehrig H, Saure D, Pfefferle T. Outcome of orthograde retreatment after failed apicoectomy: use of a mineral trioxide aggregate apical plug. J Endod. 2015;41(5)::613–20. doi: 10.1016/j.joen.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Metska ME, Parsa A, Aartman IH, Wesselink PR, Ozok AR. Volumetric changes in apical radiolucencies of endodontically treated teeth assessed by cone-beam computed tomography 1 year after orthograde retreatment. J Endod. 2013;39(12)::1504–9. doi: 10.1016/j.joen.2013.08.034. [DOI] [PubMed] [Google Scholar]
- 11.Wang ZH, Zhang MM, Wang J, Jiang L, Liang YH. Outcomes of Endodontic Microsurgery Using a Microscope and Mineral Trioxide Aggregate: A Prospective Cohort Study. J Endod. 2017;43(5)::694–98. doi: 10.1016/j.joen.2016.12.015. [DOI] [PubMed] [Google Scholar]
- 12.Barone C, Dao TT, Basrani BB, Wang N, Friedman S. Treatment outcome in endodontics: the Toronto study-phases 3, 4, and 5: apical surgery. J Endod. 2010;36(1)::28–35. doi: 10.1016/j.joen.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Hasouni MK, Hamad SA. Success rate of apicectomy of anterior and premolar teeth. Dent J. 2005;5(2)::161–7. [Google Scholar]
- 14.VonArx T, Jensen SS, Hänni S, Friedman S. Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod. 2012;38(5)::570–9. doi: 10.1016/j.joen.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997;30(5)::297–306. doi: 10.1046/j.1365-2591.1997.00092.x. [DOI] [PubMed] [Google Scholar]
- 16.Angerame D, DeBiasi M, Sossi D. Periapical healing after simplified endodontic treatments: A digital subtraction radiography study. G Ital Endod. 2013;27(2)::74–9. [Google Scholar]
- 17.Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44(7)::583–609. doi: 10.1111/j.1365-2591.2011.01872.x. [DOI] [PubMed] [Google Scholar]
- 18.Mente J, Hufnagel S, Leo M, Michel A, Gehrig H, Panagidis D. Treatment outcome of mineral trioxide aggregate or calcium hydroxide direct pulp capping: long-term results. J Endod. 2014;40(11)::1746–51. doi: 10.1016/j.joen.2014.07.019. [DOI] [PubMed] [Google Scholar]
- 19.Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: the Toronto Study Phase 1: initial treatment. J Endod. 2003;29(12)::787–93. doi: 10.1097/00004770-200312000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Farzaneh M, Abitbol S, Lawrence HP, Friedman S. Toronto Study Treatment outcome in endodontics-the Toronto Study Phase II: initial treatment. J Endod. 2004;30(5)::302–9. doi: 10.1097/00004770-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S. Treatment outcome in endodontics: the Toronto study-phases 3 and 4: orthograde retreatment. J Endod. 2008;34(2)::131–7. doi: 10.1016/j.joen.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Chevigny C, Dao TT, Basrani BR, Marquis V, Farzaneh M, Abitbol S. Treatment outcome in endodontics: the Toronto study-phase 4: initial treatment. J Endod. 2008;34(3)::258–63. doi: 10.1016/j.joen.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 23.Kvist T, Reit C. Results of endodontic retreatment: a randomized clinical study comparing surgical and nonsurgical procedures. J Endod. 1999;25(12)::814–7. doi: 10.1016/S0099-2399(99)80304-5. [DOI] [PubMed] [Google Scholar]
- 24.Gorni FG, Gagliani MM. The outcome of endodontic retreatment: a 2-yr follow-up. J Endod. 2004;30(1)::1–4. doi: 10.1097/00004770-200401000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Kruse C, Spin-Neto R, Christiansen R, Wenzel A, Kirkevang LL. Periapical Bone Healing after Apicectomy with and without Retrograde Root Filling with Mineral Trioxide Aggregate: A 6-year Follow-up of a Randomized Controlled Trial. J Endod. 2016;42(4)::533–7. doi: 10.1016/j.joen.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 26.Saini HR, Tewari S, Sangwan P, Duhan J, Gupta A. Effect of different apical preparation sizes on outcome of primary endodontic treatment: a randomized controlled trial. J Endod. 2012;38(10)::1309–15. doi: 10.1016/j.joen.2012.06.024. [DOI] [PubMed] [Google Scholar]
- 27.Dorasani G, Madhusudhana K, Chinni SK. Clinical and radiographic evaluation of single-visit and multi-visit endodontic treatment of teeth with periapical pathology: An in vivo study. J Conserv Dent. 2013;16(6): 484–8. doi: 10.4103/0972-0707.120933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters LB, Wesselink PR. Periapical healing of endodontically treated teeth in one and two visits obturated in the presence or absence of detectable microorganisms. Int Endod J. 2002;35(8)::660–7. doi: 10.1046/j.1365-2591.2002.00541.x. [DOI] [PubMed] [Google Scholar]
- 29.Ricucci D, Russo J, Rutberg M, Burleson JA, Spångberg LS. A prospective cohort study of endodontic treatments of 1,369 root canals: results after 5 years. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(6)::825–42. doi: 10.1016/j.tripleo.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 30.Weiger R, Rosendahl R, Löst C. Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesions. Int Endod J. 2000;33(3)::219–26. doi: 10.1046/j.1365-2591.1999.00298.x. [DOI] [PubMed] [Google Scholar]
- 31.Friedman S, Löst C, Zarrabian M, Trope M. Evaluation of success and failure after endodontic therapy using a glass ionomer cement sealer. J Endod. 1995;21(7)::384–90. doi: 10.1016/S0099-2399(06)80976-3. [DOI] [PubMed] [Google Scholar]
- 32.Walivaara DA, Abrahamsson P, Fogelin M. Periapical Surgery with IRM and MTA as Retrograde Root-end Fillings‒A Prospective Randomized Clinical Study of 186 Consecutive Teeth. Dentistry. 2016;6(9)::1–6. [Google Scholar]
- 33.Ferrari M, Vichi A, Fadda GM, Cagidiaco MC, Tay FR, Breschi L. A randomized controlled trial of endodontically treated and restored premolars. J Dent Res. 2012;91:72–8. doi: 10.1177/0022034512447949. [DOI] [PubMed] [Google Scholar]
- 34.Wang Q, Cheung GSP, Ng RPY. Survival of surgical endodontic treatment performed in a dental teaching hospital: a cohort study. Int Endod J. 2004;37(11)::764–75. doi: 10.1111/j.1365-2591.2004.00869.x. [DOI] [PubMed] [Google Scholar]
- 35.Zhang MM, Liang YH, Gao XJ, Jiang L, vanDer Sluis L, Wu MK. Management of Apical Periodontitis: Healing of Post-treatment Periapical Lesions Present 1 Year after Endodontic Treatment. J Endod. 2015;41(7)::1020–5. doi: 10.1016/j.joen.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 36.Patel S, Wilson R, Dawood A, Foschi F, Mannocci F. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography-part 2: a 1-year post-treatment follow-up. Int Endod J. 2012;45(8)::711–23. doi: 10.1111/j.1365-2591.2012.02076.x. [DOI] [PubMed] [Google Scholar]
- 37.Jokinen MA, Kotilainen R, Poikkeus P, Poikkeus R, Sarkki L. Clinical and radiographic study of pulpectomy and root canal therapy. Scand J Dent Res. 1978;86(5)::366–73. doi: 10.1111/j.1600-0722.1978.tb00639.x. [DOI] [PubMed] [Google Scholar]
- 38.Friedman S. In: Essential Endodontology: Prevention and Treatment of Apical Periodontitis. 2 ed. Orstavik D PFT, editor. Oxford: Blackwell Munksgaard; 2008. pp. 408–69. [Google Scholar]
- 39.Torabinejad M Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009;35(7) doi: 10.1016/j.joen.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 40.Ørstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J. 1996;29(3) doi: 10.1111/j.1365-2591.1996.tb01361.x. [DOI] [PubMed] [Google Scholar]