Abstract
This analysis investigates and scores the impact of new health price transparency rules. Using a set of novel data sources, we estimate substantial savings are possible following the implementation of the insurer price transparency rule. Specifically, we estimate annual savings to consumers, employers, and insurers by 2025, assuming a robust set of tools to allow consumers to purchase medical services. We matched claims with 70 HHS defined shoppable services by CPT and DRG codes and replaced them with an estimated median commercial allowed payment multiplied by a reduced cost of 40% based on estimates found from literature for the difference in cost between negotiated and cash payment for medical services. We consider 40% to be an upper bound estimate of the potential savings based on existing literature. Several databases are used to estimate the potential benefits of insurer price transparency. Two different all-payer claim databases were used, representing the entire insured population in the US. For this analysis, only the private insurer commercial population was examined, comprised of over 200 million covered lives as of 2021. The estimated impact of price transparency will vary significantly by region and income level. The national upper bound estimate is $80.7 billion. The national lower bound estimate is $17.6 billion. For the upper bound, the region with the most significant impact in the US will be the Midwest, with $20 billion in potential savings and an 8% reduction in medical expenditure. The region with the lowest impact will be the South, with only a 5.8% reduction. Concerning income, those at lower levels of income will have the most significant impact with a −7.4% (<100% Federal Poverty Level) to −7.5% (100%-137% Federal Poverty Level) impact. Overall, the total impact could be a 6.9% reduction for the whole privately insured population in the United States. In summary, a unique set of national data resources were used to estimate the cost savings impact medical price transparency. This analysis suggests price transparency for shoppable services may yields significant savings between $17.6 to $80.7 billion by 2025. Consumers may have strong incentives to shop with the rise in the use of high deductibles, health plans, and health savings accounts. How these potential saving are to be shared by consumers, employers and health plans has yet to be determined.
Keywords: health insurance, price transparency, consumer driven health plan, competition, health policy, all-payer claims data
What do we already know about this topic?
Price transparency has been discussed for 15 years as a national health policy, but little effect has been demonstrated beyond a handful of experiments in employer or health plan settings.
How does your research contribute to the field?
This research is the first financial, national estimate of price transparency using novel all-payer claims data at a national level.
What are your research’s implications toward theory, practice, or policy?
The implications are price transparency has the potential to reduce health cost increases significantly.
American consumers could see significant savings if government policy supported their ability to know the price of care ahead of time and share in any savings if they choose lower-cost care. This paper presents an analysis of the impact of the potential benefits of the federal government’s transparency regulatory reform and the pending implementation of the Insurance industry-focused regulation in 2022. Using novel health insurance claims data from synthetic all-payer databases, we estimate the impact of the rules on American consumers. This estimate will be an upper bound of the potential impact. The paper proceeds as follows. First, we summarize the policies and their current State of execution in the Biden Administration. Second, we describe the data and estimation methods used for our results. Third, we present several scenarios highlighting the potential impact of the transparency regulation directed at insurers.
Policy Background
The lack of health care price transparency has been noted as a significant concern for a robust market since economist Kenneth Arrow’s seminal 1963 article on the incentives of the modern US health economy.1 Providers can exert monopoly pricing power without the full information consumers need for a competitive and efficient market without price transparency. The role of public and private health insurers as third-party arbitrators of a negotiated price paid for medical care has reached an industrial scale, with over 300 million US citizens enrolled in some form of a health insurance contract with a pre-determined fee schedule unavailable to consumers. Growing evidence has shown a large variation in medical care price largely due to the ability of providers and insurers to negotiate prices opaquely.2
The public policy goal of price transparency of medical care emerged in the Administration of President George W. Bush as part of supporting consumer-driven health.3 This administration’s most significant policy achievement to promote price transparency was the development of Health Savings Accounts (HSAs) to be available to all private insurance contracts so long as HSAs were paired with a high-deductible health plan (HDHP). These health plan designs have grown from a nascent share of the health insurance market in the 2000s to employers’ fastest growing health plan design by 2021, second only to PPOs as the most preferred health insurance design.4
High deductibles were created and accelerated in the employer-sponsored section of the insurance industry as a way for employers to manage healthcare costs, including by making the customer more aware and accountable for their care.4 The accompanying HSAs have become a boon for businesses to expand revenue-generating offerings for employee benefits management, another potential retirement account for those able to manage healthcare utilization with other assets.
HSAs also functioned as a wake-up call for consumers now facing out-of-pocket costs for using healthcare and must conduct research or face severe pain in the pocketbook.
In 2019, the Administration of President Donald J. Trump created an executive order to develop federal regulations to accelerate the visibility of health care prices to all consumers. The executive order led to 2 separate federal rules; one focused on hospital price disclosure and the other on insurers’ negotiated price disclosure with all medical providers.5
The hospital rule became effective in 2021 but has had limited—yet increasing compliance by US hospitals.6,7 The hospital rule also required “clear and accessible pricing information online” in 2 formats: a “machine readable file” with common items and services and a display of shoppable services in a consumer -friendly format. The insurer rule was delayed from January 1, 2022, to July 1, 2022, for implementation by the Administration of President Joseph Biden for further clarification and implementation instructions.
The hallmark of the insurer rule was that it would require the insurers to release monthly a simple electronic file with all prices negotiated by all insurers. The insurer rule intends to provide the raw data for data application entrepreneurs to create easy-to-use medical care shopping tools for many medical procedures considered shoppable and likely priced below a deductible threshold where either HSA funds are used on a consumer’s cash account for payment.
The evidence supporting the price transparency policy will yield savings in medical expenditures is limited.8,9 The actual test of the hospital and insurer rules will require several years of data and experience to see the full impact of the policy experiment. Robinson and Brown found that providing employees the ability to choose low-cost facilities and services contributed to using low-cost facilities 21.2% more frequently and high-cost facilities 34.3% less frequently.10 Prices at low-cost facilities remained constant, and high-cost facility prices declined by 18%. Whaley et al analyzed claims data for 3 common services. They found that using the price transparency platform resulted in lower reimbursement prices in all 3 areas, albeit with a more significant reduction in laboratory and imaging than in clinician office visits.11 Other research by Christensen et al12 yield similar results in price decreases. Christensen et al also reflect the limitation in impact due to the limited price transparency structure.
A more recent comprehensive analysis of the potential impact of price transparency was completed by VanHorn et al.13 With 1 billion claims from insurers from 2017 to 2019, they estimated the opportunity cost from the impact of narrowing price variation for employers. Their results suggest a 40% reduction in expenditure for shoppable services is possible based on comparing the prices paid by commercial insurers and cash payments for medical care. Specifically, they found shifts from the top 75th percentile of negotiated prices to the cash prices would reduce employer’s hospital-related costs by 40%. This work is further supported by findings from insurer rule regulatory impact analysis of a potential savings of $1 to $5 billion.14
One of the latest studies examined impact of online advertising in New Hampshire. In 2021 Desai et al found residents’ use of provider price tool was significant but not using the data to find use lower-price providers.15 Another recent study by Whaley et al using employer data from 2017 to 2018 saw significant reduction prices for imaging but no effect on utilization if consumers were given incentives to shop for care.16 Results from 2010 to 2016 study by Gourevitch et al found the proportion of pregnant individuals who sought price information before childbirth more than doubled within the first 6 years of availability of a price transparency tool. These findings suggest that price information may help individuals anticipate their out-of-pocket childbirth costs.17 These more recent studies all vary in degree of impact, but most are showing directionally positive and significant consumer response to price transparency tools. The timetable for implementation of the new federal policies on transparency has been staggered over several years. The hospital price transparency rule is already in effect since January 1, 2021. January 1, 2023, will begin the final stage of the rule implementation, which will have Americans be provided online shopping tools for members with absolute transparency in this tool completed by January 1, 2024. The transition from the Biden administration to the Trump administration for rule implementation has been relatively unaltered.
Analysis Methodology
We seek to estimate the impact of insurer price transparency based on the full implementation of the federal rules on price transparency by 2025. To complete this analysis, several national all-payer claims databases are utilized. Several assumptions are also required for this estimation.
Shoppable Service Focus: We use the shoppable services developed by HHS. These include a combination of medical and inpatient procedures.18
CPT4 and DRG Code Matching and Replacement: We matched claims with shoppable services by CPT and DRG codes and replaced them with an estimated median commercial allowed payment multiplied by a reduced cost of 40% based on estimates found from literature for the difference in cost between negotiated and cash payment for medical services. We consider 40% to be an upper bound estimate of the potential savings.
Focus on Medical Procedure Services: We only focused on medical procedures and admissions.
Savings Reported Accrue to Health Plan & Consumer Combined: We assume that savings from transparency will go back to the combined unit of consumer and health plan.
Analysis Approach
We completed a price replacement for commercial insurance claims by CPT4 or DRG for shoppable service as defined by CMS. Before we could complete price replacement, we needed to calibrate the claims databases to 2020 dollars. After calibration, we computed the average and median allowed amounts for each CPT and DRG.
This estimate became our status quo baseline for comparison. The next step of price replacement was to take each shoppable service by CPT4 or DRG and replace it with a price less than the commercial allowed rate. This exercise aimed to show the maximum possible effect transparency could achieve if the service were shoppable. The price replacement could only be achieved if the actual CPT4 or DRG was used in the synthetic data. We found that 85% of the CPT4 or DRGs could match the data. We believe this would have been higher with a more contemporary all-payer database. As a result, our estimated impact will be more conservative than expected.
If the CPT4 and DRG matched, we then took the corresponding commercial insurance median price and discounted it by 40% based on the analysis of Vanhorn et al.13 This reduction was also to the expected saving estimate used by the White House and HHS when they presented the justification for the Executive Order to the President in 2019.
We consider this measure an upper bound because (a) it applies to entire commercially insured, (b) it does not account for a possible increase in prices from transparency in non-competitive markets with high 1 or 2 large providers, and (c) it assumes all providers offering shoppable services will discount to a cash price similar to what was found in the Vanderbilt database.
Some of the shoppable services in the HHS list are required to be provided at $0 cost sharing and prior to application of any deductible, per the Affordable Care Act. For example, screening mammograms and certain preventive visits/services. We would expect less shopping, and less opportunity for cost savings for these services, given no out-of-pocket consumer obligation and the greater likelihood of existing provider-patient relationships for these services relative to acute care services. Our estimates will take this into consideration using claims data and actual reimbursements for estimation for these services post ACA.
Other HHS shoppable services are likely to have costs that well exceed the maximum out-of-pocket limits under the Affordable Care Act and/or the high deductibles linked to HSA plans (eg, surgical procedures). In these instances, the consumer may be liable for their full deductible/OOP maximum, regardless of the total cost of the procedure. This may present less incentive to shop if the majority of the saving would accrue solely to the employer/health insurer after the deductible is paid.
Two additional estimates are also considered using the shoppable services. The first is an exclusive focus on the population enrolled in the high deductible health plans with HSAs in the employer-sponsored plan market. The second estimate examines just the digital native populations with health insurance subscribers between the ages of 26 and 42 by 2025, constituting Millennials and Generation Z. They are no longer eligible to be on their parent’s health plan.
We assume these digital natives will have the most natural incentive to shop using the online tools and applications expected to be developed from the release of insurance negotiated prices.
Data Sources
The 3 data sources used for the savings estimation are SynUsa, SYHDR, and the Vanderbilt University Cash Pay Database (VUCPD). SynUSA is a nationally representative synthetic all-payer claims database developed by HSI Network as a test bed for policy research, academics, and entrepreneurs and was used as the prototype for former President Trump’s synthetic claims database as part of the transparency executive order. There have been over 200 users since 2018.19 The database incorporates the 5 major payer categories (fee for service Medicare, Medicare Advantage, employer-sponsored health insurance, non-group private health insurance, and Medicaid). SHYDR was built by the Agency for Health Care Research and Quality (AHRQ) as part of President Trump’s Price Transparency Executive Order and has been available since 2021.20 It contains data from 3 payers (Commercial, Medicare, and Medicaid). The Vanderbilt University Cash Pay Database is based on claims transactions for 3 prominent national claims clearinghouse vendors and was used as part of President Trump’s Executive Order to estimate the saving from a Price Transparency initiative related to shoppable services. It is focused on sets of “shoppable services” CPT4/HCPCS procedure code to negotiate cash prices across all 4 major census areas of the United States. With this price replacement database, the SynUSA variables of States, Census Region, and Federal Poverty Line Percentage (FPL) to generate overall results and then sub-population analysis. The variation seen will be driven by the size of the relative populations in each category and the relative volume of each of the services used by the sub-population examined.
Results
The overall impact of price transparency on the commercial population will be $80.1 billion in 2025. This projection is the upper bound, most optimistic estimate. It assumes all shoppable services can be found, and the consumer can pay a negotiated price. The estimated savings from price transparency could be shared with the consumer and health plan. The HSA population and digital native population estimated impact values are less than the upper bound estimate with $17.6 and $26.7 billion of potential savings, respectively.
We examined the percent differences in the impact of price transparency for upper bound estimate population by 3 different subpopulations: income, region, and State. Table 1 presents the percent difference between status quo 2025 and the upper bound price transparency impact between 6 levels defined by the percent above or below the federal poverty line. Specifically, we present: <100% FPL, 100% to 137% FPL, 138% to 250% FPL, 251% to 400% FPL, 401% to 600% FPL, and >600% FPL.
Table 1.
Estimated Impact of Transparency for Private Insurance Market.
| By income levels | |||
|---|---|---|---|
| Federal poverty line (FPL) categories | Consumer/insurer savings by 2025 (Billions) | Consumers affected | Percent change savings from status quo (%) |
| <100% | $3.9 | 185 611 | −7.4 |
| 100% to 137% | $2.8 | 122 994 | −7.5 |
| 138% to 250% | $12.2 | 598 354 | −6.7 |
| 251% to 400% | $19.9 | 967 487 | −6.9 |
| 401% to 600% | $17.7 | 961 920 | −6.5 |
| >600% | $24.2 | 1 262 131 | −7.1 |
| Total | $80.7 | 4 098 497 | |
Concerning income, those at lower levels of income will have the most significant impact with a −7.4% (<100% Federal Poverty Level) to −7.5% (100%-137% Federal Poverty Level) impact. Overall, the total impact could be a 6.9% reduction for the whole privately insured population in the United States.
In terms of consumers affected, each FPL level has a population over 10 000 with the potential to be impacted by the 70 shoppable serves examined. The populations with the most significant number of consumers affected are associated with those above 250% federal poverty level. The population with the greatest impact will be those with incomes above 600% of the FPL.
The estimated impact of price transparency will vary significantly by region. As seen in Table 2, the region with the greatest impact in the US will be the Midwest, with a $20 billion potential savings and an 8% reduction in medical expenditure. The region with the lowest impact will be the South, with only a 5.8% reduction.
Table 2.
Estimated Impact of Transparency.
| By US region. | |||
|---|---|---|---|
| US federal census region | Consumer/insurer savings by 2025 (Billions) | Consumers affected | Percent change savings from status quo (%) |
| Midwest | $20.6 | 890 737 | −8.0 |
| Northeast | $17.5 | 855 741 | −7.5 |
| South | $24.9 | 1 528 539 | −5.8 |
| West | $17.7 | 823 480 | −7.0 |
| Total | $80.7 | 4 098 497 | |
The region of the US with the most consumer affected is the South. The Midwest, Northeast, and West all have a similar scale of consumers affected. A closer examination by State finds significant differences, driven mainly by the size of the population but also the volume of shoppable services used by that State’s population. As seen in Figure 1, the State with the most considerable potential impact is California. California has estimated $8.9 billion possible in savings from price transparency of shoppable services. The State with the most negligible financial impact of price transparency is Wyoming, with $0.14 billion in potential savings.
Figure 1.
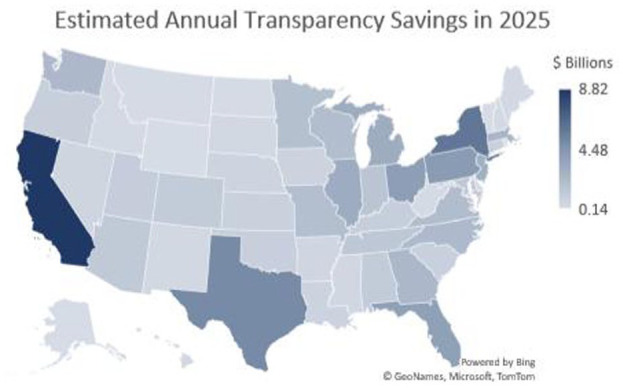
State-wide Impact of Price Transparency Savings.
To see the percent of the state change in expenditure relative to the status quo, we present Figure 2. The percent change results are inconsistent with Figure 1's estimated expenditure impact. As seen in Figure 2, all states have some level of impact with respect to percent change in estimated saving price transparency. The State with the largest impact is South Dakota, with an 11% estimated reduction in expenditure. The State with the most negligible price transparency impact is Mississippi.
Figure 2.
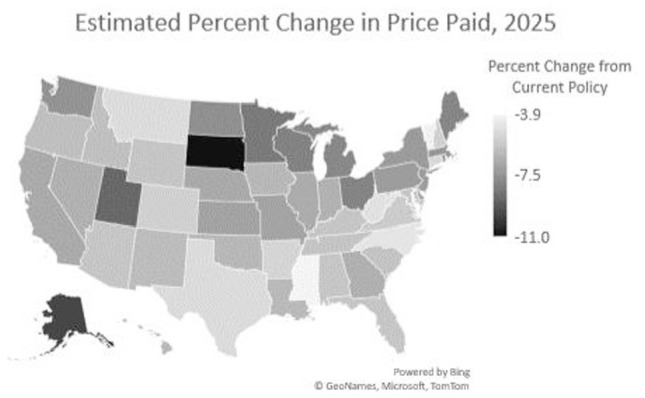
State-wide Percent Change of Price Transparency Savings
Discussion
There are 2 policy implications of this analysis. First, while all income levels are impacted—the most significant impact is for those with high incomes with more potential opportunities to have HSAs and high deductible health plans. Second, the HDHP distinction may not mean very much in the future due to the out-of-pocket expenses experienced by all health plans, not just HDHPs. A recent analysis by Brown shows that price information leads to a shift to lower-cost providers, especially for patients subject to a deductible.21 Given the growing use of deductibles it is likely that price transparency tools available to those outside of an experimental health plan setting could achieve the savings estimated in this analysis.
At the margin the income effect is greatest for lower income individuals. Without a survey of consumer preferences, it is challenging to understand why lower income cohorts would see more savings. The leading hypothesis for a subsequent analysis is the lower income group has a direct incentive for savings similar to using coupons for price reductions to stretch a tight budget.
There are several limitations to this analysis. First, the estimates reflect savings, but it is hard to know who will yield savings, the patient, the insurer, or the insured’s employer. But, if it is under the deductible, as in the HSA population, the consumer should yield all the savings. Second, we assume that competition will lower prices on average in all markets. If the savings accrues mostly to the insurer, the hope is that it will reduce the growth in year over year premiums. The extent to which that may be possible will need data following full implementation to create a possible estimate.
Savings for any party may not happen in more provider concentrated markets. The possibility of providers using the transparency data to level-up their reimbursement rate to the highest rate in a concentrated market with significant monopoly will be a concern to examine. The question, in the end, will be empirical—but at least the market change can be assessed at the provider level and monthly give the insurer price transparency rule disclosure requirements. One feature of the insurer transparency rule to examine anti-competitive effects on pricing is the monthly disclosure of prices to examine if providers do strategically respond to each other’s prices with an anti-competitive tactical decision. This information will also be valuable for anti-trust enforcement agencies that seek to regulate against anti-competitive behavior.
A third limitation is the extent of our sensitivity analysis without further prior information. For example, while we examine savings only to consumers with HDHP/HSA plans or digitally native consumers (age 26-42), we are not able to extend the analysis regarding how many consumers are expected to use these new tools, and what percentage of those will change their provider choice as a result. Until further evidence is given, it is challenging to estimate what second and third step responses will be without more data. Some of these multi-stage effects are estimated from the Parente, Feldman, and Sandy data—but the tools and populations were quite different than looking at shoppable services.
A fourth concern are unknown factors regarding the extent to which the price transparency tools will affect consumer behavior and thus impact savings. For instance, quality scores; implied quality (such as name recognition in a market); role of provider referrals in patients’ choice of specialist; etc.
Finally, the insurer price transparency rule will only be as good as the insurer compliance. A preliminary analysis of the end of December found the 5 largest national insurers in compliance with the insurer rule. While the size and complexity of the files may slow the rate of use by entrepreneurs, they could also offer a competitive advantage. Managing the size of the files may also provide a barrier to entry for rival tech firms with the skills to create and monetize the future “Expedia of medical care” for shoppable medical services.
Summary
In summary, a unique set of national data resources were used to understand the cost savings impact medical price transparency. This analysis suggests price transparency for shoppable services may yield significant savings. However, the impact will be limited by the adoption and capabilities of the current healthcare system to support shoppable services. A further consideration is who will get the savings. If most of these services are below an HDHP threshold, there is a good chance most savings will accrue to the consumer. Even more, savings are possible if these funds from tax-deferred Health Savings Accounts are used to purchase shoppable services. This analysis highlights the potential savings in 2025 of $80 billion.
That should be sufficient reason to try to make the rules in the 2 recent Administration’s Price Transparency Executive Orders codified into law as legislation.
Footnotes
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported from the Heritage Foundation.
Ethics and Consent statement: Our study did not require an ethical board approval because we used synthetic claims data with no patient identification and publicly available federal rules, regulations, and announcements.
ORCID iD: Stephen T. Parente  https://orcid.org/0000-0003-1155-9937
https://orcid.org/0000-0003-1155-9937
References
- 1. Arrow K. Uncertainty and the welfare economics of medical care. Am Econ Rev. 1963;53(5):941-973. [Google Scholar]
- 2. Cooper Z, Craig SV, Gaynor M, Van Reenen J. The price ain’t right? Hospital prices and health spending on the privately insured. Q J Econ. 2019;134(1):51-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Parente ST, Feldman R, Sandy L. Does transparency matter? The impact of provider quality and cost information on health care cost and preventive services use. J Health Med Econ. 2019;05(01):3. [Google Scholar]
- 4. Employer Health Benefits Survey. Kaiser family foundation. 2021. Accessed August 28, 2022. https://www.kff.org/report-section/ehbs-2021-summary-of-findings/
- 5. Executive Office of the President. Improving price and quality transparency in American healthcare to put patients first. 2019. Accessed August 28, 2022. https://www.federalregister.gov/documents/2019/06/27/2019-13945/improving-price-and-quality-transparency-in-american-healthcare-to-put-patients-first.
- 6. Nikpay S, Golberstein E, Neprash HT, Carroll C, Abraham JM. Taking the pulse of hospitals' response to the new price transparency rule. Med Care Res Rev. 2022;79(3):428-434. [DOI] [PubMed] [Google Scholar]
- 7. Wall Street Journal. Hospitals still not fully complying with federal price-disclosure rules. December 30, 2021. Accessed August 28, 2022. https://www.wsj.com/articles/hospital-price-public-biden-11640882507
- 8. Benavidez G, Frakt A. Price transparency in health care has been disappointing, but it doesn’t have to be. JAMA. 2019;322(13):1243-1244. [DOI] [PubMed] [Google Scholar]
- 9. Desai S, Hatfield LA, Hicks AL, et al. Offering a price transparency tool did not reduce overall spending among California public employees and retirees. Health Aff. 2017;36(8):1401-1407. doi: 10.1377/hlthaff.2016.1636 [DOI] [PubMed] [Google Scholar]
- 10. Robinson JC, Brown TT. Increases in consumer cost sharing redirect patient volumes and reduce hospital prices for orthopedic surgery. Health Aff. 2013;32(8):1392-1397. doi: 10.1377/hlthaff.2013.0188 [DOI] [PubMed] [Google Scholar]
- 11. Whaley C, Schneider Chafen J, Pinkard S, et al. Association between availability of health service prices and payments for these services. JAMA. 2014;312(16):1670-1676. doi: 10.1001/jama.2014.13373 [DOI] [PubMed] [Google Scholar]
- 12. Christensen HB, Floyd E, Maffett M. The only prescription is transparency: the effect of charge-price-transparency regulation on healthcare prices. Manage Sci. 2020;66(7):2861-2882. [Google Scholar]
- 13. Van Horn R, Laffer A, Metcalf R. The transformative potential for price transparency in healthcare: benefits for consumers and providers. Health Manag Policy Innovation. 2019;4(3):1-13. [Google Scholar]
- 14. CMS-Transparency-in-Coverage- CMS-9915-F. Center for medicare and medicaid services. Created October 27, 2020. Accessed August 28, 2022. https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/CMS-Transparency-in-Coverage-9915F.pdf
- 15. Desai SM, Shambhu S, Mehrotra A. Online advertising increased new Hampshire residents' use of provider price tool but not use of lower-price providers. Health Aff. 2021;40(3):521-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Whaley C, Sood N, Chernew M, Metcalfe L, Mehrotra A. Paying patients to use lower-priced providers. Health Serv Res. 2022;57(1):37-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gourevitch RA, Chien AT, Bambury EA, et al. Patterns of use of a price transparency tool for childbirth among pregnant individuals with commercial insurance. JAMA Netw Open. 2021;4(8):e2121410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. RevSpring. 70 CMS-specified shoppable services required by price transparency ruling. Created October 2, 2020. Accessed August 28, 2022. https://revspringinc.com/resources/blog/70-cms-specified-shoppable-services-required-by-price-transparency-ruling/
- 19. SynUSA. Synthetic health insurance analytic files. Created April 1, 2018. Accessed August 28, 2022. http://synusa.com/SynUSA_Overview.pdf
- 20. Synthetic Healthcare Database for Research (SyH-DR). Agency for healthcare research and quality. 2018. Accessed August 28, 2022. https://www.ahrq.gov/data/innovations/syh-dr.html
- 21. Brown ZY. Equilibrium effects of health care price information. Rev Econ Stat. 2019;101(4):699-712. [Google Scholar]


