Abstract
Background
The Stopping Elderly Accidents, Deaths and Injuries (STEADI) screening algorithm aligns with current fall prevention guidelines and is easy to administer within clinical practice. However, the stratification into low, moderate and high risk categories limits the meaningful interpretation of the fall-related risk factors.
Methods
Baseline measures from a modified STEADI were used to predict self-reported falls over 4 years in 3170 respondents who participated in the 2011–2015 National Health and Aging Trends Study. A point method was then applied to find coefficient-based integers and 4-year fall risk estimates from the predictive model. Sensitivity and specificity estimates from the point method and the combined moderate and high fall risk STEADI categories were compared.
Results
There were 886 (27.95%) and 387 (12.21%) respondents who were classified as moderate and high risk, respectively, when applying the stratification method. Falls in the past year (OR: 2.16; 95% CI: 1.61 to 2.89), multiple falls (OR: 2.94; 95% CI: 1.89 to 4.55) and a fear of falling (OR: 1.77; 95% CI: 1.45 to 2.16) were among the significant predictors of 4-year falls in older adults. The point method revealed integers that ranged from 0 (risk: 27.21%) to 44 (risk: 99.71%) and a score of 10 points had comparable discriminatory capacity to the combined moderate and high STEADI categories.
Conclusion
Coefficient-based integers and their risk estimates can provide an alternative interpretation of a predictive model that may be useful in determining fall risk within a clinical setting, tracking changes longitudinally and defining the effectiveness of an intervention.
INTRODUCTION
Nearly one out of every three older adults fall each year1; however, fewer than 25% of fall-related injuries are reported and older adults are completing wellness visits without fall prevention strategies being discussed by their healthcare provider.2 Fall risk screening includes measures of physical performance,3 4 multi-item risk indices and questionnaires,5 or a combination. Screening may be used to directly estimate fall risk, to better understand conditions that predict falls (eg, frailty)6 or to evaluate the likelihood of an adverse post-fall outcome (eg, functional decline, decreased quality of life).5 The timely identification of risk factors is essential to determine an appropriate and collaborative care plan.
One of the most predictive fall-related risk factors is a history of falls. It is estimated that those who fell previously may be at a 1.5–3 times higher risk for an injurious fall.7 Self-reported falls can provide reliable estimations, but fall history may be under-reported when compared with prospective calendar reports—the gold standard to record falls.8 Fear of falling is another self-report measure that has been used to predict future and frequent falls and can be exacerbated by a history of falls.9 10 Falls efficacy scales are often used to better discriminate between different levels of fear and activity types,11 12 but simply asking the older adult about their fear can be effective. Functional performance tests are often used with fall history and falling-related fear, but determining the cut-off points that best identify risk can be problematic. For example, discrepancies in the Timed Up and Go range from cut-off values ≥12 s13 to ≥16 s14 and 12 s in the five-repetition sit-to-stand test may be most predictive of older adults who suffered from multiple falls even though 30 s is commonly used.15 Frail elderly or those with dementia may have difficulty completing the functional tests; hence, subjective evaluations by health professionals may also be warranted.13 16
The CDC’s Stopping Elderly Accidents, Deaths and Injuries (STEADI) screening algorithm aligns with current fall prevention guidelines.17 It is an easy-to-administer tool created to integrate within a healthcare provider’s workflow using survey questions and functional assessments.18 The STEADI algorithm has also been modified for survey data by Lohman et al19 and validated in a nationally representative sample of older adults using data from the National Health and Aging Trends Study (NHATS). Respondents in this study had a 2.62 (95% CI: 2.29 to 2.99) and 4.76 (95% CI: 3.51 to 6.47) higher odds of experiencing a fall over 4 years if classified as moderate or high risk, respectively.19 The most useful screening tools will be able to accurately provide risk estimates, assist healthcare providers in their decision-making process and bring self-awareness to older adults who are most in need of a referral to a fall prevention programme. Therefore, the current study proposes using the point method developed by Sullivan et al20 to further the work by Lohman et al.19 The point method is a widely used statistical technique to simplify complex predictive models and to make screening more accurate and efficient within the healthcare setting. The technique by Sullivan et al20 has been cited in over 730 research articles, but has primarily been the focus for cardiovascular, respiratory, demography and surgery risk in geriatrics/gerontology. There were two studies that used this technique for frailty21 and fracture risk,22 but older adult fall-related risk profiles are lacking. The STEADI algorithm and the NHATS longitudinal, publicly available data make it possible to apply the point system to a nationally representative sample. The purpose of this study was to integrate the work from Lohman et al19 with the statistical techniques from Sullivan et al20 to determine fall risk estimates in community-dwelling older adults. This study aimed to test the hypothesis that at least one coefficient-based integer and 4-year fall risk estimate would have a comparable sensitivity and specificity to the combined moderate and high risk STEADI categories in predicting falls over 4 years, and that the continuous score would offer more information than stratification.
METHODS
Sample
This research used a nationally representative sample of Medicare beneficiaries from the NHATS. Led by a multidisciplinary research team at the Johns Hopkins Bloomberg School of Public Health and funded by the National Institute on Aging (U01AG032947), the NHATS highlights the significance of physical, cognitive, social and environmental influence on the ageing process through in-person questionnaires and physical assessments. It exists to help researchers and policymakers better understand the ageing process in order to maximise longevity and quality of life in older adults.23 The current study includes respondents who had baseline data collected in 2011 with 4 years of follow-up data. Respondents were excluded if the data were not available, they lived in a nursing home or unspecified residential facility, or had a proxy respond to the survey with insufficient fall risk information.
Measures
Self-reported falls during the 4-year follow-up period were used as the primary outcome measure. This binary variable was coded as 1 if a respondent reported a fall when asked ‘In the last 12 months, have you fallen down?’ Those who did not report any falls were coded 0 and considered non-fallers.
The self-reported and physical function measures from the modified STEADI fall risk screening algorithm were used as the predictor variables for determining the points and 4-year fall risk estimates, but descriptive characteristics were reported using the low, moderate and high fall risk STEADI stratification (figure 1). The STEADI stratification method classifies respondents as low risk if they did not report a fall in the past year, were not worried about falling, or did not feel unsafe or unsteady while standing or walking. Moderate risk was recorded if the respondent answered ‘yes’ to any of the previous questions, but passed the chair-stand and four-stage balance tests. Moderate risk was also used to describe those who did not pass the strength or balance assessments, but did not have multiple falls or a past hip fracture. High fall risk classifications were given to respondents who did not pass the strength and balance tests, and reported multiple falls in the past year or a hip fracture since they were 50 years old.
Figure 1.
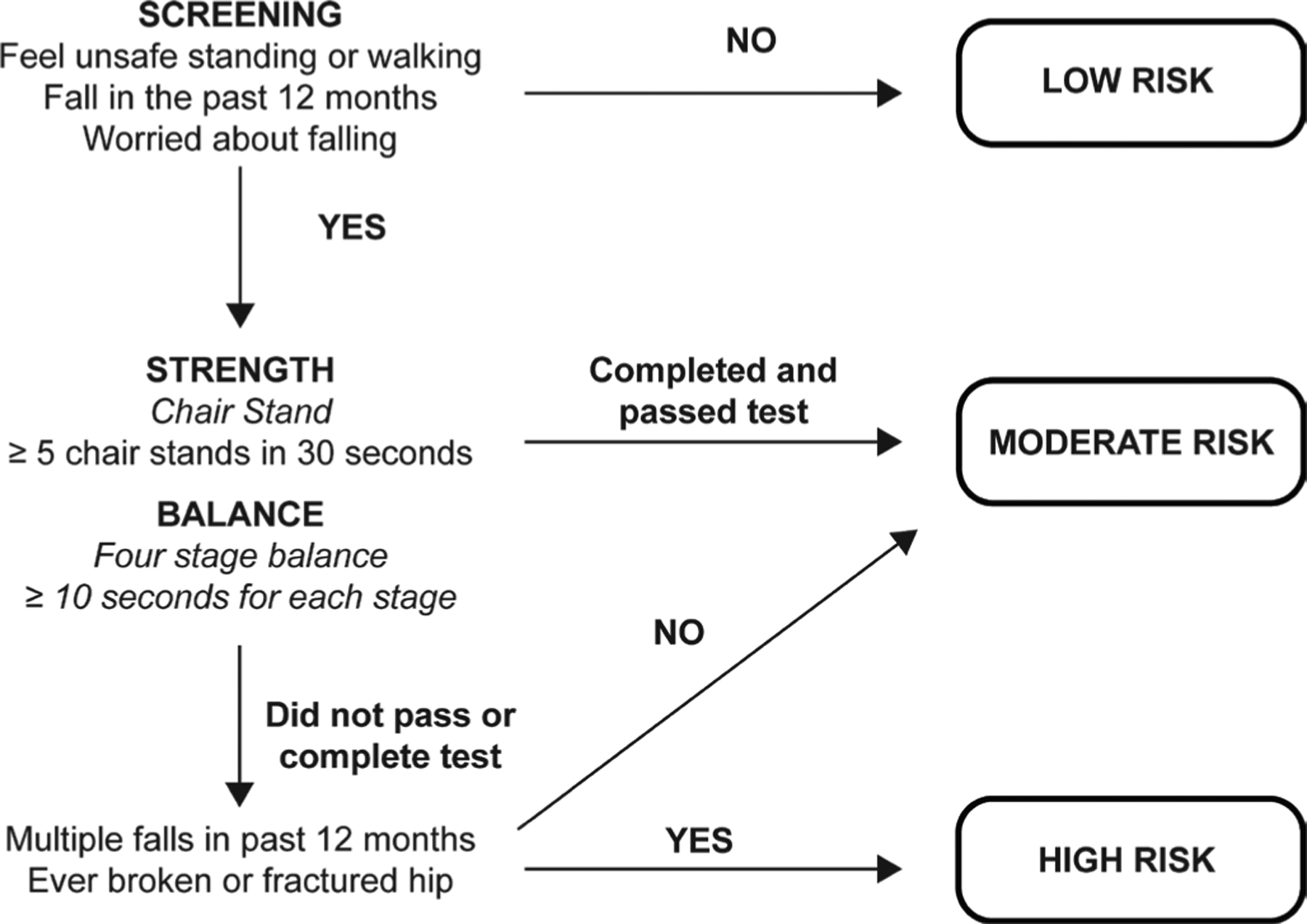
Modified Stopping Elderly Accidents, Deaths and Injuries framework.19
Covariates in the regression model were kept minimal to ensure that the points and risk estimates were useful and easy to administer in settings with fall prevention interests. Certain demographics were included since these measures are often recorded in patient electronic health records or are easily identifiable through patient interaction. Specifically, age categories,1 gender9 10 and race/ethnicity24 25 were included in the analysis since these are common fall risk influencers. The methodology to calculate the points and risk estimates also relies on a continuous measure to be used as a constant. Age has been commonly used, but age is reported categorically in the NHATS data. Therefore, a 0.05 s increase in the 3-metre walk time was used to correspond with a one point increase in the risk score since gait speed has been linked to falls and other adverse outcomes in older adults.3
Analysis
The analysis focused on expanding the work by Lohman et al19 through the application of a methodology used to calculate integer-based risk scores. Predictive models, such as logistic regressions, offer analytical techniques that quantify the impact of measurable and modifiable risk factors in the development of a disease or the occurrence of an event. Using the Framingham Heart Study for cardiovascular risk, Sullivan et al20 suggested a points system to make these complex statistical models useful to clinicians and their decision-making process. The points system used categories that reflected clinically meaningful risk factor states and determined a referent risk factor profile for each risk category. The points were determined using the equation:
where βij is the coefficient for the predictor variable, Wij is the midrange numerical value of the predictor variable, WREF is the category chosen as the reference for each predictor variable and B is a constant.
The points were rounded to the nearest negative or positive integer and then risk estimates expressed as a decimal or percentage were generated by adding the intercept, the continuous risk factors and the point total multiplied by the constant using the equation:
where X1 represents the 3-metre walk time continuous measure and the point total multiplied by the constant B approximates . The risk estimate for each point total was estimated using the equation:
The final step in the analysis compared the sensitivity and specificity from the points and risk estimates to the combined moderate and high fall risk classifications from the modified STEADI algorithm to determine which point value had a similar discriminatory capacity when classifying older adults who fell within the 4-year follow-up period. Stata V. 14.2 (StataCorp 2015; Stata Statistical Software: Release 14; College Station, Texas, USA) was used for this analysis.
RESULTS
Demographic characteristics are presented in table 1 for the 3170 included respondents. Based on the modified STEADI stratification, the majority of the respondents were classified as low fall risk (N=1897; 59.84%) with 27.95% (N=886) and 12.21% (N=387) being classified as moderate and high fall risk, respectively. The percentages of whites, women and those 80 years and older were greater in the moderate and high risk categories when compared with low fall risk. The fall risk progression from low to high also yielded increased 3-metre walk times and reduced gait speed; higher percentages of those who had falls and multiple falls in the past year; and reduced completion of the chair-stand and four-stage balance tests.
Table 1.
Baseline characteristics by stratified STEADI fall risk classifications using 2011 data from the National Health and Aging Trends Study
| Fall risk | |||
|---|---|---|---|
| Low (N=1897) | Moderate (N=886) | High (N=387) | |
| Age categories (years) | |||
| 65–69 | 481 (25.36) | 159 (17.95) | 87 (22.48) |
| 70–74 | 470 (24.78) | 179 (20.20) | 73 (18.86) |
| 75–79 | 407 (21.45) | 203 (22.91) | 79 (20.41) |
| 80–84 | 325 (17.13) | 185 (20.88) | 82 (21.19) |
| 85+ | 214 (11.28) | 160 (18.06) | 66 (17.05) |
| Race/ethnicity | |||
| White | 1394 (73.48) | 671 (75.73) | 305 (78.81) |
| African American | 384 (20.24) | 146 (16.48) | 56 (14.47) |
| Hispanic | 76 (4.01) | 51 (5.76) | 19 (4.91) |
| Other | 43 (2.27) | 18 (2.03) | 7 (1.81) |
| Gender | |||
| Male | 905 (47.71) | 277 (31.26) | 136 (35.14) |
| Female | 992 (52.29) | 609 (68.74) | 251 (64.86) |
| Fear of falling | 0 (0.00) | 597 (67.38) | 215 (55.56) |
| Fell past year | 0 (0.00) | 392 (44.24) | 367 (94.83) |
| Falls ≥2 last year | 0 (0.00) | 9 (1.02) | 348 (89.92) |
| Prior broken hip | 41 (2.16) | 2 (0.23) | 66 (17.05) |
| 3-metre walk* | 3.90±1.84 | 4.78±3.61 | 5.30±3.53 |
| Gait speed† | 0.87±0.27 | 0.76±0.27 | 0.71±0.29 |
| Chair-stand test‡ | 190 (10.02) | 199 (22.46) | 101 (26.10) |
| Balance test§ | 1500 (79.07) | 769 (86.79) | 349 (90.18) |
| Side by side | 13 (0.69) | 44 (4.97) | 22 (5.68) |
| Semitandem | 122 (6.43) | 107 (12.08) | 73 (18.86) |
| Full-tandem | 432 (22.77) | 268 (30.25) | 126 (32.56) |
| One-leg, eyes open | 976 (51.45) | 394 (44.47) | 153 (39.53) |
Expressed as frequency (percentage).
Three-metre walk time measured in mean±SD seconds.
Gait speed measured in mean±SD metres per second.
Did not complete or pass the chair-stand test.
Did not pass the overall balance test (hold each pose ≥10 s) including the side by side, semitandem, full-tandem and one-leg, eyes open stands.
STEADI, Stopping Elderly Accidents, Deaths and Injuries.
Results of the prediction model with the coefficient-based point values are presented in table 2. Coefficients, ORs, p values and 95% CIs are reported. Falls in the past year (OR: 2.16; 95% CI: 1.61 to 2.89), multiple falls in the past year (OR: 2.94; 95% CI: 1.89 to 4.55) and a fear of falling (OR: 1.77; 95% CI: 1.45 to 2.16) were significant predictors of 4-year falls in community-dwelling older adults. Other significant predictors included not able to complete the chair-stand test (OR: 1.36; 95% CI: 1.04 to 1.79), ages 75–79 (OR: 1.40; 95% CI: 1.11 to 1.78) or 80–84 years (OR: 1.78; 95% CI: 1.39 to 2.27), and being white (OR: 1.92; 95% CI: 1.57 to 2.34). The higher point values in table 2 reflect the increasing coefficients and ORs. The referent profile identified was an African American man aged 65–69 years who had no known fall risk indicators and represented a risk score of 0 points. This profile was chosen because white women and those who are older are usually a higher fall risk. The theoretical range of the point values was determined and risk estimates were calculated for each score (figure 2).
Table 2.
Prediction of 4-year fall risk (2012–2015) in community-dwelling older adults using the National Health and Aging Trends Study baseline measures included in the modified STEADI screening algorithm with risk score derived points (N=3170)
| β | OR | Points | P value | 95% CI | |
|---|---|---|---|---|---|
| Feel unsafe to stand | 0.24 | 1.27 | 2 | 0.52 | 0.61 to 2.63 |
| Fell past year | 0.77 | 2.16 | 5 | <0.001 | 1.61 to 2.89 |
| Fear of falling | 0.57 | 1.77 | 4 | <0.001 | 1.45 to 2.16 |
| 4-stage balance* | 0.08 | 1.08 | 1 | 0.56 | 0.82 to 1.43 |
| Chair-stand† | 0.31 | 1.36 | 2 | 0.03 | 1.04 to 1.79 |
| ≥2 falls past year | 1.08 | 2.94 | 7 | <0.001 | 1.89 to 4.55 |
| Past broken hip | 0.13 | 1.13 | 1 | 0.70 | 0.59 to 2.20 |
| Age category (years) | |||||
| 65–69 | Reference | 0 | |||
| 70–74 | 0.19 | 1.20 | 1 | 0.11 | 0.96 to 1.51 |
| 75–79 | 0.34 | 1.40 | 2 | 0.005 | 1.11 to 1.78 |
| 80–84 | 0.57 | 1.78 | 4 | <0.001 | 1.39 to 2.27 |
| ≥85 | 0.25 | 1.28 | 2 | 0.09 | 0.97 to 1.70 |
| Ethnicity | |||||
| White | 0.65 | 1.92 | 4 | <0.001 | 1.57 to 2.34 |
| African American | Reference | 0 | |||
| Hispanic | 0.20 | 1.22 | 1 | 0.33 | 0.81 to 1.84 |
| Other | 0.56 | 1.75 | 4 | 0.08 | 0.93 to 3.29 |
| Gender | |||||
| Male | Reference | 0 | |||
| Female | 0.11 | 1.11 | 1 | 0.26 | 0.92 to 1.35 |
| 3-metre walk (seconds) | 0.03 | 1.03 | 0.25 | 0.98 to 1.09 | |
| ≤5.05 | 0 | ||||
| 5.06–6.38 | 1 | ||||
| ≥6.39 | 2 | ||||
Complex survey weights were used to allow the data to be nationally representative of the US population.
95% CIs are based on the ORs and not the coefficients.
Three-metre walk is a continuous variable that was used as a constant and separated by categories to assign point values.
Past broken hip was any fracture of the hip since the age of 50 years.
Fear of falling was a self-reported fear by the respondent.
Did not pass the overall balance test (hold each pose ≥10 s).
Did not complete or pass the chair-stand test.
STEADI, Stopping Elderly Accidents, Deaths and Injuries.
Figure 2.
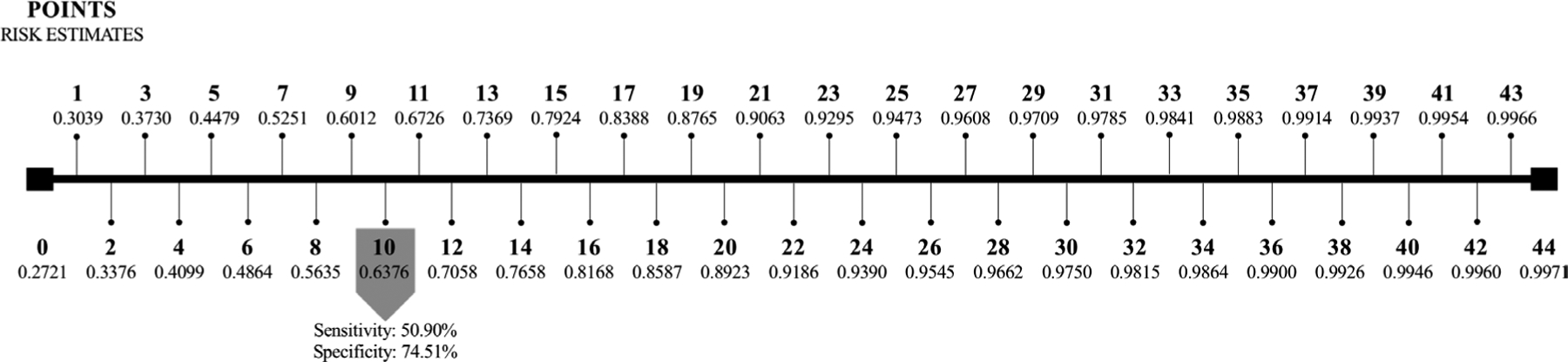
Four-year single fall risk estimates using an application of the point system and the modified STEADI algorithm in the 2011–2015 National Health and Aging Trends Study. The 48.90% sensitivity and 76.51% specificity for the combined moderate and high STEADI fall risk classifications were comparable to a score of 10 points. STEADI, Stopping Elderly Accidents, Deaths and Injuries.
Points ranged from 0 points (4-year fall risk: 27.21%) to 44 points (4-year fall risk: 99.71%) with a mean of 6.39±2.46, 12.50±3.35 and 21.16±3.96 points for the low, moderate and high STEADI classifications, respectively. The distribution of points by low and combined moderate and high STEADI fall risk can be seen in figure 3. Ten points (4-year fall risk: 63.76%) corresponded with a similar sensitivity (50.90%) and specificity (74.51%) as the combined moderate and high STEADI fall risk categories (sensitivity: 48.90%; specificity: 76.51%) in correctly classifying those who fell during the 4-year follow-up period.
Figure 3.
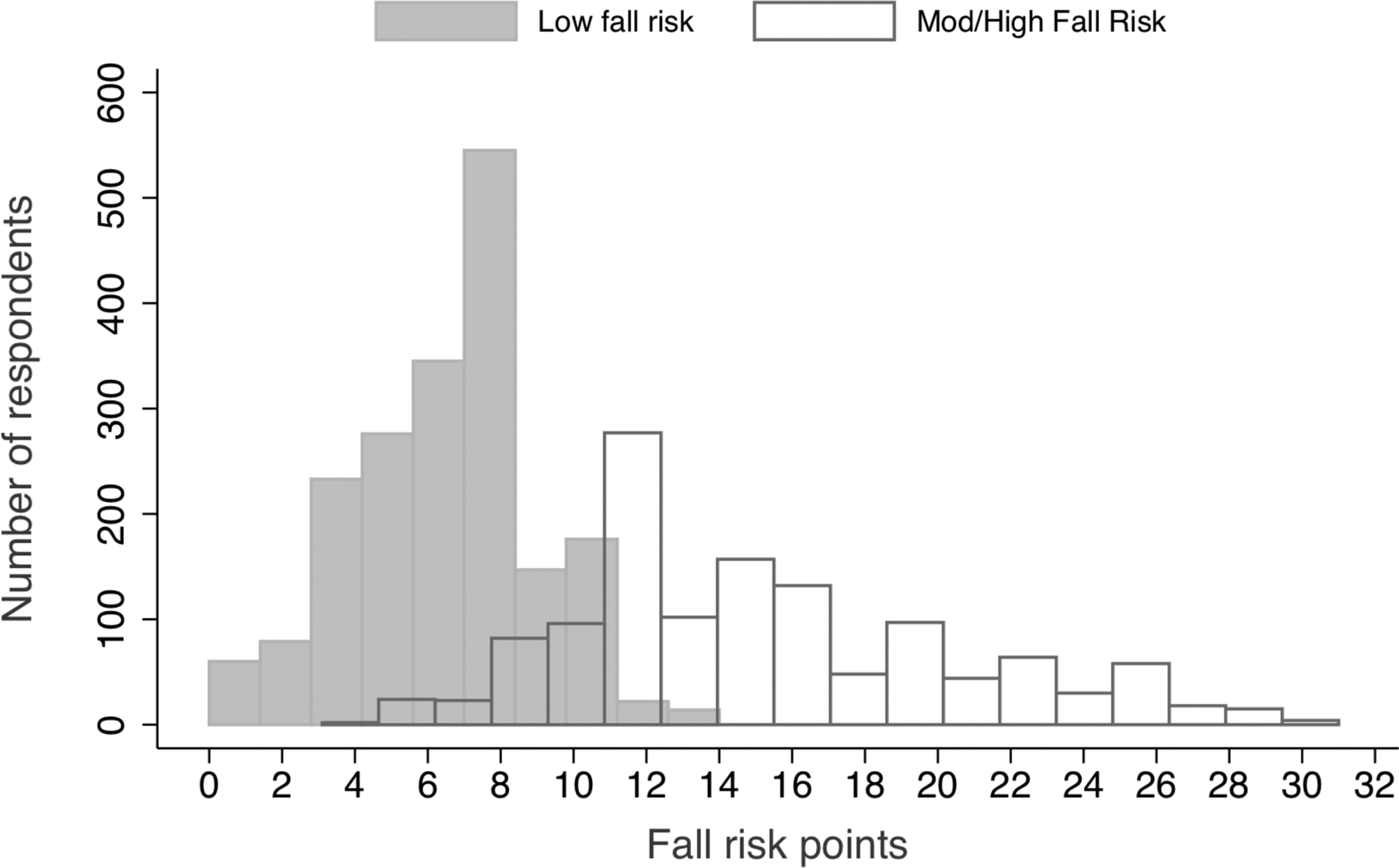
Point totals by STEADI low and combined moderate and high fall risk categories from the 2011–2015 National Health and Aging Trends Study. STEADI, Stopping Elderly Accidents, Deaths and Injuries.
DISCUSSION
Wilson et al26 first used the point method to predict coronary heart disease in the Framingham study. Their publication has been cited nearly 6000 times by researchers who have widely accepted and applied this method. Exploring the use of the point method for fall prediction in community-dwelling older adults is novel and the current study presented both the coefficient-based integers and risk estimates associated with falls over 4 years. It also compared the points and risk estimates to the moderate risk and high risk STEADI categories identified by Lohman et al.19 Healthcare providers may receive inadequate training in fall risk detection, so simplifying prediction models to aid decision support can greatly influence whether an older adult is referred into a fall prevention programme.27 It also helps the healthcare team interpret and use the coefficients or ORs from these predictive models. Additionally, the ability of the point system to be sensitive to intraindividual changes when compared with stratification makes it a clinically relevant screening tool to monitor fall risk in older adults.
Our study found that the demographics, walk time, and the modified STEADI screening algorithm had a sensitivity of 48.90% and a specificity of 76.51% when predicting falls over 4 years. The sensitivity was lower and the specificity was higher when compared with the study by Lohman et al19 using the same data source and timeframe (sensitivity/specificity: 65%). This may be due to the choice in the current study to exclude those respondents who did not have 4 years of follow-up data (N=3603) or valid walk time measurements (N=483). Nevertheless, our study still demonstrated modest discriminatory capacity in the prediction of falls over 4 years and identified a score of 10 points to be a similar sensitivity (50.90%) and specificity (74.51%) to the combined moderate and high STEADI risk categories.
Risk indicators including a fall within the past year (OR: 2.16; 95% CI: 1.61 to 2.89), multiple falls (OR: 2.94; 95% CI: 1.89 to 4.55) and a self-reported falling-related fear (OR: 1.77; 95% CI: 1.45 to 2.16) were among the strongest predictors for falls. This is consistent with past research.7 9 Healthcare providers should be encouraged to ask older adults whether they have experienced a fall or have falling-related fears due to the predictive ability and ease of reporting for these measures. Age between 75–79 years and 80–84 years was also a significant predictor in this study. ORs increased with each age category except for those respondents ≥85 years. The slight decrease in odds in this age category may be partially due to restricted mobility and fewer risky activities that could lead to falls. Additionally, being white and having poor strength in the lower extremities were strong fall predictors with a 92% and 36% increased odds, respectively, of a fall over the 4 years.
Fall risk is complex and multifaceted; therefore, it is difficult to design an instrument that captures all the fall-related risk factors and is still easy to administer within a clinical setting. For example, the Home Falls and Accidents Screening Tool was designed to capture fall risk in community-dwelling older adults at home. It was developed to be a brief and easily administered instrument that captures the risk associated with clutter, unsafe home environments and difficulty in daily activities. However, it does not account for fall history, physical strength, mobility and balance.28 The STEADI framework is also focused on risk inside the home.17 18 Home hazards may include loose rugs or carpet, steps with unstable or missing handrails, or clutter that makes walking through the house difficult. Research suggests that more than 50% of falls occur outside the home,29 which suggests a need to develop screening methods that incorporate outdoor fall-related risk factors. Nevertheless, screening tools may choose to focus on specific components of risk to not dilute the sensitivity and specificity of the instruments since there are many fall-related risk factors.
The point method can also be applied to adverse outcomes (eg, fall-related injuries, new-onset disability or loss of independent living) to help guide healthcare providers in their post-fall care plan. Mehta et al30 created a clinical index to stratify older adults by new-onset disability risk using age, baseline dependence in ≥three instrumental activities of daily living, impaired mobility at baseline, dependence in activities of daily living at the time of admission, acute stroke or metastatic cancer, severe cognitive impairment and albumin levels less than 3.0 g/dL. The points ranged from 0 to 7 with estimates or risk between 6% and 87%, respectively. Additionally, a study by Toosizadeh et al31 used elbow range of motion as well as flexion and extension speed evaluated through sensor-based movements to predict frailty in older adults. Frailty is a common predictor of falls and these researchers developed and validated the upper-extremity function index using the point method.31
This study has several important limitations to consider. First, the included predictor variables do not represent all the fall-related risk factors. These measures were selected because they would be easy to identify in a clinical setting with minimal time and space requirements. Several of the measures (eg, age, gender, race/ethnicity and fall history) would be identifiable from the electronic health record. Additional fall-related risk factors may have altered the predictive capacity of the models. Second, this study used a cross-sectional design even with the availability of the longitudinal data. Longitudinal data may provide a better understanding of how the points and risk estimates change over time and represent an exciting opportunity for future research. The continuous points and risk estimates may allow researchers to identify longitudinal changes in fall risk and provide information on the success of an intervention. Finally, this study identified points and their 4-year fall risk estimates, but it did not aim to evaluate the validity or reliability of the screening tool. It is unknown whether the instrument based on the point method can accurately and reliably predict falls in other study populations. Future research should evaluate the use of this point system in an intervention, a longitudinal study, or with older adults who may have higher fall risk such as those who are frail or have dementia; apply the point system to outdoor, environmental or other intrinsic fall-related risk factors; or validate the modified STEADI screening algorithm points and risk estimates using prospective calendar reports for falls in older adults.
CONCLUSION
The modified STEADI screening algorithm is quick and easy to administer, but the stratification used (ie, low, moderate or high categories) does not provide adequate information regarding fall risk. Instead, coefficient-based integers and their risk estimates can provide an alternative interpretation of a predictive model that may be useful in determining fall risk. This study recommends a cut-off score of 10 points using the point method in order to effectively screen older adults for fall risk within clinical or community settings.
What is already known on the subject
Unintentional falls occur in nearly 33% of community-dwelling older adults; however, older adults are often leaving primary care clinics with unidentified risk factors or without an appropriate fall prevention strategy as part of their care plan. Fall risk screening tools exist, but they generally rely on stratification into risk categories.
What this study adds
This study applies a point method to offer healthcare providers another way of classifying fall risk. The coefficient-based integers and risk estimates from a predictive model provide a continuous measure that can be used to develop actionable and responsive steps in reducing fall risk as part of an older adult’s care plan.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Data availability statement
Data are available in a public, open access repository at https://www.nhats.org/.
REFERENCES
- 1.Nilsson M, Eriksson J, Larsson B, et al. Fall risk assessment predicts Fall-Related injury, hip fracture, and head injury in older adults. J Am Geriatr Soc 2016;64:2242–50. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman GJ, Ha J, Alexander NB, et al. Underreporting of fall injuries of older adults: implications for wellness visit fall risk screening. J Am Geriatr Soc 2018;66:1195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eagles D, Perry JJ, Sirois M-J, et al. Timed up and go predicts functional decline in older patients presenting to the emergency department following minor trauma†. Age Ageing 2017;46:214–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xue Q-L, Walston JD, Fried LP, et al. Prediction of risk of falling, physical disability, and frailty by rate of decline in grip strength: the women’s health and aging study. Arch Intern Med 2011;171:1119–21. [DOI] [PubMed] [Google Scholar]
- 5.Ishimoto Y, Wada T, Kasahara Y, et al. Fall risk index predicts functional decline regardless of fall experiences among community-dwelling elderly. Geriatr Gerontol Int 2012;12:659–66. [DOI] [PubMed] [Google Scholar]
- 6.Díaz de León González E, Gutiérrez Hermosillo H, Martinez Beltran JA, et al. Validation of the frail scale in Mexican elderly: results from the Mexican health and aging study. Aging Clin Exp Res 2016;28:901–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poss JW, Hirdes JP. Very frequent fallers and future fall injury: continuous risk among community-dwelling home care recipients. J Aging Health 2016;28:587–99. [DOI] [PubMed] [Google Scholar]
- 8.Mackenzie L, Byles J, D’Este C. Validation of self-reported fall events in intervention studies. Clin Rehabil 2006;20:331–9. [DOI] [PubMed] [Google Scholar]
- 9.Delbaere K, Crombez G, Vanderstraeten G. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing 2004;33:368–73. [DOI] [PubMed] [Google Scholar]
- 10.LeBouthillier DM, Thibodeau MA, Asmundson GJG. Severity of fall-based injuries, fear of falling, and activity restriction: sex differences in a population-based sample of older Canadian adults. J Aging Health 2013;25:1378–87. [DOI] [PubMed] [Google Scholar]
- 11.Hauer KA, Kempen GIJM, Schwenk M, et al. Validity and sensitivity to change of the falls efficacy scales international to assess fear of falling in older adults with and without cognitive impairment. Gerontology 2011;57:462–72. [DOI] [PubMed] [Google Scholar]
- 12.Hauer K, Yardley L, Beyer N, et al. Validation of the falls efficacy scale and falls efficacy scale international in geriatric patients with and without cognitive impairment: results of self-report and Interview-Based questionnaires. Gerontology 2010;56:190–9. [DOI] [PubMed] [Google Scholar]
- 13.Olsson Möller U, Kristensson J, Midlöv P, et al. Predictive validity and cut-off scores in four diagnostic tests for falls – a study in frail older people at home. Phys Occup Ther Geriatr 2012;30:189–201. [Google Scholar]
- 14.Shimada H, Suzukawa M, Tiedemann A, et al. Which neuromuscular or cognitive test is the optimal screening tool to predict falls in frail community-dwelling older people? Gerontology 2009;55:532–8. [DOI] [PubMed] [Google Scholar]
- 15.Tiedemann A, Shimada H, Sherrington C, et al. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing 2008;37:430–5. [DOI] [PubMed] [Google Scholar]
- 16.Shimada H, Suzukawa M, Ishizaki T, et al. Relationship between subjective fall risk assessment and falls and fall-related fractures in frail elderly people. BMC Geriatr 2011;11:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevens JA, Phelan EA. Development of STEADI: a fall prevention resource for health care providers. Health Promot Pract 2013;14:706–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sarmiento K, Lee R. STEADI: CDC’s approach to make older adult fall prevention part of every primary care practice. J Safety Res 2017;63:105–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lohman MC, Crow RS, DiMilia PR, et al. Operationalisation and validation of the stopping elderly accidents, deaths, and injuries (STEADI) fall risk algorithm in a nationally representative sample. J Epidemiol Community Health 2017;71:1191–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sullivan LM, Massaro JM, D’Agostino RB. Presentation of multivariate data for clinical use: the Framingham study risk score functions. Stat Med 2004;23:1631–60. [DOI] [PubMed] [Google Scholar]
- 21.Gray WK, Orega G, Kisoli A, et al. Identifying frailty and its outcomes in older people in rural Tanzania. Exp Aging Res 2017;43:257–73. [DOI] [PubMed] [Google Scholar]
- 22.Graham-Steed TR, Soulos PR, Dearing N, et al. Development and validation of a prognostic index for fracture risk in older men undergoing prostate cancer treatment. J Geriatr Oncol 2014;5:343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.NHATS Public Use Data. (rounds 1–5), sponsored by the National Institute on aging (grant number NIa U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg school of public health. Available: www.nhats.org
- 24.Schiller JS, Kramarow EA, Dey AN, et al. Fall injury episodes among noninstitutionalized older adults: United States, 2001–2003. Adv Data 2007;392:1–16. [PubMed] [Google Scholar]
- 25.Gorina Y, Hoyert D, Lentzner H, et al. Trends in causes of death among older persons in the United States. Aging Trends 2005:1–12. [PubMed] [Google Scholar]
- 26.Wilson PWF, D’Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837–47. [DOI] [PubMed] [Google Scholar]
- 27.Caton C, Wiley MK, Zhao Y, et al. Improving internal medicine residents’ falls assessment and evaluation: an interdisciplinary, multistrategy program. J Am Geriatr Soc 2011;59:1941–6. [DOI] [PubMed] [Google Scholar]
- 28.Vu T-V, Mackenzie L The inter-rater and test-retest reliability of the home falls and accidents screening tool. Aust Occup Ther J 2012;59:235–42. [DOI] [PubMed] [Google Scholar]
- 29.Lai P-C, Wong W-C, Low C-T, et al. A small-area study of environmental risk assessment of outdoor falls. J Med Syst 2011;35:1543–52. [DOI] [PubMed] [Google Scholar]
- 30.Mehta KM, Pierluissi E, Boscardin WJ, et al. A clinical index to stratify hospitalized older adults according to risk for new-onset disability. J Am Geriatr Soc 2011;59:1206–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Toosizadeh N, Wendel C, Hsu C-H, et al. Frailty assessment in older adults using upper-extremity function: index development. BMC Geriatr 2017;17:117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository at https://www.nhats.org/.


