Abstract
Introduction and objective
At least one in ten patients infected with COVID develop cardiovascular complications during hospitalization, increasing the number of deaths from this cause. However, the determinants of risk are not clearly elucidated. This study aims to determine whether there is a relationship between in-hospital cardiac complications and cardiovascular history and hospital evolution.
Methods
Prospective cohort study of 373 patients with a positive diagnosis of SARS-CoV-2 admitted to an Intensive Care Unit between March and October 2021.
Results
Median age was 69 (IQR: 57–77), 29.2 % of patients presented cardiovascular complications: 21.2 % electrical, 5.9 % acute coronary syndrome and 1.9 % pulmonary thromboembolism. Age RR: 1.02 (95 % CI: 1.00–1.04; p = 0.020) and history of ischemic heart disease RR: 2.23 (95 % CI: 1.27–3.92; p = 0.005) were identified as independent predictors of in-hospital cardiac complications.
Conclusions
Age and history of ischemic heart disease were identified as independent predictor variables of cardiovascular complications in patients admitted with severe COVID-19 involvement; being significantly associated with lower survival.
Keywords: COVID-19, Cardiovascular complication, Acute coronary syndrome, Cardiac arrhythmias, Mortality
1. Introduction
As of January 2020, the World Health Organization has officially declared Novel Coronavirus Infectious Disease 2019 (COVID-19) infection as a public health emergency of international concern [1]. Its rapid spread and high rate of infection, as well as the increase in severe presentations, has had an unfavorable impact on the world population and has pushed healthcare systems to their limits due to the high demand for care.
At least one in ten patients infected with COVID develop cardiovascular complications during hospitalization, increasing the number of cardiac deaths [2]. Among the most frequent cardiovascular manifestations are atrial fibrillation, pulmonary embolism and acute coronary syndrome (ACS) [2], all associated with increased hospitalization and high mortality. Currently, the effect of SARS-CoV-2 infection on cardiac muscle, either through direct damage by the virus or the role of inflammatory mediators, is now known; however, the association with certain cardiovascular risk factors is not clearly in hospitalized severe patient populations with a different immunization schedule, in Latin American countries with limited health resources, has not been sufficiently addressed. Comparing the results with those of other authors, taking into account the particularities of our study population, is of great relevance [3], [4].
Related studies on cardiovascular complications in patients infected with COVID-19 do not include large cohort analyses, nor do they include the impact of cardiac manifestations on overall patient survival. Research in hospitalized severe patient populations with a different immunization scheme, in Latin American countries with limited health resources, has not been sufficiently addressed. Comparing the results with research by other authors, taking into account the particularities of our study population, is highly relevant. The direct effect of the virus on the myocardium and vascular endothelium, the role of pro-inflammatory cytokines, the alterations in the pulmonary parenchyma itself with the consequent increase in pulmonary pressures, and other conventional risk factors contribute to the increased occurrence of cardiovascular complications [5], [6]. The identification of independent predictors of risk of cardiac complications in hospitalized patients with COVID-19 is essential to provide better healthcare and optimize available healthcare resources.
Despite the high prevalence of COVID-19 infection, the possible association of conventional risk factors for coronary heart disease, cancer, pulmonary emphysema and certain laboratory variables with the occurrence of cardiovascular complications is unknown.
2. Objective
This study aims to determine whether there is a relationship between in-hospital cardiac complications and cardiovascular history and hospital evolution.
3. Methods
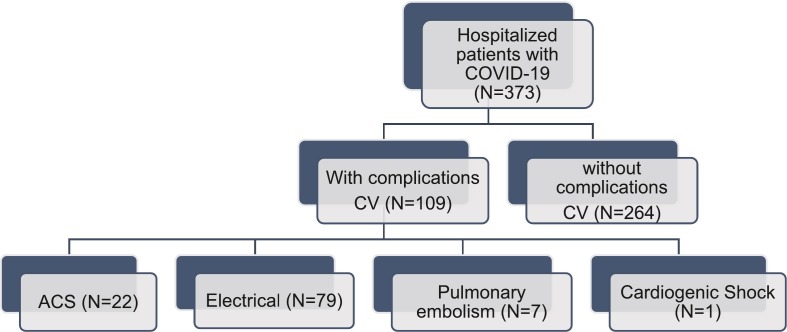
Prospective cohort study of 373 patients with a positive diagnosis of COVID-19 admitted to the Intensive Care Unit of a tertiary hospital (Havana, Cuba) between March and October 2021. The study population consisted of all patients who were consecutively admitted with a positive diagnosis of COVID-19 in the Intensive Care Unit and met the inclusion criteria and none of the exclusion criteria (Fig. 1 )
Fig. 1.
Flowchart of individuals in the study according to the inclusion and exclusion criteria.
Inclusion criteria:
-
•
Patients ≥18 years old with a positive COVID-19 diagnosis confirmed by screening test (polymerase chain reaction) for severe acute respiratory syndrome due to coronavirus 2 (SARS-CoV-2), admitted to the institution's Intensive Care Unit between March and October 2020.
Exclusion criteria:
-
•
Patients in which the variables evaluated in this study are not contained in the Intensive Care Unit database.
-
•
Patients admitted to the Intensive Care Unit with negative COVID-19 diagnosis.
For diagnosis, a nasopharyngeal swab sample was taken from all patients over 18 years of age admitted to our hospital for detection of SARS-CoV-2. The initial evaluation in the cardiology department included clinical examination, 12‑lead electrocardiogram (ECG), chest X-ray and arterial blood gas analysis. The presence of comorbidities was defined in correspondence with the data obtained from the clinical history and general physical examination.
3.1. Statistical analysis
Continuous variables were expressed as mean with standard deviation (SD) or median (interquartile range IQR), according to normal or asymmetric data distribution, which was evaluated by the Kolmogorov-Smirnov test. Categorical variables are presented as numbers and percentages.
The χ2 test was used for comparisons between qualitative variables, using the relative risk (RR) to define the intensity of this association. A bivariate logistic regression model was applied to determine the independent predictor variables of cardiovascular complications with a success rate of 70.8 %. As well as the lonk-rank test with the representation of Kaplan-Meier curves to represent survival free of cardiovascular complications in the in-hospital follow-up of patients with a positive diagnosis of COVID-19. In all cases, the confidence level was 95 % and a critical or rejection zone (alpha) of 0.05, associated with the probability value p. The SPSS version 25 statistical program was used for data analysis.
3.2. Data collection and definition of variables
For this study, the data were taken from the registry of patients admitted to the Intensive Care Unit of the hospital and the medical records.
Demographic and clinical variables: age; gender; personal pathological history: ischemic heart disease, arterial hypertension (AHT) (considered as the history of previous diagnosis recorded in the clinical history or the use of antihypertensive medication), diabetes mellitus (considered as the history of previous diagnosis recorded in the clinical history or the use of hypoglycemic medication), obesity (classified as a body mass index BMI) >30, renal failure (considered as history of previous diagnosis recorded in the medical record or glomerular filtration rate < 60 ml/min/1.73 m2), cancer (considered as history of previous diagnosis recorded in the medical record), pulmonary emphysema (considered as history of previous diagnosis recorded in the medical record or use of medication); In-hospital complications: electrical (atrioventricular blocks, supraventricular tachycardias, ventricular tachycardia and atrial fibrillation), acute coronary syndrome, shock and pulmonary thromboembolism.
Laboratory variables: creatinine (mmol/L), gamma-glutamyl transferase.
Electrical complications were determined from the interpretation of the 12‑lead ECG performed at rest. For the diagnosis of acute coronary syndrome (ACS), the fourth definition of infarction was used [7]. Pulmonary embolism was diagnosed on the basis of the results of the angiotac; if it was not available or not possible due to hemodynamic instability of the patient, direct or indirect echocardiographic signs suggestive of pulmonary embolism were considered (visualization of the thrombus, paradoxical displacement of the interventricular septum with “D” morphology, right ventricle/left ventricle ratio >1 and signs of right ventricular dysfunction).
3.3. Ethical and legal aspects
The investigators participating in this study followed the applicable ethical and legal standards, specifically the Declaration of Helsinki. Informed consent was obtained from the patients and approval was obtained from the hospital ethics committee.
4. Results
A total of 398 patients were admitted to the Intensive Care Unit with a diagnosis of COVID-19; 93.8 % presented severe COVID-19 pneumonia. The median age was 69 (RIC: 57–77), while history of AHT, diabetes mellitus and ischemic heart disease were the most frequent, the rest of the characteristics are described in Table 1 . 93.6 % of patients received invasive mechanical ventilation, while median creatinine and gamma-glutamyl transferase were 108 (88–128) and 88 (45–141) respectively. In the study 109 patients (29.2 %) presented cardiovascular complications: 79 (21.2 %) electrocardiographic, 22 (5.9 %) ACS and 7 (1.9 1 %) pulmonary thromboembolism, (Fig. 1) with atrial fibrillation being the most frequent cardiac complication 57 patients (14.2 %), the rest are described in Fig. 2 .
Table 1.
General characteristics of the population.
| Variables | n (%) | |
|---|---|---|
| Age, median (IQR) | 69 (57–77) | |
| Female gender | 162 (43,4 %) | |
| Personal history | Ischemic heart disease | 71 (19 %) |
| Arterial hypertension | 267 (71,6 %) | |
| Diabetes mellitus | 94 (25,2 %) | |
| Obesity | 112 (30 %) | |
| Renal insufficiency | 10 (2,7 %) | |
| Cancer | 18 (4,8 %) | |
| Pulmonary emphysema | 15 (4 %) | |
| Mechanical ventilation | 349 (93,6 %) | |
| Median (IQR) | ||
| Age, median (IQR) | 69 (57–77) | |
| Creatinine value (mmol/L), median (IQR) | 108 (88–128) | |
| GGT value, median (IQR) | 88 (45–141) | |
IQR: rango intercuartílico, GGT: gamma-glutamil transferase.
Fig. 2.
Distribution of in-hospital cardiovascular complications.
AF: Atrial fibrillation, AVB: atrioventricular block, VT: Ventricular tachycardia, SVT: supraventricular tachycardia, STEMI: ST elevation with myocardial infarction, NSTACS: Non-ST elevation acute coronary syndrome, EP: Pulmonary embolism.
In the multivariate analysis to determine possible independent predictors of in-hospital cardiovascular complications, age and history of ischemic heart disease were identified as independent predictor variables of in-hospital cardiac complications with RR: 1.02; (95 % CI: 1.00–1.04; p = 0.020) and RR: 2.23; (CI: 1.27–3.92; p = 0.005) respectively (Fig. 3 ).
Fig. 3.
Multivariate analysis of independent predictors of in-hospital cardiovascular complications.
In-hospital survival among severe COVID-19 patients with in-hospital cardiac complications compared to those without was significantly lower with HR: 2.06 (95 % CI: 1.08–3.93 p = 0.029) (Fig. 4 ). Despite the fact that all patients evaluated had severe complications due to the new coronavirus infection (cardiovascular, respiratory, renal or metabolic) the occurrence of cardiac complications during their admission to the Intensive Care Unit contributed to the 2.02-fold increase in mortality (95 % CI: 1.15–3.56; p = 0.007).
Fig. 4.
Survival free of in-hospital cardiovascular complications.
5. Discussion
The main findings of our study can be summarized as follows: first, patients with advanced age or previous coronary artery disease are predictors of risk of complications during hospitalization in patients with COVID-19. Second, the most common complication is atrial fibrillation. Third, suffering any of the cardiovascular complications during hospitalization for COVID-19 increases the risk of death more than twice.
Our study focuses on a Latin American population with immunization against COVID-19 with different vaccines and the limitations inherent to access to novel therapies. However, the behavior of cardiovascular complications in these patients has been similar to that of other regions with more resources such as Europe and North America [8], [9]. The control of cardiovascular risk factors, as well as the individualized treatment of these patients based on the evaluation of the risk of in-hospital complications, could be the key to our results.
A meta-analysis concluded that among the most frequent cardiovascular causes of admission to an Intensive Care Unit were cardiac arrhythmias, coronary artery disease and acute heart failure respectively [10]. Regardless of the characteristics of each population studied and the series consulted, the most common cardiovascular complications seem to be repeated as in our population [11], [12], [13]. This suggests the use of more vigorous cardiovascular prevention measures in these patients and systematic follow-up by a cardiology specialist during hospitalization.
The evolution of patients with SARS-Cov-2 as well as their short- and medium-term prognosis is determined by numerous interacting risk factors, whether or not directly related to the virus. A history of ischemic heart disease, hypertension, heart failure and arrhythmias were significantly associated with mortality in patients with COVID-19 in a systematic review [14], [15], [16], [17], [18]. In addition, other classic risk factors for coronary artery disease seem to be associated with a poor prognosis [10], [19], [20]. The present study highlights the predictive value of variables such as age and a history of previous coronary artery disease with cardiac arrhythmias, ACS and pulmonary embolism.
In the present study, advanced age was an independent predictor of cardiovascular complications (arrhythmia, acute coronary syndrome or pulmonary embolism). Several studies have evaluated the relationship of different variables with the development of cardiac complications, with age being identified as a predictor of risk of complications and increased mortality in patients admitted with COVID-19 [21], [22]. In the study by Zhang and colleagues [23], age was identified as an independent predictor of cardiovascular complications and death. The increase in more severe presentations of COVID-19 and the corresponding increase in the need for mechanical ventilation in older patients, the uncontrolled systemic inflammatory response, as well as the greater number of cardiovascular risk factors could account for the higher number of cardiac complications in these age groups [24], [25], [26].
Different authors such as Sabatino [27], Huang and collaborators [21] described the relationship between a history of cardiovascular disease and the occurrence of cardiac complications. The effect of SARS-CoV-2 infection on endothelial function, as well as the contribution to atheroma plaque instability in patients with prior coronary artery disease, contribute to the increase in acute coronary events [28], [29], [30]. In the same way, the increase in myocardial oxygen demand in severe presentations and the decrease in oxygen supply due to severe hypoxia are factors associated with the occurrence of acute coronary events, among others [5], [31], [32]. However, data from the CAPACITY-COVID registry and the LEOSS study after multivariate adjustment showed no association between different histories of ischemic heart disease and major cardiovascular complications [33]. The main difference between the CAPACITY-COVID study and the present study is the low prevalence of patients admitted to critical care units. In addition, the age and number of comorbidities among patients admitted to intensive care units compared to those hospitalized in general hospital wards in the CPACITY-COVID study was lower, which could justify the differences found.
Regardless of the impact of severe COVID-19 infection on mortality; the presence of complications during hospitalization as described in this study decreased in-hospital survival [29], [34], [35]. Recent work showed that the occurrence of cardiac arrhythmias was associated with decreased survival. In the same way, researches consulted related the occurrence of arrhythmias, heart failure and ACS with a significant decrease in survival [13], [22], [27]. Patients with cardiovascular complications according to the results of Mitrani [36], Holm and collaborators [37], as well as other multicenter studies have coincided with the results of the present work [21], [38], [39]; where the group of patients who suffered in-hospital cardiac complications presented a lower survival, given the impact that these pathologies have on a poorer prognosis.
6. Limitations
The main limitations of this research lie in the characteristics of its methodology, with a representative study population size, however, the results are collected in a single center. The presence of severe respiratory manifestations and hydroelectrolyte disorders could influence the occurrence of cardiovascular complications. Another limitation of the study is related to the evaluation of laboratory variables; only the initial data on admission to intensive care were collected. The antiarrhythmic effect of the drugs received during hospital admission was also not taken into account, despite the fact that chloroquine or azithromycin were not included in our hospital's protocol.
7. Conclusions
Advanced age and a history of ischemic heart disease were identified as independent predictor variables of cardiovascular complications in patients admitted with severe COVID-19 involvement. In the group of patients with cardiovascular complications, cardiac complications were significantly associated with lower survival. Early in-hospital risk stratification in SARS-CoV-2 positive patients that includes this cardiac profile will allow a more effective therapeutic strategy; especially in Latin American countries where current studies on the subject are not sufficient. Increased research in populations with different vaccination patterns and limited resources will allow us to know the impact and will help to better manage the resources of this epidemic in our region.
CRediT authorship contribution statement
Luis Mariano de la Torre Fonseca: Conceptualization, Methodology, Formal analysis, Writing – original draft. Robert Alarcón Cedeño: Resources, Data curation. Víctor Alfonso Jiménez Díaz: Validation, Supervision. Fabiola Isabel Loor Cedeño: Investigation, Visualization. Pablo Juan-Salvadores: Methodology, Writing – review & editing, Project administration.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Zhou W., Song L., Wang X., Xu Z., Wang S., Wang J., et al. Cardiac injury prediction and lymphocyte immunity and inflammation analysis in hospitalized patients with coronavirus disease 2019 (COVID-19) Int J Cardiol. 2021 Mar 1;326:237–242. doi: 10.1016/j.ijcard.2020.10.049. Available in. Epub 2020 Oct 22. PMID: 33098952; PMCID: PMC7577874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Linschoten M., Peters S., van Smeden M., Jewbali L.S., Schaap J., Siebelink H.M., et al. CAPACITY-COVID collaborative consortium. Cardiac complications in patients hospitalised with COVID-19. Eur Heart J Acute Cardiovasc Care. 2020 Dec;9(8):817–823. doi: 10.1177/2048872620974605. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Szekely Y., Lichter Y., Taieb P., Banai A., Hochstadt A., Merdler I., et al. Spectrum of cardiac manifestations in COVID-19. A systematic echocardiographic study. Circulación. 2020 28 de julio;142(4):342–353. doi: 10.1161/CIRCULATIONAHA.120.047971. Epub 2020 29 de mayo. PMID: 32469253; IDPM: PMC7382541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwenandar F., Japar K.V., Damay V., Hariyanto T.I., Tanaka M., Lugito N.P.H., et al. Coronavirus disease 2019 and cardiovascular system: a narrative review. Int J Cardiol Heart Vasc. 2020 <comment>Jun 3</comment>;29 doi: 10.1016/j.ijcha.2020.100557. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de la Torre Fonseca L.M. Lesión miocárdica en el paciente con COVID-19. CorSalud. 2020;12(2):171–183. [Internet] Available in: http://www.revcorsalud.sld.cu/index.php/cors/article/view/623/1205. [Google Scholar]
- 6.Chung M.K., Zidar D.A., Bristow M.R., Cameron S.J., Chan T., Harding C.V., 3rd, Kwon D.H., Singh T., Tilton J.C., Tsai E.J., Tucker N.R., Barnard J., Loscalzo J. COVID-19 and cardiovascular disease: from bench to bedside. Circ Res. 2021 Apr 16;128(8):1214–1236. doi: 10.1161/CIRCRESAHA.121.317997. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thygesen K., Alpert J.S., Jaffe A.S., Chaitman B.R., Bax J.J., Morrow D.A., et al. Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018) Glob Heart. 2018 Dec;13(4):305–338. doi: 10.1016/j.gheart.2018.08.004. Available in doi:1016/j.gheart.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Boietti Bruno R., Matias Mirofsky, Ricardo Valentini, Peuchot Verónica A., Cámera Luis A., Pollán Javier A., et al. Análisis descriptivo de 4776 pacientes internados en servicios de clínica médica POR COVID-19. Resultados del Registro Multicéntrico Argentino - REMA-COVID-19. Medicina (B. Aires) 2021 Oct;81(5):703–714. [cited 2023 Feb 12] Available in: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0025-76802021000500703&lng=es. [PubMed] [Google Scholar]
- 9.Patricia Álvarez, Valeria Acevedo, Lidia Valenzuela María, Vicente Montes, Patricia Aroca, Carla García, et al. Compromiso cardiovascular en pacientes con Síndrome Inflamatorio Pediátrico Multisistémico, asociado a infección por SARS-CoV-2. Rev Chil Cardiol. 2020 Dic;39(3):208–215. [cited 2023 Feb 13] Available in: http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0718-85602020000300208&lng=es. doi:10.4067/S0718-85602020000300208. [Google Scholar]
- 10.Hessami A., Shamshirian A., Heydari K., Pourali F., Alizadeh-Navaei R., Moosazadeh M., et al. Cardiovascular diseases burden in COVID-19: systematic review and meta-analysis. Am J Emerg Med. 2021 Aug;46:382–391. doi: 10.1016/j.ajem.2020.10.022. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Szekely Y., Lichter Y., Hochstadt A., Taieb P., Banai A., Sapir O., et al. The predictive role of combined cardiac and lung ultrasound in coronavirus disease 2019. J Am Soc Echocardiogr. 2021 junio;34(6):642–652. doi: 10.1016/j.echo.2021.02.003. Available in. Epub 2021 9 de febrero. PMID: 33571647; PMCID: PMC7870445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kunutsor S.K., Laukkanen J.A. Cardiovascular complications in COVID-19: a systematic review and meta-analysis. J Infect. 2020 Aug;81(2):e139–e141. doi: 10.1016/j.jinf.2020.05.068. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhao Y.H., Zhao L., Yang X.C., Wang P. Cardiovascular complications of SARS-CoV-2 infection (COVID-19): a systematic review and meta-analysis. Rev Cardiovasc Med. 2021 Mar 30;22(1):159–165. doi: 10.31083/j.rcm.2021.01.238. Available. In: [DOI] [PubMed] [Google Scholar]
- 14.Spinoni E.G., Mennuni M., Rognoni A., Grisafi L., Colombo C., Lio V., et al. COVID-UPO Clinical Team†. Contribution of atrial fibrillation to in-hospital mortality in patients with COVID-19. Circ Arrhythm Electrophysiol. 2021 Feb;14(2) doi: 10.1161/CIRCEP.120.009375. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Z., Shao W., Zhang J., Ma J., Huang S., Yu P., et al. Prevalence of atrial fibrillation and associated mortality among hospitalized patients with COVID-19: a systematic review and meta-analysis. Front Cardiovasc Med. 2021 <comment>Oct 13</comment>;8 doi: 10.3389/fcvm.2021.720129. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mubarik S., Liu X., Eshak E.S., Liu K., Liu Q., Wang F., et al. The association of hypertension with the severity of and mortality from the COVID-19 in the early stage of the epidemic in Wuhan, China: a multicenter retrospective cohort study. Front Med. 2021 May 12;8 doi: 10.3389/fmed.2021.623608. (Lausanne) Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cordero A., Santos García-Gallego C., Bertomeu-González V., Fácila L., Rodríguez-Mañero M., et al. Mortality associated with cardiovascular disease in patients with COVID-19. Rec Cardioclinics. 2021;56(1):30–38. doi: 10.1016/j.rccl.2020.10.005. January-March. Available in. [DOI] [Google Scholar]
- 18.Bhatia K.S., Sritharan H.P., Ciofani J., Chia J., Allahwala U.K., Chui K., et al. Association of hypertension with mortality in patients hospitalised with COVID-19. Open Heart. 2021 Dec;8(2) doi: 10.1136/openhrt-2021-001853. [Internet] Available in: http://www.revcorsalud.sld.cu/index.php/cors/article/view/623/1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L., Bi Z., Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020 May;109(5):531–538. doi: 10.1007/s00392-020-01626-9. Available. In: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noor F.M., Islam M.M. Prevalence and associated risk factors of mortality among COVID-19 patients: a meta-analysis. J Community Health. 2020 Dec;45(6):1270–1282. doi: 10.1007/s10900-020-00920-x. Available. In: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang D., Wang T., Chen Z., Yang H., Yao R., Liang Z. A novel risk score to predict diagnosis with coronavirus disease 2019 (COVID-19) in suspected patients: a retrospective, multicenter, and observational study. J Med Virol. 2020 Nov;92(11):2709–2717. doi: 10.1002/jmv.26143. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alquézar-Arbé A., Miró O., González del Castillo J., Jiménez S., Llorens P., Martín A., et al. Incidence, clinical characteristics, risk factors and outcomes of acute coronary syndrome in patients with COVID-19: results of the UMC-19-S10 10. J Emerg Med. 2021 Nov;3:1–12. doi: 10.1016/j.jemermed.2021.10.046. Available. In: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang H., Wu Y., He Y., Liu X., Liu M., Tang Y., et al. Age-related risk factors and complications of patients with COVID-19: a population-based retrospective study. Front Med. 2022 Jan 11;8 doi: 10.3389/fmed.2021.757459. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colon C.M., Barrios J.G., Chiles J.W., McElwee S.K., Russell D.W., Maddox W.R., et al. Atrial arrhythmias in COVID-19 patients. JACC Clin Electrophysiol. 2020 Sep;6(9):1189–1190. doi: 10.1016/j.jacep.2020.05.015. Disponible en doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Y., Pang S.C., Yang Y. A potential association between immunosenescence and high COVID-19 related mortality among elderly patients with cardiovascular diseases. Immun Ageing. 2021 Jun 1;18(1):25. doi: 10.1186/s12979-021-00234-z. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Napoli C., Tritto I., Benincasa G., Mansueto G., Ambrosio G. Cardiovascular involvement during COVID-19 and clinical implications in elderly patients. A review. Ann Med Surg. 2020 Aug 5;57:236–243. doi: 10.1016/j.amsu.2020.07.054. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sabatino J., De Rosa S., Di Salvo G., Indolfi C. Impact of cardiovascular risk profile on COVID-19 outcome. A meta-analysis. PLoS One. 2020 Aug 14;15(8) doi: 10.1371/journal.pone.0237131. Available in. Erratum in: PLoS One. 2020 Dec 3;15(12):e0243471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cenko E., Badimon L., Bugiardini R., Claeys M.J., De Luca G., de Wit C., et al. Cardiovascular disease and COVID-19: a consensus paper from the ESC Working Group on Coronary Pathophysiology & Microcirculation, ESC Working Group on Thrombosis and the Association for Acute CardioVascular Care (ACVC), in collaboration with the European Heart Rhythm Association (EHRA) Cardiovasc Res. 2021 Dec 17;117(14):2705–2729. doi: 10.1093/cvr/cvab298. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Long B., Brady W.J., Bridwell R.E., Ramzy M., Montrief T., Singh M., et al. Electrocardiographic manifestations of COVID-19. Am J Emerg Med. 2021 Mar;41:96–103. doi: 10.1016/j.ajem.2020.12.060. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G., et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. 2020 May 12;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zou F., Qian Z., Wang Y., Zhao Y., Bai J. Cardiac injury and COVID-19: a systematic review and meta-analysis. CJC Open. 2020 Sep;2(5):386–394. doi: 10.1016/j.cjco.2020.06.010. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nan J., Jin Y.B., Myo Y., Zhang G. Hypoxia in acute cardiac injury of coronavirus disease 2019: lesson learned from pathological studies. J Geriatr Cardiol. 2020 Apr;17(4):221–223. doi: 10.11909/j.issn.1671-5411.2020.04.010. [cited 2023 Feb 12] Available in: http://www.scielo.org.ar/scielo.php?script=sci_arttext&pid=S0025-76802021000500703&lng=es. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.CAPACITY-COVID Collaborative Consortium. LEOSS Study Group Clinical presentation, disease course, and outcome of COVID-19 in hospitalized patients with and without pre-existing cardiac disease: a cohort study across 18 countries. Eur Heart J. 2021 Nov 4 doi: 10.1093/eurheartj/ehab656. Available in. [DOI] [PubMed] [Google Scholar]
- 34.Elias P., Poterucha T.J., Jain S.S., Sayer G., Raikhelkar J., Fried J., et al. The prognostic value of electrocardiogram at presentation to emergency department in patients with COVID-19. Mayo Clin Proc. 2020 Oct;95(10):2099–2109. doi: 10.1016/j.mayocp.2020.07.028. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Retraction: cardiovascular disease, drug therapy, and mortality in COVID-19. N Engl J Med. 2020 Jun 25;382(26):2582. doi: 10.1056/NEJMc2021225. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Mitrani R.D., Dabas N., Goldberger J.J. COVID-19 cardiac injury: implications for long-term surveillance and outcomes in survivors. Heart Rhythm. 2020 Nov;17(11):1984–1990. doi: 10.1016/j.hrthm.2020.06.026. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Holm A., Jerkeman M., Sultanian P., Lundgren P., Ravn-Fischer A., Israelsson J., et al. Cohort study of the characteristics and outcomes in patients with COVID-19 and in-hospital cardiac arrest. BMJ Open. 2021 Nov 30;11(11) doi: 10.1136/bmjopen-2021-054943. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ip R.J., Ali A., Baloch Z.Q., Al-Abcha A., Jacob C., Arnautovic J., et al. Atrial fibrillation as a predictor of mortality in high risk COVID-19 patients: a multicentre study of 171 patients. Heart Lung Circ. 2021 Aug;30(8):1151–1156. doi: 10.1016/j.hlc.2021.02.010. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.D'Ascenzo F., De Filippo O., Borin A., Barbieri L., Adamo M., Morici N., et al. Impact of COVID-19 pandemic and infection on in hospital survival for patients presenting with acute coronary syndromes: a multicenter registry. Int J Cardiol. 2021 Jun 1;332:227–234. doi: 10.1016/j.ijcard.2021.03.063. Available in. [DOI] [PMC free article] [PubMed] [Google Scholar]