Case
A 40-year-old man with a strong history of heart disease in male relatives younger than 55 years of age visits his physician for an annual checkup. He appears generally fit and well and is normotensive. His fasting lipid profile reveals cholesterol (5.4 mmol/L), low-density lipoprotein (LDL) cholesterol (3.8 mmol/L), high-density lipoprotein (HDL) cholesterol (1.0 mmol/L) and triglyceride (1.2 mmol/L). His physician recommends a lower fat diet with an emphasis on a lowered intake of saturated fats (from fatty meats and high-fat dairy produce) and “trans” fatty acids (vegetable shortening and partially hydrogenated vegetable oils in processed and fast foods). When leaving the office, the patient asks, “I've heard about fish oils being ‘heart healthy.’ Should I be eating fish or taking a supplement?”
During the past few years, there has been an increase in both scientific and public interest in the role of omega-3 fatty acids found in fish and fish oils in the prevention and management of cardiovascular disease. The omega-3 fatty acids that are of particular interest for cardiovascular care include EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid), which are found predominantly in fish and fish oils.1,2,3 The basis of this heightened interest in dietary intakes of EPA and DHA comes partly from epidemiological and population studies4 indicating that increased consumption of fish as a source of omega-3 fatty acids is often associated with decreased mortality (as well as morbidity) from cardiovascular disease. Controlled-intervention trials in humans have indicated a favourable modifying effect of dietary fish oils on various risk factors for cardiovascular disease independent of their lowering of blood cholesterol.1,2,3 Dietary supplementation with encapsulated omega-3 fish oil concentrates has shown the potential to reduce both the progression of cardiovascular disease and related mortality, including sudden cardiac death.5,6
What are omega-3 fatty acids?
Omega-3 fatty acids are long-chain polyunsaturated fatty acids (18–22 carbon atoms in chain length) with the first of many double bonds beginning with the third carbon atom (when counting from the methyl end of the fatty acid molecule). The fish-based and fish-oil–based omega-3 polyunsaturated fatty acids (also referred to as n-3 PUFA) consist of EPA (20 carbon atoms, 5 double bonds) and DHA (22 carbon atoms, 6 double bonds). The general structures for EPA and DHA are shown in Fig. 1. Commonly available dietary sources of EPA and DHA are listed in Table 1. Whereas plant foods and vegetable oils lack EPA and DHA, some do contain varying amounts of the n-3 PUFA alpha-linolenic acid (ALA), which has 18 carbon atoms and 3 double bonds (Fig. 1). Many vegetable oils are greatly enriched in omega-6 fatty acids (mainly as linoleic acid in corn, safflower, sunflower and soybean oils), but canola oil (nonhydrogenated), ground flaxseed and walnuts are rich sources of ALA. The typical North American diet provides about 1–3 g of ALA per day but only 0.10–0.15 g of EPA plus DHA per day.7,8 The very high intake of n-6 PUFA, mostly as linoleic acid (LA) (Fig. 1) in our diet (12–15 g/day) from common vegetable oils (corn, safflower, soybean) and other sources, yields an overall n-6:n-3 dietary ratio (total omega-6 fatty acids in the diet: total omega-3 fatty acids in the diet) of about 8:1. Health Canada has recommended that this ratio be as low as 4:19 to reduce the competitive influence of high LA intakes on ALA metabolism to its longer chain products (such as EPA and DHA). Although high intakes of LA can provide some modest blood cholesterol lowering, experimental studies in animals have raised concerns regarding the enhancing effect of these high intakes on certain cancers.10 This association has not been established in human studies.11
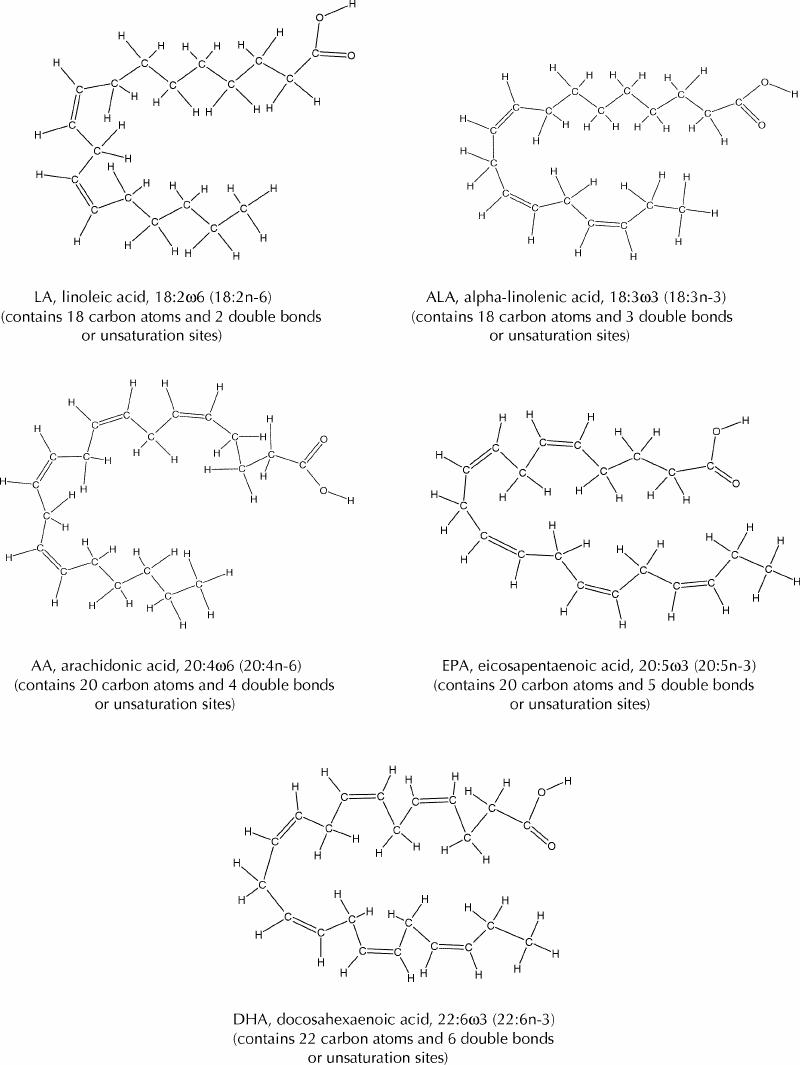
Fig. 1: Chemical structures of linoleic acid (LA), alpha-linolenic acid (ALA), arachidonic acid (AA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
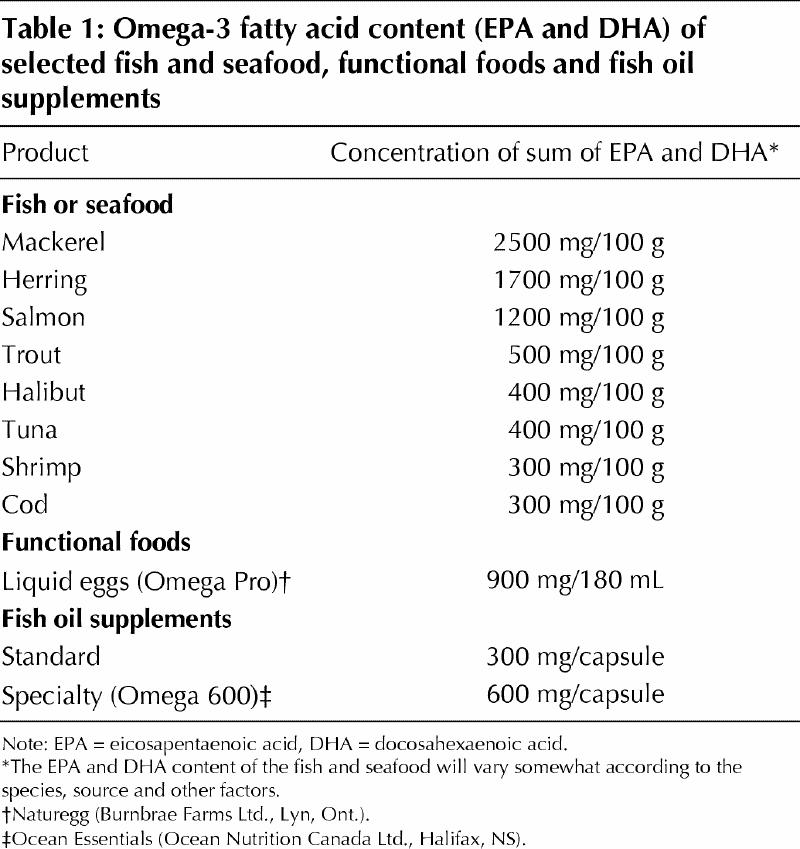
Table 1
Epidemiological evidence for the cardioprotective effects of EPA and DHA
It has long been recognized12 that disease patterns for the Greenland Inuit, when compared with those for the population of Denmark, exhibit a significantly lower rate of death from acute myocardial infarction despite only moderate differences in blood cholesterol levels. The high-fat traditional Inuit diet (Greenland; Nunavik, Que.) provides up to several grams of omega-3 fatty acid (EPA and DHA) daily in the form of marine mammals (seal, whale), wildfowl (seabirds) and various fish.12,13 Furthermore, the higher fish intakes of the Japanese population relative to that of North America have been associated with considerably lower rates of acute myocardial infarctions, other ischemic heart disease and atherosclerosis despite only moderately lower blood cholesterol levels in the Japanese population.1,14 Various studies have also indicated that long-term consumption of fish (up to 2–3 servings per week) appears to be associated with lower primary and secondary heart attack rates and death from cardiovascular disease.4,15,16 Following dietary consumption, the levels of EPA and DHA rise considerably in mammalian cells and tissues via their esterification into the 2-position (that is, the middle carbon of the glycerol backbone in a phospholipid structure) of the membrane phospholipid components. Fatty acid analyses of serum and plasma phospholipid, a biomarker for EPA and DHA intake and physiological status, have indicated that omega-3 fatty acids in general and DHA levels in particular are inversely correlated with coronary heart disease in men.17 Among the Inuit of Nunavik, progressive increases in levels of EPA and DHA in plasma phospholipid have been found both to reflect dietary intakes of these fatty acids and to be beneficially associated with key risk factors for cardiovascular disease.18
Possible biochemical and physiological mechanisms of action for EPA and DHA
The various mechanisms by which increased dietary consumption of omega-3 fatty acids from fish and fish oils is considered to favourably modify cardiovascular disease and associated disorders are outlined in Table 2. Increasing the intake of EPA and DHA results in a corresponding increase of these omega-3 fatty acids in tissue or cellular lipids and circulatory lipids1,18 along with a simultaneous reduction in the omega-6 fatty acids such as LA and arachidonic acid (AA) (Fig. 1). The fatty acid shifts are particularly pronounced in the cell membrane–bound phospholipid components. These changed profiles alter the physicochemical properties of cell membranes and their functioning and modify cell signalling, gene expression and biosynthetic processes, and eicosanoid formations (the eicosanoids formed via oxygenase enzymes acting on AA and EPA include prostaglandins, leukotrienes and thromboxanes.). The beneficial effects of omega-3 fatty acids on cardiovascular disease are mediated by both eicosanoid-dependent and eicosanoid-independent processes. For example, the reduced blood platelet reactivity (antithrombotic effect) observed with increased EPA and DHA intakes involves the reduced formation of the proaggregatory eicosanoid known as thromboxane A2 (TxA2). The replacement of AA (the omega-6 fatty acid and TxA2 precursor) in blood platelet membrane phospholipid by EPA and DHA yields less TxA2 upon platelet stimulation; furthermore, EPA has an inhibitory effect on the cyclo-oxygenase enzyme that connects AA to TxA2 thus leading to a lessened thrombogenic state (Figs. 2 and 3).
Table 2
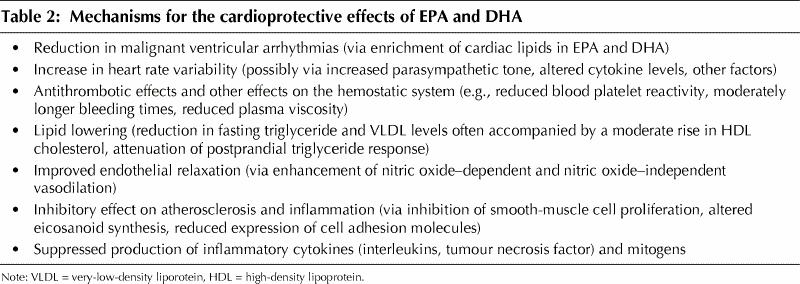
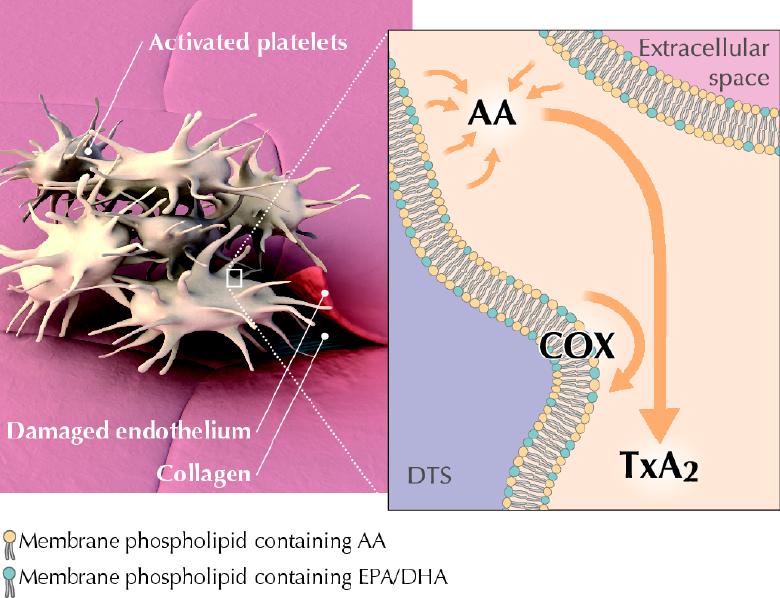
Fig. 2: Platelets are activated when they come into contact with an agonist, such as collagen exposed by damaged endothelial cells. When a diet is low in omega-3 fatty acids, activated platelets liberate AA from the phospholipids of the intracellular cell membranes known as the dense tubular system (DTS). Cyclo-oxygenase (COX) associated with the DTS catalyzes AA conversion to TxA2, leading to increased platelet aggregation, making thrombus formation more likely. Photo by: Lianne Friesen and Nicholas Woolridge
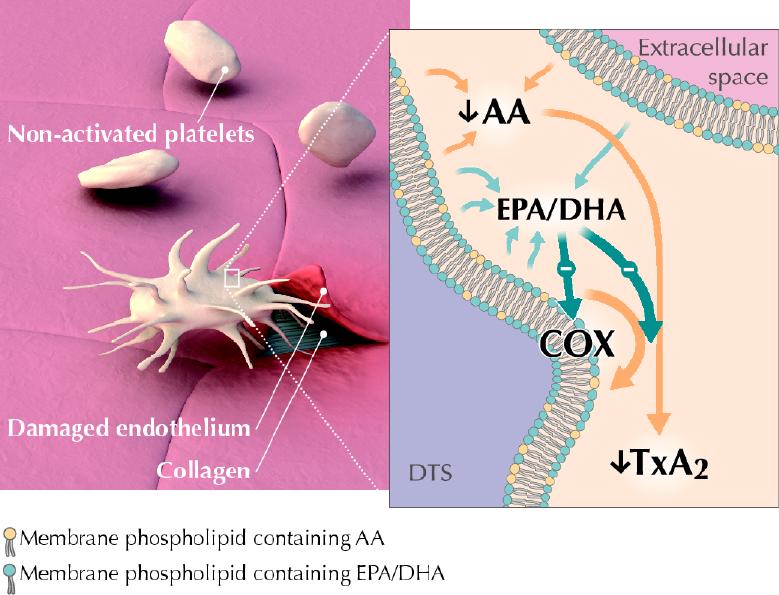
Fig. 3: When a diet is high in the omega-3 fatty acids EPA and DHA, they replace a portion of the AA in membrane phospholipids. This reduces the amount of AA available for liberation. In addition, liberated EPA and DHA inhibit the activity of COX. This results in reduced production of the proaggregatory compound thromboxane A2 (TxA2), leading to reduced platelet aggregation, making thrombus formation less likely. Photo by: Lianne Friesen and Nicholas Woolridge
Intervention studies and risk factor modification using EPA and DHA
Intervention studies using fish oil concentrates that provide EPA and DHA at intakes of up to 2–4g/day over a few weeks1,2,3 have shown that these fatty acids can favourably attenuate various risk factors for cardiovascular disease (independent of any blood cholesterol-lowering effect). These effects include an antithrombotic effect, lipid (triglyceride) lowering, reduced blood and plasma viscosity, and improvements in endothelial dysfunction.1,2,3,19 Omega-3 fatty acids accumulate to a considerable extent in various sites including circulating blood platelets, the heart and serum phospholipid. The accumulation of EPA and DHA in platelets is associated with decreased platelet adhesiveness and aggregation and an overall reduction in thrombogenicity. Antiatherogenic effects of omega-3 fatty acids have also been shown in animal studies.
Human studies have revealed the potent ability of EPA and DHA to significantly reduce circulating levels of blood triglyceride,20 which is of interest because only moderate elevations in triglyceride (approaching 1.33 mmol/L or 118 mg/dL, or above) have been associated with a progressively increased risk of ischemic heart disease.21 Within 2–3 weeks of EPA and DHA supplementation, significantly reduced blood triglyceride levels with an approximate reduction of 6%–8% (or more) per gram of EPA and DHA consumed are routinely observed. In a placebo-controlled, double-blind trial,22 a 26% lowering in fasting triglyceride levels in postmenopausal women receiving 4 g omega-3 (EPA and DHA) daily over 28 days was recently demonstrated. In cases where combined statin therapy plus certain triglyceride-lowering therapies (e.g., fibric acid derivatives) may be contraindicated, statin plus omega-3 (EPA and DHA) therapy may be an attractive alternative. Supplementation with omega-3 (EPA and DHA), as given in addition to statin therapy in patients with combined hyperlipidemia,23 was found to reduce levels of atherogenic lipoproteins while more effectively reducing the hemostatic risk profile. The antiarrhythmic potential of EPA and DHA (upon accumulation in cardiac tissue) has been considered to be yet another important mechanism24 by which consumption of these fatty acids can reduce mortality related to cardiovascular disease (particularly sudden cardiac death). This last effect is considered to be exhibited at even lower intakes of omega-3 (EPA and DHA combined) of about 1 g/day.4
Because it appears that lower heart rate variability may be used to predict an increased risk of coronary heart disease,25 mortality and arrhythmic events, evidence that 4 g/day of EPA and DHA (about 1.5% of daily energy intake) may increase heart rate variability in survivors of myocardial infarction is of interest.26 Heart rate variability, a noninvasive marker of autonomic nervous system function, is reduced with sympathetic predominance and other factors (including reduced baroflex sensitivity) that may be favourably modified by omega-3 fatty acids. Dietary supplementation with fish oil enriched with EPA and DHA (up to 3–4 g omega-3/day) has also been reported to enhance systemic large-artery endothelial function as measured in male subjects with hyperlipidemia by ultrasonic vessel wall tracking.19
Consumption of EPA and DHA at levels approaching 2 g/day is similar to that seen in large sectors of the Japanese population and well below the intakes of the Greenland Inuit. Intakes of about 3–4 g of EPA and DHA per day have resulted in a moderate increase in bleeding times that are generally lower than those seen with ASA therapy. Particular attention should be given to hemostatic factors in patients on high-dose EPA and DHA who are also receiving therapy that affects blood coagulation and thrombogenic factors. On rare occasions, mild bouts of diarrhea or other minor gastrointestinal disturbances are sometimes seen with the use of encapsulated fish oil supplementation.
What about ALA?
For those who do not consume fish, the omega-3 fatty acid known as ALA can be a dietary source of some metabolically derived EPA and DHA. The desaturation plus elongation reactions in the liver and elsewhere in the body that provide for the conversion of dietary ALA to EPA and DHA are depicted in Fig. 4. The conversion of ALA to EPA and DHA occurs to a low extent (about 10%–15% efficiency) in the adult human body.27 Nonetheless, there is evidence28 that the benefits of the Mediterranean-type diet after myocardial infarction may be partly caused by the higher intake of ALA (commonly found in nonhydrogenated canola oil, ground flaxseed and other selected ALA-enriched foods). A prospective cohort study (Nurses Health Study) revealed an inverse relation between ALA intakes and the risk of fatal ischemic heart disease among women.29 However, the Zutphen Elderly Study30 did not observe a beneficial effect of dietary ALA on the 10-year risk of coronary artery disease. The metabolic conversion of ALA to the longer chain omega-3 fatty acids (EPA and DHA) is thought to mediate any possible cardioprotective effects of dietary ALA. In contrast to the well-recognized serum triglyceride-lowering effect of EPA and DHA, most human intervention studies with ALA (e.g., using flaxseed oil) have not exhibited any lipid-lowering effects. Whereas ALA (from flaxseed oil) at a relatively high dose has been found to improve arterial compliance,31 considerably lower supplementation levels of EPA and DHA improved arterial and endothelial functioning in subjects with hypercholesterolemia19 and subjects with type 2 diabetes mellitus.32
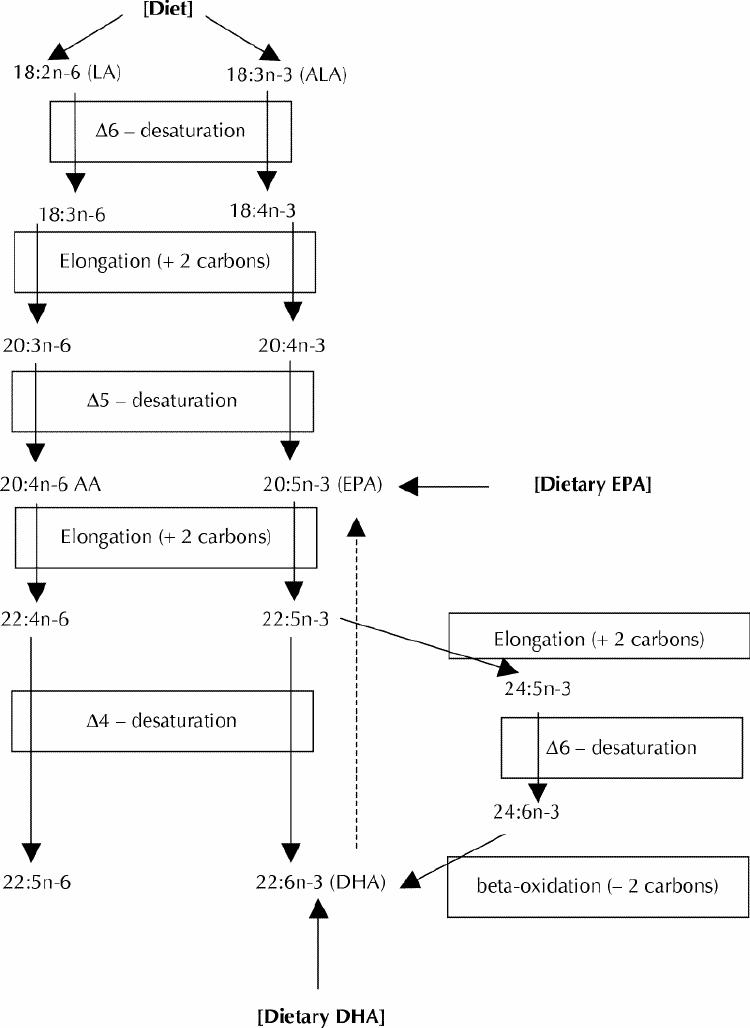
Fig. 4: Desaturation, elongation and retroconversion of polyunsaturated fatty acids.
Clinical trials with fish oil supplements and “hard” end points
Recent studies have focused upon the potential for fish oil supplements (enriched with EPA and DHA) to modify clinical end points in patients with respect to coronary atherosclerosis and myocardial infarctions. A European study of the effect of dietary omega-3 fatty acids on coronary atherosclerosis (measured via coronary angiography) in patients with cardiovascular disease using a randomized, double-blind, placebo-controlled trial has been reported.33 This study revealed that patients with coronary artery disease given omega-3 (EPA and DHA) therapy (at levels of about 1.5 g/day) over 2 years had moderately less progression and more regression of coronary artery disease (discernible, modest mitigation of atherosclerosis) than did patients on placebo. Fewer clinical cardiovascular events (fatal and nonfatal myocardial infarctions, stroke) were noted in the omega-3 group. The omega-3 supplementation was considered safe and well tolerated. Very recently, the 1999 GISSI-Prevenzione trial results have been reported from Italy.6 In this study, 11 324 patients who had experienced a myocardial infarction were assigned to supplemental interventions following the introduction of a Mediterranean-type diet (which included moderate fish consumption), as well as aggressive treatment with various pharmaceutical agents for cardiovascular care. About half the patients received an encapsulated omega-3 fish oil supplementation (providing 850–882 mg/day EPA plus DHA). Over the subsequent interval (3.5 years), the individuals who received omega-3 supplements were found to exhibit a significant reduction in overall cardiovascular deaths and a reduction in sudden cardiac death of about 45%. Vitamin E (α-tocopherol) supplementation, which was also studied in this trial, was without significant effect in this regard. These findings support the concept that, independent of blood cholesterol lowering, EPA and DHA intakes (including supplementation) can favourably influence mortality related to cardiovascular disease (particularly sudden cardiac death) via various mechanisms including antiarrhythmic effects (Table 2).
Target intakes of EPA and DHA for cardiovascular health
The mean current daily intake of EPA and DHA combined in a typical North American diet (which includes about one fish serving every 10 days) approaches 130 mg/day, which is about 0.15% of total dietary fat intake.8 Most dietary EPA and DHA is consumed in the form of fish or seafood. This dietary intake is markedly lower than Japanese intakes and only a small fraction of the EPA and DHA consumed by the Greenland and Nunavik Inuit. Fish consumed 2.5–3 times per week would provide a combined intake of about 500 mg EPA and DHA per day. This intake is about 4 times that of current North American consumption rates. Epidemiological data from the Multiple Risk Factor Intervention Trial in the United States have indicated that progressively higher intakes of the fish-derived omega-3 fatty acids (up to about 665 mg/day) over 10.5 years were associated with a progressive reduction in mortality related to coronary heart disease, as well as total mortality with no associated increase in total cancer-related mortality.34 A recent review of the existing evidence indicated that an increase in the consumption of fish may contribute to lower colorectal cancer and breast cancer risks.35
In summary, there is evidence for the beneficial effect of regular fish consumption (up to 2–3 times/week) both in healthy subjects and in those at considerable risk for coronary artery disease or with established coronary artery disease. Fried or processed fish containing partially hydrogenated fats (“trans” fatty acids) and salted or pickled fish, should be avoided. A National Institutes of Health workshop held in 1999 resulted in the recommendation of a combined average EPA and DHA intake of 650 mg/day for healthy adults.36 The newly released American Heart Association guidelines37 included the following recommendations with respect to omega-3 fatty acid supplements: “Consumption of 1 fatty fish meal per day (or alternatively, a fish oil supplement) could result in an ω3 fatty acid intake (ie, EPA and DHA) of ~900mg/d, an amount shown to beneficially affect coronary heart disease mortality rates in patients with coronary disease.” Current mean intakes (adults) of EPA and DHA (combined) are about 130 mg/d or 14%–20% of these target intakes of 650 mg/d and 900 mg/d.
Future perspectives in cardiovascular care
Future nutrition labelling and health claims should provide both listings for the omega-3 fatty acids of interest (ALA, EPA and DHA) and evidence-based health claims for EPA and DHA related to lowering of blood triglyceride levels, heart health and so on. Omega-3-enriched supplements (nutraceuticals) and functional foods (e.g., EPA- and DHA-enriched eggs and other food products) with effective quantities of EPA and DHA in various forms will become increasingly available as complementary options to fish. Significant blood triglyceride lowering has been recently reported38 in subjects fed 1000 kJ/day (240 kcal/day, that is about 10% of total daily energy intake) of a commercial liquid scrambled egg–type product containing EPA and DHA. These and other such products will offer the possibility of an overall increase in the daily consumption of EPA and DHA, which are currently consumed only in moderate quantities in the form of fish and fish oil, thereby narrowing the current nutritional gap. Clinicians and other health professionals will need to become fully educated about the evidence-based use of omega-3 fatty acids from fish oils (dose, duration, expected benefits, monitoring and so on) in the management of cardiovascular care. “Omega-3 therapeutics” will offer alternative as well as complementary options and strategies for the informed practitioner.
Treatment for the patient
Returning to the case, the physician learns that the patient rarely eats fish. It would be reasonable to suggest to the patient that he increase his intake of fish to 3 servings per week. He should also be advised to consume fish that is broiled or baked, while avoiding breaded fish products or fish sticks, fish and chips, and heavily salted or pickled fish. Depending upon the patient's preference, fish oil supplements (taken with meals) or functional food sources (e.g., liquid egg enriched in omega-3 PUFA) can serve as alternative dietary sources of the target 650–900 mg combined EPA and DHA average daily intake (Table 1).
Articles to date in this series .
Hoffer LJ. Clinical nutrition: 1. Protein–energy malnutrition in the inpatient. CMAJ 2001;165(10):1345-9.
Atkinson SA, Ward WE. Clinical nutrition: 2. The role of nutrition in the prevention and treatment of adult osteoporosis. CMAJ 2001;165(11):1511-4.
Young SN. Clinical nutrition: 3. The fuzzy boundary between nutrition and psychopharmacology. CMAJ 2002;166(2):205-9.
Footnotes
This series is supported, in part, by an unrestricted educational grant from the Danone Institute of Canada.
This article has been peer reviewed.
Acknowledgements: I wish to thank Ms. Patricia Swidinsky for her clerical work on this manuscript and Mr. Ken Stark for providing the structural configurations used in Fig. 1. I would like to dedicate this manuscript to the life and loving memory of Mr. Tom Holub.
Competing interests: Dr. Holub is a member of the Scientific Advisory Board for Ocean Nutrition Canada and received payment for attending a board meeting in 2000.
Correspondence to: Dr. Bruce J. Holub, Department of Human Biology and Nutritional Sciences, University of Guelph, Guelph ON N1G 2W1; fax 519 763-5902; bholub@uoguelph.ca
References
- 1.Holub BJ. Fish oils and cardiovascular disease. CMAJ 1989;141:1063. [PMC free article] [PubMed]
- 2.Connor WE. The importance of n-3 fatty acids in health and disease. Am J Clin Nutr 2000;71(1 Suppl):171S-5S. [DOI] [PubMed]
- 3.Angerer P, von Schacky C. n-3 Polyunsaturated fatty acids and the cardiovascular system. Curr Opin Lipidol 2000;11(1):57-63. [DOI] [PubMed]
- 4.Schmidt EB, Skou HA, Christensen JH, Dyerberg J. n-3 Fatty acids from fish and coronary artery disease: implications for public health. Public Health Nutr 2000;3(1):91-8. [DOI] [PubMed]
- 5.von Schacky C. n-3 Fatty acids and the prevention of coronary atherosclerosis. Am J Clin Nutr 2000;71(1 Suppl):224S-7S. [DOI] [PubMed]
- 6.GISSI-Prevenzione Investigators. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: results of the GISSI-Prevenzione trial. Lancet 1999;354:447-55. [PubMed]
- 7.Raper NR, Cronin FJ, Exler J. Fatty acid content in the US food supply. J Am Coll Nutr 1992;11:304-8. [DOI] [PubMed]
- 8.Kris-Etherton PM, Taylor DS, Yu-Poth S, Huth P, Moriarty K, Fishell V, et al. Polyunsaturated fatty acids in the food chain in the United States. Am J Clin Nutr 2000;71(Suppl 1):179-88. [DOI] [PubMed]
- 9.Department of Health and Welfare. Nutrient recommendations: the report of the scientific review committee. Ottawa: The Department; 1990.
- 10.Hilakivi-Clarke L, Onojafe I, Raygada M, Cho E, Clarke R, Lippman ME. Breast cancer risk in rats fed a diet high in n-6 polyunsaturated fatty acids during pregnancy. J Natl Cancer Inst 1996;18:1821-7. [DOI] [PubMed]
- 11.Zock PL, Katan MB. Linoleic acid intake and cancer risk: a review and meta-analysis. Am J Clin Nutr 1998;68:142-53. [DOI] [PubMed]
- 12.Bang HO, Dyerberg J. Lipid metabolism and ischemic heart disease in Greenland Eskimos. In: Draper HH, editor. Advances in nutrition research. New York: Plenum Publishing; 1980. p. 1-22.
- 13.Blanchet C, Dewailly E, Ayotte P, Bruneau S, Receveur O, Holub BJ. Contribution of selected traditional and market foods to the diet of Nunavik Inuit women. Can J Diet Pract Res 2000;61:50-9. [PubMed]
- 14.Menotti A, Kromhout D, Blackburn H, Fidanza F, Buzina R, Nissinen A. Food intake patterns and 25-year mortality from coronary heart disease: cross-cultural correlations in the Seven Countries Study. The Seven Countries Study Research Group. Eur J Epidemiol 1999:15:507-15. [DOI] [PubMed]
- 15.Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: Diet And Reinfarction Trial (DART). Lancet 1989;2:757-61. [DOI] [PubMed]
- 16.Daviglus ML, Jeremiah S, Orencia AJ, Dyer AR, Liu K, Greenland P, et al. Fish consumption and the 30-year risk of fatal myocardial infarction. N Engl J Med 1997;336:1046-53. [DOI] [PubMed]
- 17.Simon JA, Hodgkins ML, Browner WS, Neuhaus JM, Bernert JT, Hulley SB. Serum fatty acids and the risk of coronary heart disease. Am J Epidemiol 1995; 142:469-76. [DOI] [PubMed]
- 18.Dewailly E, Blanchet C, Lemieux S, Sauve L, Gingras S, Ayotte P, et al. n-3 Fatty acids and cardiovascular disease risk factors among the Inuit of Nunavik. Am J Clin Nutr 2001;74:464-73. [DOI] [PubMed]
- 19.Goodfellow J, Bellamy MF, Ramsey MW, Jones CJH, Lewis MJ. Dietary supplementation with marine omega-3 fatty acids improve systemic large artery endothelial function in subjects with hypercholesterolemia. J Am Coll Cardiol 2000;35(2):265-70. [DOI] [PubMed]
- 20.Harris WS. Fish oils and plasma lipid and lipoprotein metabolism in humans: a critical review. J Lipid Res 1989;30:785-807. [PubMed]
- 21.Jeppesen J, Hein HO, Suadicani P, Gyntelberg F. Triglyceride concentration and ischemic heart disease: an eight-year follow-up in the Copenhagen Male Study. Circulation 1998;97:1029-36. [DOI] [PubMed]
- 22.Stark KD, Park EJ, Maines VA, Holub BJ. Effect of a fish-oil concentrate on serum lipids in postmenopausal women receiving and not receiving hormone replacement therapy in a placebo-controlled, double-blind trial. Am J Clin Nutr 2000;72:389-94. [DOI] [PubMed]
- 23.Nordoy A, Bonna KH, Sandset PM, Hansen JB, Nilsen H. Effect of omega-3 fatty acids and simvastatin on hemastatic risk factors and postprandial hyperlipemia in patients with combined hyperlipemia. Arterioscler Thromb Vasc Biol 2000;20(1):259-65. [DOI] [PubMed]
- 24.Leaf A, Kang JX, Xiao YF, Billman GE, Voskuyl RA. The antiarrhythmic and anticonvulsant effects of dietary n-3 fatty acids. J Membr Biol 1999;172:1-11. [DOI] [PubMed]
- 25.Dekker JM, Crow RS, Folsom AR, Hannan PJ, Liao D, Swenne CA, et al. Low heart rate variability in a 2-minute rhythm strip predicts risk of coronary heart disease and mortality from several causes: the ARIC Study. Circulation 2000;102(11):1239-44. [DOI] [PubMed]
- 26.Christensen JH, Gustenhoff P, Korup E, Aaroe J, Toft E, Moller T, et al. Effect of fish oil on heart rate variability in survivors of myocardial infarction: a double blind randomised controlled trial. BMJ 1996;312(7032):677-8. [DOI] [PMC free article] [PubMed]
- 27.Emken EA, Adlof RO, Gulley RM. Dietary linoleic acid influences desaturation and acylation of deuterium-labeled linoleic acids in young adult males. Biochim Biophys Acta 1994;1213:277-88. [DOI] [PubMed]
- 28.de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 1999;99:779-85. [DOI] [PubMed]
- 29.Hu FB, Stampfer MJ, Manson JE, Rimm EB, Wolk A, Colditz GA, et al. Dietary intake of α-linolenic acid and risk of fatal ischemic heart disease among women. Am J Clin Nutr 1999;69:890-7. [DOI] [PubMed]
- 30.Oomen CM, Ocke, MC, Feskens, E, Kok FJ, Kromhout D. α-Linolenic acid intake is not beneficially associated with 10-yr risk of coronary artery disease incidence: the Zutphen Elderly Study. Am J Clin Nutr 2001;74:457-63. [DOI] [PubMed]
- 31.Nestel PJ, Pomeroy SE, Sasahara T, Yamashita T, Liang YL, Dart AM, et al. Arterial compliance in obese subjects is improved with dietary plant fatty acid from flaxseed oil despite increased LDL oxidizability. Arterioscler Thromb Vasc Biol 1997;17:1163-70. [DOI] [PubMed]
- 32.McVeigh GE, Brennan GM, Cohn JN, Finkelstein SM, Hayes RJ. Fish oil improves arterial compliance in non-insulin-dependent diabetes mellitus. Arterioscler Thromb 1994;14:1425-9. [DOI] [PubMed]
- 33.von Schacky C, Angerer P, Kothny W, Theisen K, Mudra H. The effect of dietary omega-3 fatty acids on coronary atherosclerosis: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 1999;130:554-62. [DOI] [PubMed]
- 34.Dolecek TA. Epidemiological evidence of relationships between dietary polyunsaturated fatty acids and mortality in the Multiple Risk Factor Intervention Trial. Proc Soc Expt Biol Med 1992;200:177-82. [DOI] [PubMed]
- 35.de Deckere EA. Possible beneficial effect of fish and fish n-3 polyunsaturated fatty acids in breast and colorectal cancer. Eur J Cancer Prev 1999;8:213-21. [DOI] [PubMed]
- 36.Simopoulos AP, Leaf A, Salem N. Essentiality of and recommended dietary intakes for omega-6 and omega-3 fatty acids. Ann Nutr Metab 1999;43:127-30. [DOI] [PubMed]
- 37.Krauss RM, Eckel RH, Howard B, Appel, LJ, Daniels SR, Deckelbaum RJ, et al. AHA Dietary Guidelines: revision 2000: a statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation 2000;102(18):2284-99. [DOI] [PubMed]
- 38.Rose E, Holub BJ. The effect of an emulsified egg product containing fish oil on selected cardiovascular risk factors [abstract]. American Oil Chemists' Society Annual Meeting; 2001 May 14–16; Minneapolis.


