Abstract
Background
The coronavirus disease 2019 pandemic has led to an increase in remote consultations in health care. This study aimed to assess the acceptance of video consultation as an alternative to face-to-face in-office visits in general practice (GP) and to investigate its drivers and barriers.
Methods
A cross-sectional study was conducted in Germany during the coronavirus disease 2019 pandemic from December 2020 to April 2021. Participants were recruited among patients in 16 GP surgeries. Assessed were sociodemographic and medical data as well as information and communications technology related data. Acceptance of video consultation and its predictors were determined using a modified questionnaire based on a short version of the renowned unified theory of acceptance and use of technology model.
Results
In total, 371 participants were included in the data analysis. Acceptance of video consultation was moderate. A hierarchical regression revealed acceptance was significantly predicted by the PHQ-2, taking no regular medication, computer proficiency, knowledge about digital health care solutions, no prior use of video consultation, and the unified theory of acceptance and use of technology predictors performance expectancy, effort expectancy, and social influence. The extended unified theory of acceptance and use of technology model explained significantly more variance than the restricted unified theory of acceptance and use of technology model in acceptance of video consultation.
Conclusions
In this study computer proficiency, existing knowledge about digital health care solutions and depressive symptoms functioned as drivers to acceptance, no prior use of video consultation could be identified as a potential barrier. Patients with regular medication have been particularly receptive to video consultation. The study confirmed the validity of the unified theory of acceptance and use of technology model in determining acceptance of video consultation. Considering that there is growing demand and acceptance for different approaches to engage with health care providers, additional steps should be taken to establish video consultation as a genuine alternative.
Keywords: Telemedicine < general, remote consultation, general practice, videoconferencing, unified theory of acceptance and use of technology
Introduction
Health care systems around the world have faced major challenges since the first cases of severe acute respiratory syndrome coronavirus 2 occurred in December 2019 in China.1 The World Health Organization (WHO) declared the outbreak of coronavirus disease 2019 (COVID-19) a pandemic in March 2020.2 To this date (February 2022), more than 5.7 million deaths caused by COVID-19 have been confirmed.3 Non-pharmaceutical interventions have been proven to be one of the most important measures to prevent the spread of COVID-19.4 This has not only led to a temporal reduction of social interactions but also to a lower number of face-to-face in-office visits of patients in general practitioner (GP) surgeries. Consequently, an increase in care through nonphysical encounters, such as telemedicine, became visible.5,6
Telemedicine or telehealth (hereinafter referred to only as telemedicine) is defined by the WHO as ‘the delivery of health care services, where patients and providers are separated by distance. Telehealth uses information and communications technology (ICT) for the exchange of information for the diagnosis and treatment of diseases and injuries, research and evaluation, and for the continuing education of health professionals’ (WHO, 2010).7 An increasing number of patients with chronic diseases, a shortage of GPs especially in rural or deprived areas as well as a steadily aging population will generate a rising demand for different health care solutions in the future.8,10 Telemedicine is one possible solution for the existing shortcomings of the current health care system and can change the way patients engage with their health care providers.11 It can provide more adaptable methods for patients to interact with their doctor and include communication via e-mail, phone or video.12 With the constant growth of digitization in other fields calls for the adoption of large-scale telematic services in the entire health care system have become louder.13,14 Therefore, the German Federal Ministry of Health has passed the ‘e-Health Law’ in 2015 aiming for the implementation of ICT in healthcare and demanding the promotion of telemedical services.15
Especially video consultation (VC), as part of these technologies, has become of greater interest over the last years.16 It enables medical consultation between patient and physician using synchronous online video and audio transmission as an alternative to face-to-face in-office visits.17 Technical requirements are web-enabled devices, stable internet connection, and supporting software.18 The implementation of VC has been described in several medical disciplines such as family medicine, mental health care, palliative care, dermatology, urology, and others.19,23 Prior studies revealed that VC is cost-efficient, is able to increase primary care accessibility, reduces hospitalization rate and decreases travel expenses, and waiting time.24,27 It can also help to lower appointments failure-to-appear rates, absence of work, and can contribute to save resources.28,29 In selected situations that don't require physical examination, it can substitute or supplement in-office visits and provide comparable clinical outcome.25 Despite these advantages, potential difficulties could be patients’ privacy issues, reduced therapeutic potentials, technical problems, misdiagnosis, and unequal access to online communication devices.30,31
Although previous studies have examined patients’ view of different telemedical services extensively,17 there is little research into patients’ acceptance of applying standardized and validated research methods and no study examined patients’ acceptance of VC in general practice in Germany in particular. As it is likely that the use of VC in GP will play an increasingly important role in the future, it is essential to identify factors and predictors that influence patients’ acceptance of these technologies and to understand potential barriers that discourage patients from using VC.32
The most prominent model to predict users’ motivation to use technology is the unified theory of acceptance and use of technology model (UTAUT) by Venkatesh et al.33 The UTAUT combines key aspects of eight established research models.34 One of these models is the widely known and acclaimed technology acceptance model (TAM) by Davis et al.35 It claims a person's intention to use technology is dependent on two main determinants: Perceived ease of use and perceived usefulness.35 The UTAUT adopted these predictors as performance expectancy (perceived usefulness) and effort expectancy (perceived ease of use) and incorporated two additional factors from other models: social influence and facilitating conditions. The first three constructs directly predict acceptance, which is operationalized as behavioural intention. The actual utilization is influenced by facilitating conditions and behavioural intention. Venkatesh et al.36 postulate that the predictive validity of the UTAUT could be enhanced by including additional variables such as sociodemographic and health-related data. Furthermore, they stressed that future research should focus on identifying additional influencing factors and validate the model in various technologies and target groups. Thus, an extended model with sociodemographic data, medical data, and ICT-related data as additional predictors of acceptance was developed to further enhance generalizability of the UTAUT in the context of VC usage. Nevertheless, the UTAUT model has received some criticism. Van Raaij and Schepers considered the model‘s parsimony in comparison to the TAM model.37 Additionally, according to the authors heterogeneous items were grouped together to build the model‘s constructs. Thus, the use of several items per predictor has to be reconsidered to ensure that explained variance is not increased artificially.
Literature overview
The need for and feasibility of VC implementation
The need for new ways to interact with health care providers became apparent well before the COVID-19 pandemic.38,39 As early as 2000, a systematic review by Mair et al.40 demonstrated an increasing interest in the use of telemedicine. In 2010, Stahl and Dixon41 demonstrated both patients’ and clinicians’ willingness to use VC as an alternative to face-to-face consultation. In particular, patients who were younger and had proficient computer skills showed strong interest in VC in a study by Leng et al.42 Although Huygens et al.19 reached similar conclusions, they also showed that a group of patients were reluctant to use VC, mainly because they were unaware of its availability. This was also identified as a barrier in a study by Bradford et al..43 Several studies have examined the feasibility of telemedicine in different health care systems around the world.18,44,45 For example, Angrish et al. demonstrated, that patient–provider communication via VC is feasible in India,46 and Nord et al. found that the use of VC constitutes a cost-saving opportunity.24
Patient experiences, benefits and barriers associated with VC
Many studies have examined patients’ experiences with VC.18,47,48 A systematic scoping review by Thiyagarajan et al. in 2020 showed that patients described both positive and negative experiences with VC. Although VC appears to be more convenient for patients, it is not considered superior to face-to-face in-office visits.17 The existing literature revealed that timesaving and access to primary care in rural areas are the main advantages of VC,38,49,50 whereas technical issues, safety issues and the lack of physical examinations are the leading barriers.51,52
Predictors of VC acceptance
One key objective of this study is to explore predictors of acceptance using the UTAUT, a validated research method.53,54 Previous studies on predictors of telemedicine acceptance that applied the UTAUT mostly focused on the perceptions of the elderly.55,57 Cimperman et al. examined older users’ acceptance of home telehealth services by applying an extended UTAUT model with additional contextual constructs. Effort expectancy was identified as the leading acceptance predictor.55 Similar findings were obtained by Quaosar et al.56 in their empirical study of elderly individuals’ intention to use mobile health services. Here, likewise, performance expectancy, effort expectancy and social influence were determined to be potential predictors of acceptance. This was also confirmed in a study by de Veer et al.,57 in which older people‘s intention to use e-Health was examined. Again, those who believed that e-Health would help them (performance expectancy) or would be easy to use (effort expectancy) were more likely to use e-Health than those who did not.
Telemedicine during the COVID-19 pandemic
The COVID-19 pandemic has not only significantly affected how patients and health care providers communicate; it has also accelerated research on this topic.58 However, we found no studies that examined patients’ acceptance of VC during the pandemic. Instead, studies on telemedicine during this time focused mainly on two topics: the first was the increase in usage, and the second was patient and physician satisfaction. Gilson et al.6 demonstrated a 51.4% increase in virtual visits (both video and telephone) during the COVID-19 pandemic in 2020 compared to the preceding year at an urban medical centre in the United States. Overall, satisfaction with VC was high during the pandemic. A study by Barkai et al. showed that patients reported high levels of satisfaction, whereas clinicians were more sceptical due to technical and administrative barriers.59
Aim of this study
The research goal is to investigate participants’ acceptance of VC as an alternative to face-to-face in-office visits in GP practices in Germany and to assess differences in acceptance depending on sociodemographic and medical variables. Although people with chronic diseases pose a particular burden for health care systems, little research has been conducted to explore their attitudes towards VC usage. As patients with chronical illness could specifically benefit from using remote VC services, their acceptance of VC compared to non-chronically ill people is investigated in particular. In this study, it was also examined if the applied extended UTAUT model is suited to predict acceptance of VC and which underlying factors are potential positive as well as negative predictors. In order to analyse a parsimonious UTAUT model (following Van Raaij and Schepers37) and to focus on possible additional predictors based on sociodemographic, medical, and ICT-related data, a restricted version of the UTAUT model was used. In addition, the suggested applied extended model was compared to the restricted UTAUT model, in order to investigate if the applied extended model is superior in predicting acceptance.
The existing and constantly expanding body of knowledge has allowed us to gain insight into patients’ perceptions and satisfaction with VC. However, literature on VC acceptance using validated research methods, like the UTAUT, is scarce. Consequently, this impedes the comparability of these studies. Therefore, the purpose of this study is to address the current knowledge gap on patients’ acceptance and predictors by using the validated UTAUT model. In contrast to prior research, this study aims to assess acceptance in a heterogeneous patient collective, including different age groups, healthy persons, as well as patients with minor or major diseases. This approach enables conclusions on VC acceptance in the average population attending a GP. Exploring facilitators and barriers that affect the acceptance of VC enables the evidence-based implementation of potential enhancements that could contribute to support future VC usage. Especially in the context of the ongoing COVID-19 pandemic, this could accelerate the transformation of the way patients interact with their health care providers in the near future.
Methods
Design and study population
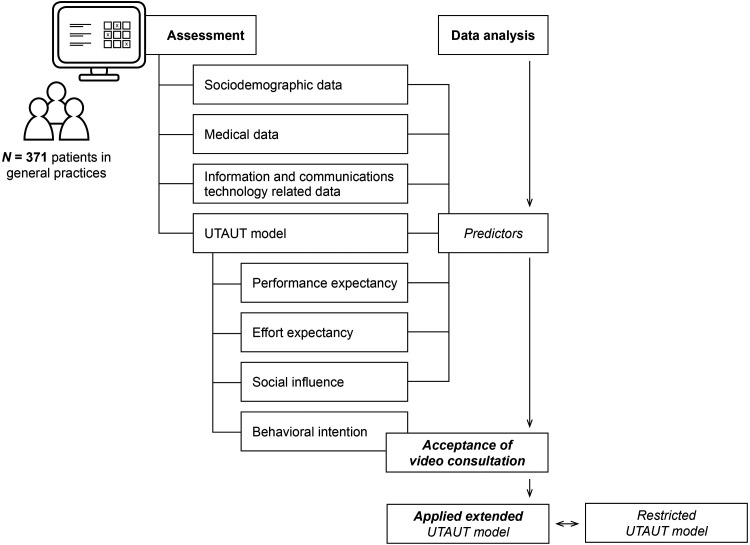
A cross-sectional study was conducted in order to assess patients’ acceptance of VC based on an online survey among patients in GP practices. Figure 1 shows the conceptual framework diagram of this study. The study was conducted in the region of North-Rhine-Westphalia, Germany. Participants were recruited among patients in 16 general practitioner practices. Initially 25 general practitioner practices were asked to support the recruitment process. No inclusion or exclusion criteria for the general practitioner practices were applied. In these practices, patients were invited to participate in the online survey via an informative flyer. Eligibility requirements were a good command of the German language, internet access, and an acute or chronic medical problem that led to the GP consultation. No further exclusion criteria were applied. Participants were also required to be aged 18 or above. Participation was voluntary, anonymous and no monetary compensation was offered. Electronic informed consent was obtained prior to the start of the questionnaire. The survey was available via the online platform Unipark (Questback GmbH) and the data collection took place from December 2020 to April 2021. Of 437 participants starting the survey, 89.47% completed it. To further improve data quality five percent of the respondents (n = 19) who completed the survey the quickest were excluded as this could be an indicator of careless or inattentive responding.60 In total, 371 participants were included in the final data analysis. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Medical Faculty of the University of Duisburg-Essen (19-89-47-BO).
Figure 1.
Conceptual framework diagram of this study.
Assessment instruments
The questionnaire was divided into three parts. In the first part, questions concerning sociodemographic aspects such as age, sex, marital status, educational level, occupational and insurance status and the population size of their place of residence were inquired. Participants were also asked for how long they have been with their GP, how often during the year they usually see their GP and if they received inpatient treatment in the last ten years. Afterwards questions about pre-existing medical conditions, mental disorder and medication were added. To assess participants’ anxiety and depression symptoms the Patient Health Questionnaire (PHQ-4)61 was applied, which is a short self-report questionnaire that includes the Patient Health Questionnaire-2 (PHQ-2) and the Generalized Anxiety Disorder-2 (GAD-2). The PHQ-2 contains two items screening for symptoms of depression over a period of two weeks on a four-point Likert scale (0 = ‘never‘ to 3 = ‘nearly every day’). A cutoff score of three or more is described to have the highest sensitivity and specificity for screening for depression.62 The GAD-2 screens for symptoms of generalized anxiety over a period of two weeks using two items on a four-point Likert-scale (0 = ‘never to’ 3 = ‘nearly every day’). A cutoff score of three or more is found to be an indicator for presence of generalized anxiety.63
In the second part of the survey self-generated questions referred to ICT usage (computer and mobile phone proficiency, internet usage behaviour, use of video telephony). Knowledge about digital health care solutions was assessed with three self-generated items. Cronbach‘s α of this scale was α = 0.85.‘ Participants were then asked if their GP already offers VC services and if they had previously used VC and, if not, if they were planning to do so in the future. The respondents were then asked if it would be important to know the GP personally before communicating via VC. It was also questioned if VC could also be used from other places than home (e.g., work place).
The third part of the questionnaire intended to understand participants’ acceptance to use VC with their GP by applying a restricted version of the UTAUT model. Three items were used to assess acceptance, which was operationalized as behavioural intention (‘I would like to try video consultation with my general practitioner’, ‘I would use video consultation with my general practitioner if offered to me’, ‘I would recommend video consultation to my friends’). Cronbach‘s α in this sample was α = .91. For each construct predicting acceptance one item was chosen. The item ‘Using video consultation with my general practitioner could improve my state of health‘ was used to assess performance expectancy, the item ‘Using video consultation with my general practitioner would be easy to learn‘ was used to measure effort expectancy and social influence was assessed via the item ‘Those close to me (e.g family, friends) would approve using video consultation’. Answers were given on a five-point Likert scale, ranging from 1 = ‘strongly disagree‘ to 5 = ‘strongly agree’.
Statistical analyses
For statistical analysis, raw data collected from the questionnaire were extracted and processed using SPSS 26 (IBM, New York) and the software R (version 4.0.3). Sum scores for PHQ-2 and GAD-2 were computed, as well as a mean score of three self-generated items regarding knowledge about digital health care solutions. The behavioural intention scale of the UTAUT model was calculated. Acceptance ( = behavioural intention) scores were divided into three parts: Scores between 1 and 2.34 indicated low acceptance, scores between 2.35 and 3.67 indicated moderate acceptance, and scores between 3.68 and 5 indicated high acceptance. Due to sufficiently large sample sizes, normality of the sampling distribution was presumed.64 For sociodemographic data, extent of general and mental health, as well as ICT variables descriptive statistics were performed. A tertial split was used to divide the sample into three age categories. Differences in acceptance between age groups, female and male participants, and between chronically ill and non-chronically ill participants were tested with analysis of variance (ANOVA) and independent t-tests. Levene's test was used to test for homoscedasticity. Multiple hierarchical regression was applied to analyse predictors of acceptance. Therefore, the following predictors were included blockwise: (a) sociodemographic data, (b) medical data, (c) ICT-related data, (d) UTAUT predictors (performance expectancy, effort expectancy, social influence). Breusch-Pagan tests were calculated to test for homoscedasticity and Durbin–Watson tests were used to eliminate autocorrelation. Normal distribution of residuals was assumed since visual inspection of qq-plots of residuals showed no signs of violations against normality. In a final step, the extended UTAUT model was tested against the restricted UTAUT model via an ANOVA. The level of significance was set to 0.05 for all tests.
Results
Sociodemographic and medical data
Of the 371 participants in this study, 51.5% (n = 191) were female. The mean age was M = 42.28 years (Mdn = 36, SD = 16.09). The youngest participant was 18 years old and the oldest was 85 years old. Most of the respondents were married or in a relationship (68.5%). In total, 97 (26.1%) participants stated being single at the time of the assessment. The substantial majority of the participants had a high standard of education, with 187 (50.4%) reporting that they graduated from college and 111 (29.9%) graduated from high school. Only 7 (1.9%) of the participants reported being currently unemployed. The remaining participants were either employed (66%), had retired (11.6%) or were still in education (14.8%). Most respondents (68.2%) were living in a city with a population size of over 100,000 residents.
In total, 255 (68.7%) of the participants suffered from a chronic condition, such as musculoskeletal disorders (36.7%, n = 136), cardiopulmonary diseases (34.5%, n = 128), ophthalmic diseases (15.9%, n = 59) or skin conditions (15.4%, n = 57). Taking the medication on a regular basis was reported by 39.1% (n = 145). The vast majority (88.4%, n = 328) stated that they had not received treatment due to a mental disorder in the last 10 years. Almost half of the participants (47.2%, n = 175) underwent inpatient treatment before. In total, 65.5% (n = 243) of the respondents consulted their GP on one or more occasions throughout the last year. Screening for generalized anxiety disorder with the GAD-2 (Msum = 1.01, SD = 1.14) revealed that 7.81% of the respondents reached the cutoff scores for generalized anxiety symptoms. Symptoms of major depression were present in 8.89% of the participants (PHQ-2, Msum = 1.10, SD = 1.16).
Around 80% (n = 293) of the participants felt confident in their skills regarding the use of the computer (n = 293) and mobile phone (n = 306) applications. Most participants stated using the internet for about three to four hours a day (M = 2.9, Mdn = 3, SD = 1.05). Only 79 (21.3%) of the respondents reported that they do not use video telephony in a private or work-related setting. In contrast, almost all participants (97%, n = 360) stated that they have never used VC with their GP before – even though 66.9% (n = 248) could imagine using VC with their GP in the future. 90.8% (n = 360) of the participants consider it important to know their GP personally prior to using VC. For a detailed overview see Table 1.
Table 1.
Sociodemographic, medical and ICT data.
| Variable | n | % | M (SD) |
|---|---|---|---|
| Age | 42.28 (16.09) | ||
| 18–30 | 123 | 33.2 | |
| 31–51 | 120 | 32.3 | |
| >51 | 128 | 34.5 | |
| Marital status | |||
| In a relationship/married | 56 | 15.1 | |
| Divorced/separated | 14 | 3.8 | |
| Widowed | 5 | 1.3 | |
| Others | 1 | 0.3 | |
| Educational level | |||
| University education | 187 | 50.4 | |
| Higher education entrance qualification | 111 | 29.9 | |
| Secondary education | 52 | 14.0 | |
| Lower secondary education | 18 | 4.9 | |
| No qualification | 3 | 0.8 | |
| Community size | |||
| 100,000 residents | 253 | 68.2 | |
| 20,000 residents | 80 | 21.6 | |
| 5000 residents | 27 | 7.3 | |
| <5000 residents | 11 | 3.0 | |
| Insurance status | |||
| Statutory health insurance | 291 | 78.4 | |
| Private health insurance | 73 | 19.7 | |
| Other | 7 | 1.9 | |
| Same GP for more than 5 years | 200 | 53.9 | |
| Number of visits per year | |||
| None | 128 | 34.5 | |
| 1–2 | 151 | 40.7 | |
| 3–5 | 65 | 17.5 | |
| 6–10 | 16 | 4.3 | |
| >10 | 11 | 3.0 | |
| Inpatient treatment | |||
| Yes, once | 102 | 27.5 | |
| Yes, more than once | 73 | 19.7 | |
| No | 196 | 52.8 | |
| Chronic disease | |||
| Yes | 116 | 31.3 | |
| No | 255 | 68.7 | |
| Regular medication | |||
| Yes | 145 | 39.1 | |
| No | 226 | 60.9 | |
| Computer proficiency | |||
| Very insecure | 23 | 6.2 | |
| Rather insecure | 55 | 14.8 | |
| Rather confident | 170 | 45.8 | |
| Very confident | 123 | 33.2 | |
| Mobile phone proficiency | |||
| Very insecure | 16 | 4.3 | |
| Rather insecure | 49 | 13.2 | |
| Rather confident | 159 | 42.9 | |
| Very confident | 147 | 39.6 | |
| Daily internet usage time | 2.90 (1.05) | ||
| Current use of video telephony | |||
| Yes | 292 | 78.7 | |
| No | 79 | 21.3 | |
| Possibility of VC with current GP | |||
| Yes | 30 | 8.1 | |
| No | 124 | 33.4 | |
| Not sure | 217 | 58.5 | |
| Prior use of VC | |||
| Yes, more than once | 0 | 0.0 | |
| Yes, once | 11 | 3.0 | |
| No | 360 | 97.0 | |
| Would use VC in the future | |||
| Very likely | 93 | 25.1 | |
| Rather likely | 155 | 41.8 | |
| Rather unlikely | 87 | 23.5 | |
| Very unlikely | 36 | 9.7 | |
| VC usage location | |||
| At workplace also | 50 | 13.5 | |
| Other places, but not at work | 93 | 25.1 | |
| Only at home | 228 | 61.5 |
GP: general practitioner; VC: video consultation; PHQ-2: Patient Health Questionnaire-2; GAD-2: generalized anxiety disorder-2.
Overall acceptance of VC by socio-demographic and medical data
Overall, the acceptance of this sample was moderate with a mean of M = 3.45 (SD = 1.02). For 76 participants (20.5%) acceptance was low, 153 participants (41.2%) showed moderate acceptance, and high acceptance was found in 142 participants (38.3%). An ANOVA showed no significant differences in acceptance between the three age groups, F2,368 = 0.106, p = 0.899. Independent t-tests revealed no significant difference in acceptance of VC regarding gender, t369 = 0.308, p = 0.758, or between chronically ill and non-chronically ill participants, t369 = 0.474, p = 0.636.
Predictors of acceptance of VC
Sociodemographic data included in the first step of multiple hierarchical regression analyses explained variance in acceptance of VC by 0.01%. (R2 = 0.001, F5,365 = 0.07, p = 0.997). No variable in the first step significantly explained acceptance. The addition of medical data in the second step (R2 = .039, F10,360 = 1.47, p = 0.150) increased the explained variance to 3.9% (Δ R2 = 0.038, F5,360 = 5.66, p < 0.001). The PHQ-2 sum score (β = 0.16, p = 0.009) and no regular medication (β = −0.36, p = 0.013) were found to significantly predict acceptance. In the third step, variables regarding ICT were included (R2 = 0.159, F17,353 = 3.94, p < 0.001), which resulted in an increase to 15.9% of explained variance in acceptance (Δ R2 =0 .120, F7,353 = 12.74, p <0.001). Computer proficiency (β = 0.28, p = 0.003), knowledge about digital health care solutions (β = 0.12, p = 0.021) and no prior use of VC (β = −0.78, p = 0.011) significantly predicted acceptance. The UTAUT predictors, added in the last step (R2 = 0.528, F20,350 = 19.56, p <0.001), changed the explained variance significantly to 52.8% in total (Δ R2 = 0.369, F3,350 = 91.03, p <0.001). Performance expectancy (β = 0.23, p <0.001), effort expectancy (β = 0.21, p <0.001) and social influence (β = 0.49, p <0.001) were significant predictors of acceptance of VC. Table 2 contains the results of multiple hierarchical regression analysis predicting acceptance of VC.
Table 2.
Results of multiple hierarchical regression analysis predicting acceptance of VC.
| Predictor | β | B | T | R 2 | Δ R2 | p value |
|---|---|---|---|---|---|---|
| Step 1: Socio-demographic data | 0.001 | 0.001 | ||||
| Sex: male | −0.07 | −0.07 | −0.88 | 0.381 | ||
| Age | 0.00 | 0.05 | 0.86 | 0.390 | ||
| Educational level | 0.01 | 0.01 | 0.31 | 0.754 | ||
| Occupational status | −0.07 | −0.09 | −1.90 | 0.058 | ||
| Same GP > 5 years | −0.08 | −0.08 | −0.97 | 0.335 | ||
| Step 2: Medical data | 0.039 | 0.038 | ||||
| Mental disorder | 0.16 | 0.16 | 1.10 | 0.274 | ||
| No chronic condition | 0.14 | 0.14 | 1.31 | 0.191 | ||
| No regular medication | −0.29 | −0.29 | −2.79 | 0.006 | ||
| PHQ-2 | 0.06 | 0.07 | 1.28 | 0.201 | ||
| GAD-2 | −0.08 | −0.09 | −1.72 | 0.086 | ||
| Step 3: ICT-related data | 0.159 | 0.120 | ||||
| Computer proficiency | 0.12 | 0.10 | 1.67 | 0.095 | ||
| Mobile phone proficiency | 0.03 | 0.02 | 0.40 | 0.688 | ||
| Daily internet usage time | 0.00 | 0.00 | 0.01 | 0.989 | ||
| No prior use of video conferencing | −0.09 | −0.09 | −0.88 | 0.380 | ||
| Knowledge about digital health care solutions | 0.00 | 0.00 | 0.01 | 0.991 | ||
| No prior use of VC | −0.33 | −0.33 | −1.44 | 0.152 | ||
| Important to know GP in person | −0.24 | −0.24 | −1.79 | 0.075 | ||
| Step 4: UTAUT predictors | 0.528 | 0.369 | ||||
| Effort expectancy | 0.21 | 0.18 | 4.05 | <0.001 | ||
| Performance expectancy | 0.23 | 0.24 | 5.44 | <0.001 | ||
| Social influence | 0.49 | 0.45 | 9.63 | <0.001 |
Note: N = 371. In Steps 2, 3 and 4 only the newly included variables are presented. β: standardized coefficient beta; B: unstandardized coefficient beta; R2: determination coefficient; ΔR2: Changes in R2. GP: general practitioner; VC: video consultation; PHQ-2: Patient Health Questionnaire-2; GAD-2: generalized anxiety disorder-2; ICT: information and communications technology; UTAUT: unified theory of acceptance and use of technology.
Comparison between restricted UTAUT and applied extended UTAUT model
Given the fact that the restricted UTAUT (three predictors only: performance expectancy, effort expectancy, social influence) reached 48.5% of explained variance in acceptance (R2 = 0.485), it was examined if the applied extended model (R2 = 0.528) is able to explain more variance in acceptance of VC. There was a significant difference in explained variance (F17,350 = 1.87, p = 0.020), indicating that the extent of explained variance could further be increased by adding context-specific variables.
Discussion
Principle results
In this study, patients’ acceptance of VC as an alternative to face-to-face consultations with their GP was examined and potential predictors of VC acceptance were determined. Overall moderate acceptance of VC could be found among the respondents. The majority of the participants showed moderate to high acceptance. In contrast to previous studies, there was no significant difference in acceptance regarding age, gender and no significant difference between chronically ill and non-chronically ill patients.47,65,66 Patients’ acceptance of VC was significantly predicted by their performance expectancy, effort expectancy, social influence. The PHQ-2 sum score, chronic medication and earlier use of VC, as well as computer proficiency and knowledge about digital health care solutions were significant predictors of acceptance. The applied extended model (consisting of the UTAUT predictors and additional variables) was superior in explaining variance of acceptance compared to the restricted model (only including performance expectancy, effort expectancy, social influence). This underlines the need to further adapt the UTAUT to increase the extent of explained variance, for instance by adding further context-specific variables.
Comparison to prior work
Although research on telemedical services has accelerated in recent years, only a little research has been conducted on the acceptance of VC in particular.17,67,68 This study was able to examine patients’ acceptance of VC with their GP across different age groups and applying standardized and validated research methods like the UTAUT model. Van Houwelingen et al. (2018) studied people‘s behavioural intention to use VC with their health care providers using the UTAUT, but only among the elderly population (aged 65 or older).69 De Veer et al.57 examined acceptance of e-Health applications using elements of the UTAUT,57 but again only among the older population (aged 57–77) and VC was not explicitly mentioned. Huygens et al.19 also investigated acceptance of internet services to communicate with the GP, but VC was not ultimately included in their UTAUT model. A study by Gardner et al.39 indicated high acceptance of VC but lacked in valid measurement instruments.
This study supports previous findings that the UTAUT has high predictive power with its construct‘s performance expectancy, effort expectancy, and social influence being significant predictors of patients’ intention to use telemedicine.19,56,57,69 Performance expectancy refers to the perception that patients will use telemedicine because they think that they can enhance their subjective health by doing so.36 Considering that performance expectancy has been identified as one of the strongest predictors of acceptance of telemedicine by numerous studies, healthcare providers should clearly demonstrate the possible benefits of using VC as an alternative to face-to-face in-office visits.55,70 By doing so, patients’ acceptance could be increased even further. Effort expectancy refers to the perception that using VC is easy and does not require too much effort.36 This may be especially vital for older users with no or little experience with ICT and in particular telemedicine. Healthcare providers and decision-makers should focus on providing easy access and offering older patients guidance and assistance to enhance acceptance. Social influence, as the third UTAUT predictor, refers to a person's belief that important others (e.g., family or friends) would approve using VC.36 Literature showed mixed results concerning the relevance of social influence as a predictor of acceptance. The original UTAUT (model) by Venkatesh et al.36 stated that social influence is only significant in a mandatory context. Even though VC usage was not mandatory, social influence was a significant predictor in the present study. Some studies came to similar results regarding the intention to use e-Health,56,71 whereas social influence was not significant in a study by de Veer et al.57 Prior research revealed that female gender is supposed to be associated with higher acceptance.47 In contrast, no difference in VC acceptance between female and male patients could be found in this study. Although several studies have demonstrated differences in technology acceptance between young and older users (often referred to as ‘digital divide’),72,74 age was not a significant predictor in the present survey.
There were no significant differences in acceptance ratings among chronically ill and non-chronically ill patients in this sample. A study by Salgado et al. (2020) described similar results regarding the acceptance of mobile health by chronically ill patients.75 This finding seems surprising, given the fact that especially chronically ill patients could benefit from using VC to maintain their health, particularly in view of the ongoing COVID-19 pandemic. VC offers the possibility of minimizing the risk of infection and remotely still be in contact with their GP. One possible explanation is that patients who need to see their doctor frequently because of a chronic condition are more likely to insist on a personal relationship with their doctor. The doctor is seen as a kind of companion through long suffering and VC may convey the impression of an impersonal atmosphere. In addition, the lack of regular physical examination, which is necessary for various chronic conditions may be a decisive aspect.
Depressive symptoms are associated with higher acceptance of VC in the present study. Other studies demonstrated that patients who suffer from depression often avoid seeking professional treatment, because of possible stigmatization.76,77 By using VC patients are offered the possibility to receive treatment in their own homes, which can contribute to an improved feeling of discretion and privacy. This can therefore lead to an increase in treatment adherence of people with depression. VC has been proven to be as effective as face-to-face visits in the treatment of depressive disorders.78,80 The use of regular medication was also a significant predictor of acceptance in the extended model of this study. A study by Ebbert et al.81 showed that a large proportion of patients are willing to use telemedical services to refill their prescriptions. Especially patients who rely on regular prescriptions could benefit from the advantages of VC like avoided travel expenses and reduced waiting times.
Leng et al.42 demonstrated in their study a positive link between increasing computer proficiency and patients’ intention to use VC. This is in line with the results of the proposed study, which showed that computer proficiency and existing knowledge about digital health care solutions were significant predictors of VC acceptance.
Facilitating conditions, as the fourth predictor of the UTAUT by Venkatesh et al.,36 were not included in the model of this study because it was intended to be a significant predictor of the actual usage, not the intention to use ( = acceptance). Although different studies showed that intention can be an indicator of actual behaviour, there is still a discrepancy between intention and actual usage, which is referred to as ‘intention-behavior gap’.82
Even though the survey was conducted during the COVID-19 pandemic, which led to an increase in remote consultations,5 only 3% of the respondents had prior experience with VC at the time of the survey. This is in accordance with previous studies, which demonstrated that VC was not frequently used by patients before the pandemic, although most of the patients would be generally willing to use VC if the possibility was offered to them.18,19,83 Besides organizational and infrastructural barriers,84,85 which led to slow implementation of VC in the broad population, missing knowledge about the availability of VC with their GP may be another reason for slow uptake. Only 8.1% of the participants stated that their GP offered VC, and 58.1% were not aware of the possibility. It is necessary to increase awareness and knowledge of VC technologies and their functions. Mittmann et al. suggested targeted marketing campaigns as a way to further promote the implementation of VC.86 Other studies have revealed high satisfaction with telemedicine during the pandemic.5,52 The COVID-19 pandemic has revealed shortcomings in the digitization of health care, and the need for improvement became visible. The current window of opportunity should be seized to overcome existing barriers and further push the implementation of VC also in a post-pandemic setting.
Theoretical implications
This study contributes important findings to the growing body of literature on telemedicine and VC. The applied extended UTAUT model was proven to be suitable for predicting VC acceptance. The identified context-specific predictors could contribute to increasing VC acceptance in the future. Future research should focus on exploring further suitable and specific predictors to enhance the viability of the UTAUT in a health-related context. The proposed predictors could also easily be applied in studies on the actual use of VC in clinical practice, enabling researchers to retrospectively examine its ultimate predictive power. One strength of this study is that it also assessed the perceptions of patients who declined to use VC, unlike most existing studies on VC, which only focused on patients’ and clinicians’ experiences after using VC. This study's approach to predicting acceptance instead of retrospectively analysing satisfaction allows to use the findings of this study in other health-related research fields and offers additional value for the implementation of VC in health care.
Practical implications
This study provides valuable implications for fostering the future implementation of VC in clinical practice. Based on the identified predictors of acceptance, the following implications are proposed to further increase acceptance ratings. As computer proficiency was identified as a predictor of VC acceptance, it is essential that health care providers and decision-makers focus on people with little to no knowledge of computers or related technology. Demographic change, which is leading to a population with an increasingly high average age, might further aggravate this issue.87 Consequently, it is important to offer tailored programmes to increase digital knowledge to these groups and to ensure that using VC applications is easy and simple (effort expectancy). Future research should therefore concentrate on approaches to simplifying VC usage and removing technical barriers. Performance expectancy also significantly predicted acceptance. This indicates that it is vitally important to demonstrate the advantages and benefits of VC to a larger group of patients. Additionally, further research is required to determine the clinical conditions in which VC is primarily perceived to improve personal health. The presence of symptoms of depression was a predictor of acceptance in this study. This may indicate that VC is particularly suitable for vulnerable groups and people with mental illnesses. Treatment of these patients often requires many hours of psychotherapy and waiting lists are long. As physical contact is not necessary, therapeutic counselling by the GP through VC could offer an alternative for those patients and at the same time relieve the health care system. This study also confirmed that VC was not frequently used before the pandemic. Other studies have demonstrated that VC usage has increased significantly during this extraordinary time; however, it remains unclear whether VC use will remain at this level.6 Therefore, steps should be taken not only to further raise awareness of VC availability but also to establish trust in its safety. Decision makers and health care providers could use this study‘s findings to increase the adoption of VC in the future.
Limitations and future research directions
Given that the study was conducted via an online survey, the main limitation is the requirement for internet access. As previous studies showed internet access is significantly lower in the elderly population younger participants were overrepresented in this study (mean age: 44.4 years).88 This could have led to an overestimation of the VC acceptance because age is ascertained to be related to the intention to use telemedicine. Furthermore, people with lower level of education are underrepresented in this study. This may be due to the fact that higher educated people are more likely to participate in research questionnaires and have a greater interest in maintaining and improving their state of health. It should also be noted that people who are willing to participate in an online survey are already more likely to use telemedical services such as VC. Thus, these selection biases could limit the generalizability of the results of this study.
Data collected in this survey were self-reported. To avoid or minimize possible emerging common-method variance, the questionnaire had a reasonable length, the participants were informed that the survey was anonymous, and their answers were treated confidentially. In order to further improve data quality, five percent of the respondents who completed the survey the quickest were excluded as this could be an indicator of careless or inattentive responding.
The UTAUT model was applied via a restricted version of the questionnaire which might have impacted the reliability of the results. Future studies should investigate the parsimony of the UTAUT model.
As stated previously this study was conducted during the COVID-19 pandemic. This could have influenced participants’ perspectives on VC usage in a positive way considering the possibility of seeking advice or treatment from their GP without the risk of infection. At this time, it is uncertain if patients’ acceptance of VC will remain at this level post-COVID-19.
Future research should include other sections of the population, especially the elderly and people with lower education. Other context-specific predictors should be examined to further improve explained variance. Moreover, the long-term effects of the COVID-19 pandemic on usage behaviour should be studied.
Conclusion
The findings of this study indicate moderate acceptance of VC as an alternative to face-to-face in-office visits. The applied UTAUT model has proven itself as a suitable and efficient method to determine the acceptance of VC. The three UTAUT constructs performance expectancy, effort expectancy, and social influence are significant predictors of patients’ acceptance to use VC and explained a high level of variance of acceptance. Furthermore, the context-specific predictors (computer proficiency, knowledge about digital health solutions, prior use of VC, symptoms of depression and regular medication) could explain a significant part of the variance of VC acceptance.
Given the fact that there is apparent demand and acceptance for alternate ways to engage with their health care providers, additional measures should be taken by decision-makers and clinicians to establish VC as a safe and viable alternative in the foreseeable future.
Footnotes
Contributorship: AB, E-MS, and MT initiated the study. AB, AE, E-MS, and MT contributed to designing the study and developing the intervention. AB administered drafted the manuscript with AE. Statistical analyses were conducted by LJ, AE, and AB. AE, AB, JidS, E-MS, LJ and MT contributed to the preparation of the manuscript. All authors read and approved the final version of the manuscript.
Ethical approval: The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Medical Faculty of the University of Duisburg-Essen (19-89-47-BO).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Open Access Publication Fund of the University of Duisburg-Essen.
Guarantor: AB.
ORCID iD: Alexander Bäuerle https://orcid.org/0000-0003-1488-8592
References
- 1.Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature 2020; 579: 265–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. WHO announces COVID-19 outbreak a pandemic, https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (2020, accessed March 22, 2021 2021).
- 3.World Health Organization. Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (2021, accessed March, 22nd, 2021 2021).
- 4.Matrajt L, Leung T. Evaluating the effectiveness of social distancing interventions to delay or flatten the epidemic curve of coronavirus disease. Emerg Infect Dis 2020; 26: 1740–1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc 2020; 27: 1132–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilson SF, Umscheid CA, Laiteerapong N, et al. Growth of ambulatory virtual visits and differential use by patient sociodemographics at one urban academic medical center during the COVID-19 pandemic: retrospective analysis. JMIR Med Inform 2020; 8: e24544–e24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. 2010.
- 8.Marengoni A, Angleman S, Melis R, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 2011; 10: 430–439. [DOI] [PubMed] [Google Scholar]
- 9.van den Bussche H. [The future problems of general practice in Germany: current trends and necessary measures]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2019; 62: 1129–1137. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Ageing and health, https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (2018, accessed March 7, 2021).
- 11.Board on Health Care Services, Insitute of Medicine. The role of telehealth in an evolving health care environment: workshop summary. Washington, DC: The National Academies Press, 2012, p.158. [PubMed] [Google Scholar]
- 12.Weinstein RS, Lopez AM, Joseph BA, et al. Telemedicine, telehealth, and mobile health applications that work: opportunities and barriers. Am J Med 2014; 127: 183–187. [DOI] [PubMed] [Google Scholar]
- 13.Raven M, Butler C, Bywood P. Video-based telehealth in Australian primary health care: current use and future potential. Aust J Prim Health 2013; 19: 283–286. [DOI] [PubMed] [Google Scholar]
- 14.Federal Ministry of Health (Germany). e-health Initiative: Kriterienkatalog zur Unterstützung der gezielten Planung, Durchführung und Evaluation von telemedizinischen Projekten. 2020.
- 15.Federal Ministry of Health (Germany). Gesetz für sichere digitale Kommunikation und Anwendungen im Gesundheitswesen sowie zur Änderung weiterer Gesetze, https://www.bgbl.de/xaver/bgbl/start.xav?startbk = Bundesanzeiger_BGBl&jumpTo = bgbl115s2408.pdf#__bgbl__%2F%2F*%5B%40attr_id%3D%27bgbl115s2408.pdf%27%5D__1615132023628 (2015, accessed March 7, 2021).
- 16.Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One 2019; 14: e0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thiyagarajan A, Grant C, Griffiths F, et al. Exploring patients’ and clinicians’ experiences of video consultations in primary care: a systematic scoping review. BJGP Open 2020; 4: bjgpopen20X101020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donaghy E, Atherton H, Hammersley V, et al. Acceptability, benefits, and challenges of video consulting: a qualitative study in primary care. Br J Gen Pract 2019; 69: e586–e594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huygens MW, Vermeulen J, Friele RD, et al. Internet services for communicating with the general practice: barely noticed and used by patients. Interact J Med Res 2015; 4: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bashshur RL, Shannon GW, Bashshur N, et al. The empirical evidence for telemedicine interventions in mental disorders. Telemed J E Health 2016; 22: 87–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jess M, Timm H, Dieperink KB. Video consultations in palliative care: a systematic integrative review. Palliat Med 2019; 33: 942–958. [DOI] [PubMed] [Google Scholar]
- 22.Lee JJ, English JC, 3rd. Teledermatology: a review and update. Am J Clin Dermatol 2018; 19: 253–260. [DOI] [PubMed] [Google Scholar]
- 23.Thelen-Perry S, Ved R, Ellimoottil C. Evaluating the patient experience with urological video visits at an academic medical center. Mhealth 2018; 4: 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nord G, Rising KL, Band RA, et al. On-demand synchronous audio video telemedicine visits are cost effective. Am J Emerg Med 2019; 37: 890–894. [DOI] [PubMed] [Google Scholar]
- 25.Crotty M, Killington M, van den Berg M, et al. Telerehabilitation for older people using off-the-shelf applications: acceptability and feasibility. J Telemed Telecare 2014; 20: 370–376. [DOI] [PubMed] [Google Scholar]
- 26.Steventon A, Bardsley M, Billings J, et al. Effect of telehealth on use of secondary care and mortality: findings from the whole system demonstrator cluster randomised trial. Br Med J 2012; 344: e3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sevean P, Dampier S, Spadoni M, et al. Patients and families experiences with video telehealth in rural/remote communities in northern Canada. J Clin Nurs 2009; 18: 2573–2579. [DOI] [PubMed] [Google Scholar]
- 28.Snoswell CL, Comans TA. Does the choice between a telehealth and an in-person appointment change patient attendance? Telemed J E Health 2020; 27: 733–738. [DOI] [PubMed] [Google Scholar]
- 29.Shaw S, Wherton J, Vijayaraghavan S, et al. Health Services and Delivery Research. Advantages and limitations of virtual online consultations in a NHS acute trust: the VOCAL mixed-methods study. vol. 6. Southampton (UK): NIHR Journals Library, 2018, pp. 1–136. [PubMed] [Google Scholar]
- 30.Greenhalgh T, Vijayaraghavan S, Wherton J, et al. Virtual online consultations: advantages and limitations (VOCAL) study. BMJ Open 2016; 6: e009388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hanna L, Fairhurst K. Using information and communication technologies to consult with patients in victorian primary care: the views of general practitioners. Aust J Prim Health 2013; 19: 166–170. [DOI] [PubMed] [Google Scholar]
- 32.Fahlbusch L, Achenbach J, Hoffmann FR. [Video consultation hours in the statutory accident insurance - application possibilities and economic evaluation]. Gesundheitswesen 2020; 83: 867–870. [DOI] [PubMed] [Google Scholar]
- 33.Dwivedi YK, Rana NP, Tamilmani K, et al. A meta-analysis based modified unified theory of acceptance and use of technology (meta-UTAUT): a review of emerging literature. Curr Opin Psychol 2020; 36: 13–18. [DOI] [PubMed] [Google Scholar]
- 34.Harst L, Lantzsch H, Scheibe M. Theories predicting End-user acceptance of telemedicine use: systematic review. J Med Internet Res 2019; 21: e13117–e13117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q 1989; 13: 319–340. [Google Scholar]
- 36.Venkatesh V, Morris MG, Davis GB, et al. User acceptance of information technology: toward a unified view. MIS Q 2003; 27: 425–478. [Google Scholar]
- 37.van Raaij EM, Schepers JJL. The acceptance and use of a virtual learning environment in China. Comput Educ 2008; 50: 838–852. [Google Scholar]
- 38.Powell RE, Henstenburg JM, Cooper G, et al. Patient perceptions of telehealth primary care video visits. Ann Family Med 2017; 15: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gardner MR, Jenkins SM, O‘Neil DA, et al. Perceptions of video-based appointments from the patient‘s home: a patient survey. Telemed J E Health 2015; 21: 281–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. Br Med J 2000; 320: 1517–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stahl JE, Dixon RF. Acceptability and willingness to pay for primary care videoconferencing: a randomized controlled trial. J Telemed Telecare 2010; 16: 147–151. [DOI] [PubMed] [Google Scholar]
- 42.Leng S, MacDougall M, McKinstry B. The acceptability to patients of video-consulting in general practice: semi-structured interviews in three diverse general practices. J Innov Health Inform 2016; 23: 41. [DOI] [PubMed] [Google Scholar]
- 43.Bradford NK, Caffery LJ, Smith AC. Awareness, experiences and perceptions of telehealth in a rural queensland community. BMC Health Serv Res 2015; 15: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schers HJ, Buitenhuis E, Besemer Y. [Video consultation in general practice: need and feasibility]. Ned Tijdschr Geneeskd 2014; 158: A8003. [PubMed] [Google Scholar]
- 45.Hammersley V, Donaghy E, Parker R, et al. Comparing the content and quality of video, telephone, and face-to-face consultations: a non-randomised, quasi-experimental, exploratory study in UK primary care. Br J Gen Pract 2019; 69: e595–e604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Angrish S, Sharma M, Bashar MA, et al. How effective is the virtual primary healthcare centers? An experience from rural India. J Family Med Prim Care 2020; 9: 465–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Polinski JM, Barker T, Gagliano N, et al. Patients’ satisfaction with and preference for telehealth visits. J Gen Intern Med 2016; 31: 269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Johansson AM, Söderberg S, Lindberg I. Views of residents of rural areas on accessibility to specialist care through videoconference. Technol Health Care 2014; 22: 147–155. [DOI] [PubMed] [Google Scholar]
- 49.Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 2017; 7: e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schifeling CH, Shanbhag P, Johnson A, et al. Disparities in video and telephone visits among older adults during the COVID-19 pandemic: cross-sectional analysis. JMIR Aging 2020; 3: e23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peters L, Greenfield G, Majeed A, et al. The impact of private online video consulting in primary care. J R Soc Med 2018; 111: 162–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Imlach F, McKinlay E, Middleton L, et al. Telehealth consultations in general practice during a pandemic lockdown: survey and interviews on patient experiences and preferences. BMC Fam Pract 2020; 21: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kalavani A, Kazerani M, Shekofteh M. Acceptance of evidence based medicine (EBM) databases by Iranian medical residents using unified theory of acceptance and use of technology (UTAUT). Health Policy Technol 2018; 7: 287–292. [Google Scholar]
- 54.Šumak B, Šorgo A. The acceptance and use of interactive whiteboards among teachers: differences in UTAUT determinants between pre-and post-adopters. Comput Human Behav 2016; 64: 602–620. [Google Scholar]
- 55.Cimperman M, Makovec Brenčič M, Trkman P. Analyzing older users’ home telehealth services acceptance behavior-applying an extended UTAUT model. Int J Med Inform 2016; 90: 22–31. [DOI] [PubMed] [Google Scholar]
- 56.Quaosar G, Hoque MR, Bao Y. Investigating factors affecting elderly‘s intention to use m-health services: an empirical study. Telemed J E Health 2018; 24: 309–314. [DOI] [PubMed] [Google Scholar]
- 57.de Veer AJ, Peeters JM, Brabers AE, et al. Determinants of the intention to use e-health by community dwelling older people. BMC Health Serv Res 2015; 15: 03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.James HM, Papoutsi C, Wherton J, et al. Spread, scale-up, and sustainability of video consulting in health care: systematic review and synthesis guided by the NASSS framework. J Med Internet Res 2021; 23: e23775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Barkai G, Gadot M, Amir H, et al. Patient and clinician experience with a rapidly implemented large-scale video consultation program during COVID-19. Int J Qual Health Care 2021; 33: mzaa165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Greszki R, Meyer M, Schoen H. Exploring the effects of removing “too fast” responses and respondents from web surveys. Public Opin Q 2015; 79: 471–503. [Google Scholar]
- 61.Kroenke K, Spitzer RL, Williams JB, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009; 50: 613–621. [DOI] [PubMed] [Google Scholar]
- 62.Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41: 1284–1292. [DOI] [PubMed] [Google Scholar]
- 63.Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 64.Schmidt AF, Finan C. Linear regression and the normality assumption. J Clin Epidemiol 2018; 98: 146–151. [DOI] [PubMed] [Google Scholar]
- 65.Nunes A, Limpo T, Castro SL. Acceptance of Mobile health applications: examining key determinants and moderators. Front Psychol 2019; 10: 2791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rodriguez JA, Betancourt JR, Sequist TD, et al. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021; 27: 21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Barsom EZ, van Hees E, Bemelman WA, et al. Measuring patient satisfaction with video consultation: a systematic review of assessment tools and their measurement properties. Int J Technol Assess Health Care 2020; 36: 356–362. [DOI] [PubMed] [Google Scholar]
- 68.Almathami HKY, Win KT, Vlahu-Gjorgievska E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J Med Internet Res 2020; 22: e16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van Houwelingen CT, Ettema RG, Antonietti MG, et al. Understanding older people‘s readiness for receiving telehealth: mixed-method study. J Med Internet Res 2018; 20: e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gücin NÖ, Berk ÖS. Technology acceptance in health care: an integrative review of predictive factors and intervention programs. Procedia – Soc Behav Sci 2015; 195: 1698–1704. [Google Scholar]
- 71.Damerau M, Teufel M, Musche V, et al. Determining acceptance of e-mental health interventions in digital psychodiabetology using a quantitative web-based survey: cross-sectional study. JMIR Form Res 2021; 5: e27436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chung JE, Park N, Wang H, et al. Age differences in perceptions of online community participation among non-users: an extension of the technology acceptance model. Comput Human Behav 2010; 26: 1674–1684. [Google Scholar]
- 73.Kim S, Choudhury A. Comparison of older and younger adults’ attitudes toward the adoption and use of activity trackers. JMIR Mhealth Uhealth 2020; 8: e18312–e18312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Song Y, Qian C, Pickard S. Age-Related digital divide during the COVID-19 pandemic in China. Int J Environ Res Public Health 2021; 18: 11285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Salgado T, Tavares J, Oliveira T. Drivers of mobile health acceptance and use from the patient perspective: survey study and quantitative model development. JMIR Mhealth Uhealth 2020; 8: e17588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cooper-Patrick L, Powe NR, Jenckes MW, et al. Identification of patient attitudes and preferences regarding treatment of depression. J Gen Intern Med 1997; 12: 431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Barney LJ, Griffiths KM, Jorm AF, et al. Stigma about depression and its impact on help-seeking intentions. Aust N Z J Psychiatry 2006; 40: 51–54. [DOI] [PubMed] [Google Scholar]
- 78.Thompson DA, Leimig R, Gower G, et al. Assessment of depressive symptoms during post-transplant follow-up care performed via telehealth. Telemed J E Health 2009; 15: 700–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Choi NG, Marti CN, Bruce ML, et al. Six-month postintervention depression and disability outcomes of in-home telehealth problem-solving therapy for depressed, low-income homebound older adults. Depress Anxiety 2014; 31: 653–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.García-Lizana F, Muñoz-Mayorga I. Telemedicine for depression: a systematic review. Perspect Psychiatr Care 2010; 46: 119–126. [DOI] [PubMed] [Google Scholar]
- 81.Ebbert JO, Ramar P, Tulledge-Scheitel SM, et al. Patient preferences for telehealth services in a large multispecialty practice. J Telemed Telecare 2021. DOI: 10.1177/1357633X20980302. [DOI] [PubMed] [Google Scholar]
- 82.Faries MD. Why we don‘t “just do it”: understanding the intention-behavior gap in lifestyle medicine. Am J Lifestyle Med 2016; 10: 322–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Brant H, Atherton H, Ziebland S, et al. Using alternatives to face-to-face consultations: a survey of prevalence and attitudes in general practice. Br J Gen Pract 2016; 66: e460–e466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Atherton H, Brant H, Ziebland S, et al. The potential of alternatives to face-to-face consultation in general practice, and the impact on different patient groups: a mixed-methods case study. Health Serv Deliv Res 2018; 6. DOI: 10.3310/hsdr06200. [DOI] [PubMed] [Google Scholar]
- 85.Saiyed S, Nguyen A, Singh R. Physician perspective and key satisfaction indicators with rapid telehealth adoption during the coronavirus disease 2019 pandemic. Telemed J E Health 2021; 27: 1225–1234. [DOI] [PubMed] [Google Scholar]
- 86.Mittmann CB K, Hoffmann F. The video consultation in the scope of the statutory health insurance – implementation, dissemination and development opportunities from a patient’s perspective. Gesundheitsökonomie und Qualitätsmanagement 2020; 25: 291–296. [Google Scholar]
- 87.Nowossadeck E, Prütz F, Teti A. Population change and the burden of hospitalization in Germany 2000-2040: decomposition analysis and projection. PLoS One 2020; 15: e0243322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Huxhold O, Otte K. Internetzugang und Internetnutzung in der zweiten Lebenshälfte. Berlin: Deutsches Zentrum für Altersfragen, 2019. [Google Scholar]