Abstract
Schwannomas are uncommon benign tumors of the peripheral nerves with a low risk of malignant transformation. They rarely affect children, can affect any part of the body but rarely occur in the lower extremity and typically present with a palpable mass, pain or neurological signs. Imaging helps to orient the diagnosis and anatomopathological examination helps to confirm it. We report a case of a 12-year-old girl who presented with left knee pain with subcutaneous mass overlying the tibial tuberosity medially. Clinical examination revealed a positive Tinel’s sign. Magnetic resonance imaging (MRI) of the knee was performed, which revealed an encapsulated subcutaneous soft tissue mass overlying the tibial tuberosity medially, eccentric to the course of the infrapatellar branch of the saphenous nerve. The patient was operated with total intracapsular excision of the lesion and the anatomopathological study of the surgical specimen came back in favor of a schwannoma. Postoperatively, the patient showed a good recovery with disappearance of pain and swelling.
Keywords: Schwannoma, Saphenous nerve, Child, Imaging, Diagnosis
Introduction
Peripheral nerve tumors are rare tumors with an incidence of 1/100 000. The vast majority of these tumors are schwannomas. These tumors develop on the Schwann cells that form the sheath of the peripheral nerves.1 Schwannomas can affect any part of the body but rarely occur in the lower limb, and is even rarer in the saphenous nerve. The incidence of schwannomas in the saphenous nerve is still unknown due to sporadic publications in the literature. This rarity leads to its misdiagnosis. The clinical presentation of these tumors is usually a palpable mass, pain or other neurological symptoms.2,3 We report a case of a schwannoma of a saphenous nerve branch in a 12-year-old girl.
Case Report
A 12-year-old child with no medical or traumatic history presented with a swelling left knee progressively increasing in size for 3 months associated with a slight pain without any particular irradiation. The physical examination found a patient in good general condition, apyretic, a subcutaneous mass overlying the tibial tuberosity medially of the left knee, with no signs of inflammation, hard consistency, fixed and slightly painful to palpation. Neurological examination revealed intact motor and sensory function with a positive Tinel’s sign. A radiograph of the knee was requested and showed an opaque oval shaped subcutaneous mass overlying the tibial tuberosity medially, well limited, with regular contours, respecting the bone cortex (Figure 1). A complementary MRI was performed and showed the presence of a subcutaneous oval shaped mass overlying the tibial tuberosity medially of the tibia, lateralized to the right, which appeared encapsulated, in T1 isosignal (compared to muscle) heterogeneous T2 hyper signal, intensely and heterogeneously enhanced after injection of gadolinium measuring 50 mm × 44 mm × 20 mm, containing cystic areas and seems to continue upwards with a nerve structure with eccentric development, associated with a discret infiltration of the peri lesion fat, without involvement of the bone structures in front of it evoking at first a schwannoma of the infra patellar branch of the saphenous nerve, given the eccentric development of the tumor in relation to the nerve fibers (Figure 2). The patient underwent surgery, a total intracapsular excision of the lesion was performed preserving the saphenous nerve. Anatomopathological study of the sections taken from the surgical excision specimen shows a tumor proliferation well limited in the periphery, with spindle-shaped cells, often arranged in short intersecting bundles and separated by collagenous fibrous tissue. The tumor cells are monomorphic without mitotic activity and adopt a pallissadic arrangement with the formation of Verocay nodules (Figure 3) confirming the diagnosis of a schwannoma. Postoperatively, the patient showed good recovery, with disappearance of pain and swelling.
Figure 1.

X-ray of the left knee, face and profile, showing the presence of an opaque, oval, well-limited, subcutaneous soft tissue mass with clear contours, respecting the adjacent bony structures, opposite the upper end of the anterior tibial tuberosity.
Figure 2.
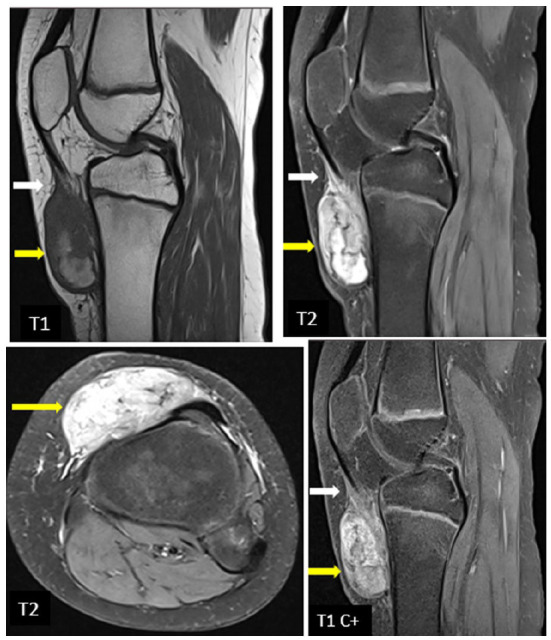
MRI of the left knee in T1 sagittal section, T2 sagittal and axial sections and T1 sagittal section after injection of gadolinium showing the presence opposite the anterior tibial tuberosity, a mass at the expense of the saphenous nerve with eccentric development, lateralized on the right, oval, appears encapsulated, in T1 isosignal (compare to the muscle) in heterogeneous T2 hyper signal, intensely and heterogeneously enhanced after injection of gadolinium, containing cystic areas, associated with a discreet infiltration of the peri lesion fat, without involvement of the bone structures in front of it, evoking first a schwannoma of the infra patellar ramus of the saphenous nerve.
Figure 3.

(A) Spindle cell tumor made of short intersecting bundles (HE × 100) and (B) tumor cells are monomorphic neuroid in appearance showing a palisading arrangement in places (HE × 200).
Discussion
Peripheral nerve tumors are rare tumors that arise from the nerve sheath. They can be distinguished as schwannomas, neurofibromas and malignant peripheral nerve sheath tumors (MPNST). Schwannomas account for about 1% of all soft tissue tumors4 and are the most frequent peripheral nerve tumors (70%).1,4 They can appear in any peripheral nerve of the body, mainly in the head and neck, and are most often located in the brachial plexus (39%), followed by a slight preponderance in the upper extremities (30%) and less occurrence in the lower extremities (24%). The saphenous nerve is rarely affected, represent less than 1% of all cases. All the path of the nerve can be the site of this tumor.5
Schwannomas can occur at any age, but predominate between 20 and 50 years of age with a sex ratio close to 1 and they rarely affect children.6,7 Malignant transformation is rare. They are encapsulated, well-defined tumors, eccentric to the nerve path. The tumors repress the nerve fascicles, hence the paucity of neurological symptoms despite the large size of lesions.6,7
Because of the slow growth rate, the duration of symptoms before diagnosis is often long, up to several years. Indeed, schwannomas of peripheral nerves are usually revealed by palpation of a swelling on the path of a nerve (43%-96%) and/or pain (85%) and/or paresthesias (25%) along the path of the nerve. The occurrence or an increased pain at night is found in 25% of cases.7,8 When the tumor is palpable, it is usually firm and mobile in the direction perpendicular to the nerve. Percussion may awaken pain or paresthesias in the path of the incriminated nerve, with a Tinel’s sign present in 65% of cases.9 Physical examination is usually normal, with schwannomas causing a preoperative motor neurological deficit in only 12% of cases.9
The diagnosis is usually made after analyzing the medical history and physical examination, and usually requires multimodal imaging including standard radiographs, ultrasound and MRI. Standard radiographs of schwannomas are usually normal or only notable for the presence of calcifications. In our case, the standard radiograph of the knee showed the presence of a subcutaneous soft tissue mass. Ultrasound is useful for more superficial tumors and has the advantage of being cost-effective, readily available and allows an initial analysis in consultation. the schwannoma appears as a hypoechoic mass, eccentric to the nerve carrier that can be visualized upstream and/or downstream of the tumor with its fibrillar structure preserved. the cross section revealed the mass in the shape of a “target.” The neurofibroma represents the differential diagnosis. unlike schwannoma, it appears as a solid mass well centered in relation to the supporting nerve, whose fibrillar structure disappears completely.10
MRI is the iconographic examination of choice in the diagnosis of schwannomas and preoperative workup. The tumor presents as an eccentric mass in the path or the root of the nerve, with the nerve being individualized at its entrance and exit from the tumor on coronal and sagittal sections. The schwannoma is classically hypo- or isosignal to the muscle on T1 sequences and hypersignal on T2 sequences, intensely and heterogeneously enhancing after injection of gadolinium and sometimes containing cystic areas. MRI distinguishes between a schwannoma and a neurofibroma. This distinction is very important, as the invasive aspect of the neurofibroma does not allow dissection of the tumor, hence the high risk of sequelae and recurrence.4
The definitive diagnosis should be based on histologic and sometimes immunohistochemical findings. Histologically, the tumor is characterized by streams of spindle cells, often with elongated nuclei arranged in a palisading pattern. Areas with thick concentrations of cells are termed Antoni type A (Verocay body), while areas with loose, irregularly arranged cells are Antoni type B. Positive immunostaining for S-100 protein indicates a Schwann cell origin.11
Neurofibromas are also derived from Schwann cells and should be considered in the histopathological examination. Unlike schwannomas, neurofibromas do not have a true capsule. Instead, they have a dense cellular consistency and an increased number of mitoses. Histologic sections show locally invasive areas, and there is no Verocay body formation. Neurofibromas are usually multifocal, which is an important clinical distinction from schwannomas.12
Surgery remains the treatment of choice for the management of schwannomas. Ambulatory surgery is usually performed under locoregional anesthesia. The surgical approach is centered on the tumor and allows exposure of the nerve upstream and downstream of the tumor. Intraoperative ultrasound can be used to accurately localize the tumor, primarily in the setting of small intradermal schwannomas or intramuscular tumors. Nerve stimulation can be used to check the motor function of the nerve intraoperatively. The primary objective of the surgery is to respect the continuity and integrity of the nerve. The surgery will therefore consist of enucleation of the schwannoma after opening the epineurium under optical magnification.5,9
The surgical results for peripheral schwannomas are good overall, with improvement in pain and sensory symptoms in nearly 90% of cases.5,9
Conclusion
Schwannoma of the saphenous nerve in children is a rare tumor, responsible for unexplained chronic pain and swelling. Diagnosis is often late at the stage of a bulky tumor. Ultrasound and MRI can differentiate schwannoma from a neurofibroma. The diagnosis is based on histological study. The eccentricity of the tumor generally allows for removal without sequelae.
Footnotes
Author Contributions: All authors contributed equally to this work.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Amine Cherraqi  https://orcid.org/0000-0003-1838-4631
https://orcid.org/0000-0003-1838-4631
Ola Messaoud  https://orcid.org/0000-0002-2798-1633
https://orcid.org/0000-0002-2798-1633
References
- 1. Chagou A, Benameur H, Hassoun J, Jaafar A. Schwannome du nerf sciatique (à propos d’un cas). Pan Afr Med J. 2020;37:233. doi: 10.11604/pamj.2020.37.233.22745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cubas Farinha N, Livraghi S. Saphenous nerve schwannoma as a cause of vascular claudication - case report and review of the literature. Br J Neurosurg. 2022;36:280-283. doi: 10.1080/02688697.2018.1524078 [DOI] [PubMed] [Google Scholar]
- 3. Albert P, Patel J, Badawy K, et al. Peripheral nerve Schwannoma: a review of varying clinical presentations and imaging findings. J Foot Ankle Surg. 2017;56:632-637. [DOI] [PubMed] [Google Scholar]
- 4. Chick G, Alnot JY, Silbermann-Hoffman O. Benign solitary tumors of the peripheral nerves. Rev Chir orthopedique reparatrice appareil Mot. 2000;86:825-834. [PubMed] [Google Scholar]
- 5. Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg. 2005;102:246-255. [DOI] [PubMed] [Google Scholar]
- 6. Martinez Algarra JC, Gastaldi Rodrigo P, Palomares Talens E. Le schwannome multiple du nerf sciatique: à propos d'un cas. Rev Chir Orthop Reparatrice Appar Mot. 1999;85(6):632-635. [PubMed] [Google Scholar]
- 7. Kralick F, Koenigsberg R. Sciatica in a patient with unusual peripheral nerve sheath tumors. Surg Neurol. 2006;66(6):634-637. [DOI] [PubMed] [Google Scholar]
- 8. Lapierre F, Rigoard P, Wager M. [Peripheral nerve tumors]. Neurochirurgie. 2009;55(4-5):413-420. [DOI] [PubMed] [Google Scholar]
- 9. Guha D, Davidson B, Nadi M, et al. Management of peripheral nerve sheath tumors: 17 years of experience at Toronto Western Hospital. J Neurosurg. 2018;128(4):1226-1234. [DOI] [PubMed] [Google Scholar]
- 10. Chiou HJ, Chou YH, Chiou SY, Liu JB, Chang CY. Peripheral nerve lesions: role of high resolution US. Radiographics. 2003;23(6):e15. [DOI] [PubMed] [Google Scholar]
- 11. Young B, Heath JW. Wheater’s Functional Histopathology: A Text and Colour Atlas, 4th ed. Churchill Livingstone; 2000. [Google Scholar]
- 12. Peace WJ, Pacelli LL, Botte MJ. Schwannoma of the femoral nerve. Curr Orthop Pract. 2009;20(6):695-697. doi: 10.1097/bco.0b013e3181be034b [DOI] [Google Scholar]


