Abstract
Objective
We investigated the prevalence and risk factors of ARI in children under 5 years old in 37 SSA countries.
Methods
Data from Demographic and Health Survey (DHS) of 37 African countries was examined in this analysis. Data from children under the age of 5 years old were examined. Forest plot was used to identify disparities in the occurrence of ARIs across SSA countries.
Results
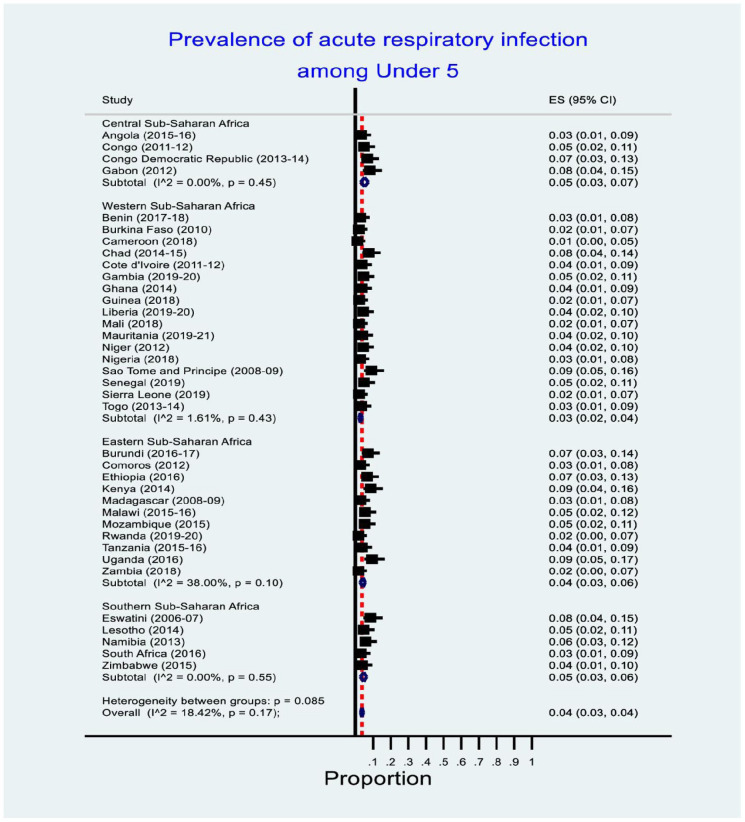
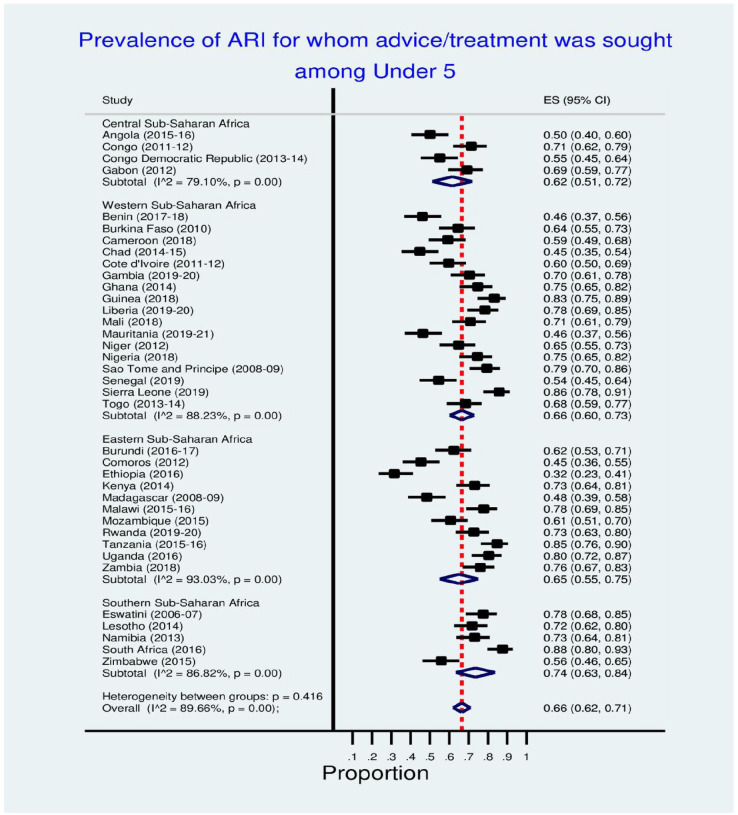
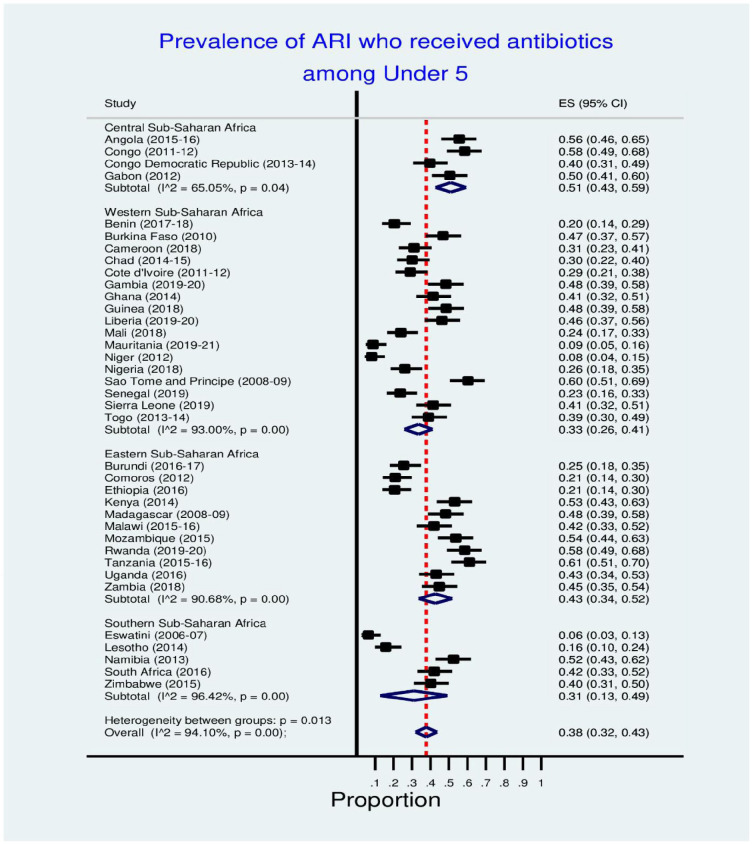
We observed a higher prevalence of ARI among children under 5 in Uganda, Kenya, Sao Tome and Principe (9% each), Gabon, Chad, Eswatini (8% each), Burundi, Ethiopia, Congo Democratic Republic (7.0% each). The prevalence of ARI among under-five children who sought medical advice/treatment from health facility was higher in South Africa (88%), Sierra Leone (86%), Tanzanian (85%), Guinea (83%) and Uganda (80%). The prevalence rate of ARI among under-five children who received antibiotics was higher in Tanzania (61%), Sao Tome and Principe (60%), Rwanda and Congo (58% each), Angola (56.0%), Mozambique (54.0%), Kenya (53.0%), Namibia (52.0%) and Gabon (50.0%). This study found that the household wealth index, maternal education, and urban residence were significantly associated with ARI (p <0.001). A higher prevalence of ARI was observed among urban residents, low income families, and those with mothers with lower education.
Conclusion
ARI prevalence could be reduced by improving household socioeconomic status, child nutrition and community awareness of indoor and outdoor pollution. Interventions and programs focused on early diagnosis, treatment and prevention of ARIs are crucial in reducing ARIs particularly in developing countries.
Keywords: acute respiratory infection, sub-Saharan countries, prevalence, under-five children
Background
Acute respiratory infections (ARIs) have been known to be among the major causes of death and illness in children who are less than 5 years old.1,2 Colds and the flu are the most frequent ARIs, which comprise both upper and lower respiratory tract illnesses.2 The World Health Organization (WHO) estimates that respiratory infections provide 6% of the worldwide disease burden, which is a larger percentage than the burdens of cancer, HIV infection, ischemic heart disease, diarrheal illness, and malaria.3 Globally, an estimated 6.6 million children under 5 die annually; 95% of these deaths occur in low-income countries, and ARIs account for a third of all deaths.3 A lower respiratory infection caused 704 000 deaths in children under 5, per the 2017 Global Burden of Disease (GBD) report.4 Globally, acute respiratory infections significantly burden healthcare systems and are a primary reason young children are admitted to hospitals.5 More than 12 million children under 5 are hospitalized yearly due to ARIs.3
Despite a sharp drop over the past 20 years,6 ARI remains to be a serious global public health fear, especially in sub-Saharan Africa (SSA). About half of all mortalities among children under 5 in 2017 were in SSA, with ARIs being the foremost source of mortality.6 A study that examined the rate and risk factors for acute lower respiratory infections (ALRIs) in children under the age of 5 years in 28 SSA countries found that the prevalence of ALRIs was 25.3% across the board.7 Children living in this region are more likely to experience multiple deprivations such as poor contact to healthcare, malnutrition, dearth of access to safe drinking water and rudimentary sanitation, HIV infection, crowded living conditions, and environmental toxins and pollutants like indoor and outdoor air pollution.8-10
Acute respiratory infection is linked with numerous factors, including children’s demographics, parents’ socio-economic levels, residence types and the environment in which they are raised. Studies in the SSA region and other emerging economies have observed a correlation between ARIs and age,7,11-13 sex,12,14 immunization status,12 HIV infection,3 diarrheal comorbidity,2,14 malnutrition14,15 and improper weaning timing.15 Several research has demonstrated the association between parental characteristics and ARIs, including parent age,13,16-18 work status12 and educational level.3,12 Other variables have been implicated to an elevated risk of ARIs, such as socioeconomic status,11,15 home type18 and household size, as well as lack of hygiene and sanitation facilities,17 have been linked with increased risk of ARIs. Smokers in the household, type of fuel used for cooking, poor drinking water quality, and lack of toilets are some examples of lifestyle and environmental factors that increase the risk of developing ARIs.3,15,17
There is a lack of information about ARI among children under 5 in SSA countries, considering the impact of ARI on morbidity and death in children under 5 within this region. However, the uneven distribution of ARI episode occurrence among the SSA countries has not been well investigated. Given that SSA has the uppermost mortality rate (55%) of under-five deaths, the accessibility of data on the incidence and danger aspects of ARI is essential for attaining the Sustainable Development Goal (SDG) of plummeting child death to at least 125 per 1000 live birth in every country.19 Therefore, it is imperative to examine the prevalence and determining factors of ARI at the regional and national levels to target future programming implications in order to lower the rates of ARI in SSA nations.
The study was designed to understand the prevalence of ARI amongst children who are under the age of 5 in SSA. The Demographic Health Survey (DHS), conducted between 2006 and 2021, was used to extract the data. The unique aspect of this study is how it examines ARI prevalence using current, nationally representative samples. The study’s findings, which offer empirical proof of country differences in ARI distribution in SSA, will address gaps in the literature. The study’s conclusions may be useful in creating provincial and national policies to lower the risk of ARI-linked morbidity and mortality.
Methods
Data Source
We investigated secondary cross-sectional statistical data from Demographic and Health Surveys (DHS) in African countries from 2006 to 2021. DHS collects data using a multistage cluster stratified sampling strategy. The stratification method was used to divide the respondents into groups based on their geographic location, which was typically defined by one’s place of residence: urban versus rural. A multi-level stratified approach was used to segment the population into first-level strata, then into second-level strata, and so on. The 2 levels of stratification in the DHS were determined by geographic location and urban/rural status. The study looked at the following countries: Angola, Cameroon, Benin, Congo Democratic Republic Burkina Faso, Burundi, Egypt, Eritrea, Chad, Comoros, Nigeria, Congo, Cote d’Ivoire, Eswatini, Ethiopia, Gabon, Gambia, Liberia, Ghana, Togo, Uganda, Guinea, Kenya, Lesotho, Madagascar, Morocco, Mozambique, Namibia, Malawi, Mali, Niger, Rwanda, Senegal, Sierra Leone, Sao Tome and Principe, South Africa, Tanzania, Zambia, Zimbabwe. DHS data is publicly available and can be found at http://dhsprogram.com/data/available-datasets.cfm.
These surveys being carried out every 5 years, started since 1984 in over 85 countries. The sampling method of data collection which is uniform across nations, allowing for the comparability of results between nations, is a significant benefit of DHS. Although the DHS was developed to supplement the fertility, and family planning, and demographic information gathered by the World Fertility Surveys (WFSs) and Contraceptive Prevalence Surveys (CPSs), it has rapidly grown to be the greatest significant basis of population investigation for the tracking of population health guides, particularly in resource-limited locations. The DHS gathers information on immunizations, maternal and infant mortality, domestic violence, fertility, female genital mutilation, communicable and non-communicable diseases, nutrition, water and sanitation, lifestyle, family planning, and other health-related concerns. DHS succeeds at acquiring high-quality data by offering adequate interviewer training, nationwide coverage, a uniform data collecting instruments, and methodological approaches of issues that are simple for legislators and decision-makers to comprehend. Epidemiologic studies that compute prevalence, movements, and disparities can be made using data from the DHS. Details about DHS have previously been made public.20 The list of researched countries and the survey year are presented in Table 1. The surveys were carried out between 2008 and 2020. Details can be found in Table 1 below.
Table 1.
Sample Size for Under-Five Children in Demographic and Health Survey, 2006 to 2021.
| Country | Survey year | Number of children |
|---|---|---|
| Angola | 2015-16 | 14 322 |
| Benin | 2017-18 | 13 589 |
| Burkina Faso | 2010 | 15 044 |
| Burundi | 2016-17 | 13 192 |
| Cameroon | 2018 | 9733 |
| Chad | 2014-15 | 18 623 |
| Comoros | 2012 | 3149 |
| Congo | 2011-12 | 9329 |
| Congo Democratic Republic | 2013-14 | 18 716 |
| Cote d’Ivoire | 2011-12 | 7776 |
| Eswatini | 2006-07 | 2812 |
| Ethiopia | 2016 | 10 641 |
| Gabon | 2012 | 6067 |
| Gambia | 2019-20 | 8362 |
| Ghana | 2014 | 5884 |
| Guinea | 2018 | 7951 |
| Kenya | 2014 | 20 964 |
| Lesotho | 2014 | 3138 |
| Liberia | 2019-20 | 5704 |
| Madagascar | 2008-09 | 12 448 |
| Malawi | 2015-16 | 17 286 |
| Mali | 2018 | 9940 |
| Mauritania | 2019-21 | 11 628 |
| Mozambique | 2015 | 5178 |
| Namibia | 2013 | 5046 |
| Niger | 2012 | 12 558 |
| Nigeria | 2018 | 33 924 |
| Rwanda | 2019-20 | 8092 |
| Sao Tome and Principe | 2008-09 | 1931 |
| Senegal | 2019 | 6125 |
| Sierra Leone | 2019 | 9899 |
| South Africa | 2016 | 3548 |
| Tanzania | 2015-16 | 10 233 |
| Togo | 2013-14 | 6979 |
| Uganda | 2016 | 15 522 |
| Zambia | 2018 | 9959 |
| Zimbabwe | 2015 | 6132 |
Selection and Measurement of Variables
Outcome
The study’s main outcome is acute respiratory infection. Respondents reported this in binary form: “yes” or “no.” Acute respiratory infections are classified into 2 types: lower respiratory tract infections and upper respiratory tract infections (ARIs). The upper respiratory tract consists of the airways from the nose to the vocal cords of the larynx. The offshoot of the airways from the trachea and bronchi to the lower respiratory tract’s bronchioles and alveoli. This was in line with earlier study.18
Independent Variables
Sex of the child: Male child versus female child; residence: urban resident versus rural resident; education of the mother: no formal education/primary versus secondary/higher education; wealth quintiles: lowest versus second versus middle versus fourth versus highest. The DHS wealth index was kept because it can be found directly in the dataset.21 The wealth index for the household in DHS was created by creating an index that is linear using ownership of asset variables and measuring it with the help of principal component analysis. In the initial survey, the wealth index was formed by giving each household a score and placing each household member based on their scores. Then, equal category distributions of 5 were fragmented with each of the population being represented as 20% and included economic indicators as well as the housing standard, household amenities, number of consumer goods, and the land holding size. We maintained the survey’s original 5 groups for the wealth index (lowest, second, middle, fourth, highest).
Analytical Approach
All of the sampling weights, the clustering as well as the stratification, were taken into consideration with the help of Stata survey module (“svy”). Percentages were used to assess the rate of occurrence. Stunting, anemia, and exclusive breastfeeding were evaluated with a forest plot analysis to see how varied they were between the countries. In order to draw conclusions from observational data, a forest plot can be used. Regarding descriptive data and the visual representation of summary statistics like prevalence, Stata software has no limits. Additionally, calculations were made for the weighted effect size (w*es) for each country’s prevalence in the forest plot. We also multiplied every effect size using the study weight to arrive at this total. The Q-test is similar to t-test for gaging countries’ heterogeneity. We also computed this as the summation of squares of the variances between the effects in each distinct study and the collective effect for all nations, with the weights assumed to be the same as those presented in the pooling procedure. Q follows a chi-square distribution with k-1 degrees of freedom (k being the total number of countries). The equality of countries is our null hypothesis. At the 5% significance level, we reject the null (hence the countries’ estimates were dissimilar). We set the significant level at 5%. The analysis was performed in Stata 14.0 version (StataCorp, College Station, TX, USA).
Ethical Approval and Informed Consent
This study looked at anonymized public domain datasets based on populations. The authors got the permission of MEASURE DHS/ICF International to use the data. When it comes to protecting respondents’ personal information, the DHS Program follows all applicable norms. When it comes to the survey, ICF International makes sure everything is in order with the US Department of Health and Human Services’ Human Subjects Protection Act. DHS team obtained consent from the several countries’ National Health Research Ethics Committees before carrying out the surveys. No more permissions were needed for this investigation. For more on our data and ethical standards, check out this link: http://goo.gl/ny8T6X.
Results
Table 1 shows the number of under-five children concerning whom information was elicited. Overall, 381 424 children were analyzed in this study.
Figure 1 shows acute respiratory infection prevalence among children less than under-5 years in sub-Saharan countries. Uganda, Kenya, Sao Tome and Principe (9.0%), Gabon, Chad, Eswatini (8.0%), Burundi, Ethiopia, Congo Democratic Republic (7.0%) have higher ARI prevalence among under-five children respectively.
Figure 1.
Prevalence of acute respiratory infection among under-5 children in sub-Saharan countries.
Table 2 shows the distribution of children who are under-5 years with symptoms of ARI in SSA countries. Based on the results, children of mothers with little or no education had higher prevalence of acute respiratory infection in comparison to the children with mothers who had higher education in most of the studied countries. There is not much difference in the distribution of ARI among rural and urban residents and among the highest household wealth quintiles and the lowest wealth quintiles in many of the studied countries. The same trend is observed in the sex of the children, as we observed disparities from different countries with regards to ARI prevalence in under-five children.
Table 2.
Distribution of Under 5 Children with Symptoms of Acute Respiratory Infection in SSA Countries.
| Country | Sex | Residence | Mother’s education | Household wealth quintiles | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Urban | Rural | No education | Primary | Secondary | Higher | Lowest | Second | Middle | Fourth | Highest | |
| Angola | 3.6 | 3 | 3.3 | 3.3 | 3.2 | 3.8 | 2.7 | 2.8 | 3.6 | 3 | 3.5 | 3.1 | 3.2 |
| Benin | 3 | 2.7 | 2.3 | 3.2 | 3.1 | 2.5 | 2.6 | 0.6 | 3.2 | 3.8 | 3 | 2.8 | 1.3 |
| Burkina Faso | 2.1 | 1.7 | 2.9 | 1.7 | 1.8 | 2.4 | 3.4 | 0 | 1.3 | 1.7 | 1.6 | 2.2 | 3 |
| Burundi | 7.4 | 6.7 | 4.1 | 7.4 | 7.1 | 7.5 | 5.3 | 1.5 | 8.8 | 8 | 6.5 | 6.2 | 5.3 |
| Cameroon | 0.9 | 1.1 | 1.1 | 0.9 | 0.4 | 1.2 | 1.3 | 1 | 0.4 | 1.4 | 1.3 | 1 | 0.8 |
| Chad | 7.6 | 7.5 | 7.7 | 7.5 | 6.6 | 9.7 | 8.5 | 6.8 | 8.8 | 7.4 | 7.5 | 6.6 | 7.3 |
| Comoros | 2.9 | 2.7 | 3.2 | 2.6 | 3.1 | 2.1 | 2.7 | 4.2 | 3.1 | 1.7 | 3.2 | 2.9 | 3.2 |
| Congo | 4.5 | 5.3 | 4.9 | 4.9 | 4.6 | 5 | 4.7 | 7.7 | 5.5 | 5.2 | 3.8 | 4.8 | 5 |
| Congo Democratic Republic | 6.9 | 6.5 | 6 | 6.9 | 7.7 | 7 | 5.9 | 2.8 | 7.1 | 6.8 | 7.3 | 6.8 | 5 |
| Cote d’Ivoire | 3.4 | 3.8 | 3.7 | 3.5 | 3.4 | 3.7 | 4.8 | 2.3 | 3.1 | 3.3 | 3.7 | 3.2 | 5.1 |
| Eswatini | 9.1 | 7.7 | 5.7 | 9.1 | 11.5 | 10.2 | 7 | 4.3 | 10.4 | 10.8 | 5 | 7.1 | 8.2 |
| Ethiopia | 6.5 | 6.7 | 4.1 | 6.9 | 6.9 | 6.3 | 5.3 | 4.4 | 5.3 | 7.2 | 8.1 | 7.9 | 4.1 |
| Gabon | 8.5 | 7.7 | 8.1 | 8.1 | 1.4 | 7 | 8.7 | 12.5 | 8.6 | 7.2 | 8.6 | 6.9 | 9.5 |
| Gambia | 5.2 | 3.9 | 4.3 | 5.1 | 4.5 | 3.5 | 5.3 | 3.5 | 4.4 | 4.2 | 4.8 | 4.3 | 5.2 |
| Ghana | 3.4 | 3.7 | 2.5 | 4.4 | 3.5 | 4 | 3.6 | 1.2 | 2.6 | 5 | 5.3 | 2.5 | 2.3 |
| Guinea | 2.2 | 2 | 1.9 | 2.2 | 2.1 | 2.3 | 2.3 | 0.5 | 1.9 | 2.4 | 2.5 | 1.9 | 1.9 |
| Kenya | 8.7 | 8.2 | 7.3 | 9.1 | 6.2 | 9.4 | 8 | 6.5 | 8.7 | 9.5 | 9.7 | 8.3 | 6.1 |
| Lesotho | 4.6 | 4.7 | 3.7 | 5 | 10.7 | 5.3 | 3.9 | 4.1 | 4.7 | 5.2 | 4.3 | 5 | 4 |
| Liberia | 4.1 | 4.7 | 3.8 | 5.1 | 4.2 | 4.3 | 4.2 | 8.9 | 5.3 | 3.8 | 3.7 | 4.3 | 5 |
| Madagascar | 3.1 | 2.7 | 4 | 2.7 | 2.9 | 2.8 | 3 | 2.7 | 2.8 | 3.2 | 2.3 | 2.9 | 3.3 |
| Malawi | 5.7 | 5.1 | 3.6 | 5.7 | 4.6 | 5.7 | 5.3 | 1.2 | 5.9 | 4.9 | 6.2 | 5.8 | 4 |
| Malawi | 7.1 | 6.5 | 6.6 | 6.8 | 5.9 | 7.1 | 6.4 | 5.4 | 6.6 | 6.5 | 7.4 | 7 | 6.4 |
| Mali | 2.1 | 1.9 | 1.2 | 2.2 | 2.2 | 1.1 | 1.7 | 1.6 | 2.9 | 2.2 | 1.3 | 1.9 | 1.6 |
| Mauritania | 4.1 | 4 | 3.3 | 4.6 | 3.8 | 4.3 | 4.1 | 3.5 | 4.4 | 4.5 | 4.5 | 3.6 | 2.8 |
| Mozambique | 5 | 5.4 | 4.9 | 5.3 | 5.4 | 5.2 | 5 | 1 | 6.1 | 3.3 | 5.4 | 6.1 | 5.2 |
| Namibia | 6.6 | 4.9 | 5.4 | 6.1 | 4.6 | 6.6 | 5.6 | 5.6 | 6.6 | 6.2 | 5.7 | 4.5 | 5.7 |
| Niger | 4.3 | 4.4 | 4.7 | 4.3 | 4.2 | 4.8 | 5.5 | 7.6 | 4.1 | 5.1 | 4 | 4.5 | 4.1 |
| Nigeria | 2.7 | 2.6 | 2 | 3.1 | 3.1 | 3.3 | 2 | 1 | 4.2 | 3 | 2.3 | 1.9 | 1.4 |
| Rwanda | 1.8 | 1.6 | 1 | 1.9 | 2.1 | 1.9 | 1 | 0.9 | 2.1 | 2.5 | 1.9 | 0.9 | 1 |
| Sao Tome and Principe | 9.6 | 8.5 | 5 | 12.7 | 3.3 | 10.4 | 6.1 | 12.4 | 8.3 | 6.7 | 10.6 | 7 | |
| Senegal | 5.4 | 4.5 | 5.7 | 4.5 | 4.6 | 5.6 | 4.4 | 12.4 | 4.1 | 5 | 4 | 5.7 | 6.3 |
| Sierra Leone | 2.2 | 1.9 | 2.2 | 1.9 | 1.6 | 2.9 | 2.5 | 1.8 | 2.2 | 1.6 | 1.8 | 3.2 | 1.6 |
| South Africa | 3.6 | 2.6 | 3.3 | 2.7 | 1.4 | 2 | 3.2 | 3.8 | 2.9 | 2.5 | 2.4 | 5 | 3 |
| Tanzania | 3.8 | 3.7 | 5.1 | 3.3 | 3.7 | 3.6 | 4.8 | 0.4 | 2.9 | 3.1 | 3.4 | 4.8 | 5.1 |
| Togo | 3.6 | 3.3 | 2.9 | 3.7 | 4 | 3.1 | 3.2 | 1.2 | 4.6 | 3 | 3.4 | 3.3 | 2.8 |
| Uganda | 9.7 | 9 | 7.1 | 10 | 11.8 | 9.6 | 8.4 | 5.8 | 12.7 | 10.5 | 9 | 8.3 | 5.5 |
| Zambia | 1.6 | 1.8 | 1.2 | 2 | 2.1 | 1.6 | 1.8 | 1.2 | 2.4 | 1.9 | 1.2 | 1.4 | 1.2 |
| Zimbabwe | 4.3 | 3.4 | 2.8 | 4.2 | 11.7 | 3.9 | 3.8 | 1.2 | 4 | 5.2 | 3.7 | 2.9 | 3.3 |
Figure 2 shows the prevalence of acute respiratory infection for whom advice or treatment was sought among under-five children. South Africa (88.0%), Tanzania (85.0%), Guinea (83.0%), Uganda (80.0%), Sao Tome and Principe (79.0%), Liberia, Eswatini and Malawi (78.0%), Zambia (76.0%), Nigeria and Ghana (75.0%), Kenya, Namibia and Rwanda (73.0%), Lesotho (72.0%), Mali and Congo (71.0%), Gambia (70.0%) have the leading prevalence of acute respiratory infection for whom advice or treatment was sought among under-five children.
Figure 2.
Prevalence of acute respiratory infection among under-5 children for whom advice/treatment was sought.
Table 3 shows the distribution of under 5 children with acute respiratory infection for whom advice or treatment was sought from a health facility or provider. Countries such as Angola, Burundi, Chad, Comoros, Congo DR, Ethiopia, Gabon, Gambia, Kenya, Liberia, Malawi, Mauritania, Mozambique, Senegal, and Zambia, have higher distribution of male under-five children with ARI for whom treatment was sought, compared to other studied countries who either have no difference among male and female under-five children with ARI, or have more females than males. Most urban residents, highest education levels and highest household wealth quintiles among most of the studied countries were observed to have sought for treatment for their under-five children’s ARI.
Table 3.
Distribution of Under 5 Children With Acute Respiratory Infection for Whom Advice or Treatment was Sought From a Health Facility or Provider.
| Country | Sex | Residence | Mother’s education | Household wealth quintiles | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Urban | Rural | No education | Primary | Secondary | Higher | Lowest | Second | Middle | Fourth | Highest | |
| Angola | 52.2 | 47.4 | 60.7 | 33.3 | 45.2 | 40 | 72.5 | 25.6 | 48.2 | 46.8 | 67.8 | 77.9 | |
| Benin | 45.8 | 46.5 | 59.7 | 39.8 | 42 | 50.3 | 61.2 | 30.2 | 49.2 | 41.9 | 53.7 | 73.8 | |
| Burkina Faso | 59 | 71.2 | 81.7 | 58.1 | 60.1 | 75.4 | 48.9 | 51.6 | 67.6 | 59.6 | 85.3 | ||
| Burundi | 65.5 | 59 | 67.7 | 62.1 | 63.4 | 60.7 | 65.4 | 61.5 | 59.2 | 56.4 | 71.5 | 67.3 | |
| Cameroon | 55.7 | 62.4 | 72.2 | 45.6 | 52.5 | 58.5 | 48.6 | 54.7 | |||||
| Chad | 46.3 | 43 | 55.6 | 41.9 | 36.9 | 49.7 | 70.4 | 31.9 | 43.8 | 39.1 | 50.5 | 65.2 | |
| Comoros | 49.2 | 41 | 50.6 | 42.9 | 52.1 | 39.4 | |||||||
| Congo | 70.6 | 72.1 | 70 | 73.7 | 47.8 | 66.9 | 73.8 | 70 | 67.2 | 59.5 | 72.2 | 89.8 | |
| Congo Democratic Republic | 58 | 51.9 | 59.8 | 53.2 | 44.2 | 52.3 | 65.4 | 45.6 | 51 | 60.6 | 55 | 69.5 | |
| Cote d’Ivoire | 60.9 | 58.4 | 68.6 | 53.7 | 58.2 | 57 | 69.8 | 47.5 | 53.2 | 54.5 | 74.8 | 70.9 | |
| Eswatini | 74.7 | 81.2 | 81.6 | 76.9 | 58.1 | 78.7 | 83.7 | 66.1 | 75.8 | 84.7 | 90.4 | 80.4 | |
| Ethiopia | 34.1 | 29.1 | 64.4 | 29.2 | 26.7 | 40.7 | 25 | 27 | 28.9 | 41 | 44.2 | ||
| Gabon | 73.4 | 63.8 | 71.2 | 56.8 | 60.6 | 72 | 52 | 78.7 | 67 | 84 | 68.3 | ||
| Gambia | 72.8 | 66.7 | 71.3 | 68.7 | 67.9 | 60.5 | 74.5 | 66.8 | 75.7 | 73.7 | 57.1 | 77.2 | |
| Ghana | 73.3 | 75.9 | 84.5 | 69.8 | 71.9 | 81.8 | 72 | 72.3 | 69.1 | 83.5 | |||
| Guinea | 82.9 | 83.5 | 96.6 | 78.3 | 84.2 | 74 | 72.9 | 87.5 | 89.1 | ||||
| Kenya | 74.4 | 71.7 | 70.1 | 74.4 | 65.9 | 73.2 | 75.1 | 74.5 | 69.4 | 77.5 | 72.7 | 69.3 | 77.3 |
| Lesotho | 68.2 | 75.4 | 70.5 | 70.2 | 76 | 68 | 72.8 | 75.3 | |||||
| Liberia | 81.4 | 75.8 | 76.3 | 80.3 | 70.6 | 87.5 | 74.5 | 70.7 | 84.3 | 71.6 | 74.6 | ||
| Madagascar | 48.4 | 48.2 | 60.9 | 46 | 39.5 | 43.7 | 71.1 | 42.5 | 36.4 | 48.5 | 53.7 | 69.3 | |
| Malawi | 76.7 | 79 | 83.5 | 77.3 | 76.2 | 78.5 | 76.5 | 77.8 | 77.3 | 77.1 | 79.1 | 78.2 | |
| Malawi | 77.2 | 74 | 67.6 | 76.9 | 74.1 | 75.3 | 79 | 69.9 | 73.5 | 80.3 | 77.7 | 76.9 | |
| Mali | 71.4 | 70.3 | 88.7 | 68.4 | 68.1 | 74.3 | 58.3 | 60.3 | 77.9 | 85.7 | |||
| Mauritania | 50 | 42.7 | 54.5 | 42.5 | 40.3 | 45.5 | 60.5 | 27.6 | 44.5 | 56.3 | 59.8 | 58.1 | |
| Mozambique | 62.7 | 58.4 | 68.5 | 57.8 | 50.8 | 61.5 | 75.3 | 52 | 61.9 | 54.8 | 72.3 | 65.1 | |
| Namibia | 74.4 | 71.5 | 83.1 | 64.6 | 58.4 | 79.1 | 57.7 | 75.2 | 79.2 | 74.6 | 85.3 | ||
| Niger | 66.2 | 63.2 | 80.8 | 62 | 61 | 88.4 | 74.2 | 56.1 | 59.1 | 64 | 66.4 | 80.5 | |
| Nigeria | 74.8 | 74.2 | 82.3 | 71.3 | 71.2 | 70.9 | 82.1 | 93.6 | 71.5 | 69.4 | 74 | 79.9 | 93.8 |
| Rwanda | 66.7 | 79.7 | 71.1 | 69 | 66.8 | 63.8 | |||||||
| Sao Tome and Principe | 74.7 | 84.8 | 80.5 | 79 | 78.4 | 86.2 | 60.6 | 80.4 | |||||
| Senegal | 59.1 | 49.1 | 59.4 | 50.8 | 50 | 44.3 | 75.8 | 54.3 | 36.4 | 43.5 | 72.9 | 61.5 | |
| Sierra Leone | 84.5 | 87.1 | 84.6 | 86.4 | 77.5 | 91.8 | 92.2 | 83.8 | 82.6 | 90.7 | 84.1 | ||
| South Africa | 87.2 | 88.3 | 87.6 | 87.7 | 90.6 | 81.2 | |||||||
| Tanzania | 85 | 84.1 | 81.9 | 86.1 | 79.3 | 86.5 | 84.6 | 76.8 | 85.1 | 84.4 | 85.1 | 90.1 | |
| Togo | 65.3 | 71.9 | 79.1 | 63.7 | 62.8 | 65.8 | 85.2 | 57.7 | 71.6 | 64.4 | 80.4 | 75.2 | |
| Uganda | 79.9 | 81 | 82.6 | 80 | 79.9 | 78.3 | 85.1 | 92 | 79.7 | 77.6 | 78.2 | 84.5 | 85.8 |
| Zambia | 81.1 | 71.6 | 88.9 | 71.9 | 64.4 | 87.7 | 69.4 | 79.7 | 59.7 | ||||
| Zimbabwe | 50.6 | 62.1 | 72.6 | 50.6 | 42.7 | 60.6 | 52.3 | 46.9 | 57.1 | 58 | 73.4 | ||
Figure 3 shows the prevalence of ARI who received antibiotics among children who were less than 5 years. Tanzania (61.0%), Sao Tome and Principe (60.0%), Rwanda and Congo (58.0%), Angola (56.0%), Mozambique (54.0%), Kenya (53.0%), Namibia (52.0%) and Gabon (50.0%) have higher prevalence of ARI who received antibiotics among children who are under-5 years of age respectively.
Figure 3.
Prevalence of acute respiratory infection among under-5 children who received antibiotics.
Table 4 shows the distribution of children under the age of 5 with symptoms of acute respiratory infection who received antibiotics. We observed that generally, under-five children with ARI who are from urban resident households, mothers with higher levels of education and households with highest household wealth quintiles, in almost all the studied countries, received antibiotics.
Table 4.
Distribution of Under 5 Children With Symptoms of Acute Respiratory Infection Who Received Antibiotics.
| Country | Sex | Residence | Mother’s education | Household wealth quintiles | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Urban | Rural | No education | Primary | Secondary | Higher | Lowest | Second | Middle | Fourth | Highest | |
| Angola | 53 | 58.3 | 61 | 46.8 | 47.9 | 54.5 | 64.7 | 41.9 | 52.2 | 53.6 | 77.5 | 60 | |
| Benin | 18.7 | 22.3 | 26.9 | 17.4 | 18.4 | 25.2 | 22.9 | 11.6 | 18.5 | 25.3 | 22.3 | 34 | |
| Burkina Faso | 44.8 | 49.3 | 60 | 42 | 44.5 | 58 | 37 | 36.9 | 44.8 | 43.1 | 64.9 | ||
| Burundi | 27.1 | 23.6 | 27.1 | 25.4 | 22.2 | 29.2 | 24.5 | 21.7 | 24.6 | 22 | 30.3 | 33.8 | |
| Cameroon | 36.8 | 26 | 27.2 | 35.2 | 32.2 | 31.3 | 34.1 | 45.5 | |||||
| Chad | 31 | 29.1 | 47 | 25.8 | 25.1 | 32.3 | 47.7 | 20.3 | 24.3 | 30.1 | 34.5 | 46.5 | |
| Comoros | 13.3 | 29.4 | 32.2 | 15.7 | 20.4 | 10.2 | |||||||
| Congo | 62.1 | 55.5 | 48.8 | 73.5 | 68.5 | 62.7 | 56.3 | 71.5 | 65.7 | 63.4 | 34.3 | 49.2 | |
| Congo Democratic Republic | 40.5 | 38.7 | 50.8 | 35.3 | 19.9 | 43.3 | 47.5 | 31.2 | 39 | 34.6 | 48.8 | 51.2 | |
| Cote d’Ivoire | 31.3 | 26.8 | 44.2 | 18.9 | 27.3 | 29.7 | 33.1 | 18.9 | 16.6 | 24.3 | 46.7 | 41.5 | |
| Eswatini | 4.4 | 8.6 | 0 | 7.4 | 17.1 | 2.2 | 6.1 | 3.9 | 9.1 | 3.7 | 8.7 | 5 | |
| Ethiopia | 21.6 | 19.6 | 53.2 | 18.2 | 16 | 29.4 | 15.3 | 19.3 | 18.8 | 25.3 | 29.9 | ||
| Gabon | 55.3 | 44.6 | 51.6 | 43.7 | 38.4 | 55.6 | 40.6 | 47.8 | 54.8 | 52 | 58.1 | ||
| Gambia | 53 | 41.6 | 47.1 | 50.3 | 44.6 | 49.2 | 50 | 43 | 56.6 | 50.6 | 37 | 53.5 | |
| Ghana | 41.2 | 41.6 | 48.3 | 38.1 | 33.6 | 34.3 | 49.3 | 32.1 | 32.3 | 51.8 | |||
| Guinea | 44.3 | 53.1 | 53.9 | 46.4 | 52.1 | 54.3 | 41.5 | 49.8 | 47.5 | ||||
| Kenya | 54.1 | 51.9 | 50 | 54.4 | 45.2 | 51.2 | 57.8 | 64.9 | 47.9 | 49.3 | 51.7 | 61.6 | 59.3 |
| Lesotho | 10.3 | 20.8 | 19.9 | 10.8 | 22.9 | 15.4 | 17.8 | 18.4 | |||||
| Liberia | 38.7 | 52.6 | 48 | 44.6 | 34.8 | 56 | 47 | 42.9 | 46.7 | 40.3 | 44 | ||
| Madagascar | 52.9 | 42.6 | 61.4 | 45.8 | 32.3 | 47.6 | 68.1 | 37.5 | 42.7 | 53.6 | 50.1 | 65.2 | |
| Malawi | 40.4 | 43.4 | 50.2 | 41 | 38.3 | 40.5 | 48.3 | 42.9 | 34.7 | 44 | 42.8 | 46.1 | |
| Malawi | 41.8 | 39.7 | 55.5 | 38.5 | 33.4 | 40.3 | 51.2 | 36 | 39.3 | 39.3 | 45.9 | 45.5 | |
| Mali | 23.3 | 24.6 | 42.4 | 21.3 | 23.8 | 25.3 | 19.9 | 7.4 | 39.6 | 23.5 | |||
| Mauritania | 10.4 | 7.3 | 10.3 | 8.2 | 7.2 | 10.7 | 7.9 | 6 | 7.9 | 13.6 | 6.4 | 12.5 | |
| Mozambique | 52.9 | 54.3 | 61.3 | 51.2 | 46.4 | 54.4 | 64.9 | 45.7 | 44.5 | 49 | 67.5 | 63.4 | |
| Namibia | 57.5 | 46.2 | 56.5 | 49.1 | 31.3 | 60.9 | 27.8 | 53.4 | 58.2 | 66 | 69.8 | ||
| Niger | 7.5 | 8.7 | 30.3 | 4.3 | 7.4 | 5.6 | 18.3 | 4.6 | 5 | 1.7 | 5 | 27.4 | |
| Nigeria | 25.4 | 26.9 | 27.9 | 25.4 | 25.7 | 24.6 | 26.7 | 36.9 | 27.5 | 24 | 27.1 | 19.6 | 34.9 |
| Rwanda | 55.3 | 62.3 | 58.6 | 53.1 | 45.7 | 55.6 | |||||||
| Sao Tome and Principe | 68.4 | 51 | 50.6 | 63.8 | 58.7 | 72 | 18.5 | 57.9 | |||||
| Senegal | 27.1 | 19.4 | 16.8 | 28.4 | 22.3 | 34.4 | 21.9 | 23 | 19.5 | 29.9 | 27.7 | 19.4 | |
| Sierra Leone | 37.1 | 46.6 | 47.7 | 37.4 | 35.5 | 28 | 55 | 22.6 | 46.3 | 31.3 | 55.1 | ||
| South Africa | 42.8 | 40.8 | 39 | 48.4 | 41.2 | 52.7 | |||||||
| Tanzania | 57.2 | 65.1 | 63.7 | 59.6 | 47.9 | 68.4 | 50.8 | 53.8 | 47.4 | 66.2 | 70.5 | 63.8 | |
| Togo | 34.6 | 43.6 | 48.9 | 34.5 | 32.2 | 40.7 | 53 | 27.8 | 46 | 36.8 | 43 | 49.1 | |
| Uganda | 43.7 | 42.2 | 47.5 | 42.1 | 31.6 | 41.8 | 51.7 | 57.5 | 34.7 | 41.6 | 44.9 | 44.7 | 62.3 |
| Zambia | 47.5 | 42.3 | 43 | 45.3 | 49.9 | 36.3 | 48.3 | 45.1 | 52.2 | ||||
| Zimbabwe | 33.7 | 47.8 | 50.6 | 36.8 | 24.5 | 45.7 | 34.8 | 37.6 | 37.1 | 31.9 | 65.9 | ||
Discussion
This study utilized the most current nationally representative data models of children under the age of 5 from 39 African nations. The study sought to examine the prevalence and distributions of Acute Respiratory Infections (ARIs) among children who are under the age of 5 children in countries within the sub-Saharan. The total prevalence of acute lower respiratory infections (ARIs) for all the countries was 5%. Individual nations with the uppermost prevalence were Burundi, Congo Democratic Republic and Ethiopia (7%) apiece, Chad and Gabon (8.0%), and Kenya, Sao Tome and Principe and Uganda had 9% each. Cameroon had the lowest prevalence of ARIs (1%). On the sub-regional levels, Central and Southern sub-Saharan countries have the highest prevalence (5%) while Western sub-Saharan sub-region has the lowest (3%) of ARIs among children of 5 years and below. The overall prevalence recorded in this study is lower than the reports from some other parts of the globe,7,22 but a confirmation of the observation by UNICEF that the majority of ARI instances or conditions and mortalities as documented from some of the infected children, are in from the sub-Saharan countries.23,24 Aside Cameroon which has 1% prevalence of ARI among the under-5 children, other studied countries had higher prevalence of the ARI but not as high as have been reported by studies in Nigeria,25 Ethiopia18 and another that comprised some African countries7 as well as from a Nepalese26 and an Indian studies.27 The discoveries could be explained by inadequate wealth-related and education status of mothers, insufficient supply of water, the prevalence of communicable diseases, and poor nutrition knowledge, that are more predominant in many Sub-Saharan countries when compared to their developed counterparts.
The prevalence of ARI among under-five whom advice/treatment was sought for was higher among Uganda 80%, Guinea 83%, Tanzanian 85%, Sierra Leone 86% and South Africa 88%.
The increasing percentage of ARI in the nations of Sub-Saharan African region could also be thought to be due to the regions’ frequent outbreaks of epidemic diseases.28 The World Health Organization (WHO)29-31 posited that nutritional supplementations is critical for the effective and proper operational activity of the immune system as well as the healthy developmental milestones of children. These reports also argue that providing nutritional supplements every 4 to 6 months is indeed an effective, quick, and low-cost strategy for improving under-five’s immune status and lowering childhood mortality and morbidity rates.32 It is not surprising, then, that in our study, children whom treatment or advice were not sought for had higher proportions of ARI than those who did.
The wealth index of the household, maternal education, and area of residence have been discovered to be positively connected with ARI manifestations in this study. It was found in our study that children who were living in urban areas in most of the studied countries had a higher odd of contracting and developing ARI symptoms in comparison with those in the rural areas of the countries. Though this is not consistent in all the countries as states such as Cameroon, Congo, Rwanda, Sao Tome and Principe, and Senegal witnessed a higher prevalence of ARI symptoms in their rural settings in comparison to the urban residents. The findings are in consistency with other research conducted previously in other regions across the world. For instance, an Indian and Ethiopian studies show that children from rural areas are often diagnosed of ARI than those in the urban cities.32,33
This study found an unequal distribution of prevalence of ARIs in males and females among different countries. Studies from different countries however, have found that either boys or girls have a higher prevalence of ARIs than the other.11,34,35 Some other studies have reported that being male or boy, having mothers with little or no education are risk factors for developing ARIs in under-5 children.36-39 Children from low-income families had the highest prevalence of ARI, while those from wealthy families had the lowest. This finding highlights the importance of wealth position of households as one of the major determinants of people’s utilization of health care services and its outcomes among the population, predominantly children. While the households with higher economic power in most nations of Sub-Saharan Africa can habitually afford to pay for healthcare out of pocket, the opposite is true for those in the poorest wealth quintiles, who can barely have enough money to eat, let alone pay for health care, particularly for the prevention of ARIs in children who are below the age of.40 Again, those who have high wealth profile are more prospective to be able to afford rudimentary necessities such as healthcare for themselves and their children. This could act as a protective factor in lowering the manifestation of ARI among children under the age of 5.7
Despite the fact that many of the sub-regional countries’ social health interventions are majorly for the poor and intended to connect the gap linking access to and utilization of health care commodities, including immunization of children.41-43 Research evidence have shown that rich people in the society tend to profit more from such intervention strategies at the expense of the poor people of the society who may actually be the targeted population for the interventions.44 Globally, inadequate living conditions pose a high-risk factor for negative health condition and are linked to insufficient use of primary health care.45 In some countries, several measures have been implemented to overwhelmed blockades to proper housing situations,46,47 including affordable housing programs and steps to increase system quality among some of the underprivileged through a health insurance scheme that is nationally based48 and community-based crisis intervention of illnesses that are prominent among children who are less than 5 years old. The findings of this study on the role of living conditions, which are determined by factors such as household wealth quintiles, place of residence, the level of education, in the advancement of ARIs among Sub-Saharan African children obviously reinforce the fact that the living standards of households, particularly sanitation, are critical in influencing the transmission of contaminations in children under the age of 5.37,49
Strengths and Limitation
Estimates for the prevalence of ARI across African children have been provided in this research. In order to make reasonable comparisons, we investigated large datasets that were nationally representative. Having the option to combine resources from multiple nations is a huge perk. This research could be used as a benchmark to compare countries’ healthcare systems. This has the potential to spur joint efforts, new policies and programs, and a call to action to combat hunger and poverty more broadly by bolstering existing initiatives. However, we collected data from multiple nations and time periods using a cross-sectional survey. Logical links might be drawn between the study’s characteristics and external factors that affect the countries’ socioeconomic situations. The political climate, the advancement of health care infrastructure, and the health policies of governments are just a few of the variables that could affect how accurately any country’s economy is captured at a particular point in time. Due to this, the prevalence of acute respiratory infection may have changed over time. This could result to possible sample bias. Furthermore, DHS does not record information on income or expenditure, 2 usual measures of wealth. Wealth index employed in this study is based on the value of a household’s assets, which is simply a representation of the economic standing of households, and its consequences are not necessarily analogous to those produced from direct capacities of revenue and disbursement.
Conclusion
Our findings on the contribution of living conditions to the progression of ARIs in Sub-Saharan African children, which are determined by factors such as the wealth quintiles of households, their places of residence, and level of education, clearly reinforce the importance of household living standards, particularly sanitation, in determining infection transmission among children under the age of 5. It was clearly observed that place of residence, levels of education and household wealth or financial status influence whether a household who had an under-five with ARI would seek medical treatment for the child or not. It is therefore, imperative that intervention programs to reduce the causes of acute respiratory infections in children who are less than 5 years old, be channeled toward the most vulnerable groups, especially the rural and urban poor, and the less educated families.
Acknowledgments
The authors thank the DHS for the approval and access to the original data.
Footnotes
Authors’ Contributions: ME, CIN, OCO, AB, AIW & CKE conceptualized the study and prepared the study design, reviewed literature, conducted data analysis and wrote the results. All the authors critically reviewed the manuscript for its intellectual content. AB had final responsibility to submit for publication.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Availability of Data and Materials: Data for this study were sourced and available here http://dhsprogram.com/data/available-datasets.cfm.
Ethics Approval and Consent to Participate: All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from participants (signed or thumb-printed).
Consent for Publication: Not applicable.
ORCID iDs: Michael Ekholuenetale  https://orcid.org/0000-0002-2372-3020
https://orcid.org/0000-0002-2372-3020
Chimezie Igwegbe Nzoputam  https://orcid.org/0000-0002-7552-9545
https://orcid.org/0000-0002-7552-9545
Amadou Barrow  https://orcid.org/0000-0002-6006-9355
https://orcid.org/0000-0002-6006-9355
Clement Kevin Edet  https://orcid.org/0000-0002-5979-8841
https://orcid.org/0000-0002-5979-8841
References
- 1. Children: improving survival and well-being. Accessed June, 16 2022. https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality
- 2. Mir F, Ariff S, Bhura M, et al. Risk factors for acute respiratory infections in children between 0 and 23 months of age in a peri-urban district in Pakistan: a matched case–control study. Front Pediatr. 2022;9:1-6. doi: 10.3389/fped.2021.704545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tazinya AA, Halle-Ekane GE, Mbuagbaw LT, Abanda M, Atashili J, Obama MT. Risk factors for acute respiratory infections in children under five years attending the Bamenda Regional Hospital in Cameroon. BMC Pulm Med. 2018;18:7. doi: 10.1186/s12890-018-0579-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Troeger C, Forouzanfar M, Rao PC, Khalil I, Brown A, Swartz S, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. 2017;17:1133-1161. doi: 10.1016/S1473-3099(17)30396-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nair H, Simões EA, Rudan I, et al. Global and regional burden of hospital admissions for severe acute lower respiratory infections in young children in 2010: a systematic analysis. Lancet. 2013;381:1380-1390. doi: 10.1016/S0140-6736(12)61901-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392:1736-1788. doi: 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Seidu A-A, Dickson KS, Ahinkorah BO, Amu H, Darteh EKM, Kumi-Kyereme A. Prevalence and determinants of acute lower respiratory infections among children under-five years in sub-Saharan Africa: evidence from demographic and health surveys. SSM - Popul Health. 2019;8:100443. doi: 10.1016/j.ssmph.2019.100443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Simen-Kapeu A, Bogler L, Weber A-C, et al. Prevalence of diarrhoea, acute respiratory infections, and malaria over time (1995-2017): a regional analysis of 23 countries in west and Central Africa. J Glob Health. 2021;11:13008. doi: 10.7189/jogh.11.13008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ekholuenetale M, Tudeme G, Onikan A, Ekholuenetale CE. Socioeconomic inequalities in hidden hunger, undernutrition, and overweight among under-five children in 35 sub-Saharan Africa countries. J Egypt Public Health Assoc. 2020;95:9. doi: 10.1186/s42506-019-0034-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ekholuenetale M, Okonji OC, Nzoputam CI, Barrow A. Inequalities in the prevalence of stunting, anemia and exclusive breastfeeding among African children. BMC Pediatr. 2022;22:333. doi: 10.1186/s12887-022-03395-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Akinyemi JO, Morakinyo OM. Household environment and symptoms of childhood acute respiratory tract infections in Nigeria, 2003-2013: a decade of progress and stagnation. BMC Infect Dis. 2018;18:296. doi: 10.1186/s12879-018-3207-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barrow A, Ayobami A, Chidozie Azubuike P, Cham D. Prevalence and determinants of acute respiratory infections among children under five years in rural settings of the Gambia: evidence from a national survey. Glob J Epidemiol Infect Dis. 2022;2:23-32. [Google Scholar]
- 13. Dagne H, Andualem Z, Dagnew B, Taddese AA. Acute respiratory infection and its associated factors among children under-five years attending pediatrics ward at University of Gondar Comprehensive Specialized Hospital, Northwest Ethiopia: institution-based cross-sectional study. BMC Pediatr. 2020;20:93. doi: 10.1186/s12887-020-1997-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hasan MM, Saha KK, Yunus RM, Alam K. Prevalence of acute respiratory infections among children in India: regional inequalities and risk factors. Matern Child Health J. 2022;26:1594-1602. doi: 10.1007/s10995-022-03424-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bhat RY, Manjunath N. Correlates of acute lower respiratory tract infections in children under 5 years of age in India. Int J Tuberc Lung Dis. 2013;17:418-422. doi: 10.5588/ijtld.12.0117 [DOI] [PubMed] [Google Scholar]
- 16. Risk factors for hospital admission due to acute lower respiratory tract infection in Guarani indigenous children in southern Brazil: a population-based case-control study - Cardoso - 2013 - Tropical Medicine & International Health - Wiley Online Library. Accessed June, 17 2022. https://onlinelibrary.wiley.com/doi/full/10.1111/tmi.12081 [DOI] [PubMed]
- 17. Lutpiatina L, Sulistyorini L, Notobroto HB, Raya RP, Utama RD, Thuraidah A. Multilevel analysis of lifestyle and household environment for toddlers with symptoms of acute respiratory infection (ARI) in Indonesia in 2007, 2012, and 2017. Glob Pediatr Health. 2022;9:2333794X221078700. doi: 10.1177/2333794X221078700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andualem Z, Nigussie Azene Z, Dessie A, Dagne H, Dagnew B. Acute respiratory infections among under-five children from households using biomass fuel in Ethiopia: systematic review and meta-analysis. Multidiscip Respir Med. 2020;15:710. doi: 10.4081/mrm.2020.710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Child Mortality. In: UNICEF DATA. Accessed June, 18 2022. https://data.unicef.org/topic/child-survival/under-five-mortality/
- 20. Corsi DJ, Neuman M, Finlay JE, Subramanian SV. Demographic and health surveys: a profile. Int J Epidemiol. 2012;41:1602-1613. doi: 10.1093/ije/dys184 [DOI] [PubMed] [Google Scholar]
- 21. Rutstein SO, Staveteig S. Making the Demographic and Health Surveys Wealth Index Comparable. DHS Methodological Reports No. 9; 2014. Rockville, MD: ICF International. [Google Scholar]
- 22. Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2:25-32. doi: 10.1016/S1473-3099(01)00170-0 [DOI] [PubMed] [Google Scholar]
- 23. UNICEF, World Health Organization. Ending preventable child deaths from pneumonia and diarrhoea by 2025: the integrated global action plan for pneumonia and diarrhoea (GAPPD). 2013. Accessed June, 18 2022. https://apps.who.int/iris/handle/10665/79200
- 24. Woldeamanuel BT. Socioeconomic, demographic, and environmental determinants of under-5 mortality in Ethiopia: evidence from Ethiopian Demographic and Health Survey, 2016. Child Dev Res. 2019;2019:1-15. doi: 10.1155/2019/1073782 [DOI] [Google Scholar]
- 25. Fienemika AE. Prevalence of acute respiratory infections among children under-five years old in a hospital in Port Harcourt, Nigeria: a two year follow-up study. J Respir Med. 2018;2: 6. [Google Scholar]
- 26. Ghimire P, Gachhadar R, Piya N, Shrestha K, Shrestha K. Prevalence and factors associated with acute respiratory infection among under-five children in selected tertiary hospitals of Kathmandu Valley. PLoS One. 2022;17:e0265933. doi: 10.1371/journal.pone.0265933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Murarkar S, Gothankar J, Doke P, Dhumale G, Pore PD, Lalwani S, et al. Prevalence of the acute respiratory infections and associated factors in the rural areas and urban slum areas of Western Maharashtra, India: a community-based cross-sectional study. Front Public Health. 2021;9. doi: 10.3389/fpubh.2021.723807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ekaza E, Kadjo HA, Coulibaly D, et al. Investigation of an outbreak of acute respiratory disease in Côte D’Ivoire in April 2007. Afr J Infect Dis. 2014;8:36-39. [PMC free article] [PubMed] [Google Scholar]
- 29. Imdad A, Mayo-Wilson E, Herzer K, Bhutta ZA. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst Rev. 2017;3:CD008524. doi: 10.1002/14651858.CD008524.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vitamin A. Accessed October, 27 2022. https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization/integration/linking-with-other-health-interventions/vitamin-a
- 31. Imdad A, Mayo-Wilson E, Haykal MR, et al. Vitamin A supplementation for preventing morbidity and mortality in children from six months to five years of age. Cochrane Database Syst Rev. 2022;3:CD008524. doi: 10.1002/14651858.CD008524.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Selvaraj K, Chinnakali P, Majumdar A, Krishnan IS. Acute respiratory infections among under-5 children in India: A situational analysis. J Nat Sci Biol Med. 2014;5:15-20. doi: 10.4103/0976-9668.127275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Merera AM. Determinants of acute respiratory infection among under-five children in rural Ethiopia. BMC Infect Dis. 2021;21:1203. doi: 10.1186/s12879-021-06864-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ramani VK, Pattankar J, Puttahonnappa SK. Acute respiratory infections among under-five age group children at urban slums of Gulbarga City: a longitudinal study. J Clin Diagn Res. 2016;10:LC08-LC13. doi: 10.7860/JCDR/2016/15509.7779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Islam F, Sarma R, Debroy A, Kar S, Pal R. Profiling acute respiratory tract infections in children from Assam, India. J Glob Infect Dis. 2013;5:8-14. doi: 10.4103/0974-777X.107167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kundu S, Kundu S, Banna MHA, Ahinkorah BO, Seidu A-A, Okyere J. Prevalence of and factors associated with childhood diarrhoeal disease and acute respiratory infection in Bangladesh: an analysis of a nationwide cross-sectional survey. BMJ Open. 2022;12:e051744. doi: 10.1136/bmjopen-2021-051744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hasan MM, Richardson A. How sustainable household environment and knowledge of healthy practices relate to childhood morbidity in South Asia: analysis of survey data from Bangladesh, Nepal and Pakistan. BMJ Open. 2017;7:e015019. doi: 10.1136/bmjopen-2016-015019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Apanga PA, Kumbeni MT. Factors associated with diarrhoea and acute respiratory infection in children under-5 years old in Ghana: an analysis of a national cross-sectional survey. BMC Pediatr. 2021;21:78. doi: 10.1186/s12887-021-02546-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hossain MS, Tasnim S, Chowdhury MA, Chowdhury FF, Hossain D, Rahman MM. Under-five children’s acute respiratory infection dropped significantly in Bangladesh: an evidence from Bangladesh demographic and health survey, 1996-2018. Acta Paediatr. 2022;111:1981-1994. doi: 10.1111/apa.16447 [DOI] [PubMed] [Google Scholar]
- 40. Nicholas A, Edward N-A, Bernardin S. The effect of health expenditure on selected maternal and child health outcomes in Sub-Saharan Africa. Int J Soc Econ. 2016;43:1386-1399. [Google Scholar]
- 41. Biset Wagaw G, Tadesse AW, Ambaye GY. Willingness to join community based health insurance among households in South Wollo, Northeast Ethiopia: A community-based cross-sectional study. PLoS One. 2022;17:e0261642. doi: 10.1371/journal.pone.0261642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Garedew MG, Sinkie SO, Handalo DM, et al. Al. Willingness to join and Pay for community-based health insurance among rural households of selected districts of Jimma Zone, Southwest Ethiopia. Clin Outcomes Res. 2020;12:45-55. doi: 10.2147/CEOR.S227934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Haile M, Ololo S, Megersa B. Willingness to join community-based health insurance among rural households of Debub Bench District, Bench Maji Zone, Southwest Ethiopia. BMC Public Health. 2014;14:591. doi: 10.1186/1471-2458-14-591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hammer-Fomuki E, Okwen PM, Ranft U, Gardemann J, Schikowski T. Attitudes of health care professionals towards mutual health organizations: evidence from two regions in the Northwest Province of Cameroon. J Public Health. 2016;24:175-183. doi: 10.1007/s10389-016-0716-9 [DOI] [Google Scholar]
- 45. Astale T, Chenault M. Help-seeking behavior for children with acute respiratory infection in Ethiopia: results from 2011 Ethiopia Demographic and Health Survey. PLoS One. 2015;10:e0142553. doi: 10.1371/journal.pone.0142553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ameh SO, Osafo BT. Housing policies: the experiences and constraints of housing industry in Ghana. Adv Soc Sci Res J. 2020;7:416-434. doi: 10.14738/assrj.79.9026 [DOI] [Google Scholar]
- 47. Boamah NA. Housing Policy in Ghana: the feasible paths. Ghana J Dev Stud. 2014;11:1-18. doi: 10.4314/gjds.v11i1.1 [DOI] [Google Scholar]
- 48. Duku SKO, Nketiah-Amponsah E, Janssens W, Pradhan M. Perceptions of healthcare quality in Ghana: does health insurance status matter? PLoS One. 2018;13:e0190911. doi: 10.1371/journal.pone.0190911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Sultana S. Household environmental factors and childhood acute respiratory infection in Bangladesh: findings from National. J Health Res. 2017;31:S189-S194. [Google Scholar]