Abstract
Background
Caregiving is a strong source of stress and leads the family caregiver to experience the burden of being responsible for the care of a severely mentally ill family member. The Burden Assessment Scale (BAS) assesses burden in family caregivers. This study aimed to analyze the psychometric properties of the BAS in a sample of family caregivers of people diagnosed with Borderline Personality Disorder (BPD).
Methods
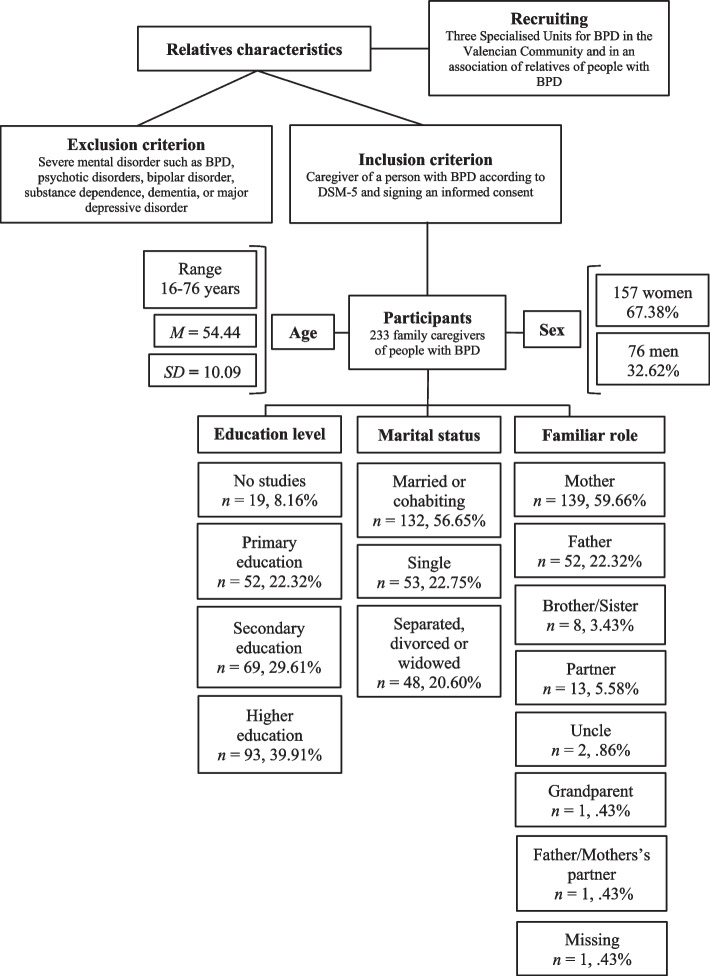
Participants were 233 Spanish family caregivers (157 women and 76 men aged between 16–76 years old, M = 54.44, SD = 10.09) of people diagnosed with BPD. The BAS, the Multicultural Quality of Life Index, and the Depression Anxiety Stress Scale-21 were used.
Results
An exploratory analysis resulted in a three-factor 16-item model (Disrupted Activities; Personal and Social Dysfunction; Worry, Guilt, and Being Overwhelmed) with an excellent fit (χ2(101) = 56.873, p = 1.000, CFI = 1.000, TLI = 1.000, RMSEA = .000, SRMR = .060), good internal consistency (ω = .93), a negative correlation with quality of life, and a positive correlation with anxiety, depression, and stress.
Conclusion
The model obtained for the BAS is a valid, reliable, and useful tool for assessing burden in family caregivers of relatives diagnosed with BPD.
Keywords: Family caregivers, Burden, Burden Assessment Scale, Borderline personality disorder, Psychometric properties
Introduction
Caring for people diagnosed with a severe mental disorder (SMD) usually falls on their relatives, for whom such responsibility is a strong source of stress and leads them to experience burden (e.g. [26]). Burden includes two dimensions, objective (financial problems, limitations on personal activity, household disruption, and social interactions) and subjective (shame, stigma, guilt, resentment, grief, and worry) (e.g. [35]), and can be conditioned by many variables (e.g. [40, 42]).
Family caregiving of people diagnosed with borderline personality disorder
Bailey and Grenyer [4], in a review of several studies about burden and support needs of carers of people with borderline personality disorder (BPD) [16, 18–20, 39], found that (1) the caregivers experienced elevated objective and subjective burden, grief, impaired empowerment, and mental health problems, including depression and anxiety, and (2) scores on both objective and subjective burden were half a standard deviation above the mean, compared to caregivers of inpatients with other SMD (e.g. schizophrenia). These authors concluded that caring for a relative diagnosed with BPD seems to be harder and more burdensome than caring for a family member with another SMD, due to the psychopathological characteristics of BPD [2].
Kay et al. [27] found that family members who were caring for their relatives diagnosed with BPD: (1) described their relatives as experiencing emotional, behavioral, interpersonal, and self-dysregulation problems; (2) expressed negative feelings towards their relatives; (3) experienced social humiliation, financial strain, and marital discord; (4) wanted to move forward and improve their mental health; (5) experienced a challenging process of adaptation and coping; and (6) experienced a quest for harmony and integration. These authors concluded that being knowledgeable about the relative’s mental disorder is quite important because it can empower the caregiver. This conclusion, however, contrasts with the results obtained by Hoffman et al. [18], who found that the greater the knowledge about the BPD, the higher the level of family members’ burden, depression, distress, and hostility toward their relatives diagnosed with BPD. In this regard, “there is a consensus on the necessity that relatives of BPD subjects should have the opportunity to receive state-of-the-art, evidence-based information on BPD and its available treatments, in order to destigmatize the BPD diagnosis as well as the role of the family in BPD development” ([14], 3) [18–20].
Jørgensen et al. [26] found that higher BPD severity at the end of mentalization-based treatment (one year) in adolescents predicted family caregiver burden, and that biological mothers could be more burdened than other types of caregivers. These authors suggested that caregivers, especially biological mothers, of adolescents with more severe levels of BPD could be particularly vulnerable to feelings of burden and, therefore, need more support [8].
The Burden Assessment Scale
Reinhard et al. [36] stated that the burden measures proposed up to that time had some limitations that underrepresented the burden of families who do not live with their mentally ill relative. According to these authors, there was a need for a measure of burden that was independent of the living situation of the ill family member and that focused on specific caregiver consequences. Likewise, these authors argued that it was necessary to have a brief, valid, and reliable assessment tool that focuses on specific objective and subjective caregiver consequences, in order to test the effectiveness of programs designed to alleviate the burden on family caregivers of people diagnosed with SMD. With these issues in mind, Horwitz and Reinhard [21] developed the Burden Assessment Scale (BAS), a 19-item scale for assessing both subjective and objective burden in family caregivers of people diagnosed with SMD.
Several studies have analyzed the psychometric properties of the BAS, obtaining different results for both the number of factors and the items included in each factor (Table 1). Horwitz and Reinhard [21], Reinhard et al. [36], and Aydemir et al. [3] obtained a five-factor model. Murdoch et al. [33] obtained a four-factor model. Hunger et al. [22] found that the model with the best fit had four correlated factors, and it was obtained from Reinhard et al.’s [36] study. Ivarsson et al. [23] and Kwak et al. [29] obtained a three-factor model, and Guada et al. [17] obtained a two-factor model. Hunger et al. [22] used confirmatory procedures, whereas the other studies used principal component analysis.
Table 1.
Models proposed for the BAS
| Study | Sample | Factorial procedures, factors obtained, and internal consistency of the BAS | Validity of the BAS and other significant results |
|---|---|---|---|
| Horwitz and Reinhard [21] | 94 family members of severely mentally ill adults who participated in a community aftercare program in New Jersey (The Club) |
1. Financial Distress (items 1 and 6) [OB] 2. Personal Activity (items 2–5) [OB] 3. Negative Effects on Social Interactions (items 7–10) [OB] 4. Feelings, Attitudes, and Emotions (items 11–16, and 19) [SB] 5. Worry (items 17 and 18) [SB] |
|
| Reinhard et al. [36] |
Sample 1 (Club): the sample used in Horwitz and Reinhard [21] study Women: 77 (81.9%) Men: 17 (18.1%) Mage = 58 Sample 2 (DMH&H): 94 family members of mentally ill adults who participated in a study of the New Jersey’s DMH&H Women: 64 (68.1%) Men: 29 (30.8%) Mage = 56.5 |
PCA with Varimax rotation Sample 1 (Club): 1. Disrupted Activities (items 2, 4–8, and 15) [OB] 2. Personal Distress (items 1, 9–11, 14, 15, and 19) [SB] 3. Guilt (items 2, 13, and 17) [SB] 4. Time Perspective (items 16 and 18) [SB] 5. Worry (items 3, 12 and 15) [SB] Sample 2 (DMH&H): 1. Disrupted Activities (items 3–8) [OB] 2. Personal Distress (items 10, 11, 14, and 15) [SB] 3. Time Perspective (items 16, 18, and 19) [SB] 4. Guilt (items 12, 13, and 17) [SB] 5. Basic Social Functioning (items 2 and 9) [OB] Whole BAS α = .89 (Sample 1) and .91 (Sample 2) |
Burden was higher for DMH&H family members than for Club family members Families in both samples: 1.- Reported the greatest average burden from their worry about the future and unrelenting grief 2.- Considered missing days at work, friction with neighbors, and guilt for causing the illness as least burdensome A lower score on the BAS was obtained over the six-month period after an intensive family support services program (the ill family member’s age and diagnosis were not predictive, nor was the involvement of the ill family member’s mother) Differential reduction in burden could be explained by service use: The more types of services received and the more single family contacts, the greater the reported reduction in family burden Families with more members involved in intensive family-support services are less likely to experience reductions in burden |
| Ivarsson et al. [23] |
256 Swedish caregivers for individuals with SMDs Women: 82 (32%) Men: 174 (68%) Age range 18–81 years (M = 39.3, SD = ns) |
PCA with Varimax rotation (minimum λ > .40): 1. Activity Limitation (items 1–8, and 15; α = .88) 2. Worry and Guilt (items 12, 13, 16–18; α = .73) 3. Social Strain (items 9–11, 14, and 19; α = .75) Whole BAS α = .90 |
The greatest perceived burden in caregivers: worry about the future The least perceived burden in caregivers: friction with others The caregivers experienced: 1. More activity limitations in relation to the youngest clients, those who had an elementary educational level, and those who lived with a partner 2. More feelings of worry and guilt in relation to the younger clients than to the older ones 3. More social strain in relation to the female clients and those who had an elementary educational level |
| Aydemir et al. (2012)a [3] |
100 Turkish volunteers who were caregivers of outpatients diagnosed with SMDs (schizophrenia, bipolar disorder, major depression, and anxiety) Women: 44 (44%) Men: 56 (56%) Age: M = 41.9, SD = 15.1 |
PCA with Varimax rotation (minimum λ > .40): 1. Limitations in Daily Life (9 items) 2. Worry for the Patient (5 items) 3. Negative Emotions (2 items) 4. Disruption in Activities (2 items) 5. Losses of the Caregiver (1 item) Whole BAS α = .89 |
Correlation with the Perceived Family Burden r = .49 Correlation with the Zarit Caregiver Burden Scale, r = . 61 |
| Guada et al. [17] |
106 family caregivers (86.2% women) of people diagnosed with schizophrenia 94 participants were African-American Participants were living in Los Angeles, USA Age range 18–80 years old Age M = 47 years old |
PCA with Varimax rotation (limited to 2 factors): 1. Emotional Reactions of Caregiving (Items 9–19) [SB] 2. Daily Impacts of Caretaking (Items 1–8) [OB] |
|
| Kwak et al. [29] |
256 Korean family caregivers (84 men, 172 women) of people diagnosed with schizophrenia Age range 21–78 (M = 54.4, SD = 11.2) |
Reliability and validity of the Korean version of the BAS (K-BAS) PCA with Varimax rotation (minimum λ = .40): 1. Activity Limitations (Items 1–8) 2. Social Strain (Items 9–11, 14–16, and 19) 3. Feelings of Worry and Guilt (Items 12, 13, 17, and 18) K-BAS α = .91 K-BAS test–retest reliability = .86, p < .001 |
Convergent validity: 1. Correlation between the K-BAS and the FBS: r = .80, p < .001 Divergent validity: 1. Correlation between the K-BAS and KDAI-10: r = -.21, p = .001 2. Correlation between the K-BAS and SUMD-K: r = -.02, p = .796 |
| Murdoch et al. [33] | Canadian family caregivers of 300 children and adolescents diagnosed with SMD seeking services within a major city |
PCA with Varimax rotation (minimum λ = .40): 1. Role Restriction (Items 1–7) 2. Family Impact (Items 8, 9, 14, and 15) 3. Public Embarrassment (Items 10, 11, and 19) 4. Guilt and Worry (Items 12, 13, 16, and 17) SB: Items 1–10 OB: Items 11–18 (although Item 18 did not load in any factor, because it loaded < .40 in all four factors) |
|
| Hunger et al. [22] |
215 relatives (72% women, 28% men) of German mentally ill people Age range 18–77 (M = 32, SD = 14) |
CFA (Maximum-Likelihood method) Authors tested several models for the BAS. Model with the best fit was one with four correlated factors: 1. Disrupted Activities (Items 1–8) 2. Personal Distress (Items 9–11, 14, and 15) 3. Time Perspective (Items 16, 18, and 19) 4. Guilt (Items 12, 13, and 17) Internal consistency: Whole BAS, α = .92 (95% CI [.90, .93]) Subscales, α from .64 to .92 (95% CIs [.55 to. 92]) |
Note. PCA Principal Component Analysis, CFA Confirmatory Factor Analysis, DMH&H Division of Mental Health & Hospitals, KDAI-10 Korean version of Drug Attitude Inventory-10, SUMD-K Korean version of the Scale to Assess Unawareness of Mental Disorder, FBS Family Burden Scale, [OB] Objective Burden, [SB] Subjective Burden, ns not stated
aIt was not possible to offer the items included in each factor because that information was not available in the paper (neither in the body of the text nor in the corresponding table is the composition of the factors adequately given)
In these studies, the internal consistency of the BAS ranged from questionable, as in the case of the factor Guilt (α = .64) in Hunger et al.’s [22] study, to good, α > .90. The BAS also showed good test–retest reliability in Kwak et al.’s [29] study, r = .86, p < .001. Likewise, in Aydemir et al. [3] and Kwak et al. [29] studies, the BAS showed divergent and/or convergent validity.
Some of these studies did not meet the requirements for accepting the result of the factor analyses performed. Horwitz and Reinhard [21] accepted two factors that included only two items each: Financial Distress included items 1 (Financial problems) and 6 (Upset household routine), and Worry included items 17 (Worry makes illness worse) and 18 (Worry about the future). Reinhard et al. [36] accepted items 2 (Missed work/school) and 15 (Felt trapped) in several factors in the model obtained with The Club sample. Similarly, these authors accepted one factor (Time Perspective) that included only items 16 (Upset about relative’s change) and 18 (Worry about the future), and they did not indicate in which factor item 1 (Financial problems) should be included (this was probably because this item loaded < .40 in the five factors they found) in the model obtained for the BAS with the DMH&H sample. Aydemir et al. [3] accepted two factors (Negative Emotions and Disruption in Activities) that only included two items, and they accepted one factor (Loss of the Caregivers) that only contained one item.
These results suggest the desirability of further investigating the structure of the BAS, an instrument that is widely used to assess the burden of family caregivers of people diagnosed with SMD.
The present study
This study aimed to analyze the psychometric properties of the BAS in a sample of Spanish caregivers of people diagnosed with BPD, concretely to test the underlying factors of that scale and the fit of the obtained model using exploratory and confirmatory procedures respectively, as well as its internal consistency and construct validity. To our knowledge, this is the first study to analyze the psychometric properties of the BAS in the Spanish population.
Method
Participants
Participants were 233 family caregivers of people diagnosed with BPD who were receiving psychological treatment in three Specialized Units for Personality Disorders and from an Association of Relatives of people with BPD in Spain (Fig. 1). The sample was collected over a period of three years (2018–2021). To be part of the research, the inclusion criteria were (a) being a caregiver of a relative with a diagnosis of BPD according to the Diagnostic and Statistical Manual of Mental Disorders [2] and (b) agreeing to and signing an informed consent regarding their voluntary participation in the study and the confidential treatment of their data. Exclusion criterion was to be diagnosed with an SMD, such as BPD, psychotic disorder, bipolar disorder, substance dependence, dementia, or major depressive disorder.
Fig. 1.
Flowchart of participants’ sociodemographic characteristics
Instruments
Burden Assessment Scale (BAS; [36])
The BAS is a 19-item scale that assesses both the subjective and objective burden of caregiving within the past six months. Subjective burden includes emotions, attitudes, and concerns associated with the caregiver role; objective burden covers observable aspects such as reduced personal time or financial problems. Answers are coded on a four-point Likert scale (1 = Not at all; 4 = A lot). The higher the score the higher level of caregiver burden. Internal consistency of the BAS in this study was ω = .93, 95% CI [.91, .94].
Multicultural Quality of Life Index (MQLI; [32])
We used the Spanish adaptation [31]. The MQLI is a 10-item scale that assesses physical and emotional well-being, self-care, occupational and interpersonal functioning, socio-emotional and community support, personal and spiritual fulfillment, and an overall perception of quality of life. Answers are coded on a 10-point Likert scale (1 = Bad,10 = Excellent). Internal consistency of the MQLI in this study was ϖ = .91, 95% CI [.90, .93].
Depression Anxiety Stress Scale-21 (DASS-21; [30])
We used the Spanish adaptation [13]. The DASS-21 assesses self-perceived physical and subjective symptoms of anxiety, depressive feelings, and behavioral manifestations of stress. Responses are coded on a Likert scale (0 = It did not happen to me,3 = It happened to me most of the time). In this study, internal consistency estimates were ω = .88, 95% CI [0.85, 0.90] for anxiety, ϖ = .90, 95% CI [.88, .92] for depression, and ω = .89, 95% CI [.87, .92] for stress.
Statistical analyses
First, descriptive statistics, corrected item-total correlations, and McDonald’s ω change if an item was dropped from the BAS were calculated in the whole sample (n = 233). In addition to McDonald’s ω, the Average Interitem Correlation (AIC) of the BAS was analyzed (according to Clark and Watson [5], the AIC score should be between .15 and .50).
Second, an Exploratory Factor Analysis (EFA) using Weighted Least Squares (Bartlett’s test showed inequality of variances) with Oblimin rotation was performed in randomized Subsample 1 (n = 114, 48.93%) [7] in order to obtain a model for the BAS. The Measure of Sampling Adequacy (MSA) was calculated (a score of .50 is an acceptable limit for retaining a variable in the EFA, and a score of .80 is meritorious) (e.g. [41]). To assign an item to a factor, the factor loading had to be ≥ .40. To accept a factor in the model, it had to include at least three items with a loading ≥ .40. If an item had a factor loading ≥ .40 on two or more factors, the factor with a loading difference of ≥ .05 from the rest of the factors was chosen.
Third, a CFA of the model obtained for the BAS was carried out in randomized Subsample 2 (n = 119, 51.07%) [43]. Because Mardia’s coefficient was > 5 and data were ordinal, Diagonally Weighted Least Squares (DWLS) and robust methods were used [38]. Fit indices used were the Chi-Square (χ2), the Comparative Fit Index (CFI) and the Tucker-Lewis Index (TLI) (a value ≥ .90 suggests an acceptable fit, and a value ≥ .95 suggests a good model fit), the Root Mean Square Error of Approximation (RMSEA) and the Standardized Root Mean Square Residual (SRMS) (a value ≤ .08 suggests an acceptable model fit, and a value ≤ .05 suggests a good model fit) (e.g. [28]).
Fourth, to determine both the concurrent and divergent validity of the model for the BAS obtained in this study, the correlations with the MQLI and DASS-2 were analyzed using Spearman’s rho (ρ) and interpreted according to Cohen [6]. To carry out all the statistical analyses mentioned in this section, the JASP 0.16.1 software [24] was used.
Procedure
An independent translator translated the scales above described from English to Spanish. Then, back-translation was carried out by another independent translator. Both translators were fluent speakers of both languages. Then, the authors of this study reviewed both the English and Spanish versions of each scale, which resulted in common format translations. The translated version of each scale was once again reviewed by an independent specialist in psychopathology. The last reviewed version of each scale was used in this study.
Participants were informed about the nature of this study, the treatment of the data, and the voluntary nature of their participation. Diagnostic interviews using the clinician version of the Structured Clinical Interview for DSM-5 (SCID-5) [12] were conducted in a clinical setting by psychologists with more than 10 years of experience in the assessment and treatment of mental disorders. Participants that met the inclusion criteria signed the informed consent form and completed the assessment protocol.
Results
Descriptive statistics of the BAS
Table 2 shows the descriptive statistics of the BAS. All the corrected item-total correlations were > .40 [.416, .718]. The mean for item 10 was 1.51, and this item was included in Factor 2. The mean score on item 1 was low (M = 1.92). The highest mean score was on item 18 (M = 3.70), close to the maximum of the scale. The mean for item 19 (M = 2.70) was comparable to that of other BAS items that were included in any factor (e.g. items 16 and 17, among others). Both the mean and kurtosis of item 18 stood out.
Table 2.
Descriptive statistics of the BAS in the whole sample
| BAS item | M | SD | Sk | K | ω if item dropped | Corrected r(item-total) |
|---|---|---|---|---|---|---|
| 1. Financial problems | 1.92 | 1.15 | .575 | -.896 | .93 | .433 |
| 2. Missed work/school | 2.00 | 1.14 | .347 | -.991 | .92 | .560 |
| 3. Difficulty concentrating | 2.95 | 1.01 | -.585 | -.668 | .92 | .698 |
| 4. Change personal plans | 2.71 | 1.16 | -.333 | -1.218 | .92 | .680 |
| 5. Reduced leisure time | 2.82 | 1.07 | -.416 | -1.005 | .92 | .704 |
| 6. Upset household routine | 2.86 | 1.06 | -.517 | -.803 | .92 | .718 |
| 7. Less time for friends | 2.67 | 1.10 | -.291 | -1.161 | .92 | .665 |
| 8. Neglected family’s needs | 2.49 | 1.02 | -.106 | -1.023 | .92 | .713 |
| 9. Family friction | 2.88 | 1.01 | -.449 | -.811 | .92 | .614 |
| 10. Friction with others | 1.51 | .99 | 1.081 | .497 | .93 | .512 |
| 11. Embarrassed | 2.11 | 1.20 | .249 | -1.071 | .92 | .649 |
| 12. Guilty for not helping enough | 2.54 | 1.13 | -.073 | -1.130 | .92 | .569 |
| 13. Guilty for causing illness | 2.29 | 1.19 | .085 | -1.164 | .92 | .590 |
| 14. Resented demands | 2.12 | 1.11 | .096 | -.843 | .92 | .635 |
| 15. Felt trapped | 2.67 | 1.17 | -.354 | -1.031 | .92 | .711 |
| 16. Upset about relative’s change | 2.76 | 1.11 | -.474 | -.765 | .92 | .624 |
| 17. Worry about making illness worse | 2.67 | 1.10 | -.281 | -1.010 | .92 | .578 |
| 18. Worry about the future | 3.70 | .64 | -2.594 | 8.014 | .93 | .481 |
| 19. Stigma upsetting | 2.75 | 1.11 | -.406 | -.952 | .93 | .416 |
Note. N = 233. Standard error of skewness = .159; Standard error of kurtosis = .318
As indicated above, the BAS showed good internal consistency, ω = .93, 95% CI [0.91, 0.94]. The AIC = .399, 95% CI [.351, .444] suggested that the items of the BAS were reasonably homogenous and contained enough unique variance to avoid being isomorphic with each other [34].
Exploratory factor analysis of the BAS
All the MSAs for the BAS items were > .800, and the MSA for the whole BAS was 0.900. The solution showed a three-factor model for the BAS: Factor 1 contained 7 items (2–8), Factor 2 contained 6 items (9–11 and 14–16), and Factor 3 contained 3 items (12, 13, and 17) (Table 3). Items 1, 18, and 19 on the BAS loaded < .40 in all of the factors obtained. These factors showed a good internal consistency: whole scale, ϖ = 0.92, 95% CI [.89, .94], Factor 1, ϖ = .91, 95% CI [.88, .93], Factor 2, ϖ = .85, 95% CI [.81, .98], and Factor 3, ϖ = .86, 95% CI [.81, .90].
Table 3.
Exploratory factor analysis of the BAS in Subsample 1
| BAS item | MSA | Factor | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| 5. Reduced leisure time | .886 | .947 | ||
| 7. Less time for friends | .889 | .852 | ||
| 4. Change personal plans | .923 | .731 | ||
| 6. Upset household routine | .957 | .703 | ||
| 8. Neglected family’s needs | .938 | .637 | ||
| 3. Difficulty concentrating | .937 | .499 | ||
| 2. Missed work/school | .926 | .409 | ||
| 11. Embarrassed | .895 | .781 | ||
| 14. Resented demands | .887 | .763 | ||
| 10. Friction with others | .843 | .676 | ||
| 9. Family friction | .941 | .532 | ||
| 16. Upset about relative’s change | .924 | .471 | ||
| 15. Felt trapped | .954 | .452 | ||
| 13. Guilty for causing illness | .810 | .926 | ||
| 12. Guilty for not helping enough | .838 | .794 | ||
| 17. Worry about making illness worse | .863 | .638 | ||
| Sum of Square Loadingsa | 4.159 | 2.948 | 2.468 | |
| Proportion of variancea | .219 | .155 | .130 | |
| Cumulative proportion of variancea | .219 | .374 | .504 | |
| McDonald’s ϖ | .91 | .85 | .86 | |
Note. N = 114. Bartlett’s test: χ2(171) = 1096.121, p < .000; Chi-squared test: χ2(101) = 93.357, p = .693. Extraction method: Weighted Least Square. Rotation method: Oblimin. Items 1, 18, and 19 did load < .40. Blanks represent loading < .40. MSA = Measure of Sampling Adequacy (.50 is an acceptable limit for retaining a variable for the EFA; e.g. [41]. Overall MSA = .900
aRotated solution
The factors correlated positively at the .001 level: ρ(F1-F2) = .531, ρ(F1-F3) = .460, and ρ(F2-F3) = .458. The effect sizes of these correlations were between intermediate and strong [6]. Factor 1 was called “Disrupted Activities”, Factor 2 was called “Personal and Social Dysfunction”, and Factor 3 was called “Worry, Guilt, and Being Overwhelmed”. Factor 1 refers to objective burden, whereas Factor 2 and Factor 3 refer to subjective burden.
Confirmatory factor analysis of the model obtained for the BAS
The model obtained for the BAS showed an excellent fit: χ2(101) = 56.873, p = 1.000, CFI = 1.000, TLI = 1.000, RMSEA = .000, 95% CI [.000, .000], SRMR = .060. All the parameters were significant at the .01 level (Fig. 2).
Fig. 2.
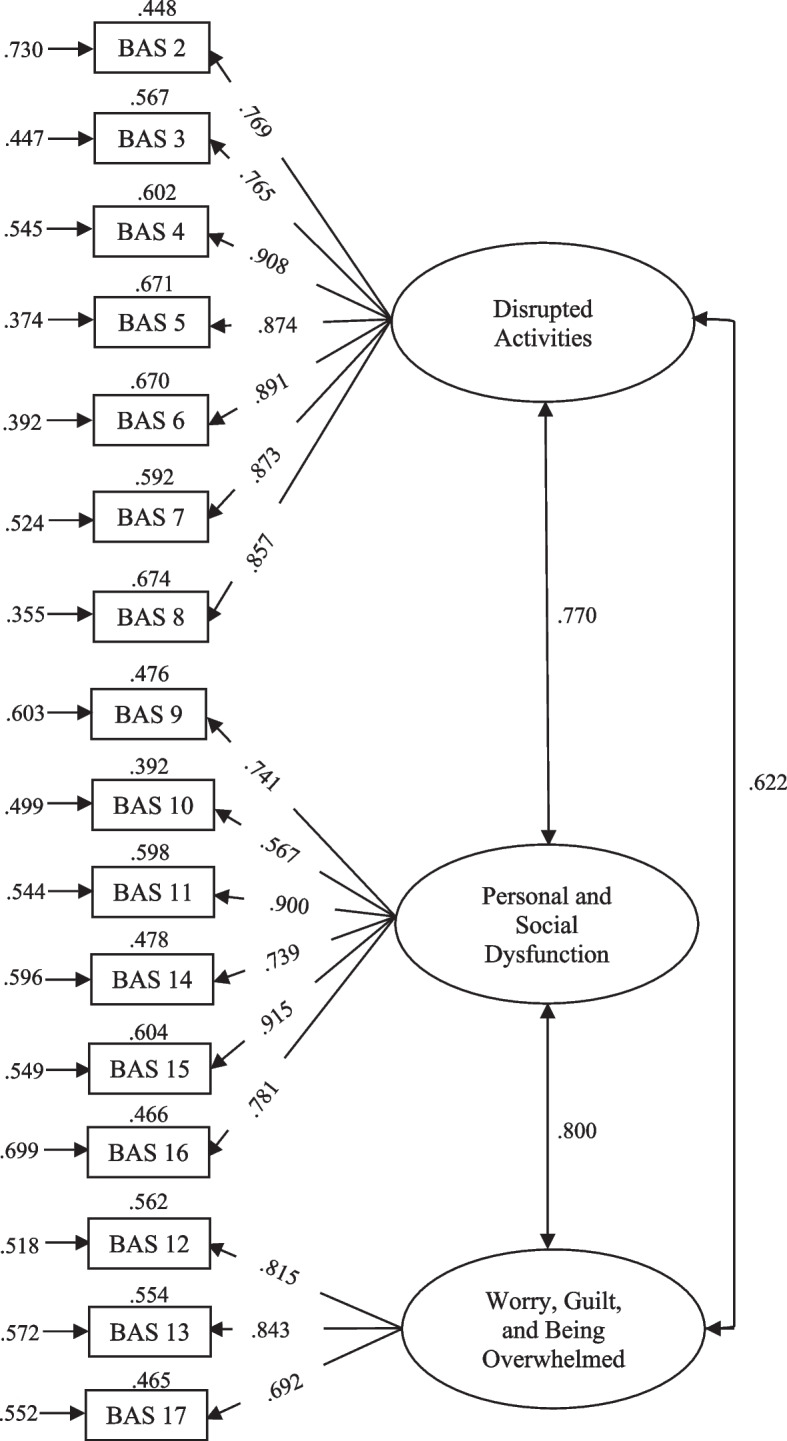
Model for the BAS obtained in the present study. Note. Values at the top of each rectangle are R2; values at the left of each rectangle are errors
Concurrent and divergent validity of the model obtained for the BAS
Correlations between the BAS, the MQLI, and the DASS-21 were in the expected direction and had effect sizes that varied between intermediate and strong [6] (Table 4).
Table 4.
Correlations (Spearman’s ρ) between the BAS, the MQLI, and the DASS-21 scales
| Variable | Burden total | Disrupted Activities | Worry, Guilt, and Being Overwhelmed | Personal and Social Dysfunction |
|---|---|---|---|---|
| Quality of Life | -.405*** I | -.365*** I | -.321*** I | -.384*** I |
| Anxiety | .500*** S | .419*** I | .486*** I | .441*** I |
| Depression | .479*** I | .393*** I | .487*** I | .403*** I |
| Stress | .529*** S | .463*** I | .505*** S | .448*** I |
Note. N = 233. S = Strong effect size; I = Intermediate effect size [6]
*** p < .001
Discussion
This study aimed to test the underlying factors, provide evidence about its internal consistency, and analyze the fit and construct validity of the BAS in a sample of Spanish caregivers of people diagnosed with BPD.
Structural validity of the model obtained for the BAS
Pioneering work by Horwitz and Reinhard [21] and Reinhard et al. [36] obtained five-factor models for the BAS. As indicated above, these studies failed to meet some of the basic requirements for exploratory factor studies, such as not accepting factors with less than three items or not including the same item in two or more factors. In our opinion, the lack of methodological rigor in these studies suggested the need for a more rigorous analysis of the structure of this scale. Subsequent studies obtained two-factor [17], three-factor [23, 29], four-factor [22, 33], and five-factor [3] models for the BAS.
We obtained a three-factor model for the BAS (Disrupted Activities; Worry, Guilt, and Being Overwhelmed; and Personal and Social Dysfunction) using exploratory procedures, as in Ivarsson et al. [23] (Activity Limitation,Worry and Guilt; and Social Strain) and Kwak et al. [29] (Activity Limitation,Social Strain; and Feelings of Worry and Guilt), with a similar distribution of items per factor, but small differences: in contrast to the studies by Ivarsson et al. [23] and Kwak et al. [29], in our study, item 1 was not included in the disrupted or limited activities factor, item 19 was not included in the social factor, and item 18 was not included in the worry-and-guilt factor.
It is worthy to note that (1) the mean for item 10 (Friction with others) was the lowest, and this item was included in Factor 2 (Personal and Social Dysfunction); (2) the mean score on item 1 (Financial problems) was low; (3) the highest mean score was on item 18 (Worry about the future), close to the maximum of the scale; and (4) the mean for item 19 (Stigma upsetting) was comparable to that of other BAS items that were included in any factor (e.g. items 16 (Upset about relative’s change) and 17 (Worry about making illness worse), among others). With regard to item 1 (Financial problems), its non-inclusion could be due to the fact that financial problems, even if they exist, are not significantly related to caring for a relative with an SMD (e.g. expenses for psychiatric medication, psychotherapy costs, help from external caregivers, among others). Regarding items 18 (Worry about future) and 19 (Stigma upsetting), it is possible that in the past 6 months the family caregivers have not felt a significant amount of worry about the future or upset due to the stigma of having a relative diagnosed with an SMD (it should be noted that the items on the BAS are responded to in relation to the following statement: “Please, would you tell me to what extent you have had any of the following experiences in the past 6 months?”). It would be interesting to investigate how family caregivers interpret worrying about the future: is it concern about possible economic hardship, the evolution of their relative diagnosed with BPD, or the future understood in a vague and diffuse way? Likewise, it would be interesting to find out whether family caregivers are aware of the meaning of the term “stigma” and, therefore, respond appropriately to that item. It must be noted that, in the present study, the sample was exclusively composed of family caregivers of people diagnosed with BPD, unlike previous studies that used samples composed of people with different diagnoses of SMD. The different composition of the samples used in these studies may have led to the differences in the results of the BAS structural analyses.
Previous studies that analyzed the structure of the BAS used Principal Component Analysis (PCA) with Varimax rotation, with the exception of Hunger et al. [22], who used CFA. Both PCA and Varimax assume uncorrelated factors (e.g. [25]). We used an EFA, specifically the Weighted Least Squares extraction method with Oblimin rotation method [15], because we assumed that the factors underlying the BAS items were correlated (like [22]. The assumption that factors are not correlated seems unlikely in the case of psychological variables, such as those measured by the BAS. Objective and subjective burden are correlated aspects or facets of the same burden experience. Therefore, it seems more appropriate to assume that the BAS factors are correlated and use an oblique rotation method (such as Oblimin) rather than an orthogonal method (such as Varimax) in the EFA (e.g. [15]).
We tested the model obtained for the BAS using confirmatory procedures in Subsample 2. Results showed the goodness of this model. Only Hunger et al. [22] tested the BAS structure using confirmatory procedures, although in reality these authors analyzed the models proposed by Reinhard et al. [36], but introducing a new parameter, i.e. correlations between the factors.
In conclusion, the present study offers a cross-analysis, both exploratory and confirmatory, of the BAS, and it proposes a reduced three-factor model with 16 items that shows good structural properties.
Internal consistency of the model obtained for the BAS
The model for the BAS obtained in this study showed good internal consistency, with estimations between .85 and 0.91 for the factors and .92 for the whole scale, which are similar to those obtained in previous studies that found Cronbach’s alphas between .89 [3, 36] and .92 [22] for the whole BAS. One exception is the study by Hunger et al. [22], who found a Cronbach’s alpha of .64 for the Guilt subscale (which contained the items, 12, 13, and 17,these items were included in the Worry, Guilt, and Being Overwhelmed factor obtained in our study), an alpha of .74 for the Time Perspective subscale, and an alpha of .78 for the Personal Distress subscale.
Construct validity of the model obtained for the BAS
As expected, the factors in the model for the BAS obtained in this study correlated negatively with quality of life and positively with anxiety, depression, and stress. These results are comparable to those obtained in the study by Kwak et al. [29], and support the construct validity of that scale.
Limitations of this study and suggestions for future studies
Some limitations of the present study should be mentioned. Regarding the sample, it would be desirable to confirm the structure obtained for the BAS in a larger sample than the one we used. It would also be interesting to analyze the invariance of this scale with regard to sex and other variables of clinical interest. For example, in our study, most of family caregivers of people diagnosed with BPD were biological mothers, and as previous studies have found, this population could be more vulnerable to feelings of burden than other caregivers and, therefore, need more support [26]. It would be interesting to test the BAS invariance between groups of caregivers. Likewise, it would be interesting to analyze whether the caregivers of people diagnosed with BPD suffer some psychological disorder, such as anxiety and depression among others, as a result of their family member’s disorder, in order to analyze its impact in the relationship with her/him and whether it can be a factor of aggravation of the disorder suffered by the relative under their care.
It would be interesting to have repeated measurements in a longitudinal design, in order to analyze the test–retest reliability of the model obtained for the BAS, and to confirm the construct validity of this scale using scales other than the ones used in our study.
It would be useful to take into account the psychological health of family caregivers of people diagnosed with SMD (e.g. [37]), and to know whether they are receiving pharmacological treatment and/or psychotherapy.
Future studies should consider the socio-economic status of the family caregivers, in order to identify factors that might facilitate or hinder the care of a relative diagnosed with an SMD, and assess the possibility of drafting statements that are more in line with the content of each item on the BAS.
It would be interesting to analyze the psychometric properties of the BAS model obtained in our study in family caregivers of people diagnosed with an SMD other than BPD, chronic disabilities or degenerative diseases, among others.
Conclusion
The BAS can be a useful instrument for clinicians, who can assess burden in family caregivers of people diagnosed with BPD (or another SMD) and improve the efficiency of programs designed to provide resources and develop skills to manage the symptoms of the burden of caring, such as Family Connections (e.g. [10, 11, 20]), and positively influence their mental health and personal well-being (e.g. [1, 9]). Scores on the BAS before and after the program can be a valid and reliable indicator of change in the family caregivers of people with a diagnosis of SMD. The model for the BAS obtained in this study is a valid, reliable, and useful tool for assessing burden in family caregivers of relatives diagnosed with BPD.
Authors’ contributions
All authors participated in the design of this study. IFF and SFB prepared the initial data, searched and analyzed the literature, and developed the Introduction. JGA performed the statistical analyses and wrote Method and Results. IF collaborated in the statistical analyses of the data. SP, JHM and VG collaborated with the other authors and developed the Discussion. All authors reviewed the manuscript submitted to the journal and participated equally in revising the manuscript to respond to reviewers' comments. The author(s) read and approved the final manuscript.
Funding
This study was funded by the Regional Ministry of Innovation, Universities, Science, and the Digital Society of the Valencian Government, Valencian Community, Spain (project code: AICO/2021/161), and partially funded by (1) the Ministry of Science, Innovation and Universities by means of an FPU grant (FPU15/07177) awarded to Sara Fonseca-Baeza (co-author), (2) CIBEROBN, an initiative of ISCIII (ISC III CB06 03/0052), (3) the Ministry of Education, Culture and Sport by means of an FPU grant (FPU17/04210) awarded to Isabel Fernández-Felipe (co-author), and (4) the Ministry of Science and Innovation (project code: MCIN/AEI/10.13039/501100011033) by means of a Predoctoral grant (PRE2019-089021) awarded to Irene Fernández (co-author).
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from 10.7910/DVN/8MU95A (Harvard Dataverse).
Declarations
Ethics approval and consent to participate
This study is part of a project approved by the Ethics Committee of the University of Valencia, Spain (UV-INV_ETICA-1623849). This study was not preregistered. Participants that met the inclusion criteria signed the informed consent form and completed the assessment protocol.
Consent for publication
No applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Joaquín García-Alandete, Email: joaquin.garcia-alandete@uv.es.
Isabel Fernández-Felipe, Email: fernandi@uji.es.
Sara Fonseca-Baeza, Email: sara.fonseca@uv.es.
Irene Fernández, Email: irene.fernandez@uv.es.
Sandra Pérez, Email: sandra.perez@uv.es.
José H. Marco, Email: jose.h.marco@uv.es
Verónica Guillén, Email: veronica.guillen@uv.es.
References
- 1.Akbari M, Alavi M, Irajpour A, Maghsoudi J. Challenges of family caregivers of patients with mental disorders in Iran: a narrative review. Iran J Nurs Midwifery Res. 2018;23(5):329–337. doi: 10.4103/ijnmr.IJNMR_122_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5 2013. [Google Scholar]
- 3.Aydemir Ö, Sücüllüoğlu D, Akdeniz F, Kalayci F. Hastalık Yükü Değerlendirme Ölçeği’nin Türkçe Sürümünün Güvenilirlik ve Geçerliliği [Reliability and Validity of the Turkish Version of the Burden Assessment Scale]. Nöropsikiyatri Arşivi. 2012;49:276–80. 10.4274/npa.y6179.
- 4.Bailey RC, Grenyer BFS. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–258. doi: 10.1097/HRP.0b013e3182a75c2c. [DOI] [PubMed] [Google Scholar]
- 5.Clark LA, Watson D. Constructing validity: basic issues in objective scale development. Psychol Assess. 1995;7(3):309–319. doi: 10.1037/1040-3590.7.3.309. [DOI] [Google Scholar]
- 6.Cohen J. Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum; 1988.
- 7.Costello AB, Osborne J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract Assess Res Eval. 2005;10(7):1–9. doi: 10.7275/jyj1-4868. [DOI] [Google Scholar]
- 8.Dunne E, Rogers B. “It’s Us That Have to Deal with it Seven Days a Week”: Carers and Borderline Personality Disorder. Community Ment Health J. 2012;49(6):643–648. doi: 10.1007/s10597-012-9556-4. [DOI] [PubMed] [Google Scholar]
- 9.Durmaz H, Okanli A. Investigation of the effect of self-efficacy levels of caregiver family members of the individuals with schizophrenia on burden of care. Arch Psychiatr Nurs. 2014;28(4):290–294. doi: 10.1016/j.apnu.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Fernández-Felipe I, Díaz-García A, Marco JH, García-Palacios A, Guillén Botella V. “Family Connections”, a DBT-Based Program for Relatives of People with Borderline Personality Disorder during the COVID-19 Pandemic: A Focus Group Study. Int J Environ Res Public Health. 2021;19(1):79. doi: 10.3390/ijerph19010079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernández-Felipe I, Guillén V, Marco JH, Díaz-García A, Botella C, Jorquera M, Baños R, García-Palacios A. Efficacy of “Family Connections”, a program for relatives of people with borderline personality disorder, in the Spanish population: Study protocol for a randomized controlled trial. BMC Psychiatry. 2020;20:302. doi: 10.1186/s12888-020-02708-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.First MB, Williams JBW, Benjamin LS, Spitzer RL. Structured Clinical Interview for DSM-5 Disorders, Clinician Version (SCID-5-CV). American Psychiatric Association; 2016.
- 13.Fonseca-Pedrero E, Paino M, Lemos-Giráldez S, Múñiz J. Propiedades psicométricas de la Depression Anxiety and Stress Scales-21 (DASS-21) en universitarios españoles [Psychometric properties of the Depression Anxiety and Stress Scales-21 (DASS-21) in Spanish undergraduates] Ansiedad y Estrés. 2010;16(2–3):215–226. [Google Scholar]
- 14.Fossati A, Somma A. Improving family functioning to (hopefully) improve treatment efficacy of borderline personality disorder: an opportunity not to dismiss. Psychopathology. 2018;51(2):149–159. doi: 10.1159/000486603. [DOI] [PubMed] [Google Scholar]
- 15.Gaskin CJ, Happell B. On exploratory factor analysis: a review of recent evidence, an assessment of current practice, and recommendations for future use. Int J Nurs Stud. 2014;51(3):511–521. doi: 10.1016/j.ijnurstu.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Goodman M, Patil U, Triebwasser J, Hoffman P, Weinstein ZA, New A. Parental burden associated with borderline personality disorder in female offspring. J Pers Disord. 2011;25(1):59–74. doi: 10.1521/pedi.2011.25.1.59. [DOI] [PubMed] [Google Scholar]
- 17.Guada J, Land H, Han J. An exploratory factor analysis of the burden assessment scale with a sample of African-American Families. Community Ment Health J. 2011;47(2):233–242. doi: 10.1007/s10597-010-9298-0. [DOI] [PubMed] [Google Scholar]
- 18.Hoffman PD, Buteau E, Hooley JM, Fruzzetti AE, Bruce ML. Family members’ knowledge about borderline personality disorder: Correspondence with their levels of depression, burden, distress, and expressed emotion. Fam Process. 2003;42(4):469–478. doi: 10.1111/J.1545-5300.2003.00469.X. [DOI] [PubMed] [Google Scholar]
- 19.Hoffman PD, Fruzzetti AE, Buteau E. Understanding and engaging families: an education, skills and support program for relatives impacted by borderline personality disorder. J Ment Health. 2007;16(1):69–82. doi: 10.1080/09638230601182052. [DOI] [Google Scholar]
- 20.Hoffman PD, Fruzzetti AE, Buteau E, Neiditch ER, Penney D, Bruce M, Hellmans F, Struening E. Family connections: a program for relatives of persons with borderline personality disorder. Fam Process. 2005;44(2):217–225. doi: 10.1111/j.1545-5300.2005.00055.x. [DOI] [PubMed] [Google Scholar]
- 21.Horwitz A, Reinhard S. Family management of labeled mental illness in a deinstitutionalized era: an exploratory study. Perspectives on Social Problems. 1992;4:111–127. [Google Scholar]
- 22.Hunger C, Krause L, Hilzinger R, Ditzen B, Schweitzer J. When Significant Others Suffer: German Validation of the Burden Assessment Scale (BAS) PLoS One. 2016;11(10):e0163101. doi: 10.1371/journal.pone.0163101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ivarsson A-B, Sidenvall B, Carlsson M. The factor structure of the Burden Assessment Scale and the perceived burden of caregivers for individuals with severe mental disorders. Scand J Caring Sci. 2004;18(4):396–401. doi: 10.1111/j.1471-6712.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- 24.JASP Team. JASP (Version 0.16.1) [Computer Software]. 2022. https://jasp-stats.org/
- 25.Jolliffe IT, Cadima J. Principal component analysis: a review and recent developments. Philos Trans Royal Soc Math Phys Eng Sci. 2016;374(2065):20150202. doi: 10.1098/rsta.2015.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jørgensen MS, Storebø OJ, Poulsen S, Simonsen E. Burden and Treatment satisfaction among caregivers of adolescents with borderline personality disorder. Fam Process. 2021;60(3):772–787. doi: 10.1111/famp.12593. [DOI] [PubMed] [Google Scholar]
- 27.Kay ML, Poggenpoel M, Myburgh CP, Downing C. Experiences of family members who have a relative diagnosed with borderline personality disorder. Curationis. 2018;41(1):e1–e9. doi: 10.4102/curationis.v41i1.1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kline RB. Principles and Practice of Structural Equation Modeling (4th ed.). Guilford; 2016.
- 29.Kwak HJ, Lee B, Jeong JH, Hong SC, Han JH, Park EJ, Jeon YW, Han SI, Seo HJ. The Reliability and Validity of the Korean Version of Burden Assessment Scale (K-BAS) J Korean Neuropsychiatr Assoc. 2013;52(4):197–200. doi: 10.4306/jknpa.2013.52.4.197. [DOI] [Google Scholar]
- 30.Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd ed. Psychology Foundation; 1995.
- 31.Marco JH, Fernández-Felipe I, García-Alandete J, García-Palacios A, Baños RM, Fonseca-Baeza S, Pérez S, Guillén V. Multicultural Quality of Life Index in relatives of people with Borderline Personality Disorder: Confirmatory factor analysis and psychometric properties. Front Psychiatry. 2022;13:897692. doi: 10.3389/fpsyt.2022.897692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mezzich JE, Cohen NL, Ruiperez MA, Banzato CE, Zapata-Vega MI. The multicultural quality of life index: presentation and validation. J Eval Clin Pract. 2011;17(2):357–364. doi: 10.1111/j.1365-2753.2010.01609.x. [DOI] [PubMed] [Google Scholar]
- 33.Murdoch DD, Rahman A, Barsky V, Maunula S, Cawthorpe D. The use of the burden assessment scale with families of a pediatric population. Community Ment Health J. 2014;50(4):1–8. doi: 10.1007/s10597-014-9724-9. [DOI] [PubMed] [Google Scholar]
- 34.Piedmont RL. Inter-item correlations. In Michalos AC (Ed.), Encyclopedia of quality of life and well-being research. 2014. Springer. 10.1007/978-94-007-0753-5_1493
- 35.Reinhard SC, Horwitz AV. Caregiver burden: differentiating the content and consequences of family caregiving. J Marriage Fam. 1995;57(3):741–750. doi: 10.2307/353928. [DOI] [Google Scholar]
- 36.Reinhard SC, Gubman GD, Horwitz AV, Minsky SK. Burden assessment scale for families of the seriously mentally ill. Eval Program Plann. 1994;17:261–269. doi: 10.1016/0149-7189(94)90004-3. [DOI] [Google Scholar]
- 37.Sansone RA, Sansone LA. The families of borderline patients: The psychological environment revisited. Psychiatry. 2009;6(2):19–24. [PMC free article] [PubMed] [Google Scholar]
- 38.Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/BF02296192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scheirs JGM, Bok S. Psychological distress in caretakers or relatives of patients with borderline personality disorder. Int J Soc Psychiatry. 2007;53(3):195–203. doi: 10.1177/0020764006074554. [DOI] [PubMed] [Google Scholar]
- 40.Souza A, Guimarães RA, de Araúj D, de Assis RM, de Almeida LM, Souza MR, Nogueira DJ, Barbosa MA. Factors associated with the burden of family caregivers of patients with mental disorders: a cross-sectional study. BMC Psychiatry. 2017;17(1):353. doi: 10.1186/s12888-017-1501-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Taherdoost H, Sahibuddin S, Jalaliyoon N. Exploratory factor analysis; concepts and theory. In Balicki J. (Coord.), Advances in applied and pure mathematics. 2014. pp. 375–382. https://hal.archives-ouvertes.fr/hal-02557344
- 42.Udoh EE, Omorere DE, Sunday O, Osasu OS, Amoo BA. Psychological distress and burden of care among family caregivers of patients with mental illness in a neuropsychiatric outpatient clinic in Nigeria. PLoS One. 2021;16(5):e0250309. doi: 10.1371/journal.pone.0250309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolf EJ, Harrington KM, Clark SL, Miller MW. Sample size requirements for structural equation models: an evaluation of power, bias, and solution propriety. Educ Psychol Measur. 2013;73(6):913–934. doi: 10.1177/0013164413495237. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from 10.7910/DVN/8MU95A (Harvard Dataverse).